Molecular Typing of Ukrainian Bacillus anthracis Strains by Combining Whole-Genome Sequencing Techniques
Abstract
:1. Introduction
2. Materials and Methods
2.1. Strain Origin
2.2. DNA Isolation and Sequencing
2.3. Processing of Sequencing Data
2.4. Comparison to Public Database Entries
2.5. Genotyping
3. Results
3.1. Genome Sequencing
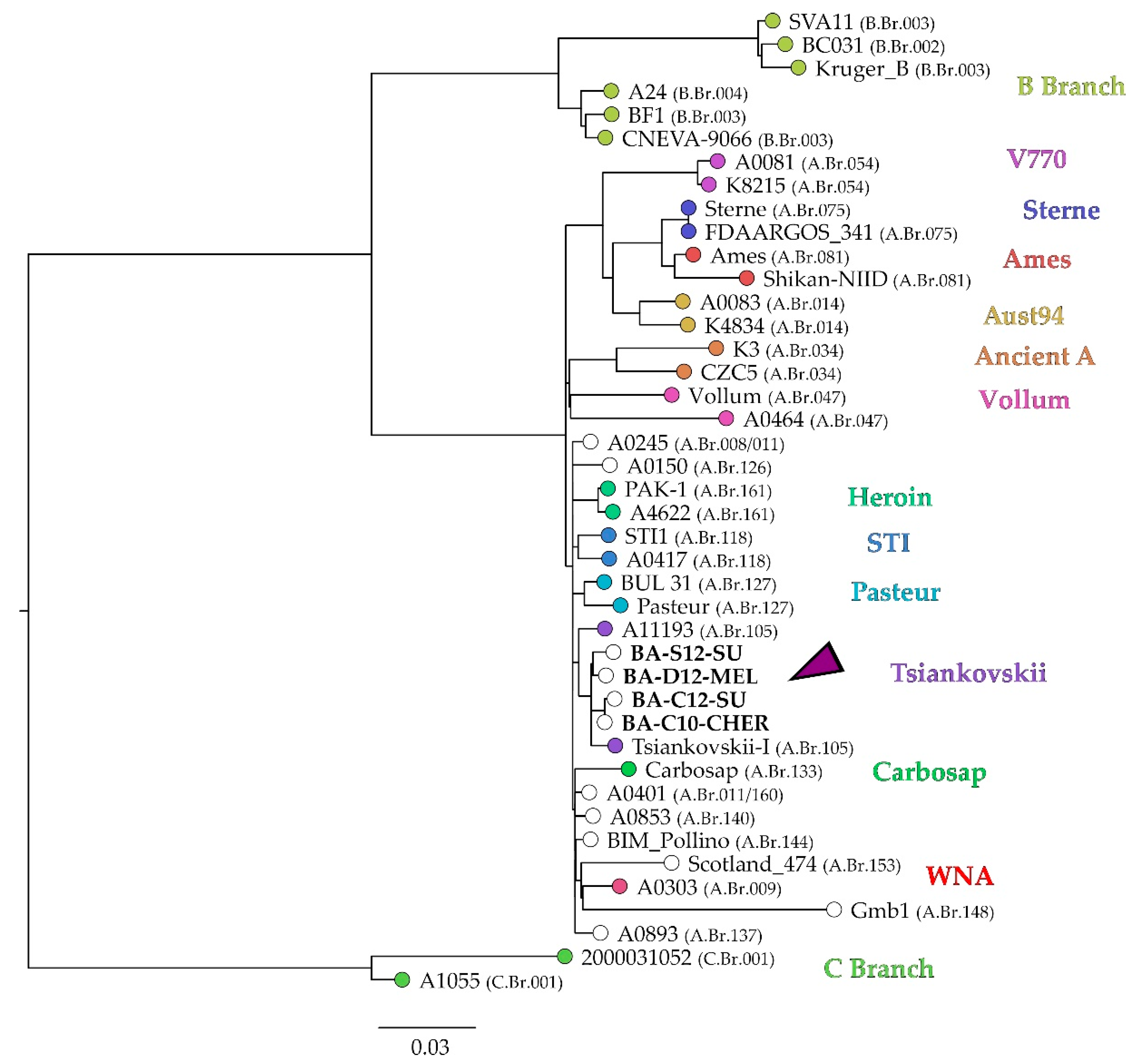
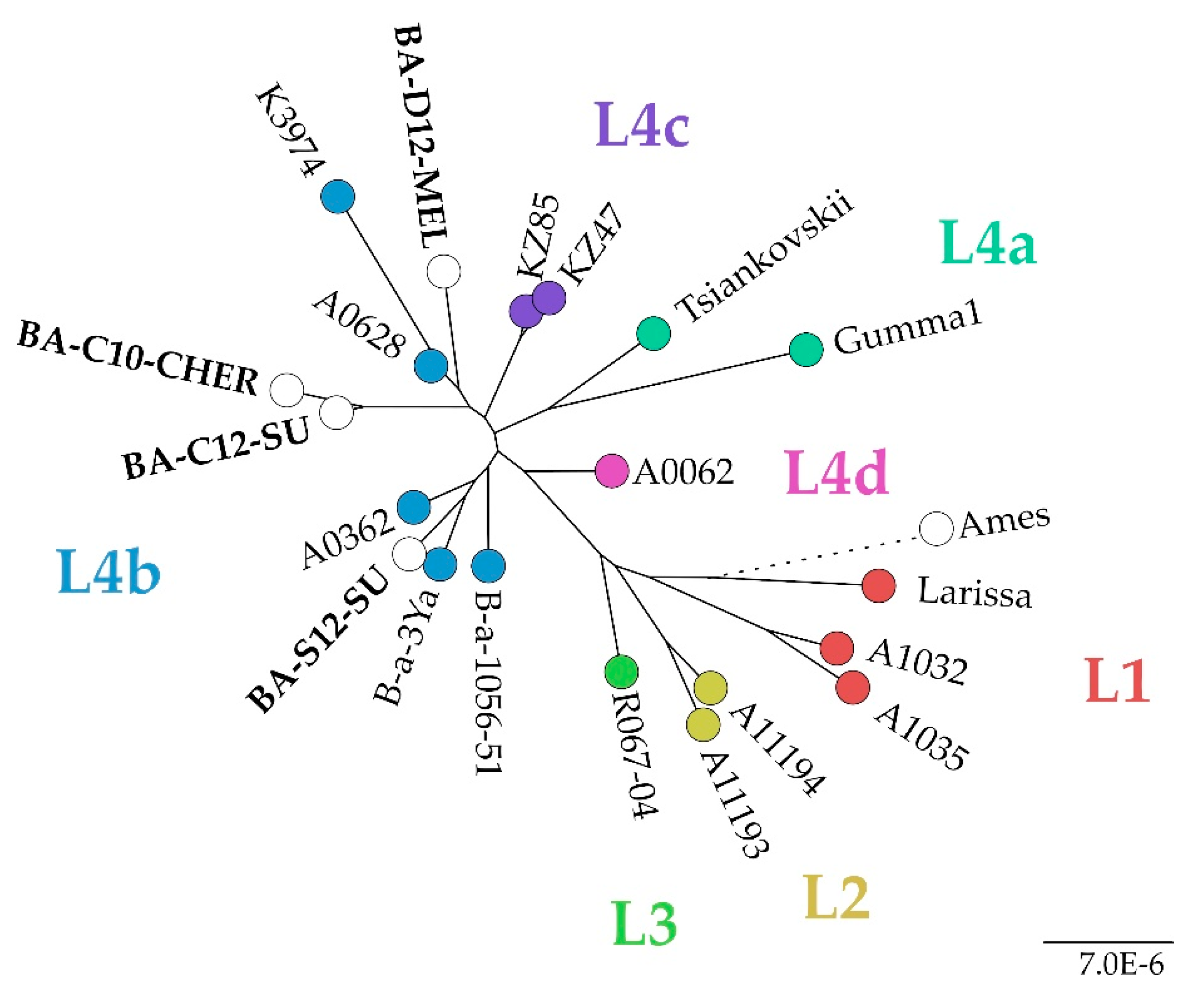
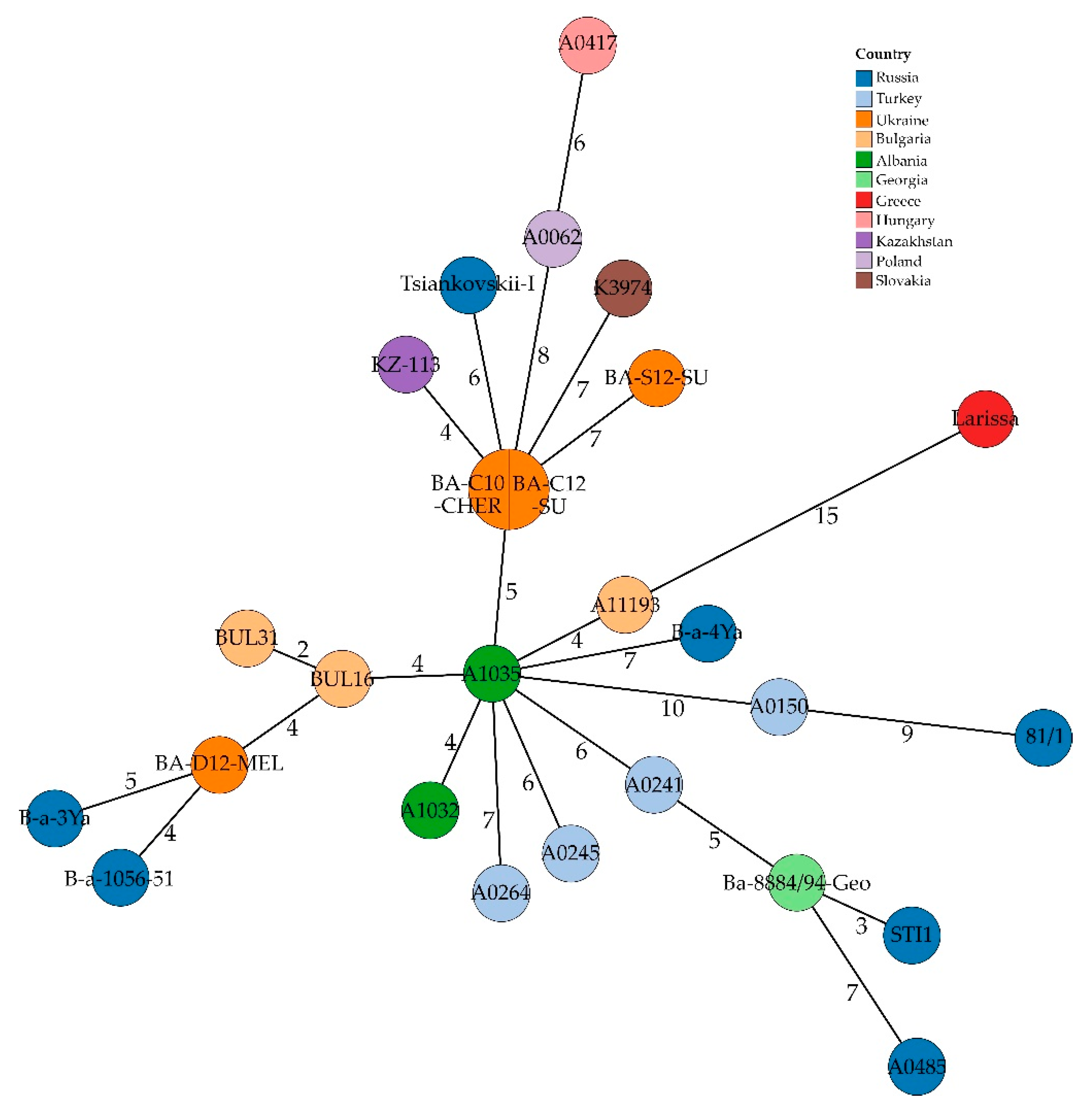
3.2. Genotyping
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oude Munnink, B.B.; Worp, N.; Nieuwenhuijse, D.F.; Sikkema, R.S.; Haagmans, B.; Fouchier, R.A.M.; Koopmans, M. The next phase of SARS-CoV-2 surveillance: Real-time molecular epidemiology. Nat. Med. 2021, 27, 1518–1524. [Google Scholar] [CrossRef] [PubMed]
- Pilo, P.; Frey, J. Bacillus anthracis: Molecular taxonomy, population genetics, phylogeny and patho-evolution. Infect. Genet. Evol. 2011, 11, 1218–1224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wattiau, P.; Klee, S.R.; Fretin, D.; Van Hessche, M.; Menart, M.; Franz, T.; Chasseur, C.; Butaye, P.; Imberechts, H. Occurrence and genetic diversity of Bacillus anthracis strains isolated in an active wool-cleaning factory. Appl. Environ. Microbiol. 2008, 74, 4005–4011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popescu, R.; Pistol, A.; Miltaru, L.; Caplan, D.; Cucuiu, R.; Popovici, F. Two cases of infection with Bacillus anthracis, Romania, October 2011. Euro. Surveill. 2011, 16, 20008. [Google Scholar] [CrossRef]
- Carlson, C.J.; Kracalik, I.T.; Ross, N.; Alexander, K.A.; Hugh-Jones, M.E.; Fegan, M.; Elkin, B.T.; Epp, T.; Shury, T.K.; Zhang, W.; et al. The global distribution of Bacillus anthracis and associated anthrax risk to humans, livestock and wildlife. Nat. Microbiol. 2019, 4, 1337–1343. [Google Scholar] [CrossRef] [Green Version]
- Pilo, P.; Perreten, V.; Frey, J. Molecular epidemiology of Bacillus anthracis: Determining the correct origin. Appl. Environ. Microbiol. 2008, 74, 2928–2931. [Google Scholar] [CrossRef] [Green Version]
- Elvander, M.; Persson, B.; Sternberg Lewerin, S. Historical cases of anthrax in Sweden 1916-1961. Transbound. Emerg. Dis. 2017, 64, 892–898. [Google Scholar] [CrossRef] [Green Version]
- Bezymennyi, M.; Bagamian, K.H.; Barro, A.; Skrypnyk, A.; Skrypnyk, V.; Blackburn, J.K. Spatio-temporal patterns of livestock anthrax in Ukraine during the past century (1913–2012). Appl. Geogr. 2014, 54, 129–138. [Google Scholar] [CrossRef]
- Timofeev, V.; Bahtejeva, I.; Mironova, R.; Titareva, G.; Lev, I.; Christiany, D.; Borzilov, A.; Bogun, A.; Vergnaud, G. Insights from Bacillus anthracis strains isolated from permafrost in the tundra zone of Russia. PLoS ONE 2019, 14, e0209140. [Google Scholar] [CrossRef] [Green Version]
- Chiaverini, A.; Abdel-Glil, M.Y.; Linde, J.; Galante, D.; Rondinone, V.; Fasanella, A.; Camma, C.; D’Alterio, N.; Garofolo, G.; Tomaso, H. Whole genome sequencing for studying Bacillus anthracis from an outbreak in the Abruzzo region of Italy. Microorganisms 2020, 8, 87. [Google Scholar] [CrossRef] [Green Version]
- Gobeli Brawand, S.; Kittl, S.; Dettwiler, M.; Thomann, A.; Feyer, S.; Cachim, J.; Theubet, G.; Liechti, N.; Wittwer, M.; Schurch, N.; et al. An unusual case of bovine anthrax in the canton of Jura, Switzerland in 2017. BMC Vet. Res. 2019, 15, 265. [Google Scholar] [CrossRef] [Green Version]
- Stratilo, C.W.; Bader, D.E. Genetic diversity among Bacillus anthracis soil isolates at fine geographic scales. Appl. Environ. Microbiol. 2012, 78, 6433–6437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biloivan, O.V.; Stegniy, B.T.; Gerilovych, A.P.; Arefiev, V.L.; Wölfel, R.; Schwarz, J.; Popp, C.; Grass, G. Screening of possibly anthrax-contaminated burial sites in eastern and southern Ukraine. Agric. Sci. Pract. 2020, 7, 3–14. [Google Scholar] [CrossRef]
- Hugh-Jones, M.; Blackburn, J. The ecology of Bacillus anthracis. Mol. Asp. Med. 2009, 30, 356–367. [Google Scholar] [CrossRef] [PubMed]
- Bagamian, K.H.; Skrypnyk, A.; Rodina, Y.; Bezymennyi, M.; Nevolko, O.; Skrypnyk, V.; Blackburn, J.K. Serological anthrax surveillance in wild boar (Sus scrofa) in Ukraine. Vector Borne Zoonotic Dis. 2014, 14, 618–620. [Google Scholar] [CrossRef]
- Keim, P.; Grunow, R.; Vipond, R.; Grass, G.; Hoffmaster, A.; Birdsell, D.N.; Klee, S.R.; Pullan, S.; Antwerpen, M.; Bayer, B.N.; et al. Whole genome analysis of injectional anthrax identifies two disease clusters spanning more than 13 years. EBioMedicine 2015, 2, 1613–1618. [Google Scholar] [CrossRef] [Green Version]
- Price, E.P.; Seymour, M.L.; Sarovich, D.S.; Latham, J.; Wolken, S.R.; Mason, J.; Vincent, G.; Drees, K.P.; Beckstrom-Sternberg, S.M.; Phillippy, A.M.; et al. Molecular epidemiologic investigation of an anthrax outbreak among heroin users, Europe. Emerg. Infect. Dis. 2012, 18, 1307–1313. [Google Scholar] [CrossRef]
- Keim, P.; Van Ert, M.N.; Pearson, T.; Vogler, A.J.; Huynh, L.Y.; Wagner, D.M. Anthrax molecular epidemiology and forensics: Using the appropriate marker for different evolutionary scales. Infect. Genet. Evol. 2004, 4, 205–213. [Google Scholar] [CrossRef]
- Keim, P.; Gruendike, J.M.; Klevytska, A.M.; Schupp, J.M.; Challacombe, J.; Okinaka, R. The genome and variation of Bacillus anthracis. Mol. Asp. Med. 2009, 30, 397–405. [Google Scholar] [CrossRef] [Green Version]
- Abdel-Glil, M.Y.; Chiaverini, A.; Garofolo, G.; Fasanella, A.; Parisi, A.; Harmsen, D.; Jolley, K.A.; Elschner, M.C.; Tomaso, H.; Linde, J.; et al. A whole-genome-based gene-by-gene typing system for standardized high-resolution strain typing of Bacillus anthracis. J. Clin. Microbiol. 2021, 59, e0288920. [Google Scholar] [CrossRef]
- Bruce, S.A.; Schiraldi, N.J.; Kamath, P.L.; Easterday, W.R.; Turner, W.C. A classification framework for Bacillus anthracis defined by global genomic structure. Evol. Appl. 2020, 13, 935–944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Ert, M.N.; Easterday, W.R.; Huynh, L.Y.; Okinaka, R.T.; Hugh-Jones, M.E.; Ravel, J.; Zanecki, S.R.; Pearson, T.; Simonson, T.S.; U’Ren, J.M.; et al. Global genetic population structure of Bacillus anthracis. PLoS ONE 2007, 2, e461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sahl, J.W.; Pearson, T.; Okinaka, R.; Schupp, J.M.; Gillece, J.D.; Heaton, H.; Birdsell, D.; Hepp, C.; Fofanov, V.; Noseda, R.; et al. A Bacillus anthracis genome sequence from the Sverdlovsk 1979 autopsy specimens. mBio 2016, 7, e01501–e01516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antwerpen, M.; Beyer, W.; Bassy, O.; Ortega-Garcia, M.V.; Cabria-Ramos, J.C.; Grass, G.; Wolfel, R. Phylogenetic placement of isolates within the Trans-Eurasian clade A.Br.008/009 of Bacillus anthracis. Microorganisms 2019, 7, 689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biloivan, O.V.; Stegniy, B.T.; Arefiev, V.L.; Solodiankin, O.S.; Gerilovych, A.P.; Duerr, A.; Schwarz, J.; Grass, G.; Napnenko, O.O.; Deryabin, O.M. Phylogenetic analysis of Ukrainian Bacillus anthracis strains from various sources. J. Vet. Med. Biotechnol. Biosaf. 2018, 4, 5–11. [Google Scholar] [CrossRef]
- Blackburn, J.K.; Skrypnyk, A.; Bagamian, K.H.; Nikolich, M.P.; Bezymennyi, M.; Skrypnyk, V. Anthrax in a backyard domestic dog in Ukraine: A case report. Vector Borne Zoonotic Dis. 2014, 14, 615–617. [Google Scholar] [CrossRef]
- Wood, D.E.; Lu, J.; Langmead, B. Improved metagenomic analysis with Kraken 2. Genome Biol. 2019, 20, 257. [Google Scholar] [CrossRef] [Green Version]
- Seemann, T. Prokka: Rapid prokaryotic genome annotation. Bioinformatics 2014, 30, 2068–2069. [Google Scholar] [CrossRef]
- Murigneux, V.; Roberts, L.W.; Forde, B.M.; Phan, M.-D.; Nhu, N.T.K.; Irwin, A.D.; Harris, P.N.A.; Paterson, D.L.; Schembri, M.A.; Whiley, D.M.; et al. MicroPIPE: Validating an end-to-end workflow for high-quality complete bacterial genome construction. BMC Genom. 2021, 22, 474. [Google Scholar] [CrossRef]
- De Coster, W.; D’Hert, S.; Schultz, D.T.; Cruts, M.; Van Broeckhoven, C. NanoPack: Visualizing and processing long-read sequencing data. Bioinformatics 2018, 34, 2666–2669. [Google Scholar] [CrossRef]
- Gurevich, A.; Saveliev, V.; Vyahhi, N.; Tesler, G. QUAST: Quality assessment tool for genome assemblies. Bioinformatics 2013, 29, 1072–1075. [Google Scholar] [CrossRef] [PubMed]
- Keim, P.; Price, L.B.; Klevytska, A.M.; Smith, K.L.; Schupp, J.M.; Okinaka, R.; Jackson, P.J.; Hugh-Jones, M.E. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 2000, 182, 1928–1936. [Google Scholar] [CrossRef] [Green Version]
- Jain, C.; Rodriguez-R, L.M.; Phillippy, A.M.; Konstantinidis, K.T.; Aluru, S. High throughput ANI analysis of 90K prokaryotic genomes reveals clear species boundaries. Nat. Commun. 2018, 9, 5114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lärkeryd, A.; Myrtennäs, K.; Karlsson, E.; Dwibedi, C.K.; Forsman, M.; Larsson, P.; Johansson, A.; Sjödin, A. CanSNPer: A hierarchical genotype classifier of clonal pathogens. Bioinformatics 2014, 30, 1762–1764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, Z.; Alikhan, N.F.; Sergeant, M.J.; Luhmann, N.; Vaz, C.; Francisco, A.P.; Carrico, J.A.; Achtman, M. GrapeTree: Visualization of core genomic relationships among 100,000 bacterial pathogens. Genome Res. 2018, 28, 1395–1404. [Google Scholar] [CrossRef] [Green Version]
- Treangen, T.J.; Ondov, B.D.; Koren, S.; Phillippy, A.M. The harvest suite for rapid core-genome alignment and visualization of thousands of intraspecific microbial genomes. Genome Biol. 2014, 15, 524. [Google Scholar] [CrossRef] [Green Version]
- Stamatakis, A. RAxML version 8: A tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics 2014, 30, 1312–1313. [Google Scholar] [CrossRef]
- Jünemann, S.; Sedlazeck, F.J.; Prior, K.; Albersmeier, A.; John, U.; Kalinowski, J.; Mellmann, A.; Goesmann, A.; von Haeseler, A.; Stoye, J.; et al. Updating benchtop sequencing performance comparison. Nat. Biotechnol. 2013, 31, 294–296. [Google Scholar] [CrossRef] [Green Version]
- Shevtsov, A.; Lukhnova, L.; Izbanova, U.; Vernadet, J.-P.; Kuibagarov, M.; Amirgazin, A.; Ramankulov, Y.; Vergnaud, G. Bacillus anthracis phylogeography: New clues from Kazakhstan, Central Asia. Front. Microbiol. 2021, 12, 778225. [Google Scholar] [CrossRef]
- Aanensen, D.M.; Feil, E.J.; Holden, M.T.; Dordel, J.; Yeats, C.A.; Fedosejev, A.; Goater, R.; Castillo-Ramirez, S.; Corander, J.; Colijn, C.; et al. Whole-genome sequencing for routine pathogen surveillance in public health: A population snapshot of invasive Staphylococcus aureus in Europe. mBio 2016, 7, e00444-16. [Google Scholar] [CrossRef] [Green Version]
- Nadon, C.; Van Walle, I.; Gerner-Smidt, P.; Campos, J.; Chinen, I.; Concepcion-Acevedo, J.; Gilpin, B.; Smith, A.M.; Man Kam, K.; Perez, E.; et al. PulseNet International: Vision for the implementation of whole genome sequencing (WGS) for global food-borne disease surveillance. Euro. Surveill. 2017, 22, 30544. [Google Scholar] [CrossRef] [PubMed]
- Hirabayashi, A.; Yanagisawa, H.; Takahashi, H.; Yahara, K.; Boeing, P.; Wolfenden, B.; Nov, V.; Lorn, V.; Veng, M.; Ann, V.; et al. On-site genomic epidemiological analysis of antimicrobial-resistant bacteria in Cambodia with portable laboratory equipment. Front. Microbiol 2021, 12, 675463. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, H.P.; Bugrysheva, J.V.; Conley, A.B.; Gulvik, C.A.; Cherney, B.; Kolton, C.B.; Marston, C.K.; Saile, E.; Swaney, E.; Lonsway, D.; et al. Rapid nanopore whole-genome sequencing for anthrax emergency preparedness. Emerg. Infect. Dis. 2020, 26, 358–361. [Google Scholar] [CrossRef] [PubMed]
- Berbers, B.; Saltykova, A.; Garcia-Graells, C.; Philipp, P.; Arella, F.; Marchal, K.; Winand, R.; Vanneste, K.; Roosens, N.H.C.; De Keersmaecker, S.C.J. Combining short and long read sequencing to characterize antimicrobial resistance genes on plasmids applied to an unauthorized genetically modified Bacillus. Sci Rep. 2020, 10, 4310. [Google Scholar] [CrossRef] [PubMed]
- Gargis, A.S.; Cherney, B.; Conley, A.B.; McLaughlin, H.P.; Sue, D. Rapid detection of genetic engineering, structural variation, and antimicrobial resistance markers in bacterial biothreat pathogens by nanopore sequencing. Sci. Rep. 2019, 9, 13501. [Google Scholar] [CrossRef]
- De Maio, N.; Shaw, L.P.; Hubbard, A.; George, S.; Sanderson, N.D.; Swann, J.; Wick, R.; AbuOun, M.; Stubberfield, E.; Hoosdally, S.J.; et al. Comparison of long-read sequencing technologies in the hybrid assembly of complex bacterial genomes. Microb. Genom. 2019, 5, e000294. [Google Scholar] [CrossRef]
- Pisarenko, S.V.; Eremenko, E.I.; Ryazanova, A.G.; Kovalev, D.A.; Buravtseva, N.P.; Aksenova, L.Y.; Evchenko, A.Y.; Semenova, O.V.; Bobrisheva, O.V.; Kuznetsova, I.V.; et al. Genotyping and phylogenetic location of one clinical isolate of Bacillus anthracis isolated from a human in Russia. BMC Microbiol. 2019, 19, 165. [Google Scholar] [CrossRef]
- Deneke, C.; Uelze, L.; Brendebach, H.; Tausch, S.H.; Malorny, B. Decentralized investigation of bacterial outbreaks based on hashed cgMLST. Front. Microbiol. 2021, 12, 649517. [Google Scholar] [CrossRef]
- Lüth, S.; Deneke, C.; Kleta, S.; Al Dahouk, S. Translatability of WGS typing results can simplify data exchange for surveillance and control of Listeria monocytogenes. Microb. Genom. 2021, 7, mgen000491. [Google Scholar] [CrossRef]
- O’Reilly, J.E.; Puttick, M.N.; Pisani, D.; Donoghue, P.C.J. Probabilistic methods surpass parsimony when assessing clade support in phylogenetic analyses of discrete morphological data. Palaeontology 2018, 61, 105–118. [Google Scholar] [CrossRef] [Green Version]
- Eremenko, E.; Pechkovskii, G.; Pisarenko, S.; Ryazanova, A.; Kovalev, D.; Semenova, O.; Aksenova, L.; Timchenko, L.; Golovinskaya, T.; Bobrisheva, O.; et al. Phylogenetics of Bacillus anthracis isolates from Russia and bordering countries. Infect. Genet. Evol. 2021, 92, 104890. [Google Scholar] [CrossRef] [PubMed]
- Gierczyński, R.; Jakubczak, A.; Jagielski, M. Extended multiple-locus variable-number tandem-repeat analysis of Bacillus anthracis strains isolated in Poland. Pol. J. Microbiol. 2009, 58, 3–7. [Google Scholar] [PubMed]
- Pearson, T.; Busch, J.D.; Ravel, J.; Read, T.D.; Rhoton, S.D.; U’Ren, J.M.; Simonson, T.S.; Kachur, S.M.; Leadem, R.R.; Cardon, M.L.; et al. Phylogenetic discovery bias in Bacillus anthracis using single-nucleotide polymorphisms from whole-genome sequencing. Proc. Natl. Acad. Sci. USA 2004, 101, 13536–13541. [Google Scholar] [CrossRef] [Green Version]
- Agren, J.; Finn, M.; Bengtsson, B.; Segerman, B. Microevolution during an Anthrax outbreak leading to clonal heterogeneity and penicillin resistance. PLoS ONE 2014, 9, e89112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- FAO/Unesco. Soil Map of the World 1:5,000,000, Volume I, Legend; Unesco: Paris, France, 1974. [Google Scholar]


| Strain | Source | Year | Oblast/Province | Rajon/District | City |
|---|---|---|---|---|---|
| BA-C10-CHER | cattle | 2010 | Chernivtsi | Dniester | Khotyn |
| BA-D12-MEL | dog | 2012 | Zaporizhia | Melitopol | Voznesenka |
| BA-C12-SU | cattle | 2012 | Cherkasy | Cherkasy | Smila |
| BA-S12-SU | soil | 2012 | Sumy | Sumy | Sumy |
| Strain | Method | Coverage | Bases | Contigs | Indels per 100 kbp | N50 | L50 | RGF% * |
|---|---|---|---|---|---|---|---|---|
| BA-C10-CHER | SRS | 158 | 5,461,659 | 72 | 4.14 | 204,605 | 7 | 99.095 |
| ONT | 293 | 5,506,898 | 3 | 9.28 | 5,230,398 | 1 | 99.995 | |
| ONT/SRS | - | 5,506,660 | 3 | 4.42 | 5,230,171 | 1 | 99.995 | |
| BA-D12-MEL | SRS | 123 | 5,464,102 | 77 | 4.04 | 172,867 | 10 | 99.059 |
| ONT | 356 | 5,506,420 | 3 | 9.07 | 5,229,931 | 1 | 99.995 | |
| ONT/SRS | - | 5,506,276 | 3 | 4.32 | 5,229,793 | 1 | 99.995 | |
| BA-C12-SU | SRS | 85 | 5,450,437 | 144 | 4.21 | 117,282 | 14 | 98.762 |
| ONT | 377 | 5,506,896 | 3 | 9.18 | 5,230,396 | 1 | 99.995 | |
| ONT/SRS | - | 5,506,662 | 3 | 4.51 | 5,230,173 | 1 | 99.995 | |
| BA-S12-SU | SRS | 160 | 5,613,511 | 958 | 3.98 | 289,064 | 7 | 99.052 |
| ONT | 369 | 5,506,632 | 3 | 8.67 | 5,230,160 | 1 | 99.992 | |
| ONT/SRS | - | 5,506,423 | 3 | 4.45 | 5,229,957 | 1 | 99.992 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brangsch, H.; Golovko, A.; Pinchuk, N.; Deriabin, O.; Kyselova, T.; Linde, J.; Melzer, F.; Elschner, M.C. Molecular Typing of Ukrainian Bacillus anthracis Strains by Combining Whole-Genome Sequencing Techniques. Microorganisms 2022, 10, 461. https://doi.org/10.3390/microorganisms10020461
Brangsch H, Golovko A, Pinchuk N, Deriabin O, Kyselova T, Linde J, Melzer F, Elschner MC. Molecular Typing of Ukrainian Bacillus anthracis Strains by Combining Whole-Genome Sequencing Techniques. Microorganisms. 2022; 10(2):461. https://doi.org/10.3390/microorganisms10020461
Chicago/Turabian StyleBrangsch, Hanka, Anatolii Golovko, Nataliia Pinchuk, Oleg Deriabin, Tetiana Kyselova, Jörg Linde, Falk Melzer, and Mandy Carolina Elschner. 2022. "Molecular Typing of Ukrainian Bacillus anthracis Strains by Combining Whole-Genome Sequencing Techniques" Microorganisms 10, no. 2: 461. https://doi.org/10.3390/microorganisms10020461
APA StyleBrangsch, H., Golovko, A., Pinchuk, N., Deriabin, O., Kyselova, T., Linde, J., Melzer, F., & Elschner, M. C. (2022). Molecular Typing of Ukrainian Bacillus anthracis Strains by Combining Whole-Genome Sequencing Techniques. Microorganisms, 10(2), 461. https://doi.org/10.3390/microorganisms10020461






