High Prevalence of Strongyloides among South Asian Migrants in Primary Care―Associations with Eosinophilia and Gastrointestinal Symptoms
Abstract
1. Introduction
2. Materials and Methods
- Patients who attended for non-specific gastrointestinal symptoms (with which they had presented at least twice over a six-month period and without diagnosis or treatment).
- Patients whose most recent full blood count (within last three months) demonstrated eosinophilia (defined as equal to or greater than 0.5 cells × 109/L).
- Patients attending the in-practice phlebotomy service for a full blood count, for any reason. These patients formed the control group.
3. Statistical Analysis
4. Results
4.1. Baseline Results
4.2. Analyses of Associations with Strongyloides Diagnosis
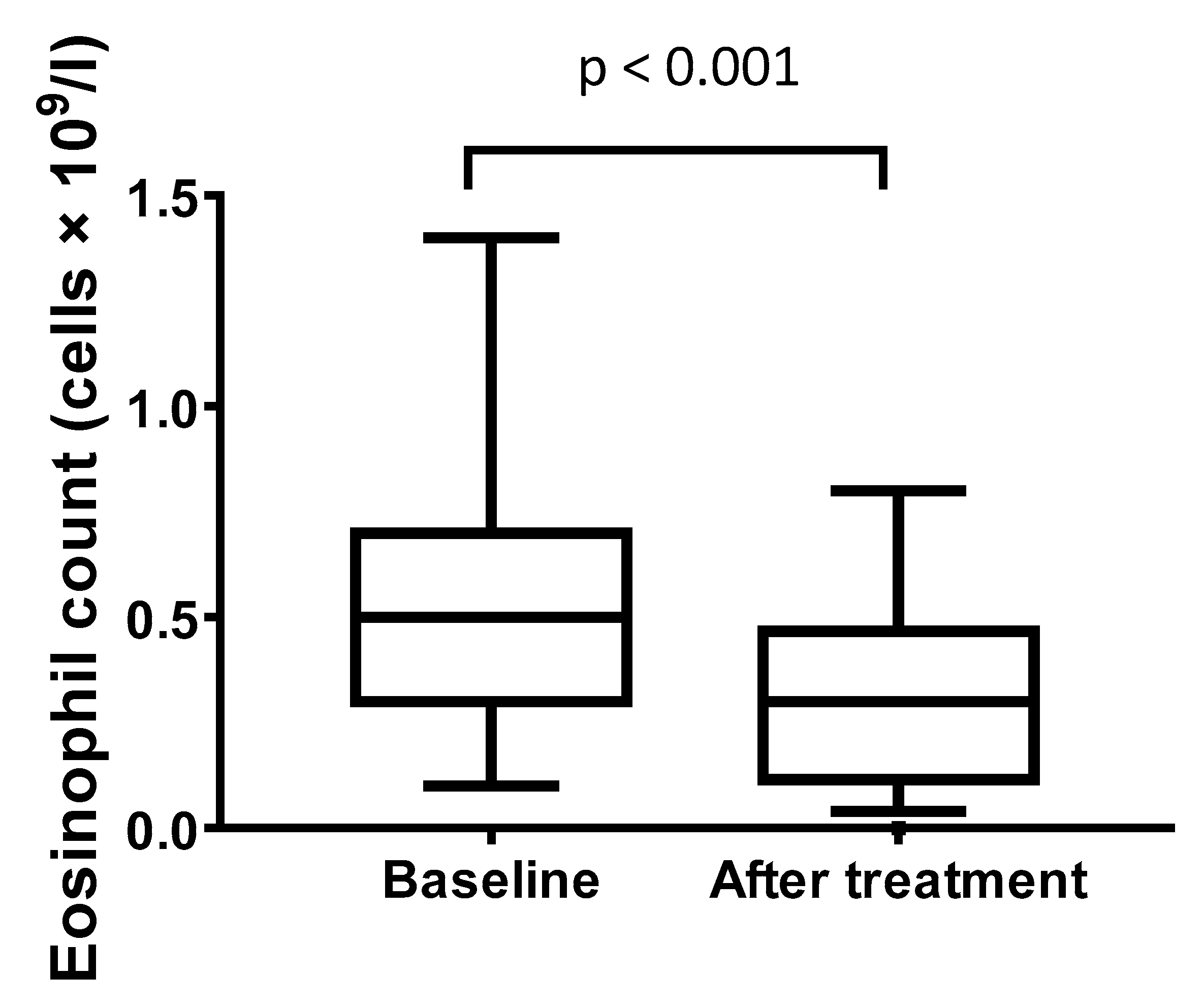
4.3. Treatment and Follow-up
4.4. Associations between Treatment and GI Symptoms
5. Discussion
Author Contributions
Funding
Acknowledgements
Conflicts of Interest
References
- Bisoffi, Z.; Buonfrate, D.; Montresor, A.; Requena-Méndez, A.; Muñoz, J.; Krolewiecki, A.J.; Gotuzzo, E.; Mena, M.A.; Chiodini, P.L.; Anselmi, M.; et al. Strongyloides stercoralis: A plea for action. PLoS Negl. Trop. Dis. 2013, 7, e2214. [Google Scholar] [CrossRef]
- Asundi, A.; Beliavsky, A.; Liu, X.J.; Akaberi, A.; Schwarzer, G.; Bisoffi, Z.; Requena-Méndez, A.; Shrier, I.; Greenaway, C. Prevalence of strongyloidiasis and schistosomiasis among migrants: A systematic review and meta-analysis. Lancet Glob. Health 2019, 7, e236–e248. [Google Scholar] [CrossRef]
- Buonfrate, D.; Angheben, A.; Gobbi, F.; Muñoz, J.; Requena-Mendez, A.; Gotuzzo, E.; Mena, M.A.; Bisoffi, Z. Imported strongyloidiasis: Epidemiology, presentations, and treatment. Curr. Infect. Dis. Rep. 2012, 14, 256–262. [Google Scholar] [CrossRef]
- Montes, M.; Sawhney, C.; Barros, N. Strongyloides stercoralis: There but not seen. Curr. Opin. Infect. Dis. 2010, 23, 500–504. [Google Scholar] [CrossRef]
- Viney, M.E.; Lok, J.B. Strongyloides spp. WormBook Online Rev. C Elegans Biol. 2007, pp. 1–15. Available online: https://europepmc.org/article/PMC/3091011 (accessed on 6 February 2020).
- Gill, G.V.; Welch, E.; Bailey, J.W.; Bell, D.R.; Beeching, N.J. Chronic Strongyloides stercoralis infection in former British Far East prisoners of war. QJM Mon. J. Assoc. Physicians 2004, 97, 789–795. [Google Scholar] [CrossRef]
- Buonfrate, D.; Requena-Mendez, A.; Angheben, A.; Muñoz, J.; Gobbi, F.; Van Den Ende, J.; Bisoffi, Z. Severe strongyloidiasis: A systematic review of case reports. BMC Infect. Dis. 2013, 13, 78. [Google Scholar] [CrossRef]
- Requena-Méndez, A.; Buonfrate, D.; Gomez-Junyent, J.; Zammarchi, L.; Bisoffi, Z.; Muñoz, J. Evidence-Based Guidelines for Screening and Management of Strongyloidiasis in Non-Endemic Countries. Am. J. Trop. Med. Hyg. 2017, 97, 645–652. [Google Scholar] [CrossRef]
- Muennig, D.P. The cost-effectiveness of ivermectin vs. albendazole in the presumptive treatment of strongyloidiasis in immigrants to the United States. Epidemiol. Infect. 2005, 132, 1055–1063. [Google Scholar] [CrossRef]
- Maskery, B.; Coleman, M.S.; Weinberg, M.; Zhou, W.; Rotz, L.; Klosovsky, A.; Cantey, P.T.; Fox, L.M.; Cetron, M.S.; Stauffer, W.M. Economic Analysis of the Impact of Overseas and Domestic Treatment and Screening Options for Intestinal Helminth Infection among US-Bound Refugees from Asia. PLoS Negl. Trop. Dis. 2016, 10, e0004910. [Google Scholar] [CrossRef]
- González, A.; Gallo, M.; Valls, M.E.; Muñoz, J.; Puyol, L.; Pinazo, M.J.; Mas, J.; Gascon, J. Clinical and epidemiological features of 33 imported Strongyloides stercoralis infections. Trans. R. Soc. Trop. Med. Hyg. 2010, 104, 613–616. [Google Scholar] [CrossRef]
- Smith, P.J.; Theis, B.; McCartney, S.; Brown, M. Republished research: Helminths: An unrecognised disease burden prevalent among migrants in the gastroenterology clinic. Postgrad. Med. J. 2012, 88, 28–33. [Google Scholar] [CrossRef]
- Wallis, E.M.; Fiks, A.G. Nonspecific abdominal pain in pediatric primary care: Evaluation and outcomes. Acad. Pediatr. 2015, 15, 333–339. [Google Scholar] [CrossRef]
- Sudarshi, S.; Stümpfle, R.; Armstrong, M.; Ellman, T.; Parton, S.; Krishnan, P.; Chiodini, P.L.; Whitty, C.J.M. Clinical presentation and diagnostic sensitivity of laboratory tests for Strongyloides stercoralis in travellers compared with immigrants in a non-endemic country. Trop. Med. Int. Health 2003, 8, 728–732. [Google Scholar] [CrossRef]
- Francis, C.Y.; Morris, J.; Whorwell, P.J. The irritable bowel severity scoring system: A simple method of monitoring irritable bowel syndrome and its progress. Aliment. Pharmacol. Ther. 1997, 11, 395–402. [Google Scholar] [CrossRef]
- Mahadeva, S.; Chan, W.-K.; Mohazmi, M.; Sujarita, R.; Goh, K.-L. Validation study of the Leeds Dyspepsia Questionnaire in a multi-ethnic Asian population. J. Gastroenterol. Hepatol. 2011, 26, 1669–1676. [Google Scholar] [CrossRef]
- Longstreth, G.F.; Thompson, W.G.; Chey, W.D.; Houghton, L.A.; Mearin, F.; Spiller, R.C. Functional Bowel Disorders. Gastroenterology 2006, 130, 1480–1491. [Google Scholar] [CrossRef]
- Tamarozzi, F.; Martello, E.; Giorli, G.; Fittipaldo, A.; Staffolani, S.; Montresor, A.; Bisoffi, Z.; Buonfrate, D. Morbidity Associated with Chronic Strongyloides stercoralis Infection: A Systematic Review and Meta-Analysis. Am. J. Trop. Med. Hyg. 2019, 100, 1305–1311. [Google Scholar] [CrossRef]
- Checkley, A.M.; Chiodini, P.L.; Dockrell, D.H.; Bates, I.; Thwaites, G.E.; Booth, H.L.; Brown, M.; Wright, S.G.; Grant, A.D.; Mabey, D.C.; et al. Eosinophilia in returning travellers and migrants from the tropics: UK recommendations for investigation and initial management. J. Infect. 2010, 60, 1–20. [Google Scholar] [CrossRef]
- Luvira, V.; Trakulhun, K.; Mungthin, M.; Naaglor, T.; Chantawat, N.; Pakdee, W.; Phiboonbanakit, D.; Dekumyoy, P. Comparative Diagnosis of Strongyloidiasis in Immunocompromised Patients. Am. J. Trop. Med. Hyg. 2016, 95, 401–404. [Google Scholar] [CrossRef]
- Schär, F.; Trostdorf, U.; Giardina, F.; Khieu, V.; Muth, S.; Marti, H.; Vounatsou, P.; Odermatt, P. Strongyloides stercoralis: Global Distribution and Risk Factors. PLoS Negl. Trop. Dis. 2013, 7, e2288. [Google Scholar] [CrossRef]
- McGuire, E.; Welch, C.; Melzer, M. Is Strongyloides seropositivity associated with diabetes mellitus? A retrospective case-control study in an East London NHS Trust. Trans. R. Soc. Trop. Med. Hyg. 2019, 113, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Spiller, R.; Aziz, Q.; Creed, F.; Emmanuel, A.; Houghton, L.; Hungin, P.; Jones, R.; Kumar, D.; Rubin, G.; Trudgill, N.; et al. Guidelines for the management of Irritable Bowel Syndrome. Gut 2007, 56, 1770–1798. [Google Scholar] [CrossRef] [PubMed]
- Ford, A.C.; Quigley, E.M.M.; Lacy, B.E.; Lembo, A.J.; Saito, Y.A.; Schiller, L.R.; Soffer, E.E.; Spiegel, B.M.R.; Moayyedi, P. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am. J. Gastroenterol. 2014, 109, 1547–1561. [Google Scholar] [CrossRef] [PubMed]
- Ming, D.K.; Armstrong, M.; Lowe, P.; Chiodini, P.L.; Doherty, J.F.; Whitty, C.J.M.; McGregor, A.C. Clinical and Diagnostic Features of 413 Patients Treated for Imported Strongyloidiasis at the Hospital for Tropical Diseases, London. Am. J. Trop. Med. Hyg. 2019, 101, 428–431. [Google Scholar] [CrossRef] [PubMed]
- De Kaminsky, R.G. Evaluation of three methods for laboratory diagnosis of Strongyloides stercoralis infection. J. Parasitol. 1993, 79, 277–280. [Google Scholar] [CrossRef] [PubMed]
- Change Institute. Communities and Local Government: London the Bangladeshi Muslim Community in England: Understanding Muslim Ethnic Communities; Communities and Local Government: London, UK, 2009; ISBN 978-1-4098-1273-9.
- Szczepura, A. Access to health care for ethnic minority populations. Postgrad. Med. J. 2005, 81, 141–147. [Google Scholar] [CrossRef]
- Buonfrate, D.; Salas-Coronas, J.; Muñoz, J.; Maruri, B.T.; Rodari, P.; Castelli, F.; Zammarchi, L.; Bianchi, L.; Gobbi, F.; Cabezas-Fernández, T.; et al. Multiple-dose versus single-dose ivermectin for Strongyloides stercoralis infection (Strong Treat 1 to 4): A multicentre, open-label, phase 3, randomised controlled superiority trial. Lancet Infect. Dis. 2019, 19, 1181–1190. [Google Scholar] [CrossRef]
- Agbata, E.N.; Morton, R.L.; Bisoffi, Z.; Bottieau, E.; Greenaway, C.; Biggs, B.-A.; Montero, N.; Tran, A.; Rowbotham, N.; Arevalo-Rodriguez, I.; et al. Effectiveness of Screening and Treatment Approaches for Schistosomiasis and Strongyloidiasis in Newly-Arrived Migrants from Endemic Countries in the EU/EEA: A Systematic Review. Int. J. Environ. Res. Public. Health 2019, 16, 11. [Google Scholar] [CrossRef]
| Control (Reference Cohort) (n = 120) | Eosinophilia Cohort (n = 223) * | p-Value | GI Cohort (n = 177) | p-Value | |
|---|---|---|---|---|---|
| Laboratory Parameters | |||||
| Strongyloides serology Negative Positive | 105 (87.5%) 15 (12.5%) | 148 (66.4%) 75 (33.6%) | OR (95% CI): 3.55 (1.93–6.52), p < 0.001 aOR (95% CI): 3.54 (1.88–6.67), p < 0.001 | 148 (83.6%) 29 (16.4%) | OR (95% CI): 1.37 (0.70–2.68), p = 0.36 aOR (95% CI): 1.46 (0.74–2.89), p = 0.27 |
| Median eosinophil count cells × 109/L (IQR) | 0.2 (0.1–0.3) | 0.6 (0.5–0.7) | <0.001 | 0.2 (0.1–0.4) | 0.008 |
| Median serology titre for patients with positive serology (IQR) | 1.2 (1.1–1.5) | 1.6 (1.2–3.0) | 0.03 | 1.3 (1.2–2.0) | NS |
| Sociodemographic Variables | |||||
| Median age in years (IQR) | 51 (42–60) | 47 (37–62) | NS | 47 (37–60) | NS |
| Male sex | 44 (36.7%) | 127 (57.0%) | 0.001 | 63 (35.8%) | NS |
| Bangladesh as country of birth | 107 (89.2%) | 193 (86.6%) | NS | 161 (91.0%) | NS |
| Median number of years living in UK (IQR) | 23 (14–32) | 26 (15–37) | NS | 23 (14–31) | NS |
| Median number of years since last travel to endemic area (IQR) | 2 (1–5) | 2 (1–5) | NS | 3 (1–6) | NS |
| Impact on Life | |||||
| Median quality of life impact score (IQR) Mean quality of life impact score | 0 (0–4) 10 | 0 (0–35) 19 | 0.001 | 36 (0–69) 39 | <0.001 |
| Median IBS score (IQR) | 10 (0–104) | 54 (0–160) | 0.002 | 188 (73–291) | <0.001 |
| Work missed No days missed Fewer than 30 days More than 30 days | 102 (85.0%) 4 (3.3%) 3 (2.5%) | 186 (83.4%) 28 (12.6%) 6 (2.7%) | 0.03 | 105 (59.3%) 40 (22.6%) 26 (14.7%) | <0.001 |
| Medical History | |||||
| History of GI investigations | 36 (30.0%) | 87 (39.0%) | NS | 106 (60.9%) | <0.001 |
| History of atopy | 45 (37.5%) | 100 (44.8%) | NS | 83 (48.5%) | NS |
| Strongyloides Negative (n = 388) | Strongyloides Positive (n = 115) | p-Value | |
|---|---|---|---|
| Characteristics | |||
| Male sex | 163 (42.3%) | 62 (53.9%) | 0.03 |
| Median age (IQR) | 48 (37–61) | 49 (42–59) | NS |
| Median eosinophil count (IQR) | 0.4 (0.2–0.5) | 0.5 (0.3–0.7) | <0.001 |
| Median number of years in the UK (IQR) | 24 (14–32) | 26 (15–37) | NS |
| Bangladesh heritage | 344 (88.7%) | 102 (88.7%) | NS |
| No work days missed | 294 (75.8%) | 90 (78.3%) | NS |
| Underlying immunosuppression | 1 (0.3%) | 1 (0.9%) | NS |
| Median impact on quality of life score | 0 (0–37) | 0 (0–54) | NS |
| Median IBS Score | 76 (0–200) | 70 (0–181) | NS |
| Symptoms | |||
| Abdominal Pain | 184 (47.4%) | 46 (40.0%) | |
| Distension | 145 (37.4%) | 53 (46.1%) | |
| Vomiting | 36 (9.3%) | 9 (7.8%) | |
| Indigestion | 172 (44.3%) | 48 (41.7%) | |
| Diarrhoea | 82 (21.1%) | 19 (16.5%) | |
| Constipation | 171 (44.1%) | 51 (44.4%) | |
| Flatulence | 162 (41.8%) | 38 (33.0%) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baker, E.C.; Ming, D.K.; Choudhury, Y.; Rahman, S.; Smith, P.J.; Muñoz, J.; Chiodini, P.L.; Griffiths, C.J.; Whitty, C.J.M.; Brown, M. High Prevalence of Strongyloides among South Asian Migrants in Primary Care―Associations with Eosinophilia and Gastrointestinal Symptoms. Pathogens 2020, 9, 103. https://doi.org/10.3390/pathogens9020103
Baker EC, Ming DK, Choudhury Y, Rahman S, Smith PJ, Muñoz J, Chiodini PL, Griffiths CJ, Whitty CJM, Brown M. High Prevalence of Strongyloides among South Asian Migrants in Primary Care―Associations with Eosinophilia and Gastrointestinal Symptoms. Pathogens. 2020; 9(2):103. https://doi.org/10.3390/pathogens9020103
Chicago/Turabian StyleBaker, Elinor Chloe, Damien K. Ming, Yasmin Choudhury, Shahedur Rahman, Philip J. Smith, Jose Muñoz, Peter L. Chiodini, Chris J. Griffiths, Christopher J. M. Whitty, and Michael Brown. 2020. "High Prevalence of Strongyloides among South Asian Migrants in Primary Care―Associations with Eosinophilia and Gastrointestinal Symptoms" Pathogens 9, no. 2: 103. https://doi.org/10.3390/pathogens9020103
APA StyleBaker, E. C., Ming, D. K., Choudhury, Y., Rahman, S., Smith, P. J., Muñoz, J., Chiodini, P. L., Griffiths, C. J., Whitty, C. J. M., & Brown, M. (2020). High Prevalence of Strongyloides among South Asian Migrants in Primary Care―Associations with Eosinophilia and Gastrointestinal Symptoms. Pathogens, 9(2), 103. https://doi.org/10.3390/pathogens9020103





