Mycobacterium avium Subspecies paratuberculosis: Human Exposure through Environmental and Domestic Aerosols
Abstract
:1. Introduction

2. Results
2.1. Aerosols
2.1.1. The Efficiency of Recovery of Bacteria from the Foam Collection Substrate
2.1.2. Analysis of River Taff Foam Collection Substrates
2.1.2.1. Culture
| Date (MM/DD/YY) | Filter Level | Culturable Counts (R2A Agar) Mean CFUs m−3 (Standard Deviation) | Direct Counts (DAPI) Mean Cells m−3 (Standard Deviation) |
|---|---|---|---|
| 11.09.10 | Top | 1.11 × 104 (±3.21 × 103) | 1.89 × 105 (±9.62 × 104) |
| Upper Middle | 6.01 × 104 (±1.17 × 104) | 1.60 × 105 (±6.27 × 104) | |
| Lower Middle | ND | ND | |
| Bottom | 1.19 × 102 (±1.06 × 102) | ND | |
| 05.24.11 | Top | 1.58 × 104 (±8.17 × 1032) | 2.58 × 105 (±1.47 × 105) |
| Middle | ND | ND | |
| Bottom | ND | ND | |
| 06.15.11 | Top | 5.65 × 104 (±2.56 × 104) | ND |
| Middle | ND | ND | |
| Bottom | ND | ND | |
| 08.17.11 | Top | 5.86 × 104 (±4.23 × 103) | 5.20 × 107 (±2.46 × 107) |
| Upper middle | 1.27 × 105 (±2.45 × 104) | ND | |
| Lower middle | 2.12 × 102 (±9.68 × 101) | ND | |
| Bottom | 0 | ND | |
| 09.21.11 | Top | 3.50 × 104 (±2.19 × 104) | 2.75 × 105 (±1.64 × 105) |
| Upper middle | 2.26 × 103 (±1.73 × 102) | 3.91 × 104 (±1.16 × 104) | |
| Lower middle | 3.90 × 101 (±5.08 × 10°) | ND | |
| Bottom | 0 | ND |
2.1.2.2. Molecular Analyses
| Date (MM/DD/YY) | Filter Level | Eubacterial 16S rrn Gene | Mycobacterium spp. 16-23S rRNA ITS (gMyc) (CE m−3) | Map IS900 (CE m−3) | Map F57 (CE m−3) |
|---|---|---|---|---|---|
| 11.09.10 | Top | + | 0 | 0 | 0 |
| Upper Middle | + | 0 | 1–10 | 0 | |
| Lower middle | - | 0 | 0 | 0 | |
| Bottom | - | 0 | 0 | 0 | |
| 05.24.11 | Top | + | 0 | 0 | 0 |
| 06.15.11 | Top | + | 0 | 0 | 0 |
| 08.17.11 | Top | + | 1–10 | 0 | 0 |
| Upper middle | + | 0 | 0 | 0 | |
| Lower middle | - | 0 | 0 | 0 | |
| Bottom | - | 0 | 0 | 0 | |
| 09.21.11 | Top | + | 0 | 0 | 0 |
| Upper middle | + | 0 | 0 | 0 | |
| Lower middle | - | 0 | 0 | 0 | |
| Bottom | - | 0 | 0 | 0 |
2.2. Showers
| Sample Location/Number | Microscopy and Culture | qPCR | |||
|---|---|---|---|---|---|
| Direct Counts and Standard Deviation. (Cells L−1) | Mycobacterial Culture (MGIT) | Mycobacterium spp. (CE L−1) | Map IS900 (CE L−1) | Map F57 (CE L−1) | |
| Cumbria-1 | ND | ND | 104–105 | 0 | 0 |
| Cumbria-2H | ND | - | 106–107 | 0 | 0 |
| Cumbria-2 | ND | - | 106–107 | 0 | 0 |
| Cumbria-3 | ND | - | 103–104 | 0 | 0 |
| Cumbria-4 | ND | - | 102–103 | 0 | 0 |
| Cumbria-5 | ND | ND | 0 | 0 | 0 |
| Cumbria-6 | ND | ND | 0 | 0 | 0 |
| Lancashire-1 | ND | ND | 103–104 | 0 | 0 |
| Lancashire-2 | ND | ND | 107–108 | 1–10 | 0 |
| Lancashire-3 | ND | - | 107–108 | 0 | 0 |
| Lancashire-4 | 7.95 × 108 (±4.02 × 108) | - | 105–106 | 0 | 0 |
| Lancashire-5 | ND | - | 106–107 | 0 | 0 |
| Lancashire-6 | ND | ND | 108–109 | 0 | 0 |
| Lancashire-7 | ND | + | 106–107 | 0 | 0 |
| Lancashire-8 | ND | - | 103–104 | 0 | 0 |
| Lancashire-9 | 1.91 × 109 (±6.07 × 108) | - | 106–107 | 0 | 0 |
| Lancashire-10 | 1.63 × 109 (±5.05 × 108) | + | 107–108 | 0 | 0 |
| Merseyside -1 | ND | - | 108–109 | 103–104 | 101–102 |
| Merseyside-2 | ND | - | 107–108 | 102–103 | 102–103 |
| Merseyside-3 | ND | - | 107–108 | 0 | 0 |
| West Sussex-1aH | ND | ND | 107–108 | 0 | 0 |
| West Sussex-1a | ND | ND | 106–107 | 0 | 0 |
| West Sussex-1bH | ND | - | 106–107 | 0 | 0 |
| West Sussex-1b | ND | + | 107–108 | 0 | 0 |
| West Sussex-2a | 1.64 × 109 (±7.39 × 108) | - | 109–101° | 0 | 0 |
| West Sussex-2b | 2.25 × 109 (±1.02 × 109) | - | 104–105 | 0 | 0 |
| West Sussex-3aH | ND | - | 104–105 | 0 | 0 |
| West Sussex-3a | ND | - | 105–106 | 0 | 0 |
| West Sussex-3b | ND | + | 105–106 | 0 | 0 |
| West Sussex-4H | ND | - | 104–105 | 0 | 0 |
2.3. Discussion
2.3.1. River Aerosols
2.3.2. Shower Heads
3. Experimental Section
3.1. Bacterial Strains and Culture
3.2. Sampling Sites
3.3. Shower Sampling
3.3.1. Recovery of Mycobacteria from Shower Biofilms
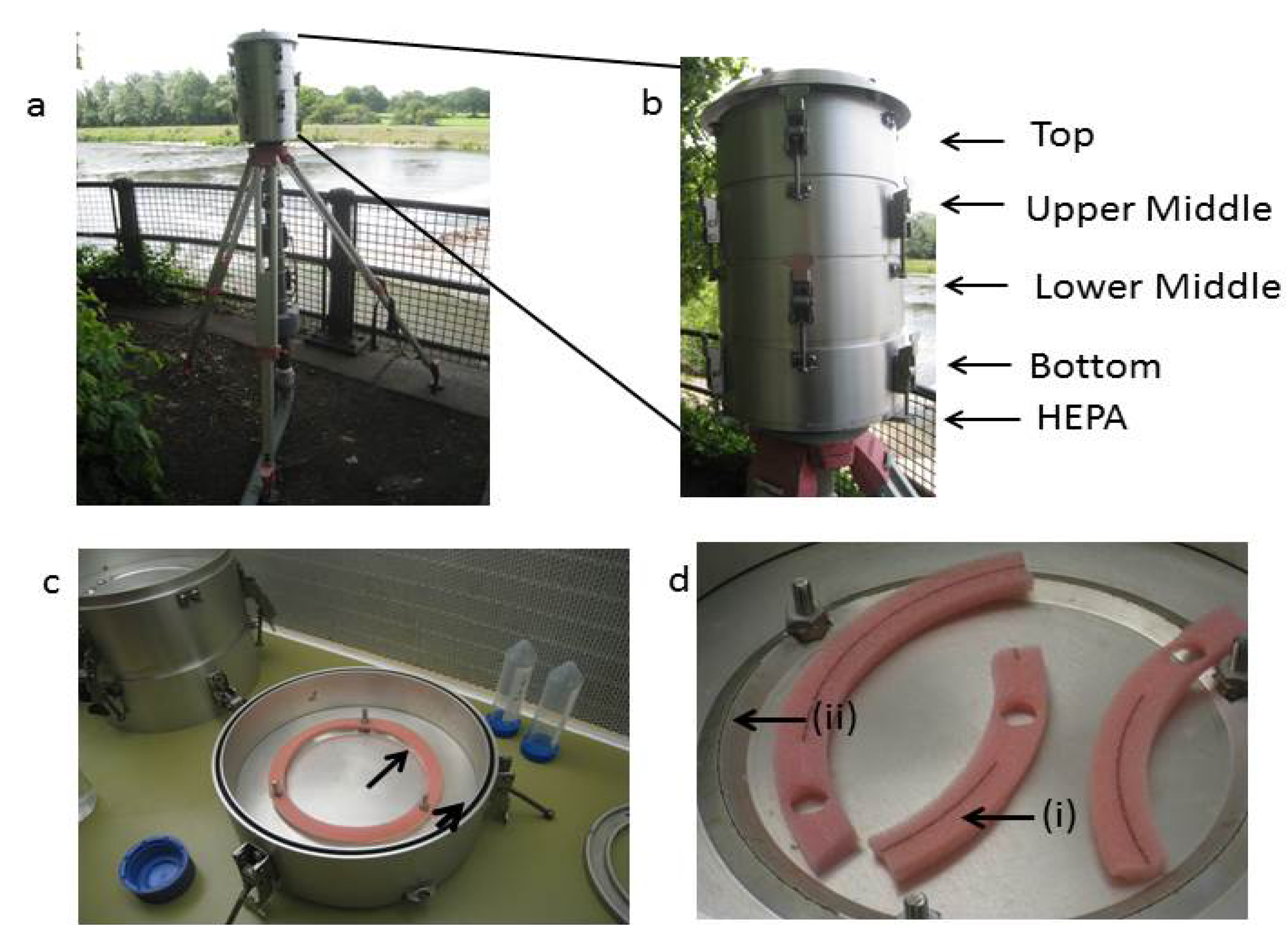
3.4. Aerosol Sampling
3.4.1. Collection
3.4.2. Controlled Assessment of the Efficiency of Cell Recovery from Foam Substrates
3.5. Direct Microscope Counts
3.6. DNA Extraction
3.7. PCR Amplification and qPCR
| Oligonucleotide | Sequence and Fluorophore/Quencher (5'→3') | Target Gene | Reference |
|---|---|---|---|
| pE (forward) | AAACTCAAAGGAATTGACGG | Eubacterial 16S rrn gene | [59] |
| pH’ (reverse) | AAGGAGGTGATCCAGCCGCA | Eubacterial 16S rrn gene | |
| MimmFP (forward) | TTGATGTGCAGACGGATTCC | M. immunogenum rpoB | [55] |
| MimmRP (reverse) | CAACCTCGCGCCAACG | M. immunogenum rpoB | |
| MimmTP (hydrolysis probe) | VIC-TTGAATGGTTGGTCGGCTCGCC-TAMRA | M. immunogenum rpoB | |
| gMycFP * (forward) | GGGGTGTGGTGTTTGAG | Mycobacterium genus 16S-23S rrn gene ITS | [60] |
| gMycRP * (reverse) | CTCCCACGTCCTTCATC | Mycobacterium genus 16S-23S rrn gene ITS | |
| gMycP * (hydrolysis probe) | 6FAM-TGGATAGTGGTTGCGAGCATC-TAMRA | Mycobacterium genus 16S-23S rrn gene ITS | |
| IS900qPCRF (forward) | GATGGCCGAAGGAGATTG | M. avium subsp. paratuberculosis IS900 | [61] |
| IS900qPCRR (reverse) | CACAACCACCTCCGTAACC | M. avium subsp. paratuberculosis IS900 | |
| IS900qPCRTM (hydrolysis probe) | 6FAM–ATTGGATCGCTGTGTAAGGACACGT–BHQ | M. avium subsp. paratuberculosis IS900 | |
| F57-F (forward) | TACGAGCACGCAGGCATTC | M. avium subsp. paratuberculosisF57 | [62] |
| F57-R (reverse) | CGGTCCAGTTCGCTGTCAT | M. avium subsp. paratuberculosisF57 | |
| F57 Taqmanmgb (hydrolysis probe) | VIC-CCTGACCACCCTTC-MGB | M. avium subsp. paratuberculosisF57 |
4. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- Thorel, M.F.; Krichevsky, M.; Levyfrebault, V.V. Numerical taxonomy of mycobactin-dependent mycobacteria, emended description of Mycobacterium avium, and description of Mycobacterium avium subsp avium subsp-nov, Mycobacterium avium subsp paratuberculosis subsp-nov, and Mycobacterium avium subsp silvaticum subsp-nov. Int. J. Syst. Bact. 1990, 40, 254–260. [Google Scholar] [CrossRef]
- Chacon, O.; Bermudez, L.E.; Barletta, R.G. Johne’s disease, inflammatory bowel disease, and Mycobacterium paratuberculosis. A. Rev. Microbiol. 2004, 58, 329–363. [Google Scholar] [CrossRef]
- Nielsen, S.S.; Toft, N. A review of prevalences of paratuberculosis in farmed animals in Europe. Prev. Vet. Med. 2009, 88, 1–14. [Google Scholar] [CrossRef]
- Buergelt, C.D.; Hall, C.; McEntee, K.; Duncan, J.R. Pathological evaluation of para-tuberculosis in naturally infected cattle. Vet. Path. 1978, 15, 196–207. [Google Scholar] [CrossRef]
- Over, K.; Crandall, P.G.; O’Bryan, C.A.; Ricke, S.C. Current perspectives on Mycobacterium avium subsp. paratuberculosis, johne’s disease, and crohn’s disease: A review. Crit. Rev. Microbiol. 2011, 37, 141–156. [Google Scholar] [CrossRef]
- Clarke, C.J. The pathology and pathogenesis of paratuberculosis in ruminants and other species. J. Comp. Pathol. 1997, 116, 217–261. [Google Scholar] [CrossRef]
- McClure, H.M.; Chiodini, R.J.; Anderson, D.C.; Swenson, R.B.; Thayer, W.R.; Coutu, J.A. Mycobacterium-paratuberculosis infection in a colony of stumptail macaques (Macaca arctoides). J. Infect. Dis. 1987, 155, 1011–1019. [Google Scholar] [CrossRef]
- Feller, M.; Huwiler, K.; Stephan, R.; Altpeter, E.; Shang, A.; Furrer, H.; Pfyffer, G.E.; Jemmi, T.; Baumgartner, A.; Egger, M. Mycobacterium avium subspecies paratuberculosis and crohn’s disease: A systematic review and meta-analysis. Lancet Infect. Dis. 2007, 7, 607–613. [Google Scholar] [CrossRef]
- Chiodini, R.J.; Chamberlin, W.M.; Sarosiek, J.; McCallum, R.W. Crohn’s disease and the mycobacterioses: A quarter century later. Causation or simple association? Crit. Rev. Microbiol. 2012, 38, 52–93. [Google Scholar] [CrossRef]
- Bull, T.J.; McMinn, E.J.; Sidi-Boumedine, K.; Skull, A.; Durkin, D.; Neild, P.; Rhodes, G.; Pickup, R.; Hermon-Taylor, J. Detection and verification of Mycobacterium avium subsp. paratuberculosis in fresh ileocolonic mucosal biopsy specimens from individuals with and without crohn’s disease. J. Clin. Microbiol. 2003, 41, 2915–2923. [Google Scholar] [CrossRef]
- Larsen, J.W.A.; Ware, J.K.W.; Kluver, P. Epidemiology of bovine Johne’s disease (bjd) in beef cattle herds in australia. Aust. Vet. J. 2012, 90, 6–13. [Google Scholar] [CrossRef]
- Olsen, I.; Siguroardottir, O.G.; Djonne, B. Paratuberculosis with special reference to cattle—A review. Vet. Q 2002, 24, 12–28. [Google Scholar] [CrossRef]
- Sorensen, O.; Rawluk, S.; Wu, J.; Manninen, K.; Ollis, G. Mycobacterium paratuberculosis in dairy herds in alberta. Can. Vet. J 2003, 44, 221–226. [Google Scholar]
- United States Department of Agriculture. Johne’s disease on U. S. Dairies, 1991–2007. Available online: http://www.aphis.usda.gov/animal_health/nahms/dairy/downloads/dairy07/Dairy07_is_Johnes.pdf (accessed on 11 July 2014).
- Department of the Environment, Food and Rural Affairs (UK). An Integrated Strategy to Determine the Herd Level Prevalence of Johne’s Disease in the uk Dairy Herd. Available online: http://archive.defra.gov.uk/foodfarm/farmanimal/diseases/atoz/documents/johnes-report0911.pdf (accessed on 11 July 2014).
- Caldow, G.; Strain, S.A.J.; Chapman, Z.; Kemp, R.; Cook, A.J. A survey to estimate the herd level prevalence of paratuberculosis in the dairy herd of the united kingdom. Cattle Pract. 2007, 15, 169–171. [Google Scholar]
- Whittington, R.J.; Marsh, I.B.; Reddacliff, L.A. Survival of Mycobacterium avium subsp. paratuberculosis in dam water and sediment. Appl. Environ. Microbiol. 2005, 71, 5304–5308. [Google Scholar] [CrossRef]
- Larsen, A.B.; Merkal, B.S.; Vardaman, T.H. Survival time of Mycobacterium paratuberculosis. Am. J. Vet. Res. 1956, 17, 549–551. [Google Scholar]
- Pickup, R.W.; Rhodes, G.; Arnott, S.; Sidi-Boumedine, K.; Bull, T.J.; Weightman, A.; Hurley, M.; Hermon-Taylor, J. Mycobacterium avium subsp. paratuberculosis in the catchment area and water of the river taff in south wales, united kingdom, an its potential relationship to clustering of crohn’s disease cases in the city of cardiff. Appl. Environ. Microbiol. 2005, 71, 2130–2139. [Google Scholar] [CrossRef]
- Pickup, R.W.; Rhodes, G.; Bull, T.J.; Arnott, S.; Sidi-Boumedine, K.; Hurley, M.; Hermon-Taylor, J. Mycobacterium avium subsp. paratuberculosis in lake catchments, in river water abstracted for domestic use, and in effluent from domestic sewage treatment works: Diverse opportunities for environmental cycling and human exposure. Appl. Environ. Microbiol. 2006, 72, 4067–4077. [Google Scholar] [CrossRef]
- Beumer, A.; King, D.; Donohue, M.; Mistry, J.; Covert, T.; Pfaller, S. Detection of Mycobacterium avium subsp. paratuberculosis in drinking water and biofilms by quantitative pcr. Appl. Environ. Microbiol. 2010, 76, 7367–7370. [Google Scholar] [CrossRef]
- Klanicova, B.; Seda, J.; Slana, I.; Slany, M.; Pavlik, I. The tracing of mycobacteria in drinking water supply systems by culture, conventional, and real time pcrs. Curr. Microbiol. 2013, 67, 725–731. [Google Scholar] [CrossRef]
- Falkinham, J.O. Ecology of nontuberculous mycobacteria-where do human infections come from? Preface. Sem. Resp. Crit. Care 2013, 34, 95–102. [Google Scholar] [CrossRef]
- Aboagye, G.; Rowe, M.T. Occurrence of Mycobacterium avium subspecies paratuberculosis in raw water and water treatment operations for the production of potable water. Wat. Res. 2011, 45, 3271–3278. [Google Scholar] [CrossRef]
- Gill, C.O.; Saucier, L.; Meadus, W.J. Mycobacterium avium subsp paratuberculosis in dairy products, meat, and drinking water. J. Fd Prot. 2011, 74, 480–499. [Google Scholar] [CrossRef]
- Hruska, K.; Kaevska, M. Mycobacteria in water, soil, plants and air: A review. Vete. Med. 2012, 57, 623–679. [Google Scholar]
- Feazel, L.M.; Baumgartner, L.K.; Peterson, K.L.; Frank, D.N.; Harris, J.K.; Pace, N.R. Opportunistic pathogens enriched in showerhead biofilms. P. Natl. Acad. Sci. USA 2009, 106, 16393–16398. [Google Scholar] [CrossRef]
- Thomson, R.; Tolson, C.; Carter, R.; Coulter, C.; Huygens, F.; Hargreaves, M. Isolation of nontuberculous mycobacteria (ntm) from household water and shower aerosols in patients with pulmonary disease caused by ntm. Am. J. Clin. Microb. 2013, 51, 3006–3011. [Google Scholar] [CrossRef]
- Falkinham, J.O., III; Iseman, M.D.; de Haas, P.; van Soolingen, D. Mycobacterium avium in a shower linked to pulmonary disease. J. Water Health 2008, 6, 209–213. [Google Scholar]
- Gunesh, S.; Thomas, G.A.O.; Williams, G.T.; Roberts, A.; Hawthorne, A.B. The incidence of crohn’s disease in cardiff over the last 75 years: An update for 1996–2005. Aliment. Pharm. Therap. 2008, 27, 211–219. [Google Scholar]
- Gunesh, S.K.; Hawthorne, B.A.; Thomas, G.A.O.; Williams, G.T.; Roberts, A. Incidence of crohn’s disease still rising in cardiff: 1931–2005. Gut 2007, 56, A110–A111. [Google Scholar]
- Yapp, T.R.; Stenson, R.; Thomas, G.A.O.; Lawrie, B.W.; Williams, G.T.; Hawthorne, A.B. Crohn’s disease incidence in cardiff from 1930: An update for 1991–1995. Eur. J. Gastroen. Hepat. 2000, 12, 907–911. [Google Scholar] [CrossRef]
- Thomas, G.A.O.; Millarjones, D.; Rhodes, J.; Roberts, G.M.; Williams, G.T.; Mayberry, J.F. Incidence of crohn’s-disease in cardiff over 60 years—1986–1990 an update. Eur. J. Gastroen. Hepat. 1995, 7, 401–405. [Google Scholar]
- Rose, J.D.R.; Roberts, G.M.; Williams, G.; Mayberry, J.F.; Rhodes, I. Cardiff crohns-disease jubilee—The incidence over 50 years. Gut 1988, 29, 346–351. [Google Scholar] [CrossRef]
- Mayberry, J.F.; Hitchens, R.A.N. Distribution of crohn’s disease in cardiff. Soc. Sci. Med. 1978, 12, 137–138. [Google Scholar] [CrossRef]
- Mayberry, J.F. Recent epidemiology of ulcerative colitis and crohn’s disease in cardiff. Int. J. Colorect. Dis. 1989, 4, 39–46. [Google Scholar] [CrossRef]
- Jones, T.; Moreno, T.; BeruBe, K.; Richards, R. The physicochemical characterisation of microscopic airborne particles in south wales: A review of the locations and methodologies. Sci. Total. Environ. 2006, 360, 43–59. [Google Scholar] [CrossRef]
- Xu, Z.; Wu, Y.; Shen, F.; Chen, Q.; Tan, M.; Yao, M. Bioaerosol science, technology, and engineering: Past, present, and future. Aerosol. Sci. Tech. 2011, 45, 1337–1349. [Google Scholar] [CrossRef]
- Li, M.; Qi, J.; Zhang, H.; Huang, S.; Li, L.; Gao, D. Concentration and size distribution of bioaerosols in an outdoor environment in the qingdao coastal region. Sci. Total. Environ. 2011, 409, 3812–3819. [Google Scholar] [CrossRef]
- Xu, Z.; Wei, K.; Wu, Y.; Shen, F.; Chen, Q.; Li, M.; Yao, M. Enhancing bioaerosol sampling by andersen impactors using mineral-oil-spread agar plate. PLoS One 2013, 8, e56896. [Google Scholar]
- Rhodes, G.; Henrys, P.; Thomson, B.C.; Pickup, R.W. Mycobacterium avium subspecies paratuberculosis is widely distributed in british soils and waters: Implications for animal and human health. Envir. Microbiol. 2013, 15, 2761–2774. [Google Scholar]
- Primm, T.P.; Lucero, C.A.; Falkinham, J.O. Health impacts of environmental mycobacteria. Clin. Microbiol. Rev. 2004, 17, 98–106. [Google Scholar] [CrossRef]
- Woodcock, A.H.; Kientzler, C.F.; Arons, A.B.; Blanchard, D.C. Giant condensation nuclei from bursting bubbles. Nature 1953, 172, 1144–1145. [Google Scholar] [CrossRef]
- Falkinham, J.O. Nontuberculous mycobacteria in the environment. Clin. Chest. Med. 2002, 23, 529–551. [Google Scholar] [CrossRef]
- Glazer, C.S.; Martyny, J.W.; Lee, B.; Sanchez, T.L.; Sells, T.M.; Newman, L.S.; Murphy, J.; Heifets, L.; Rose, C.S. Nontuberculous mycobacteria in aerosol droplets and bulk water samples from therapy pools and hot tubs. J. Occup. Health. Environ. Hygiene 2007, 4, 831–840. [Google Scholar] [CrossRef]
- Falkinham, J.O. Mycobacterial aerosols and respiratory disease. Emerg. Infect. Dis. 2003, 9, 763–767. [Google Scholar] [CrossRef]
- Wendt, S.L.; George, K.L.; Parker, B.C.; Gruft, H.; Falkinham, J.O. Epidemiology of infection by nontuberculous mycobacteria. Iii. Isolation of potentially pathogenic mycobacteria from aerosols. Am. Rev. Resp. Dis. 1980, 122, 259–263. [Google Scholar]
- Corner, L.A.L.; Pfeiffer, D.U.; Abbott, K.A. Unanswered questions about the transmission of Mycobacterium avium subspecies paratuberculosis. Vet. J. 2003, 165, 182–183. [Google Scholar] [CrossRef]
- Corner, L.A.L.; Pfeiffer, D.U.; Abbott, K.A. The respiratory tract as a hypothetical route of infection of cattle with Mycobacterium avium subspecies paratuberculosis. Aus. Vet. J. 2004, 82, 170–173. [Google Scholar] [CrossRef]
- Eisenberg, S.W.F.; Nielen, M.; Santema, W.; Houwers, D.J.; Heederik, D.; Koets, A.P. Detection of spatial and temporal spread of Mycobacterium avium subspecies paratuberculosis in the environment of a cattle farm through bio-aerosols. Vet. Microbiol. 2010, 143, 284–292. [Google Scholar] [CrossRef]
- Eisenberg, S.W.F.; Nielen, M.; Koets, A.P. Within-farm transmission of bovine paratuberculosis: Recent developments. Vet. Quart. 2012, 32, 31–35. [Google Scholar] [CrossRef]
- Eisenberg, S.W.F.; Koets, A.D.P.; Nielen, M.; Heederik, D.; Mortier, R; de Buck, J.; Orsel, K. Intestinal infection following aerosol challenge of calves with Mycobacterium avium subspecies paratuberculosis. Vet. Res. 2011, 42, 1–9. [Google Scholar]
- Mayberry, J. Review of environmental-factors and crohns-disease. Acta Hepato-Gastroenterol. 1979, 26, 257–259. [Google Scholar]
- Mayberry, J.; Rhodes, J.; Hughes, L.E. Incidence of crohn disease in cardiff between 1934 and 1977. Gut 1979, 20, 602–608. [Google Scholar] [CrossRef]
- Rhodes, G.; Fluri, A.; Gerber, M.; Henderson, A.; Ruefenacht, A.; Pickup, R.W. Detection of Mycobacterium immunogenum by real-time quantitative taqman pcr. J. Microbiol. Meth. 2008, 73, 266–268. [Google Scholar] [CrossRef]
- Kavouras, I.G.; Ferguson, S.T.; Wolfson, J.M.; Koutrakis, P. Development and validation of a high-volume, low-cutoff inertial impactor. Inhal. Toxicol. 2000, 12, 35–50. [Google Scholar] [CrossRef]
- Kavouras, I.G.; Koutrakis, P. Use of polyurethane foam as the impaction substrate/collection medium in conventional inertial impactors. Aerosol. Sci. Tech. 2001, 34, 46–56. [Google Scholar] [CrossRef]
- Porter, K.G.; Feig, Y.S. The use of dapi for identifying and counting aquatic microflora. Limnol. Oceanogr. 1980, 25, 943–948. [Google Scholar] [CrossRef]
- Edwards, U.; Rogall, T.; Blocker, H.; Emde, M.; Bottger, E.C. Isolation and direct complete nucleotide determination of entire genes—Characterization of a gene coding for 16s-ribosomal rna. Nucl. Acids Res. 1989, 17, 7843–7853. [Google Scholar] [CrossRef]
- Van Coppenraet, E.S.B.; Lindeboom, J.A.; Prins, J.M.; Peeters, M.F.; Claas, E.C.J.; Kuijper, E.J. Real-time pcr assay using fine-needle aspirates and tissue biopsy specimens for rapid diagnosis of mycobacterial lymphadenitis in children. Am. J. Clin. Microb. 2004, 42, 2644–2650. [Google Scholar] [CrossRef]
- Slana, I.; Kralik, P.; Kralova, A.; Pavlik, I. On-farm spread of Mycobacterium avium subsp paratuberculosis in raw milk studied by is900 and f57 competitive real time quantitative pcr and culture examination. Int. J. Food. Microbiol. 2008, 128, 250–257. [Google Scholar] [CrossRef]
- Schoenenbrucher, H.; Abdurnawjood, A.; Failing, K.; Buelte, M. New triplex real-time pcr assay for detection of Mycobacterium avium subsp paratuberculosis in bovine feces. Appl. Environ. Microbiol. 2008, 74, 2751–2758. [Google Scholar] [CrossRef]
- Li, L.L.; Bannantine, J.P.; Zhang, Q.; Amonsin, A.; May, B.J.; Alt, D.; Banerji, N.; Kanjilal, S.; Kapur, V. The complete genome sequence of mycobacterium avium subspecies paratuberculosis. P. Natl. Acad. Sci. USA 2005, 102, 12344–12349. [Google Scholar] [CrossRef]
- Poupart, P.; Coene, M.; Vanheuverswyn, H.; Cocito, C. Preparation of a specific rna probe for detection of Mycobacterium paratuberculosis and diagnosis of johnes disease. Am. J. Clin. Microb. 1993, 31, 1601–1605. [Google Scholar]
- Bustin, S.A.; Benes, V.; Garson, J.A.; Hellemans, J.; Huggett, J.; Kubista, M.; Mueller, R.; Nolan, T.; Pfaffl, M.W.; Shipley, G.L.; et al. The miqe guidelines: Minimum information for publication of quantitative real-time pcr experiments. Clin. Chem. 2009, 55, 611–622. [Google Scholar] [CrossRef]
- Eisenberg, S.; Nielen, M.; Hoeboer, J.; Bouman, M.; Heederik, D.; Koets, A. Mycobacterium avium subspecies paratuberculosis in bioaerosols after depopulation and cleaning of two cattle barns. Vet. Rec. 2011, 168, 587. [Google Scholar] [CrossRef]
- Kudo, K.; Sano, H.; Takahashi, H.; Kuronuma, K.; Yokota, S.; Fujii, N.; Shimada, K.; Yano, I.; Kumazawa, Y.; Voelker, D.; et al. Pulmonary collectins enhance phagocytosis of Mycobacterium avium through increased activity of mannose receptors. J. Immunol. 2004, 172, 7592–7602. [Google Scholar] [CrossRef]
- Storch, I.; Sachar, D.; Catz, S. Pulmonary manifestations of inflammatory bowel disease. Inflamm. Bowel Dis. 2003, 9, 104–115. [Google Scholar] [CrossRef]
- Bonniere, P.; Wallaert, B.; Cortot, A.; Marchandise, X.; Riou, Y.; Tonnel, A.B.; Colombel, J.F.; Voisin, C.; Paris, J.C. Latent pulmonary involvement in crohn’s disease: Biological, functional, bronchoalveolar lavage and scintigraphic studies. Gut 1986, 27, 919–925. [Google Scholar] [CrossRef]
- Calder, C.J.; Lacy, D.; Raafat, F.; Weller, P.H.; Booth, I.W. Crohn’s disease with pulmonary involvement in a 3 year old boy. Gut 1993, 34, 1636–1638. [Google Scholar] [CrossRef]
- Casey, M.B.; Tazelaar, H.D.; Myers, J.L.; Hunninghake, G.W.; Kakar, S.; Kalra, S.X.; Ashton, R.; Colby, T.V. Noninfectious lung pathology in patients with crohn’s disease. Am. J. Surg. Path. 2003, 27, 213–219. [Google Scholar] [CrossRef]
- Louis, E.; Louis, R.; Shute, J.; Lau, L.; Franchimont, D.; Radermecker, M.; Djukanovic, R.; Belaiche, J. Bronchial eosinophillic infiltration in crohn’s disease in the absence of pulmonary disease. Clin. Exp. Allergy 1999, 29, 660–666. [Google Scholar] [CrossRef]
- Mansi, A.; Cucchiara, S.; Greco, L.; Sarnelli, P.; Franco, M.T.; Santamaria, F. Bronchial hyperresponsiveness in children and adolescents with crohn’s disease. Am. J. Resp. Crit. Care 2000, 161, 1051–1054. [Google Scholar] [CrossRef]
- Hermon-Taylor, J. Gut pathogens: Invaders and turncoats in a complex cosmos. Gut Pathog. 2009, 1, 1–3. [Google Scholar] [CrossRef]
- Bannantine, J.P.; Bermudez, L.E. No holes barred: Invasion of the intestinal mucosa by Mycobacterium avium subspecies paratuberculosis. Infect. Immun. 2013, 81, 3960–3965. [Google Scholar] [CrossRef]
- Naser, S.A.; Ghobrial, G.; Romero, C.; Valentine, J.F. Culture of Mycobacterium avium subsp. paratuberculosis from the blood of patients with crohn’s disease. Lancet 2004, 364, 1039–1044. [Google Scholar] [CrossRef]
- Autschbach, F.; Eisold, S.; Hinz, U.; Zinser, S.; Linnebacher, M.; Giese, T.; Loffler, T.; Buchler, M.W.; Schmidt, J. High prevalence of Mycobacterium avium subspecies paratuberculosis is 900 DNA in gut tissues from individuals with crohn’s disease. Gut 2005, 54, 944–949. [Google Scholar] [CrossRef]
- Di Sabatino, A.; Paccagnini, D.; Vidali, F.; Rosu, V.; Biancheri, P.; Cossu, A.; Zanetti, S.; Corazza, G.R.; Sechi, L.A. Detection of Mycobacterium avium subspecies paratuberculosis (map)-specific is900 DNA and antibodies against map peptides and lysate in the blood of crohn’s disease patients. Inflamm. Bowel Dis. 2011, 17, 1254–1255. [Google Scholar] [CrossRef]
- Sechi, L.A.; Scanu, A.M.; Molicotti, P.; Cannas, S.; Mura, M.; Dettori, G.; Fadda, G.; Zanetti, S. Detection and isolation of Mycobacterium avium subspecies paratuberculosis from intestinal mucosal biopsies of patients with and without crohn’s disease in sardinia. Am. J. Gastroenterol. 2005, 100, 1529–1536. [Google Scholar] [CrossRef]
- Abubakar, I.; Myhill, D.; Aliyu, S.H.; Hunter, P.R. Detection of Mycobacterium avium subsp. paratuberculosis from patients with crohn’s disease using nucleic acid-based techniques: A systematic review and meta-analysis. Inflamm. Bowel Dis. 2008, 14, 401–410. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Rhodes, G.; Richardson, H.; Hermon-Taylor, J.; Weightman, A.; Higham, A.; Pickup, R. Mycobacterium avium Subspecies paratuberculosis: Human Exposure through Environmental and Domestic Aerosols. Pathogens 2014, 3, 577-595. https://doi.org/10.3390/pathogens3030577
Rhodes G, Richardson H, Hermon-Taylor J, Weightman A, Higham A, Pickup R. Mycobacterium avium Subspecies paratuberculosis: Human Exposure through Environmental and Domestic Aerosols. Pathogens. 2014; 3(3):577-595. https://doi.org/10.3390/pathogens3030577
Chicago/Turabian StyleRhodes, Glenn, Hollian Richardson, John Hermon-Taylor, Andrew Weightman, Andrew Higham, and Roger Pickup. 2014. "Mycobacterium avium Subspecies paratuberculosis: Human Exposure through Environmental and Domestic Aerosols" Pathogens 3, no. 3: 577-595. https://doi.org/10.3390/pathogens3030577
APA StyleRhodes, G., Richardson, H., Hermon-Taylor, J., Weightman, A., Higham, A., & Pickup, R. (2014). Mycobacterium avium Subspecies paratuberculosis: Human Exposure through Environmental and Domestic Aerosols. Pathogens, 3(3), 577-595. https://doi.org/10.3390/pathogens3030577





