Antimicrobial Resistance and Molecular Epidemiology of Corynebacterium striatum Isolated in a Tertiary Hospital in Turkey
Abstract
1. Introduction
2. Results
2.1. Demographic and Clinical Characteristics of Patients
2.2. Antibiotic Resistance Profiles of Isolates
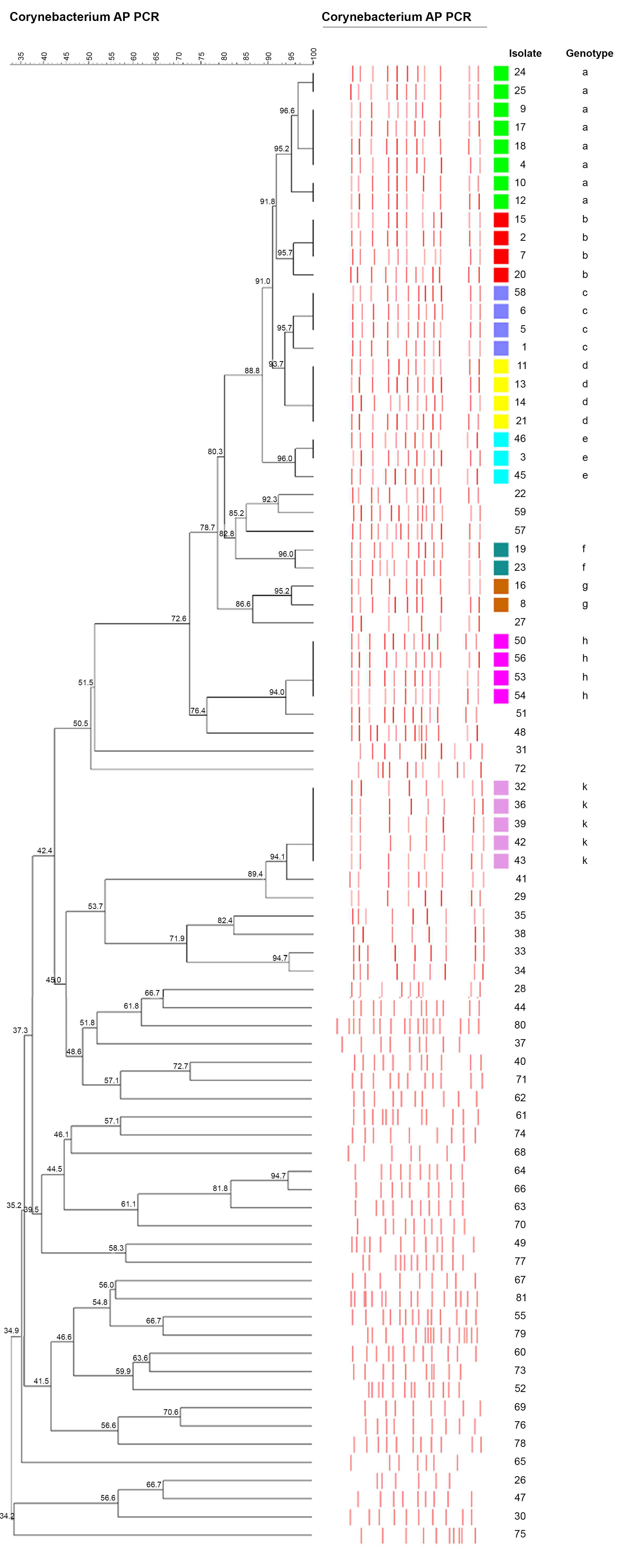
2.3. AP-PCR Results
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Isolation and Identification of C. striatum Strains
4.3. Antibiotic Susceptibility Testing
4.4. Determination of the Clonal Relationship among C. striatum Strains
4.5. Statistical Analysis
4.6. Ethical Approval
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kim, R.; Reboli, A.C. Other Coryneform Bacteria and Rhodococci. In Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 8th ed.; Bennet, J.E., Dolin, R., Blaser, M.J., Eds.; Elsevier Inc.: Philadelphia, PA, USA, 2015; Volume 2, pp. 2373–2382. [Google Scholar]
- Funke, G.; Bernard, K.A. Coryneform Gram-Positive Rods. In Manual of Clinical Microbiology, 11th ed.; Jorgensen, J.H., Pfaller, M.A., Carroll, K.C., Funke, G., Landry, M.L., Richter, S.S., Warnock, D.W., Eds.; American Society for Microbiology Press: Washington, DC, USA, 2015; Volume 1, pp. 474–503. [Google Scholar]
- Nhan, T.X.; Parienti, J.J.; Badiou, G.; Leclercq, R.; Cattoir, V. Microbiological investigation and clinical significance of Corynebacterium spp. in respiratory specimens. Diagn. Microbiol. Infect. Dis. 2012, 74, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Bernard, K. The genus Corynebacterium and other medically relevant coryneform-like bacteria. J. Clin. Microbiol. 2012, 50, 3152–3158. [Google Scholar] [CrossRef] [PubMed]
- Hahn, W.O.; Werth, B.J.; Butler-Wu, S.M.; Rakita, R.M. Multidrug-resistant Corynebacterium striatum associated with increased use of parenteral antimicrobial drugs. Emerg. Infect. Dis. 2016, 22, 1908–1914. [Google Scholar] [CrossRef] [PubMed]
- Bowstead, T.T.; Santiago, S.M. Pleuropulmonary infection due to Corynebacterium striatum. Br. J. Dis. Chest 1980, 74, 198–200. [Google Scholar] [CrossRef]
- Leonard, R.B.; Nowowiejski, D.J.; Warren, J.J.; Finn, D.J.; Coyle, M.B. Molecular evidence of person-to-person transmission of a pigmented strain of Corynebacterium striatum in intensive care units. J. Clin. Microbiol. 1994, 32, 164–169. [Google Scholar] [CrossRef]
- Kammoun, M.M.; Regaieg, K.; Bahloul, M.; Ammar, R.; Bouaziz, M. Corynebacterium striatum meningitis. Med. Mal. Infect. 2016, 46, 454–456. [Google Scholar] [CrossRef]
- Ramos, J.N.; Souza, C.; Faria, Y.V.; da Silva, E.C.; Veras, J.F.C.; Baio, P.V.P.; Seabra, S.H.; de Oliveira Moreira, L.; Hirata Júnior, R.; Mattos-Guaraldi, A.L.; et al. Bloodstream and catheter-related infections due to different clones of multidrug-resistant and biofilm producer Corynebacterium striatum. BMC Infect. Dis. 2019, 19, 672. [Google Scholar] [CrossRef]
- Lee, J.Y.; Lee, S.H.; Kim, W.H. Three-valve Endocarditis Caused by Corynebacterium striatum. Korean Circ. J. 2018, 48, 861–862. [Google Scholar] [CrossRef]
- Verma, R.; Kravitz, G. Corynebacterium striatum empyema and osteomyelitis in a patient with advanced rheumatoid arthritis. BMJ Case Rep. 2016. [Google Scholar] [CrossRef]
- Renom, F.; Gomila, M.; Garau, M.; Gallegos, M.D.C.; Guerrero, D.; Lalucat, J.; Soriano, J.B. Respiratory infection by Corynebacterium striatum: Epidemiological and clinical determinants. New Microbes. New Infect. 2014, 2, 106–114. [Google Scholar] [CrossRef]
- Verroken, A.; Bauraing, C.; Deplano, A.; Bogaerts, P.; Huang, D.; Wauters, G.; Glupczynski, Y. Epidemiological investigation of a nosocomial outbreak of multidrug-resistant Corynebacterium striatum at one Belgian university hospital. Clin. Microbiol. Infect. 2014, 20, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Qin, L.; Sakai, Y.; Bao, R.; Xie, H.; Masunaga, K.; Miura, M.; Hashimoto, K.; Tanamachi, C.; Hu, B.; Watanabe, H. Characteristics of multidrug-resistant Corynebacterium spp. isolated from blood cultures from hospitalized patients in Japan. Jpn. J. Infect. Dis. 2017, 70, 152–157. [Google Scholar] [CrossRef] [PubMed]
- McMullen, A.R.; Anderson, N.; Wallace, M.A.; Shupe, A.; Burnham, C.A. When good bugs go bad: Epidemiology and antimicrobial resistance profiles of Corynebacterium striatum, an emerging multidrug-resistant, opportunistic pathogen. Antimicrob. Agents Chemother. 2017, 61, e01111–e01117. [Google Scholar] [CrossRef] [PubMed]
- Asgin, N. In-vitro Antibiotic Resistance Profile of Corynebacterium striatum Strains Isolated from Clinical Samples. ANKEM Derg. 2019, 33, 102–107. [Google Scholar]
- Tran, T.T.; Jaijakul, S.; Lewis, C.T.; Diaz, L.; Panesso, D.; Kaplan, H.B.; Murray, B.E.; Wanger, A.; Arias, C.A. Native valve endocarditis caused by Corynebacterium striatum with heterogeneous high-level daptomycin resistance: Collateral damage from daptomycin therapy? Antimicrob. Agents Chemother. 2012, 56, 3461–3464. [Google Scholar] [CrossRef] [PubMed]
- Ajmal, S.; Saleh, O.A.; Beam, E. Development of high-grade daptomycin resistance in a patient being treated for Corynebacterium striatum infection. Antimicrob. Agents Chemother. 2017, 61, e00705–e00717. [Google Scholar] [CrossRef]
- Wang, Y.; Du, X.; Cui, J.; Wang, K.; Zhang, L.; Han, Y. Rapid transmission of multidrug-resistant Corynebacterium striatum among susceptible patients in a tertiary hospital in China. J. Infect. Dev. Ctries. 2016, 10, 1299–1305. [Google Scholar] [CrossRef]
- Suh, J.W.; Ju, Y.; Lee, C.K.; Sohn, J.W.; Kim, M.J.; Yoon, Y.K. Molecular epidemiology and clinical significance of Corynebacterium striatum isolated from clinical specimens. Infect. Drug Resist. 2019, 4, 161–171. [Google Scholar] [CrossRef]
- Martínez-Martínez, L.; Pascual, A.; Bernard, K.; Suárez, A.I. Antimicrobial susceptibility pattern of Corynebacterium striatum. Antimicrob. Agents Chemother. 1996, 40, 2671–2672. [Google Scholar] [CrossRef]
- Martínez-Martínez, L.; Suárez, A.I.; Winstanley, J.; Ortega, M.C.; Bernard, K. Phenotypic characteristics of 31 strains of Corynebacterium striatum isolated from clinical samples. J. Clin. Microbiol. 1995, 33, 2458–2461. [Google Scholar] [CrossRef]
- Alibi, S.; Ferjani, A.; Boukadida, J.; Cano, M.E.; Fernández-Martínez, M.; Martínez-Martínez, L.; Navas, J. Occurrence of Corynebacterium striatum as an emerging antibiotic-resistant nosocomial pathogen in a Tunisian hospital. Sci. Rep. 2017, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhou, H.; Chen, D.; Du, P.; Lan, R.; Qiu, X.; Hou, X.; Liu, Z.; Sun, L.; Xu, S.; et al. Whole-Genome Sequencing Reveals a Prolonged and Persistent Intrahospital Transmission of Corynebacterium striatum, an Emerging Multidrug-Resistant Pathogen. J. Clin. Microbiol. 2019, 57, e00683-19. [Google Scholar] [CrossRef] [PubMed]
- Shariff, M.; Aditi, A.; Beri, K. Corynebacterium striatum: An emerging respiratory pathogen. J. Infect. Dev. Ctries. 2018, 12, 581–586. [Google Scholar] [CrossRef]
- Olender, A. Mechanisms of Antibiotic Resistance in Corynebacterium spp. Causing Infections in People. In Antibiotic Resistant Bacteria. A Continuous Challenge in the New Millennium, 1st ed.; Pana, M., Ed.; In Tech Open: London, UK, 2012; Volume 1, pp. 387–402. [Google Scholar]
- Mumcuoglu, I.; Hazırolan, G.; Kurşun, Ş.; Aksu, N. Evaluation of the Corynebacterium striatum isolated with increasing frequency in one of the training and research hospital. Turk Hij. Den. Biyo. Derg. 2015, 72, 281–288. [Google Scholar] [CrossRef]
- Neemuchwala, A.; Soares, D.; Ravirajan, V.; Marchand-Austin, A.; Kus, J.V.; Patel, S.N. In vitro antibiotic susceptibility pattern of non-diphtheriae Corynebacterium isolates in Ontario, Canada, from 2011 to 2016. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef]
- Ortiz-Pérez, A.; Martín-De-Hijas, N.Z.; Esteban, J.; Fernández-Natal, M.I.; García-Cía, J.I.; Fernández-Roblas, R. High frequency of macrolide resistance mechanisms in clinical isolates of Corynebacterium species. Microb. Drug Resist. 2010, 16, 273–277. [Google Scholar] [CrossRef]
- Barberis, C.M.; Sandoval, E.; Rodriguez, C.H.; Ramírez, M.S.; Famiglietti, A.; Almuzara, M.; Vay, C. Comparison between disk diffusion and agar dilution methods to determine in vitro susceptibility of Corynebacterium spp. clinical isolates and update of their susceptibility. J. Glob. Antimicrob. Resist. 2018, 14, 246–252. [Google Scholar] [CrossRef]
- Campanila, F.; Carretto, E.; Barbarini, D.; Grigis, A.; Falcone, M.; Goglio, A.; Venditti, M.; Stefani, S. Clonal multidrug-resistant Corynebacterium striatum strains, Italy. Emerg. Infect. Dis. 2009, 15, 75–78. [Google Scholar] [CrossRef]
- Fernandez-Cuenca, F. Applications of PCR techniques for molecular epidemiology of infectious diseases. Enferm. Infecc. Microbiol. Clin. 2004, 22, 355–360. [Google Scholar]
- Baio, P.V.P.; Mota, H.F.; Freitas, A.D.; Gomes, D.L.; Ramos, J.N.; Sant’Anna, L.O.; Souza, M.C.; Camello, T.C.; Hirata, J.R.; Vieira, V.V.; et al. Clonal multidrug-resistant Corynebacterium striatum within a nosocomial environment Rio de Janeiro, Brazil. Mem. Inst. Oswaldo Cruz. 2013, 108, 23–29. [Google Scholar] [CrossRef]
- Masroor, N.; Doll, M.; Stevens, M.; Bearman, G. Approaches to hand hygiene monitoring: From low to high technology approaches. Int. J. Infect. Dis. 2017, 65, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Godbout, E.J.; Masroor, N.; Doll, M.; Edmond, M.B.; Bearman, G.; Stevens, M.P. Bare below the elbows in an academic medical center. Am. J. Infect. Control. 2019, 4, 1030–1031. [Google Scholar] [CrossRef] [PubMed]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 7.1, 2017. Available online: http://www.eucast.org/ast_of_bacteria/previous_versions_of_documents/ (accessed on 10 April 2019).
- Ayan, M.; Kuzucu, C.; Durmaz, R.; Aktas, E.; Cizmeci, Z. Analysis of three outbreaks due to Klebsiella species in a neonatal intensive care unit. Infect. Control Hosp. Epidemiol. 2003, 24, 495–500. [Google Scholar] [CrossRef] [PubMed]
| Data | Number (%) |
|---|---|
| Age (years) | |
| 40–59 | 12 (14.8) |
| 60–79 | 42 (51.9) |
| ≥80 | 27 (33.3) |
| Gender | |
| Female | 39 (48.1) |
| Male | 42 (51.9) |
| Hospital Unit | |
| Intensive Care Unit (ICU) | 68 (84.0) |
| Surgical ICU | 23 (28.4) |
| İnternal medicine ICU | 22 (27.2) |
| Reanimation ICU | 16 (19.8) |
| Coronary ICU | 7 (8.6) |
| Wards | 13 (16.0) |
| General surgery | 5 (6.2) |
| Palliative care | 4 (4.9) |
| Respiratory | 4 (4.9) |
| Specimens | |
| Blood | 35 (43.2) |
| Endotracheal aspirate | 24 (29.6) |
| Wound | 11 (13.6) |
| Sputum | 7 (8.7) |
| Bronchoalveolar lavage fluid | 4 (4.9) |
| Underlying Diseases | |
| *COPD | 18 (22.2) |
| Heart failure/ attack | 14 (17.3) |
| Cerebrovascular disease | 12 (14.8) |
| Cardiac arrest | 9 (11.1) |
| Renal failure | 9 (11.1) |
| Acute abdomen with ileus | 8 (9.9) |
| Surgical site infection | 7 (8.6) |
| Sepsis | 5 (6.2) |
| Gastrointestinal hemorrhage | 4 (4.9) |
| Traumatic pneumothorax | 4 (4.9) |
| Femur fracture | 3 (3.7) |
| Hepatobiliary diseases | 3 (3.7) |
| Total (n = 81) | ICUs (n = 68) | Wards (n = 13) | P-value | |
|---|---|---|---|---|
| Antibiotic | n (%) | n (%) | n (%) | |
| Erythromycin | 64 (79) | 55 (80.8) | 9 (69.2) | 0.363 |
| Clindamycin | 71 (87.7) | 59 (86.6) | 12 (92.3) | 0.578 |
| Gentamicin | 28 (34.6) | 23 (33.8) | 5 (38.5) | 0.747 |
| Ciprofloxacin | 81 (100) | 68 (100) | 13 (100) | Na |
| Penicillin | 81 (100) | 68 (100) | 13 (100) | Na |
| Cefotaxime | 81 (100) | 68 (100) | 13 (100) | Na |
| Ciprofloxacin | 81 (100) | 68 (100) | 13 (100) | Na |
| Tetracycline | 81 (100) | 68 (100) | 13 (100) | Na |
| Vancomycin | 0 (0) | 0 (0) | 0 (0) | Na |
| Linezolid | 0 (0) | 0 (0) | 0 (0) | Na |
| Strain no | Department | Source | Isolation Date | Antibiotic Susceptibility | Genotype |
|---|---|---|---|---|---|
| 4 | surgical ICU | EA | 13.4.2015 | Va, Lzd | a |
| 9 | internal medicine ICU | EA | 18.4.2015 | Va, Lzd, Gn, E | a |
| 10 | reanimation ICU | EA | 8.2.2016 | Va, Lzd | a |
| 12 | surgical ICU | Blood | 2.10.2015 | Va, Lzd | a |
| 17 | internal medicine ICU | EA | 4.10.2015 | Va, Lzd, Gn, E, Da | a |
| 18 | palliative care unit | wound | 27.12.2015 | Va, Lzd, E | a |
| 24 | coronary ICU | sputum | 21.11.2015 | Va, Lzd | a |
| 25 | surgical ICU | wound | 7.2.2015 | Va, Lzd | a |
| 2 | surgical ICU | Blood | 8.4.2015 | Va, Lzd, Gn | b |
| 7 | internal medicine ICU | EA | 19.10.2015 | Va, Lzd, Gn | b |
| 15 | reanimation ICU | EA | 10.1.2015 | Va, Lzd, Gn | b |
| 20 | palliative care unit | sputum | 13.12.2015 | Va, Lzd, Gn | b |
| 58 | internal medicine ICU | BLF | 11.5.2015 | Va, Lzd, Gn | c |
| 1 | surgical ICU | Blood | 30.1.2015 | Va, Lzd, Gn | c |
| 5 | reanimation ICU | EA | 7.2.2015 | Va, Lzd, Gn | c |
| 6 | internal medicine ICU | Blood | 29.5.2015 | Va, Lzd, E | c |
| 11 | internal medicine ICU | Blood | 5.5.2015 | Va, Lzd, Gn | d |
| 13 | surgical ICU | EA | 23.10.2015 | Va, Lzd, Gn | d |
| 14 | internal medicine ICU | BLF | 26.8.2015 | Va, Lzd | d |
| 21 | surgical ICU | EA | 14.1.2016 | Va, Lzd | d |
| 3 | internal medicine ICU | EA | 4.1.2016 | Va, Lzd | e |
| 45 | internal medicine ICU | sputum | 6.11.2015 | Va, Lzd | e |
| 46 | internal medicine ICU | EA | 4.12.2015 | Va, Lzd | e |
| 19 | surgical ICU | wound | 17.4.2015 | Va, Lzd, Gn | f |
| 23 | surgical ICU | sputum | 4.2.2015 | Va, Lzd, Gn | f |
| 8 | internal medicine ICU | BLF | 3.4.2015 | Va, Lzd, Gn | g |
| 16 | internal medicine ICU | Blood | 24.3.2015 | Va, Lzd, Gn | g |
| 50 | surgical ICU | Blood | 24.7.2015 | Va, Lzd, Gn | h |
| 53 | surgical ICU | Blood | 1.4.2015 | Va, Lzd, Gn | h |
| 54 | coronary ICU | EA | 8.1.2015 | Va, Lzd, Gn, E, Da | h |
| 56 | coronary ICU | sputum | 24.2.2015 | Va, Lzd, Gn | h |
| 32 | surgical ICU | EA | 21.12.2015 | Va, Lzd | k |
| 36 | reanimation ICU | Blood | 23.5.2015 | Va, Lzd, Gn, E, Da | k |
| 39 | reanimation ICU | EA | 4.7.2015 | Va, Lzd | k |
| 42 | surgical ICU | EA | 20.5.2015 | Va, Lzd, Gn | k |
| 43 | reanimation ICU | BLF | 23.11.2015 | Va, Lzd, Gn, E | k |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asgin, N.; Otlu, B. Antimicrobial Resistance and Molecular Epidemiology of Corynebacterium striatum Isolated in a Tertiary Hospital in Turkey. Pathogens 2020, 9, 136. https://doi.org/10.3390/pathogens9020136
Asgin N, Otlu B. Antimicrobial Resistance and Molecular Epidemiology of Corynebacterium striatum Isolated in a Tertiary Hospital in Turkey. Pathogens. 2020; 9(2):136. https://doi.org/10.3390/pathogens9020136
Chicago/Turabian StyleAsgin, Nergis, and Baris Otlu. 2020. "Antimicrobial Resistance and Molecular Epidemiology of Corynebacterium striatum Isolated in a Tertiary Hospital in Turkey" Pathogens 9, no. 2: 136. https://doi.org/10.3390/pathogens9020136
APA StyleAsgin, N., & Otlu, B. (2020). Antimicrobial Resistance and Molecular Epidemiology of Corynebacterium striatum Isolated in a Tertiary Hospital in Turkey. Pathogens, 9(2), 136. https://doi.org/10.3390/pathogens9020136




