Ocular Symptoms in Pre- and Perimenopausal Woman Infected with Demodex spp.
Abstract
1. Introduction
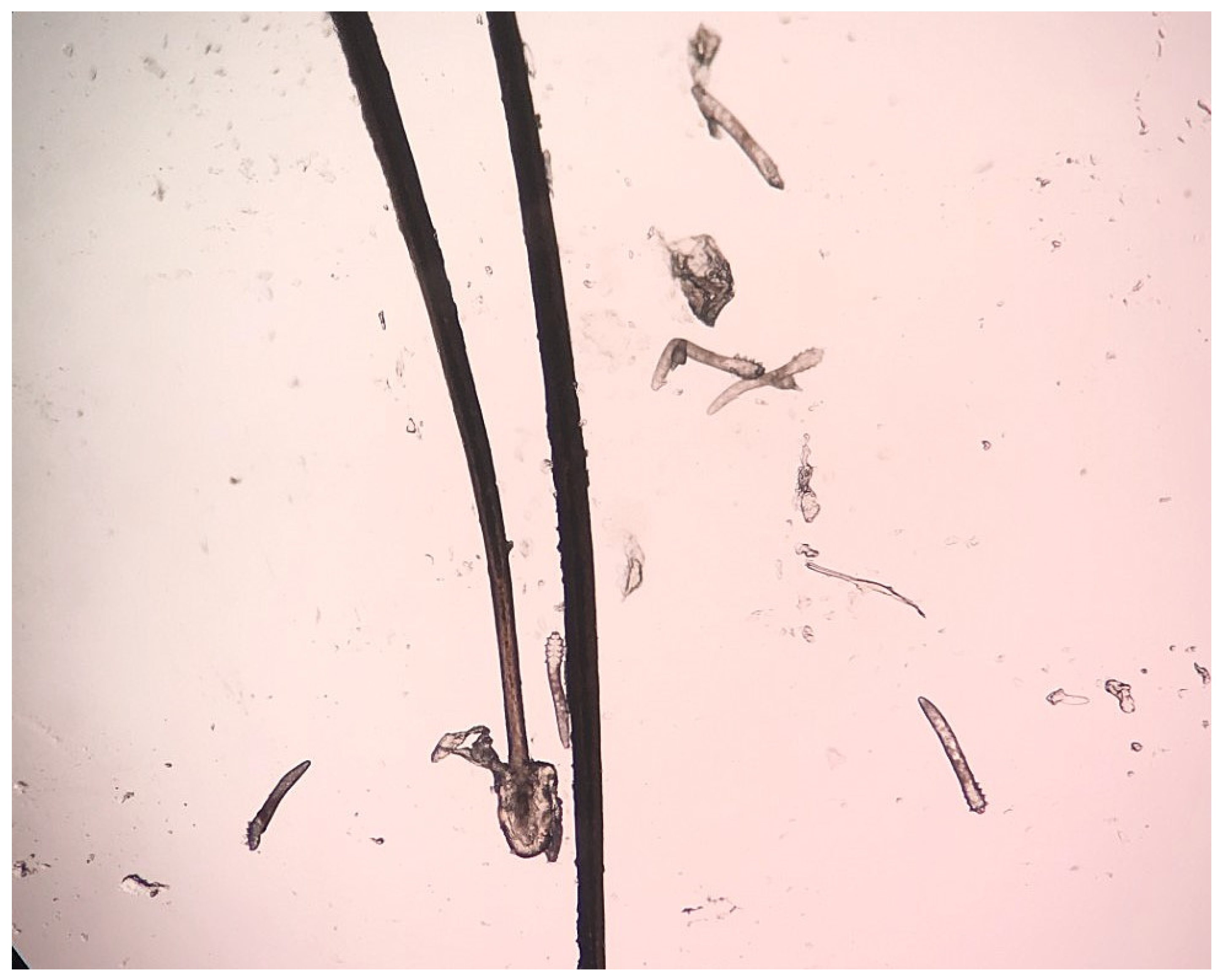
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Luo, X.; Li, J.; Chen, C.; Tseng, S.; Liang, L. Ocular demodicosis as a potential cause of ocular surface inflammation. Cornea 2017, 36, S9–S14. [Google Scholar] [CrossRef] [PubMed]
- Fromstein, S.R.; Harthan, J.S.; Patel, J.; Opitz, D.L. Demodex blepharitis: Clinical perspectives. Clin. Optom. 2018, 10, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Rhee, M.K.; Yeu, E.; Barnett, M.; Rapuano, C.J.; Dhaliwal, D.K.; Nichols, K.K.; Karpecki, P.; Mah, F.S.; Chan, A.; Mun, J.; et al. Demodex blepharitis: A comprehensive review of the disease, current management, and emerging therapies. Eye Contact Lens 2023, 49, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Rusiecka-Ziolkowska, J.; Nokiel, M.; Fleischer, M. Demodex—An old pathogen or a new one? Adv. Clin. Exp. Med. 2014, 23, 295–298. [Google Scholar] [CrossRef]
- Rather, P.A.; Hassan, I. Human Demodex mite: The versatile mite of dermatological importance. Indian J. Dermatol. 2014, 59, 60–66. [Google Scholar] [CrossRef]
- Toka Özer, T.; Akyürek, Ö.; Durmaz, S. Association between Demodex folliculorum and metabolic Syndrome. J. Cosmet. Dermatol. 2020, 19, 3145–3149. [Google Scholar] [CrossRef]
- Cheng, A.M.; Hwang, J.; Dermer, H.; Galor, A. Prevalence of ocular demodicosis in an older population and its association with symptoms and signs of dry eye. Cornea 2021, 40, 995–1001. [Google Scholar] [CrossRef]
- Li, J.; Luo, X.; Liao, Y.; Liang, L. Age differences in ocular demodicosis: Demodex profiles and clinical manifestations. Ann. Transl. Med. 2021, 9, 791. [Google Scholar] [CrossRef]
- Aydin, E.; Demir, H.D.; Demirturk, F.; Caliskan, A.C.; Aytan, H.; Erkorkmaz, U. Corneal topographic changes in premenopausal and postmenopausal women. BMC Ophthalmol. 2007, 7, 9. [Google Scholar] [CrossRef]
- Birgul, R.; Turan, G. Comparison of changes in eye findings of premenopausal and postmenopausal women. Cureus 2021, 13, e14319. [Google Scholar] [CrossRef]
- Truong, S.; Cole, N.; Stapleton, F.; Golebiowski, B. Sex hormones and the dry eye. Clin. Exp. Optom. 2014, 97, 324–336. [Google Scholar] [CrossRef] [PubMed]
- Sędzikowska, A.; Oseka, M.; Grytner-Ziecina, B. Ocular symptoms reported by patients infested with Demodex mites. Acta Parasitol. 2016, 61, 808–814. [Google Scholar] [CrossRef] [PubMed]
- Szkup, M.; Owczarek, A.J.; Schneider-Matyka, D.; Brodowski, J.; Łój, B.; Grochans, E. Associations between the components of metabolic syndrome and the polymorphisms in the peroxisome proliferator-activated receptor gamma (PPAR-γ), the fat mass and obesity-associated (FTO), and the melanocortin-4 receptor (MC4R) genes. Aging 2018, 10, 72–82. [Google Scholar] [CrossRef] [PubMed]
- Desch, C.; Nutting, W.B. Demodex folliculorum (Simons) and Demodex brevis Akbulatova of man: Redescription and reevaluation. J. Parasitol. 1972, 58, 169–177. [Google Scholar] [CrossRef]
- Lee, S.H.; Chun, Y.S.; Kim, J.H.; Kim, E.S.; Kim, J.C. The relationship between Demodex and ocular discomfort. Investig. Ophthalmol. Vis. Sci. 2010, 51, 2906–2911. [Google Scholar] [CrossRef]
- Chudzicka-Strugała, I.; Gołębiewska, I.; Brudecki, G.; Elamin, W.; Zwoździak, B. Demodicosis in different age groups and alternative treatment options—A review. J. Clin. Med. 2023, 12, 1649. [Google Scholar] [CrossRef]
- Zeytun, E.; Karakurt, Y. Prevalence and load of Demodex folliculorum and Demodex brevis (Acari: Demodicidae) in patients with chronic blepharitis in the province of Erzincan, Turkey. J. Med. Entomol. 2019, 56, 2–9. [Google Scholar] [CrossRef]
- Enginyurt, O.; Karaman, U.; Cetin, F.; Ozer, A. The prevalence of Demodex species and its relationship with the metabolic syndrome in women of Malatya Province, Turkey. Jundishapur J. Microbiol. 2015, 8, e24322. [Google Scholar] [CrossRef]
- Kemal, M.; Sümer, Z.; Toker, M.I.; Erdoğan, H.; Topalkara, A.; Akbulut, M. The prevalence of Demodex folliculorum in blepharitis patients and the normal population. Ophthalmic Epidemiol. 2005, 12, 287–290. [Google Scholar] [CrossRef]
- Lacey, N.; Kavanagh, K.; Tseng, S.C. Under the lash: Demodex mites in human diseases. Biochemist 2009, 31, 2–6. [Google Scholar] [CrossRef]
- Liu, J.; Sheha, H.; Tseng, S.C. Pathogenic role of Demodex mites in blepharitis. Curr. Opin. Allergy Clin. Immunol. 2010, 10, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Wesolowska, M.; Knysz, B.; Reich, A.; Blazejewska, D.; Czarnecki, M.; Gladysz, A.; Pozowski, A.; Misiuk-Hojlo, M. Prevalence of Demodex spp. in eyelash follicles in different populations. Arch. Med. Sci. 2014, 10, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Bohdanowicz, D.; Raszeja-Kotelba, B. Demodex in the pathogenesis of certain skin diseases. Post Dermatol. Alergol. 2001, 18, 51–53. [Google Scholar]
- Zhong, J.; Tan, Y.; Li, S.; Peng, L.; Wang, B.; Deng, Y.; Yuan, J. The Prevalence of Demodex folliculorum and Demodex brevis in cylindrical dandruff patients. J. Ophthalmol. 2019, 2019, 8949683. [Google Scholar] [CrossRef]
- Gao, Y.Y.; Di Pascuale, M.A.; Elizondo, A.; Tseng, S.C. Clinical treatment of ocular demodecosis by lid scrub with tea tree oil. Cornea 2007, 26, 136–143. [Google Scholar] [CrossRef]
- Biernat, M.M.; Rusiecka-Ziółkowska, J.; Piątkowska, E.; Helemejko, I.; Biernat, P.; Gościniak, G. Occurrence of Demodex species in patients with blepharitis and in healthy individuals: A 10-year observational study. Jpn. J. Ophthalmol. 2018, 62, 628–633. [Google Scholar] [CrossRef]

| Group | Number/% of Infected Women | |||
|---|---|---|---|---|
| Demodex spp. | D. folliculorum | D. brevis | Coinfection of D. folliculorum and D. brevis | |
| pre- and perimenopausal women (n = 253) | 75/29.64 | 72/28.45 | 1/0.40 | 2/0.79 |
| young women (n = 204) | 25/12.25 | 25/12.25 | 0 | 0 |
| χ2 test value | χ2 = 20.0; p < 0.001 | χ2 = 20.8; p < 0.001 | ||
| Group | The Intensity of Demodex spp. Infestation | ||
|---|---|---|---|
| Low | Medium | High | |
| pre- and perimenopausal women | 56/74.67% | 13/17.33% | 6/8.0% |
| young women | 19/76.0% | 4/16.0% | 2/8.0% |
| χ2 test or Fisher’s Exact Test p value | p = 0.87 | p = 0.88 | p = 1.00 |
| Symptoms | Uninfected | Infected | χ2 Test Value | |||
|---|---|---|---|---|---|---|
| Total | The Intensity of Demodex spp. Infestation | |||||
| Low | Medium | High | ||||
| itching, n (%) | 102 (57.30) | 47 (62.67) | 33 (70.21) | 10 (21.28) | 4 (8.51) | χ2 = 0.63; p = 0.43 |
| tearing, n (%) | 61 (34.27) | 36 (48.00) | 31 (86.11) | 3 (8.33) | 2 (5.56) | χ2 = 4.21; p = 0.04 |
| redness, n (%) | 30 (16.85) | 23 (30.67) | 16 (69.57) | 5 (21.74) | 2 (8.70) | χ2 = 6.08; p = 0.01 |
| dryness of the eyes, n (%) | 40 (22.47) | 27 (36.00) | 24 (88.89) | 2 (7.41) | 1 (3.70) | χ2 = 4.96; p = 0.03 |
| foreign body sensation, n (%) | 26 (14.61) | 14 (18.67) | 12 (85.71) | 1 (7.14) | 1 (7.14) | χ2 = 0.65; p = 0.42 |
| eyelash loss, n (%) | 9 (5.06) | 6 (8.00) | 4 (66.67) | 1 (16.67) | 1 (16.67) | χ2 = 0.82; p = 0.37 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kosik-Bogacka, D.; Łanocha-Arendarczyk, N.; Pilarczyk, R.; Schneider-Matyka, D.; Kot, K.; Grzeszczak, K.; Pyzia, J.; Grochans, E. Ocular Symptoms in Pre- and Perimenopausal Woman Infected with Demodex spp. Pathogens 2025, 14, 297. https://doi.org/10.3390/pathogens14030297
Kosik-Bogacka D, Łanocha-Arendarczyk N, Pilarczyk R, Schneider-Matyka D, Kot K, Grzeszczak K, Pyzia J, Grochans E. Ocular Symptoms in Pre- and Perimenopausal Woman Infected with Demodex spp. Pathogens. 2025; 14(3):297. https://doi.org/10.3390/pathogens14030297
Chicago/Turabian StyleKosik-Bogacka, Danuta, Natalia Łanocha-Arendarczyk, Renata Pilarczyk, Daria Schneider-Matyka, Karolina Kot, Konrad Grzeszczak, Joanna Pyzia, and Elżbieta Grochans. 2025. "Ocular Symptoms in Pre- and Perimenopausal Woman Infected with Demodex spp." Pathogens 14, no. 3: 297. https://doi.org/10.3390/pathogens14030297
APA StyleKosik-Bogacka, D., Łanocha-Arendarczyk, N., Pilarczyk, R., Schneider-Matyka, D., Kot, K., Grzeszczak, K., Pyzia, J., & Grochans, E. (2025). Ocular Symptoms in Pre- and Perimenopausal Woman Infected with Demodex spp. Pathogens, 14(3), 297. https://doi.org/10.3390/pathogens14030297







