Possible Interactions between Malaria, Helminthiases and the Gut Microbiota: A Short Review
Abstract
:1. Introduction
2. Malaria
3. Helminthiases
4. The Gut Microbiota
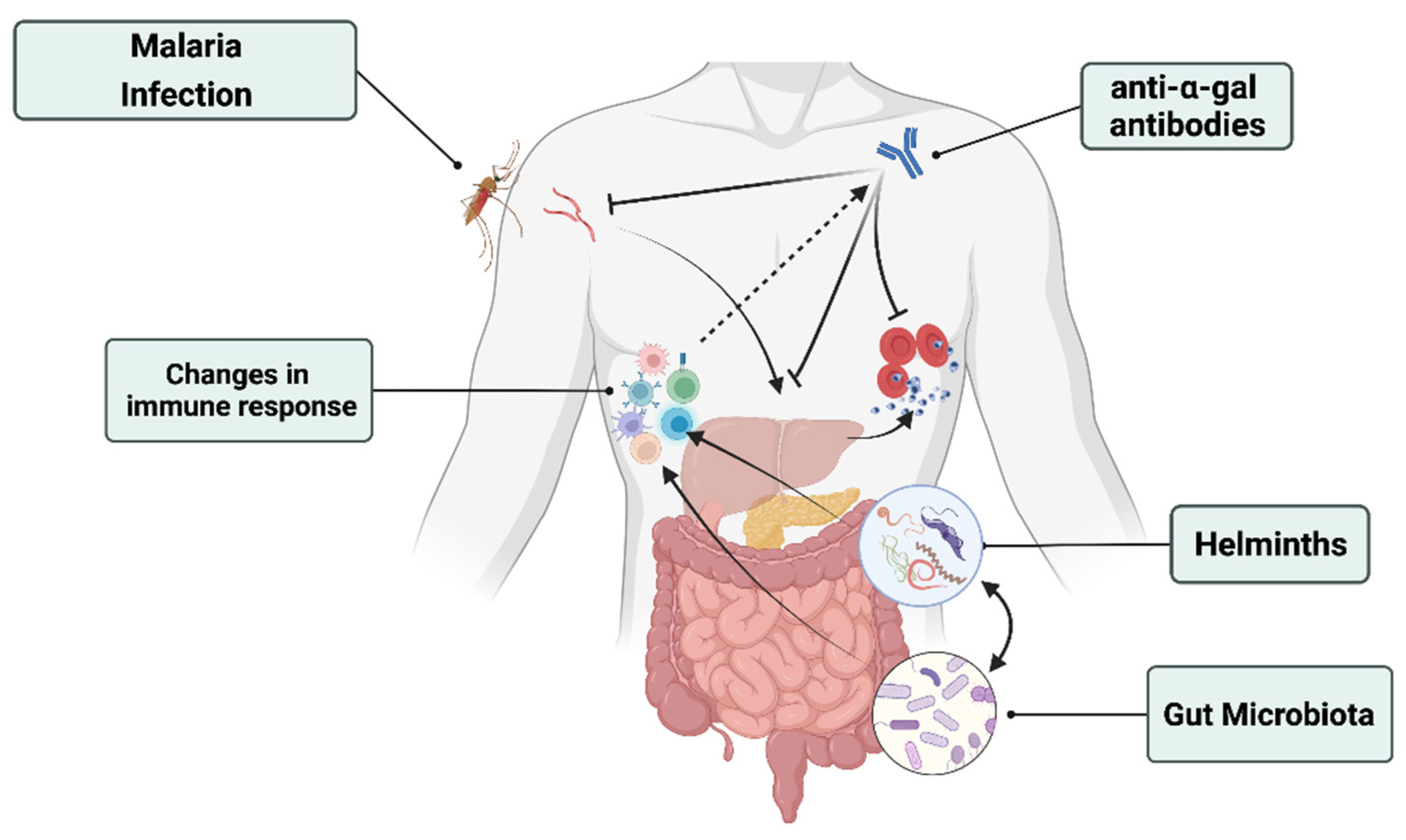
5. Interactions: Malaria, Helminthiases, and the Gut Microbiota
5.1. The Gut Microbiota Modulates Plasmodium Infection Risk and Transmission
5.2. The Gut Microbiota Modulates Malaria Disease Severity
5.3. Malaria-Modulated Changes on Gut Microbiota
5.4. Helminths and the Gut Microbiota
| Players (Host) | Key Findings | References |
|---|---|---|
| P. yoelii, gut microbiota and NTS (mice) | P. yoelii infection, through modifying the gut microbiota, decreases resistance to intestinal colonization of non-typhoidal salmonella (NTS) and malarial immune effects may promote susceptibility to disseminated NTS infections. Increase in Firmicutes and decrease in Bacteroidetes plus short-lived reduction in Proteobacteria were reported. | [51] |
| P. berghei and gut microbiota (mice) | Malaria infection was demonstrated to cause intestinal and cerebral pathologies through modifying the gut microbiota shown by the decrease in Firmicutes and increase in Proteobacteria. | [52] |
| P. yoelii and gut microbiota (mice) | Genetically similar mice purchased from two different vendors have shown different susceptibility to malaria due to their different gut microbiota composition. | [59] |
| P. berghei ANKA infection and microbiota (mice) | P. berghei ANKA infected mice show higher number of fecal Acinetobacter, Lactobacillus, and Lachnospiraceae_NK4A136_group. | [53] |
| P. berghei, P. yoelii and gut microbiota (mice) | The gut microbiota elicits the productions of anti–α-gal antibodies against malaria’s causative agent’s sporozoites which leads to blocking transmission. | [47] |
| P. berghei, P. chabaudi, P. yoelii and gut microbiota (mice) | Specific members (Lactobacillus and Bifidobacterium) of the gut microbiota were responsible for the modulation of the severity of malaria. | [50] |
| P. falciparum and gut microbiota (humans) | Specific compositions (Bifidobacterium, Streptococcus, and family Ruminococcaceae) of the human gut microbiota can modulate the risk if malaria infection. | [48] |
| P. falciparum and gut microbiota (humans) | Malaria episodes and Artemether-Lemefantrine (AL) treatment did not cause major changes in the gut microbiota composition. | [54] |
6. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Word Malaria Report 2021; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Hotez, P.J.; Brindley, P.J.; Bethony, J.M.; King, C.H.; Pearce, E.J.; Jacobson, J. Helminth infections: The great neglected tropical diseases Find the latest version: Review series Helminth infections: The great neglected tropical diseases. J. Clin. Investig. 2008, 118, 1311–1321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cani, P.D. Human gut microbiome: Hopes, threats and promises. Gut 2018, 6, 1716–1725. [Google Scholar] [CrossRef]
- de Vos, W.M.; Tilg, H.; Van Hul, M.; Cani, P.D. Gut microbiome and health: Mechanistic insights. Gut 2022. [Google Scholar] [CrossRef] [PubMed]
- WHO. World Malaria Report 2017; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- GMP/WHO. World Malaria Report 2019; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Mishra, M.; Mishra, V.K.; Kashaw, V.; Iyer, A.K.; Kashaw, S.K. Comprehensive review on various strategies for antimalarial drug discovery. Eur. J. Med. Chem. 2017, 125, 1300–1320. [Google Scholar] [CrossRef]
- World Health Organization. Global Technical Strategy for Malaria 2016–2030, Global Malaria Programme World Health Organization; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Laishram, D.D.; Sutton, P.L.; Nanda, N.; Sharma, V.L.; Sobti, R.C.; Carlton, J.M.; Joshi, H. The complexities of malaria disease manifestations with a focus on asymptomatic malaria. Malar. J. 2012, 11, 29. [Google Scholar] [CrossRef] [Green Version]
- Ashley, E.A.; Phyo, A.P.; Woodrow, C.J. Malaria. Lancet 2018, 391, 1608–1621. [Google Scholar] [CrossRef]
- Milner, D.A. Malaria Pathogenesis. Cold Spring Harb. Perspect. Med. 2017, 8, a025569. [Google Scholar] [CrossRef] [Green Version]
- Moxon, C.A.; Gibbins, M.; McGuinness, D.; Milner, D.A.; Marti, M. New Insights into Malaria Pathogenesis. Annu. Rev. Pathol. Mech. Dis. 2020, 15, 315–343. [Google Scholar] [CrossRef] [Green Version]
- López, C.; Yepes-Pérez, Y.; Hincapié-Escobar, N.; Diaz-Arevalo, D.; Patarroyo, M.A. What Is Known about the Immune Response Induced by Plasmodium vivax Malaria Vaccine Candidates? Front. Immunol. 2017, 8, 126. [Google Scholar] [CrossRef] [Green Version]
- Crompton, P.D.; Moebius, J.; Portugal, S.; Waisberg, M.; Hart, G.; Garver, L.S.; Miller, L.H.; Barillas-Mury, C.; Pierce, S.K. Mysteries of a Deadly Infectious Disease. Annu. Rev. Immunol. 2014, 32, 157–187. [Google Scholar] [CrossRef] [Green Version]
- Waide, M.L.; Polidoro, R.; Powell, W.L.; Denny, J.E.; Kos, J.; Tieri, D.A.; Watson, C.T.; Schmidt, N.W. Gut Microbiota Composition Modulates the Magnitude and Quality of Germinal Centers during Plasmodium Infections. Cell Rep. 2020, 33, 108503. [Google Scholar] [CrossRef] [PubMed]
- Kurup, S.; Obeng-Adjei, N.; Anthony, S.M.; Traore, B.; Doumbo, O.K.; Butler, N.; Crompton, P.D.; Harty, J.T. Regulatory T cells impede acute and long-term immunity to blood-stage malaria through CTLA-4. Nat. Med. 2017, 23, 1220–1225. [Google Scholar] [CrossRef]
- Modiano, D.; Petrarca, V.; Sirima, B.S.; Nebié, I.; Diallo, D.; Esposito, F.; Coluzzi, M. Different response to Plasmodium falciparum malaria in West African sympatric ethnic groups. Proc. Natl. Acad. Sci. USA 1996, 93, 13206–13211. [Google Scholar] [CrossRef] [Green Version]
- Dhangadamajhi, G.; Kar, A.; Rout, R.; Dhangadamajhi, P. A meta-analysis of TLR4 and TLR9 SNPs implicated in severe malaria. Rev. Soc. Bras. Med. Trop. 2017, 50, 153–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trottier, H.; Elliott, S.J. World Health Organization recommends first malaria vaccine. Can. J. Public Health 2021, 112, 967–969. [Google Scholar] [CrossRef]
- Gause, W.C.; Maizels, R.M. Macrobiota—Helminths as active participants and partners of the microbiota in host intestinal homeostasis. Curr. Opin. Microbiol. 2016, 32, 14–18. [Google Scholar] [CrossRef] [Green Version]
- WHO. WHO_TRS_972_eng.pdf.part. Research Priorities for Helminth Infections. Available online: https://apps.who.int/iris/bitstream/handle/10665/75922/WHO_TRS_972_eng.pdf?sequence=1&isAllowed=y (accessed on 22 March 2022).
- Gazzinelli-Guimaraes, P.H.; Nutman, T.B. Helminth parasites and immune regulation. F1000Research 2018, 7, 1685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rujeni, N.; Morona, D.; Ruberanziza, E.; Mazigo, H.D. Schistosomiasis and soil-transmitted helminthiasis in Rwanda: An update on their epidemiology and control. Infect. Dis. Poverty 2017, 6, 8. [Google Scholar] [CrossRef] [Green Version]
- Afolabi, M.O.; Ale, B.M.; Dabira, E.D.; Agbla, S.C.; Bustinduy, A.L.; Ndiaye, J.L.A.; Greenwood, B. Malaria and helminth co-infections in children living in endemic countries: A systematic review with meta-analysis. PLOS Negl. Trop. Dis. 2021, 15, e0009138. [Google Scholar] [CrossRef] [PubMed]
- Abbate, J.L.; Ezenwa, V.O.; Guégan, J.-F.; Choisy, M.; Nacher, M.; Roche, B. Disentangling complex parasite interactions: Protection against cerebral malaria by one helminth species is jeopardized by co-infection with another. PLOS Negl. Trop. Dis. 2018, 12, e0006483. [Google Scholar] [CrossRef] [Green Version]
- Degarege, A.; Animut, A.; Legesse, M.; Erko, B. Malaria severity status in patients with soil-transmitted helminth infections. Acta Trop. 2009, 112, 8–11. [Google Scholar] [CrossRef]
- Degarege, A.; Legesse, M.; Medhin, G.; Animut, A.; Erko, B. Malaria and related outcomes in patients with intestinal helminths: A cross-sectional study. BMC Infect. Dis. 2012, 12, 291. [Google Scholar] [CrossRef] [Green Version]
- Nacher, M.; Singhasivanon, P.; Yimsamran, S.; Manibunyong, W.; Thanyavanich, N.; Wuthisen, P.; Looareesuwan, S. Intestinal Helminth Infections Are Associated with Increased Incidence of Plasmodium falciparum Malaria in Thailand. J. Parasitol. 2002, 88, 55. [Google Scholar] [CrossRef]
- Kwenti, T.E.; Nkume, F.A.; Tanjeko, A.T.; Kwenti, T.D.B. The Effect of Intestinal Parasitic Infection on the Clinical Outcome of Malaria in Coinfected Children in Cameroon. PLoS Negl. Trop. Dis. 2016, 10, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Mulu, A.; Kassu, A.; Legesse, M.; Erko, B.; Nigussie, D.; Shimelis, T.; Belyhun, Y.; Moges, B.; Ota, F.; Elias, D. Helminths and malaria co-infections are associated with elevated serum IgE. Parasites Vectors 2014, 7, 240. [Google Scholar] [CrossRef] [Green Version]
- Paone, P.; Cani, P.D. Mucus barrier, mucins and gut microbiota: The expected slimy partners? Gut 2020, 69, 2232–2243. [Google Scholar] [CrossRef] [PubMed]
- Cani, P.D.; Van Hul, M.; Lefort, C.; Depommier, C.; Rastelli, M.; Everard, A. Microbial regulation of organismal energy homeostasis. Nat. Metab. 2019, 1, 34–46. [Google Scholar] [CrossRef]
- Rinninella, E.; Raoul, P.; Cintoni, M.; Franceschi, F.; Miggiano, G.A.D.; Gasbarrini, A.; Mele, M.C. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. 2019. Microorganisms 2019, 7, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huttenhower, C.; Gevers, D.; Knight, R.; Abubucker, S.; Badger, J.H.; Chinwalla, A.T.; Creasy, H.H.; Earl, A.M.; FitzGerald, M.G.; Fulton, R.S.; et al. Structure, function and diversity of the healthy human microbiome. Nature 2012, 486, 207–214. [Google Scholar]
- Wang, B.; Yao, M.; Lv, L.; Ling, Z.; Li, L. The Human Microbiota in Health and Disease. Engineering 2017, 3, 71–82. [Google Scholar] [CrossRef]
- The Human Microbiome Project Consortium. A framework for human microbiome research. Nature 2012, 486, 215–221. [Google Scholar] [CrossRef] [Green Version]
- Dethlefsen, L.; Relman, D.A. Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc. Natl. Acad. Sci. USA 2011, 108 (Suppl. 1), 4554–4561. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Filippo, C.; Cavalieri, D.; Di Paola, M.; Ramazzotti, M.; Poullet, J.B.; Massart, S.; Collini, S.; Pieraccini, G.; Lionetti, P. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl. Acad. Sci. USA 2010, 107, 14691–14696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cani, P.D.; Moens de Hase, E.; Van Hul, M. Gut Microbiota and Host Metabolism: From Proof of Concept to Therapeutic Intervention. Microorganisms 2021, 9, 1302. [Google Scholar] [CrossRef]
- Cohen, I.; Ruff, W.E.; Longbrake, E.E. Influence of immunomodulatory drugs on the gut microbiota. Transl. Res. 2021, 233, 144–161. [Google Scholar] [CrossRef]
- Kamada, N.; Chen, G.Y.; Inohara, N.; Núñez, G. Control of pathogens and pathobionts by the gut microbiota. Nat. Immunol. 2013, 14, 685–690. [Google Scholar] [CrossRef]
- Bhatt, A.P.; Redinbo, M.R.; Bultman, S.J. The role of the microbiome in cancer development and therapy. CA Cancer J. Clin. 2017, 67, 326–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jheeta, S.; Smith, D. Seeing the wood for the trees: A new way to view the human intestinal microbiome and its connection with non-communicable disease. Med. Hypotheses 2019, 125, 70–74. [Google Scholar] [CrossRef]
- Cani, P.D.; Delzenne, N. The gut microbiome as therapeutic target. Pharmacol. Ther. 2011, 130, 202–212. [Google Scholar] [CrossRef]
- Langan, D.; Kim, E.Y.; Moudgil, K.D. Modulation of autoimmune arthritis by environmental ‘hygiene’ and commensal microbiota. Cell. Immunol. 2019, 339, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Holm, J.B.; Sorobetea, D.; Kiilerich, P.; Ramayo-Caldas, Y.; Estellé, J.; Ma, T.; Madsen, L.; Kristiansen, K.; Svensson-Frej, M. Data from: Chronic Trichuris muris Infection Decreases Diversity of the Intestinal Microbiota and Concomitantly Increases the Abundance of Lactobacilli. PLoS ONE 2015, 10, e0125495. [Google Scholar] [CrossRef]
- Yilmaz, B.; Portugal, S.; Tran, T.M.; Gozzelino, R.; Ramos, S.; Gomes, J.; Regalado, A.; Cowan, P.J.; d’Apice, A.J.; Chong, A.S.; et al. Article Gut Microbiota Elicits a Protective Immune Response against Malaria Transmission. Cell 2014, 159, 1277–1289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yooseph, S.; Kirkness, E.F.; Tran, T.M.; Harkins, D.M.; Jones, M.B.; Torralba, M.G.; O’Connell, E.; Nutman, T.B.; Doumbo, S.; Doumbo, O.K.; et al. Stool microbiota composition is associated with the prospective risk of Plasmodium falciparum infection. BMC Genom. 2015, 16, 631. [Google Scholar] [CrossRef]
- Mandal, R.K.; Denny, J.E.; Namazzi, R.; Opoka, R.O.; Datta, D.; John, C.C.; Schmidt, N.W. Dynamic modulation of spleen germinal center reactions by gut bacteria during Plasmodium infection. Cell Rep. 2021, 35, 109094. [Google Scholar] [CrossRef]
- Villarino, N.F.; LeCleir, G.R.; Denny, J.E.; Dearth, S.P.; Harding, C.L.; Sloan, S.S.; Gribble, J.L.; Campagna, S.R.; Wilhelm, S.W.; Schmidt, N.W. Composition of the gut microbiota modulates the severity of malaria. Proc. Natl. Acad. Sci. USA 2016, 113, 2235–2240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mooney, J.; Lokken, K.L.; Byndloss, M.; George, M.D.; Velazquez, E.M.; Faber, F.; Butler, B.P.; Walker, G.T.; Ali, M.M.; Potts, R.; et al. Inflammation-associated alterations to the intestinal microbiota reduce colonization resistance against non-typhoidal Salmonella during concurrent malaria parasite infection. Sci. Rep. 2015, 5, srep14603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taniguchi, T.; Miyauchi, E.; Nakamura, S.; Hirai, M.; Suzue, K.; Imai, T.; Nomura, T.; Handa, T.; Okada, H.; Shimokawa, C.; et al. Plasmodium berghei ANKA causes intestinal malaria associated with dysbiosis. Sci. Rep. 2015, 5, 15699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guan, W.; Yang, S.; Zhao, Y.; Cheng, W.; Song, X.; Yao, Y.; Xie, Y.; Du, W.; Li, J. Observation of the Gut Microbiota Profile in C57BL/6 Mice Induced by Plasmodium berghei ANKA Infection. Front. Cell. Infect. Microbiol. 2021, 11, 680383. [Google Scholar] [CrossRef]
- Mandal, R.K.; Crane, R.J.; Berkley, J.; Gumbi, W.; Wambua, J.; Ngoi, J.M.; Ndungu, F.; Schmidt, N.W. Longitudinal Analysis of Infant Stool Bacteria Communities Before and After Acute Febrile Malaria and Artemether-Lumefantrine Treatment. J. Infect. Dis. 2018, 220, 687–698. [Google Scholar] [CrossRef] [PubMed]
- Ling, F.; Steinel, N.; Weber, J.; Ma, L.; Smith, C.; Correa, D.; Zhu, B.; Bolnick, D.; Wang, G. The gut microbiota response to helminth infection depends on host sex and genotype. ISME J. 2020, 14, 1141–1153. [Google Scholar] [CrossRef]
- Kupritz, J.; Angelova, A.; Nutman, T.B.; Gazzinelli-Guimaraes, P.H. Helminth-Induced Human Gastrointestinal Dysbiosis: A Systematic Review and Meta-Analysis Reveals Insights into Altered Taxon Diversity and Microbial Gradient Collapse. mBio 2021, 12, e0289021. [Google Scholar] [CrossRef]
- Myhill, L.J.; Stolzenbach, S.; Mejer, H.; Krych, L.; Jakobsen, S.R.; Kot, W.; Skovgaard, K.; Canibe, N.; Nejsum, P.; Nielsen, D.S.; et al. Parasite-Probiotic Interactions in the Gut: Bacillus sp. and Enterococcus faecium Regulate Type-2 Inflammatory Responses and Modify the Gut Microbiota of Pigs During Helminth Infection. Front. Immunol. 2022, 12, 793260. [Google Scholar] [CrossRef]
- Barelli, C.; Donati, C.; Albanese, D.; Pafčo, B.; Modrý, D.; Rovero, F.; Hauffe, H.C. Interactions between parasitic helminths and gut microbiota in wild tropical primates from intact and fragmented habitats. Sci. Rep. 2021, 11, 21569. [Google Scholar] [CrossRef]
- Stough, J.M.A.; Dearth, S.P.; Denny, J.E.; LeCleir, G.R.; Schmidt, N.W.; Campagna, S.R.; Wilhelm, S.W. Functional Characteristics of the Gut Microbiome in C57BL/6 Mice Differentially Susceptible to Plasmodium yoelii. Front. Microbiol. 2016, 7, 1520. [Google Scholar] [CrossRef] [Green Version]
- Hansen, D.S.; Schofield, L. Natural Regulatory T Cells in Malaria: Host or Parasite Allies? PLOS Pathog. 2010, 6, e1000771. [Google Scholar] [CrossRef] [Green Version]
- Ishikawa, H.; Tanaka, K.; Maeda, Y.; Aiba, Y.; Hata, A.; Tsuji, N.M.; Koga, Y.; Matsumoto, T. Effect of intestinal microbiota on the induction of regulatory CD25+ CD4+ T cells. Clin. Exp. Immunol. 2008, 153, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; He, C.; Cong, Y.; Liu, Z. Regulatory immune cells in regulation of intestinal inflammatory response to microbiota. Mucosal Immunol. 2015, 8, 969–978. [Google Scholar] [CrossRef]
- Sun, S.; Luo, L.; Liang, W.; Yin, Q.; Guo, J.; Rush, A.M.; Lv, Z.; Liang, Q.; Fischbach, M.A.; Sonnenburg, J.L.; et al. Bifidobacterium alters the gut microbiota and modulates the functional metabolism of T regulatory cells in the context of immune checkpoint blockade. Proc. Natl. Acad. Sci. USA 2020, 117, 27509–27515. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mutoni, J.d.; Coutelier, J.-P.; Rujeni, N.; Mutesa, L.; Cani, P.D. Possible Interactions between Malaria, Helminthiases and the Gut Microbiota: A Short Review. Microorganisms 2022, 10, 721. https://doi.org/10.3390/microorganisms10040721
Mutoni Jd, Coutelier J-P, Rujeni N, Mutesa L, Cani PD. Possible Interactions between Malaria, Helminthiases and the Gut Microbiota: A Short Review. Microorganisms. 2022; 10(4):721. https://doi.org/10.3390/microorganisms10040721
Chicago/Turabian StyleMutoni, Jean d’Amour, Jean-Paul Coutelier, Nadine Rujeni, Leon Mutesa, and Patrice D. Cani. 2022. "Possible Interactions between Malaria, Helminthiases and the Gut Microbiota: A Short Review" Microorganisms 10, no. 4: 721. https://doi.org/10.3390/microorganisms10040721
APA StyleMutoni, J. d., Coutelier, J.-P., Rujeni, N., Mutesa, L., & Cani, P. D. (2022). Possible Interactions between Malaria, Helminthiases and the Gut Microbiota: A Short Review. Microorganisms, 10(4), 721. https://doi.org/10.3390/microorganisms10040721








