Genomic Comparison of Salmonella Enteritidis Strains Isolated from Laying Hens and Humans in the Abruzzi Region during 2018
Abstract
1. Introduction
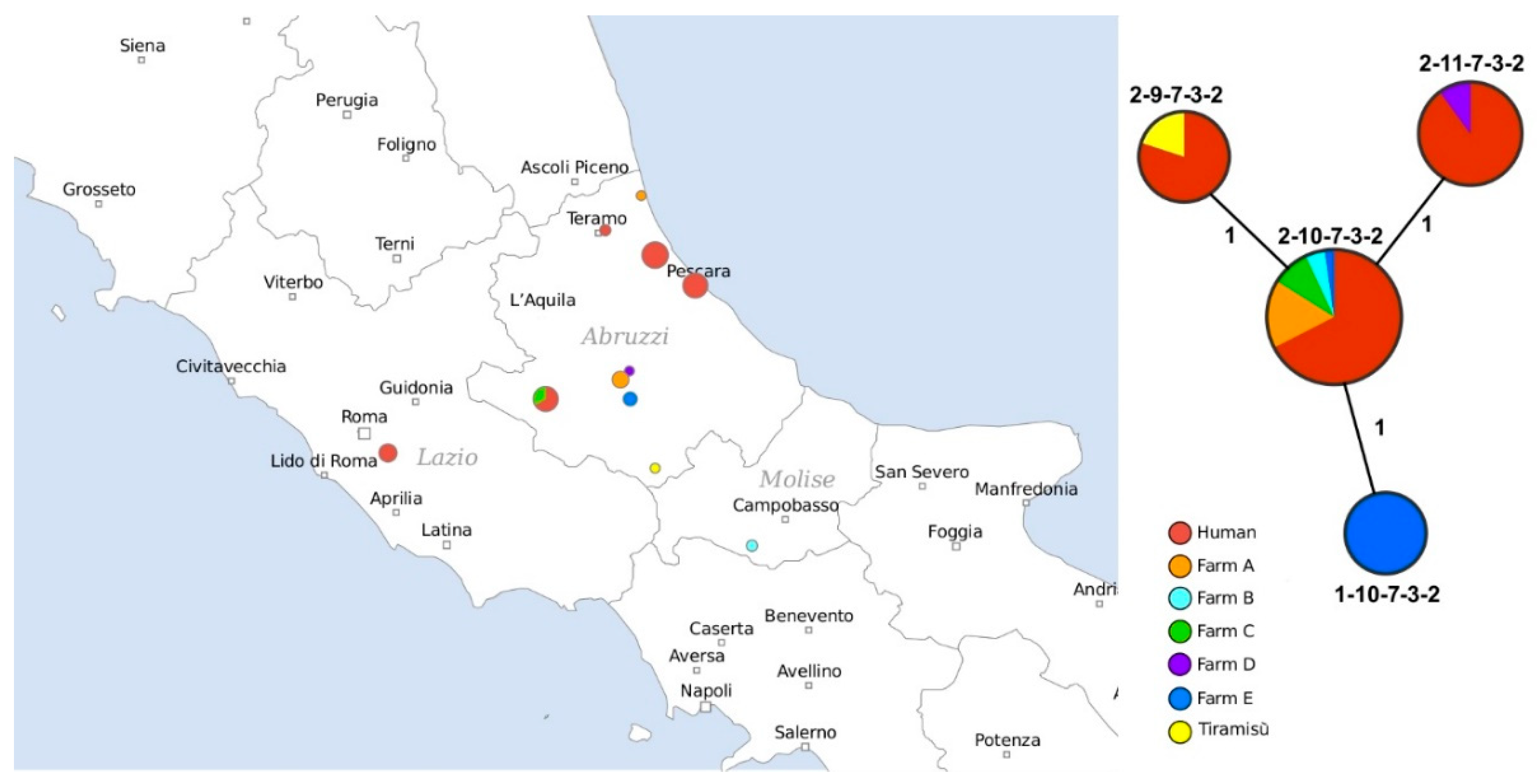
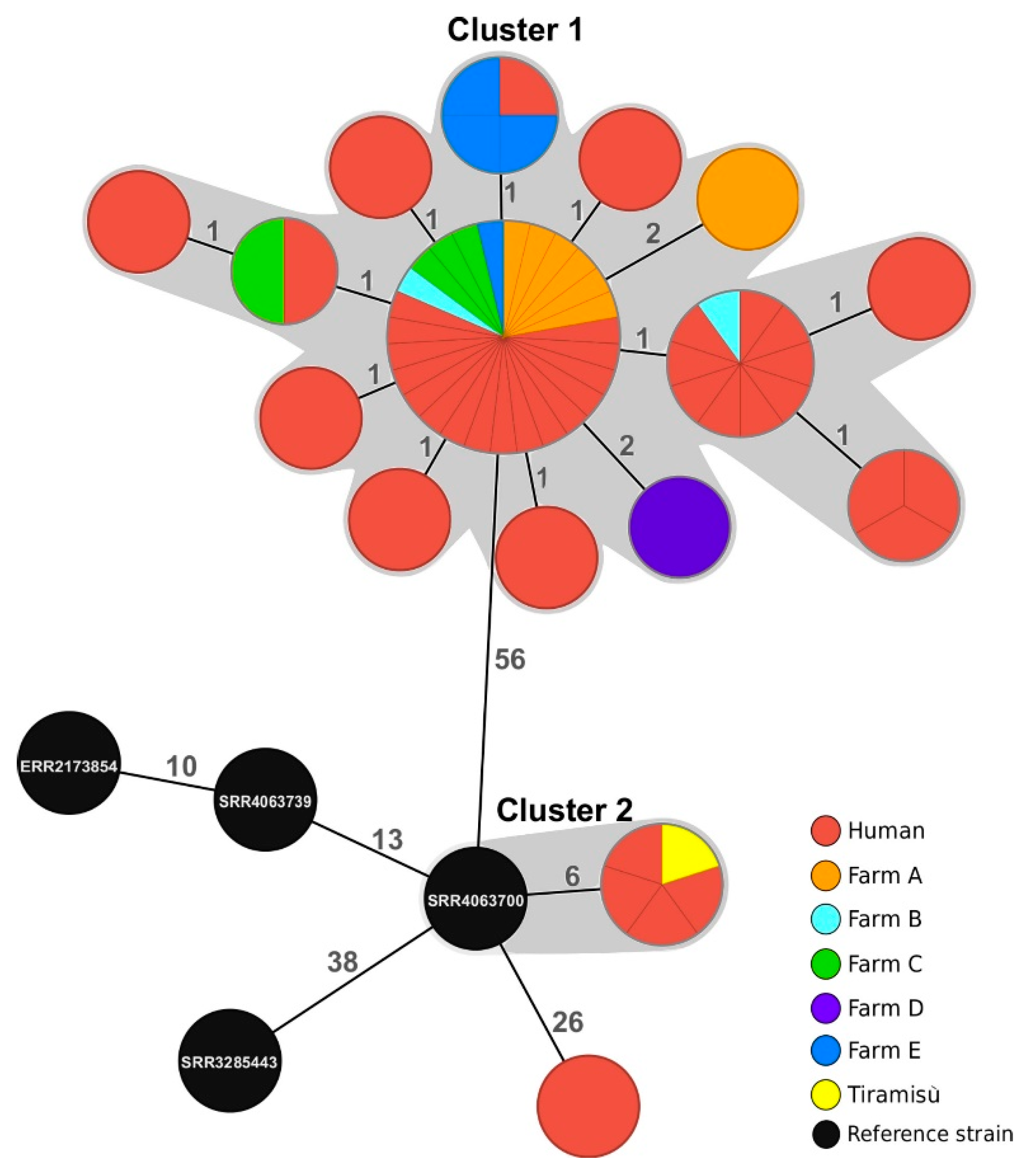
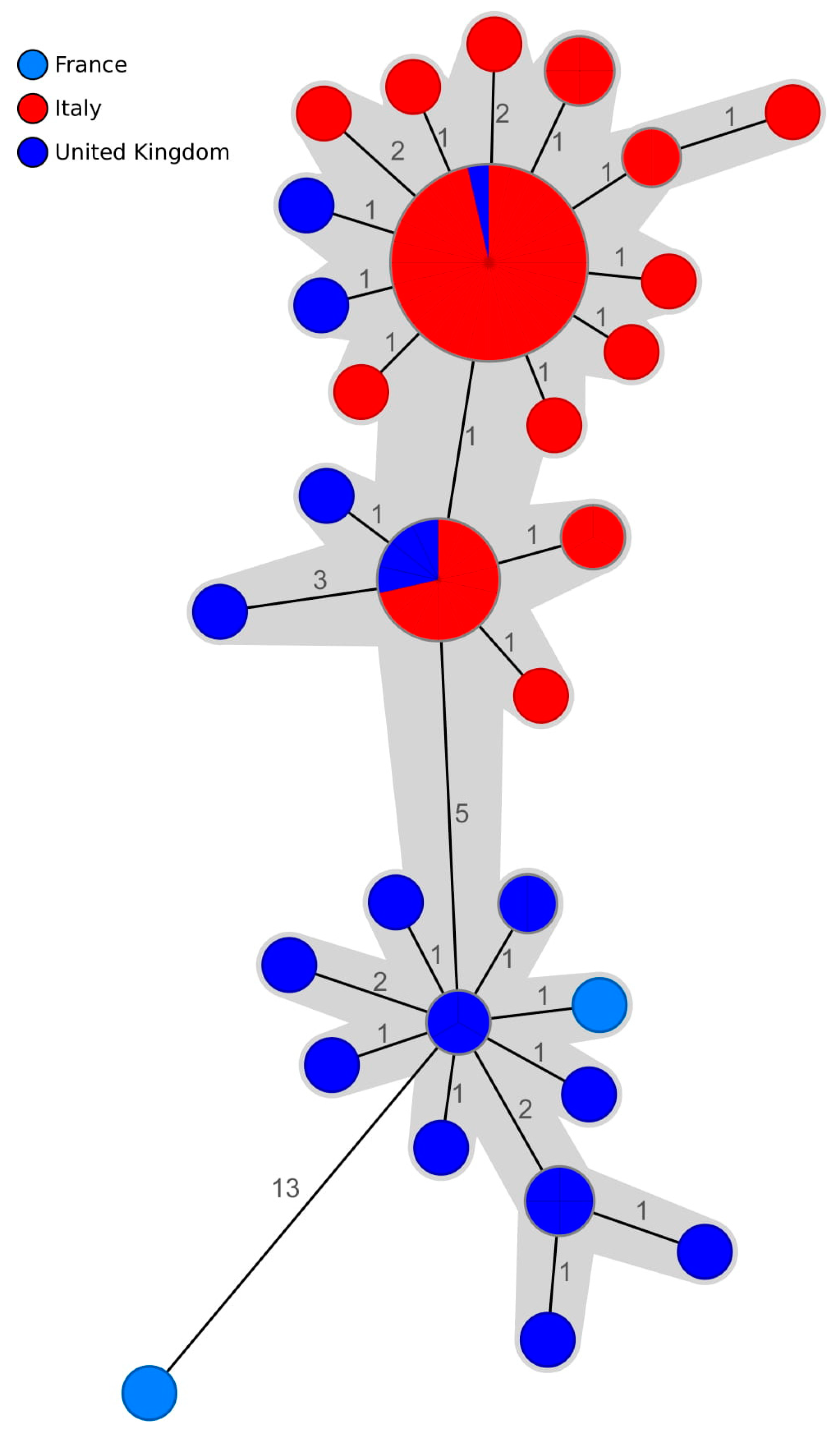
2. Results
3. Discussion
4. Materials and Methods
4.1. Dataset
4.2. Salmonella Culture and Serotyping
4.3. Multilocus Variable-Number Tandem Repeat Analysis
4.4. Next-Generation Sequencing
4.5. In Silico MLVA Analysis
4.6. MLST and Core-Genome MLST Analysis
4.7. SNP Address Assignment
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- EFSA and ECDC (European Food Safety Authority and European Centre for Disease Prevention and Control). The European union one health 2018 zoonoses report. EFSA J. 2019, 17, e05926. [Google Scholar] [CrossRef]
- Suzuki, S. Pathogenicity of salmonella enteritidis in poultry. Int. J. Food Microbiol. 1994, 21, 89–105. [Google Scholar] [CrossRef]
- Calvert, N.; Murphy, L.; Smith, A.; Copeland, D. A hotel-based outbreak of Salmonella enterica subsp. Enterica serovar Enteritidis (Salmonella Enteritidis) in the United Kingdom, 2006. Euro Surveill. Bull. Eur. Sur Les Mal. Transm. Eur. Commun. Dis. Bull. 2007, 12, 222. [Google Scholar] [CrossRef]
- Whiley, H.; Ross, K. Salmonella and eggs: From production to plate. Int. J. Environ. Res. Public Health 2015, 12, 2543–2556. [Google Scholar] [CrossRef] [PubMed]
- HPA. Salmonella Enteritidis PT1 associated with consumption of liquid egg product. In Health Protection Report 6; Health Protection Agency: London, UK, 2012; Volume 6, Available online: http://www.hpa.org.uk/hpr/archives/2012/hpr4212.pdf (accessed on 20 April 2020).
- Keerthirathne, T.P.; Ross, K.; Fallowfield, H.; Whiley, H. Reducing Risk of Salmonellosis through Egg Decontamination Processes. Int. J. Environ. Res. Public Health 2017, 14. [Google Scholar] [CrossRef]
- HPA. Two outbreaks of salmonellosis in the United Kingdom and Channel Islands putatively linked to imported pasteurised egg products. In Health Protection Report 1; Health Protection Agency: London, UK, 2007; Volume 1, Available online: http://www.hpa.org.uk/hpr/archives/2007/hpr4507.pdf (accessed on 20 April 2020).
- Wattiau, P.; Boland, C.; Bertrand, S. Methodologies for Salmonella enterica subsp. enterica subtyping: Gold standards and alternatives. Appl. Environ. Microbiol. 2011, 77, 7877–7885. [Google Scholar] [CrossRef]
- Hormansdorfer, S.; Messelhausser, U.; Rampp, A.; Schonberger, K.; Dallman, T.; Allerberger, F.; Kornschober, C.; Sing, A.; Wallner, P.; Zapf, A. Re-evaluation of a 2014 multi-country European outbreak of Salmonella Enteritidis phage type 14b using recent epidemiological and molecular data. Euro Surveill. Bull. Eur. Sur Les Mal. Transm. Eur. Commun. Dis. Bull. 2017, 22. [Google Scholar] [CrossRef]
- Foley, S.L.; Zhao, S.; Walker, R.D. Comparison of molecular typing methods for the differentiation of Salmonella foodborne pathogens. Foodborne Pathog. Dis. 2007, 4, 253–276. [Google Scholar] [CrossRef]
- Beranek, A.; Mikula, C.; Rabold, P.; Arnhold, D.; Berghold, C.; Lederer, I.; Allerberger, F.; Kornschober, C. Multiple-locus variable-number tandem repeat analysis for subtyping of Salmonella enterica subsp. enterica serovar Enteritidis. Int. J. Med Microbiol. 2009, 299, 43–51. [Google Scholar] [CrossRef]
- Boxrud, D.; Pederson-Gulrud, K.; Wotton, J.; Medus, C.; Lyszkowicz, E.; Besser, J.; Bartkus, J.M. Comparison of multiple-locus variable-number tandem repeat analysis, pulsed-field gel electrophoresis, and phage typing for subtype analysis of Salmonella enterica serotype Enteritidis. J. Clin. Microbiol. 2007, 45, 536–543. [Google Scholar] [CrossRef]
- Peters, T.; Bertrand, S.; Bjorkman, J.T.; Brandal, L.T.; Brown, D.J.; Erdosi, T.; Heck, M.; Ibrahem, S.; Johansson, K.; Kornschober, C.; et al. Multi-laboratory validation study of multilocus variable-number tandem repeat analysis (MLVA) for Salmonella enterica serovar Enteritidis, 2015. Euro Surveill. Bull. Eur. Sur Les Mal. Transm. Eur. Commun. Dis. Bull. 2017, 22. [Google Scholar] [CrossRef]
- Bertrand, S.; de Bex, G.D.L.; Wildemauwe, C.; Lunguya, O.; Phoba, M.F.; Ley, B.; Jacobs, J.; Vanhoof, R.; Mattheus, W. Correction: Multi Locus Variable-Number Tandem Repeat (MLVA) Typing Tools Improved the Surveillance of Salmonella Enteritidis: A 6 Years Retrospective Study. PLoS ONE 2018, 13, e0198527. [Google Scholar] [CrossRef] [PubMed]
- Taylor, A.J.; Lappi, V.; Wolfgang, W.J.; Lapierre, P.; Palumbo, M.J.; Medus, C.; Boxrud, D. Characterization of foodborne outbreaks of salmonella enterica serovar enteritidis with whole-genome sequencing single nucleotide polymorphism-based analysis for surveillance and outbreak detection. J. Clin. Microbiol. 2015, 53, 3334–3340. [Google Scholar] [CrossRef] [PubMed]
- Chattaway, M.A.; Dallman, T.J.; Larkin, L.; Nair, S.; McCormick, J.; Mikhail, A.; Hartman, H.; Godbole, G.; Powell, D.; Day, M.; et al. The transformation of reference microbiology methods and surveillance for salmonella with the use of whole genome sequencing in england and wales. Front. Public Health 2019, 7, 317. [Google Scholar] [CrossRef] [PubMed]
- Wuyts, V.; Denayer, S.; Roosens, N.H.; Mattheus, W.; Bertrand, S.; Marchal, K.; Dierick, K.; De Keersmaecker, S.C. Whole genome sequence analysis of salmonella enteritidis PT4 outbreaks from a national reference laboratory’s viewpoint. PLoS Curr. 2015, 7. [Google Scholar] [CrossRef]
- Dangel, A.; Berger, A.; Messelhausser, U.; Konrad, R.; Hormansdorfer, S.; Ackermann, N.; Sing, A. Genetic diversity and delineation of Salmonella Agona outbreak strains by next generation sequencing, Bavaria, Germany, 1993 to 2018. Euro Surveill. Bull. Eur. Sur Les Mal. Transm. Eur. Commun. Dis. Bull. 2019, 24. [Google Scholar] [CrossRef]
- EFSA and ECDC (European Food Safety Authority and European Centre for Disease Prevention and Control). Multi-country outbreak of Salmonella Enteritidis infections linked to eggs, third update – 6 February 2020. EFSA Supporting Publ. 2020, 17, 1799E. [Google Scholar] [CrossRef]
- Inns, T.; Ashton, P.M.; Herrera-Leon, S.; Lighthill, J.; Foulkes, S.; Jombart, T.; Rehman, Y.; Fox, A.; Dallman, T.; De Pinna, E.; et al. Prospective use of whole genome sequencing (WGS) detected a multi-country outbreak of Salmonella Enteritidis. Epidemiol. Infect. 2017, 145, 289–298. [Google Scholar] [CrossRef]
- Eggs Recall for Salmonella Enteritidis. Available online: http://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=3524 (accessed on 22 April 2020).
- Augère-Granier, M.L. European Parliament. The EU Poultry Meat and Egg Sector: Main Features, Challenges and Prospects: In-depth Analysis; Publications Office of the European Union: Brussels, Belgium, 2019. [Google Scholar]
- EFSA BIOHAZ Panel (EFSA Panel on Biological Hazards); Koutsoumanis, K.; Allende, A.; Alvarez-Ordóñez, A.; Bolton, D.; Bover-Cid, S.; Chemaly, M.; De Cesare, A.; Herman, L.; Hilbert, F.; et al. Salmonella control in poultry flocks and its public health impact. EFSA J. 2019, 17, e05596. [Google Scholar] [CrossRef]
- Pijnacker, R.; Dallman, T.J.; Tijsma, A.S.L.; Hawkins, G.; Larkin, L.; Kotila, S.M.; Amore, G.; Amato, E.; Suzuki, P.M.; Denayer, S.; et al. An international outbreak of Salmonella enterica serotype Enteritidis linked to eggs from Poland: A microbiological and epidemiological study. Lancet Infect. Dis. 2019, 19, 778–786. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control, European Food Safety Authority. Multi-country outbreak of Salmonella Agona infections possibly linked to ready-to-eat food. EFSA Supporting Publ. 2018, 15, 1465E. [Google Scholar] [CrossRef]
- Pearce, M.E.; Alikhan, N.-F.; Dallman, T.J.; Zhou, Z.; Grant, K.; Maiden, M.C.J. Comparative analysis of core genome MLST and SNP typing within a European Salmonella serovar Enteritidis outbreak. Int. J. Food Microbiol. 2018, 274, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ewing, W.H. The nomenclature of Salmonella, its usage, and definitions for the three species. Can. J. Microbiol. 1972, 18, 1629–1637. [Google Scholar] [CrossRef] [PubMed]
- Guibourdenche, M.; Roggentin, P.; Mikoleit, M.; Fields, P.I.; Bockemuhl, J.; Grimont, P.A.; Weill, F.X. Supplement 2003–2007 (No. 47) to the White-Kauffmann-Le Minor scheme. Res. Microbiol. 2010, 161, 26–29. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, K.L.; Peters, T.M.; de Pinna, E.; Wain, J. Standardisation of multilocus variable-number tandem-repeat analysis (MLVA) for subtyping of Salmonella enterica serovar Enteritidis. Eurosurveillance 2011, 16, 19942. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, M.; Sousa, A.; Ramirez, M.; Francisco, A.P.; Carrico, J.A.; Vaz, C. PHYLOViZ 2.0: Providing scalable data integration and visualization for multiple phylogenetic inference methods. Bioinformatics (Oxford, England) 2017, 33, 128–129. [Google Scholar] [CrossRef] [PubMed]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics (Oxford, England) 2014, 30, 2114–2120. [Google Scholar] [CrossRef]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A.D.; et al. SPAdes: A new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. J. Comput. Mol. Cell Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef]
- Zhou, Z. The EnteroBase user’s guide, with case studies on Salmonella transmissions, Yersinia pestis phylogeny, and Escherichia core genomic diversity. Genome Res. 2020, 30, 138–152. [Google Scholar] [CrossRef]
- Alikhan, N.F.; Zhou, Z.; Sergeant, M.J. A genomic overview of the population structure of Salmonella. PLoS Genet. 2018, 14, e1007261. [Google Scholar] [CrossRef]
- Zhou, Z.; Alikhan, N.F. GrapeTree: Visualization of core genomic relationships among 100,000 bacterial pathogens. Genome Res. 2018, 28, 1395–1404. [Google Scholar] [CrossRef] [PubMed]
- Dallman, T.; Ashton, P.; Schafer, U.; Jironkin, A.; Painset, A.; Shaaban, S.; Hartman, H.; Myers, R.; Underwood, A.; Jenkins, C.; et al. SnapperDB: A database solution for routine sequencing analysis of bacterial isolates. Bioinformatics (Oxford, England) 2018, 34, 3028–3029. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Durbin, R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics (Oxford, England) 2010, 26, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Van der Auwera, G.A.; Carneiro, M.O.; Hartl, C.; Poplin, R.; Del Angel, G.; Levy-Moonshine, A.; Jordan, T.; Shakir, K.; Roazen, D.; Thibault, J.; et al. From FastQ data to high confidence variant calls: The Genome Analysis Toolkit best practices pipeline. Curr. Protoc. Bioinform. 2013, 43. [Google Scholar] [CrossRef]
| Sample ID | Isolation Source | Farm Name | MLVA | cgMLST Profile | cgMLST Cluster | SNP Address |
|---|---|---|---|---|---|---|
| 2018-AZ-4484-1-4 | Chicken | Farm A | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 |
| 2018-AZ-4706-1-2 | Chicken | Farm C | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.8 |
| 2018-AZ-4766-1-2 | Chicken | Farm A | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 |
| 2018-AZ-4767-1-2 | Chicken | Farm A | 2-10-7-3-2 | 3078 | 2.2.2.2.2.2.2 | |
| 2018-AZ-5011-1-3 | Chicken | Farm A | 2-10-7-3-2 | 3071 | Cluster 2 | 2.2.2.2.2.2.34 |
| 2018-AZ-5621-1-12 | Farm environment | Farm C | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.24 |
| 2018-AZ-5621-1-13 | Farm environment | Farm C | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.23 |
| 2018-AZ-5715-1-3 | Chicken | Farm E | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 |
| 2018-AZ-5718-1-2 | Chicken | Farm E | 1-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.9 |
| 2018-AZ-5718-2-2 | Farm environment | Farm E | 1-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.9 |
| 2018-AZ-6087-1-21 | Chicken | Farm D | 2-11-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.25 |
| 2018-AZ-6266-1-2 | Chicken | Farm C | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 |
| 2018-AZ-7226-1-2 | Chicken | Farm E | 1-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.51 |
| 2018-CB-3223-1-7 | Tiramisù | 2-9-7-3-2 | 3071 | Cluster 2 | 2.7.7.20.20.20.20 | |
| 2018-CB-3513-1-11 | Farm environment | Farm B | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 |
| 2018-CB-3513-1-16 | Farm environment | Farm B | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 |
| 2018-PE-6339-1-11 | Chicken | Farm A | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 |
| 2018-TE-12516-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.66 | |
| 2018-TE-12881-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-14038-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.49 | |
| 2018-TE-15229-1-1 | Chicken | Farm A | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 |
| 2018-TE-16067-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.39 | |
| 2018-TE-16075-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-17020-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-17030-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-17605-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.42 | |
| 2018-TE-19012-1-1 | Farm environment | Farm A | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.31 |
| 2018-TE-19126-1-1 | Human | 2-11-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.16 | |
| 2018-TE-19129-1-1 | Human | 2-11-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.16 | |
| 2018-TE-19130-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-19418-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-20273-1-2 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.45 | |
| 2018-TE-20299-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-20303-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.17 | |
| 2018-TE-20304-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.8 | |
| 2018-TE-20305-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-22807-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.42 | |
| 2018-TE-24761-1-10 | Human | 2-11-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.59 | |
| 2018-TE-24761-1-11 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.45 | |
| 2018-TE-24761-1-13 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.45 | |
| 2018-TE-24761-1-3 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-24761-1-4 | Human | 2-11-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.19 | |
| 2018-TE-24761-1-5 | Human | 2-11-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.11 | |
| 2018-TE-24761-1-9 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.30 | |
| 2018-TE-26653-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-26653-1-2 | Human | 2-11-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.11 | |
| 2018-TE-26653-1-3 | Human | 2-11-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.11 | |
| 2018-TE-26653-1-6 | Human | 2-11-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.11 | |
| 2018-TE-26685-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.26 | |
| 2018-TE-26685-1-2 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.26 | |
| 2018-TE-26685-1-3 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.26 | |
| 2018-TE-26685-1-4 | Human | 2-9-7-3-2 | 3071 | Cluster 2 | 2.7.7.20.20.20.20 | |
| 2018-TE-26685-1-5 | Human | 2-9-7-3-2 | 3071 | Cluster 2 | 2.7.7.20.20.20.20 | |
| 2018-TE-26685-1-6 | Human | 2-9-7-3-2 | 3071 | Cluster 2 | 2.7.7.20.20.20.20 | |
| 2018-TE-26685-1-7 | Human | 2-9-7-3-2 | 3071 | Cluster 2 | 2.7.7.20.20.20.20 | |
| 2018-TE-5787-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.57 | |
| 2018-TE-5788-1-1 | Human | 2-11-7-3-2 | 1915 | 2.7.7.28.28.28.28 | ||
| 2018-TE-7355-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.2 | |
| 2018-TE-8898-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.67 | |
| 2018-TE-8904-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.10 | |
| 2018-TE-9213-1-1 | Human | 2-10-7-3-2 | 1915 | Cluster 1 | 2.2.2.2.2.2.6 | |
| ERR2173854 | Chicken | 2-10-7-3-2 | 3077 | 2.7.7.7.7.7.7 | ||
| SRR3285443 | Human | 2-9-7-3-2 | 384 | 2.7.15.15.15.15.15 | ||
| SRR4063700 | Human | 2-9-7-3-2 | 387 | Cluster 2 | 2.7.7.20.52.52.52 | |
| SRR4063739 | Human | 2-10-8-3-2 | 546 | 2.7.7.7.21.21.21 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Marcantonio, L.; Janowicz, A.; Zilli, K.; Romantini, R.; Bilei, S.; Paganico, D.; Persiani, T.; Di Donato, G.; Di Giannatale, E. Genomic Comparison of Salmonella Enteritidis Strains Isolated from Laying Hens and Humans in the Abruzzi Region during 2018. Pathogens 2020, 9, 349. https://doi.org/10.3390/pathogens9050349
Di Marcantonio L, Janowicz A, Zilli K, Romantini R, Bilei S, Paganico D, Persiani T, Di Donato G, Di Giannatale E. Genomic Comparison of Salmonella Enteritidis Strains Isolated from Laying Hens and Humans in the Abruzzi Region during 2018. Pathogens. 2020; 9(5):349. https://doi.org/10.3390/pathogens9050349
Chicago/Turabian StyleDi Marcantonio, Lisa, Anna Janowicz, Katiuscia Zilli, Romina Romantini, Stefano Bilei, Daniela Paganico, Tiziana Persiani, Guido Di Donato, and Elisabetta Di Giannatale. 2020. "Genomic Comparison of Salmonella Enteritidis Strains Isolated from Laying Hens and Humans in the Abruzzi Region during 2018" Pathogens 9, no. 5: 349. https://doi.org/10.3390/pathogens9050349
APA StyleDi Marcantonio, L., Janowicz, A., Zilli, K., Romantini, R., Bilei, S., Paganico, D., Persiani, T., Di Donato, G., & Di Giannatale, E. (2020). Genomic Comparison of Salmonella Enteritidis Strains Isolated from Laying Hens and Humans in the Abruzzi Region during 2018. Pathogens, 9(5), 349. https://doi.org/10.3390/pathogens9050349





