Assessment of the Virulence of the Burkholderia mallei Strain BAC 86/19 in BALB/c Mice
Abstract
1. Introduction
2. Materials and Methods
2.1. Bacteria
2.2. Mice Infection
2.3. Bacteremia
2.4. Determination of CFU in Tissues
2.5. Statistics
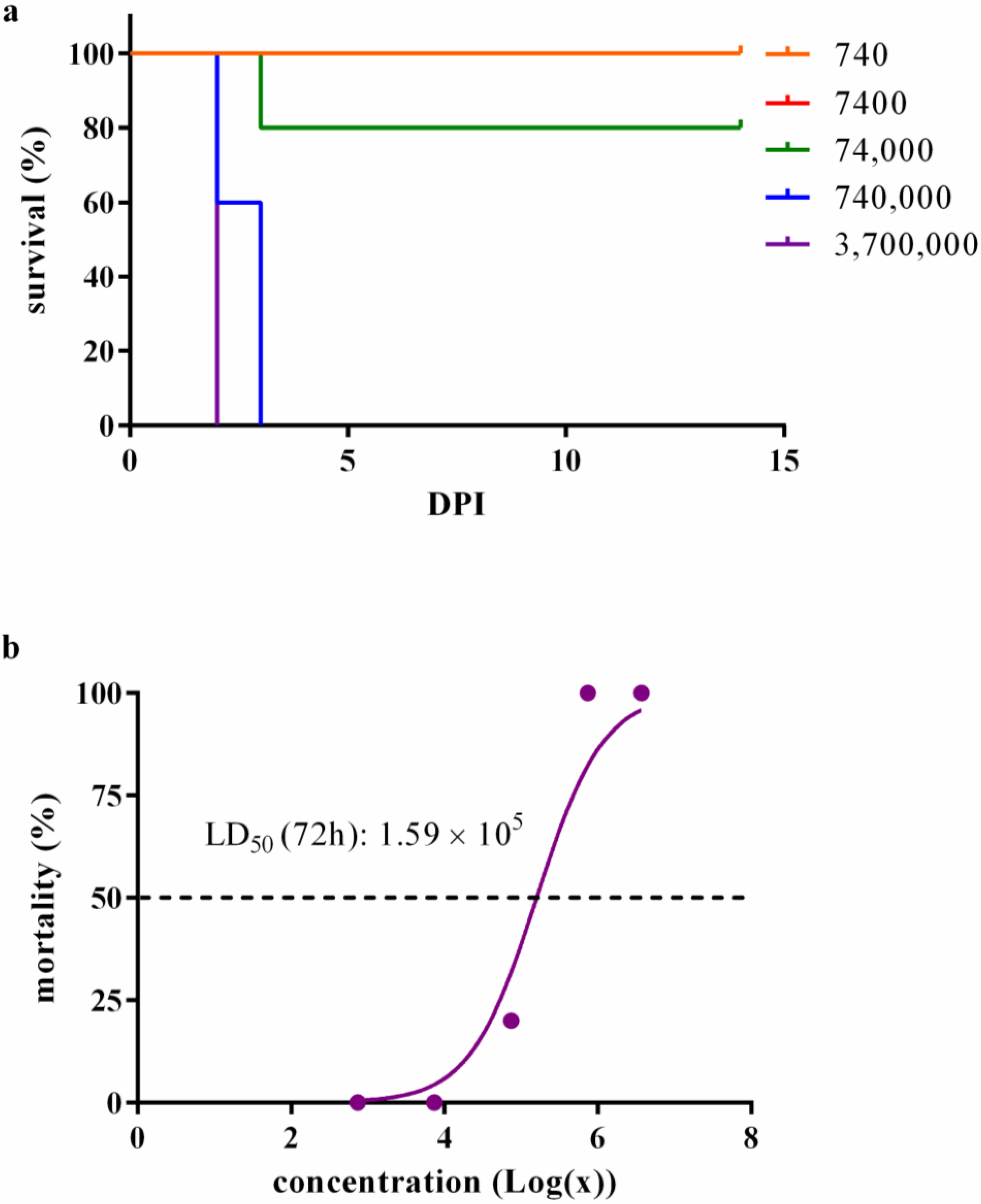
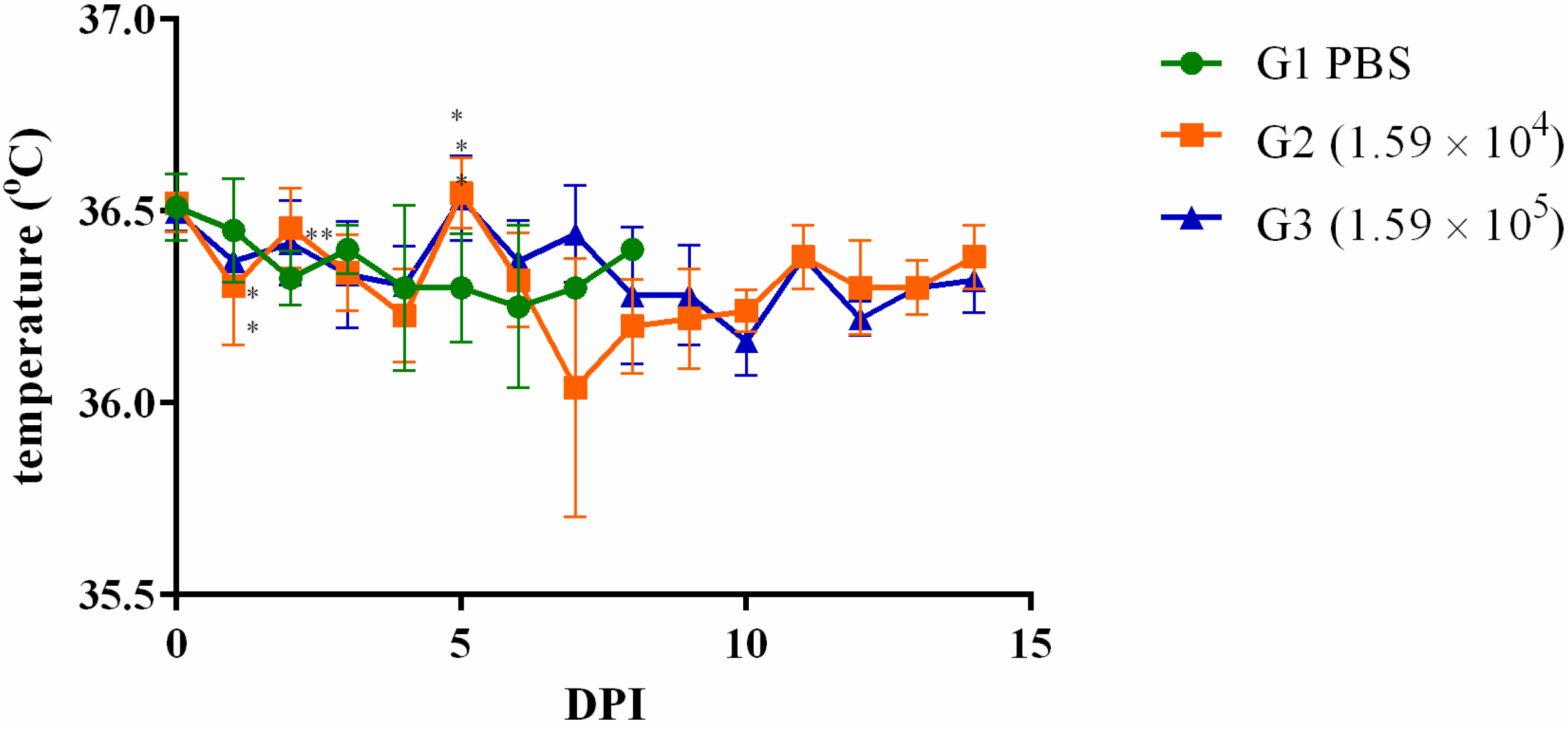
3. Results
4. Discussion
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Whitlock, G.C.; Mark Estes, D.; Torres, A.G. Glanders: Off to the races with Burkholderia mallei. FEMS Microbiol. Lett. 2007, 277, 115–122. [Google Scholar] [CrossRef]
- Van Zandt, K.E.; Greer, M.T.; Gelhaus, H.C. Glanders: An overview of infection in humans. Orphanet J. Rare Dis. 2013, 8, 131. [Google Scholar] [CrossRef]
- Khan, A.S.; Levitt, A.M.; Sage, M.J. Biological and chemical terrorism; strategic plan for preparedness and response: Recommendations of the CDC Strategic Planning Workgroup. MMWR Morb. Mortal. Wkly. Rep. 2000, 49, 1–14. [Google Scholar]
- Georgiev, V.S. Defense Against Biological Weapons (Biodefense). In National Institute of Allergy and Infectious Diseases, NIH; Humana Press: Totowa, NJ, USA, 2009; pp. 221–305. [Google Scholar] [CrossRef]
- Khan, I.; Wieler, L.H.; Melzer, F.; Elschner, M.C.; Muhammad, G.; Ali, S.; Sprague, L.D.; Neubauer, H.; Saqib, M. Glanders in animals: A review on epidemiology, clinical presentation, diagnosis and countermeasures. Transbound. Emerg. Dis. 2013, 60, 204–221. [Google Scholar] [CrossRef]
- Neubauer, H.; Sprague, L.D.; Zacharia, R.; Tomaso, H.; Al Dahouk, S.; Wernery, R.; Wernery, U.; Scholz, H.C. Serodiagnosis of Burkholderia mallei infections in horses: State-of-the-art and perspectives. J. Vet. Med. B Infect. Dis. Vet. Public Health 2005, 52, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Kettle, A.N.B.; Nicoletti, P.L. Glanders. In Equine Infectious Diseases; Sellon, D.C., Long, M.T., Eds.; Sauders Elsevier: St. Louis, MO, USA, 2013; pp. 333–337. [Google Scholar]
- Dvorak, G.D.; Spickler, A.R. Glanders. J. Am. Vet. Med. Assoc. 2008, 233, 570–577. [Google Scholar] [CrossRef]
- Mota, R.A.; Brito, M.F.; Castro, F.J.; Massa, M. Glanders in horses and mules of the states of Pernambuco and Alagoas, Brazil. Pesqui. Vet. Bras. 2000, 20, 155–159. [Google Scholar] [CrossRef]
- Mota, R.A.; Junior, J.W.P. Current status of glanders in Brazil: Recent advances and challenges. Braz. J. Microbiol. 2022, 53, 2273–2285. [Google Scholar] [CrossRef] [PubMed]
- Judy, B.M.; Whitlock, G.C.; Torres, A.G.; Estes, D.M. Comparison of the in vitro and in vivo susceptibilities of Burkholderia mallei to Ceftazidime and Levofloxacin. BMC Microbiol. 2009, 9, 88. [Google Scholar] [CrossRef]
- Mott, T.M.; Vijayakumar, S.; Sbrana, E.; Endsley, J.J.; Torres, A.G. Characterization of the Burkholderia mallei tonB mutant and its potential as a backbone strain for vaccine development. PLoS Neglected Trop. Dis. 2015, 9, e0003863. [Google Scholar] [CrossRef]
- DeShazer, D.; Waag, D.M.; Fritz, D.L.; Woods, D.E. Identification of a Burkholderia mallei polysaccharide gene cluster by subtractive hybridization and demonstration that the encoded capsule is an essential virulence determinant. Microb. Pathog. 2001, 30, 253–269. [Google Scholar] [CrossRef]
- Wikraiphat, C.; Charoensap, J.; Utaisincharoen, P.; Wongratanacheewin, S.; Taweechaisupapong, S.; Woods, D.E.; Bolscher, J.G.; Sirisinha, S. Comparative in vivo and in vitro analyses of putative virulence factors of Burkholderia pseudomallei using lipopolysaccharide, capsule and flagellin mutants. FEMS Immunol. Med. Microbiol. 2009, 56, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Schell, M.A.; Ulrich, R.L.; Ribot, W.J.; Brueggemann, E.E.; Hines, H.B.; Chen, D.; Lipscomb, L.; Kim, H.S.; Mrázek, J.; Nierman, W.C. Type VI secretion is a major virulence determinant in Burkholderia mallei. Mol. Microbiol. 2007, 64, 1466–1485. [Google Scholar] [CrossRef] [PubMed]
- Memišević, V.; Zavaljevski, N.; Pieper, R.; Rajagopala, S.V.; Kwon, K.; Townsend, K.; Yu, C.; Yu, X.; DeShazer, D.; Reifman, J. Novel Burkholderia mallei virulence factors linked to specific host-pathogen protein interactions. Mol. Cell. Proteom. 2013, 12, 3036–3051. [Google Scholar] [CrossRef] [PubMed]
- Brangsch, H.; Saqib, M.; Sial, A.U.R.; Melzer, F.; Linde, J.; Elschner, M.C. Sequencing-Based Genotyping of Pakistani Burkholderia mallei Strains: A Useful Way for Investigating Glanders Outbreaks. Pathogens 2022, 11, 614. [Google Scholar] [CrossRef]
- Appelt, S.; Rohleder, A.M.; Jacob, D.; von Buttlar, H.; Georgi, E.; Mueller, K.; Wernery, U.; Kinne, J. Genetic diversity and spatial distribution of Burkholderia mallei by core genome-based multilocus sequence typing analysis. PLoS ONE 2022, 17, e0270499. [Google Scholar] [CrossRef]
- Winn, W.C.; Allen, S.D.; Janda, M.W.; Koneman, E.W.; Procop, G.W.; Schreckenberger, P.C.; Woods, G.L. Bacilos Gram-negativos não fermentadores. In Diagnóstico Microbiológico: Texto e Atlas Colorido, 6th ed.; Koneman, E.W., Ed.; Guanabara Koogan: Rio de Janeiro, Brazil, 2008. [Google Scholar]
- Quinn, P.; Markey, B.K.; Carter, M.E.; Donnelly, W.; Leonard, F.C. Microbiologia Veterinária e Doenças Infecciosas; Artmed Editora: Porto Alegre, Brazil, 2005. [Google Scholar]
- Merwyn, S.; Kumar, S.; Agarwal, G.; Rai, G. Evaluation of PCR, DNA hybridization and immunomagnetic separation—PCR for detection of Burkholderia mallei in artificially inoculated environmental samples. Indian J. Microbiol. 2010, 50, 172–178. [Google Scholar] [CrossRef][Green Version]
- Abreu, D.C.; Gomes, A.S.; Tessler, D.K.; Chiebao, D.P.; Del Fava, C.; Romaldini, A.H.d.C.N.; Araujo, M.C.; Pompei, J.; Marques, G.F.; Harakava, R. Systematic monitoring of glanders-infected horses by complement fixation test, bacterial isolation, and PCR. Vet. Anim. Sci. 2020, 10, 100147. [Google Scholar] [CrossRef]
- Lafontaine, E.R.; Zimmerman, S.M.; Shaffer, T.L.; Michel, F.; Gao, X.; Hogan, R.J. Use of a safe, reproducible, and rapid aerosol delivery method to study infection by Burkholderia pseudomallei and Burkholderia mallei in mice. PLoS ONE 2013, 8, e76804. [Google Scholar] [CrossRef]
- Moore, E.S.; Cleland, T.A.; Williams, W.O.; Peterson, C.M.; Singh, B.; Southard, T.L.; Pasch, B.; Labitt, R.N.; Daugherity, E.K. Comparing phlebotomy by tail tip amputation, facial vein puncture, and tail vein incision in C57BL/6 mice by using physiologic and behavioral metrics of pain and distress. J. Am. Assoc. Lab. Anim. Sci. 2017, 56, 307–317. [Google Scholar]
- Chen, C.-Y.; Nace, G.W.; Irwin, P.L. A 6 × 6 drop plate method for simultaneous colony counting and MPN enumeration of Campylobacter jejuni, Listeria monocytogenes, and Escherichia coli. J. Microbiol. Methods 2003, 55, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Falcão, M.V.D.; Silveira, P.P.; Santana, V.L.; da Rocha, L.O.; Chaves, K.P.; Mota, R.A. First record of Burkholderia mallei Turkey 10 strain originating from glanderous horses from Brazil. Braz. J. Microbiol. 2019, 50, 1125–1127. [Google Scholar] [CrossRef] [PubMed]
- Kettle, A.N.; Wernery, U. Glanders and the risk for its introduction through the international movement of horses. Equine Vet. J. 2016, 48, 654–658. [Google Scholar] [CrossRef] [PubMed]
- Suniga, P.A.P.; Mantovani, C.; Santos, M.G.; Rieger, J.S.G.; Gaspar, E.B.; Dos Santos, F.L.; Mota, R.A.; Chaves, K.P.; Egito, A.A.; Nassar, A.F.C. Molecular detection of Burkholderia mallei in different geographic regions of Brazil. Braz. J. Microbiol. 2023, 54, 1275–1285. [Google Scholar] [CrossRef]
- Fritz, D.; Vogel, P.; Brown, D.; Deshazer, D.; Waag, D. Mouse model of sublethal and lethal intraperitoneal glanders (Burkholderia mallei). Vet. Pathol. 2000, 37, 626–636. [Google Scholar] [CrossRef]
- Barnes, K.B.; Bayliss, M.; Davies, C.; Richards, M.I.; Laws, T.R.; Vente, A.; Harding, S.V. Efficacy of finafloxacin in a murine model of inhalational glanders. Front. Microbiol. 2022, 13, 1057202. [Google Scholar] [CrossRef]
- Peacock, S.J.; Schweizer, H.P.; Dance, D.A.; Smith, T.L.; Gee, J.E.; Wuthiekanun, V.; DeShazer, D.; Steinmetz, I.; Tan, P.; Currie, B.J. Management of accidental laboratory exposure to Burkholderia pseudomallei and B. mallei. Emerg. Infect. Dis. 2008, 14, e2. [Google Scholar] [CrossRef]
- Schully, K.L.; Bell, M.G.; Ward, J.M.; Keane-Myers, A.M. Oropharyngeal aspiration of Burkholderia mallei and Burkholderia pseudomallei in BALB/c mice. PLoS ONE 2014, 9, e115066. [Google Scholar] [CrossRef]
- Tapia, D.; Sanchez-Villamil, J.I.; Torres, A.G. Multicomponent gold nano-glycoconjugate as a highly immunogenic and protective platform against Burkholderia mallei. NPJ Vaccines 2020, 5, 82. [Google Scholar] [CrossRef]
- Khakhum, N.; Bharaj, P.; Myers, J.N.; Tapia, D.; Walker, D.H.; Endsley, J.J.; Torres, A.G. Evaluation of Burkholderia mallei Δ tonB Δ hcp1 (CLH001) as a live attenuated vaccine in murine models of glanders and melioidosis. PLoS Neglected Trop. Dis. 2019, 13, e0007578. [Google Scholar] [CrossRef]
- Hatcher, C.L.; Mott, T.M.; Muruato, L.A.; Sbrana, E.; Torres, A.G. Burkholderia mallei CLH001 attenuated vaccine strain is immunogenic and protects against acute respiratory glanders. Infect. Immun. 2016, 84, 2345–2354. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, S.M.; Michel, F.; Hogan, R.J.; Lafontaine, E.R. The autotransporter BpaB contributes to the virulence of Burkholderia mallei in an aerosol model of infection. PLoS ONE 2015, 10, e0126437. [Google Scholar] [CrossRef] [PubMed]
- Majerczyk, C.; Kinman, L.; Han, T.; Bunt, R.; Greenberg, E.P. Virulence of Burkholderia mallei quorum-sensing mutants. Infect. Immun. 2013, 81, 1471–1478. [Google Scholar] [CrossRef] [PubMed]
- Bozue, J.A.; Chaudhury, S.; Amemiya, K.; Chua, J.; Cote, C.K.; Toothman, R.G.; Dankmeyer, J.L.; Klimko, C.P.; Wilhelmsen, C.L.; Raymond, J.W. Phenotypic characterization of a novel virulence-factor deletion strain of Burkholderia mallei that provides partial protection against inhalational glanders in mice. Front. Cell. Infect. Microbiol. 2016, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Dyke, J.S.; Huertas-Diaz, M.C.; Michel, F.; Holladay, N.E.; Hogan, R.J.; He, B.; Lafontaine, E.R. The Peptidoglycan-associated lipoprotein Pal contributes to the virulence of Burkholderia mallei and provides protection against lethal aerosol challenge. Virulence 2020, 11, 1024–1040. [Google Scholar] [CrossRef]
- Massey, S.; Johnston, K.; Mott, T.M.; Judy, B.M.; Kvitko, B.H.; Schweizer, H.P.; Estes, D.M.; Torres, A.G. In vivo bioluminescence imaging of Burkholderia mallei respiratory infection and treatment in the mouse model. Front. Microbiol. 2011, 2, 174. [Google Scholar] [CrossRef]
- Zhang, S.; Feng, S.-H.; Li, B.; Kim, H.-Y.; Rodriguez, J.; Tsai, S.; Lo, S.-C. In vitro and in vivo studies of monoclonal antibodies with prominent bactericidal activity against Burkholderia pseudomallei and Burkholderia mallei. Clin. Vaccine Immunol. 2011, 18, 825–834. [Google Scholar] [CrossRef]
- Fritz, D.L.; Vogel, P.; Brown, D.R.; Waag, D.M. The hamster model of intraperitoneal Burkholderia mallei (glanders). Vet. Pathol. 1999, 36, 276–291. [Google Scholar] [CrossRef]
- Klimko, C.P.; Treviño, S.R.; Moreau, A.M.; Aponte Cuadrado, M.J.; Meyer, J.R.; Fetterer, D.P.; Welkos, S.L.; Worsham, P.L.; Kreiselmeier, N.; Soffler, C. The impact of age and sex on mouse models of melioidosis. Pathogens 2020, 9, 113. [Google Scholar] [CrossRef]
- Titball, R.W.; Russell, P.; Cuccui, J.; Easton, A.; Haque, A.; Atkins, T.; Sarkar-Tyson, M.; Harley, V.; Wren, B.; Bancroft, G.J. Burkholderia pseudomallei: Animal models of infection. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, S111–S116. [Google Scholar] [CrossRef]
- Whitlock, G.C.; Valbuena, G.A.; Popov, V.L.; Judy, B.M.; Estes, D.M.; Torres, A.G. Burkholderia mallei cellular interactions in a respiratory cell model. J. Med. Microbiol. 2009, 58, 554. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaspar, E.B.; Santos, L.R.d.; Egito, A.A.d.; Santos, M.G.d.; Mantovani, C.; Rieger, J.d.S.G.; Abrantes, G.A.d.S.; Suniga, P.A.P.; Favacho, J.d.M.; Pinto, I.B.; et al. Assessment of the Virulence of the Burkholderia mallei Strain BAC 86/19 in BALB/c Mice. Microorganisms 2023, 11, 2597. https://doi.org/10.3390/microorganisms11102597
Gaspar EB, Santos LRd, Egito AAd, Santos MGd, Mantovani C, Rieger JdSG, Abrantes GAdS, Suniga PAP, Favacho JdM, Pinto IB, et al. Assessment of the Virulence of the Burkholderia mallei Strain BAC 86/19 in BALB/c Mice. Microorganisms. 2023; 11(10):2597. https://doi.org/10.3390/microorganisms11102597
Chicago/Turabian StyleGaspar, Emanuelle Baldo, Lenita Ramires dos Santos, Andréa Alves do Egito, Maria Goretti dos Santos, Cynthia Mantovani, Juliana da Silva Gomes Rieger, Guilherme Augusto de Sousa Abrantes, Paula Adas Pereira Suniga, Júlia de Mendonça Favacho, Ingrid Batista Pinto, and et al. 2023. "Assessment of the Virulence of the Burkholderia mallei Strain BAC 86/19 in BALB/c Mice" Microorganisms 11, no. 10: 2597. https://doi.org/10.3390/microorganisms11102597
APA StyleGaspar, E. B., Santos, L. R. d., Egito, A. A. d., Santos, M. G. d., Mantovani, C., Rieger, J. d. S. G., Abrantes, G. A. d. S., Suniga, P. A. P., Favacho, J. d. M., Pinto, I. B., Nassar, A. F. d. C., Santos, F. L. d., & Araújo, F. R. d. (2023). Assessment of the Virulence of the Burkholderia mallei Strain BAC 86/19 in BALB/c Mice. Microorganisms, 11(10), 2597. https://doi.org/10.3390/microorganisms11102597





