Autoantibody Profiling in Plasma of Dengue Virus–Infected Individuals
Abstract
:1. Introduction
2. Results
2.1. Characteristics of the Study Population
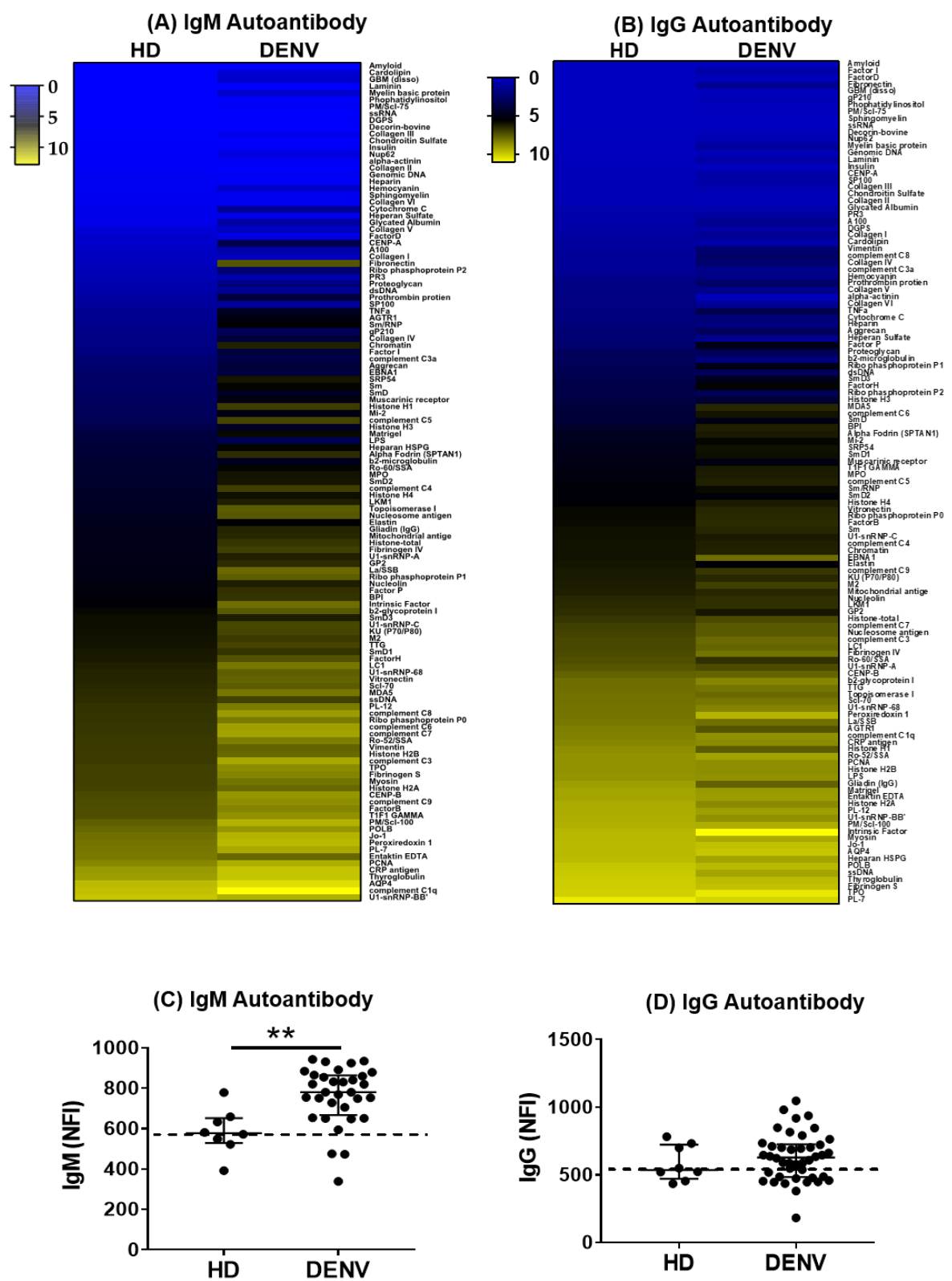
2.2. Autoantibody Profiles in DENV-Infected Patients
2.3. Increased IgG Autoantibody NFI Are Associated with Primary DENV Infection
2.4. Decreased Autoantibodies Correlate with Severity
3. Discussion
4. Materials and Methods
4.1. Ethics Statement
4.2. Patient Samples
4.3. Protein Microarray
4.4. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Katzelnick, L.C.; Fonville, J.M.; Gromowski, G.D.; Arriaga, J.B.; Green, A.; James, S.L.; Lau, L.; Montoya, M.; Wang, C.; Van Blargan, L.A.; et al. Dengue viruses cluster antigenically but not as discrete serotypes. Science 2015, 349, 1338–1343. [Google Scholar] [CrossRef] [Green Version]
- Wilder-Smith, A.; Ooi, E.E.; Horstick, O.; Wills, B. Dengue. Lancet 2019, 393, 350–363. [Google Scholar] [CrossRef]
- Guzmán, M.G.; Kouri, G.; Valdes, L.; Bravo, J.; Alvarez, M.; Vazques, S.; Delgado, I.; Halstead, S.B. Epidemiologic Studies on Dengue in Santiago de Cuba, 1997. Stud. Financ. Adm. Athens 2000, 152, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Sangkawibha, N.; Rojanasuphot, S.; Ahandrik, S. Risk factors in dengue shock syndrome: A prospective epidemiologic study in Rayong, Thailand. Public Health 1984, 107, 357–361. [Google Scholar] [CrossRef]
- Harris, E. Dengue. Lancet 2015, 385, 453–465. [Google Scholar]
- Wrammert, J.; Onlamoon, N.; Akondy, R.S.; Perng, G.C.; Polsrila, K.; Chandele, A.; Kwissa, M.; Pulendran, B.; Wilson, P.C.; Wittawatmongkol, O.; et al. Rapid and Massive Virus-Specific Plasmablast Responses during Acute Dengue Virus Infection in Humans. J. Virol. 2012, 86, 2911–2918. [Google Scholar] [CrossRef] [Green Version]
- Salje, H.; Cummings, D.A.T.T.; Rodriguez-Barraquer, I.; Katzelnick, L.C.; Lessler, J.; Klungthong, C.; Thaisomboonsuk, B.; Nisalak, A.; Weg, A.; Ellison, D.; et al. Reconstruction of antibody dynamics and infection histories to evaluate dengue risk. Nature 2018, 557, 719–723. [Google Scholar] [CrossRef]
- Upasani, V.; Vo, H.T.M.; Ung, S.; Heng, S.; Laurent, D.; Choeung, R.; Duong, V.; Sorn, S.; Ly, S.; Rodenhuis-Zybert, I.A.; et al. Impaired antibody-independent immune response of b cells in patients with acute dengue infection. Front. Immunol. 2019, 10, 2500. [Google Scholar] [CrossRef] [Green Version]
- Priyamvada, L.; Cross-reactive, D.H.; Plasmablasts, M. B Cell Responses during Secondary Dengue Virus Infection Are Dominated by Highly Cross-Reactive, Memory-Derived Plasmablasts. J. Virol. 2016, 90, 5574–5585. [Google Scholar] [CrossRef] [Green Version]
- Ramon, A.; Correa, V.; Carolina, A.; Rosa, E.; Papa, P.; Theresa, A.; De Morais, S.; Maria, L.; Peçanha, T. Dengue Virus Directly Stimulates Polyclonal B Cell Activation. PLoS ONE 2015, 10, e0143391. [Google Scholar]
- Upasani, V.; Vo, H.T.; Auerswald, H.; Laurent, D.; Heng, S.; Duong, V.; Rodenhuis-zybert, I.A.; Dussart, P.; Cantaert, T. Direct infection of B cells by dengue virus modulates B cell responses in a Cambodian paediatric cohort. Front. Immunol. 2020, in press. [Google Scholar]
- Balakrishnan, T.; Bela-ong, D.B.; Toh, Y.X.; Flamand, M.; Devi, S.; Koh, M.B.; Hibberd, M.L.; Ooi, E.E.; Low, J.G.; Leo, Y.S.; et al. Dengue Virus Activates Polyreactive, Natural IgG B Cells after Primary and Secondary Infection. PLoS ONE 2011, 6, e29430. [Google Scholar] [CrossRef] [PubMed]
- Cantaert, T.; Schickel, J.N.; Bannock, J.M.; Ng, Y.S.; Massad, C.; Delmotte, F.R.; Yamakawa, N.; Glauzy, S.; Chamberlain, N.; Kinnunen, T.; et al. Decreased somatic hypermutation induces an impaired peripheral B cell tolerance checkpoint. J. Clin. Investig. 2016, 126, 4289–4302. [Google Scholar] [CrossRef]
- Wardemann, H.; Yurasov, S.; Schaefer, A.; Young, J.W.; Meffre, E.; Nussenzweig, M.C. Predominant autoantibody production by early human B cell precursors. Science 2003, 301, 1374–1377. [Google Scholar] [CrossRef] [Green Version]
- Menard, L.; Cantaert, T.; Chamberlain, N.; Tangye, S.G.; Riminton, D.S.; Church, J.A.; Klion, A.D.; Cunningham-Rundles, C.; Nichols, K.E.; Meffre, E.; et al. Signaling lymphocytic activation molecule (SLAM)/SLAM- associated protein pathway regulates human B-cell tolerance. J. Allergy Clin. Immunol. 2008, 23, 1149–1161. [Google Scholar] [CrossRef] [Green Version]
- Weiskopf, D.; Sette, A. T-cell immunity to infection with dengue virus in humans. Front. Immunol. 2014, 5, 93. [Google Scholar] [CrossRef] [Green Version]
- Jardim, D.L.F.; Tsukumo, D.M.L.; Angerami, R.N.; Filho, M.A.D.C.; Saad, M.J.A. Autoimmune features caused by dengue fever: A case report. Braz. J. Infect. Dis. 2012, 16, 92–95. [Google Scholar] [CrossRef] [Green Version]
- Morel, Z.; Ramírez, A. Autoimmune Response in Children With Dengue. Case Reports. Reumatol. Clín. 2014, 10, 257–259. [Google Scholar] [CrossRef]
- Rajadhyaksha, A.; Mehra, S. Dengue fever evolving into systemic lupus erythematosus and lupus nephritis: A case report. Lupus 2012, 21, 999–1002. [Google Scholar] [CrossRef]
- Li, H.-M.; Huang, Y.-K.; Su, Y.-C.; Kao, C.-H. Increased risk of autoimmune diseases in dengue patients: A population-based cohort study. J. Infect. 2018, 77, 212–219. [Google Scholar]
- García, G.; González, N.; Pérez, A.B.; Sierra, B.; Aguirre, E.; Rizo, D.; Izquierdo, A.; Sánchez, L.; Díaz, D.; Lezcay, M.; et al. Long-term persistence of clinical symptoms in dengue-infected persons and its association with immunological disorders. Int. J. Infect. Dis. 2011, 15, 38–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chien, Y.W.; Wang, C.C.; Wang, Y.P.; Lee, C.Y.; Perng, G.C. Risk of leukemia after dengue virus infection: A population-based cohort study. Cancer Epidemiol. Biomark. Prev. 2020, 29, 558–564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, C.C.; Yen, Y.C.; Lee, C.Y.; Lin, C.F.; Huang, C.C.; Tsai, C.W.; Chuang, T.W.; Bai, C.H. Lower risk of primary Sjogren’s syndrome in patients with dengue virus infection: A nationwide cohort study in Taiwan. Clin. Rheumatol. 2020, 1–10. [Google Scholar] [CrossRef]
- Lin, C.F.; Lei, H.Y.; Shiau, A.L.; Liu, C.C.; Liu, H.S.; Yeh, T.M.; Chen, S.H.; Lin, Y.S. Antibodies from dengue patient sera cross-react with endothelial cells and induce damage. J. Med. Virol. 2003, 69, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Chuang, Y.-C.; Lei, H.-Y.; Lin, Y.-S.; Liu, H.-S.; Wu, H.-L.; Yeh, T.-M. Dengue Virus-Induced Autoantibodies Bind to Plasminogen and Enhance Its Activation. J. Immunol. 2011, 187, 6483–6490. [Google Scholar] [CrossRef] [PubMed]
- Chuang, Y.C.; Lin, Y.S.; Liu, H.S.; Wang, J.R.; Yeh, T.M. Antibodies against thrombin in dengue patients contain both anti-thrombotic and pro-fibrinolytic activities. Thromb. Haemost. 2013, 110, 358–365. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.F.; Lei, H.Y.; Liu, C.C.; Liu, H.S.; Yeh, T.M.; Wang, S.T.; Yang, T.I.; Sheu, F.C.; Kuo, C.F.; Lin, Y.S. Generation of IgM anti-platelet autoantibody in dengue patients. J. Med. Virol. 2001, 63, 143–149. [Google Scholar] [CrossRef]
- Ojha, A.; Nandi, D.; Batra, H.; Singhal, R.; Annarapu, G.K.; Bhattacharyya, S.; Seth, T.; Dar, L.; Medigeshi, G.R.; Vrati, S.; et al. Platelet activation determines the severity of thrombocytopenia in dengue infection. Sci. Rep. 2017, 7, 1–10. [Google Scholar] [CrossRef]
- Lin, C.-F.; Chiu, S.-C.; Hsiao, Y.-L.; Wan, S.-W.; Lei, H.-Y.; Shiau, A.-L.; Liu, H.-S.; Yeh, T.-M.; Chen, S.-H.; Liu, C.-C.; et al. Expression of Cytokine, Chemokine, and Adhesion Molecules during Endothelial Cell Activation Induced by Antibodies against Dengue Virus Nonstructural Protein 1. J. Immunol. 2005, 174, 395–403. [Google Scholar] [CrossRef]
- Oishi, K.; Inoue, S.; Cinco, M.T.D.D.; Dimaano, E.M.; Alera, M.T.P.; Alfon, J.A.R.; Abanes, F.; Cruz, D.J.M.; Matias, R.R.; Matsuura, H.; et al. Correlation between increased platelet-associated IgG and thrombocytopenia in secondary dengue virus infections. J. Med. Virol. 2003, 71, 259–264. [Google Scholar] [CrossRef]
- Liu, I.-J.; Chiu, C.-Y.; Chen, Y.-C.; Wu, H.-C. Molecular Mimicry of Human Endothelial Cell Antigen by Autoantibodies to Nonstructural Protein 1 of Dengue Virus. J. Biol. Chem. 2011, 286, 9726–9736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falconar, A.K.I. The dengue virus nonstructural-1 protein (NS1) generates antibodies to common epitopes on human blood clotting, integrin/adhesin proteins and binds to human endothelial cells: Potential implications in haemorrhagic fever pathogenesis. Arch. Virol. 1997, 142, 897–916. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.L.; Sun, D.S.; Su, M.T.; Lien, T.S.; Chen, Y.H.; Lin, C.Y.; Huang, C.H.; King, C.C.; Li, C.R.; Chen, T.H.; et al. Suppressed humoral immunity is associated with dengue nonstructural protein NS1-elicited anti-death receptor antibody fractions in mice. Sci. Rep. 2020, 10, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simon-Lorière, E.; Duong, V.; Tawfik, A.; Ung, S.; Ly, S.; Casadémont, I.; Prot, M.; Courtejoie, N.; Bleakley, K.; Buchy, P.; et al. Increased adaptive immune responses and proper feedback regulation protect against clinical dengue. Sci. Transl. Med. 2017, 9, eaal5088. [Google Scholar] [CrossRef] [Green Version]
- WHO Dengue Guidelines for Diagnosis, Treatment, Prevention and Control; Geneva World Health Organization Press: Geneva, Switzerland, 1997; Volume 6, pp. 39–48.
- Zhu, H.; Luo, H.; Yan, M.; Zuo, X.; Li, Q.Z. Autoantigen Microarray for High-throughput Autoantibody Profiling in Systemic Lupus Erythematosus. Genom. Proteom. Bioinforma. 2015, 13, 210–218. [Google Scholar] [CrossRef] [Green Version]
- Sfriso, P.; Ghirardello, A.; Botsios, C.; Tonon, M.; Zen, M.; Bassi, N.; Bassetto, F.; Doria, A. Infections and autoimmunity: The multifaceted relationship. J. Leukoc. Biol. 2010, 87, 385–395. [Google Scholar] [CrossRef]
- Harel, M.; Shoenfeld, Y. Predicting and preventing autoimmunity, myth or reality? Ann. N. Y. Acad. Sci. 2006, 1069, 322–345. [Google Scholar] [CrossRef]
- Montes, C.L.; Acosta-Rodríguez, E.V.; Merino, M.C.; Bermejo, D.A.; Gruppi, A. Polyclonal B cell activation in infections: Infectious agents’ devilry or defense mechanism of the host? J. Leukoc. Biol. 2007, 82, 1027–1032. [Google Scholar] [CrossRef]
- Racine, R.; Winslow, G.M. IgM in microbial infections: Taken for granted? Immunol. Lett. 2009, 125, 79–85. [Google Scholar] [CrossRef] [Green Version]
- Changal, K.H.; Raina, A.H.; Raina, A.; Raina, M.; Bashir, R.; Latief, M.; Mir, T.; Changal, Q.H. Differentiating secondary from primary dengue using IgG to IgM ratio in early dengue: An observational hospital based clinico-serological study from North India. BMC Infect. Dis. 2016, 16, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Horns, F.; Dekker, C.L.; Quake, S.R. Memory B Cell Activation, Broad Anti-influenza Antibodies, and Bystander Activation Revealed by Single-Cell Transcriptomics. Cell Rep. 2020, 30, 905–913.e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gujarati, T.P.; Ambika, G. Virus antibody dynamics in primary and secondary dengue infections. J. Math. Biol. 2014, 69, 1773–1800. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, B.; Longo, P.; Miley, M.J.; Montoya, M.; Harris, E.; De Silva, A.M. Dissecting the human serum antibody response to secondary dengue virus infections. PLoS Negl. Trop. Dis. 2017, 11, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, D.W.; Green, S.; Kalayanarooj, S.; Innis, B.L.; Nimmannitya, S.; Suntayakorn, S.; Endy, T.P.; Raengsakulrach, B.; Rothman, A.L.; Ennis, F.A.; et al. Dengue Viremia Titer, Antibody Response Pattern, and Virus Serotype Correlate with Disease Severity. J. Infect. Dis. 2000, 181, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Halstead, S.B.; Nimmannitya, S.; Cohen, S.N. Observations related to pathogenesis of dengue hemorrhagic fever. IV. Relation of disease severity to antibody response and virus recovered. Yale J. Boil. Med. 1969, 42, 311–328. [Google Scholar]
- Gunman, M.G.; Martwez, E.; Bravo, J. Clinical and serologic study of Cuban children with dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS). Bull. Pan Am. Health Organ. 1980, 21, 279. [Google Scholar]
- Rivera-Correa, J.; Rodriguez, A. Divergent Roles of Antiself Antibodies during Infection. Trends Immunol. 2018, 39, 515–522. [Google Scholar] [CrossRef]
- Nagele, E.P.; Han, M.; Acharya, N.K.; DeMarshall, C.; Kosciuk, M.C.; Nagele, R.G. Natural IgG Autoantibodies Are Abundant and Ubiquitous in Human Sera, and Their Number Is Influenced By Age, Gender, and Disease. PLoS ONE 2013, 8, e60726. [Google Scholar] [CrossRef] [Green Version]
- Hue, K.D.T.; Tuan, T.V.; Thi, H.T.N.; Bich, C.T.N.; Le Anh, H.H.; Wills, B.A.; Simmons, C.P. Validation of an internally controlled one-step real-time multiplex RT-PCR assay for the detection and quantitation of dengue virus RNA in plasma. J. Virol. Methods 2011, 177, 168–173. [Google Scholar] [CrossRef] [Green Version]
- Goldstein, L.D.; Chen, Y.J.J.; Wu, J.; Chaudhuri, S.; Hsiao, Y.C.; Schneider, K.; Hoi, K.H.; Lin, Z.; Guerrero, S.; Jaiswal, B.S.; et al. Massively parallel single-cell B-cell receptor sequencing enables rapid discovery of diverse antigen-reactive antibodies. Commun. Biol. 2019, 2, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Jayathilaka, D.; Gomes, L.; Jeewandara, C.; Jayarathna, G.S.B.; Herath, D.; Perera, P.A.; Fernando, S.; Wijewickrama, A.; Hardman, C.S.; Ogg, G.S.; et al. Role of NS1 antibodies in the pathogenesis of acute secondary dengue infection. Nat. Commun. 2018, 9, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loizou, S.; Singh, E.; Wypkema, R.A.A. Anticardiolipin, anti-b2-glycoprotein I and antiprothrombin antibodies in black South African patients with infectious disease. Ann. Rheum. Dis. 2003, 62, 1106–1111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Groot, P.G.; Urbanus, R.T. The significance of autoantibodies against β2-glycoprotein I. Blood 2012, 120, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Kouser, L.; Abdul-Aziz, M.; Nayak, A.; Stover, C.M.; Sim, R.B.; Kishore, U. Properdin and factor H: Opposing players on the alternative complement pathway “see-saw”. Front. Immunol. 2013, 4, 93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silveira, G.F.; Wowk, P.F.; Cataneo, A.H.D.; Dos Santos, P.F.; Delgobo, M.; Stimamiglio, M.A.; Lo Sarzi, M.; Thomazelli, A.P.F.S.; Conchon-Costa, I.; Pavanelli, W.R.; et al. Human T lymphocytes are permissive for dengue virus replication. J. Virol. 2018, 92, e02181-17. [Google Scholar] [CrossRef] [Green Version]
- Agmon-Levin, N.; Damoiseaux, J.; Kallenberg, C.; Sack, U.; Witte, T.; Herold, M.; Bossuyt, X.; Musset, L.; Cervera, R.; Plaza-Lopez, A.; et al. International recommendations for the assessment of autoantibodies to cellular antigens referred to as anti-nuclear antibodies. Ann. Rheum. Dis. 2014, 73, 17–23. [Google Scholar] [CrossRef] [Green Version]
- Koraka, P.; Suharti, C.; Setiati, T.E.; Mairuhu, A.T.A.; Van Gorp, E.; Hach, C.E.; Juffrie, M.; Sutaryo, J.; Van Der Meer, G.M.; Groen, J.; et al. Kinetics of dengue virus-specific serum immunoglobulin classes and subclasses correlate with clinical outcome of infection. J. Clin. Microbiol. 2001, 39, 4332–4338. [Google Scholar] [CrossRef] [Green Version]
- Yurasov, S.; Nussenzweig, M.C. Regulation of autoreactive antibodies. Curr. Opin. Rheumatol. 2007, 19, 421–426. [Google Scholar] [CrossRef]
- Garcia-Carrasco, M.; Ramos, M.; Cervera, R.; Font, J.; Vidal, J.; Muñoz, F.J.; Miret, C.; Espinosa, G.; Ingelmo, M. Hepatitis C virus infection in “primary” Sjogren’s syndrome: Prevalence and clinical significance in a series of 90 patients. Ann. Rheum. Dis. 1997, 56, 173–175. [Google Scholar] [CrossRef] [Green Version]
- Duong, V.; Lambrechts, L.; Paul, R.E.; Ly, S.; Lay, R.S.; Long, K.C.; Huy, R.; Tarantola, A.; Scott, T.W.; Sakuntabhai, A.; et al. Asymptomatic humans transmit dengue virus to mosquitoes. Proc. Natl. Acad. Sci. USA 2015, 112, 14688–14693. [Google Scholar] [CrossRef] [Green Version]



| Characteristics | HD | ASD | DF | DHF | p-Value |
|---|---|---|---|---|---|
| (n = 8) | (n = 11) | (n = 13) | (n = 8) | ||
| Age (year) | 8.9 ± 5.6 | 11.5 ± 3.1 | 9.9 ± 3.0 | 10.1 ± 2.9 | 0.4 a |
| Sex (n, %) | 0.3 b | ||||
| Female | 4 (50%) | 3 (30%) | 7 (53.9%) | 5 (62.5%) | |
| Day of Fever (day) | NA | NA | 7.3 ± 0.8 | 7.1 ± 0.8 | 0.8 c |
| Temp (°C) | NA | NA | 37.6 ± 1 | 36.9 ± 0.4 | 0.1 c |
| Pulse (bpm) | NA | NA | 100 ± 15 | 96 ± 14 | 0.6 c |
| Systolic Blood Pressure (mmHg) | NA | NA | 100 ± 10 | 98 ± 10 | 0.8 c |
| Diastolic Blood Pressure (mmHg) | NA | NA | 63 ± 11 | 63 ± 9 | 0.8 c |
| Hematocrit (%) | NA | NA | 38.5 ± 3.9 | 43.1 ± 4.8 | 0.05 c |
| Platelets (10^9/l) | NA | NA | 149 ± 96 | 61 ± 38 | 0.003 c |
| Viral Load (Log10 copy/mL) | NA | 1.17 × 103 | 4.65 × 104 | 6.21 × 104 | 0.02 a |
| Serotype (n) | |||||
| DENV-1 | NA | 8 (72.73%) | 10 (76.9%) | 7 (87.5%) | |
| DENV-2 | NA | 2 (18.18%) | 0 (0%) | 1 (12.5%) | |
| DENV-4 | NA | 1 (9.09%) | 2 (15.4%) | 0 (0%) | |
| Undetermined | 0 (0%) | 1 (7.7%) | 0 (0%) | ||
| Type of Infection (n, %) | |||||
| Primary Infection | NA | 3 (27.3%) | 3 (23.1%) | 0 (0%) | |
| Secondary Infection | NA | 8 (72.7%) | 10 (76.9%) | 8 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vo, H.T.M.; Duong, V.; Ly, S.; Li, Q.-Z.; Dussart, P.; Cantaert, T. Autoantibody Profiling in Plasma of Dengue Virus–Infected Individuals. Pathogens 2020, 9, 1060. https://doi.org/10.3390/pathogens9121060
Vo HTM, Duong V, Ly S, Li Q-Z, Dussart P, Cantaert T. Autoantibody Profiling in Plasma of Dengue Virus–Infected Individuals. Pathogens. 2020; 9(12):1060. https://doi.org/10.3390/pathogens9121060
Chicago/Turabian StyleVo, Hoa Thi My, Veasna Duong, Sowath Ly, Quan-Zhen Li, Philippe Dussart, and Tineke Cantaert. 2020. "Autoantibody Profiling in Plasma of Dengue Virus–Infected Individuals" Pathogens 9, no. 12: 1060. https://doi.org/10.3390/pathogens9121060
APA StyleVo, H. T. M., Duong, V., Ly, S., Li, Q.-Z., Dussart, P., & Cantaert, T. (2020). Autoantibody Profiling in Plasma of Dengue Virus–Infected Individuals. Pathogens, 9(12), 1060. https://doi.org/10.3390/pathogens9121060






