Antimicrobial Resistance and Clonal Lineages of Staphylococcus aureus from Cattle, Their Handlers, and Their Surroundings: A Cross-Sectional Study from the One Health Perspective
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Collection
2.2. S. aureus Isolation
2.3. Antimicrobial Susceptibility Testing
2.4. Antimicrobial Resistance and Virulence Genes
2.5. Molecular Typing
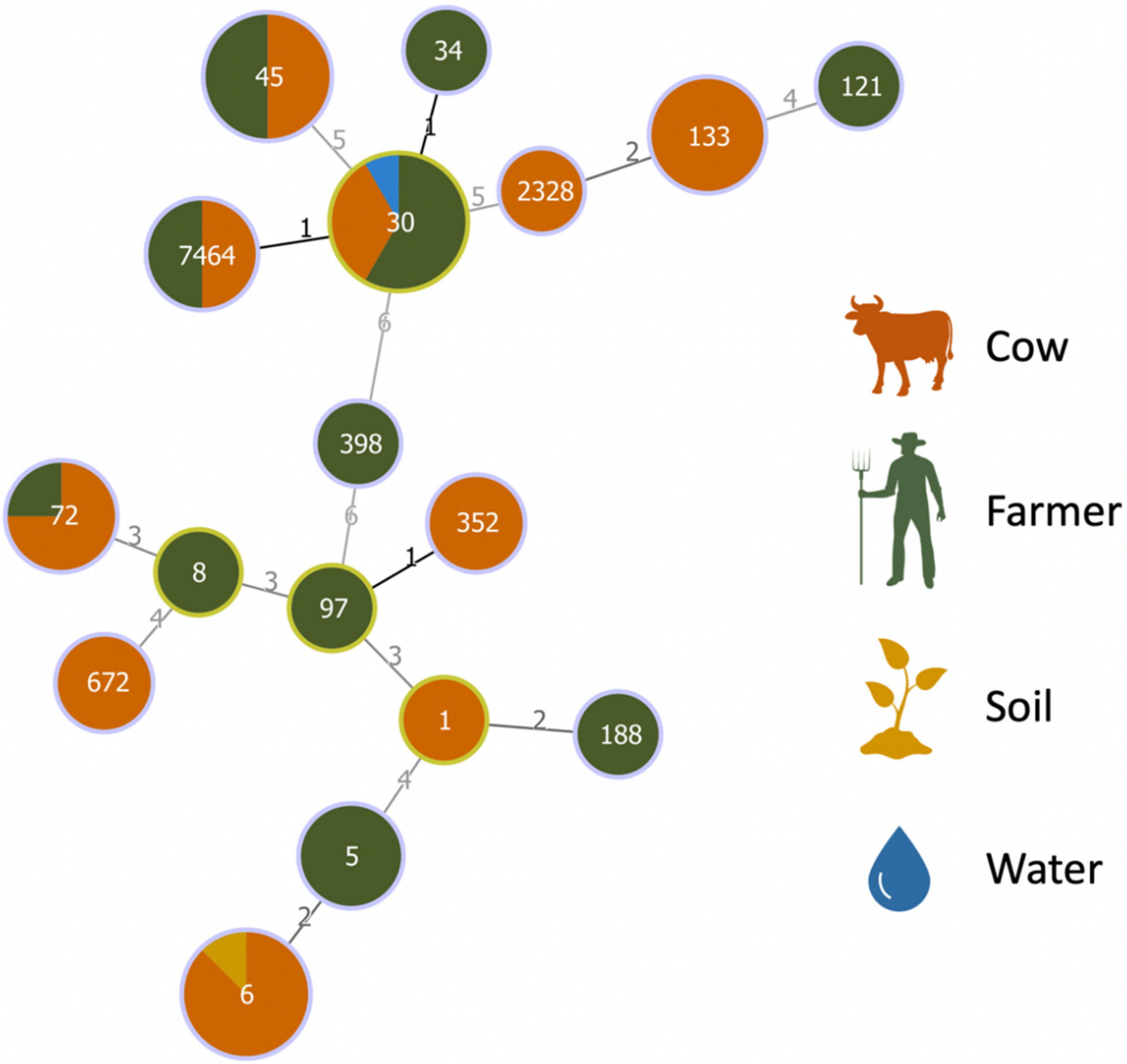
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chambers, H.F.; Deleo, F.R. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat. Rev. Microbiol. 2009, 7, 629–641. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, P.M.; Kock, R.; Kachani, M.; Kunkel, R.; Thomas, J.; Gilbert, J.; Wallace, R.; Blackmore, C.; Wong, D.; Karesh, W.; et al. Toward proof of concept of a one health approach to disease prediction and control. Emerg. Infect. Dis. 2013, 19, e130265. [Google Scholar] [CrossRef] [PubMed]
- Schwabe, C.W. The challenge of “one medicine”. In Veterinary Medicine and Human Health, 3rd ed.; Williams & Wilkins: Baltimore, MD, USA, 1984; pp. 1–15. [Google Scholar]
- Rabinowitz, P.; Scotch, M.; Conti, L. Human and animal sentinels for shared health risks. Vet. Ital. 2009, 45, 23. [Google Scholar] [PubMed]
- Mackenzie, J.S.; Jeggo, M. The One Health Approach—Why Is It So Important? Trop. Med. Infect. Dis. 2019, 4, 88. [Google Scholar] [CrossRef] [Green Version]
- Boqvist, S.; Söderqvist, K.; Vågsholm, I. Food safety challenges and One Health within Europe. Acta Vet. Scand. 2018, 60, 1. [Google Scholar] [CrossRef]
- Ceric, O.; Tyson, G.H.; Goodman, L.B.; Mitchell, P.K.; Zhang, Y.; Prarat, M.; Cui, J.; Peak, L.; Scaria, J.; Antony, L. Enhancing the one health initiative by using whole genome sequencing to monitor antimicrobial resistance of animal pathogens: Vet-LIRN collaborative project with veterinary diagnostic laboratories in United States and Canada. BMC Vet. Res. 2019, 15, 130. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Ten Threats to Global Health in 2019; World Health Organization: Geneva, Switzerland, 2019.
- More, S.J. European perspectives on efforts to reduce antimicrobial usage in food animal production. Ir. Vet. J. 2020, 73, 2. [Google Scholar] [CrossRef] [Green Version]
- Taylor, T.A.; Unakal, C.G. Staphylococcus aureus. Available online: https://www.statpearls.com/ (accessed on 9 December 2021).
- Tong, S.Y.C.; Davis, J.S.; Eichenberger, E.; Holland, T.L.; Fowler, V.G., Jr. Staphylococcus aureus infections: Epidemiology, pathophysiology, clinical manifestations, and management. Clin. Microbiol. Rev. 2015, 28, 603–661. [Google Scholar] [CrossRef] [Green Version]
- Silva, V.; Capelo, J.L.; Igrejas, G.; Poeta, P. Molecular Epidemiology of Staphylococcus aureus Lineages in Wild Animals in Europe: A Review. Antibiotics 2020, 9, 122. [Google Scholar] [CrossRef] [Green Version]
- Mukherjee, R. Antimicrobial Resistance in Staphylococcus aureus; Priyadarshini, A., Ed.; IntechOpen: Rijeka, Croatia, 2021; Chapter 5; ISBN 978-1-83962-743-9. [Google Scholar]
- Cheung, G.Y.C.; Bae, J.S.; Otto, M. Pathogenicity and virulence of Staphylococcus aureus. Virulence 2021, 12, 547–569. [Google Scholar] [CrossRef]
- Sieber, R.N.; Skov, R.L.; Nielsen, J.; Schulz, J.; Price, L.B.; Aarestrup, F.M.; Larsen, A.R.; Stegger, M.; Larsen, J. Drivers and dynamics of methicillin-resistant livestock-associated Staphylococcus aureus CC398 in pigs and humans in Denmark. MBio 2018, 9, e02142-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hogan, P.G.; Mork, R.L.; Boyle, M.G.; Muenks, C.E.; Morelli, J.J.; Thompson, R.M.; Sullivan, M.L.; Gehlert, S.J.; Merlo, J.R.; McKenzie, M.G. Interplay of personal, pet, and environmental colonization in households affected by community-associated methicillin-resistant Staphylococcus aureus. J. Infect. 2019, 78, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Adamu, J.Y.; Raufu, A.I.; Chimaroke, F.C.; Ameh, J.A. Antimicrobial susceptibility testing of Staphylococcus aureus isolated from apparently healthy humans and animals in Maiduguri, Nigeria. Int. J. Biomed. Health Sci. 2021, 6, 191–195. [Google Scholar]
- Kearney, A.; Kinnevey, P.; Shore, A.; Earls, M.; Poovelikunnel, T.T.; Brennan, G.; Humphreys, H.; Coleman, D.C. The oral cavity revealed as a significant reservoir of Staphylococcus aureus in an acute hospital by extensive patient, healthcare worker and environmental sampling. J. Hosp. Infect. 2020, 105, 389–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, V.; Ferreira, E.; Manageiro, V.; Reis, L.; Tejedor-Junco, M.T.; Sampaio, A.; Capelo, J.L.; Caniça, M.; Igrejas, G.; Poeta, P. Distribution and Clonal Diversity of Staphylococcus aureus and Other Staphylococci in Surface Waters: Detection of ST425-t742 and ST130-t843 mecC-Positive MRSA Strains. Antibiotics 2021, 10, 1416. [Google Scholar] [CrossRef]
- Silva, V.; Ribeiro, J.; Rocha, J.; Manaia, C.M.; Silva, A.; Pereira, J.E.; Maltez, L.; Capelo, J.L.; Igrejas, G.; Poeta, P. High Frequency of the EMRSA-15 Clone (ST22-MRSA-IV) in Hospital Wastewater. Microorganisms 2022, 10, 147. [Google Scholar] [CrossRef]
- Silva, V.; Caniça, M.; Capelo, J.L.; Igrejas, G.; Poeta, P. Diversity and genetic lineages of environmental staphylococci: A surface water overview. FEMS Microbiol. Ecol. 2020, 96, fiaa191. [Google Scholar] [CrossRef]
- McCarthy, A.J.; Lindsay, J.A.; Loeffler, A. Are all meticillin-resistant Staphylococcus aureus (MRSA) equal in all hosts? Epidemiological and genetic comparison between animal and human MRSA. Vet. Dermatol. 2012, 23, 267-e54. [Google Scholar] [CrossRef]
- Matuszewska, M.; Murray, G.G.R.; Harrison, E.M.; Holmes, M.A.; Weinert, L.A. The Evolutionary Genomics of Host Specificity in Staphylococcus aureus. Trends Microbiol. 2020, 28, 465–477. [Google Scholar] [CrossRef]
- Smith, E.M.; Needs, P.F.; Manley, G.; Green, L.E. Global distribution and diversity of ovine-associated Staphylococcus aureus. Infect. Genet. Evol. 2014, 22, 208–215. [Google Scholar] [CrossRef] [Green Version]
- Murray, S.; Pascoe, B.; Meric, G.; Mageiros, L.; Yahara, K.; Hitchings, M.D.; Friedmann, Y.; Wilkinson, T.S.; Gormley, F.J.; Mack, D. Recombination-mediated host adaptation by avian Staphylococcus aureus. Genome Biol. Evol. 2017, 9, 830–842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shepheard, M.A.; Fleming, V.M.; Connor, T.R.; Corander, J.; Feil, E.J.; Fraser, C.; Hanage, W.P. Historical zoonoses and other changes in host tropism of Staphylococcus aureus, identified by phylogenetic analysis of a population dataset. PLoS ONE 2013, 8, e62369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haag, A.F.; Fitzgerald, J.R.; Penadés, J.R. Staphylococcus aureus in Animals. Gram-Positive Pathog. 2019, 7, 731–746. [Google Scholar]
- Resch, G.; François, P.; Morisset, D.; Stojanov, M.; Bonetti, E.J.; Schrenzel, J.; Sakwinska, O.; Moreillon, P. Human-to-bovine jump of Staphylococcus aureus CC8 is associated with the loss of a β-hemolysin converting prophage and the acquisition of a new staphylococcal cassette chromosome. PLoS ONE 2013, 8, e58187. [Google Scholar] [CrossRef]
- Krukowski, H.; Bakuła, Z.; Iskra, M.; Olender, A.; Bis-Wencel, H.; Jagielski, T. The first outbreak of methicillin-resistant Staphylococcus aureus in dairy cattle in Poland with evidence of on-farm and intrahousehold transmission. J. Dairy Sci. 2020, 103, 10577–10584. [Google Scholar] [CrossRef]
- Spoor, L.E.; McAdam, P.R.; Weinert, L.A.; Rambaut, A.; Hasman, H.; Aarestrup, F.M.; Kearns, A.M.; Larsen, A.R.; Skov, R.L.; Fitzgerald, J.R. Livestock origin for a human pandemic clone of community-associated methicillin-resistant Staphylococcus aureus. MBio 2013, 4, e00356-13. [Google Scholar] [CrossRef] [Green Version]
- Garcia, J.E.Y. Catálogo de Raças Autóctones de Castela e Leão (Espanha); Rei Afonso Henriques Foundation: Salamanca, Spain, 2002. [Google Scholar]
- Correia, S.; Silva, V.; García-Díez, J.; Teixeira, P.; Pimenta, K.; Pereira, J.E.; Oliveira, S.; Rocha, J.; Manaia, C.M.; Igrejas, G.; et al. One Health Approach Reveals the Absence of Methicillin-Resistant Staphylococcus aureus in Autochthonous Cattle and Their Environments. Front. Microbiol. 2019, 10, 2735. [Google Scholar] [CrossRef] [Green Version]
- Silva, V.; Caniça, M.; Ferreira, E.; Vieira-Pinto, M.; Saraiva, C.; Pereira, J.E.; Capelo, J.L.; Igrejas, G.; Poeta, P. Multidrug-Resistant Methicillin-Resistant Coagulase-Negative Staphylococci in Healthy Poultry Slaughtered for Human Consumption. Antibiotics 2022, 11, 365. [Google Scholar] [CrossRef]
- Van Wamel, W.J.B.; Rooijakkers, S.H.M.; Ruyken, M.; van Kessel, K.P.M.; van Strijp, J.A.G. The innate immune modulators staphylococcal complement inhibitor and chemotaxis inhibitory protein of Staphylococcus aureus are located on beta-hemolysin-converting bacteriophages. J. Bacteriol. 2006, 188, 1310–1315. [Google Scholar] [CrossRef] [Green Version]
- Harmsen, D.; Claus, H.; Witte, W.; Rothganger, J.; Claus, H.; Turnwald, D.; Vogel, U. Typing of Methicillin-Resistant Staphylococcus aureus in a University Hospital Setting by Using Novel Software for spa Repeat Determination and Database Management. J. Clin. Microbiol. 2003, 41, 5442–5448. [Google Scholar] [CrossRef] [Green Version]
- Enright, M.C.; Day, N.P.; Davies, C.E.; Peacock, S.J.; Spratt, B.G. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J. Clin. Microbiol. 2000, 38, 1008–1015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shopsin, B.; Mathema, B.; Alcabes, P.; Said-Salim, B.; Lina, G.; Matsuka, A.; Martinez, J.; Kreiswirth, B.N. Prevalence of agr specificity groups among Staphylococcus aureus strains colonizing children and their guardians. J. Clin. Microbiol. 2003, 41, 456–459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Juhász-Kaszanyitzky, E.; Jánosi, S.; Somogyi, P.; Dán, A.; van der Graaf-van Bloois, L.; van Duijkeren, E.; Wagenaar, J.A. MRSA transmission between cows and humans. Emerg. Infect. Dis. 2007, 13, 630–632. [Google Scholar] [CrossRef] [PubMed]
- Locatelli, C.; Cremonesi, P.; Caprioli, A.; Carfora, V.; Ianzano, A.; Barberio, A.; Morandi, S.; Casula, A.; Castiglioni, B.; Bronzo, V.; et al. Occurrence of methicillin-resistant Staphylococcus aureus in dairy cattle herds, related swine farms, and humans in contact with herds. J. Dairy Sci. 2017, 100, 608–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmidt, T.; Kock, M.M.; Ehlers, M.M. Molecular Characterization of Staphylococcus aureus Isolated from Bovine Mastitis and Close Human Contacts in South African Dairy Herds: Genetic Diversity and Inter-Species Host Transmission. Front. Microbiol. 2017, 8, 511. [Google Scholar] [CrossRef] [Green Version]
- Santos, R.P.; Souza, F.N.; Oliveira, A.C.D.; de Souza Filho, A.F.; Aizawa, J.; Moreno, L.Z.; da Cunha, A.F.; Cortez, A.; Della Libera, A.M.M.P.; Heinemann, M.B.; et al. Molecular Typing and Antimicrobial Susceptibility Profile of Staphylococcus aureus Isolates Recovered from Bovine Mastitis and Nasal Samples. Animals 2020, 10, 2143. [Google Scholar] [CrossRef]
- Rahimi, H.; Dastmalchi Saei, H.; Ahmadi, M. Nasal Carriage of Staphylococcus aureus: Frequency and Antibiotic Resistance in Healthy Ruminants. Jundishapur J. Microbiol. 2015, 8, e22413. [Google Scholar] [CrossRef] [Green Version]
- Khemiri, M.; Abbassi, M.S.; Couto, N.; Mansouri, R.; Hammami, S.; Pomba, C. Genetic characterisation of Staphylococcus aureus isolated from milk and nasal samples of healthy cows in Tunisia: First report of ST97-t267-agrI-SCCmecV MRSA of bovine origin in Tunisia. J. Glob. Antimicrob. Resist. 2018, 14, 161–165. [Google Scholar] [CrossRef]
- Gharsa, H.; Slama, K.B.; Gómez-Sanz, E.; Lozano, C.; Zarazaga, M.; Messadi, L.; Boudabous, A.; Torres, C. Molecular Characterization of Staphylococcus aureus from Nasal Samples of Healthy Farm Animals and Pets in Tunisia. Vector-Borne Zoonotic Dis. 2015, 15, 109–115. [Google Scholar] [CrossRef]
- Garipcin, M.; Seker, E. Nasal carriage of methicillin-resistant Staphylococcus aureus in cattle and farm workers in Turkey. Vet. Arh. 2015, 85, 117–129. [Google Scholar]
- Claudia, L.; Andreas, P.; Bernhard, K. Staphylococcus aureus Colonization of the Human Nose and Interaction with Other Microbiome Members. Microbiol. Spectr. 2019, 7, 2–7. [Google Scholar] [CrossRef]
- El-Ashker, M.; Monecke, S.; Gwida, M.; Saad, T.; El-Gohary, A.; Mohamed, A.; Reißig, A.; Frankenfeld, K.; Gary, D.; Müller, E.; et al. Molecular characterisation of methicillin-resistant and methicillin-susceptible Staphylococcus aureus clones isolated from healthy dairy animals and their caretakers in Egypt. Vet. Microbiol. 2022, 267, 109374. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.F.; Pisanic, N.; Rhodes, S.M.; Brown, A.; Keller, H.; Nadimpalli, M.; Christ, A.; Ludwig, S.; Ordak, C.; Spicer, K.; et al. Occurrence of Staphylococcus aureus in swine and swine workplace environments on industrial and antibiotic-free hog operations in North Carolina, USA: A One Health pilot study. Environ. Res. 2018, 163, 88–96. [Google Scholar] [CrossRef]
- Papadopoulos, P.; Papadopoulos, T.; Angelidis, A.S.; Boukouvala, E.; Zdragas, A.; Papa, A.; Hadjichristodoulou, C.; Sergelidis, D. Prevalence of Staphylococcus aureus and of methicillin-resistant S. aureus (MRSA) along the production chain of dairy products in north-western Greece. Food Microbiol. 2018, 69, 43–50. [Google Scholar] [CrossRef]
- Peterson, A.E.; Davis, M.F.; Awantang, G.; Limbago, B.; Fosheim, G.E.; Silbergeld, E.K. Correlation between animal nasal carriage and environmental methicillin-resistant Staphylococcus aureus isolates at U.S. horse and cattle farms. Vet. Microbiol. 2012, 160, 539–543. [Google Scholar] [CrossRef]
- Schulz., J.; Friese, A.; Klees, S.; Tenhagen, B.A.; Fetsch, A.; Rösler, U.; Hartung, H. Longitudinal Study of the Contamination of Air and of Soil Surfaces in the Vicinity of Pig Barns by Livestock-Associated Methicillin-Resistant Staphylococcus aureus. Appl. Environ. Microbiol. 2012, 78, 5666–5671. [Google Scholar] [CrossRef] [Green Version]
- Levin-Edens, E.; Bonilla, N.; Meschke, J.S.; Roberts, M.C. Survival of environmental and clinical strains of methicillin-resistant Staphylococcus aureus [MRSA] in marine and fresh waters. Water Res. 2011, 45, 5681–5686. [Google Scholar] [CrossRef]
- Mechesso, A.F.; Kim, S.-J.; Park, H.-S.; Choi, J.-H.; Song, H.-J.; Kim, M.H.; Lim, S.; Yoon, S.-S.; Moon, D.-C. First detection of Panton-Valentine leukocidin–positive methicillin-resistant Staphylococcus aureus ST30 in raw milk taken from dairy cows with mastitis in South Korea. J. Dairy Sci. 2021, 104, 969–976. [Google Scholar] [CrossRef]
- Simon, A.C.; Baldo, V.; Losio, N.; Filipello, V.; Colagiorgi, A.; Scali, F.; Zanardi, E.; Ghidini, S.; Ianieri, A.; Alborali, G.L. Molecular characterization of Methicillin-resistant Staphylococcus aureus isolated from the pig production chain in Northern Italy. Ital. J. Food Saf. 2020, 9, 8412. [Google Scholar] [CrossRef]
- Aanensen, D.M.; Feil, E.J.; Holden, M.T.G.; Dordel, J.; Yeats, C.A.; Fedosejev, A.; Goater, R.; Castillo-Ramírez, S.; Corander, J.; Colijn, C. Whole-genome sequencing for routine pathogen surveillance in public health: A population snapshot of invasive Staphylococcus aureus in Europe. MBio 2016, 7, e00444-16. [Google Scholar] [CrossRef] [Green Version]
- Tavares, A.; Faria, N.A.; de Lencastre, H.; Miragaia, M. Population structure of methicillin-susceptible Staphylococcus aureus (MSSA) in Portugal over a 19-year period (1992–2011). Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 423–432. [Google Scholar] [CrossRef]
- Silva, V.; Lopes, A.F.; Soeiro, V.; Caniça, M.; Manageiro, V.; Pereira, J.E.; Maltez, L.; Capelo, J.L.; Igrejas, G.; Poeta, P. Nocturnal Birds of Prey as Carriers of Staphylococcus aureus and Other Staphylococci: Diversity, Antimicrobial Resistance and Clonal Lineages. Antibiotics 2022, 11, 240. [Google Scholar] [CrossRef]
- Papadimitriou-Olivgeris, M.; Drougka, E.; Fligou, F.; Dodou, V.; Kolonitsiou, F.; Filos, K.S.; Anastassiou, E.D.; Petinaki, E.; Marangos, M.; Spiliopoulou, I. Spread of Tst–Positive Staphylococcus aureus Strains Belonging to ST30 Clone among Patients and Healthcare Workers in Two Intensive Care Units. Toxins 2017, 9, 270. [Google Scholar] [CrossRef] [Green Version]
- Park, C.; Lee, D.-G.; Kim, S.W.; Choi, S.-M.; Park, S.H.; Chun, H.-S.; Choi, J.-H.; Yoo, J.-H.; Shin, W.S.; Kang, J.H. Predominance of community-associated methicillin-resistant Staphylococcus aureus strains carrying staphylococcal chromosome cassette mec type IVA in South Korea. J. Clin. Microbiol. 2007, 45, 4021–4026. [Google Scholar] [CrossRef] [Green Version]
- Salgueiro, V.; Manageiro, V.; Bandarra, N.M.; Ferreira, E.; Clemente, L.; Caniça, M. Genetic Relatedness and Diversity of Staphylococcus aureus from Different Reservoirs: Humans and Animals of Livestock, Poultry, Zoo, and Aquaculture. Microorganisms 2020, 8, 1345. [Google Scholar] [CrossRef]
- Hyukmin, L.; Eun-Jeong, Y.; Dokyun, K.; Wook, K.J.; Kwang-Jun, L.; Soo, K.H.; Ree, K.Y.; Hee, S.J.; Hwan, S.J.; Seob, S.K.; et al. Ceftaroline Resistance by Clone-Specific Polymorphism in Penicillin-Binding Protein 2a of Methicillin-Resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2022, 62, e00485-18. [Google Scholar] [CrossRef] [Green Version]
- Effelsberg, N.; Stegger, M.; Peitzmann, L.; Altinok, O.; Coombs, G.W.; Pichon, B.; Kearns, A.; Randad, P.R.; Heaney, C.D.; Bletz, S.; et al. Global Epidemiology and Evolutionary History of Staphylococcus aureus ST45. J. Clin. Microbiol. 2022, 59, e02198-20. [Google Scholar] [CrossRef]
- Dastmalchi Saei, H.; Panahi, M. Genotyping and antimicrobial resistance of Staphylococcus aureus isolates from dairy ruminants: Differences in the distribution of clonal types between cattle and small ruminants. Arch. Microbiol. 2020, 202, 115–125. [Google Scholar] [CrossRef]
- Akkou, M.; Bouchiat, C.; Antri, K.; Bes, M.; Tristan, A.; Dauwalder, O.; Martins-Simoes, P.; Rasigade, J.-P.; Etienne, J.; Vandenesch, F.; et al. New host shift from human to cows within Staphylococcus aureus involved in bovine mastitis and nasal carriage of animal’s caretakers. Vet. Microbiol. 2018, 223, 173–180. [Google Scholar] [CrossRef]
- Silva, V.; Gabriel, S.I.; Borrego, S.B.; Tejedor-Junco, M.T.; Manageiro, V.; Ferreira, E.; Reis, L.; Caniça, M.; Capelo, J.L.; Igrejas, G.; et al. Antimicrobial Resistance and Genetic Lineages of Staphylococcus aureus from Wild Rodents: First Report of mecC-Positive Methicillin-Resistant S. aureus (MRSA) in Portugal. Animals 2021, 11, 1537. [Google Scholar] [CrossRef]
- Mairi, A.; Touati, A.; Pantel, A.; Zenati, K.; Martinez, A.Y.; Dunyach-Remy, C.; Sotto, A.; Lavigne, J.-P. Distribution of Toxinogenic Methicillin-Resistant and Methicillin-Susceptible Staphylococcus aureus from Different Ecological Niches in Algeria. Toxins 2019, 11, 500. [Google Scholar] [CrossRef] [Green Version]
- Goudarzi, M.; Goudarzi, H.; Sá Figueiredo, A.M.; Udo, E.E.; Fazeli, M.; Asadzadeh, M.; Seyedjavadi, S.S. Molecular Characterization of Methicillin Resistant Staphylococcus aureus Strains Isolated from Intensive Care Units in Iran: ST22-SCCmec IV/t790 Emerges as the Major Clone. PLoS ONE 2016, 11, e0155529. [Google Scholar] [CrossRef] [Green Version]
- Benito, D.; Gómez, P.; Aspiroz, C.; Zarazaga, M.; Lozano, C.; Torres, C. Molecular characterization of Staphylococcus aureus isolated from humans related to a livestock farm in Spain, with detection of MRSA-CC130 carrying mecC gene: A zoonotic case? Enferm. Infecc. Microbiol. Clin. 2016, 34, 280–285. [Google Scholar] [CrossRef]
- Seinige, D.; Von Altrock, A.; Kehrenberg, C. Genetic diversity and antibiotic susceptibility of Staphylococcus aureus isolates from wild boars. Comp. Immunol. Microbiol. Infect. Dis. 2017, 54, 7–12. [Google Scholar] [CrossRef]
- Sheet, O.H.; Grabowski, N.T.; Klein, G.; Reich, F.; Abdulmawjood, A. Characterisation of mecA gene negative Staphylococcus aureus isolated from bovine mastitis milk from Northern Germany. Folia Microbiol. 2019, 64, 845–855. [Google Scholar] [CrossRef]
- Cvetnić, L.; Samardžija, M.; Duvnjak, S.; Habrun, B.; Cvetnić, M.; Jaki Tkalec, V.; Đuričić, D.; Benić, M. Multi Locus Sequence Typing and spa Typing of Staphylococcus aureus Isolated from the Milk of Cows with Subclinical Mastitis in Croatia. Microorganisms 2021, 9, 725. [Google Scholar] [CrossRef]
- Kroning, I.S.; Haubert, L.; Kleinubing, N.R.; Jaskulski, I.B.; Scheik, L.K.; Ramires, T.; da Silva, W.P. New spa types, resistance to sanitisers and presence of efflux pump genes in Staphylococcus aureus from milk. Int. Dairy J. 2020, 109, 104712. [Google Scholar] [CrossRef]
- Schaumburg, F.; Köck, R.; Leendertz, F.H.; Becker, K. Airport door handles and the global spread of antimicrobial-resistant bacteria: A cross sectional study. Clin. Microbiol. Infect. 2016, 22, 1010–1011. [Google Scholar] [CrossRef]
- Ji, X.; Krüger, H.; Feßler, A.T.; Liu, J.; Zeng, Z.; Wang, Y.; Wu, C.; Schwarz, S. A novel SCCmec type V variant in porcine MRSA ST398 from China. J. Antimicrob. Chemother. 2020, 75, 484–486. [Google Scholar] [CrossRef]
- Tegegne, H.A.; Madec, J.-Y.; Haenni, M. Is methicillin-susceptible Staphylococcus aureus (MSSA) CC398 a true animal-independent pathogen? J. Glob. Antimicrob. Resist. 2022, 29, 120–123. [Google Scholar] [CrossRef]
- Tegegne, H.A.; Florianová, M.; Gelbíčová, T.; Karpíšková, R.; Koláčková, I. Detection and molecular characterization of methicillin-resistant Staphylococcus aureus isolated from bulk tank milk of cows, sheep, and goats. Foodborne Pathog. Dis. 2019, 16, 68–73. [Google Scholar] [CrossRef]
- Zhang, K.; Sparling, J.; Chow, B.L.; Elsayed, S.; Hussain, Z.; Church, D.L.; Gregson, D.B.; Louie, T.; Conly, J.M. New quadriplex PCR assay for detection of methicillin and mupirocin resistance and simultaneous discrimination of Staphylococcus aureus from coagulase-negative staphylococci. J. Clin. Microbiol. 2004, 42, 4947–4955. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schnellmann, C.; Gerber, V.; Rossano, A.; Jaquier, V.; Panchaud, Y.; Doherr, M.G.; Thomann, A.; Straub, R.; Perreten, V. Presence of new mecA and mph(C) variants conferring antibiotic resistance in Staphylococcus spp. isolated from the skin of horses before and after clinic admission. J. Clin. Microbiol. 2006, 44, 4444–4454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sutcliffe, J.; Grebe, T.; Tait-Kamradt, A.; Wondrack, L. Detection of erythromycin-resistant determinants by PCR. Antimicrob. Agents Chemother. 1996, 40, 2562–2566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomez-Sanz, E.; Torres, C.; Lozano, C.; Fernandez-Perez, R.; Aspiroz, C.; Ruiz-Larrea, F.; Zarazaga, M. Detection, molecular characterization, and clonal diversity of methicillin-resistant Staphylococcus aureus CC398 and CC97 in Spanish slaughter pigs of different age groups. Foodborne Pathog. Dis. 2010, 7, 1269–1277. [Google Scholar] [CrossRef]
- Wondrack, L.; Massa, M.; Yang, B.V.; Sutcliffe, J. Clinical strain of Staphylococcus aureus inactivates and causes efflux of macrolides. Antimicrob. Agents Chemother. 1996, 40, 992–998. [Google Scholar] [CrossRef] [Green Version]
- Lina, G.; Quaglia, A.; Reverdy, M.E.; Leclercq, R.; Vandenesch, F.; Etienne, J. Distribution of genes encoding resistance to macrolides, lincosamides, and streptogramins among staphylococci. Antimicrob. Agents Chemother. 1999, 43, 1062–1066. [Google Scholar] [CrossRef] [Green Version]
- Bozdogan, B.; Berrezouga, L.; Kou, M.S.; Yurek, D.A.; Farley, K.A.; Stockman, B.J.; Leclercq, R. A new resistance gene, linB, conferring resistance to lincosamides by nucleotidylation in Enterococcus faecium HM1025. Antimicrob. Agents Chemother. 1999, 43, 925–929. [Google Scholar] [CrossRef] [Green Version]
- Lozano, C.; Aspiroz, C.; Rezusta, A.; Gómez-Sanz, E.; Simon, C.; Gómez, P.; Ortega, C.; Revillo, M.J.; Zarazaga, M.; Torres, C. Identification of novel vga(A)-carrying plasmids and a Tn5406-like transposon in meticillin-resistant Staphylococcus aureus and Staphylococcus epidermidis of human and animal origin. Int. J. Antimicrob. Agents 2012, 40, 306–312. [Google Scholar] [CrossRef]
- Hammerum, A.M.; Jensen, L.B.; Aarestrup, F.M. Detection of the satA gene and transferability of virginiamycin resistance in Enterococcus faecium from food- animals. FEMS Microbiol. Lett. 1998, 168, 145–151. [Google Scholar] [CrossRef]
- Aarestrup, F.M.; Agers, L.Y.; Ahrens, P.; JŁrgensen, J.C.; Madsen, M.; Jensen, L.B. Antimicrobial susceptibility and presence of resistance genes in staphylococci from poultry. Vet. Microbiol. 2000, 74, 353–364. [Google Scholar] [CrossRef]
- Van de Klundert, J.A.M.; Vliegenthart, J.S. PCR detection of genes coding for aminoglycoside-modifying enzymes. In Diagnostic Molecular Microbiology: Principles and Applications; Persing, D.H., Smith, T.F., Tenover, F.C., White, T.J., Eds.; American Society for Microbiology: Washington, DC, USA, 1993; pp. 547–552. [Google Scholar]
- Kehrenberg, C.; Schwarz, S. Distribution of Florfenicol Resistance Genes fexA and cfr among Chloramphenicol-Resistant Staphylococcus Isolates. Antimicrob. Agents Chemother. 2006, 50, 1156–1163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, H.; Wang, Y.; Wu, C.; Schwarz, S.; Shen, Z.; Jeon, B.; Ding, S.; Zhang, Q.; Shen, J. A novel phenicol exporter gene, fexB, found in enterococci of animal origin. J. Antimicrob. Chemother. 2012, 67, 322–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mclaws, F.; Chopra, I.; O’Neill, A.J. High prevalence of resistance to fusidic acid in clinical isolates of Staphylococcus epidermidis. J. Antimicrob. Chemother. 2008, 61, 1040–1043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, H.J.; Hung, W.C.; Tseng, S.P.; Tsai, J.C.; Hsueh, P.R.; Teng, L.J. Fusidic acid resistance determinants in Staphylococcus aureus clinical isolates. Antimicrob. Agents Chemother. 2010, 54, 4985–4991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Antibiotics | Resistant | Susceptible |
|---|---|---|
| Positive Strains n (%) | Positive Strains n (%) | |
| Penicillin (1U) | 36 (62.1) | 22 (37.9) |
| Chloramphenicol (30 μg) | 2 (3.5) | 56 (96.5) |
| Clindamycin (2 μg) | 2 (3.5) | 56 (96.5) |
| Erythromycin (15 μg) | 4 (6.9) | 54 (93.1) |
| Fusidic acid (10 μg) | 1 (1.7) | 57 (98.3) |
| Gentamicin (10 μg) | 4 (6.9) | 54 (93.1) |
| Kanamycin (30 μg) | 3 (5.2) | 55 (94.8) |
| Tetracycline (30 μg) | 3 (5.2) | 55 (94.8) |
| Tobramycin (10 μg) | 4 (6.9) | 54 (93.1) |
| Farm | Isolate | Source | Molecular Typing | Antimicrobial Resistance | Virulence Factors | ||||
|---|---|---|---|---|---|---|---|---|---|
| ST (CC) | spa | agr | Phenotype | Genotype | IEC System | Other Genes | |||
| 3 | VS3218 | Cow | 6 (5) | t16615 | I | PEN | blaZ | hla, hlb, hld | |
| 6 | VS3219 | Human | 45 (45) | t563 | I | PEN | blaZ | hla, hlb, hld | |
| 10 | VS3220 | Cow | 6 (5) | t16615 | I | Susceptible | hla, hlb, hld | ||
| VS3221 | Cow | 6 (5) | t16615 | I | FD | hla, hlb, hld | |||
| VS3222 | Cow | 133 (133) | t4735 | I | Susceptible | hla, hlb, hld | |||
| 13 | VS3223 | Cow | 672 | t959 | I | PEN, CN, TOB, KAN, TET | blaZ, aac(6′)-aph(2″), aph(3′)-IIIa, tetK | hla, hlb, hld | |
| VS3224 | Cow | 6 (5) | t16615 | I | Susceptible | hla, hlb, hld | |||
| VS3225 | Cow | 6 (5) | t16615 | I | PEN, CN, TOB, KAN | blaZ, aac(6′)-aph(2″), aph(3′)-IIIa | hla, hlb, hld | ||
| VS3226 | Cow | 6 (5) | t16615 | I | TET | tetK | hla, hlb, hld | ||
| VS3227 | Human | 30 (30) | t012 | III | PEN | blaZ | hla, hlb, hld, tst | ||
| VS3228 | Human | 30 (30) | t012 | III | PEN | blaZ | hla, hlb, hld, tst | ||
| VS3229 | Human | 30 (30) | t9413 | III | PEN | blaZ | hla, hlb, hld | ||
| 14 | VS3230 | Soil | 6 (5) | t16615 | I | Susceptible | hla, hlb, hld | ||
| 15 | VS3231 | Cow | 6 (5) | t16615 | I | Susceptible | hla, hlb, hld | ||
| VS3232 | Cow | 6 (5) | t16615 | I | Susceptible | hla, hlb, hld | |||
| 16 | VS3233 | Cow | 30 (30) | t9413 | III | PEN | blaZ | hla, hlb, hld | |
| VS3234 | Cow | 30 (30) | t9413 | III | PEN | blaZ | hla, hlb, hld | ||
| VS3235 | Cow | 30 (30) | t9413 | III | PEN | blaZ | hla, hlb, hld | ||
| VS3236 | Human | 5 (5) | t045 | II | PEN | blaZ | hla, hlb, hld | ||
| VS3237 | Human | 97 (97) | t189 | I | Susceptible | hla, hlb, hld | |||
| VS3238 | Human | 30 (30) | t018 | III | ERY | ermB | hla, hlb, hld, tst | ||
| VS3239 | Human | 30 (30) | t9413 | III | PEN | blaZ | hla, hlb, hld | ||
| VS3240 | Human | 30 (30) | t018 | III | PEN | blaZ | hla, hlb, hld, tst | ||
| VS3241 | Cow | 30 (30) | t9413 | III | PEN | blaZ | hla, hlb, hld | ||
| 17 | VS3242 | Cow | 133 (133) | t7355 | I | PEN, CN, TOB, KAN | blaZ, aac(6′)-aph(2″), aph(3′)-IIIa, str | hla, hlb, hld | |
| 20 | VS3243 | Human | 5 | t002 | II | PEN | blaZ | hla, hlb, hld | |
| 25 | VS3244 | Human | 121 (121) | t162 | IV | Susceptible | E | hla, hld | |
| 39 | VS3245 | Cow | 7464 (30) | t871 | III | Susceptible | hla, hlb, hld | ||
| VS3246 | Cow | 45 (45) | t015 | I | PEN | B | hla, hld | ||
| VS3247 | Cow | 352 (97) | t267 | I | Susceptible | hla, hlb, hld | |||
| VS3248 | Cow | 7464 (30) | t871 | III | Susceptible | hla, hlb, hld | |||
| 42 | VS3249 | Cow | 2328 (133) | t3750 | III | Susceptible | hla, hlb, hld | ||
| 46 | VS3250 | Human | 45 (45) | t350 | I | PEN | blaZ | hla, hlb, hld | |
| 47 | VS3251 | Cow | 45 (45) | t706 | I | PEN | blaZ | B | hla, hld |
| VS3252 | Human | 34 (30) | t414 | III | PEN | blaZ | hla, hlb, hld, tst | ||
| 48 | VS3253 | Human | 45 (45) | t015 | I | PEN | blaZ | hla, hlb, hld | |
| VS3254 | Human | 188 (188) | t189 | I | PEN, CN, TOB | blaZ, aac(6′)-aph(2″) | hla, hlb, hld | ||
| 49 | VS3255 | Cow | 133 (133) | t18899 | I | Susceptible | hla, hlb, hld | ||
| VS3256 | Cow | 133 (133) | t18899 | I | Susceptible | hla, hlb, hld | |||
| 52 | VS3257 | Cow | 672 | t959 | I | Susceptible | G | hla, hld | |
| VS3258 | Cow | 672 | t959 | I | Susceptible | G | hla, hld | ||
| VS3259 | Human | 8 | t008 | I | PEN, ERY | blaZ, ermC | hla, hlb, hld | ||
| VS3260 | Human | (30) | t012 | III | PEN | blaZ | hla, hlb, hld | ||
| VS3261 | Human | 30 (30) | t012 | III | PEN | blaZ | hla, hlb, hld | ||
| 55 | VS3262 | Water | 30 (30) | t018 | III | Susceptible | hla, hlb, hld, tst | ||
| 56 | VS3263 | Human | 5 | 45 | II | PEN | blaZ | hla, hlb, hld | |
| 58 | VS3264 | Human | 398 | t571 | I | PEN, ERY, CD, TET | blaZ, ermT, tetK | hla, hlb, hld | |
| 60 | VS3265 | Cow | 72 (8) | t148 | I | PEN | blaZ | hla, hlb, hld | |
| VS3266 | Cow | 352 (97) | t359 | I | PEN | blaZ | hla, hlb, hld | ||
| VS3267 | Cow | 72 (8) | t148 | I | PEN | blaZ | hla, hlb, hld | ||
| 62 | VS3268 | Cow | 45 (45) | t350 | I | PEN | blaZ | hla, hlb, hld | |
| VS3269 | Cow | 45 (45) | t7669 | I | PEN | blaZ | B | hla, hld | |
| VS3270 | Human | (30) | t012 | III | PEN, ERY, CD | blaZ, ermC | hla, hlb, hld | ||
| VS3271 | Human | 45 (45) | t7669 | I | PEN | blaZ | B | hla, hlb, hld | |
| 63 | VS3272 | Cow | 133 (133) | t18899 | I | Susceptible | hla, hlb, hld | ||
| VS3273 | Cow | 1 (1) | t2207 | III | Susceptible | hla, hlb, hld | |||
| 64 | VS3274 | Cow | 72 (8) | t148 | I | PEN, C | blaZ, catpC221 | hla, hlb, hld | |
| VS3275 | Human | 72 (8) | t148 | I | PEN, C | blaZ, catpC221 | hla, hlb, hld | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, V.; Correia, S.; Rocha, J.; Manaia, C.M.; Silva, A.; García-Díez, J.; Pereira, J.E.; Semedo-Lemsaddek, T.; Igrejas, G.; Poeta, P. Antimicrobial Resistance and Clonal Lineages of Staphylococcus aureus from Cattle, Their Handlers, and Their Surroundings: A Cross-Sectional Study from the One Health Perspective. Microorganisms 2022, 10, 941. https://doi.org/10.3390/microorganisms10050941
Silva V, Correia S, Rocha J, Manaia CM, Silva A, García-Díez J, Pereira JE, Semedo-Lemsaddek T, Igrejas G, Poeta P. Antimicrobial Resistance and Clonal Lineages of Staphylococcus aureus from Cattle, Their Handlers, and Their Surroundings: A Cross-Sectional Study from the One Health Perspective. Microorganisms. 2022; 10(5):941. https://doi.org/10.3390/microorganisms10050941
Chicago/Turabian StyleSilva, Vanessa, Susana Correia, Jaqueline Rocha, Célia M. Manaia, Adriana Silva, Juan García-Díez, José Eduardo Pereira, Teresa Semedo-Lemsaddek, Gilberto Igrejas, and Patrícia Poeta. 2022. "Antimicrobial Resistance and Clonal Lineages of Staphylococcus aureus from Cattle, Their Handlers, and Their Surroundings: A Cross-Sectional Study from the One Health Perspective" Microorganisms 10, no. 5: 941. https://doi.org/10.3390/microorganisms10050941
APA StyleSilva, V., Correia, S., Rocha, J., Manaia, C. M., Silva, A., García-Díez, J., Pereira, J. E., Semedo-Lemsaddek, T., Igrejas, G., & Poeta, P. (2022). Antimicrobial Resistance and Clonal Lineages of Staphylococcus aureus from Cattle, Their Handlers, and Their Surroundings: A Cross-Sectional Study from the One Health Perspective. Microorganisms, 10(5), 941. https://doi.org/10.3390/microorganisms10050941









