Multi-Omics Endotypes in ICU Sepsis-Induced Immunosuppression
Abstract
1. Introduction
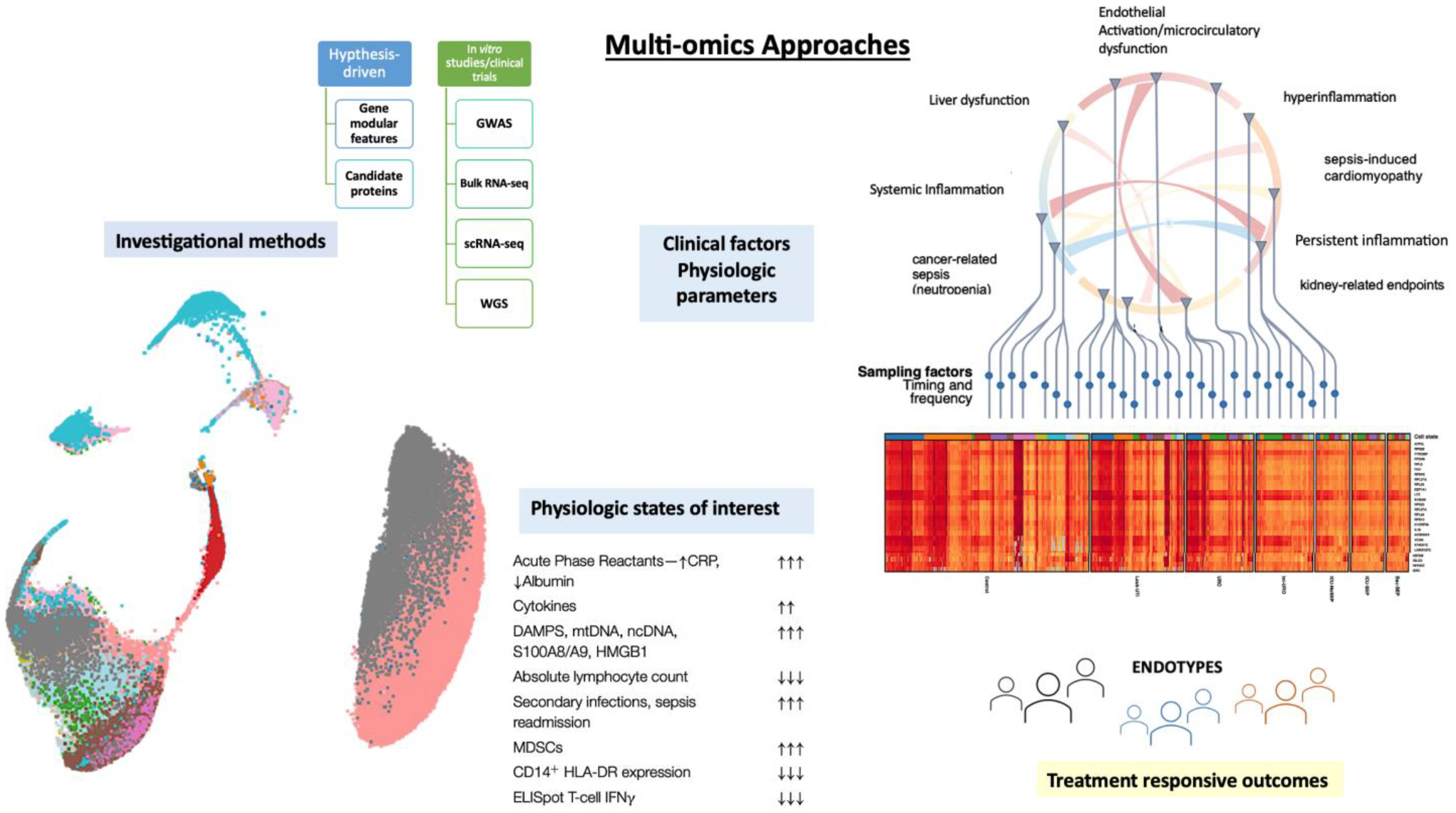
2. Multi-Omics Single-Cell Data Integration for Immunological Profiling
2.1. The Identification of Deleterious Neutrophil States and Altered Granulopoiesis in Sepsis
2.2. Transcriptomic Driven Endotype in Sepsis Immunocompromised Patients
2.3. Transcriptomic Landscape of Chronic Critical Illness in Late Sepsis
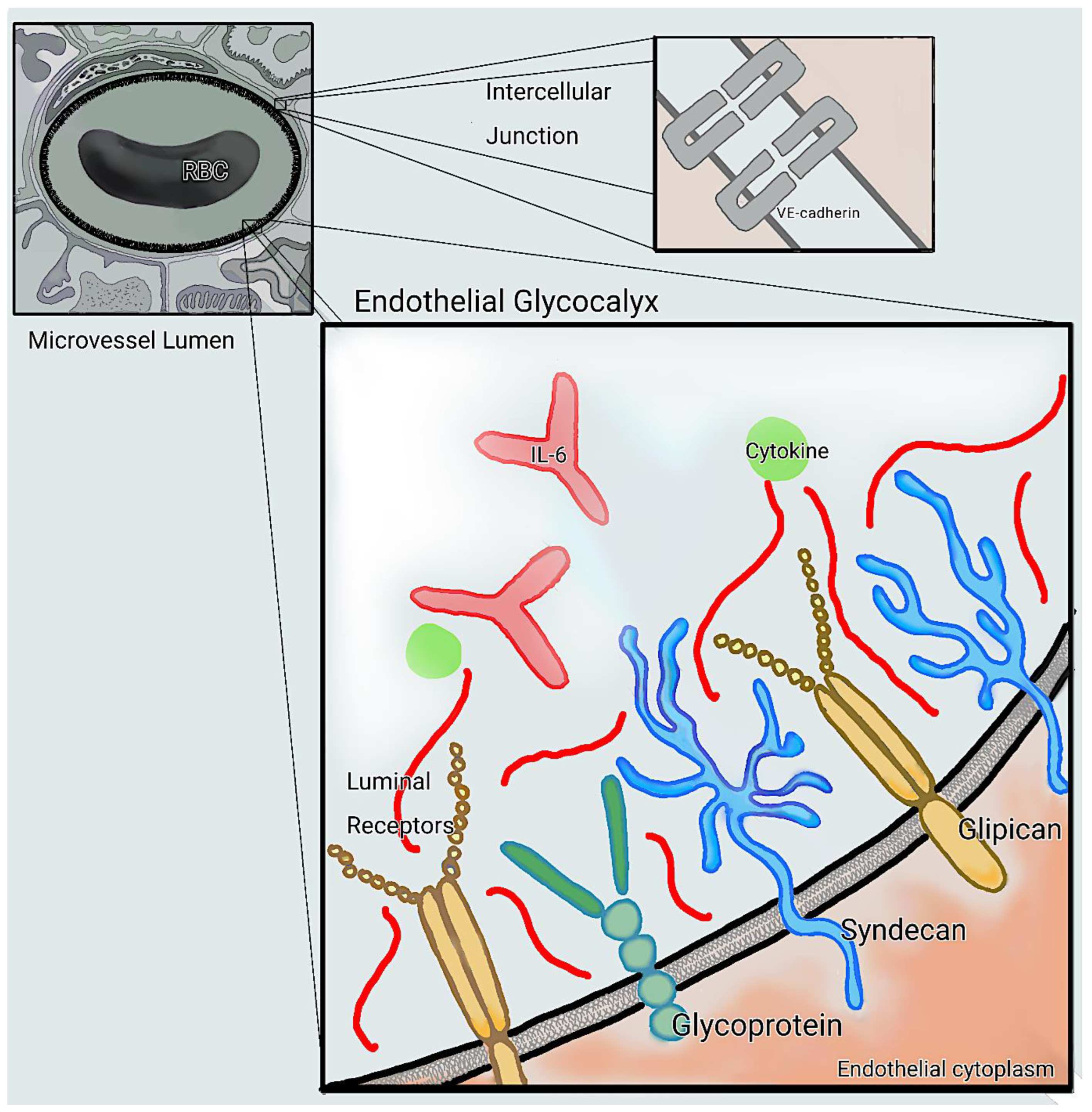
3. Omics of Endothelial Dysfunction and Microcirculatory Alterations
3.1. Sepsis-Induced Metabolic Changes and Microcirculatory Damage
3.2. Biomarkers of Endothelial Damage to Assess Treatment Response in Critical Illness
4. Gene Modular Features Informing Clinically Relevant Endotypes
4.1. Hepatic Injury Dysregulation in Sepsis
4.2. Sepsis Induced Cardiomyopathy (SICM) Gene Modular Features
5. Continuous Metrics Measuring Endotypes and Clinical Response in ICU
5.1. Transcriptomic and Immunological Metrics Guiding Immunotherapy
5.2. Pharmacologic Immune Modulation in Sepsis
6. Conclusions
Funding
Conflicts of Interest
References
- Fleischmann-Struzek, C.; Mellhammar, L.; Rose, N.; Cassini, A.; Rudd, K.E.; Schlattmann, P.; Allegranzi, B.; Reinhart, K. Incidence and mortality of hospital-and ICU-treated sepsis: Results from an updated and expanded systematic review and meta-analysis. Intensive Care Med. 2020, 46, 1552–1562. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, T.E.; Liesenfeld, O.; Wacker, J.; He, Y.D.; Rawling, D.; Remmel, M.; Coyle, S.; Midic, U.; Kotsaki, A.; Kanavou, A.; et al. Validation of Inflammopathic, Adaptive, and Coagulopathic Sepsis Endotypes in Coronavirus Disease 2019. Crit. Care Med. 2021, 49, e170–e178. [Google Scholar] [CrossRef] [PubMed]
- DeMerle, K.M.; Angus, D.C.M.; Baillie, J.K.M.; Brant, E.; Calfee, C.S.M.; Carcillo, J.; Chang, C.-C.H.; Dickson, R.; Evans, I.M.; Gordon, A.C.; et al. Sepsis Subclasses: A Framework for Development and Interpretation. Crit. Care Med. 2021, 49, 748–759. [Google Scholar] [CrossRef] [PubMed]
- Grondman, I.; Koeken, V.; Karageorgos, A.; Li, W.; Antonakos, N.; Zhang, B.; Damoraki, G.; Xu, C.J.; Giamarellos-Bourboulis, E.; Li, Y.; et al. Single-cell transcriptomics identifies different immune signatures between macrophage activation-like syndrome and immune paralysis in sepsis. Medrxiv 2023. [Google Scholar] [CrossRef]
- Pelaia, T.M.; Shojaei, M.; McLean, A.S. The Role of Transcriptomics in Redefining Critical Illness. Crit. Care 2023, 27, 89. [Google Scholar] [CrossRef]
- Zimmerman, J.J. Fccm The Classic Critical Care Conundrum Encounters Precision Medicine*. Pediatr. Crit. Care Med. 2023, 24, 251–253. [Google Scholar] [CrossRef]
- Muriello, M.; Basel, D. Rapid Exome and Genome Sequencing in the Intensive Care Unit. Crit. Care Clin. 2022, 38, 173–184. [Google Scholar] [CrossRef]
- Chien, J.-Y.; Yu, C.-J.; Hsueh, P.-R. Utility of Metagenomic Next-Generation Sequencing for Etiological Diagnosis of Patients with Sepsis in Intensive Care Units. Microbiol. Spectr. 2022, 10, e0074622. [Google Scholar] [CrossRef]
- Wang, C.; Li, Y.; Li, S.; Chen, M.; Hu, Y. Proteomics Combined with RNA Sequencing to Screen Biomarkers of Sepsis. Infect. Drug Resist. 2022, 15, 5575–5587. [Google Scholar] [CrossRef]
- Martinez, G.S.; Ostadgavahi, A.T.; Al-Rafat, A.M.; Garduno, A.; Cusack, R.; Bermejo-Martin, J.F.; Martin-Loeches, I.; Kelvin, D. Model-interpreted outcomes of artificial neural networks classifying immune biomarkers associated with severe infections in ICU. Front. Immunol. 2023, 14, 1137850. [Google Scholar] [CrossRef]
- Bai, Y.; Xia, J.; Huang, X.; Chen, S.; Zhan, Q. Using machine learning for the early prediction of sepsis-associated ARDS in the ICU and identification of clinical phenotypes with differential responses to treatment. Front. Physiol. 2022, 13, 2591. [Google Scholar] [CrossRef] [PubMed]
- Tyler, S.R.; Chun, Y.; Ribeiro, V.M.; Grishina, G.; Grishin, A.; Hoffman, G.E.; Do, A.N.; Bunyavanich, S. Merged Affinity Network Association Clustering: Joint multi-omic/clinical clustering to identify disease endotypes. Cell Rep. 2021, 35, 108975. [Google Scholar] [CrossRef] [PubMed]
- Kyriazopoulou, E.; on behalf of the Hellenic Sepsis Study Group; Leventogiannis, K.; Norrby-Teglund, A.; Dimopoulos, G.; Pantazi, A.; Orfanos, S.E.; Rovina, N.; Tsangaris, I.; Gkavogianni, T.; et al. Macrophage activation-like syndrome: An immunological entity associated with rapid progression to death in sepsis. BMC Med. 2017, 15, 172. [Google Scholar] [CrossRef] [PubMed]
- Gómez, H.; Anderko, R.R.; Carcillo, J.A. Identifying inflammatory phenotypes to target mechanism-specific treatments in sepsis. Cell Rep. Med. 2022, 3, 100823. [Google Scholar] [CrossRef]
- Bodinier, M.; Peronnet, E.; Brengel-Pesce, K.; Conti, F.; Rimmelé, T.; Textoris, J.; Vedrine, C.; Quemeneur, L.; Griffiths, A.D.; Tan, L.K.; et al. Monocyte Trajectories Endotypes Are Associated With Worsening in Septic Patients. Front. Immunol. 2021, 12, 795052. [Google Scholar] [CrossRef]
- Sadaka, F.; EthmaneAbouElMaali, C.; Cytron, M.A.; Fowler, K.; Javaux, V.M.; O’brien, J. Predicting Mortality of Patients With Sepsis: A Comparison of APACHE II and APACHE III Scoring Systems. J. Clin. Med. Res. 2017, 9, 907–910. [Google Scholar] [CrossRef]
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A. Assessment of clinical criteria for sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 762–774. [Google Scholar] [CrossRef]
- Sinapidis, D.; Kosmas, V.; Vittoros, V.; Koutelidakis, I.M.; Pantazi, A.; Stefos, A.; Katsaros, K.E.; Akinosoglou, K.; Bristianou, M.; Toutouzas, K.; et al. Progression into sepsis: An individualized process varying by the interaction of comorbidities with the underlying infection. BMC Infect. Dis. 2018, 18, 242. [Google Scholar] [CrossRef]
- Leijte, G.P.; Rimmelé, T.; Kox, M.; Bruse, N.; Monard, C.; Gossez, M.; Monneret, G.; Pickkers, P.; Venet, F. Monocytic HLA-DR expression kinetics in septic shock patients with different pathogens, sites of infection and adverse outcomes. Crit. Care 2020, 24, 110. [Google Scholar] [CrossRef]
- Davenport, E.E.; Burnham, K.L.; Radhakrishnan, J.; Humburg, P.; Hutton, P.; Mills, T.C.; Rautanen, A.; Gordon, A.C.; Garrard, C.; Hill, A.V.; et al. Genomic landscape of the individual host response and outcomes in sepsis: A prospective cohort study. Lancet Respir. Med. 2016, 4, 259–271. [Google Scholar] [CrossRef]
- Kwok, A.J.; Allcock, A.; Ferreira, R.C.; Smee, M.; Cano-Gamez, E.; Burnham, K.L.; Zurke, Y.-X.; McKechnie, S.; Monaco, C.; Udalova, I.; et al. Identification of deleterious neutrophil states and altered granulopoiesis in sepsis. Medrxiv 2022. [Google Scholar] [CrossRef]
- Shakoory, B.; Carcillo, J.A.; Chatham, W.W.; Amdur, R.L.; Zhao, H.; Dinarello, C.A.; Opal, S.M. Interleukin-1 receptor blockade is associated with reduced mortality in sepsis patients with features of the macrophage activation syndrome: Re-analysis of a prior Phase III trial. Crit. Care Med. 2016, 44, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Steinhagen, F.; Schmidt, S.V.; Schewe, J.-C.; Peukert, K.; Klinman, D.M.; Bode, C. Immunotherapy in sepsis—Brake or accelerate? Pharmacol. Ther. 2020, 208, 107476. [Google Scholar] [CrossRef]
- Nathan, N.; Sculier, J.P.; Ameye, L.; Paesmans, M.; Bogdan-Dragos, G.; Meert, A.P. Sepsis and septic shock definitions in patients with cancer admitted in ICU. J. Intensive Care Med. 2021, 36, 255–261. [Google Scholar] [CrossRef]
- Camou, F.; Didier, M.; Leguay, T.; Milpied, N.; Daste, A.; Ravaud, A.; Mourissoux, G.; Guisset, O.; Issa, N. Long-term prognosis of septic shock in cancer patients. Support. Care Cancer 2019, 28, 1325–1333. [Google Scholar] [CrossRef]
- Gudiol, C.; Albasanz-Puig, A.; Cuervo, G.; Carratalà, J. Understanding and Managing Sepsis in Patients With Cancer in the Era of Antimicrobial Resistance. Front. Med. 2021, 8, 636547. [Google Scholar] [CrossRef] [PubMed]
- Alkhateeb, T. Development, Expansion and Role of Myeloid-Derived Suppressor Cells in Post-Sepsis Immune Suppression. Doctoral Dissertation, East Tennessee State University, Johnson City, TN, USA, 2020. [Google Scholar]
- Washburn, M.L.; Wang, Z.; Walton, A.H.; Goedegebuure, S.P.; Figueroa, D.J.; Van Horn, S.; Grossman, J.; Remlinger, K.; Madsen, H.; Brown, J.; et al. T Cell– and Monocyte-Specific RNA-Sequencing Analysis in Septic and Nonseptic Critically Ill Patients and in Patients with Cancer. J. Immunol. 2019, 203, 1897–1908. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-W.; Bennion, K.B.; Swift, D.A.; Morrow, K.N.; Zhang, W.; Oami, T.; Coopersmith, C.M.; Ford, M.L. Tumor-Specific T Cells Exacerbate Mortality and Immune Dysregulation during Sepsis. J. Immunol. 2021, 206, 2412–2419. [Google Scholar] [CrossRef]
- Vigneron, C.; Mirouse, A.; Merdji, H.; Rousseau, C.; Cousin, C.; Alby-Laurent, F.; Mira, J.-P.; Chiche, J.-D.; Llitjos, J.-F.; Pène, F. Sepsis inhibits tumor growth in mice with cancer through Toll-like receptor 4-associated enhanced Natural Killer cell activity. Oncoimmunology 2019, 8, e1641391. [Google Scholar] [CrossRef]
- Riché, F.; Chousterman, B.G.; Valleur, P.; Mebazaa, A.; Launay, J.-M.; Gayat, E. Protracted immune disorders at one year after ICU discharge in patients with septic shock. Crit. Care 2018, 22, 42. [Google Scholar] [CrossRef]
- Shankar-Hari, M.; Saha, R.; Wilson, J.; Prescott, H.C.; Harrison, D.; Rowan, K.; Rubenfeld, G.D.; Adhikari, N.K.J. Rate and risk factors for rehospitalisation in sepsis survivors: Systematic review and meta-analysis. Intensive Care Med. 2020, 46, 619–636. [Google Scholar] [CrossRef] [PubMed]
- Calsavara, A.J.; Nobre, V.; Barichello, T.; Teixeira, A.L. Post-sepsis cognitive impairment and associated risk factors: A systematic review. Aust. Crit. Care 2018, 31, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Fenner, B.P.; Darden, D.B.; Kelly, L.S.; Rincon, J.; Brakenridge, S.C.; Larson, S.D.; Moore, F.A.; Efron, P.A.; Moldawer, L.L. Immunological Endotyping of Chronic Critical Illness After Severe Sepsis. Front. Med. 2021, 7, 616694. [Google Scholar] [CrossRef] [PubMed]
- Darden, D.B.; Ghita, G.L.; Wang, Z.; Stortz, J.A.; Lopez, M.-C.; Cox, M.C.; Hawkins, R.B.; Rincon, J.C.; Kelly, L.S.; Fenner, B.P.; et al. Chronic Critical Illness Elicits a Unique Circulating Leukocyte Transcriptome in Sepsis Survivors. J. Clin. Med. 2021, 10, 3211. [Google Scholar] [CrossRef]
- Darden, D.B.; Dong, X.; Brusko, M.A.; Kelly, L.; Fenner, B.; Rincon, J.C.; Dirain, M.L.; Ungaro, R.; Nacionales, D.C.; Gauthier, M.; et al. A Novel Single Cell RNA-seq Analysis of Non-Myeloid Circulating Cells in Late Sepsis. Front. Immunol. 2021, 12, 696536. [Google Scholar] [CrossRef]
- Darden, D.B.; Bacher, R.; Brusko, M.A.; Knight, P.; Hawkins, R.B.; Cox, M.C.; Dirain, M.L.; Ungaro, R. Single cell RNA-SEQ of human myeloid derived suppressor cells in late sepsis reveals multiple subsets with unique transcriptional responses: A pilot study. Shock 2021, 55, 587. [Google Scholar] [CrossRef]
- Joffre, J.; Hellman, J.; Ince, C.; Ait-Oufella, H. Endothelial responses in sepsis. Am. J. Respir. Crit. Care Med. 2020, 202, 361–370. [Google Scholar] [CrossRef]
- Hasin, Y.; Seldin, M.; Lusis, A. Multi-omics approaches to disease. Genome Biol. 2017, 18, 83. [Google Scholar] [CrossRef]
- Ricaño-Ponce, I.; Riza, A.-L.; de Nooijer, A.H.; Pirvu, A.; Dorobantu, S.; Dragos, A.; Streata, I.; Roskanovic, M.; Grondman, I.; Dumitrescu, F.; et al. Characterization of sepsis inflammatory endotypes using circulatory proteins in patients with severe infection: A prospective cohort study. BMC Infect. Dis. 2022, 22, 778. [Google Scholar] [CrossRef]
- Mazer, M.B.; Caldwell, C.; Hanson, J.; Mannion, D.; Turnbull, I.R.; Drewry, A.; Osborne, D.; Walton, A.; Blood, T.; Moldawer, L.L.; et al. A whole blood enzyme-linked immunospot assay for functional immune endotyping of septic patients. J. Immunol. 2021, 206, 23–36. [Google Scholar] [CrossRef]
- Astapenko, D.; Benes, J.; Cerny, V. Clinical Relevance of the Endothelial Glycocalyx in Critically Ill Patients. Annu. Update Intensive Care Emerg. Med. 2020, 2020, 213–222. [Google Scholar] [CrossRef]
- Alphonsus, C.S.; Rodseth, R. The endothelial glycocalyx: A review of the vascular barrier. Anaesthesia 2014, 69, 777–784. [Google Scholar] [CrossRef] [PubMed]
- An, G.; Nieman, G.; Vodovotz, Y. Computational and systems biology in trauma and sepsis: Current state and future perspectives. Int. J. Burn. Trauma 2012, 2, 1. [Google Scholar]
- Olivier, M.; Asmis, R.; Hawkins, G.A.; Howard, T.D.; Cox, L.A. The Need for Multi-Omics Biomarker Signatures in Precision Medicine. Int. J. Mol. Sci. 2019, 20, 4781. [Google Scholar] [CrossRef]
- Langston, J.C.; Rossi, M.T.; Yang, Q.; Ohley, W.; Perez, E.; E Kilpatrick, L.; Prabhakarpandian, B.; Kiani, M.F. Omics of endothelial cell dysfunction in sepsis. Vasc. Biol. 2022, 4, R15–R34. [Google Scholar] [CrossRef]
- Itenov, T.S.; Murray, D.D.; Jensen, J.U.S. Sepsis: Personalized Medicine Utilizing ‘Omic’ Technologies—A Paradigm Shift? Healthcare 2018, 6, 111. [Google Scholar] [CrossRef]
- Alsaffar, H.; Martino, N.; Garrett, J.P.; Adam, A.P. Interleukin-6 promotes a sustained loss of endothelial barrier function via Janus kinase-mediated STAT3 phosphorylation and de novo protein synthesis. Am. J. Physiol. Physiol. 2018, 314, C589–C602. [Google Scholar] [CrossRef] [PubMed]
- Murakami, M.; Kamimura, D.; Hirano, T. Pleiotropy and Specificity: Insights from the Interleukin 6 Family of Cytokines. Immunity 2019, 50, 812–831. [Google Scholar] [CrossRef]
- Amalakuhan, B.; Habib, S.A.; Mangat, M.; Reyes, L.F.; Rodriguez, A.H.; Hinojosa, C.A.; Soni, N.J.; Gilley, R.P.; Bustamante, C.A.; Anzueto, A.; et al. Endothelial adhesion molecules and multiple organ failure in patients with severe sepsis. Cytokine 2016, 88, 267–273. [Google Scholar] [CrossRef]
- Leone, M.; Boutière, B.; Camoin-Jau, L.; Albanèse, J.; Horschowsky, N.; Mège, J.-L.; Martin, C.; Dignat-George, F. Systemic endothelial activation is greater in septic than in traumatic-hemorrhagic shock but does not correlate with endothelial activation in skin biopsies. Crit. Care Med. 2002, 30, 808–814. [Google Scholar] [CrossRef]
- Murakami, J.; Ohtani, A.; Murata, S. Protective effect of T-686, an inhibitor of plasminogen activator inhibitor-1 production, against the lethal effect of lipopolysaccharide in mice. Jpn. J. Pharmacol. 1997, 75, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Renckens, R.; Roelofs, J.J.T.H.; Bonta, P.I.; Florquin, S.; de Vries, C.J.M.; Levi, M.; Carmeliet, P.; Veer, C.V.; van der Poll, T. Plasminogen activator inhibitor type 1 is protective during severe Gram-negative pneumonia. Blood 2007, 109, 1593–1601. [Google Scholar] [CrossRef]
- Jambusaria, A.; Hong, Z.; Zhang, L.; Srivastava, S.; Jana, A.; Toth, P.T.; Dai, Y.; Malik, A.B.; Rehman, J. Author response: Endothelial heterogeneity across distinct vascular beds during homeostasis and inflammation. Elife 2019, 9, e51413. [Google Scholar] [CrossRef] [PubMed]
- Lipowsky, H.H. Microvascular Rheology and Hemodynamics. Microcirculation 2005, 12, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Burghoff, S.; Schrader, J. Secretome of Human Endothelial Cells under Shear Stress. J. Proteome Res. 2011, 10, 1160–1169. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.-X.; Jiang, H.-L.; Chen, X.-H. Endothelial cell metabolism in sepsis. World J. Emerg. Med. 2023, 14, 10. [Google Scholar] [CrossRef]
- Yang, K.; Fan, M.; Wang, X.; Xu, J.; Wang, Y.; Gill, P.S.; Ha, T.; Liu, L.; Hall, J.V.; Williams, D.L.; et al. Lactate induces vascular permeability via disruption of VE-cadherin in endothelial cells during sepsis. Sci. Adv. 2022, 8, eabm8965. [Google Scholar] [CrossRef]
- Mao, L.; Sun, M.; Chen, Z.; Zeng, Z.; Wu, J.; Chen, Z.; Zhang, W.; Huang, Q. The Pyruvate Dehydrogenase Complex Mitigates LPS-Induced Endothelial Barrier Dysfunction by Metabolic Regulation. Shock. Inj. Inflamm. Sepsis: Lab. Clin. Approaches 2022, 57, 308–317. [Google Scholar] [CrossRef]
- Wang, L.; Cao, Y.; Gorshkov, B.; Zhou, Y.; Yang, Q.; Xu, J.; Ma, Q.; Zhang, X.; Wang, J.; Mao, X.; et al. Ablation of endothelial Pfkfb3 protects mice from acute lung injury in LPS-induced endotoxemia. Pharmacol. Res. 2019, 146, 104292. [Google Scholar] [CrossRef]
- Gill, S.E.; Rohan, M.; Mehta, S. Role of pulmonary microvascular endothelial cell apoptosis in murine sepsis-induced lung injury in vivo. Respir. Res. 2015, 16, 109. [Google Scholar] [CrossRef]
- Wang, Z.; Rui, T.; Yang, M.; Valiyeva, F.; Kvietys, P.R. Alveolar Macrophages from Septic Mice Promote Polymorphonuclear Leukocyte Transendothelial Migration via an Endothelial Cell Src Kinase/NADPH Oxidase Pathway. J. Immunol. 2008, 181, 8735–8744. [Google Scholar] [CrossRef]
- Fatmi, A.; Saadi, W.; Beltrán-García, J.; García-Giménez, J.L.; Pallardó, F.V. The Endothelial Glycocalyx and Neonatal Sepsis. Int. J. Mol. Sci. 2023, 24, 364. [Google Scholar] [CrossRef]
- Goligorsky, M.S.; Sun, D. Glycocalyx in Endotoxemia and Sepsis. Am. J. Pathol. 2020, 190, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.-L.; Pai, M.-H.; Shih, Y.-M.; Shih, J.-M.; Yeh, S.-L. Intravenous Arginine Administration Promotes Proangiogenic Cells Mobilization and Attenuates Lung Injury in Mice with Polymicrobial Sepsis. Nutrients 2017, 9, 507. [Google Scholar] [CrossRef]
- Wijnands, K.A.P.; Hoeksema, M.A.; Meesters, D.M.; van den Akker, N.M.S.; Molin, D.G.M.; Briedé, J.J.; Ghosh, M.; Köhler, S.E.; Van Zandvoort, M.A.M.J.; De Winther, M.P.J.; et al. Arginase-1 Deficiency Regulates Arginine Concentrations and NOS2-Mediated NO Production during Endotoxemia. PLoS ONE 2014, 9, e86135. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-J.; Chan, O.-W.; Hsiao, H.-J.; Wang, Y.; Hsia, S.-H.; Chiu, C.-H. Decreased ADAMTS 13 Activity is Associated with Disease Severity and Outcome in Pediatric Severe Sepsis. Medicine 2016, 95, e3374. [Google Scholar] [CrossRef] [PubMed]
- Anand, D.; Ray, S.; Srivastava, L.M.; Bhargava, S. Evolution of serum hyaluronan and syndecan levels in prognosis of sepsis patients. Clin. Biochem. 2016, 49, 768–776. [Google Scholar] [CrossRef]
- Huang, X.; Hu, H.; Sun, T.; Zhu, W.; Tian, H.; Hao, D.; Wang, T.; Wang, X. Plasma Endothelial Glycocalyx Components as a Potential Biomarker for Predicting the Development of Disseminated Intravascular Coagulation in Patients with Sepsis. J. Intensive Care Med. 2021, 36, 1286–1295. [Google Scholar] [CrossRef]
- Zonda, G.I.; Zonda, R.; Cernomaz, T.A.; Paduraru, L.; Avasiloaiei, A.L.; Grigoriu, B.D. Endocan—A potential diagnostic marker for early onset sepsis in neonates. J. Infect. Dev. Ctries. 2019, 13, 311–317. [Google Scholar] [CrossRef]
- Saldir, M.; Tunc, T.; Cekmez, F.; Cetinkaya, M.; Kalayci, T.; Fidanci, K.; Babacan, O.; Erdem, G.; Kocak, N.; Sari, E.; et al. Endocan and Soluble Triggering Receptor Expressed on Myeloid Cells-1 as Novel Markers for Neonatal Sepsis. Pediatr. Neonatol. 2015, 56, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Ince, C. The microcirculation is the motor of sepsis. Crit. Care 2005, 9, S13–S19. [Google Scholar] [CrossRef]
- De Backer, D.; Creteur, J.; Preiser, J.C.; Dubois, M.J.; Vincent, J.L. Microvascular blood flow is altered in patients with sepsis. Am. J. Respir. Crit. Care Med. 2002, 166, 98–104. [Google Scholar] [CrossRef]
- De Backer, D.; Donadello, K.; Sakr, Y.; Ospina-Tascon, G.; Salgado, D.; Scolletta, S.; Vincent, J.L. Microcirculatory alterations in patients with severe sepsis: Impact of time of assessment and relationship with outcome. Crit. Care Med. 2013, 41, 791–799. [Google Scholar] [CrossRef]
- Dilken, O.; Ergin, B.; Ince, C. Assessment of sublingual microcirculation in critically ill patients: Consensus and debate. Ann. Transl. Med. 2020, 8, 793. [Google Scholar] [CrossRef] [PubMed]
- Cusack, R.; Leone, M.; Rodriguez, A.H.; Martin-Loeches, I. Endothelial Damage and the Microcirculation in Critical Illness. Biomedicines 2022, 10, 3150. [Google Scholar] [CrossRef] [PubMed]
- Leone, M.; Blidi, S.; Antonini, F.; Meyssignac, B.; Bordon, S.; Garcin, F.; Charvet, A.; Blasco, V.; Albanese, J.; Martin, C. Oxygen tissue saturation is lower in nonsurvivors than in survivors after early resuscitation of septic shock. J. Am. Soc. Anesthesiol. 2009, 111, 366–371. [Google Scholar] [CrossRef]
- Pries, A.R.; Secomb, T.W.; Gaehtgens, P. The endothelial surface layer. Pflugers Arch. 2000, 440, 653–666. [Google Scholar] [CrossRef] [PubMed]
- Chelazzi, C.; Villa, G.; Mancinelli, P.; De Gaudio, A.R.; Adembri, C. Glycocalyx and sepsis-induced alterations in vascular permeability. Crit. Care 2015, 19, 26. [Google Scholar] [CrossRef]
- Mehta, D.; Malik, A.B. Signaling mechanisms regulating endothelial permeability. Physiol. Rev. 2006, 86, 279–367. [Google Scholar] [CrossRef]
- Martin-Fernandez, M.; Vaquero-Roncero, L.M.; Almansa, R.; Gómez-Sánchez, E.; Martín, S.; Tamayo, E.; Esteban-Velasco, M.C.; Ruiz-Granado, P.; Aragón, M.; Calvo, D.; et al. Endothelial dysfunction is an early indicator of sepsis and neutrophil degranulation of septic shock in surgical patients. BJS Open 2020, 4, 524–534. [Google Scholar] [CrossRef]
- Fang, Y.; Li, C.; Shao, R.; Yu, H.; Zhang, Q. The role of biomarkers of endothelial activation in predicting morbidity and mortality in patients with severe sepsis and septic shock in intensive care: A prospective observational study. Thromb. Res. 2018, 171, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Ince, C. Personalized physiological medicine. Crit. Care 2017, 21, 308. [Google Scholar] [CrossRef] [PubMed]
- Edul, V.S.K.; Ince, C.; Navarro, N.; Previgliano, L.; Risso-Vazquez, A.; Rubatto, P.N.; Dubin, A. Dissociation between sublingual and gut microcirculation in the response to a fluid challenge in postoperative patients with abdominal sepsis. Ann. Intensive Care 2014, 4, 39. [Google Scholar] [CrossRef] [PubMed]
- Mehta, C.; Gao, P.; Bhatt, D.L.; Harrington, R.A.; Skerjanec, S.; Ware, J.H. Optimizing trial design: Sequential, adaptive, and enrichment strategies. Circulation 2009, 119, 597–605. [Google Scholar] [CrossRef]
- Stanski, N.L.; Wong, H.R. Prognostic and predictive enrichment in sepsis. Nat. Rev. Nephrol. 2019, 16, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Temmesfeld-Wollbrück, B.; Hocke, A.C.; Suttorp, N.; Hippenstiel, S. Adrenomedullin and endothelial barrier function. Thromb. Haemost. 2007, 98, 944–951. [Google Scholar] [CrossRef]
- Tsakadze, N.; Zakaria, R.; Matheson, P.; Garrison, R. Mechanism of adrenomedullin (AM)-mediated vasodilation in rat ileum. Circulation 2006, 16, 775. [Google Scholar] [CrossRef]
- Samson, W.K. Adrenomedullin and the control of fluid and electrolyte homeostasis. Annu. Rev. Physiol. 1999, 61, 363–389. [Google Scholar] [CrossRef]
- Czyzyk, T.A.; Ning, Y.; Hsu, M.-S.; Peng, B.; Mains, R.E.; Eipper, B.A.; Pintar, J.E. Deletion of peptide amidation enzymatic activity leads to edema and embryonic lethality in the mouse. Dev. Biol. 2005, 287, 301–313. [Google Scholar] [CrossRef]
- Isumi, Y.; Shoji, H.; Sugo, S.; Tochimoto, T.; Yoshioka, M.; Kangawa, K.; Matsuo, H.; Minamino, N. Regulation of Adrenomedullin Production in Rat Endothelial Cells. Endocrinology 1998, 139, 838–846. [Google Scholar] [CrossRef]
- Tomoda, Y.; Isumi, Y.; Katafuchi, T.; Minamino, N. Regulation of adrenomedullin secretion from cultured cells. Peptides 2001, 22, 1783–1794. [Google Scholar] [CrossRef] [PubMed]
- Agorreta, J.; Zulueta, J.J.; Montuenga, L.M.; Garayoa, M. Adrenomedullin expression in a rat model of acute lung injury induced by hypoxia and LPS. Am. J. Physiol. Cell. Mol. Physiol. 2005, 288, L536–L545. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Chaudry, I.H.; Wang, P. The small intestine is an important source of adrenomedullin release during polymicrobial sepsis. Am. J. Physiol. Integr. Comp. Physiol. 2001, 281, R654–R660. [Google Scholar] [CrossRef] [PubMed]
- Hocke, A.C.; Temmesfeld-Wollbrueck, B.; Schmeck, B.; Berger, K.; Frisch, E.M.; Witzenrath, M.; Brell, B.; Suttorp, N.; Hippenstiel, S. Perturbation of endothelial junction proteins by Staphylococcus aureus α-toxin: Inhibition of endothelial gap formation by adrenomedullin. Histochem. Cell Biol. 2006, 126, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Struck, J.; Tao, C.; Morgenthaler, N.G.; Bergmann, A. Identification of an Adrenomedullin precursor fragment in plasma of sepsis patients. Peptides 2004, 25, 1369–1372. [Google Scholar] [CrossRef] [PubMed]
- Buendgens, L.; Yagmur, E.; Ginsberg, A.; Weiskirchen, R.; Wirtz, T.; Abu Jhaisha, S.; Eisert, A.; Luedde, T.; Trautwein, C.; Tacke, F.; et al. Midregional Proadrenomedullin (MRproADM) Serum Levels in Critically Ill Patients Are Associated with Short-Term and Overall Mortality during a Two-Year Follow-Up. Mediat. Inflamm. 2020, 2020, 7184803. [Google Scholar] [CrossRef]
- Valenzuela-Sánchez, F.; Valenzuela-Méndez, B.; De Austria, R.B.; Rodríguez-Gutiérrez, J.F.; García, E.; Fernández-Ruiz, L.; González-García, M.; Rello, J. Plasma levels of mid-regional pro-adrenomedullin in sepsis are associated with risk of death. Minerva Anestesiol. 2018, 85, 366–375. [Google Scholar] [CrossRef] [PubMed]
- Elke, G.; the SepNet Critical Care Trials Group; Bloos, F.; Wilson, D.C.; Brunkhorst, F.M.; Briegel, J.; Reinhart, K.; Loeffler, M.; Kluge, S.; Nierhaus, A.; et al. The use of mid-regional proadrenomedullin to identify disease severity and treatment response to sepsis—A secondary analysis of a large randomised controlled trial. Crit. Care 2018, 22, 79. [Google Scholar] [CrossRef]
- Andrés, C.; Andaluz-Ojeda, D.; Cicuendez, R.; Nogales, L.; Martín, S.; Martin-Fernandez, M.; Almansa, R.; Bermejo-Martin, J.F. MR-proADM to detect specific types of organ failure in infection. Eur. J. Clin. Investig. 2020, 50, e13246. [Google Scholar] [CrossRef]
- Geven, C.; Kox, M.; Pickkers, P. Adrenomedullin and Adrenomedullin-Targeted Therapy as Treatment Strategies Relevant for Sepsis. Front. Immunol. 2018, 9, 292. [Google Scholar] [CrossRef]
- Wagner, K.; Wachter, U.; A Vogt, J.; Scheuerle, A.; McCook, O.; Weber, S.; Gröger, M.; Stahl, B.; Georgieff, M.; Möller, P.; et al. Adrenomedullin binding improves catecholamine responsiveness and kidney function in resuscitated murine septic shock. Intensive Care Med. Exp. 2013, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Geven, C.; Peters, E.; Schroedter, M.; Struck, J.; Bergmann, A.; McCook, O.; Radermacher, P.; Kox, M.; Pickkers, P. Effects of the Humanized Anti-Adrenomedullin Antibody Adrecizumab (HAM8101) on Vascular Barrier Function and Survival in Rodent Models of Systemic Inflammation and Sepsis. Shock 2018, 50, 648–654. [Google Scholar] [CrossRef]
- Voors, A.A.; Kremer, D.; Geven, C.; Ter Maaten, J.M.; Struck, J.; Bergmann, A.; Pickkers, P.; Metra, M.; Mebazaa, A.; Düngen, H.-D.; et al. Adrenomedullin in heart failure: Pathophysiology and therapeutic application. Eur. J. Heart Fail. 2019, 21, 163–171. [Google Scholar] [CrossRef]
- Bertrand, J.; Bollmann, M. Soluble syndecans: Biomarkers for diseases and therapeutic options. Br. J. Pharmacol. 2018, 176, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulou, A.N.; Multhaupt, H.A.; Couchman, J.R. Syndecans in wound healing, inflammation and vascular biology. Int. J. Biochem. Cell Biol. 2007, 39, 505–528. [Google Scholar] [CrossRef]
- Subramanian, S.V.; Fitzgerald, M.L.; Bernfield, M. Regulated Shedding of Syndecan-1 and -4 Ectodomains by Thrombin and Growth Factor Receptor Activation. J. Biol. Chem. 1997, 272, 14713–14720. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Sarmiento, J.; Molina, C.F.; Salazar-Pelaez, L.M.; Flórez, S.; Alarcón-Forero, L.C.; Sarta, M.; Hernández-Sarmiento, R.; Villar, J.C. Biomarkers of glycocalyx injury and endothelial activation are associated with clinical outcomes in patients with sepsis: A systematic review and meta-analysis. J. Intensive Care Med. 2023, 38, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Nelson, A.; Berkestedt, I.; Bodelsson, M. Circulating glycosaminoglycan species in septic shock. Acta Anaesthesiol. Scand. 2014, 58, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Jannaway, M.; Yang, X.; Meegan, J.E.; Coleman, D.C.; Yuan, S.Y. Thrombin-cleaved syndecan-3/-4 ectodomain fragments mediate endothelial barrier dysfunction. PLoS ONE 2019, 14, e0214737. [Google Scholar] [CrossRef] [PubMed]
- Sack, K.D.; Kellum, J.A.; Parikh, S.M. The Angiopoietin-Tie2 Pathway in Critical Illness. Crit. Care Clin. 2020, 36, 201–216. [Google Scholar] [CrossRef]
- Lukasz, A.; Hillgruber, C.; Oberleithner, H.; Kusche-Vihrog, K.; Pavenstädt, H.; Rovas, A.; Hesse, B.; Goerge, T.; Kümpers, P. Endothelial glycocalyx breakdown is mediated by angiopoietin-2. Cardiovasc. Res. 2017, 113, 671–680. [Google Scholar] [CrossRef] [PubMed]
- Drost, C.C.; Rovas, A.; Kusche-Vihrog, K.; Van Slyke, P.; Kim, H.; Hoang, V.C.; Maynes, J.T.; Wennmann, D.O.; Pavenstädt, H.; Linke, W.; et al. Tie2 activation promotes protection and reconstitution of the endothelial glycocalyx in human sepsis. Thromb. Haemost. 2019, 119, 1827–1838. [Google Scholar] [PubMed]
- Rovas, A.; Osiaevi, I.; Buscher, K.; Sackarnd, J.; Tepasse, P.R.; Fobker, M.; Kühn, J.; Braune, S.; Göbel, U.; Thölking, G.; et al. Microvascular dysfunction in COVID-19: The MYSTIC study. Angiogenesis 2021, 24, 145–157. [Google Scholar] [CrossRef]
- Siner, J.M.; Bhandari, V.; Engle, K.M.; Elias, J.A.; Siegel, M.D. Elevated serum angiopoietin 2 levels are associated with increased mortality in sepsis. Shock 2009, 31, 348–353. [Google Scholar] [CrossRef]
- Yang, K.-Y.; Liu, K.-T.; Chen, Y.-C.; Chen, C.-S.; Lee, Y.-C.; Perng, R.-P.; Feng, J.-Y. Plasma soluble vascular endothelial growth factor receptor-1 levels predict outcomes of pneumonia-related septic shock patients: A prospective observational study. Crit. Care 2011, 15, R11. [Google Scholar] [CrossRef]
- ProCESS Investigators. A randomized trial of protocol-based care for early septic shock. N. Engl. J. Med. 2014, 370, 1683–1693. [Google Scholar] [CrossRef] [PubMed]
- Hou, P.C.; Filbin, M.R.; Wang, H.; Ngo, L.; Huang, D.T.; Aird, W.C.; Yealy, D.M.; Angus, D.C.; Kellum, J.A.; Shapiro, N.I.; et al. Endothelial permeability and hemostasis in septic shock: Results from the ProCESS trial. Chest 2017, 152, 22–31. [Google Scholar] [CrossRef]
- Beyer, D.; Hoff, J.; Sommerfeld, O.; Zipprich, A.; Gaßler, N.; Press, A.T. The liver in sepsis: Molecular mechanism of liver failure and their potential for clinical translation. Mol. Med. 2022, 28, 84. [Google Scholar] [CrossRef]
- Shi, R.; Wang, J.; Zhang, Z.; Leng, Y.; Chen, A.F. ASGR1 promotes liver injury in sepsis by modulating monocyte-to-macrophage differentiation via NF-κB/ATF5 pathway. Life Sci. 2023, 315, 121339. [Google Scholar] [CrossRef]
- Li, M.; Cai, S.-Y.; Boyer, J.L. Mechanisms of bile acid mediated inflammation in the liver. Mol. Asp. Med. 2017, 56, 45–53. [Google Scholar] [CrossRef]
- Xerri, A.; Gallardo, F.; Kober, F.; Mathieu, C.; Fourny, N.; Tran, T.T.; Mege, J.-L.; Singer, M.; Lalevée, N.; Bernard, M.; et al. Female hormones prevent sepsis-induced cardiac dysfunction: An experimental randomized study. Sci. Rep. 2022, 12, 4939. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Qian, H.; Zheng, N.; Lu, Q.; Han, Y. GYY4137 ameliorates sepsis-induced cardiomyopathy via NLRP3 pathway. Biochim. et Biophys. Acta (BBA)-Mol. Basis Dis. 2022, 1868, 166497. [Google Scholar] [CrossRef]
- Pu, J.; Gao, F.; He, Y. Integrated Bioinformatics Analysis Reveals APEX1 as a Potential Biomarker for Septic Cardiomyopathy. BioRxiv 2023. [Google Scholar] [CrossRef]
- Liu, V.X.; Fielding-Singh, V.; Greene, J.D.; Baker, J.M.; Iwashyna, T.J.; Bhattacharya, J.; Escobar, G.J. The timing of early antibiotics and hospital mortality in sepsis. Am. J. Respir. Crit. Care Med. 2017, 196, 856–863. [Google Scholar] [CrossRef]
- Scicluna, B.P.; A van Vught, L.; Zwinderman, A.H.; A Wiewel, M.; E Davenport, E.; Burnham, K.L.; Nürnberg, P.; Schultz, M.J.; Horn, J.; Cremer, O.L.; et al. Classification of patients with sepsis according to blood genomic endotype: A prospective cohort study. Lancet Respir. Med. 2017, 5, 816–826. [Google Scholar] [CrossRef] [PubMed]
- Wong, H.R.; Cvijanovich, N.; Lin, R.; Allen, G.L.; Thomas, N.J.; Willson, D.F.; Freishtat, R.J.; Anas, N.; Meyer, K.; A Checchia, P.; et al. Identification of pediatric septic shock subclasses based on genome-wide expression profiling. BMC Med. 2009, 7, 34. [Google Scholar] [CrossRef]
- Seymour, C.W.; Kennedy, J.N.; Wang, S.; Chang, C.-C.H.; Elliott, C.; Xu, Z.; Berry, S.; Clermont, G.; Cooper, G.; Gomez, H.; et al. Derivation, Validation, and Potential Treatment Implications of Novel Clinical Phenotypes for Sepsis. JAMA 2019, 321, 2003–2017. [Google Scholar] [CrossRef]
- Sweeney, T.E.; Azad, T.; Donato, M.; Haynes, W.A.; Perumal, T.M.; Henao, R.; Bermejo-Martin, J.F.; Almansa, R.; Tamayo, E.; Howrylak, J.A.; et al. Unsupervised Analysis of Transcriptomics in Bacterial Sepsis Across Multiple Datasets Reveals Three Robust Clusters. Crit. Care Med. 2018, 46, 915–925. [Google Scholar] [CrossRef] [PubMed]
- Nusshag, C.; Morath, C.; Uhle, F.; Sweeney, T.; Liesenfeld, O.; Merle, U.; Zeier, M.; Brenner, T.; Weigand, M.A. 1189: Transcriptomic endotypes implicate a unique risk profile for kidney-related outcomes in sepsis. Crit. Care Med. 2022, 51, 593. [Google Scholar] [CrossRef]
- Leventogiannis, K.; Kyriazopoulou, E.; Antonakos, N.; Kotsaki, A.; Tsangaris, I.; Markopoulou, D.; Grondman, I.; Rovina, N.; Theodorou, V.; Antoniadou, E.; et al. Toward personalized immunotherapy in sepsis: The PROVIDE randomized clinical trial. Cell Rep. Med. 2022, 3, 100817. [Google Scholar] [CrossRef]
- Vandewalle, J.; Luypaert, A.; De Bosscher, K.; Libert, C. Therapeutic Mechanisms of Glucocorticoids. Trends Endocrinol. Metab. 2018, 29, 42–54. [Google Scholar] [CrossRef]
- Vandewalle, J.; Libert, C. Glucocorticoids in Sepsis: To Be or Not to Be. Front. Immunol. 2020, 11, 1318. [Google Scholar] [CrossRef] [PubMed]
- Martin-Loeches, I.; Torres, A. Corticosteroids for CAP, influenza and COVID-19: When, how and benefits or harm? Eur. Respir. Rev. 2021, 30, 200346. [Google Scholar] [CrossRef] [PubMed]
- Antcliffe, D.B.; Burnham, K.L.; Al-Beidh, F.; Santhakumaran, S.; Brett, S.J.; Hinds, C.J.; Ashby, D.; Knight, J.C.; Gordon, A.C. Transcriptomic Signatures in Sepsis and a Differential Response to Steroids. From the VANISH Randomized Trial. Am. J. Respir. Crit. Care Med. 2019, 199, 980–986. [Google Scholar] [CrossRef]
- Venkatesh, B.; Finfer, S.; Cohen, J.; Rajbhandari, D.; Arabi, Y.; Bellomo, R.; Billot, L.; Correa, M.; Glass, P.; Harward, M. ADRENAL Trial Investigators and the Australian–New Zealand Intensive Care Society Clinical Trials Group. Adjunctive Glucocorticoid Therapy in Patients with Septic Shock. N. Engl. J. Med. 2018, 378, 797–808. [Google Scholar] [CrossRef]
- Keh, D.; Boehnke, T.; Weber-Cartens, S.; Schulz, C.; Ahlers, O.; Bercker, S.; Volk, H.D.; Doecke, W.D.; Falke, K.J.; Gerlach, H. Immunologic and hemodynamic effects of “low-dose” hydrocortisone in septic shock: A double-blind, randomized, placebo-controlled, crossover study. Am. J. Respir. Crit. Care Med. 2003, 167, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Bentzer, P.; Fjell, C.; Walley, K.R.; Boyd, J.; Russell, J.A. Plasma cytokine levels predict response to corticosteroids in septic shock. Intensive Care Med. 2016, 42, 1970–1979. [Google Scholar] [CrossRef]
- Martin-Loeches, I.; the GRECIA group; Muriel-Bombín, A.; Ferrer, R.; Artigas, A.; Sole-Violan, J.; Lorente, L.; Andaluz-Ojeda, D.; Prina-Mello, A.; Herrán-Monge, R.; et al. The protective association of endogenous immunoglobulins against sepsis mortality is restricted to patients with moderate organ failure. Ann. Intensive Care 2017, 7, 44. [Google Scholar] [CrossRef]
- Jarczak, D.; Kluge, S.; Nierhaus, A. Use of Intravenous Immunoglobulins in Sepsis Therapy—A Clinical View. Int. J. Mol. Sci. 2020, 21, 5543. [Google Scholar] [CrossRef]
- Nakamori, Y.; Park, E.J.; Shimaoka, M. Immune deregulation in sepsis and septic shock: Reversing immune paralysis by targeting PD-1/PD-L1 pathway. Front. Immunol. 2021, 11, 624279. [Google Scholar] [CrossRef]
- Hotchkiss, R.S.; Colston, E.; Yende, S.; Angus, D.C.; Moldawer, L.L.; Crouser, E.D.; Martin, G.S.; Coopersmith, C.M.; Brakenridge, S.; Mayr, F.B.; et al. Immune checkpoint inhibition in sepsis: A Phase 1b randomized, placebo-controlled, single ascending dose study of anti-PD-L1 (BMS-936559). Crit. Care Med. 2019, 47, 632. [Google Scholar] [CrossRef] [PubMed]
| Conditions | Therapeutics (s) | Phase | Patients [n] | Trial Identifier | Status |
|---|---|---|---|---|---|
| Severe Sepsis with Septic shock | Two dosing frequencies of recombinant Interleukin-7 (CYT107) treatment to restore absolute lymphocyte counts in sepsis patients; IRIS-7B | Phase 2 | 27 | NCT02640807 | Completed |
| Sepsis and Septic Shock | Effects of Interferon-gamma on Sepsis-induced Immunoparalysis, | Phase 3 | 4 | NCT01649921 | Completed |
| Severe Sepsis and Septic Shock | PD-1/PD-L1 pathway inhibition in sepsis, BMS-936559 | Phase 1b/2a | 35 | NCT02576457 | Terminated |
| Septic Neonates with Neutropenia | Macrophage colony stimulating factor (GM-CSF) in septic neonates with neutropenia | Phase 1 | 280 | ISRCTN42553489 | Completed |
| Septic Shock | Allogeneic mesenchymal stromal cells (CISS) | Phase 1/Phase 2 | 9 | NCT02421484 | Completed |
| Sepsis and Macrophage Activation Syndrome | Treatment with recombinant human interferon-gamma or anakinra validation (PROVIDE) | Phase 2 | 36 | NCT03332225 | Completed |
| Pediatric Sepsis-induced MODS | GM-CSF for Reversal of immunoparalysis | Phase 4 | 120 | NCT03769844 | Active, not Recruiting |
| Sepsis | Drug: Anakinra or rhIFNγ adjunctive immunotherapy (ImmunoSep) | Phase 2 | 280 | NCT04990232 | Recruiting |
| Sepsis | Long-term Effects of Thymosin Alpha 1 Treatment | Phase 1/Phase 2 Drug interventions have been done in previous clinical studies | 900 | NCT04901104 | Not yet recruiting |
| Phenotype | The observable traits or characteristics of an organism governing morphology, development, behavior, and properties, resulting from the interaction of its genome with its environment. |
| Endotype | A link to a single molecular mechanism and those that share etiological and pathogenic pathways with nonlinear dynamic interactions that may or may not be present in all patients, or in each patient at all time points. |
| Omics | Characterisation of the biological signal in respect of a disease or subtype of disease process. |
| Metabolomics | Study of the metabolic substrates produced and their timing during a disease or pathological process. |
| Proteomics | Description of the nature, quantity and timing of proteins produced during a disease or pathological process. |
| Genomics | Focus on the structure, function, evolution and editing of the DNA comprising the complete set of genes of an organism. |
| Transcriptomics | Examination of the changes in transcription of RNA information coded in an organism’s DNA that is present in a sample (a cell, tissue, or organ) at a given time. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garduno, A.; Cusack, R.; Leone, M.; Einav, S.; Martin-Loeches, I. Multi-Omics Endotypes in ICU Sepsis-Induced Immunosuppression. Microorganisms 2023, 11, 1119. https://doi.org/10.3390/microorganisms11051119
Garduno A, Cusack R, Leone M, Einav S, Martin-Loeches I. Multi-Omics Endotypes in ICU Sepsis-Induced Immunosuppression. Microorganisms. 2023; 11(5):1119. https://doi.org/10.3390/microorganisms11051119
Chicago/Turabian StyleGarduno, Alexis, Rachael Cusack, Marc Leone, Sharon Einav, and Ignacio Martin-Loeches. 2023. "Multi-Omics Endotypes in ICU Sepsis-Induced Immunosuppression" Microorganisms 11, no. 5: 1119. https://doi.org/10.3390/microorganisms11051119
APA StyleGarduno, A., Cusack, R., Leone, M., Einav, S., & Martin-Loeches, I. (2023). Multi-Omics Endotypes in ICU Sepsis-Induced Immunosuppression. Microorganisms, 11(5), 1119. https://doi.org/10.3390/microorganisms11051119








