Patients with Newly Diagnosed Cervical Cancer Should Be Screened for Anal Human Papillomavirus (HPV) and Anal Dysplasia: Results of Cost and Quality Analysis
Abstract
1. Introduction
2. Methods
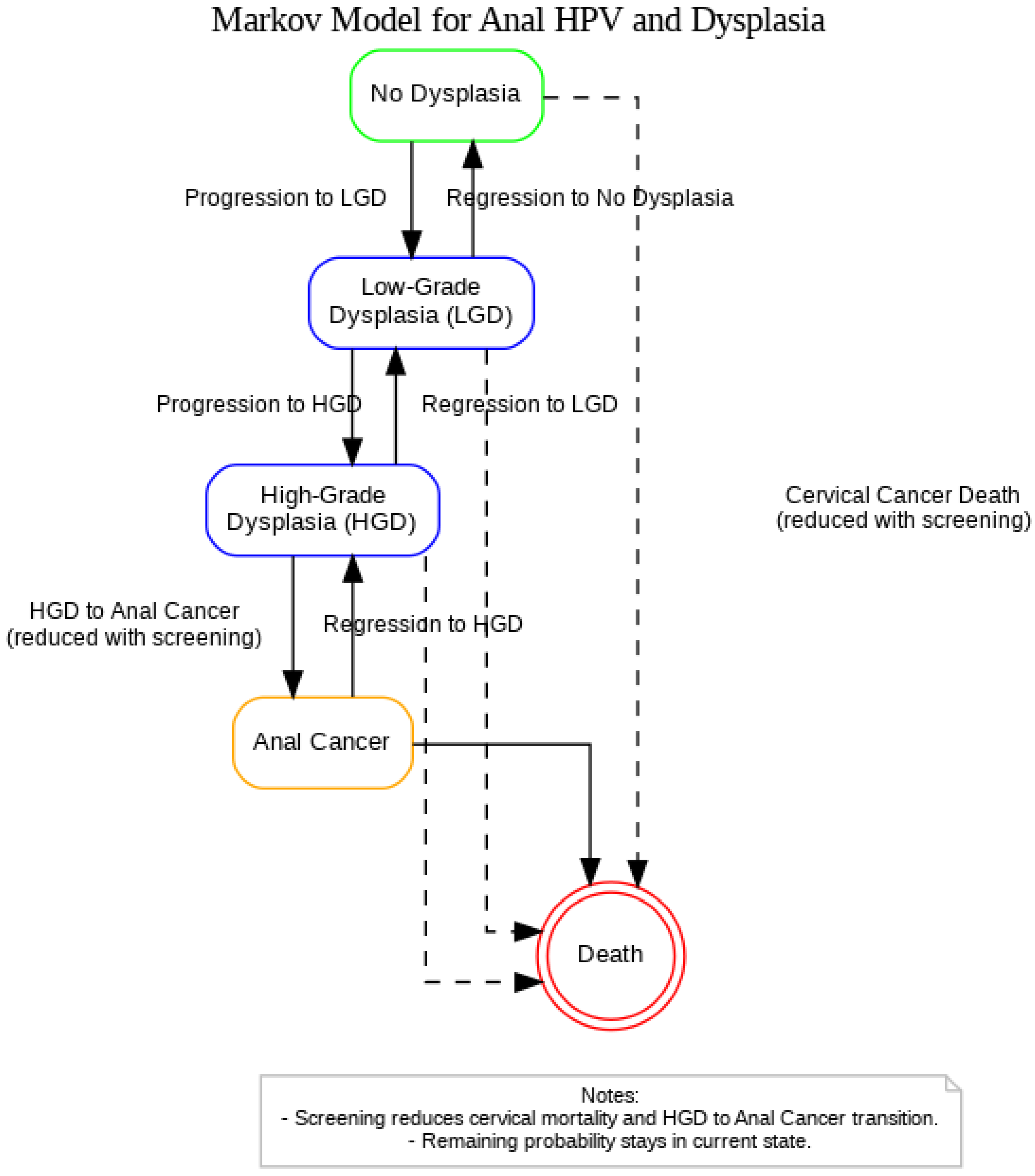
2.1. Model Development
2.2. Cost Analysis
2.3. Sensitivity Analysis
2.4. Outcomes Determined from the Model
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Milner, D.A. Diagnostic Pathology: Infectious Diseases; Elsevier Health Sciences: Amsterdam, The Netherlands, 2015; p. 40. ISBN 978-0-323-40037-4. [Google Scholar]
- American Cancer Society. Cancer Statistics Center. Available online: https://cancerstatisticscenter.cancer.org/ (accessed on 16 July 2025).
- Hernandez, B.Y.; McDuffie, K.; Zhu, X.; Wilkens, L.R.; Killeen, J.; Kessel, B.; Wakabayashi, M.T.; Bertram, C.C.; Easa, D.; Ning, L.; et al. Anal human papillomavirus infection in women and its relationship with cervical infection. Cancer Epidemiol. Biomark. Prev. 2005, 14, 2550–2556. [Google Scholar] [CrossRef]
- Stier, E.A.; Clarke, M.A.; Deshmukh, A.A.; Wentzensen, N.; Liu, Y.; Poynten, I.M.; Cavallari, E.N.; Fink, V.; Barroso, L.F.; Clifford, G.M.; et al. The International Anal Neoplasia Society’s consensus guidelines for anal cancer screening. Int. J. Cancer 2024, 154, 1694–1702. [Google Scholar] [CrossRef]
- Goldie, S.J.; Kuntz, K.M.; Weinstein, M.C.; Freedberg, K.A.; Welton, M.L.; Palefsky, J.M. The Clinical Effectiveness and Cost-effectiveness of Screening for Anal Squamous Intraepithelial Lesions in Homosexual and Bisexual HIV-Positive Men. JAMA 1999, 281, 1822–1829. [Google Scholar] [CrossRef]
- Robinson, A.; Ehrenpreis, E.; Dang, N.; Virdi, R.; Lafazanos, Y. Analysis of temporal trends in anal cancer incidence by sex, age, and ethnicity, 2017–2021. In Proceedings of the Scientific Day, Advocate Aurora Health, Park Ridge, IL, USA, 21 May 2025. [Google Scholar]
- Bala, M.V.; Mauskopf, J.A. Optimal assignment of treatments to health states using a Markov decision model: An introduction to basic concepts. Pharmacoeconomics 2006, 24, 345–354. [Google Scholar] [CrossRef]
- Sehnal, B.; Dusek, L.; Cibula, D.; Zima, T.; Halaska, M.; Driak, D.; Slama, J. The relationship between the cervical and anal HPV infection in women with cervical intraepithelial neoplasia. J. Clin. Virol. 2014, 59, 18–23. [Google Scholar] [CrossRef]
- American Cancer Society. Key Statistics for Cervical Cancer. American Cancer Society. 2025. Available online: https://www.cancer.org/cancer/types/cervical-cancer/about/key-statistics.html (accessed on 16 July 2025).
- Cronin, B.; Bregar, A.; Luis, C.; Schechter, S.; DiSilvestro, P.; Pisharodi, L.; Sung, C.J.; Raker, C.; Clark, M.; Robison, K. Evaluation of anal cytology and dysplasia in women with a history of lower genital tract dysplasia and malignancy. Gynecol. Oncol. 2016, 141, 492–496. [Google Scholar] [CrossRef]
- Oon, S.-F.; Winter, D.C. Perianal condylomas, anal squamous intraepithelial neoplasms and screening: A review of the literature. J. Med. Screen. 2010, 17, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Palefsky, J.M.; Lee, J.Y.; Jay, N.; Goldstone, S.E.; Darragh, T.M.; Dunlevy, H.A.; Palefsky, J.M. Treatment of anal high-grade squamous intraepithelial lesions to prevent anal cancer. N. Engl. J. Med. 2022, 386, 2273–2282. [Google Scholar] [CrossRef] [PubMed]
- Goldstone, S.E.; Uronis, H.E.; Deshmukh, A.A. Long-term outcomes of adding HPV vaccine to the anal intraepithelial neoplasia treatment regimen in HIV-positive men who have sex with men. Clin. Infect. Dis. 2015, 61, 1527–1535. [Google Scholar] [CrossRef]
- National Cancer Institute. SEER Cancer Stat Facts: Anus, Anal Canal and Anorectum Cancer. Surveillance, Epidemiology, and End Results Program. Available online: https://seer.cancer.gov/statfacts/html/anus.html (accessed on 15 July 2025).
- National Cancer Institute. SEER Cancer Stat Facts: Cervix Uteri Cancer. Surveillance, Epidemiology, and End Results Program. Available online: https://seer.cancer.gov/statfacts/html/cervix.html (accessed on 16 July 2025).
- Social Security Administration. Actuarial Life Table, 2022, as Used in the 2025 Trustees Report. 2025. Available online: https://www.ssa.gov/oact/STATS/table4c6.html (accessed on 16 July 2025).
- Meunning, B.P. Cost-Effectiveness Analysis in Health, 3rd ed.; John Wiley & Sons: San Francisco, CA, USA, 2016. [Google Scholar]
- Owens, D.K. Interpretation of cost-effectiveness analyses. J. Gen. Intern. Med. 1998, 13, 716–717. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare; Medicaid Services. Physician Fee Schedule Overview. Available online: https://www.cms.gov/medicare/physician-fee-schedule/search/overview (accessed on 5 July 2025).
- Deshmukh, A.A.; Chiao, E.Y.; Das, P.; Cantor, S.B.; Shete, S. Healthcare costs associated with anal cancer treatment: Evidence from a U.S. commercially insured population. Cancer Med. 2023, 12, 16923–16931. [Google Scholar] [CrossRef]
- Ehrenpreis, E.D.; Smith, D.G. Patients with newly diagnosed cervical cancer should be screened for anal human papilloma virus and anal dysplasia: Results of a pilot study using a STELLA computer simulation and economic model. Papillomavirus Res. 2018, 5, 38–45. [Google Scholar] [CrossRef]
- Shvetsov, Y.B.; Hernandez, B.Y.; McDuffie, K.; Wilkens, L.R.; Zhu, X.; Ning, L.; Killeen, J.; Kamemoto, L.; Goodman, M.T. Duration and clearance of anal human papillomavirus (HPV) infection among women: The Hawaii HPV cohort study. Clin. Infect. Dis. 2009, 48, 536–546. [Google Scholar] [CrossRef] [PubMed]
- US Bureau of Labor Statistics. Consumer Price Index (CPI). U.S. Department of Labor. Available online: https://www.bls.gov/cpi/ (accessed on 16 July 2025).
- Sauter, C.; Peeken, J.C.; Borm, K.; Diehl, C.; Münch, S.; Combs, S.E.; Dapper, H. Quality of life in patients treated with radiochemotherapy for primary diagnosis of anal cancer. Sci. Rep. 2022, 12, 4416. [Google Scholar] [CrossRef] [PubMed]
- Cooley, J.J.P.; Maguire, F.B.; Morris, C.R.; Parikh-Patel, A.; Abrahão, R.; Chen, H.A.; Keegan, T.H.M. Cervical cancer stage at diagnosis and survival among women ≥65 years in California. Cancer Epidemiol. Biomark. Prev. 2023, 32, 91–97. [Google Scholar] [CrossRef] [PubMed]
- American Association for Cancer Research. Cervical cancer stage at diagnosis and survival. Cancer Epidemiol. Biomark. Prev. 2023, 32, 91. [Google Scholar] [CrossRef]
- Sunesen, K.G.; Nørgaard, M.; Thorlacius-Ussing, O.; Laurberg, S. Immunosuppressive disorders and risk of anal squamous cell carcinoma: A nationwide cohort study in Denmark, 1978–2005. Int. J. Cancer 2010, 127, 675–684. [Google Scholar] [CrossRef]
- Silverstein, M.D.; Loftus, E.V.; Sandborn, W.J.; Tremaine, W.J.; Feagan, B.G.; Nietert, P.J.; Harmsen, W.S.; Zinsmeister, A.R. Clinical course and costs of care for Crohn’s disease: Markov model analysis of a population-based cohort. Gastroenterology 1999, 117, 49–57. [Google Scholar] [CrossRef]
- National Center for Biotechnology Information. Anal Cancer. In StatPearls; StatPearls Publishing: Tampa/St. Petersburg, FL, USA, 2019. Available online: https://www.ncbi.nlm.nih.gov/books/NBK543650/ (accessed on 16 July 2025).
- Gosens, K.C.; Richel, O.; Prins, J.M. Human papillomavirus as a cause of anal cancer and the role of screening. Curr. Opin. Infect. Dis. 2017, 30, 87–92. [Google Scholar] [CrossRef]
- Slama, J.; Sehnal, B.; Dusek, L.; Zima, T.; Cibula, D. Impact of risk factors on prevalence of anal HPV infection in women with simultaneous cervical lesion. Neoplasma 2015, 62, 308–314. [Google Scholar] [CrossRef]
- UK National Screening Committee. Criteria for Appraising the Viability Effectiveness Appropriateness of a Screening Programme, GOV. UK. Available online: https://www.gov.uk/government/publications/evidence-review-criteria-national-screening-programmes/criteria-for-appraising-the-viability-effectiveness-and-appropriateness-of-a-screening-programme (accessed on 29 September 2022).
- Scholefield, J.H.; Nugent, K.P. Anal Cancer: Position Statement of the Association of Coloproctology of Great Britain and Ireland. Color. Dis. 2011, 13 (Suppl. 1), 1–52. [Google Scholar] [CrossRef]
- Li, Y.; Pan, Q.; Li, Y.; Tang, L.; Ren, R. Chinese expert consensus on diagnosis and treatment of anal cancer. Glob. Community Med. 2024, 4, e000013. [Google Scholar] [CrossRef]
- Marks, D.K.; Goldstone, S.E. Electrocautery ablation of high-grade anal squamous intraepithelial lesions in HIV-negative and HIV-positive men who have sex with men. J. Acquir. Immune Defic. Syndr. 2012, 59, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Pineda, C.E.; Berry, J.M.; Jay, N.; Palefsky, J.M.; Welton, M.L. High-resolution anoscopy targeted surgical destruction of anal high-grade squamous intraepithelial lesions: A ten-year experience. Dis. Colon Rectum 2008, 51, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Benevolo, M.; Donà, M.G.; Ravenda, P.S.; Chiocca, S. Anal human papillomavirus infection: Prevalence, diagnosis and treatment of related lesions. Expert Rev. Anti-Infect. Ther. 2016, 14, 465–477. [Google Scholar] [CrossRef] [PubMed]
| Annual incidence of cervical cancer in the US attributable to HPV | 13,820 [2] |
| % of women with a history of cervical high-grade dysplasia or microinvasive cancer with anal HPV | 48.3% [8] |
| Total number of women with a history of cervical high-grade dysplasia or microinvasive cancer with anal HPV | 5550 |
| Average age at time of diagnosis of cervical cancer | 50 [9] |
| % of women with a history of genital cancer initially having anal ASC-US | 19.4% [10] |
| % of women with a history of cervical cancer initially having no anal dysplasia | 50.8% [10] |
| % of women with a history of high-grade cervical cytology initially having anal low-grade dysplasia | 16% [10] |
| % of women with a history of genital cancer initially having anal high-grade dysplasia | 3% [10] |
| % of women with anal HPV and no dysplasia that develop high-grade dysplasia over two years | 8% [11] |
| % of women with anal HPV and low-grade dysplasia that develop high-grade dysplasia over two years | 36% [11] |
| % of women with anal HPV and ASC-US that develop high-grade dysplasia over two years | 62% [12] |
| ACUS cytology equivalents (based on 1-year follow-up cytology in MSM) | ACUS represents normal = 58%, ACUS represents LGD = 24%, ACUS represents HSIL = 18%, ACUs represents cancer = 0 [5] |
| Histological progression and regression (based on 1-year follow-up in MSM) | Progression: Normal to LGD = 1.9%, Normal to HGD = 1.78%, Normal to cancer = 0%, LGD to HGD = 16.5%, LGD to anal cancer = 0.05% (estimated), HGD to anal cancer = 3.6% Regression: LGD to normal = 22.65%, HGD to LGD = 22% (estimated), HGD to normal = 11.36% [5,13] |
| Annual anal cancer death rate | 8.96% [14] |
| Five-year anal cancer death rate | 29.4% [14] |
| Annual death rate from cervical cancer | 11.73% [15] |
| Five-year death rate from cervical cancer | 32.6% [15] |
| Average life expectancy for a female age 49 | 32.95 [16] |
| Quality of life weight adjustment for anal cancer | 0.56 [5] |
| Quality of life weight adjustment after treatment for anal HGD | 0.9 [5] |
| Quality of life weight adjustment for cervical cancer | 0.7 [17] |
| Quality-adjusted life expectancy woman age 49 | 21.6 [18] |
| Quality-adjusted life expectancy woman age 49 surviving cervical cancer | 21.6 × 0.7 = 15.12 |
| Quality-adjusted life expectancy woman age 49 surviving cervical cancer treated for anal HGD | 15.1 × 0.9 = 13.6 |
| Cost of HPV screen * | USD 104 [19] |
| Cost of anal cytology * | USD 72 [19] |
| Cost of treatment of anal HGD * | USD 281 [19] |
| Cost of high-resolution anoscopy and biopsy * | USD 288 [19] |
| Cost of anal cancer treatment * | USD 150,000 [20] |
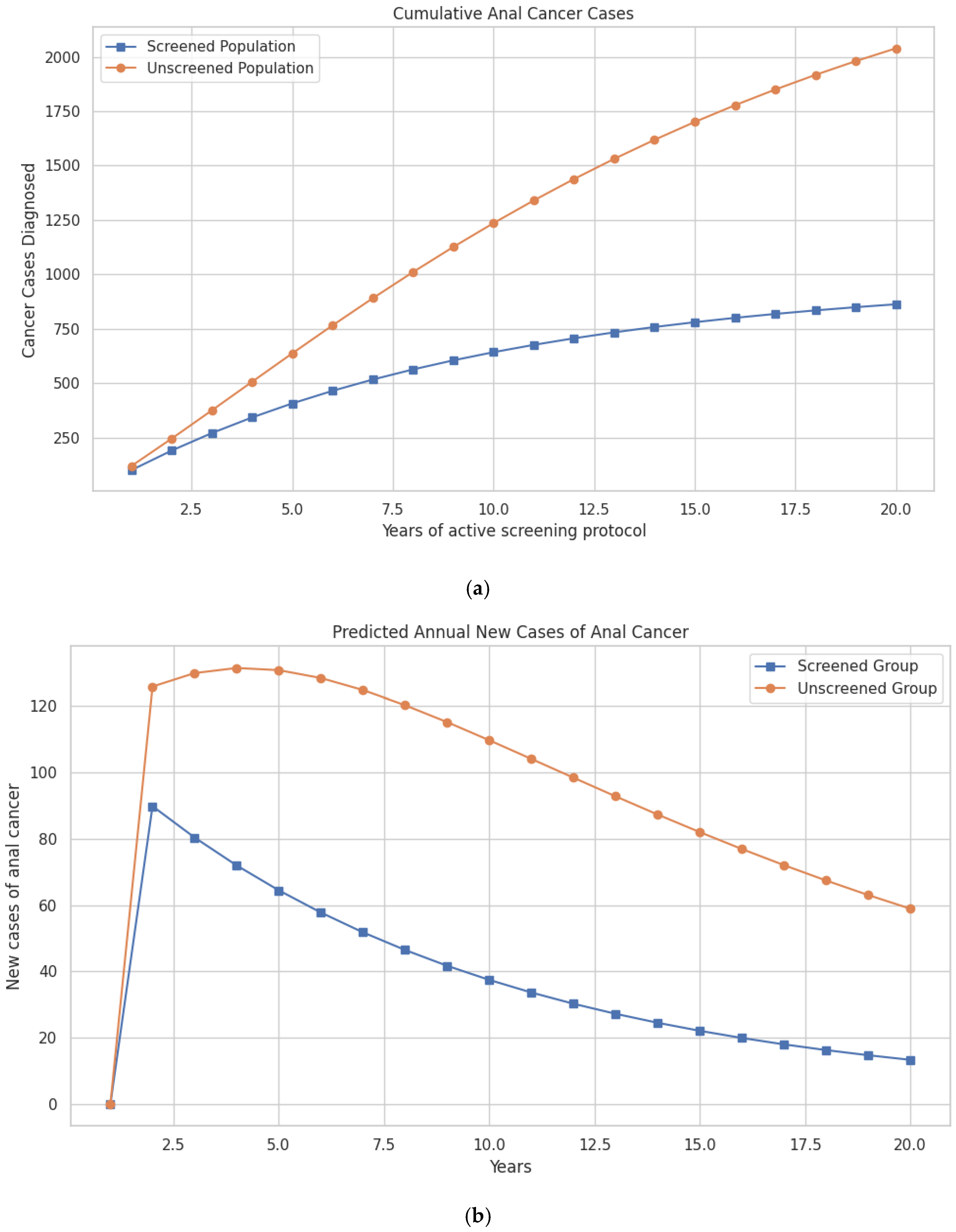
| Year | Anal Cancers (Unscreened) | Anal Cancers (Screened) | Cancer Deaths (Unscreened) | Cancer Deaths (Screened) |
|---|---|---|---|---|
| 1 | 119 | 101 | 356 | 182 |
| 2 | 295 | 199 | 1045 | 399 |
| 3 | 373 | 271 | 2036 | 1066 |
| 4 | 507 | 343 | 3338 | 1706 |
| 5 | 637 | 407 | 4704 | 2605 |
| 6 | 791 | 460 | 5787 | 3476 |
| 7 | 891 | 505 | 6787 | 4755 |
| 8 | 1011 | 563 | 11,076 | 6048 |
| 9 | 1136 | 603 | 13,657 | 7428 |
| 10 | 1236 | 646 | 16525 | 9074 |
| 11 | 1340 | 676 | 19,179 | 10751 |
| 12 | 1438 | 702 | 21,919 | 12,954 |
| 13 | 1510 | 729 | 24,729 | 14,984 |
| 14 | 1618 | 758 | 28,744 | 16,544 |
| 15 | 1740 | 780 | 29,744 | 18,614 |
| 16 | 1817 | 803 | 33,147 | 20,039 |
| 17 | 1919 | 830 | 37947 | 22967 |
| 18 | 1987 | 855 | 43,447 | 25,856 |
| 19 | 1809 | 879 | 48,987 | 28,439 |
| 20 | 2039 | 863 | 51,553 | 31,115 |
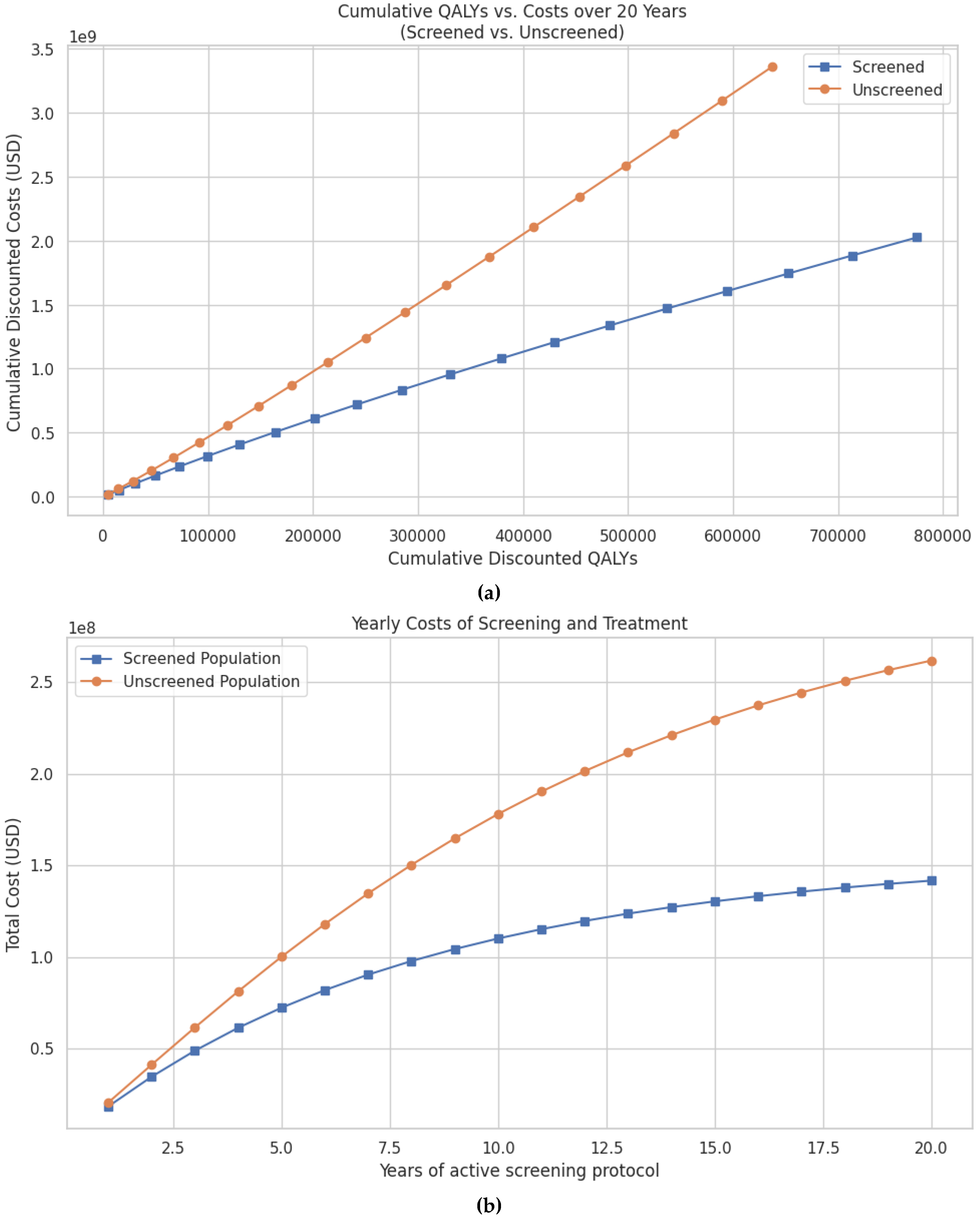
| Costs in Unscreened Group (Cancer Care Only) | Costs in Screened Group (HPV Screening, Annual Cytology, Treatment of HSIL, and Cancer Care) | Cost Difference | Cost per Anal Cancer Prevented | Cost per Anal Cancer Death Prevented | Cost per Quality-of-Life Year Saved | |
|---|---|---|---|---|---|---|
| 5 years | USD 304,498,048 | USD 235,563,777 | USD 68,934,271 | USD 120,416 | USD 12,438 | USD 12,926 |
| 10 years | USD 1050,234,416 | USD 720,133,360 | USD 330,101,055 | USD 117,506 | USD 10,640 | USD 11,830 |
| 20 years | USD 3355,123,274 | USD 2024,718,550 | USD 1330,404,723 | USD 109,222 | USD 7649 | USD 9610 |
| Cure Rate of Anal High-Grade Dysplasia | Cost per QALY Gained 5 Years | Cost per QALY Gained 10 Years | Cost per QALY Gained 20 Years |
|---|---|---|---|
| 0.38 | USD 3622.22 | USD 3049.97 | USD 2049.48 |
| 0.48 | USD 5229.36 | USD 4514.67 | USD 3289.81 |
| 0.58 | USD 6834.47 | USD 5984.13 | USD 4540.34 |
| 0.78 | USD 10,038.51 | USD 8937.30 | USD 7072.34 |
| 0.88 | USD 11,637.40 | USD 10,420.96 | USD 8354.02 |
| 0.98 | USD 13,234.15 | USD 11,909.33 | USD 9646.29 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berber, L.; Foy, O.; Cantu, J., Jr.; Ehrenpreis, E.D. Patients with Newly Diagnosed Cervical Cancer Should Be Screened for Anal Human Papillomavirus (HPV) and Anal Dysplasia: Results of Cost and Quality Analysis. Pathogens 2025, 14, 1007. https://doi.org/10.3390/pathogens14101007
Berber L, Foy O, Cantu J Jr., Ehrenpreis ED. Patients with Newly Diagnosed Cervical Cancer Should Be Screened for Anal Human Papillomavirus (HPV) and Anal Dysplasia: Results of Cost and Quality Analysis. Pathogens. 2025; 14(10):1007. https://doi.org/10.3390/pathogens14101007
Chicago/Turabian StyleBerber, Lukus, Olivia Foy, Jesus Cantu, Jr., and Eli D. Ehrenpreis. 2025. "Patients with Newly Diagnosed Cervical Cancer Should Be Screened for Anal Human Papillomavirus (HPV) and Anal Dysplasia: Results of Cost and Quality Analysis" Pathogens 14, no. 10: 1007. https://doi.org/10.3390/pathogens14101007
APA StyleBerber, L., Foy, O., Cantu, J., Jr., & Ehrenpreis, E. D. (2025). Patients with Newly Diagnosed Cervical Cancer Should Be Screened for Anal Human Papillomavirus (HPV) and Anal Dysplasia: Results of Cost and Quality Analysis. Pathogens, 14(10), 1007. https://doi.org/10.3390/pathogens14101007






