High Levels of IL-1β, TNF-α and MIP-1α One Month after the Onset of the Acute SARS-CoV-2 Infection, Predictors of Post COVID-19 in Hospitalized Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients’ Selection and Experimental Design
2.2. Plasma Cytokines Quantification
2.3. Reactive Oxygen Species (ROS) Quantification
2.4. Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics of the Study Population
3.2. Post COVID-19 Symptomatology
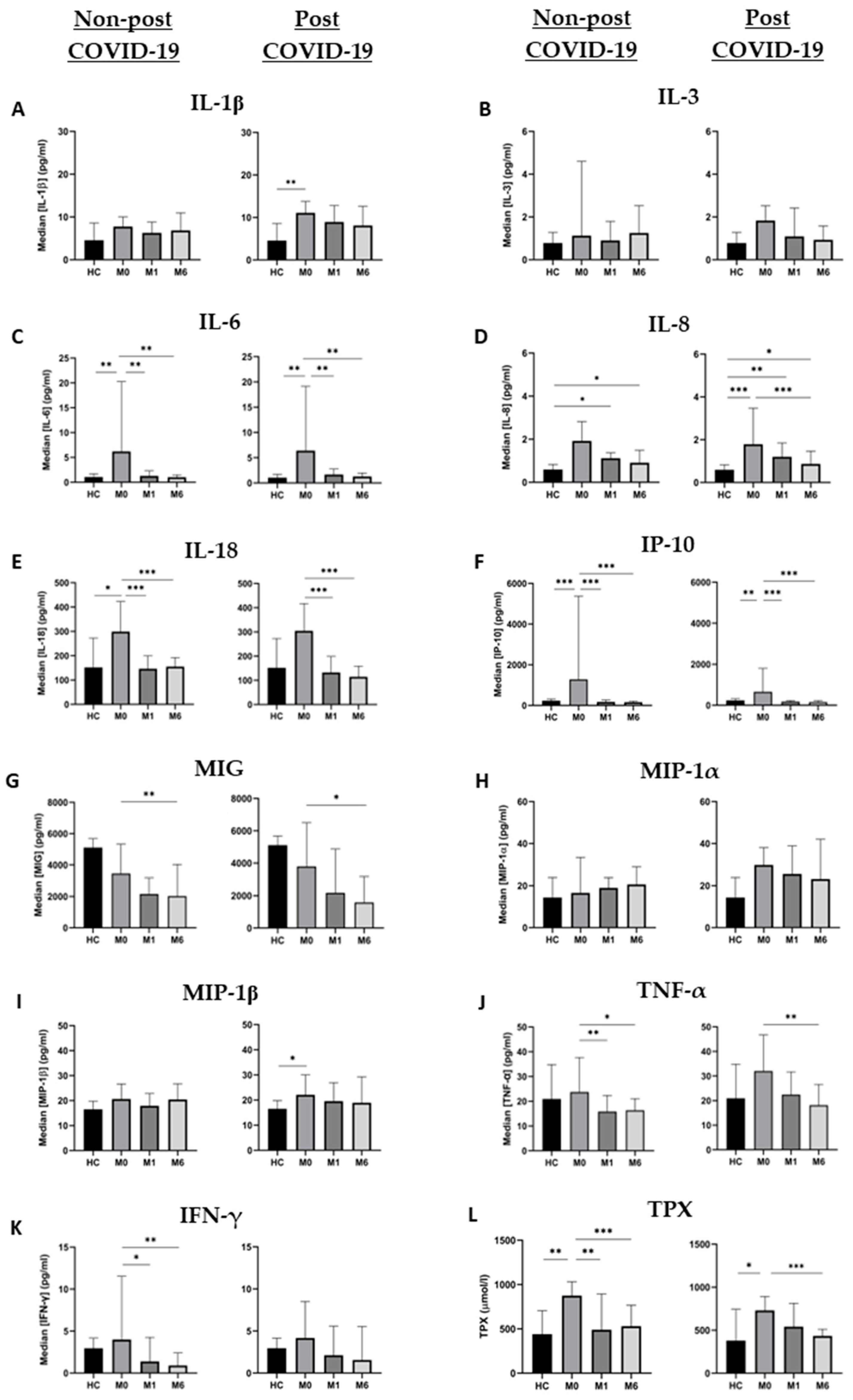
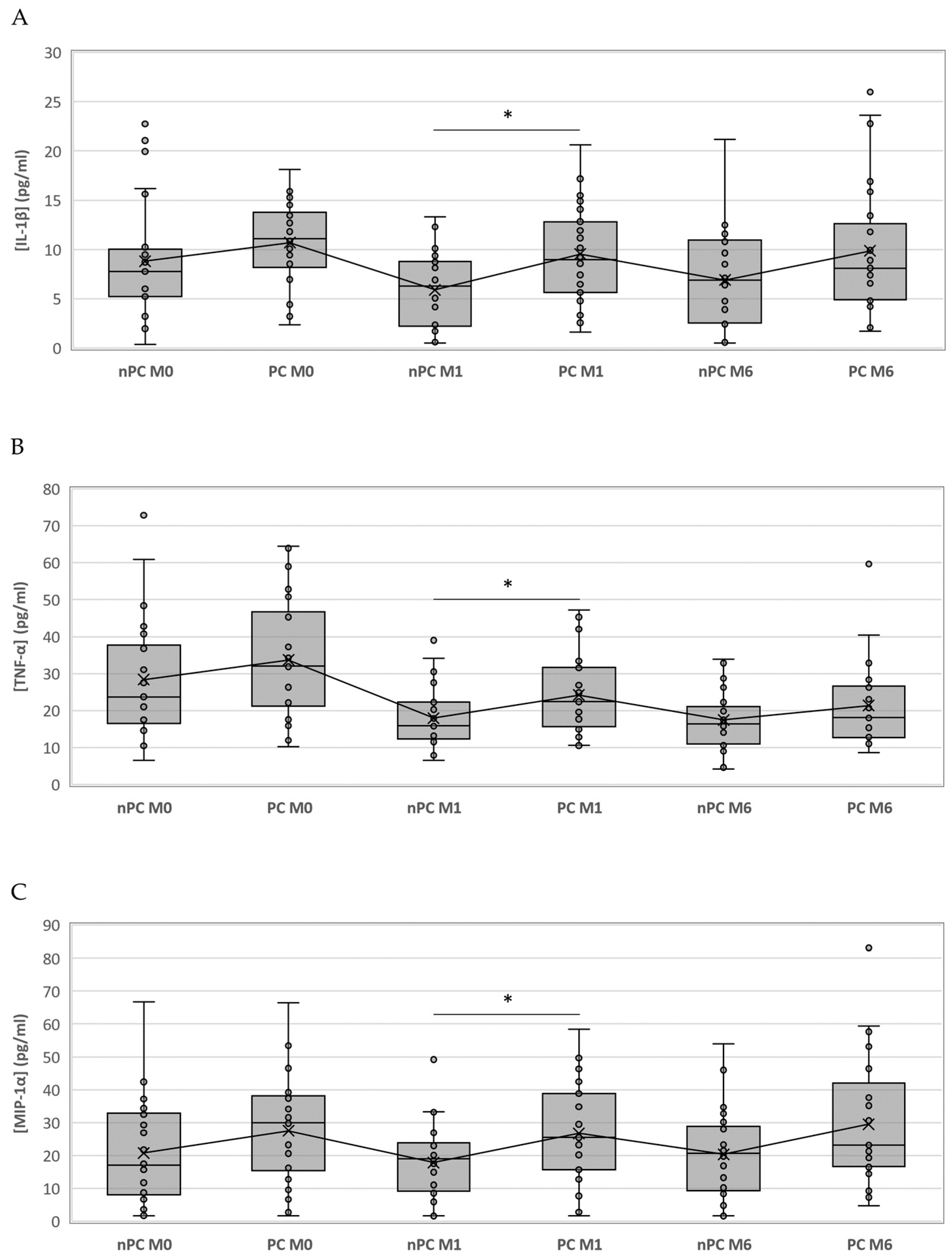
3.3. Non-Post and Post COVID-19 Cytokine Dynamics
3.4. Non-Post and Post COVID-19 Total Peroxides Dynamics
3.5. Predictive Model for Post COVID-19
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sharma, A.; Tiwari, S.; Deb, M.K.; Marty, J.L. Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2): A Global Pandemic and Treatment Strategies. Int. J. Antimicrob. Agents 2020, 56, 106054. [Google Scholar] [CrossRef] [PubMed]
- With the International Public Health Emergency Ending, WHO/Europe Launches Its Transition Plan for COVID-19. Available online: https://www.who.int/europe/news/item/12-06-2023-with-the-international-public-health-emergency-ending--who-europe-launches-its-transition-plan-for-covid-19 (accessed on 25 August 2023).
- Lai, C.-C.; Shih, T.-P.; Ko, W.-C.; Tang, H.-J.; Hsueh, P.-R. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus Disease-2019 (COVID-19): The Epidemic and the Challenges. Int. J. Antimicrob. Agents 2020, 55, 105924. [Google Scholar] [CrossRef] [PubMed]
- Montani, D.; Savale, L.; Noel, N.; Meyrignac, O.; Colle, R.; Gasnier, M.; Corruble, E.; Beurnier, A.; Jutant, E.-M.; Pham, T.; et al. Post-Acute COVID-19 Syndrome. Eur. Respir. Rev. 2022, 31, 210185. [Google Scholar] [CrossRef]
- Post COVID-19 Condition (Long COVID). Available online: https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition#:~:text=Definition,months%20with%20no%20other%20explanation (accessed on 4 July 2023).
- Romero-Duarte, Á.; Rivera-Izquierdo, M.; Guerrero-Fernández de Alba, I.; Pérez-Contreras, M.; Fernández-Martínez, N.F.; Ruiz-Montero, R.; Serrano-Ortiz, Á.; González-Serna, R.O.; Salcedo-Leal, I.; Jiménez-Mejías, E.; et al. Sequelae, Persistent Symptomatology and Outcomes after COVID-19 Hospitalization: The ANCOHVID Multicentre 6-Month Follow-up Study. BMC Med. 2021, 19, 129. [Google Scholar] [CrossRef] [PubMed]
- Wahlgren, C.; Forsberg, G.; Divanoglou, A.; Östholm Balkhed, Å.; Niward, K.; Berg, S.; Levi, R. Two-Year Follow-up of Patients with Post-COVID-19 Condition in Sweden: A Prospective Cohort Study. Lancet Reg. Health-Eur. 2023, 28, 100595. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major Findings, Mechanisms and Recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Maamar, M.; Artime, A.; Pariente, E.; Fierro, P.; Ruiz, Y.; Gutiérrez, S.; Tobalina, M.; Díaz-Salazar, S.; Ramos, C.; Olmos, J.M.; et al. Post-COVID-19 Syndrome, Low-Grade Inflammation and Inflammatory Markers: A Cross-Sectional Study. Curr. Med. Res. Opin. 2022, 38, 901–909. [Google Scholar] [CrossRef]
- Hu, B.; Huang, S.; Yin, L. The Cytokine Storm and COVID-19. J. Med. Virol. 2021, 93, 250–256. [Google Scholar] [CrossRef]
- Diarimalala, R.O.; Wei, Y.; Hu, D.; Hu, K. Inflammasomes during SARS-CoV-2 Infection and Development of Their Corresponding Inhibitors. Front. Cell Infect. Microbiol. 2023, 13, 1218039. [Google Scholar] [CrossRef]
- Williams, E.S.; Martins, T.B.; Shah, K.S.; Hill, H.R.; Coiras, M.; Spivak, A.M.; Planelles, V. Cytokine Deficiencies in Patients with Long-COVID. J. Clin. Cell Immunol. 2022, 13, 672. [Google Scholar]
- Peluso, M.J.; Lu, S.; Tang, A.F.; Durstenfeld, M.S.; Ho, H.; Goldberg, S.A.; Forman, C.A.; Munter, S.E.; Hoh, R.; Tai, V.; et al. Markers of Immune Activation and Inflammation in Individuals with Postacute Sequelae of Severe Acute Respiratory Syndrome Coronavirus 2 Infection. J. Infect. Dis. 2021, 224, 1839–1848. [Google Scholar] [CrossRef] [PubMed]
- Acosta-Ampudia, Y.; Monsalve, D.M.; Rojas, M.; Rodríguez, Y.; Zapata, E.; Ramírez-Santana, C.; Anaya, J.-M. Persistent Autoimmune Activation and Proinflammatory State in Post-Coronavirus Disease 2019 Syndrome. J. Infect. Dis. 2022, 225, 2155–2162. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.-J.; Liu, S.-H.; Manachevakul, S.; Lee, T.-A.; Kuo, C.-T.; Bello, D. Biomarkers in Long COVID-19: A Systematic Review. Front. Med. 2023, 10, 1085988. [Google Scholar] [CrossRef] [PubMed]
- Montazersaheb, S.; Hosseiniyan Khatibi, S.M.; Hejazi, M.S.; Tarhriz, V.; Farjami, A.; Ghasemian Sorbeni, F.; Farahzadi, R.; Ghasemnejad, T. COVID-19 Infection: An Overview on Cytokine Storm and Related Interventions. Virol. J. 2022, 19, 92. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, C.; Huang, F.; Yang, Y.; Wang, F.; Yuan, J.; Zhang, Z.; Qin, Y.; Li, X.; Zhao, D.; et al. Elevated Plasma Levels of Selective Cytokines in COVID-19 Patients Reflect Viral Load and Lung Injury. Natl. Sci. Rev. 2020, 7, 1003–1011. [Google Scholar] [CrossRef]
- Del Valle, D.M.; Kim-Schulze, S.; Huang, H.-H.; Beckmann, N.D.; Nirenberg, S.; Wang, B.; Lavin, Y.; Swartz, T.H.; Madduri, D.; Stock, A.; et al. An Inflammatory Cytokine Signature Predicts COVID-19 Severity and Survival. Nat. Med. 2020, 26, 1636–1643. [Google Scholar] [CrossRef]
- Codina, H.; Vieitez, I.; Gutierrez-Valencia, A.; Skouridou, V.; Martínez, C.; Patiño, L.; Botero-Gallego, M.; Trujillo-Rodríguez, M.; Serna-Gallego, A.; Muñoz-Muela, E.; et al. Elevated Anti-SARS-CoV-2 Antibodies and IL-6, IL-8, MIP-1β, Early Predictors of Severe COVID-19. Microorganisms 2021, 9, 2259. [Google Scholar] [CrossRef]
- Mahallawi, W.H.; Khabour, O.F.; Zhang, Q.; Makhdoum, H.M.; Suliman, B.A. MERS-CoV Infection in Humans Is Associated with a pro-Inflammatory Th1 and Th17 Cytokine Profile. Cytokine 2018, 104, 8–13. [Google Scholar] [CrossRef]
- Wong, C.K.; Lam, C.W.K.; Wu, A.K.L.; Ip, W.K.; Lee, N.L.S.; Chan, I.H.S.; Lit, L.C.W.; Hui, D.S.C.; Chan, M.H.M.; Chung, S.S.C.; et al. Plasma Inflammatory Cytokines and Chemokines in Severe Acute Respiratory Syndrome. Clin. Exp. Immunol. 2004, 136, 95–103. [Google Scholar] [CrossRef]
- Choudhury, S.M.; Ma, X.; Abdullah, S.W.; Zheng, H. Activation and Inhibition of the NLRP3 Inflammasome by RNA Viruses. J. Inflamm. Res. 2021, 14, 1145–1163. [Google Scholar] [CrossRef]
- Schultheiß, C.; Willscher, E.; Paschold, L.; Gottschick, C.; Klee, B.; Henkes, S.-S.; Bosurgi, L.; Dutzmann, J.; Sedding, D.; Frese, T.; et al. The IL-1β, IL-6, and TNF Cytokine Triad Is Associated with Post-Acute Sequelae of COVID-19. Cell Rep. Med. 2022, 3, 100663. [Google Scholar] [CrossRef] [PubMed]
- Kyriazopoulou, E.; Huet, T.; Cavalli, G.; Gori, A.; Kyprianou, M.; Pickkers, P.; Eugen-Olsen, J.; Clerici, M.; Veas, F.; Chatellier, G.; et al. Effect of Anakinra on Mortality in Patients with COVID-19: A Systematic Review and Patient-Level Meta-Analysis. Lancet Rheumatol. 2021, 3, e690–e697. [Google Scholar] [CrossRef] [PubMed]
- Patterson, B.K.; Francisco, E.B.; Yogendra, R.; Long, E.; Pise, A.; Rodrigues, H.; Hall, E.; Herrera, M.; Parikh, P.; Guevara-Coto, J.; et al. Persistence of SARS CoV-2 S1 Protein in CD16+ Monocytes in Post-Acute Sequelae of COVID-19 (PASC) up to 15 Months Post-Infection. Front. Immunol. 2022, 12, 746021. [Google Scholar] [CrossRef]
- Bertoni, A.; Penco, F.; Mollica, H.; Bocca, P.; Prigione, I.; Corcione, A.; Cangelosi, D.; Schena, F.; Del Zotto, G.; Amaro, A.; et al. Spontaneous NLRP3 Inflammasome-Driven IL-1-β Secretion Is Induced in Severe COVID-19 Patients and Responds to Anakinra Treatment. J. Allergy Clin. Immunol. 2022, 150, 796–805. [Google Scholar] [CrossRef] [PubMed]
- Pan, P.; Shen, M.; Yu, Z.; Ge, W.; Chen, K.; Tian, M.; Xiao, F.; Wang, Z.; Wang, J.; Jia, Y.; et al. SARS-CoV-2 N Protein Promotes NLRP3 Inflammasome Activation to Induce Hyperinflammation. Nat. Commun. 2021, 12, 4664. [Google Scholar] [CrossRef] [PubMed]
- Queiroz, M.A.F.; das Neves, P.F.M.; Lima, S.S.; da Lopes, J.C.; da Torres, M.K.S.; Vallinoto, I.M.V.C.; Bichara, C.D.A.; dos Santos, E.F.; de Brito, M.T.F.M.; da Silva, A.L.S.; et al. Cytokine Profiles Associated With Acute COVID-19 and Long COVID-19 Syndrome. Front. Cell Infect. Microbiol. 2022, 12, 922422. [Google Scholar] [CrossRef]
- Torres-Ruiz, J.; Lomelín-Gascón, J.; Lira Luna, J.; Vargas-Castro, A.S.; Pérez-Fragoso, A.; Nuñez-Aguirre, M.; Alcalá-Carmona, B.; Absalón-Aguilar, A.; Balderas-Miranda, J.T.; Maravillas-Montero, J.L.; et al. Novel Clinical and Immunological Features Associated with Persistent Post-Acute Sequelae of COVID-19 after Six Months of Follow-up: A Pilot Study. Infect. Dis. 2023, 55, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Newell, K.L.; Waickman, A.T. Inflammation, Immunity, and Antigen Persistence in Post-Acute Sequelae of SARS-CoV-2 Infection. Curr. Opin. Immunol. 2022, 77, 102228. [Google Scholar] [CrossRef]
- Liu, Q.; Mak, J.W.Y.; Su, Q.; Yeoh, Y.K.; Lui, G.C.-Y.; Ng, S.S.S.; Zhang, F.; Li, A.Y.L.; Lu, W.; Hui, D.S.-C.; et al. Gut Microbiota Dynamics in a Prospective Cohort of Patients with Post-Acute COVID-19 Syndrome. Gut 2022, 71, 544–552. [Google Scholar] [CrossRef]
- Pérez-González, A.; Araújo-Ameijeiras, A.; Fernández-Villar, A.; Crespo, M.; Poveda, E.; Cabrera, J.J.; del Campo, V.; de Araujo, B.G.; Gómez, C.; Leiro, V.; et al. Long COVID in Hospitalized and Non-Hospitalized Patients in a Large Cohort in Northwest Spain, a Prospective Cohort Study. Sci. Rep. 2022, 12, 3369. [Google Scholar] [CrossRef]

| Controls | Total | Post COVID | Non-Post COVID | p-Value | |
|---|---|---|---|---|---|
| Patients in follow-up, n (%) | 14 | 54 (100%) | 27 (50%) | 27 (50%) | |
| Demographics | |||||
| Age, in years, median [IQR] | 53.5 [47–57] | 59.5 [51.25–68] | 58 [52–64] | 62 [51–68.5] | p = 0.342 |
| <55 | 7 (50%) | 18 (33.33%) | 10 (37.04%) | 8 (29.63%) | |
| ≥55 | 7 (50%) | 36 (66.67%) | 17 (62.96%) | 19 (70.37%) | |
| Male sex, n (%) | 8 (57.14) | 22 (40.74%) | 11 (40.74%) | 11 (40.74%) | p = 1.000 |
| Comorbidities | |||||
| Obesity, n (%) | 2 (14.29%) | 20 (37.04%) | 12 (44.44%) | 8 (29.63%) | p = 0.398 |
| Hypertension, n (%) | 1 (7.14%) | 17 (31.48%) | 8 (29.63%) | 9 (33.33%) | p = 1.000 |
| Chronic obstructive pulmonary disease, n (%) | 0 (0%) | 4 (7.41%) | 3 (11.11%) | 1 (3.70%) | p = 0.610 |
| Diabetes mellitus, n (%) | 0 (0%) | 10 (18.52%) | 4 (14.81%) | 6 (22.22%) | p = 0.728 |
| Asthma, n (%) | 0 (0%) | 4 (7.41%) | 4 (14.81%) | 0 (0%) | p = 0.111 |
| HIV infection, n (%) | 0 (0%) | 2 (3.70%) | 2 (7.4%) | 0 (0%) | p = 0.491 |
| Chronic kidney disease, n (%) | 0 (0%) | 1 (1.85%) | 1 (3.7%) | 0 (0%) | p = 1.000 |
| Chronic inflammatory disease | 0 (0%) | 2 (3.7%) | 1 (3.7%) | 1 (3.7%) | p = 1.000 |
| Severity | |||||
| Days from symptoms onset to SARS-CoV-2 confirmation, median [IQR] | 4 [2–7] | 4 [2–9] | 5 [3–7] | p = 1.000 | |
| Days of hospitalization, median [IQR] | 7 [4–9.75] | 6 [4–15] | 8 [5–9] | p = 0.610 | |
| Admission to ICU, n (%) | 11 (20.37%) | 6 (22.22%) | 5 (18.52%) | p = 1.000 | |
| Days in ICU, median [IQR] | 13 [6–19] | 15.5 [12.5–23.75] | 8 [5–8] | p = 0.113 | |
| Invasive mechanical ventilation, n (%) | 8 (14.81%) | 5 (18.52%) | 3 (11.11%) | p = 0.704 | |
| Tobacco use | |||||
| Active smoker, n (%) | 1 (7.14%) | 4 (7.41%) | 2 (7.41%) | 2 (7.41%) | p = 1.000 |
| Former smoker, n (%) | 5 (35.71%) | 26 (48.15%) | 13 (48.15%) | 13 (48.15%) | p = 1.000 |
| Post COVID | Non-Post COVID | p-Value | |
|---|---|---|---|
| Patients in follow-up, n | 27 | 27 | |
| Symptoms on admission | |||
| Fever, n (%) | 21 (77.78%) | 20 (74.07%) | p = 1.000 |
| Dyspnea, n (%) | 17 (62.96%) | 19 (70.37%) | p = 0.773 |
| Cough, n (%) | 17 (62.96%) | 17 (62.96%) | p = 1.000 |
| Diarrhea, n (%) | 9 (33.33%) | 9 (33.33%) | p = 1.000 |
| Myalgia, n (%) | 6 (22.22%) | 8 (29.63%) | p = 0.757 |
| Anosmia, n (%) | 5 (18.52%) | 8 (29.63%) | p = 0.526 |
| Chest pain, n (%) | 8 (29.63%) | 2 (7.41%) | p = 0.076 |
| ARDS, n (%) | 6 (22.22%) | 2 (7.41%) | p = 0.250 |
| Post COVID-19 | ||
|---|---|---|
| Patients in follow-up, n | 27 | |
| Nervous system symptoms, n (%) | 7 (25.93%) | |
| Anosmia, n (%) | 1 (3.70%) | |
| Ageusia, n (%) | 2 (7.40%) | |
| Headache, n (%) | 2 (7.40%) | |
| Migraine, n (%) | 1 (3.70%) | |
| Mood disorders, n (%) | 1 (3.70%) | |
| Behavioral disorder, n (%) | 3 (11.11%) | |
| Thoracic symptoms, n (%) | 16 (59.25%) | |
| Dyspnea | MRC 1, n (%) | 11 (40.74%) |
| MRC 2, n (%) | 2 (7.40%) | |
| MRC 3, n (%) | 0 (0%) | |
| MRC 4, n (%) | 0 (0%) | |
| Chest pain, n (%) | 3 (11.11%) | |
| Cough, n (%) | 3 (11.11%) | |
| Musculoskeletal Symptoms, n (%) | 7 (25.93%) | |
| Myalgias, n (%) | 3 (11.11%) | |
| Arthralgias, n (%) | 4 (14.81%) | |
| General symptoms, n (%) | 12 (44.44%) | |
| Asthenia, n (%) | 10 (37.03%) | |
| Hair loss, n (%) | 4 (14.81%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alonso-Domínguez, J.; Gallego-Rodríguez, M.; Martínez-Barros, I.; Calderón-Cruz, B.; Leiro-Fernández, V.; Pérez-González, A.; Poveda, E. High Levels of IL-1β, TNF-α and MIP-1α One Month after the Onset of the Acute SARS-CoV-2 Infection, Predictors of Post COVID-19 in Hospitalized Patients. Microorganisms 2023, 11, 2396. https://doi.org/10.3390/microorganisms11102396
Alonso-Domínguez J, Gallego-Rodríguez M, Martínez-Barros I, Calderón-Cruz B, Leiro-Fernández V, Pérez-González A, Poveda E. High Levels of IL-1β, TNF-α and MIP-1α One Month after the Onset of the Acute SARS-CoV-2 Infection, Predictors of Post COVID-19 in Hospitalized Patients. Microorganisms. 2023; 11(10):2396. https://doi.org/10.3390/microorganisms11102396
Chicago/Turabian StyleAlonso-Domínguez, Jacobo, María Gallego-Rodríguez, Inés Martínez-Barros, Beatriz Calderón-Cruz, Virginia Leiro-Fernández, Alexandre Pérez-González, and Eva Poveda. 2023. "High Levels of IL-1β, TNF-α and MIP-1α One Month after the Onset of the Acute SARS-CoV-2 Infection, Predictors of Post COVID-19 in Hospitalized Patients" Microorganisms 11, no. 10: 2396. https://doi.org/10.3390/microorganisms11102396
APA StyleAlonso-Domínguez, J., Gallego-Rodríguez, M., Martínez-Barros, I., Calderón-Cruz, B., Leiro-Fernández, V., Pérez-González, A., & Poveda, E. (2023). High Levels of IL-1β, TNF-α and MIP-1α One Month after the Onset of the Acute SARS-CoV-2 Infection, Predictors of Post COVID-19 in Hospitalized Patients. Microorganisms, 11(10), 2396. https://doi.org/10.3390/microorganisms11102396








