Occurrence and Molecular Study of Hypermucoviscous/Hypervirulence Trait in Gut Commensal K. pneumoniae from Healthy Subjects
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population, Stool Samples, and Identification of Gut Commensal Kp Isolates
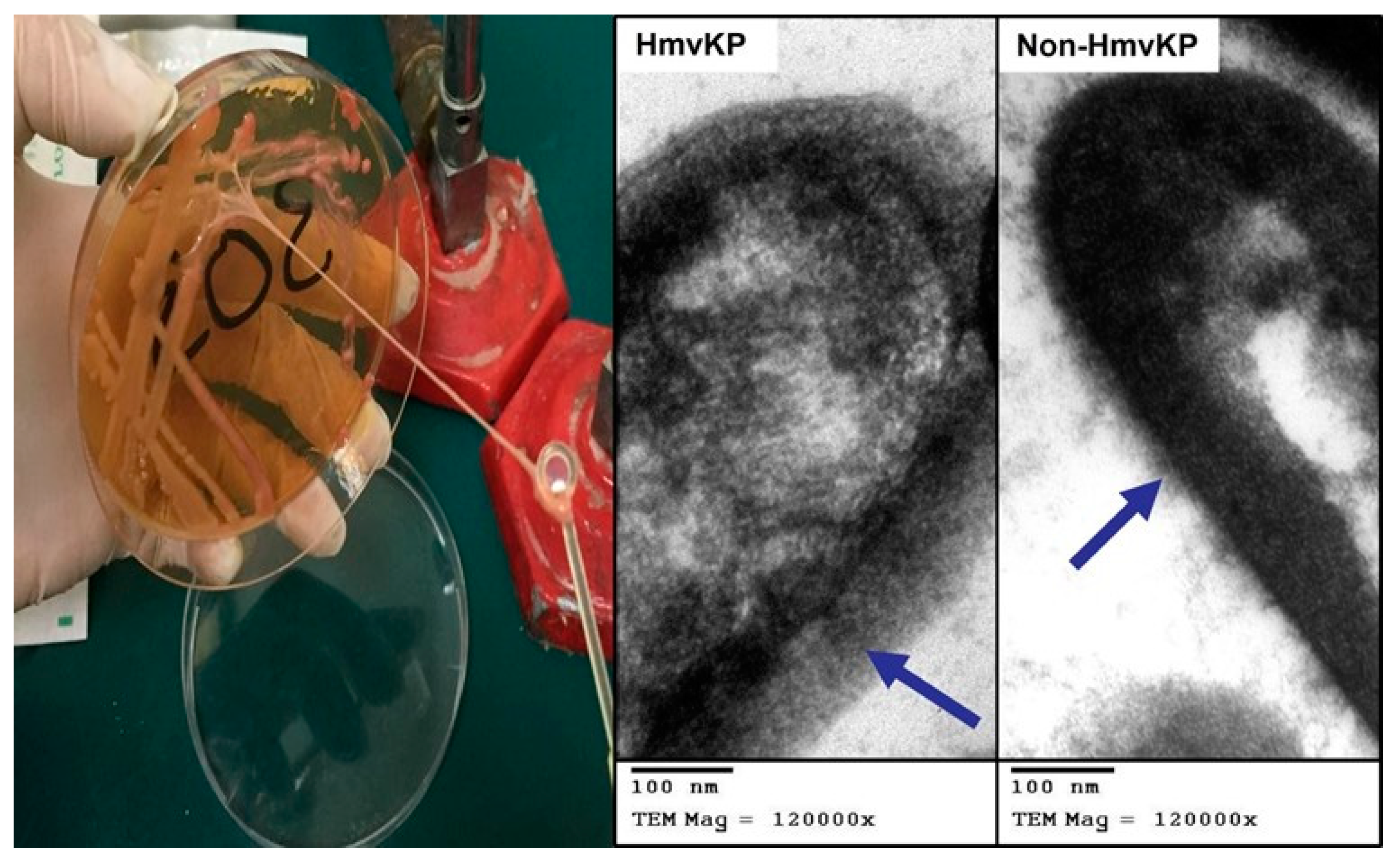
2.2. Phenotypic Assay for Identification of Hypermucoviscosity Character
2.3. Antimicrobial Susceptibility Testing and Screening for Extended-Spectrum β-Lactamase (ESBLs) Producers
2.4. Quantitative Biofilm Formation Assay
2.5. PCR-Based Molecular Study
2.5.1. DNA Extraction and PCR Oligonucleotide Primers
2.5.2. Detection of Hypermucoviscousity Phenotype-Associated Genes
2.6. Transmission Electron Microscopy (TEM) Study
2.7. Statistical Analysis
3. Results
3.1. Identification and Frequency of HmvKp Isolates among Stool Isolates
3.2. Antimicrobial Resistance Profiles of HmvKp and Non-HmvKp Isolates
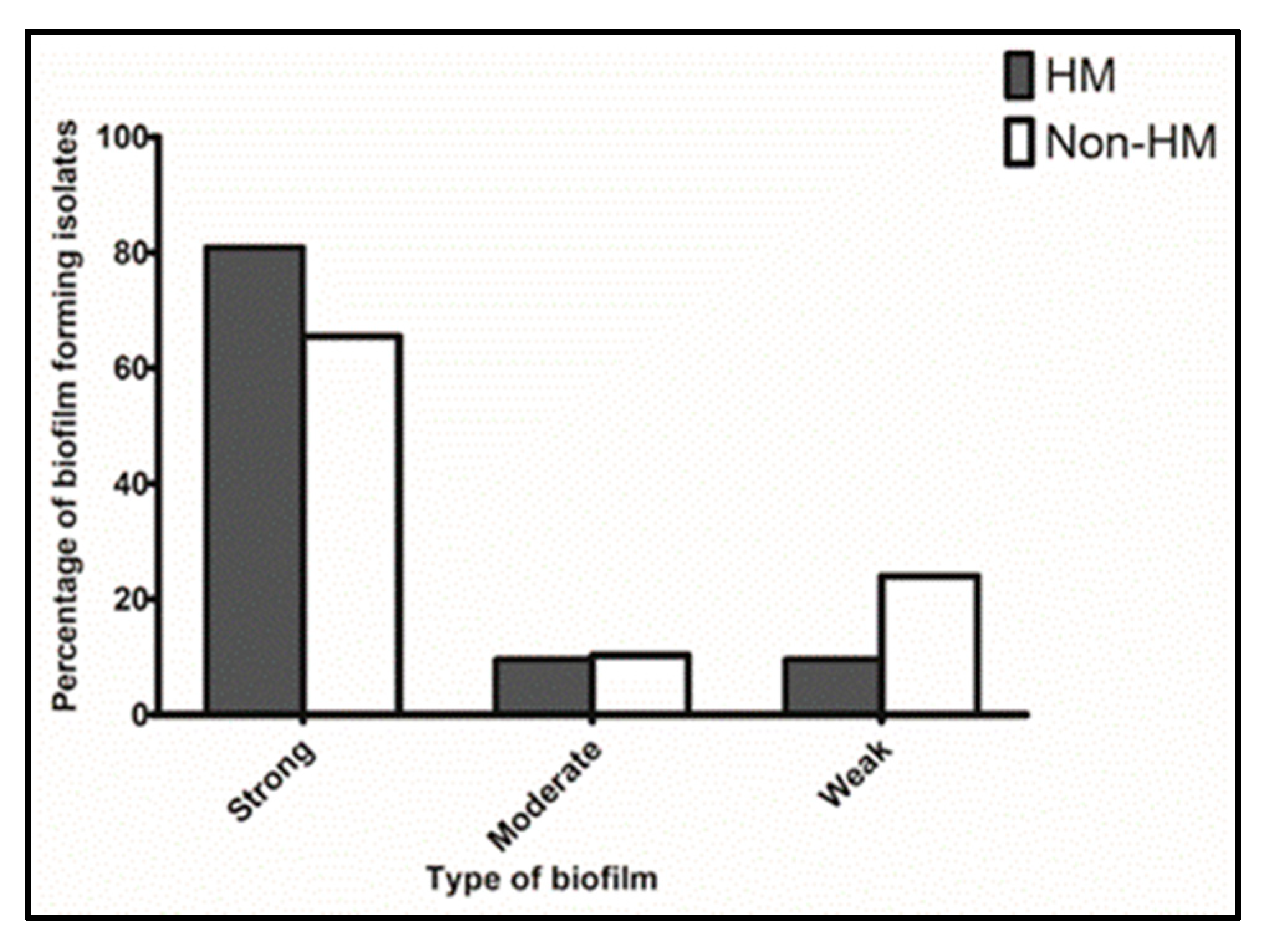
3.3. Biofilm Formation Characters among HmvKp and Non-HmvKp Phenotypes
3.4. Distribution of Hypermucoviscosity Phenotype-Related Virulence Genes among HmvKp and Non-HmvKp Isolates
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Strakova, N.; Korena, K.; Karpiskova, R. Klebsiella pneumoniae producing bacterial toxin colibactin as a risk of colorectal cancer development—A systematic review. Toxicon 2021, 197, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Fung, C.-P.; Lin, Y.-T.; Lin, J.-C.; Chen, T.-L.; Yeh, K.-M.; Chang, F.-Y.; Chuang, H.-C.; Wu, H.-S.; Tseng, C.-P.; Siu, L.K. Klebsiella pneumoniae in gastrointestinal tract and pyogenic liver abscess. Emerg. Infect. Dis. 2012, 18, 1322–1325. [Google Scholar] [CrossRef] [PubMed]
- Pomakova, D.K.; Hsiao, C.B.; Beanan, J.M.; Olson, R.; MacDonald, U.; Keynan, Y.; Russo, T.A. Clinical and phenotypic differences between classic and hypervirulent Klebsiella pneumonia: An emerging and under-recognized pathogenic variant. Eur. J. Clin. Microbiol. Infect. Dis. 2012, 31, 981–989. [Google Scholar] [CrossRef] [PubMed]
- Kaur, C.P.; Vadivelu, J.; Chandramathi, S. Impact of Klebsiella pneumoniae in lower gastrointestinal tract diseases. J. Dig. Dis. 2018, 19, 262–271. [Google Scholar] [CrossRef]
- Paczosa, M.K.; Mecsas, J. Klebsiella pneumoniae: Going on the offense with a strong defense. Microbiol. Mol. Biol. Rev. 2016, 80, 629–661. [Google Scholar] [CrossRef]
- Jung, H.-J.; Littmann, E.R.; Seok, R.; Leiner, I.M.; Taur, Y.; Peled, J.; Van Den Brink, M.; Ling, L.; Chen, L.; Kreiswirth, B.N.; et al. Genome-wide screening for enteric colonization factors in carbapenem-resistant ST258 Klebsiella pneumoniae. MBio 2019, 10, e02663-18. [Google Scholar] [CrossRef]
- Martin, R.M.; Cao, J.; Brisse, S.; Passet, V.; Wu, W.; Zhao, L.; Malani, P.N.; Rao, K.; Bachman, M.A. Molecular epidemiology of colonizing and infecting isolates of Klebsiella pneumoniae. MSphere 2016, 1, e00261-16. [Google Scholar] [CrossRef]
- Lobo, A.S.; Tellis, R.; Moosabba, M.S.; Roche, R. Hypermucoviscous uropathogenic strains of Klebsiella pneumoniae producing extended spectrum beta-lactamase: An experience in South Indian tertiary care hospital. IP Int. J. Compr. Adv. Pharm. 2019, 4, 1–4. [Google Scholar] [CrossRef]
- Shon, A.S.; Bajwa, R.P.; Russo, T.A. Hypervirulent (hypermucoviscous) Klebsiella pneumoniae: A new and dangerous breed. Virulence 2013, 4, 107–118. [Google Scholar] [CrossRef]
- Catalán-Nájera, J.C.; Garza-Ramos, U.; Barrios-Camacho, H. Hypervirulence and hypermucoviscosity: Two different but complementary Klebsiella spp. phenotypes? Virulence 2017, 8, 1111–1123. [Google Scholar] [CrossRef]
- Abdulall, A.K.; Tawfick, M.M.; El Manakhly, A.R.; El Kholy, A. Carbapenem-resistant Gram-negative bacteria associated with catheter-related bloodstream infections in three intensive care units in Egypt. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 1647–1652. [Google Scholar] [CrossRef] [PubMed]
- Choby, J.E.; Howard-Anderson, J.; Weiss, D.S. Hypervirulent Klebsiella pneumoniae—Clinical and molecular perspectives. J. Intern. Med. 2020, 287, 283–300. [Google Scholar] [CrossRef]
- Nadasy, K.A.; Domiati-Saad, R.; Tribble, M.A. Invasive Klebsiella pneumoniae syndrome in North America. Clin. Infect. Dis. 2007, 45, e25–e28. [Google Scholar] [CrossRef] [PubMed]
- Ragheb, S.M.; Tawfick, M.M.; El-Kholy, A.A.; Abdulall, A.K. Phenotypic and genotypic features of Klebsiella pneumoniae harboring carbapenemases in Egypt: OXA-48-like carbapenemases as an investigated model. Antibiotics 2020, 9, 852. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, E.R.; Aly, S.A.; Halby, H.M.; Ahmed, S.H.; Zakaria, A.M.; El-Asheer, O.M. Epidemiological typing of multidrug-resistant Klebsiella pneumoniae, which causes paediatric ventilator-associated pneumonia in Egypt. J. Med. Microbiol. 2017, 66, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Sayeed, M.A.; Latif, N.; Mahmood, S.F. Hypermucoviscous Klebsiella syndrome it’s in the community! JPMA 2017, 67, 1930. [Google Scholar]
- Farag, A.M.; Tawfick, M.M.; Abozeed, M.Y.; Shaban, E.A.; Abo-Shadi, M.A. Microbiological profile of ventilator-associated pneumonia among intensive care unit patients in tertiary Egyptian hospitals. J. Infect. Dev. Ctries. 2020, 14, 153–161. [Google Scholar] [CrossRef]
- Osama, D.; El-Mahallawy, H.; Mansour, M.T.; Hashem, A.; Attia, A.S. Molecular characterization of carbapenemase-producing Klebsiella pneumoniae isolated from Egyptian pediatric cancer patients including a strain with a rare gene-combination of β-lactamases. Infect. Drug. Resist. 2021, 14, 335–348. [Google Scholar] [CrossRef]
- Surgers, L.; Boyd, A.; Girard, P.M.; Arlet, G.; Decré, D. ESBL-producing strain of hypervirulent Klebsiella pneumoniae K2, France. Emerg. Infect. Dis. 2016, 22, 1687–1688. [Google Scholar] [CrossRef]
- Gonzalez-Ferrer, S.; Peñaloza, H.F.; Budnick, J.A.; Bain, W.G.; Nordstrom, H.R.; Lee, J.S.; Van Tyne, D. Finding order in the chaos: Outstanding questions in Klebsiella pneumoniae pathogenesis. Infect. Immun. 2021, 89, e00693-20. [Google Scholar] [CrossRef]
- Marr, C.M.; Russo, T.A. Hypervirulent Klebsiella pneumoniae: A new public health threat. Expert Rev. Anti. Infect. 2019, 17, 71–73. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Chen, D.; Xu, G.; Huang, W.; Wang, X. Molecular epidemiology and drug resistant mechanism in carbapenem-resistant Klebsiella pneumoniae isolated from pediatric patients in Shanghai, China. PLoS ONE 2018, 13, e0194000. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Guo, J. Hypervirulent Klebsiella pneumoniae (hypermucoviscous and aerobactin positive) infection over 6 years in the elderly in China: Antimicrobial resistance patterns, molecular epidemiology and risk factor. Ann. Clin. Microbiol. Antimicrob. 2019, 18, 4. [Google Scholar] [CrossRef] [PubMed]
- Harada, S.; Doi, Y. Hypervirulent Klebsiella pneumoniae: A call for consensus definition and international collaboration. J. Clin. Microbiol. 2018, 56, e00959-18. [Google Scholar] [CrossRef]
- Lee, H.-C.; Chuang, Y.-C.; Yu, W.-L.; Lee, N.-Y.; Chang, C.-M.; Ko, N.-Y.; Wang, L.-R.; Ko, W.-C. Clinical implications of hypermucoviscosity phenotype in Klebsiella pneumoniae isolates: Association with invasive syndrome in patients with community-acquired bacteraemia. J. Intern. Med. 2006, 259, 606–614. [Google Scholar] [CrossRef]
- Struve, C.; Roe, C.C.; Stegger, M.; Stahlhut, S.G.; Hansen, D.S.; Engelthaler, D.M.; Andersen, P.S.; Driebe, E.M.; Keim, P.; Krogfelt, K.A. Mapping the evolution of hypervirulent Klebsiella pneumoniae. MBio 2015, 6, e00630-15. [Google Scholar] [CrossRef]
- Russo, T.A.; Marr, C.M. Hypervirulent Klebsiella pneumoniae. Clin. Microbiol. Rev. 2019, 32, e00001-19. [Google Scholar] [CrossRef]
- Lee, C.-R.; Lee, J.H.; Park, K.S.; Jeon, J.H.; Kim, Y.B.; Cha, C.-J.; Jeong, B.C.; Lee, S.H. Antimicrobial resistance of hypervirulent Klebsiella pneumoniae: Epidemiology, hypervirulence-associated determinants, and resistance mechanisms. Front. Cell. Infect. Microbiol. 2017, 7, 483. [Google Scholar] [CrossRef]
- Li, B.; Zhao, Y.; Liu, C.; Chen, Z.; Zhou, D. Molecular pathogenesis of Klebsiella pneumoniae. Futur. Microbiol. 2014, 9, 1071–1081. [Google Scholar] [CrossRef]
- Stanley, I.J.; Kajumbula, H.; Bazira, J.; Kansiime, C.; Rwego, I.B.; Asiimwe, B.B. Multidrug resistance among Escherichia coli and Klebsiella pneumoniae carried in the gut of out-patients from pastoralist communities of Kasese district, Uganda. PLoS ONE 2018, 13, e0200093. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing. Clinical and Laboratory Standards Institute, Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically, M07Ed11, 11th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018. [Google Scholar]
- Nyenje, M.E.; Green, E.; Ndip, R.N. Evaluation of the effect of different growth media and temperature on the suitability of biofilm formation by Enterobacter cloacae strains isolated from food samples in South Africa. Molecules 2013, 18, 9582–9593. [Google Scholar] [CrossRef] [PubMed]
- Tahaei, S.A.S.; Stájer, A.; Barrak, I.; Ostorházi, E.; Szabó, D.; Gajdács, M. Correlation between biofilm-formation and the antibiotic resistant phenotype in Staphylococcus aureus isolates: A laboratory-based study in Hungary and a review of the literature. Infect. Drug. Resist. 2021, 14, 1155–1168. [Google Scholar] [CrossRef] [PubMed]
- Queipo-Ortuño, M.I.; De Dios Colmenero, J.; Macias, M.; Bravo, M.J.; Morata, P. Preparation of bacterial DNA template by boiling and effect of immunoglobulin G as an inhibitor in real-time PCR for serum samples from patients with brucellosis. Clin. Vaccine Immunol. 2008, 15, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Tan, T.Y.; Ong, M.; Cheng, Y.; Ng, L.S.Y. Hypermucoviscosity, rmpA, and aerobactin are associated with community-acquired Klebsiella pneumoniae bacteremic isolates causing liver abscess in Singapore. J. Microbiol. Immunol. Infect. 2019, 52, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Russo, T.A.; Olson, R.; Fang, C.-T.; Stoesser, N.; Miller, M.; MacDonald, U.; Hutson, A.; Barker, J.H.; La Hoz, R.M.; Johnson, J.R.; et al. Identification of biomarkers for differentiation of hypervirulent Klebsiella pneumoniae from classical K. pneumoniae. J. Clin. Microbiol. 2018, 56, e00776-18. [Google Scholar] [CrossRef]
- Luo, Y.; Wang, Y.; Ye, L.; Yang, J. Molecular epidemiology and virulence factors of pyogenic liver abscess causing Klebsiella pneumoniae in China. Clin. Microbiol. Infect. 2014, 20, O818–O824. [Google Scholar] [CrossRef]
- Yu, W.L.; Ko, W.C.; Cheng, K.C.; Lee, H.C.; Ke, D.S.; Lee, C.C.; Fung, C.P.; Chuang, Y.C. Association between rmpA and magA genes and clinical syndromes caused by Klebsiella pneumoniae in Taiwan. Clin. Infect. Dis. 2006, 42, 1351–1358. [Google Scholar] [CrossRef]
- Zhu, J.; Wang, T.; Chen, L.; Du, H. Virulence factors in hypervirulent Klebsiella pneumoniae. Front. Microbiol. 2021, 12, 642484. [Google Scholar] [CrossRef]
- Elken, E.M.; Tan, Z.; Wang, Q.; Jiang, X.; Wang, Y.; Wang, Y.M.; Ma, H.X. Impact of Sub-MIC Eugenol on Klebsiella pneumoniae Biofilm Formation via Upregulation of rcsB. Front. Vet. Sci. 2022, 9, 945491. [Google Scholar] [CrossRef]
- Decré, D.; Verdet, C.; Emirian, A.; Le Gourrierec, T.; Petit, J.C.; Offenstadt, G.; Maury, E.; Brisse, S.; Arlet, G. Emerging severe and fatal infections due to Klebsiella pneumoniae in two university hospitals in France. J. Clin. Microbiol. 2011, 49, 3012–3014. [Google Scholar] [CrossRef]
- Lee, C.H.; Liu, J.W.; Su, L.H.; Chien, C.C.; Li, C.C.; Yang, K.D. Hypermucoviscosity associated with Klebsiella pneumoniae-mediated invasive syndrome: A prospective cross-sectional study in Taiwan. Int. J. Infect. Dis. 2010, 14, e688–e692. [Google Scholar] [CrossRef]
- Lee, I.R.; Molton, J.S.; Wyres, K.L.; Gorrie, C.; Wong, J.; Hoh, C.H.; Teo, J.; Kalimuddin, S.; Lye, D.C.; Archuleta, S.; et al. Differential host susceptibility and bacterial virulence factors driving Klebsiella liver abscess in an ethnically diverse population. Sci. Rep. 2016, 6, 29316. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Yang, X.; Chan, E.W.C.; Chen, S. The hypermucoviscosity of hypervirulent K. pneumoniae confers the ability to evade neutrophil-mediated phagocytosis. Virulence 2021, 12, 2050–2059. [Google Scholar] [CrossRef] [PubMed]
- Tan, T.Y.; Cheng, Y.; Ong, M.; Ng, L.S.Y. Performance characteristics and clinical predictive value of the string test for detection of hepato-virulent Klebsiella pneumoniae isolated from blood cultures. Diagn. Microbiol. Infect. Dis. 2014, 78, 127–128. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.C.; Lu, M.C.; Tang, H.L.; Liu, H.C.; Chen, C.H.; Liu, K.S.; Lin, C.; Chiou, C.S.; Chiang, M.K.; Chen, C.M.; et al. Assessment of hypermucoviscosity as a virulence factor for experimental Klebsiella pneumoniae infections: Comparative virulence analysis with hypermucoviscosity-negative strain. BMC Microbiol. 2011, 11, 50. [Google Scholar] [CrossRef]
- Yu, W.L.; Ko, W.C.; Cheng, K.C.; Lee, C.C.; Lai, C.C.; Chuang, Y.C. Comparison of prevalence of virulence factors for Klebsiella pneumoniae liver abscesses between isolates with capsular K1/K2 and non-K1/K2 serotypes. Diagn. Microbiol. Infect. Dis. 2008, 62, 1–6. [Google Scholar] [CrossRef]
- Hagiya, H.; Watanabe, N.; Maki, M.; Murase, T.; Otsuka, F. Clinical utility of string test as a screening method for hypermucoviscosity-phenotype Klebsiella pneumoniae. Acute Med. Surg. 2014, 1, 245–246. [Google Scholar] [CrossRef]
- Elbrolosy, A.; Eissa, N.; Al- Rajhy, N.; El- Mahdy, E.; Mostafa, R. Characterization of virulence genetic profile and resistance patterns of clinical Klebsiella pneumoniae isolates: Classic versus hypermucoviscous phenotypes. Microbes Infect. Dis. 2021, 2, 516–528. [Google Scholar] [CrossRef]
- Wu, H.; Li, D.; Zhou, H.; Sun, Y.; Guoling Shen, D. Bacteremia and other body site infection caused by hypervirulent and classic Klebsiella pneumoniae. Microb. Pathog. 2017, 104, 254–262. [Google Scholar] [CrossRef]
- Cubero, M.; Grau, I.; Tubau, F.; Pallares, R.; Domínguez, M.A.; Liñares, J.; Ardanuy, C. Hypervirulent Klebsiella pneumoniae clones causing bacteraemia in adults in a teaching hospital in Barcelona, Spain (2007-2013). Clin. Microbiol. Infect. 2016, 22, 154–160. [Google Scholar] [CrossRef]
- Lin, Z.W.; Zheng, J.X.; Bai, B.; Xu, G.J.; Lin, F.J.; Chen, Z.; Sun, X.; Qu, D.; Yu, Z.-j.; Deng, Q.-w. Characteristics of Hypervirulent Klebsiella pneumoniae: Does low expression of rmpA contribute to the absence of hypervirulence? Front. Microbiol. 2020, 11, 436. [Google Scholar] [CrossRef]
- Amraie, H.; Shakib, P.; Rouhi, S.; Bakhshandeh, N.; Zamanzad, B. Prevalence assessment of magA gene and antimicrobial susceptibility of Klebsiella pneumoniae isolated from clinical specimens in Shahrekord, Iran. Iran. J. Microbiol. 2014, 6, 311–316. [Google Scholar]
- Albarracin, L.; Ortiz Moyano, R.; Vargas, J.M.; Andrade, B.G.N.; Cortez Zamar, J.; Dentice Maidana, S.; Fukuyama, K.; Kurata, S.; Jure, M.Á.; Kitazawa, H.; et al. Genomic and Immunological Characterisation of Hypermucoviscous Carbapenem-Resistant Klebsiella pneumoniae ST25 Isolates from Northwest Argentina. Int. J. Mol. Sci. 2022, 23, 7316. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.T.; Chuang, Y.P.; Shun, C.T.; Chang, S.C.; Wang, J.T. A Novel Virulence Gene in Klebsiella pneumoniae Strains Causing Primary Liver Abscess and Septic Metastatic Complications. J. Exp. Med. 2004, 199, 697–705. [Google Scholar] [CrossRef] [PubMed]
- Zamani, A.; Mashouf, R.Y.; Namvar, A.M.E.; Alikhani, M.Y. Detection of magA gene in Klebsiella spp. isolated from clinical samples. Iran. J. Basic. Med. Sci. 2013, 16, 173–176. [Google Scholar]
- Yeh, K.-M.; Kurup, A.; Siu, L.K.; Koh, Y.L.; Fung, C.-P.; Lin, J.-C.; Chen, T.-L.; Chang, F.-Y.; Koh, T.-H. Capsular serotype K1 or K2, rather than magA and rmpA, is a major virulence determinant for Klebsiella pneumoniae liver abscess in Singapore and Taiwan. J. Clin. Microbiol. 2007, 45, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Chou, A.; Nuila, R.E.; Franco, L.M.; Stager, C.E.; Atmar, R.L.; Zechiedrich, L. Prevalence of hypervirulent Klebsiella pneumoniae-associated genes rmpA and magA in two tertiary hospitals in Houston, TX, USA. J. Med. Microbiol. 2016, 65, 1047–1048. [Google Scholar] [CrossRef]
- Chung, D.R.; Lee, S.S.; Lee, H.R.; Kim, H.B.; Choi, H.J.; Eom, J.S.; Kim, J.S.; Choi, Y.H.; Lee, J.S.; Chung, M.H.; et al. Emerging invasive liver abscess caused by K1 serotype Klebsiella pneumoniae in Korea. J. Infect. 2007, 54, 578–583. [Google Scholar] [CrossRef]
- Guo, Y.; Wang, S.; Zhan, L.; Jin, Y.; Duan, J.; Hao, Z.; Lv, J.; Qi, X.; Chen, L.; Kreiswirth, B.N.; et al. Microbiological and clinical characteristics of hypermucoviscous Klebsiella pneumoniae isolates associated with invasive infections in China. Front. Cell. Infect. Microbiol. 2017, 7, 24. [Google Scholar] [CrossRef]
- Sanikhani, R.; Moeinirad, M.; Solgi, H.; Hadadi, A.; Shahcheraghi, F.; Badmasti, F. The face of hypervirulent Klebsiella pneumoniae isolated from clinical samples of two Iranian teaching hospitals. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 1–13. [Google Scholar] [CrossRef]
- Candan, E.D.; Aksöz, N. Klebsiella pneumoniae: Characteristics of carbapenem resistance and virulence factors. Acta Biochim. Pol. 2015, 62, 867–874. [Google Scholar] [CrossRef] [PubMed]
- Gómez, M.; Valverde, A.; Del Campo, R.; Rodríguez, J.M.; Maldonado-Barragán, A. Phenotypic and molecular characterization of commensal, community-acquired and nosocomial Klebsiella spp. Microorganisms 2021, 9, 2344. [Google Scholar] [CrossRef] [PubMed]
- Holt, K.E.; Wertheim, H.; Zadoks, R.N.; Baker, S.; Whitehouse, C.A.; Dance, D.; Jenney, A.; Connor, T.R.; Hsu, L.Y.; Severin, J.; et al. Genomic analysis of diversity, population structure, virulence, and antimicrobial resistance in Klebsiella pneumoniae, an urgent threat to public health. Proc. Natl. Acad. Sci. USA 2015, 112, E3574–E3581. [Google Scholar] [CrossRef] [PubMed]
- Amaretti, A.; Righini, L.; Candeliere, F.; Musmeci, E.; Bonvicini, F.; Gentilomi, G.A.; Rossi, M.; Raimondi, S. Antibiotic resistance, virulence factors, phenotyping, and genotyping of non-Escherichia coli Enterobacterales from the gut microbiota of healthy subjects. Int. J. Mol. Sci. 2020, 21, 1847. [Google Scholar] [CrossRef] [PubMed]
- Remya, P.A.; Shanthi, M.; Sekar, U. Characterisation of virulence genes associated with pathogenicity in Kleb. Pneumoniae. Indian J. Med. Microbiol. 2019, 37, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Lepuschitz, S.; Hauser, K.; Schriebl, A.; Schlagenhaufen, C.; Stöger, A.; Chakeri, A.; Vötsch, K.; Pekard-Amenitsch, S.; Springer, B.; Allerberger, F.; et al. Fecal Klebsiella pneumoniae carriage is intermittent and of high clonal diversity. Front. Microbiol. 2020, 11, 581081. [Google Scholar] [CrossRef]
- Peng, W.; Wang, Y.; Fu, Y.; Deng, Z.; Lin, S.; Liang, R. Characterization of the Tellurite-Resistance Properties and Identification of the Core Function Genes for Tellurite Resistance in Pseudomonas citronellolis SJTE-3. Microorganisms 2022, 10, 95. [Google Scholar] [CrossRef]
- Passet, V.; Brisse, S. Association of tellurite resistance with hypervirulent clonal groups of Klebsiella pneumoniae. J. Clin. Microbiol. 2015, 53, 1380–1382. [Google Scholar] [CrossRef]
- Aher, T.; Roy, A.; Kumar, P. Molecular detection of virulence genes associated with pathogenicity of Klebsiella spp. isolated from the respiratory tract of apparently healthy as well as sick goats. Isr. J. Vet. Med. 2012, 67, 249–252. [Google Scholar]
- Guerra, M.E.S.; Destro, G.; Vieira, B.; Lima, A.S.; Ferraz, L.F.C.; Hakansson, A.P.; Darrieux, M.; Converso, T.R. Klebsiella pneumoniae Biofilms and Their Role in Disease Pathogenesis. Front. Cell. Infect. Microbiol. 2022, 12, 555. [Google Scholar] [CrossRef]
- Obaid, W.F.; Hasson, S.O. Pattern of Multi Drug Resistance with Biofilm Formation among Klebsiella pneumonia isolated from Fecal Samples of Diarrheal Iraqi Patients. Ann. Rom. Soc. Cell. Biol. 2021, 25, 5350–5360. [Google Scholar]
- Nirwati, H.; Sinanjung, K.; Fahrunissa, F.; Wijaya, F.; Napitupulu, S.; Hati, V.P.; Hakim, M.S.; Meliala, A.; Aman, A.T.; Nuryastuti, T. Biofilm formation and antibiotic resistance of Klebsiella pneumoniae isolated from clinical samples in a tertiary care hospital, Klaten, Indonesia. BMC Proc. 2019, 13, 20. [Google Scholar] [CrossRef]
- Hassan, A.; Usman, J.; Kaleem, F.; Omair, M.; Khalid, A.; Iqbal, M. Evaluation of different detection methods of biofilm formation in the clinical isolates. Braz. J. Infect. Dis. 2011, 15, 305–311. [Google Scholar] [CrossRef]
- Soto, E.; Dennis, M.M.; Beierschmitt, A.; Francis, S.; Sithole, F.; Halliday-Simmons, I.; Palmour, R. Biofilm formation of hypermucoviscous and non-hypermucoviscous Klebsiella pneumoniae recovered from clinically affected African green monkey (Chlorocebus aethiops sabaeus). Microb. Pathog. 2017, 107, 198–201. [Google Scholar] [CrossRef] [PubMed]
- Tutelyan, A.V.; Shlykova, D.S.; Voskanyan, S.L.; Gaponov, A.M.; Pisarev, V.M. Molecular Epidemiology of Hypervirulent, K. pneumoniae and Problems of Healthcare Associated Infections. Bull. Exp. Biol. Med. 2022, 172, 507–522. [Google Scholar] [CrossRef] [PubMed]
- Lan, Y.; Zhou, M.; Jian, Z.; Yan, Q.; Wang, S.; Liu, W. Prevalence of pks gene cluster and characteristics of Klebsiella pneumoniae-induced bloodstream infections. J. Clin. Lab. Anal. 2019, 33, e22838. [Google Scholar] [CrossRef] [PubMed]
- Huynh, B.-T.; Passet, V.; Rakotondrasoa, A.; Diallo, T.; Kerleguer, A.; Hennart, M.; De Lauzanne, A.; Herindrainy, P.; Seck, A.; Bercion, R.; et al. Klebsiella pneumoniae carriage in low-income countries: Antimicrobial resistance, genomic diversity and risk factors. Gut. Microbes 2020, 11, 1287–1299. [Google Scholar] [CrossRef]
- Bhurle, A.; Devnikar, A.; Sonth, S.; Solabannavar, S. Antibiogram and Detection of ESBL Production in Klebsiella species Isolated from Various Clinical Samples. Int. J. Curr. Microbiol. Appl. Sci. 2018, 7, 1184–1189. [Google Scholar] [CrossRef]
- Rock, C.; Thom, K.A.; Masnick, M.; Johnson, J.K.; Harris, A.D.; Morgan, D.J. Frequency of Klebsiella pneumoniae carbapenemase (KPC)–producing and non-KPC-producing Klebsiella species contamination of healthcare workers and the environment. Infect. Control. Hosp. Epidemiol. 2014, 35, 426–429. [Google Scholar] [CrossRef]
- Gorrie, C.L.; Mirčeta, M.; Wick, R.R.; Edwards, D.J.; Thomson, N.R.; Strugnell, R.A.; Pratt, N.F.; Garlick, J.S.; Watson, K.M.; Pilcher, D.V.; et al. Gastrointestinal carriage is a major reservoir of Klebsiella pneumoniae infection in intensive care patients. Clin. Infect. Dis. 2017, 65, 208–215. [Google Scholar] [CrossRef]
- Paterson, D.L.; Mulazimoglu, L.; Casellas, J.M.; Ko, W.C.; Goossens, H.; Von Gottberg, A.; Mohapatra, S.; Trenholme, G.M.; Klugman, K.P.; McCormack, J.G.; et al. Epidemiology of ciprofloxacin resistance and its relationship to extended-spectrum β-lactamase production in Klebsiella pneumoniae isolates causing bacteremia. Clin. Infect. Dis. 2000, 30, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Karimi, K.; Zarei, O.; Sedighi, P.; Taheri, M.; Doosti-Irani, A.; Shokoohizadeh, L. Investigation of antibiotic resistance and biofilm formation in clinical isolates of Klebsiella pneumoniae. Int. J. Microbiol. 2021, 5573388. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.P.; Rama, P.S.; Gurushanthappa, V.; Manipura, R.; Srinivasan, K. Extended-spectrum beta-lactamases producing Escherichia coli and Klebsiella pneumoniae: A multi-centric study across Karnataka. J. Lab. Physicians 2014, 6, 7–13. [Google Scholar] [PubMed]
- Elmonir, W.; El-Aziz, N.A.; Tartor, Y.; Moustafa, S.; Remela, E.A.; Eissa, R.; Saad, H.; Tawab, A. Emergence of colistin and carbapenem resistance in extended-spectrum β-lactamase producing Klebsiella pneumoniae isolated from chickens and humans in Egypt. Biology 2021, 10, 373. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. WHO 2017, 2017, 1–7. [Google Scholar]
- Pouch, S.M.; Patel, G. Multidrug-resistant Gram-negative bacterial infections in solid organ transplant recipients—Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin. Transpl. 2019, 33, e13594. [Google Scholar] [CrossRef]
- Tawfick, M.M.; Elshamy, A.A.; Mohamed, K.T.; El Menofy, N.G. Gut commensal Escherichia coli, a high-risk reservoir of transferable plasmid-mediated antimicrobial resistance traits. Infect. Drug. Resist. 2022, 15, 1077–1091. [Google Scholar] [CrossRef]
| Antimicrobial Agent | Susceptibility | HmvKp | Non-HmvKp | ||||
|---|---|---|---|---|---|---|---|
| No. | % 1 | No. | % 2 | No. | % 2 | ||
| Gentamicin | S | 27 | 54% | 10 | 37% | 17 | 63% |
| R | 23 | 46% | 11 | 47.8% | 12 | 52.2% | |
| Amikacin | S | 37 | 74% | 14 | 37.8% | 23 | 62.2% |
| R | 13 | 26% | 7 | 53.8% | 6 | 46.2% | |
| Amoxicillin-clavulanic acid | S | 14 | 28% | 2 | 14.3% | 12 | 85.7% |
| R | 36 | 72% | 19 | 52.8% | 17 | 47.2% | |
| Piperacillin-Tazobactam | S | 26 | 52% | 10 | 38.5% | 16 | 61.5% |
| R | 24 | 48% | 11 | 45.8% | 13 | 54.2% | |
| Cefotaxime | S | 3 | 6% | 2 | 66.7% | 1 | 33.3% |
| R | 47 | 94% | 19 | 40.4% | 28 | 59.6% | |
| Ceftazidime | S | 15 | 30% | 7 | 46.7% | 8 | 53.3% |
| R | 35 | 70% | 14 | 40% | 21 | 60% | |
| Aztreonam | S | 15 | 30% | 6 | 40% | 9 | 60% |
| R | 35 | 70% | 15 | 42.9% | 20 | 57.1% | |
| Imipenem | S | 23 | 46% | 9 | 39% | 14 | 61% |
| R | 27 | 54% | 12 | 44.4% | 15 | 55.6% | |
| Meropenem | S | 26 | 52% | 9 | 34.6% | 17 | 65.4% |
| R | 24 | 48% | 12 | 50% | 12 | 50% | |
| Ertapenem | S | 29 | 58% | 10 | 34.5% | 19 | 65.5% |
| R | 21 | 42% | 11 | 52.4% | 10 | 47.6% | |
| Ciprofloxacin | S | 0 | 0% | 0 | 0% | 0 | 0% |
| R | 50 | 100% | 21 | 42% | 29 | 58% | |
| Tetracycline | S | 20 | 40% | 5 | 25% | 15 | 75% |
| R | 30 | 60% | 16 | 53.3% | 14 | 46.7% | |
| Colistin | S | 43 | 86% | 21 | 48.8% | 22 | 51.2% |
| R | 7 | 14% | 0 | 0% | 7 | 100% | |
| ESBLs producer | 38 | 76% 3 | 15 | 39.5% | 23 | 60.5% | |
| Target Gene | Total No. (%) 1 | HmvKp (n = 21) | Non-HmvKp (n = 29) | ||||
|---|---|---|---|---|---|---|---|
| No. | % 2 | % 3 | No. | % 2 | % 4 | ||
| For Capsular Serotype | |||||||
| serotype K1 (magA) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| serotype K2 (wzy) | 15 (30%) | 13 | 86.7% | 61.9% | 2 | 13.3% | 6.9% |
| Virulence Genes | |||||||
| terW | 49 (98%) | 21 | 42.9% | 100% | 28 | 57.1% | 96.6% |
| wabG | 48 (96%) | 19 | 39.6% | 90.5% | 29 | 60.4% | 100% |
| uge | 47 (94%) | 18 | 38.3% | 85.7% | 29 | 61.7% | 100% |
| entB | 46 (92%) | 19 | 41.3% | 90.5% | 27 | 58.7% | 93.1% |
| irp2 | 37 (74%) | 9 | 24.3% | 42.9% | 28 | 75.7% | 96.6% |
| KfuBc | 22 (44%) | 8 | 36.4% | 38.1% | 14 | 63.6% | 48.3% |
| iucA | 1 (2%) | 1 | 100% | 4.8% | 0 | 0% | 0% |
| iroB, rmpA, rmpA2 | 0 | 0 | 0% | 0% | 0 | 0% | 0% |
| Genotypic Profile | Total No. (%) 1 | HmvKp (n = 21) | Non-HmvKp (n = 29) | ||
|---|---|---|---|---|---|
| No. | % 2 | No. | % 3 | ||
| terW-KfuBc-wabG-uge-irp2-entB | 13 (26%) | 0 | 0% | 13 | 44.8% |
| terW-wabG-uge-irp2-entB | 12 (24%) | 0 | 0% | 12 | 41.4% |
| terW-wabG-uge-entB | 3 (6%) | 3 | 14.3% | 0 | 0% |
| terW-wabG-uge-entB-K2 | 3 (6%) | 3 | 14.3% | 0 | 0% |
| terW-KfuBc-wabG-uge-irp2-entB-K2 | 3 (6%) | 3 | 14.3% | 0 | 0% |
| terW-wabG-uge-irp2-entB | 2 (4%) | 2 | 9.5% | 0 | 0% |
| terW-wabG-uge-irp2-entB-K2 | 2 (4%) | 2 | 9.5% | 0 | 0% |
| KfuBc-wabG-uge-entB | 1 (2%) | 0 | 0% | 1 | 3.4% |
| terW-KfuBc-wabG-uge-entB | 1 (2%) | 1 | 4.8% | 0 | 0% |
| terW-wabG-uge-irp2 | 1 (2%) | 0 | 0% | 1 | 3.4% |
| terW-wabG-uge-irp2-entB-K2 | 1 (2%) | 0 | 0% | 1 | 3.4% |
| terW-wabG-uge-irp2-K2 | 1 (2%) | 0 | 0% | 1 | 3.4% |
| terW-uge-entB | 1 (2%) | 1 | 4.8% | 0 | 0% |
| terW-KfuBc-uge-entB-K2 | 1 (2%) | 1 | 4.8% | 0 | 0% |
| terW-KfuBc-wabG-irp2-entB | 1 (2%) | 1 | 4.8% | 0 | 0% |
| terW-KfuBc-wabG-K2 | 1 (2%) | 1 | 4.8% | 0 | 0% |
| terW-KfuBc-wabG-uge--K2 | 1 (2%) | 1 | 4.8% | 0 | 0% |
| terW-wabG-irp2-entB-K2 | 1 (2%) | 1 | 4.8% | 0 | 0% |
| terW-wabG-uge-entB-K2-iucA | 1 (2%) | 1 | 4.8% | 0 | 0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osama, D.M.; Zaki, B.M.; Khalaf, W.S.; Mohamed, M.Y.A.; Tawfick, M.M.; Amin, H.M. Occurrence and Molecular Study of Hypermucoviscous/Hypervirulence Trait in Gut Commensal K. pneumoniae from Healthy Subjects. Microorganisms 2023, 11, 704. https://doi.org/10.3390/microorganisms11030704
Osama DM, Zaki BM, Khalaf WS, Mohamed MYA, Tawfick MM, Amin HM. Occurrence and Molecular Study of Hypermucoviscous/Hypervirulence Trait in Gut Commensal K. pneumoniae from Healthy Subjects. Microorganisms. 2023; 11(3):704. https://doi.org/10.3390/microorganisms11030704
Chicago/Turabian StyleOsama, Dina M., Bishoy M. Zaki, Wafaa S. Khalaf, Marwa Yousry A. Mohamed, Mahmoud M. Tawfick, and Heba M. Amin. 2023. "Occurrence and Molecular Study of Hypermucoviscous/Hypervirulence Trait in Gut Commensal K. pneumoniae from Healthy Subjects" Microorganisms 11, no. 3: 704. https://doi.org/10.3390/microorganisms11030704
APA StyleOsama, D. M., Zaki, B. M., Khalaf, W. S., Mohamed, M. Y. A., Tawfick, M. M., & Amin, H. M. (2023). Occurrence and Molecular Study of Hypermucoviscous/Hypervirulence Trait in Gut Commensal K. pneumoniae from Healthy Subjects. Microorganisms, 11(3), 704. https://doi.org/10.3390/microorganisms11030704





