Undetectable = Untransmittable: A Cross-Population Systematic Review and Meta-Analysis on Awareness and Acceptance
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Eligibility
2.2.1. Inclusion Criteria
2.2.2. Data Extraction
2.2.3. Quality and Publication Bias Assessment
2.2.4. Statistical Analysis
3. Results
3.1. Results of the Meta-Analysis
3.2. Evaluation of Quality of Studies and Risk of Bias
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- The Joint United Nations Programme on HIV/AIDS (UNAIDS). Global HIV & AIDS Statistics—Fact Sheet. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 30 June 2025).
- Global HIV Prevention Coalition (GPC). HIV Prevention: From Crisis to Opportunity. Available online: https://www.unaids.org/sites/default/files/media_asset/2023-global-hiv-prevention-coalition-scorecards-key-findings_en.pdf (accessed on 30 June 2025).
- About—Prevention Access Campaign. Available online: https://preventionaccess.org/about-2/ (accessed on 16 January 2024).
- George, G.; Beckett, S.; Reddy, T.; Govender, K.; Cawood, C.; Khanyile, D.; Kharsany, A.B.M. Role of Schooling and Comprehensive Sexuality Education in Reducing HIV and Pregnancy Among Adolescents in South Africa. J. Acquir. Immune Defic. Syndr. 2022, 90, 270–275. [Google Scholar] [CrossRef]
- Shangani, S.; Escudero, D.; Kirwa, K.; Harrison, A.; Marshall, B.; Operario, D. Effectiveness of peer-led interventions to increase HIV testing among men who have sex with men: A systematic review and meta-analysis. AIDS Care 2017, 29, 1003–1013. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.M.; Perry, N.S.; Horvath, K.J.; Smith, L.R. A systematic review of mHealth interventions for HIV prevention and treatment among gay, bisexual, and other men who have sex with men. Transl. Behav. Med. 2020, 10, 1211–1220. [Google Scholar] [CrossRef]
- Cohen, M.S.; Chen, Y.Q.; McCauley, M.; Gamble, T.; Hosseinipour, M.C.; Kumarasamy, N.; Hakim, J.G.; Kumwenda, J.; Grinsztejn, B.; Pilotto, J.H.S.; et al. Antiretroviral Therapy for the Prevention of HIV-1 Transmission. N. Engl. J. Med. 2016, 375, 830–839. [Google Scholar] [CrossRef] [PubMed]
- Rodger, A.J.; Cambiano, V.; Bruun, T.; Vernazza, P.; Collins, S.; van Lunzen, J.; Corbelli, G.M.; Estrada, V.; Geretti, A.M.; Beloukas, A.; et al. Sexual Activity Without Condoms and Risk of HIV Transmission in Serodifferent Couples When the HIV-Positive Partner Is Using Suppressive Antiretroviral Therapy. JAMA 2016, 316, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Rodger, A.J.; Cambiano, V.; Bruun, T.; Vernazza, P.; Collins, S.; Degen, O.; Corbelli, G.M.; Estrada, V.; Geretti, A.M.; Beloukas, A.; et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): Final results of a multicentre, prospective, observational study. Lancet 2019, 393, 2428–2438. [Google Scholar] [CrossRef]
- Hull, M.; Lange, J.; Montaner, J.S.G. Treatment as Prevention–Where Next? Curr. HIV/AIDS Rep. 2014, 11, 496–504. [Google Scholar] [CrossRef]
- Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine HIV Pre-Exposure Prophylaxis: Clinical Guidelines. Update April 2018—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/29682309/ (accessed on 26 April 2021).
- Hesse, B.W.; Nelson, D.E.; Kreps, G.L.; Croyle, R.T.; Arora, N.K.; Rimer, B.K.; Viswanath, K. Trust and sources of health information: The impact of the Internet and its implications for health care providers: Findings from the first Health Information National Trends Survey. Arch. Intern. Med. 2005, 165, 2618–2624. [Google Scholar] [CrossRef]
- Cingolani, A.; Tavelli, A.; Calvino, G.V.; Maggiolo, F.; Girardi, E.; Cozzi-Lepri, A.; Perziano, A.; Meli, P.; Camposeragna, A.; Mattioli, S.; et al. Awareness and perception of accuracy of the Undetectable=Untransmittable message (U=U) in Italy: Results from a survey among PLWHA, infectious-diseases physicians and people having unprotected sex. AIDS Care 2023, 35, 923–933. [Google Scholar] [CrossRef]
- Bor, J.; Fischer, C.; Modi, M.; Richman, B.; Kinker, C.; King, R.; Calabrese, S.K.; Mokhele, I.; Sineke, T.; Zuma, T.; et al. Changing Knowledge and Attitudes Towards HIV Treatment-as-Prevention and “Undetectable = Untransmittable”: A Systematic Review. AIDS Behav. 2021, 25, 4209–4224. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- World Bank Open Data. Available online: https://data.worldbank.org (accessed on 18 September 2023).
- Agarwal, H.; Yeatts, K.; Chung, S.R.; Harrison-Quintana, J.; Torres, T.S. Perceived Accuracy Around Undetectable = Untransmitable Among Sexual and Gender Minorities Using Smartphones in India. AIDS Behav. 2024, 28, 1039–1046. [Google Scholar] [CrossRef]
- Avelino-Silva, V.I.; Vasconcelos, R.; Cerqueira, N.B.; Marcus, U.; Schmidt, A.J.; Veras, M.A. Predictors of knowledge of and access to biomedical prevention among MSM and transgender men in Latin America: Results from the Latin American internet survey. HIV Med. 2022, 23, 764–773. [Google Scholar] [CrossRef]
- Ayala, G.; Santos, G.-M.; Arreola, S.; Garner, A.; Makofane, K.; Howell, S. Blue-Ribbon Boys: Factors associated with PrEP use, ART use and undetectable viral load among gay app users across six regions of the world. J. Int. AIDS Soc. 2018, 21 (Suppl. 5), e25130. [Google Scholar] [CrossRef]
- Cao, W.; Li, J.; Sun, S.; Sturm, C.; Peng, L.; Gu, J.; Hao, C.; Hou, F.; Wei, D.; You, X.; et al. HIV Serostatus Disclosure Among Men Who Have Sex with Men in China in the Era of U=U and PrEP. AIDS Behav. 2022, 26, 1477–1488. [Google Scholar] [CrossRef]
- Card, K.G.; St Denis, F.; Higgins, R.; Klassen, B.; Ablona, A.; Rutherford, L.; Jollimore, J.; Ibanez-Carrasco, F.; Lachowsky, N.J. Who knows about U=U? Social positionality and knowledge about the (un)transmissibility of HIV from people with undetectable viral loads. AIDS Care 2022, 34, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, P.B.; Westmoreland, D.A.; Patel, V.V.; Grov, C. Awareness and Acceptability of Undetectable = Untransmittable Among a U.S. National Sample of HIV-Negative Sexual and Gender Minorities. AIDS Behav. 2021, 25, 634–644. [Google Scholar] [CrossRef]
- Chinbunchorn, T.; Thaneerat, N.; Howell, S.; Sowaprux, T.; Phiphatkunarnon, P.; Lujintanon, S.; Kaewpoowat, Q.; Phanuphak, P.; Phanuphak, N.; Ramautarsing, R.A. Assessment of U=U understanding, PrEP awareness, HIV risk behaviours and factors associated with low HIV knowledge among users of Hornet, an online dating application for LGBTQ, in Thailand. Sex. Transm. Infect. 2023, 99, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Coyne, R.; Noone, C. Investigating the effect of undetectable = untransmittable message frames on HIV stigma: An online experiment. AIDS Care 2022, 34, 55–59. [Google Scholar] [CrossRef]
- Coyne, R.; Walsh, J.C.; Noone, C. Awareness, Understanding and HIV Stigma in Response to Undetectable = Untransmittable Messages: Findings from a Nationally Representative Sample in the United Kingdom. AIDS Behav. 2022, 26, 3818–3826. [Google Scholar] [CrossRef]
- De Vito, A.; Colpani, A.; Zauli, B.; Meloni, M.C.; Fois, M.; Fiore, V.; Pintus, G.A.; Nardi, V.G.; Babudieri, S.; Madeddu, G. How Little Do We Know about HIV and STIs Prevention? Results from a Web-Based Survey among the General Population. Healthcare 2022, 10, 59. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, R.C.; Torres, T.S.; Ceccato, M.D.G.B.; Bezerra, D.R.; Thombs, B.D.; Luz, P.M.; Harel, D. Development and Evaluation of Short-Form Measures of the HIV/AIDS Knowledge Assessment Tool Among Sexual and Gender Minorities in Brazil: Cross-sectional Study. JMIR Public Health Surveill. 2022, 8, e30676. [Google Scholar] [CrossRef]
- Ferreira, R.C.; Torres, T.S.; Marins, L.M.S.; das Graças, B.; Ceccato, M.; Bezerra, D.R.B.; Luz, P.M. HIV knowledge and its correlation with the Undetectable = Untransmittable slogan in Brazil. Rev. Saude Publica 2022, 56, 87. [Google Scholar] [CrossRef]
- Forbes, K. How a Sample of the Heterosexual HIV+ Community in London Understand and Feel About U=U. HIV Med. 2018, 19 (Suppl. S2), S50. Available online: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed19&NEWS=N&AN=621999002 (accessed on 15 November 2023).
- Huntingdon, B.; de Wit, J.; Duracinsky, M.; Juraskova, I. Belief, Covariates, and Impact of the “Undetectable = Untransmittable” Message Among People Living with HIV in Australia. AIDS Patient Care STDS 2020, 34, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.C.; Meng, X.J.; Hu, T.; Luo, D.; Cao, H.; Lin, Q.H.; Zou, H.C. Survey on the cognition of the ‘undetectable equals untransmittable’ concept among HIV-infected men who have sex with men receiving antiviral treatment. Zhonghua Liu Xing Bing Xue Za Zhi 2023, 44, 1610–1615. [Google Scholar] [CrossRef]
- MacGibbon, J.; Bavinton, B.R.; Broady, T.R.; Ellard, J.; Murphy, D.; Calabrese, S.K.; Kalwicz, D.A.; Heath-Paynter, D.; Molyneux, A.; Power, C.; et al. Familiarity with, perceived accuracy of, and willingness to rely on Undetectable=Untransmittable (U=U) among gay and bisexual men in Australia: Results of a national cross-sectional survey. Sex. Health 2023, 20, 211–222. [Google Scholar] [CrossRef]
- McKay, T.; Akre, E.-R.; Henne, J.; Kari, N.; Conway, A.; Gothelf, I. LGBTQ+ Affirming Care May Increase Awareness and Understanding of Undetectable = Untransmittable among Midlife and Older Gay and Bisexual Men in the US South. Int. J. Environ. Res. Public Health 2022, 19, 534. [Google Scholar] [CrossRef]
- Meanley, S.; Connochie, D.; Bonett, S.; Flores, D.D.; Bauermeister, J.A. Awareness and Perceived Accuracy of Undetectable = Untransmittable: A Cross-Sectional Analysis with Implications for Treatment as Prevention Among Young Men Who Have Sex with Men. Sex. Transm. Dis. 2019, 46, 733–736. [Google Scholar] [CrossRef]
- Meunier, E.; Siegel, K.; Sundelson, A.E.; Schrimshaw, E.W. Stages of Adoption of “Treatment as Prevention” Among HIV-Negative Men Who Have Sex with Men Who Engage in Exchange Sex. AIDS Patient Care STDS 2020, 34, 380–391. [Google Scholar] [CrossRef]
- Nunes, N.N.; Vasconcelos, R.; Cortez, A.L.; Ferreira-Filho, E.; Kobayasi, R.; Willets, C.; Cocuzza, M.; Avelino-Silva, V.I. Is U=U consistently known and implemented? A survey among different medical specialists in Brazil. Int. J. STD AIDS 2023, 34, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Okoli, C.; Van de Velde, N.; Richman, B.; Allan, B.; Castellanos, E.; Young, B.; Brough, G.; Eremin, A.; Corbelli, G.M.; Mc Britton, M.; et al. Undetectable equals untransmittable (U=U): Awareness and associations with health outcomes among people living with HIV in 25 countries. Sex. Transm. Infect. 2021, 97, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Rendina, H.J.; Talan, A.J.; Cienfuegos-Szalay, J.; Carter, J.A.; Shalhav, O. Treatment Is More Than Prevention: Perceived Personal and Social Benefits of Undetectable = Untransmittable Messaging Among Sexual Minority Men Living with HIV. AIDS Patient Care STDS 2020, 34, 444–451. [Google Scholar] [CrossRef]
- Rendina, H.J.; Cienfuegos-Szalay, J.; Talan, A.; Jones, S.S.; Jimenez, R.H. Growing Acceptability of Undetectable = Untransmittable but Widespread Misunderstanding of Transmission Risk: Findings from a Very Large Sample of Sexual Minority Men in the United States. J. Acquir. Immune Defic. Syndr. 2020, 83, 215–222. [Google Scholar] [CrossRef]
- Ripamonti, D.; Poliseno, M.; Mazzola, G.; Colletti, P.; Di Biagio, A.; Celesia, B.M.; Gori, A.; Bellagamba, R.; Madeddu, G.; Nozza, S.; et al. Perceptions of U=U Among Italian Infectious Diseases Specialists: A Nationwide Survey on Providers’ Attitudes Toward the Risk of HIV Transmission in Virologically Suppressed Patients. AIDS Res. Hum. Retroviruses 2022, 38, 847–855. [Google Scholar] [CrossRef]
- Rivera, A.V.; Carrillo, S.A.; Braunstein, S.L. Prevalence of U=U Awareness and Its Association with Anticipated HIV Stigma Among Low-Income Heterosexually Active Black and Latino Adults in New York City, 2019. AIDS Patient Care STDS 2021, 35, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.; Buttenheim, A.; Schmucker, L.; Bekker, L.-G.; Thirumurthy, H.; Joseph Davey, D. Undetectable = Untransmittable (U=U) Messaging Increases Uptake of HIV Testing Among Men: Results from a Pilot Cluster Randomized Trial. AIDS Behav. 2021, 25, 3128–3136. [Google Scholar] [CrossRef]
- Stutterheim, S.E.; Kuijpers, K.J.R.; Walden, M.I.; Finkenflugel, R.N.N.; Brokx, P.A.R.; Bos, A.E.R. Trends in HIV Stigma Experienced by People Living with HIV in the Netherlands: A Comparison of Cross-Sectional Surveys Over Time. AIDS Educ. Prev. 2022, 34, 33–52. [Google Scholar] [CrossRef]
- Torres, T.S.; Cox, J.; Marins, L.M.; Bezerra, D.R.; Veloso, V.G.; Grinsztejn, B.; Luz, P.M. A call to improve understanding of Undetectable equals Untransmittable (U=U) in Brazil: A web-based survey. J. Int. AIDS Soc. 2020, 23, e25630. [Google Scholar] [CrossRef]
- Wilkinson, A.L.; Draper, B.L.; Pedrana, A.E.; Asselin, J.; Holt, M.; Hellard, M.E.; Stoove, M. Measuring and understanding the attitudes of Australian gay and bisexual men towards biomedical HIV prevention using cross-sectional data and factor analyses. Sex. Transm. Infect. 2018, 94, 309–314. [Google Scholar] [CrossRef]
- Wu, J.; Fairley, C.K.; Grace, D.; Chow, E.P.F.; Ong, J.J. Agreement of and discussion with clients about Undetectable equals Untransmissible among general practitioners in Australia: A cross-sectional survey. Sex. Health 2023, 20, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Adams, N.; Brady, M.; Ormerod, N.; Radcliffe, K.; Sullivan, A. U=U: Patient and Staff Awareness, Understanding and Impact. In Proceedings of the British HIV Association (BHIVA) Spring Conference, Bournemouth, UK, 2–5 April 2019; Volume 20, p. 9. [Google Scholar]
- Cadeliña, J. Condom Use Among Men Who Have Sex with Men Within Metro Manila, Philippines: Associations with Attitude Towards Its Use and Sexual Health Outcomes. Master’s Thesis, De La Salle University, Manila, Philippines, 2019. Available online: https://animorepository.dlsu.edu.ph/etd_masteral/6614 (accessed on 17 November 2023).
- Clement, M.E.; Zimmerman, R.; Grimm, J.; Schwartz, J. Awareness of U=U Among Gay and Bisexual Men Who Have Sex with Men. Open Forum Infect. Dis. 2019, 6 (Suppl. 2), S461. [Google Scholar] [CrossRef]
- Clifford, K.; Nixon, E.; Dean, G. Developing an Educational Package for Dental Staff to Address HIV Stigma and Discrimination. In Proceedings of the BHIVA/BASHH Conference, Brighton, UK, 5–8 March 2021; p. 173. [Google Scholar]
- Colpani, A.; De Vito, A.; Zauli, B.; Fiore, V.; Nardi, V.G.; Pintus, G.A.; Babudieri, S.; Madeddu, G. How much do we know about HIV and STIs? A comparison between students receiving a brief training and the general population. In Proceedings of the 18th European AIDS Conference (EACS 2021), Online & London, UK, 27–30 October 2021; p. 281. [Google Scholar]
- García, Á.L.; Martín-Zaragoza, L.; Rubio-Ruiz, L.; Martínez-Nieto, C.; Velez-Diaz-Pallares, M.; Sanmartin-Fenollera, P.; Peña-Pedrosa, J.A.; Onteniente-González, A.; Bedoya-del-Olmo, L.M.; Iglesias-Peinado, I.; et al. 6ER-031 Knowledge about human immunodeficiency virus (HIV) transmission in people living with HIV in antiretroviral therapy. Eur. J. Hosp. Pharm. 2023, 30 (Suppl. 1), A169. [Google Scholar] [CrossRef]
- Htun, W.L.; Hodgson, C.; Potts, S.; Carroll, K.; Sweeney, J. HIV Knowledge Survey in a District Hospital. In Proceedings of the British HIV Association (BHIVA) Spring Conference 2023, Gateshead, UK, 24–26 April 2023. Abstract P080. [Google Scholar]
- Katsarolis, I.; Tsami, B. Έρευνα κοινής γνώμης για τις γνώσεις, απόψεις και στάσεις για την HIV λοίμωξη στην Ελλάδα. 2021. Available online: https://aids.org.gr/wp-content/uploads/2023/02/2021-1125-27_EEMAA_CongressAIDS33_Supplement_D.pdf (accessed on 17 November 2023).
- Keane, A.; Heskin, J.; Lyons, F. Junior doctors’ knowledge and education needs in relation to the use of antiretroviral therapy (ART) in HIV prevention. In Proceedings of the 6th Annual Conference of the British HIV Association (BHIVA)–Digital Conference, Online, 22–24 November 2020; pp. 16–74. [Google Scholar]
- Mastrogianni, E.; Protopapas, K.; Leonidou, L.; Roussos, S.; Iliadi, E.; Mpasoulis, D.; Oikonomopoulou, X.; Thomas, K.; Antoniadou, A.; Psychogiou, M. H έλλειψη βασικών γνώσεων σε επαγγελματίες υγείας αποτελεί βασική αιτία του στίγματος που σχετίζεται με την HIV λοίμωξη—Μελέτη «ΙAΣΩ». 2021. Available online: https://aids.org.gr/wp-content/uploads/2023/02/2021-1125-27_EEMAA_CongressAIDS33_Supplement_D.pdf (accessed on 17 November 2023).
- Reyes-Díaz, M.; Schmidt, A.; Veras, M.; Stuardo, V.; Casabona, J.; Cáceres, C. Impact of Undetectable=Untransmissible (U=U) Knowledge on Mental Health Outcomes Among HIV+ MSM in the Latin-American MSM Internet Survey (LAMIS). 2020. Available online: https://www.sidastudi.org/es/registro/a53b7fb378a8e080017a1aeacc9b0663 (accessed on 17 November 2023).
- Shongwe, M.; Mohamed, R.; Soliman, S.; AbdAllah, M.; Raslan, E.; Helal, S.; Aiad, K.; Elshirbeny, M.; Gamal, M.; Cordie, A. Healthcare Professionals Knowledge, Attitudes and Practices on HIV/AIDS Care in Our Hospitals. In Proceedings of the 18th European AIDS Conference (EACS 2021), Online & London, UK, 27–30 October 2021; p. 269. [Google Scholar]
- Rendina, H.J.; Parsons, J.T. Factors associated with perceived accuracy of the Undetectable = Untransmittable slogan among men who have sex with men: Implications for messaging scale-up and implementation. J. Int. AIDS Soc. 2018, 21. [Google Scholar] [CrossRef]
- Grace, D.; Stewart, M.; Blaque, E.; Ryu, H.; Anand, P.; Gaspar, M.; Worthington, C.; Gilbert, M. Challenges to communicating the Undetectable equals Untransmittable (U=U) HIV prevention message: Healthcare provider perspectives. PLoS ONE 2022, 17, e0271607. [Google Scholar] [CrossRef] [PubMed]
- Ngure, K.; Ongolly, F.; Dolla, A.; Awour, M.; Mugwanya, K.K.; Irungu, E.; Mugo, N.; Bukusi, E.A.; Morton, J.; Odoyo, J.; et al. “I just believe there is a risk” understanding of undetectable equals untransmissible (U=U) among health providers and HIV-negative partners in serodiscordant relationships in Kenya. J. Int. AIDS Soc. 2020, 23, e25466. [Google Scholar] [CrossRef]
- Greene, R.E.; Luong, A.; Barton, S.C.; Kapadia, F.; Halkitis, P.N. Assessing Gaps in the HIV Care Continuum in Young Men Who Have Sex with Men: The P18 Cohort Study. J. Assoc. Nurses AIDS Care 2018, 29, 475–478. [Google Scholar] [CrossRef]
- Onoya, D.; Sineke, T.; King, R.; Mokhele, I.; Sharma, S.; Dukashe, M.; Cele, R.; Bokaba, D.; Inglis, R.; Sigasa, S.; et al. Designing effective U=U communication strategies considering the needs of PLHIV, their partners, and healthcare worker constraints in South African clinics. PLoS ONE 2023, 18, e0295920. [Google Scholar] [CrossRef]
| Prevalence Rates | |||
|---|---|---|---|
| n | ES (95%CI:) | Heterogeneity I2, p | |
| MSM | |||
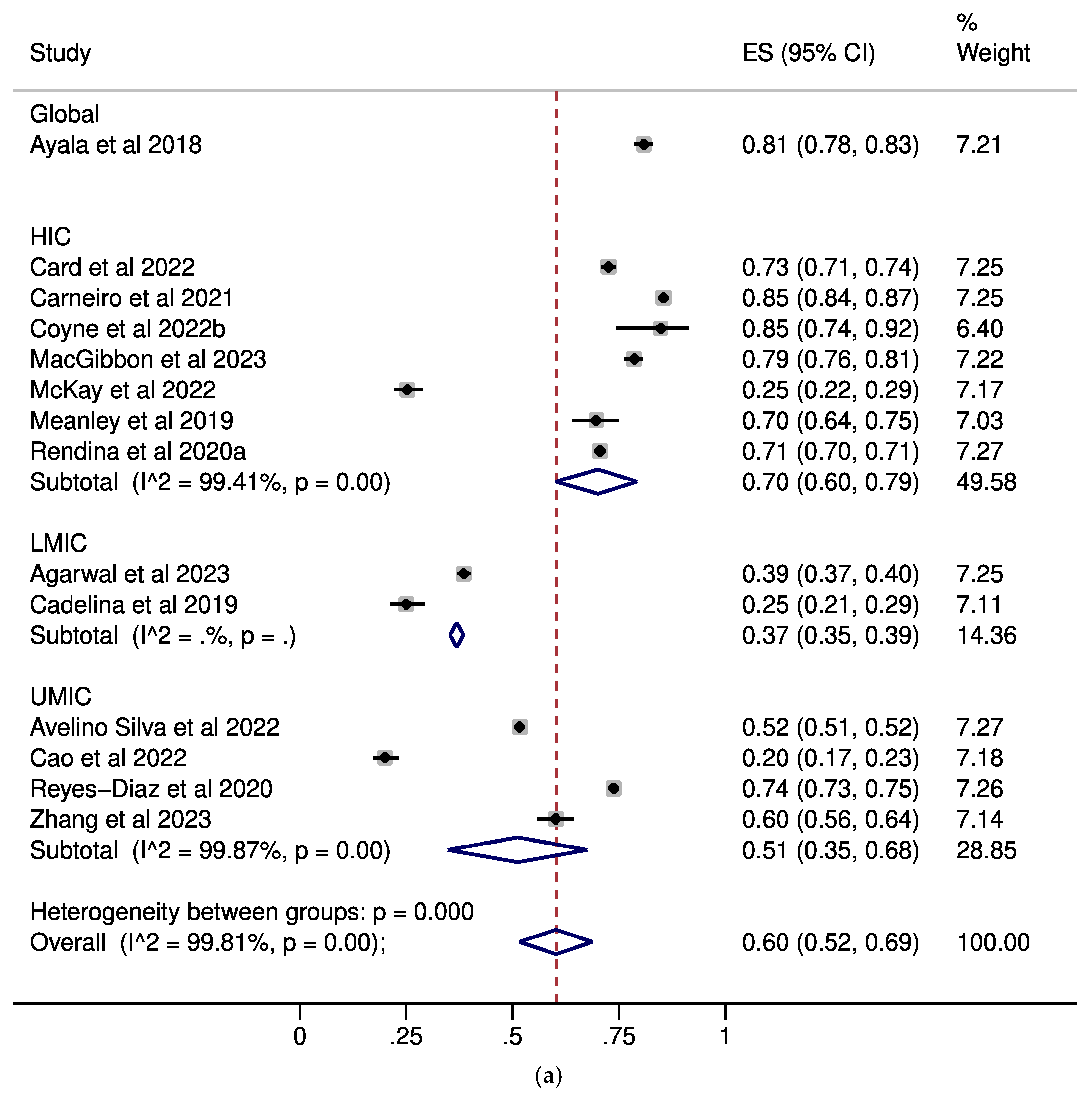
| U=U awareness | |||
| Overall Analysis | 14 | 0.60 (0.52–0.69) | 99.81%, p < 0.001 |
| Subgroups by Income Status | |||
| HIC | 7 | 0.70 (0.60–0.69) | 99.41%, p < 0.001 |
| UMIC | 4 | 0.51 (0.35–0.68) | NC |
| LMIC | 2 | 0.37 (0.35–0.39) | NC |
| Global | 1 | 0.81 (0.78–0.83) | NC |
| Subgroup by PLWH Percentage | |||
| Any HIV Status | 5 | 0.54 (0.40–0.67) | 99.70%, p < 0.001 |
| HIV-Negative/Unknown | 3 | 0.59 (0.14–0.96) | NC |
| PLWH | 4 | 0.72 (0.68–0.76) | 97.32%, p < 0.001 |
| Not Reported | 2 | 0.33 (0.9–0.37) | NC |
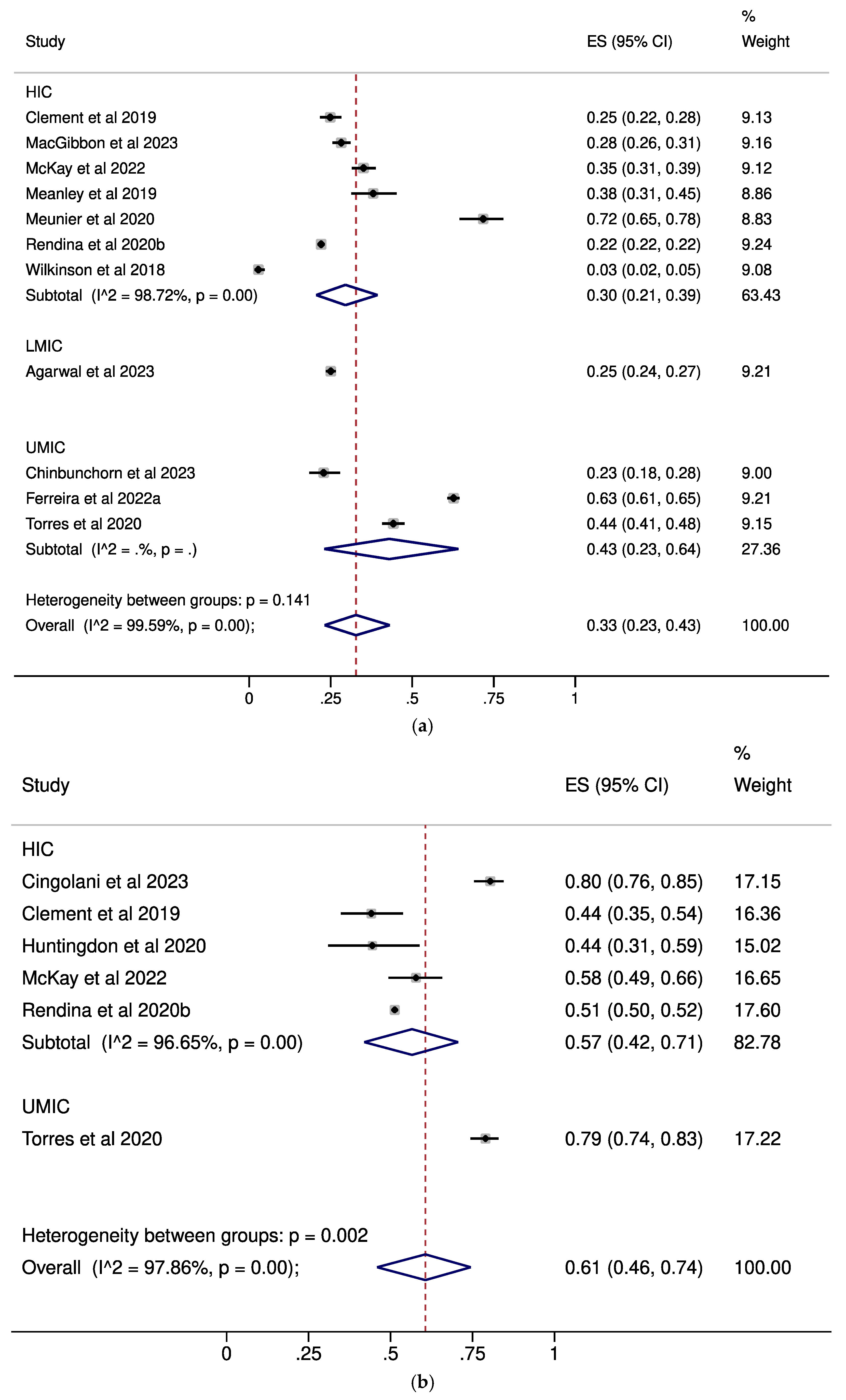
| U=U complete acceptance | |||
| Overall Analysis | 12 | 0.33 (0.23–0.43) | 99.59%, p < 0.001 |
| Subgroups by Income Status | |||
| HIC | 8 | 0.30 (0.21–0.39) | 98.72%, p < 0.001 |
| UMIC | 3 | 0.43 (0.23–0.64) | NC |
| LMIC | 1 | 0.25 (0.24–0.27) | NC |
| Subgroups by PLWH percentage | |||
| Any HIV Status | 7 | 0.31 (0.20–0.43) | 99.68%, p < 0.001 |
| HIV-Negative/Unknown | 4 | 0.36 (0.09–0.69) | 99.41%, p < 0.001 |
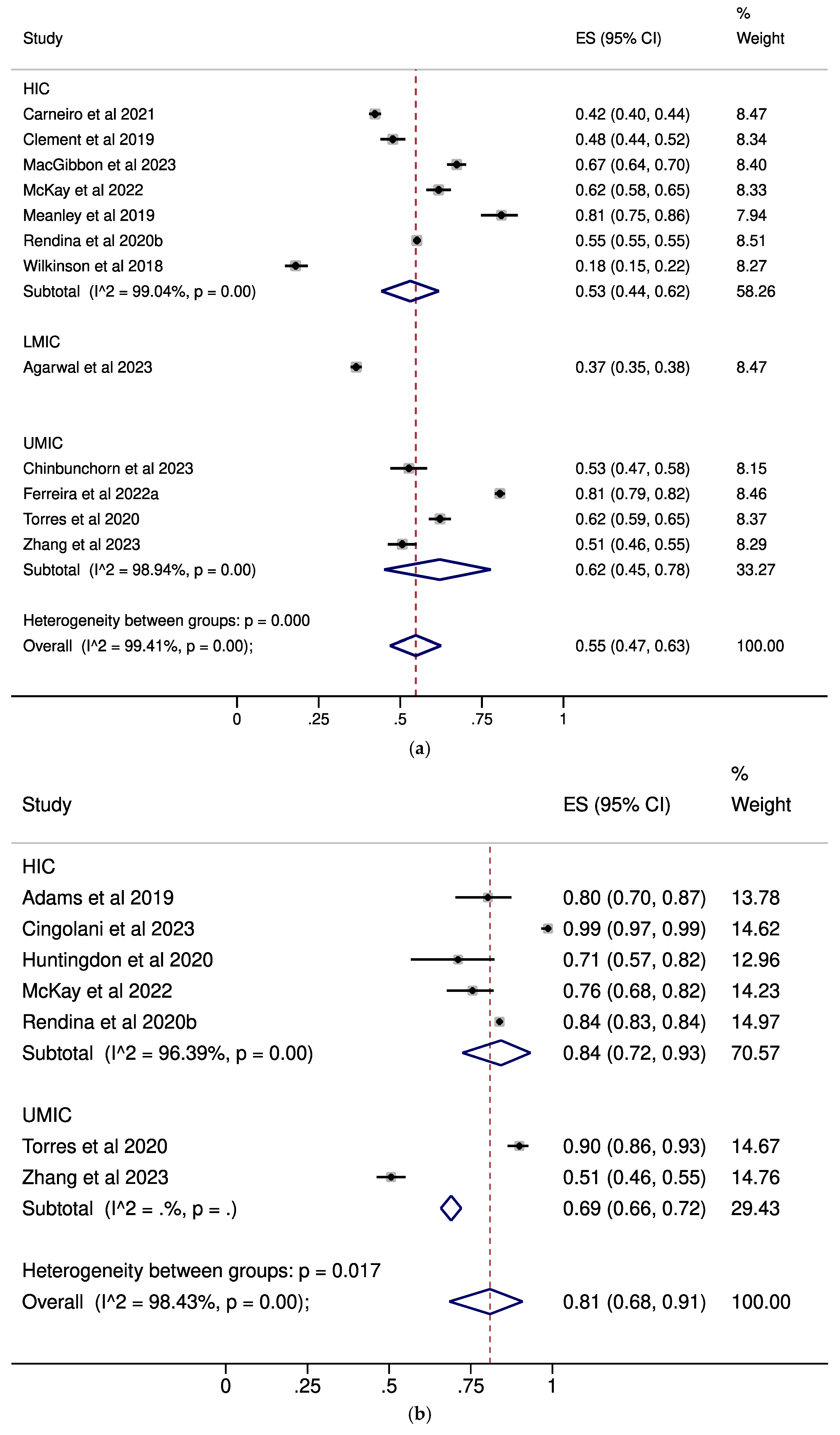
| U=U any acceptance | |||
| Overall Analysis | 12 | 0.55 (0.47–0.63) | 99.46%, p < 0.001 |
| Subgroups by Income Status | |||
| HIC | 7 | 0.53 (0.44–0.62) | 99.04%, p < 0.001 |
| UMIC | 4 | 0.62 (0.45–0.78) | NC |
| LMIC | 1 | 0.37 (0.35–0.38) | NC |
| Subgroups by PLWH percentage | |||
| Any HIV Status | 7 | 0.58 (0.47–0.68) | 99.54%, p < 0.001 |
| HIV-Negative/Unknown | 4 | 0.51 (0.31–0.70) | 99.2%, p < 0.001 |
| PLWH | 1 | 0.51 (0.46–0.63) | NC |
| PLWH | |||
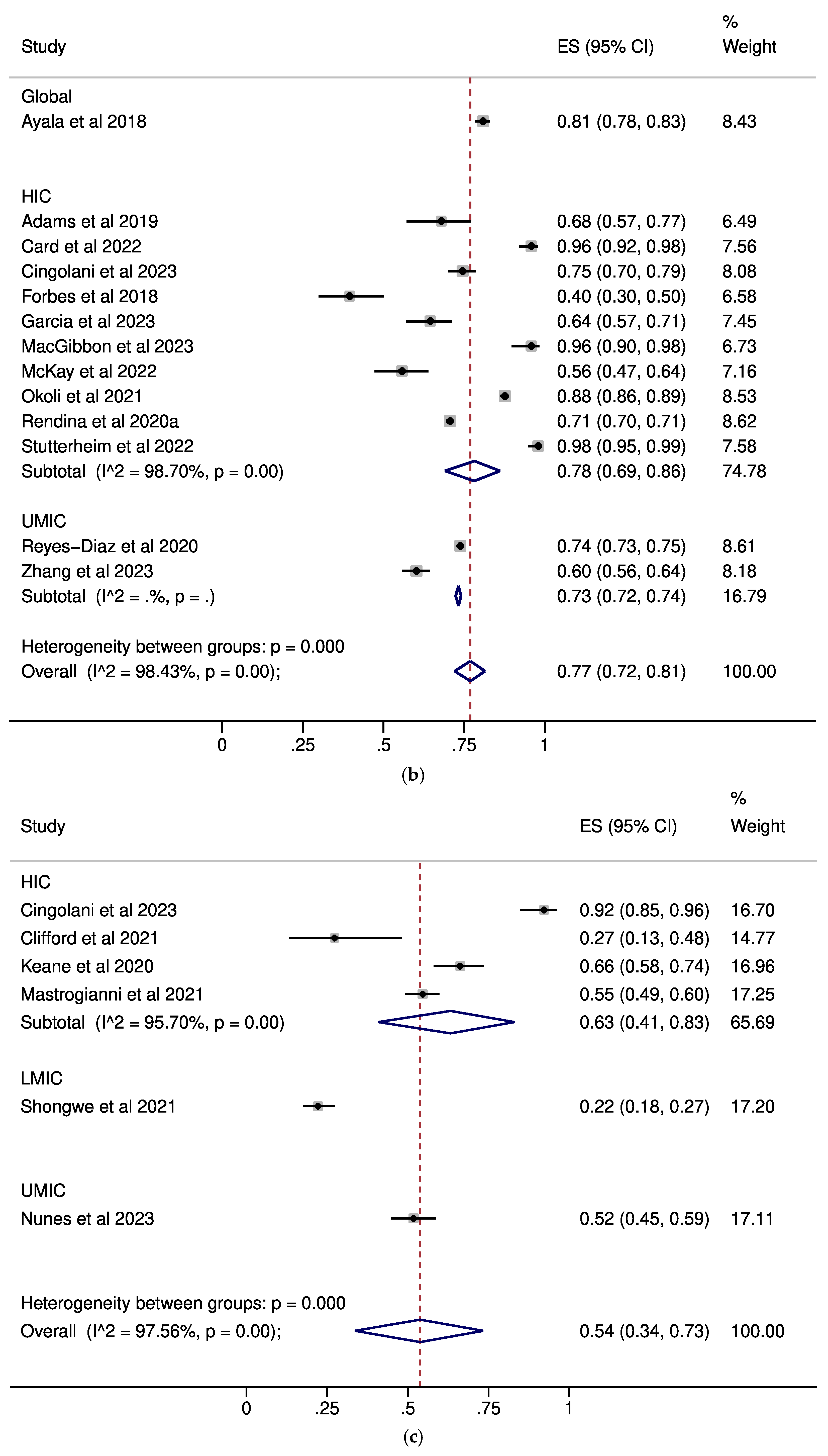
| U=U awareness | |||
| Overall Analysis | 13 | 0.77 (0.72–0.81) | 98.43%, p < 0.001 |
| Subgroups by Income Status | |||
| HIC | 10 | 0.78 (0.69–0.86) | 98.70%, p < 0.001 |
| UMIC | 2 | 0.73 (0.72–0.74) | NC |
| Global | 1 | 0.81 (0.78–0.83) | NC |
| Subgroups by Sexual Orientation | |||
| MSM | 7 | 0.77 (0.73–0.81) | 97.71%, p<.001 |
| MSM and Heterosexual | 3 | 0.88 (0.76–0.97) | NC |
| MSM and Heterosexual | 3 | 0.88 (0.76–0.97) | NC |
| Heterosexual | 1 | 0.40 (0.30–0.50) | NC |
| Not Reported | 2 | 0.66 (0.60–0.71) | NC |
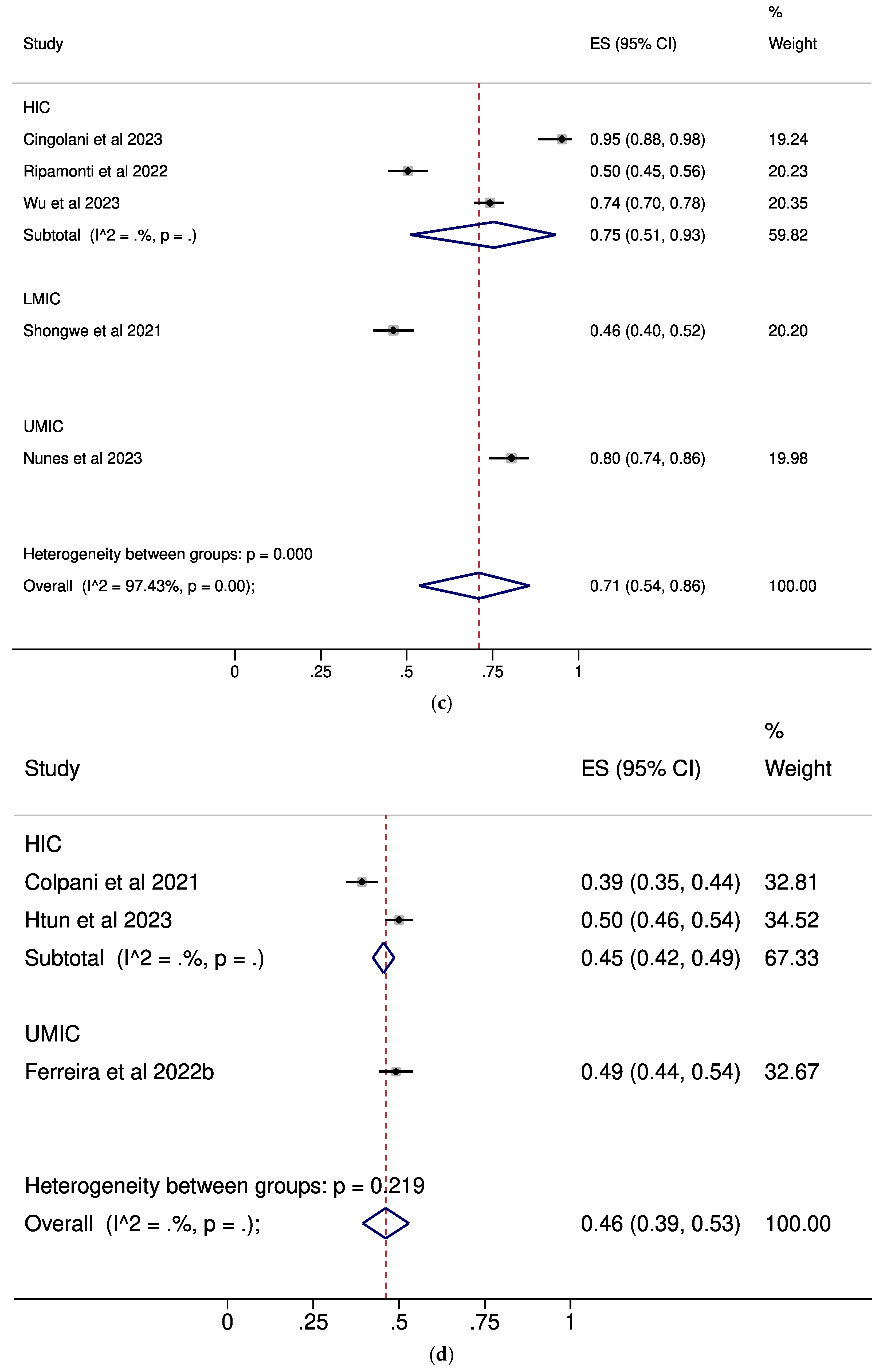
| U=U complete acceptance | |||
| Overall Analysis | 6 | 0.61 (0.46–0.74) | 97.86%, p < 0.001 |
| Subgroups by Income Status | |||
| HIC | 5 | 0.57 (0.42–0.83) | 96.65%, p < 0.001 |
| UMIC | 1 | 0.79 (0.74–0.83) | NC |
| Subgroups by Sexual Orientation | |||
| MSM | 3 | 0.51 (0.46–0.57) | NC |
| MSM and Heterosexual | 3 | 0.71 (0.57–0.83) | NC |
| U=U any acceptance | |||
| Overall Analysis | 7 | 0.81 (0.68–0.91) | 98.43%, p < 0.001 |
| Subgroups by Income Status | |||
| HIC | 5 | 0.84 (0.72–0.93) | 96.39%, p < 0.001 |
| UMIC | 2 | 0.69 (0.66–0.72) | NC |
| Subgroups by Sexual Orientation | |||
| MSM | 3 | 0.71 (0.45–0.91) | NC |
| MSM and Heterosexual | 3 | 0.90 (0.75–0.99) | NC |
| Not Reported | 1 | 0.80 (0.70–0.87) | NC |
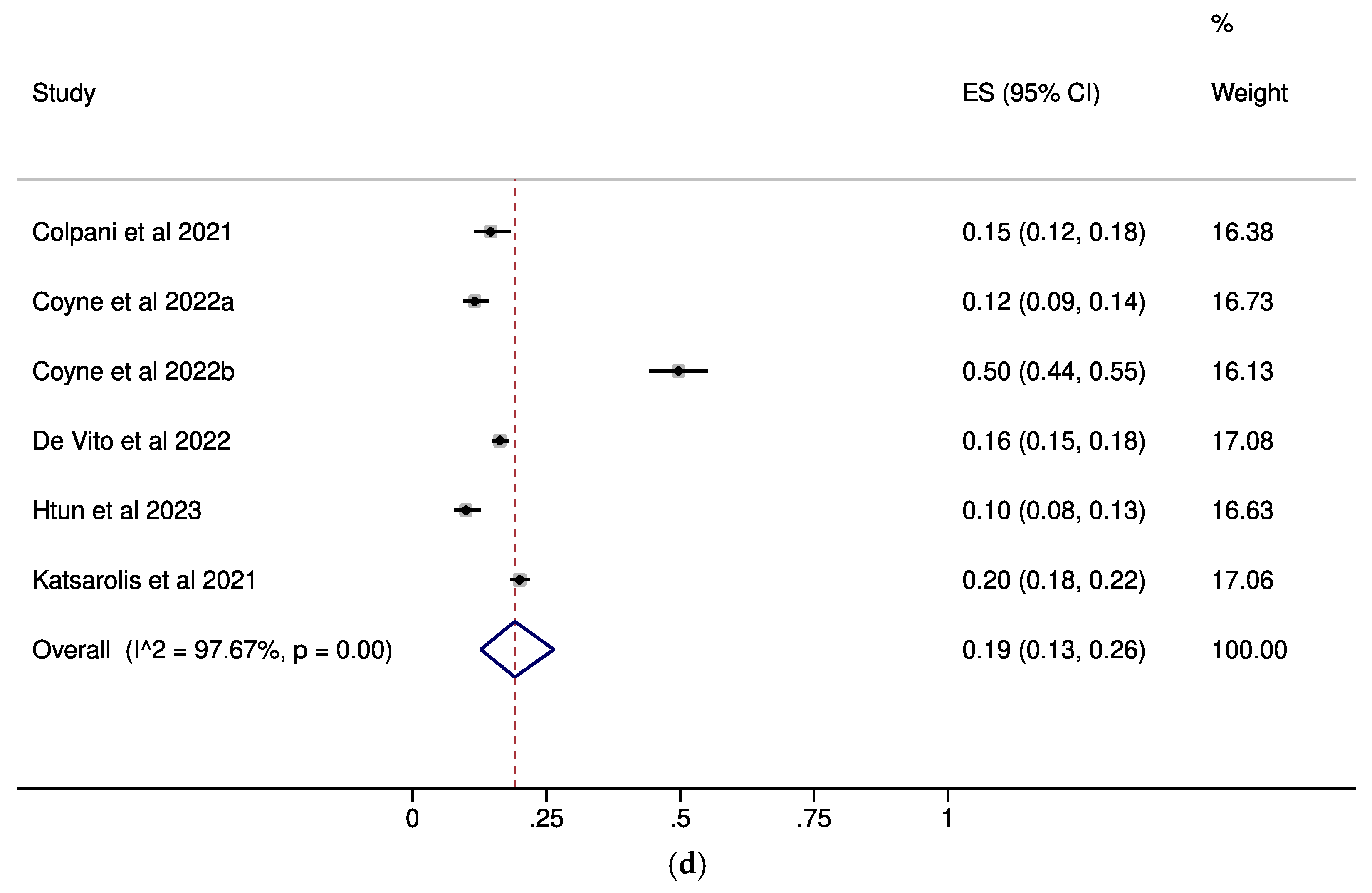
| Healthcare Professionals | |||
| U=U awareness | |||
| Overall Analysis | 6 | 0.54 (0.34–0.73) | 97.56%, p < 0.001 |
| Subgroups by Income Status | |||
| HIC | 4 | 0.63 (0.41–0.83) | 95.7%, p < 0.001 |
| UMIC | 1 | 0.52 (0.45–0.59) | NC |
| LMIC | 1 | 0.22 (0.18–0.27) | NC |
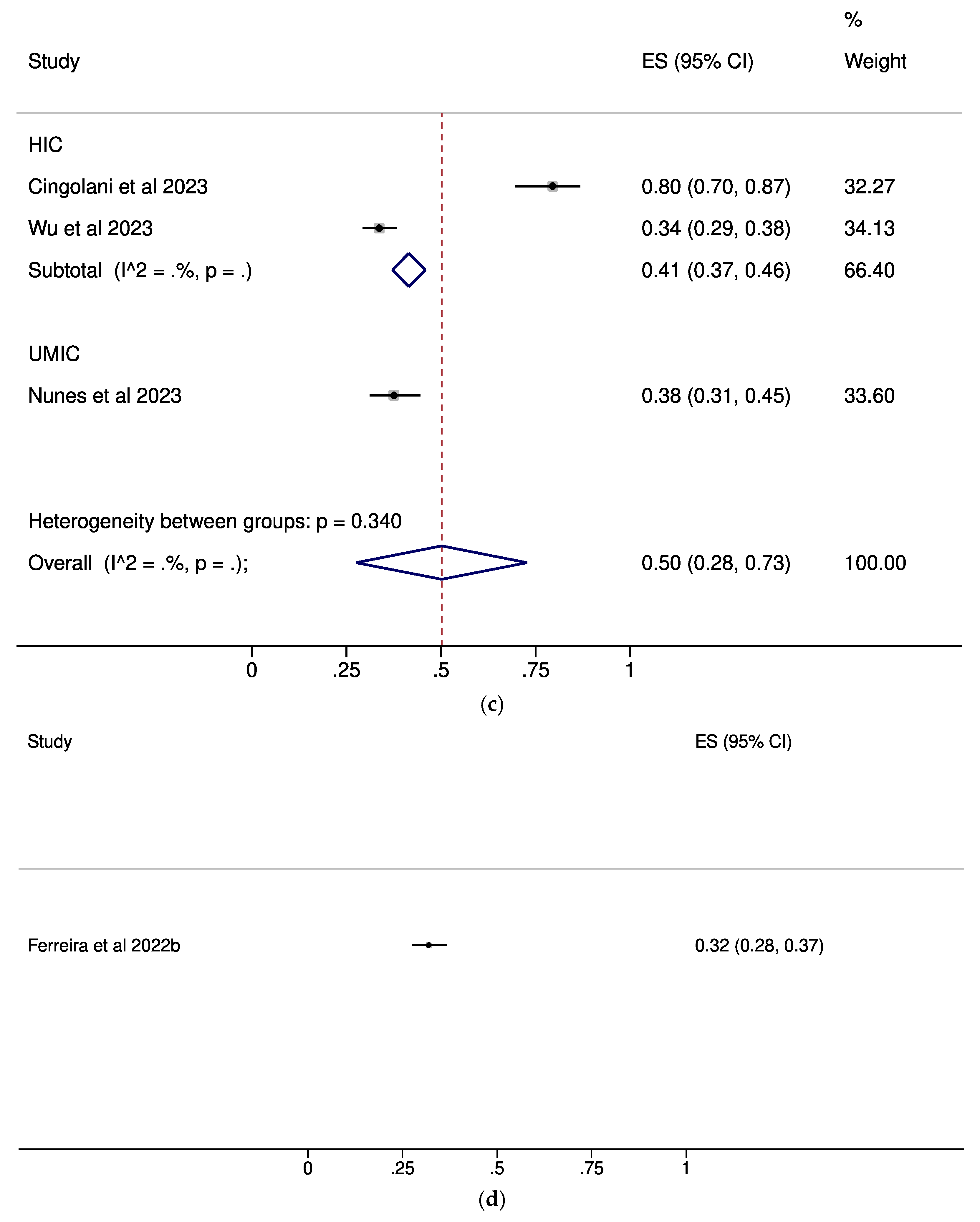
| U=U complete acceptance | |||
| Overall Analysis | 3 | 0.50 (0.28–0.73) | NC |
| Subgroups by Income Status | |||
| HIC | 2 | 0.41 (0.37–0.46) | NC |
| UMIC | 1 | 0.38 (0.31–0.45) | NC |
| U=U any acceptance | |||
| Overall Analysis | 5 | 0.71 (0.54–0.86) | 97.43%, p < 0.001 |
| Subgroups by Income Status | |||
| HIC | 3 | 0.75 (0.51–0.93) | NC |
| UMIC | 1 | 0.80 (0.74–0.86) | NC |
| LMIC | 1 | 0.46 (0.40–0.52) | NC |
| General Population | |||
| U=U awareness | |||
| Overall Analysis | 6 | 0.19 (0.13–0.26) | 97.67%, p < 0.001 |
| U=U complete acceptance | |||
| Overall Analysis | 1 | 0.32 (0.28–0.37) | NC |
| U=U any acceptance | |||
| Overall Analysis | 3 | 0.46 (0.39–0.53) | NC |
| Subgroups by Income Status | |||
| HIC | 2 | 0.45 (0.42–0.49) | NC |
| UMIC | 1 | 0.49 (0.44–0.54) | NC |
| Miscellaneous groups | |||
| U=U awareness | |||
| HIV-Negative People Having Unprotected Sex | 1 | 0.47 (0.43–0.51) | NC |
| Heterosexual Black and Latino Adults | 1 | 0.35 (0.31–0.39) | NC |
| Men Presenting for An HIV Test | 1 | 0.70 (0.64–0.76) | NC |
| HIV-Negative People Having Unprotected Sex | 1 | 0.67 (0.62–0.72) | NC |
| HIV-Negative/Unknown HIV Status, Non-Gay Non-Bisexual | 1 | 0.17 (0.14–0.21) | NC |
| U=U any acceptance | |||
| HIV-Negative People Having Unprotected Sex | 1 | 0.98 (0.95–0.99) | NC |
| HIV-Negative/Unknown HIV Status, Non-Gay Non-Bisexual | 1 | 0.31 (0.27–0.35) | NC |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Georgiadis, N.; Katsimpris, A.; Halkitis, P.N.; Kaba, E.; Tzanakaki, G.; Vassilakou, T.; Beloukas, A.; Sergentanis, T.N. Undetectable = Untransmittable: A Cross-Population Systematic Review and Meta-Analysis on Awareness and Acceptance. Pathogens 2025, 14, 673. https://doi.org/10.3390/pathogens14070673
Georgiadis N, Katsimpris A, Halkitis PN, Kaba E, Tzanakaki G, Vassilakou T, Beloukas A, Sergentanis TN. Undetectable = Untransmittable: A Cross-Population Systematic Review and Meta-Analysis on Awareness and Acceptance. Pathogens. 2025; 14(7):673. https://doi.org/10.3390/pathogens14070673
Chicago/Turabian StyleGeorgiadis, Nikolaos, Andreas Katsimpris, Perry N. Halkitis, Evridiki Kaba, Georgina Tzanakaki, Tonia Vassilakou, Apostolos Beloukas, and Theodoros N. Sergentanis. 2025. "Undetectable = Untransmittable: A Cross-Population Systematic Review and Meta-Analysis on Awareness and Acceptance" Pathogens 14, no. 7: 673. https://doi.org/10.3390/pathogens14070673
APA StyleGeorgiadis, N., Katsimpris, A., Halkitis, P. N., Kaba, E., Tzanakaki, G., Vassilakou, T., Beloukas, A., & Sergentanis, T. N. (2025). Undetectable = Untransmittable: A Cross-Population Systematic Review and Meta-Analysis on Awareness and Acceptance. Pathogens, 14(7), 673. https://doi.org/10.3390/pathogens14070673










