A Four-Year Study of Antibiotic Resistance, Prevalence and Biofilm-Forming Ability of Uropathogens Isolated from Community- and Hospital-Acquired Urinary Tract Infections in Southern Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Urine Specimen Collection
2.2. Bacterial Identification and Antibiotic Test
2.3. Biofilm Formation in Bacterial Isolates from Urine Samples
2.4. Data Analysis
3. Results
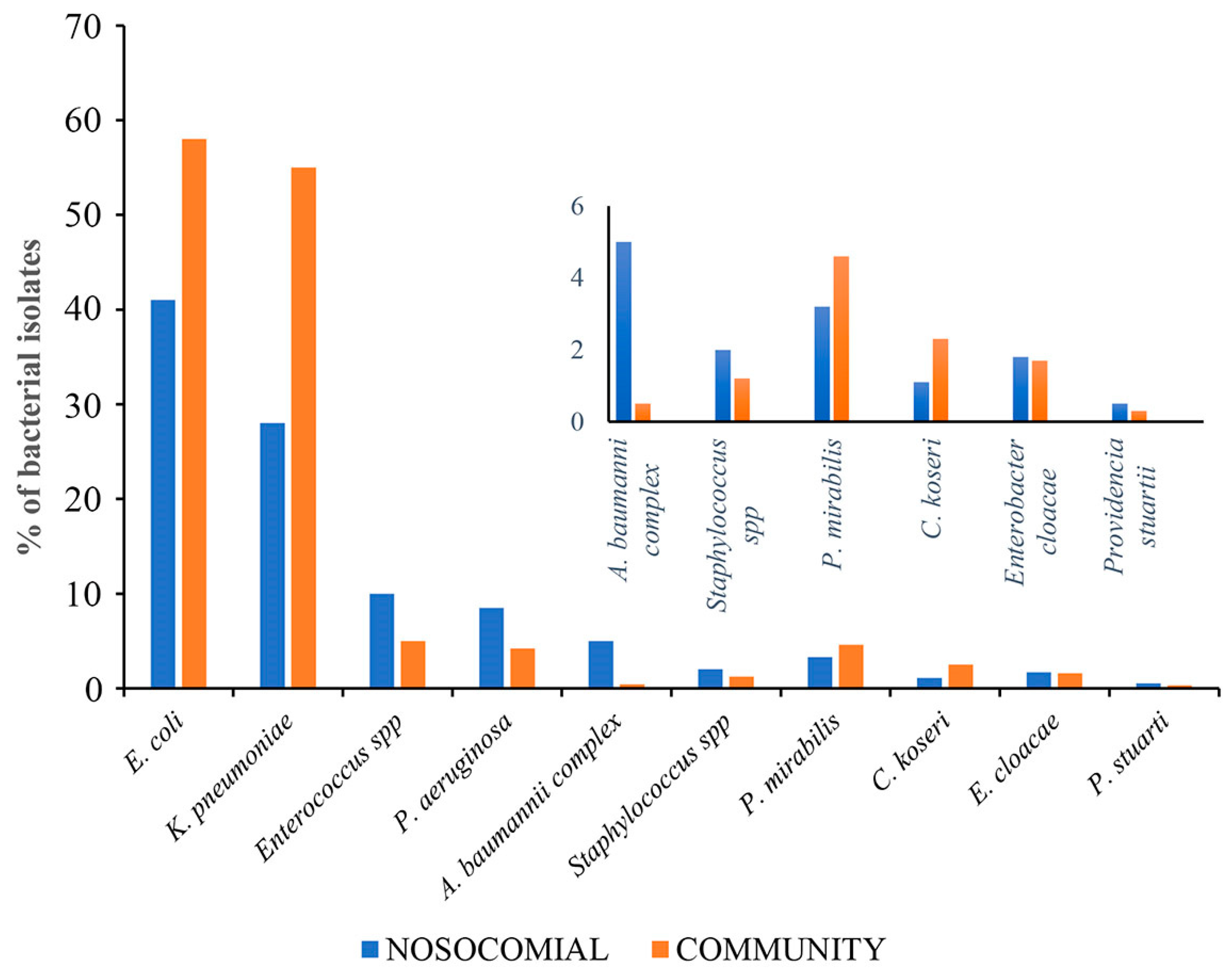
3.1. Hospital and Community Uropathogen Isolates
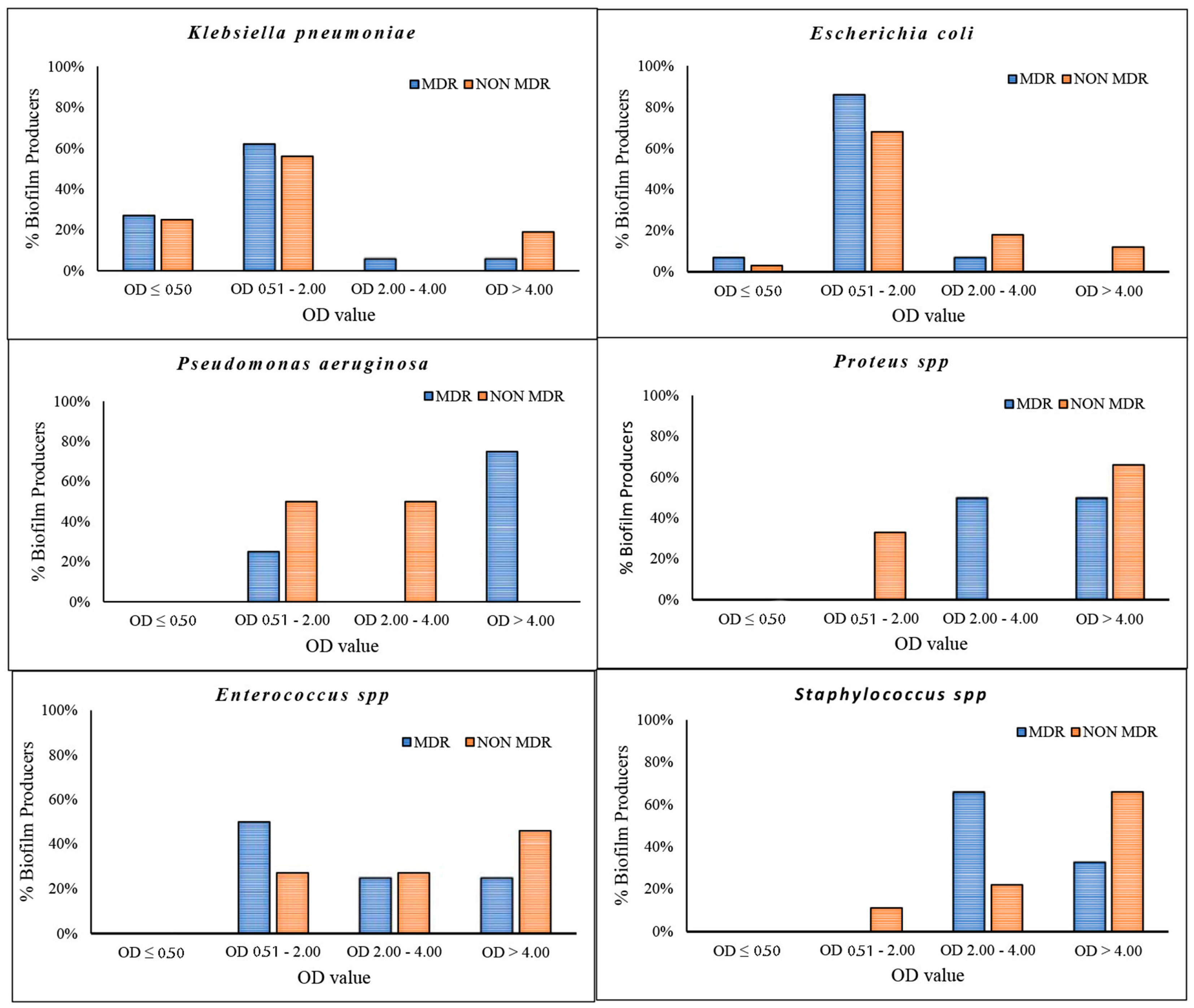
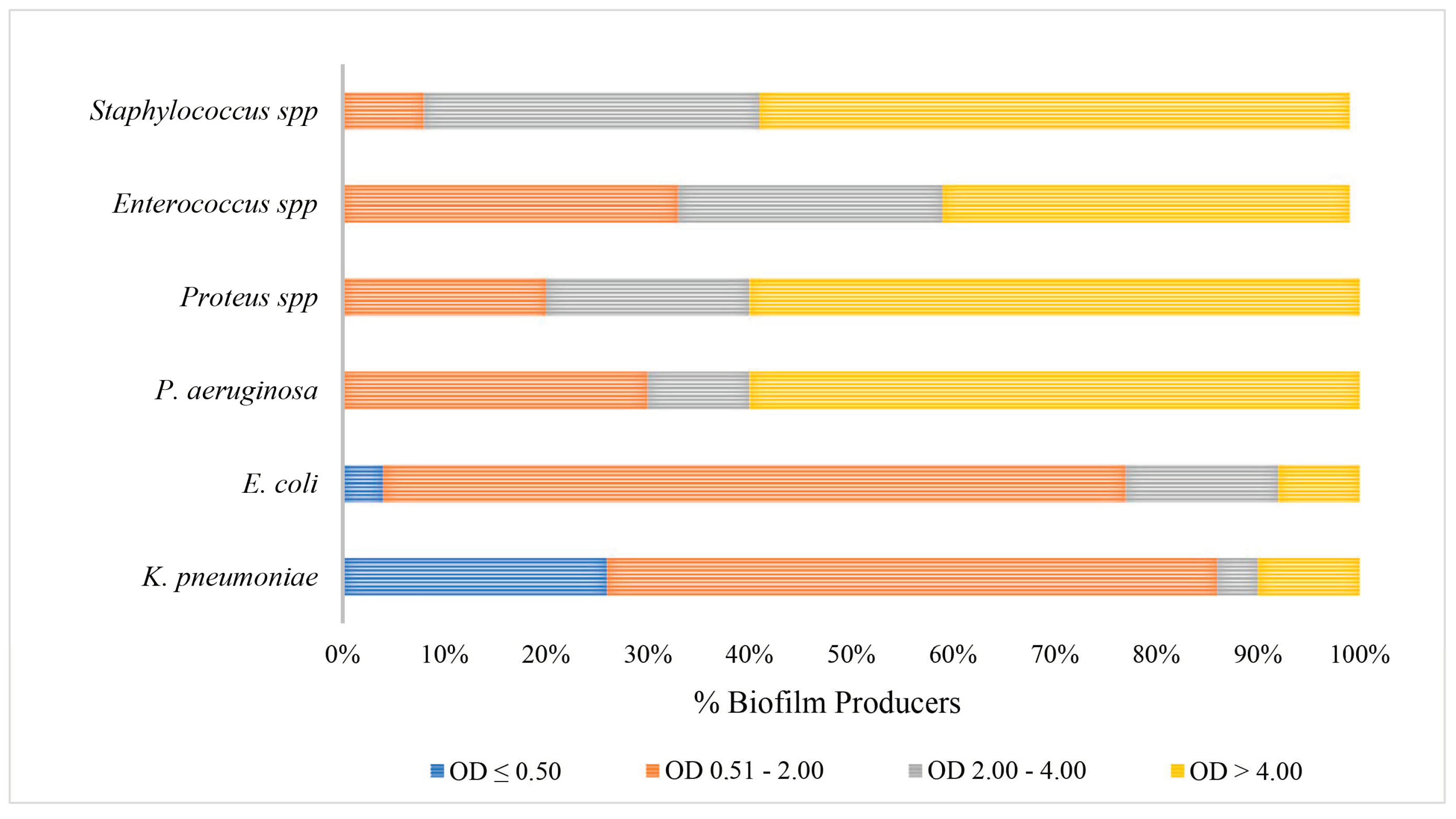
3.2. Antimicrobial Susceptibility Patterns from 2019 to 2023
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mancuso, G.; Trinchera, M.; Midiri, A.; Zummo, S.; Vitale, G.; Biondo, C. Novel Antimicrobial Approaches to Combat Bacterial Biofilms Associated with Urinary Tract Infections. Antibiotics 2024, 13, 154. [Google Scholar] [CrossRef] [PubMed]
- Truong, W.R.; Yamaki, J. Re: Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline. J. Urol. 2019, 202, 1273–1274. [Google Scholar] [CrossRef] [PubMed]
- Glover, M.; Moreira, C.G.; Sperandio, V.; Zimmern, P. Recurrent urinary tract infections in healthy and nonpregnant women. Urol. Sci. 2014, 25, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bergamin, P.A.; Kiosoglous, A.J. Surgical management of recurrent urinary tract infections: A review. Transl. Androl. Urol. 2017, 6, S153–S162. [Google Scholar] [CrossRef]
- Mancuso, G.; Midiri, A.; Gerace, E.; Marra, M.; Zummo, S.; Biondo, C. Urinary Tract Infections: The Current Scenario and Future Prospects. Pathogens 2023, 12, 623. [Google Scholar] [CrossRef] [PubMed]
- Flores-Mireles, A.L.; Walker, J.N.; Caparon, M.; Hultgren, S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015, 13, 269–284. [Google Scholar] [CrossRef] [PubMed]
- Werneburg, G.T. Catheter-Associated Urinary Tract Infections: Current Challenges and Future Prospects. Res. Rep. Urol. 2022, 14, 109–133. [Google Scholar] [CrossRef] [PubMed]
- Govindarajan, D.K.; Kandaswamy, K. Virulence factors of uropathogens and their role in host pathogen interactions. Cell Surf. 2022, 8, 100075. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhou, Z.; Zheng, L.; Gong, Z.; Li, Y.; Jin, Y.; Huang, Y.; Chi, M. Urinary Tract Infections Caused by Uropathogenic Escherichia coli: Mechanisms of Infection and Treatment Options. Int. J. Mol. Sci. 2023, 24, 10537. [Google Scholar] [CrossRef] [PubMed]
- Tiseo, G.; Brigante, G.; Giacobbe, D.R.; Maraolo, A.E.; Gona, F.; Falcone, M.; Giannella, M.; Grossi, P.; Pea, F.; Rossolini, G.M.; et al. Diagnosis and management of infections caused by multidrug-resistant bacteria: Guideline endorsed by the Italian Society of Infection and Tropical Diseases (SIMIT), the Italian Society of Anti-Infective Therapy (SITA), the Italian Group for Antimicrobial Stewardship (GISA), the Italian Association of Clinical Microbiologists (AMCLI) and the Italian Society of Microbiology (SIM). Int. J. Antimicrob. Agents 2022, 60, 106611. [Google Scholar] [CrossRef]
- van Belkum, A.; Bachmann, T.T.; Ludke, G.; Lisby, J.G.; Kahlmeter, G.; Mohess, A.; Becker, K.; Hays, J.P.; Woodford, N.; Mitsakakis, K.; et al. Developmental roadmap for antimicrobial susceptibility testing systems. Nat. Rev. Microbiol. 2019, 17, 51–62. [Google Scholar] [CrossRef]
- Sachdev, C.; Anjankar, A.; Agrawal, J. Self-Medication With Antibiotics: An Element Increasing Resistance. Cureus 2022, 14, e30844. [Google Scholar] [CrossRef] [PubMed]
- Almagor, J.; Temkin, E.; Benenson, I.; Fallach, N.; Carmeli, Y.; The DRIVE-AB Consortium. The impact of antibiotic use on transmission of resistant bacteria in hospitals: Insights from an agent-based model. PLoS ONE 2018, 13, e0197111. [Google Scholar] [CrossRef]
- Biondo, C. New Insights into the Pathogenesis and Treatment of Urinary Tract Infections. Pathogens 2023, 12, 1213. [Google Scholar] [CrossRef]
- Tang, K.W.K.; Millar, B.C.; Moore, J.E. Antimicrobial Resistance (AMR). Br. J. Biomed. Sci. 2023, 80, 11387. [Google Scholar] [CrossRef] [PubMed]
- Barchitta, M.; Quattrocchi, A.; Maugeri, A.; La Rosa, M.C.; La Mastra, C.; Sessa, L.; Cananzi, P.; Murolo, G.; Oteri, A.; Basile, G.; et al. Antibiotic Consumption and Resistance during a 3-Year Period in Sicily, Southern Italy. Int. J. Environ. Res. Public Health 2019, 16, 2253. [Google Scholar] [CrossRef] [PubMed]
- Maione, A.; Galdiero, E.; Cirillo, L.; Gambino, E.; Gallo, M.A.; Sasso, F.P.; Petrillo, A.; Guida, M.; Galdiero, M. Prevalence, Resistance Patterns and Biofilm Production Ability of Bacterial Uropathogens from Cases of Community-Acquired Urinary Tract Infections in South Italy. Pathogens 2023, 12, 537. [Google Scholar] [CrossRef]
- Gaurav, A.; Bakht, P.; Saini, M.; Pandey, S.; Pathania, R. Role of bacterial efflux pumps in antibiotic resistance, virulence, and strategies to discover novel efflux pump inhibitors. Microbiology 2023, 169, 001333. [Google Scholar] [CrossRef] [PubMed]
- Maharjan, G.; Khadka, P.; Siddhi Shilpakar, G.; Chapagain, G.; Dhungana, G.R. Catheter-Associated Urinary Tract Infection and Obstinate Biofilm Producers. Can. J. Infect. Dis. Med. Microbiol. 2018, 2018, 7624857. [Google Scholar] [CrossRef]
- Uruen, C.; Chopo-Escuin, G.; Tommassen, J.; Mainar-Jaime, R.C.; Arenas, J. Biofilms as Promoters of Bacterial Antibiotic Resistance and Tolerance. Antibiotics 2020, 10, 3. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Mohler, J.; Mahajan, S.D.; Schwartz, S.A.; Bruggemann, L.; Aalinkeel, R. Microbial Biofilm: A Review on Formation, Infection, Antibiotic Resistance, Control Measures, and Innovative Treatment. Microorganisms 2023, 11, 1614. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.; Davies, D. Origins and evolution of antibiotic resistance. Microbiol. Mol. Biol. Rev. 2010, 74, 417–433. [Google Scholar] [CrossRef] [PubMed]
- Danese, P.N. Antibiofilm approaches: Prevention of catheter colonization. Chem. Biol. 2002, 9, 873–880. [Google Scholar] [CrossRef] [PubMed]
- Kouchak, F.; Askarian, M. Nosocomial infections: The definition criteria. Iran. J. Med. Sci. 2012, 37, 72–73. [Google Scholar] [PubMed]
- Pirkani, G.S.; Awan, M.A.; Abbas, F.; Din, M. Culture and PCR based detection of bacteria causing urinary tract infection in urine specimen. Pak. J. Med. Sci. 2020, 36, 391–395. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, G.; Midiri, A.; Zummo, S.; Gerace, E.; Scappatura, G.; Biondo, C. Extended-spectrum beta-lactamase & carbapenemase-producing fermentative Gram-negative bacilli in clinical isolates from a University Hospital in Southern Italy. New Microbiol. 2021, 44, 227–233. [Google Scholar] [PubMed]
- Gaur, P.; Hada, V.; Rath, R.S.; Mohanty, A.; Singh, P.; Rukadikar, A. Interpretation of Antimicrobial Susceptibility Testing Using European Committee on Antimicrobial Susceptibility Testing (EUCAST) and Clinical and Laboratory Standards Institute (CLSI) Breakpoints: Analysis of Agreement. Cureus 2023, 15, e36977. [Google Scholar] [CrossRef] [PubMed]
- Alamri, A.; Hamid, M.E.; Abid, M.; Alwahhabi, A.M.; Alqahtani, K.M.; Alqarni, M.S.; Abomughaid, M. Trend analysis of bacterial uropathogens and their susceptibility pattern: A 4-year (2013–2016) study from Aseer region, Saudi Arabia. Urol. Ann. 2018, 10, 41–46. [Google Scholar] [CrossRef]
- Serretiello, E.; Folliero, V.; Santella, B.; Giordano, G.; Santoro, E.; De Caro, F.; Pagliano, P.; Ferro, M.; Aliberti, S.M.; Capunzo, M.; et al. Trend of Bacterial Uropathogens and Their Susceptibility Pattern: Study of Single Academic High-Volume Center in Italy (2015–2019). Int. J. Microbiol. 2021, 2021, 5541706. [Google Scholar] [CrossRef]
- Kasew, D.; Desalegn, B.; Aynalem, M.; Tila, S.; Diriba, D.; Afework, B.; Getie, M.; Biset, S.; Baynes, H.W. Antimicrobial resistance trend of bacterial uropathogens at the university of Gondar comprehensive specialized hospital, northwest Ethiopia: A 10 years retrospective study. PLoS ONE 2022, 17, e0266878. [Google Scholar] [CrossRef]
- Stepanovic, S.; Vukovic, D.; Hola, V.; Di Bonaventura, G.; Djukic, S.; Cirkovic, I.; Ruzicka, F. Quantification of biofilm in microtiter plates: Overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. J. Pathol. Microbiol. Immunol. 2007, 115, 891–899. [Google Scholar] [CrossRef]
- Christensen, G.D.; Baldassarri, L.; Simpson, W.A. Methods for studying microbial colonization of plastics. Methods Enzymol. 1995, 253, 477–500. [Google Scholar] [CrossRef] [PubMed]
- Szumilas, M. Explaining odds ratios. J. Can. Acad. Child Adolesc. Psychiatry 2010, 19, 227–229. [Google Scholar]
- Chowdhury, S.S.; Tahsin, P.; Xu, Y.; Mosaddek, A.S.M.; Muhamadali, H.; Goodacre, R. Trends in Antimicrobial Resistance of Uropathogens Isolated from Urinary Tract Infections in a Tertiary Care Hospital in Dhaka, Bangladesh. Antibiotics 2024, 13, 925. [Google Scholar] [CrossRef] [PubMed]
- Alshaikh, S.A.; El-Banna, T.; Sonbol, F.; Farghali, M.H. Correlation between antimicrobial resistance, biofilm formation, and virulence determinants in uropathogenic Escherichia coli from Egyptian hospital. Ann. Clin. Microbiol. Antimicrob. 2024, 23, 20. [Google Scholar] [CrossRef]

| Hospital | 2019 | 2020 | 2021 | 2022 | 2023 |
|---|---|---|---|---|---|
| E. coli | 220 | 121 | 160 | 138 | 173 |
| K. pneumoniae | 115 | 87 | 125 | 112 | 184 |
| P. aeruginosa | 44 | 22 | 35 | 32 | 39 |
| E. faecium | 21 | 19 | 13 | 7 | 4 |
| E. faecalis | 31 | 20 | 28 | 17 | 25 |
| Community | 2019 | 2020 | 2021 | 2022 | 2023 |
| E. coli | 140 | 77 | 94 | 107 | 149 |
| K. pneumoniae | 40 | 35 | 37 | 49 | 73 |
| P. aeruginosa | 11 | 5 | 9 | 5 | 9 |
| E. faecium | 2 | 0 | 0 | 0 | 0 |
| E. faecalis | 12 | 6 | 5 | 11 | 8 |
| (A) | ||||
|---|---|---|---|---|
| NOSOCOMIAL | E. coli | K. pneumoniae | P. aeruginosa | A. baumannii Complex |
| PENICILLIN/INHIBITOR | 31% | 66.4% | ||
| CIPROFLOXACIN | 41% | 59% | 25% | 98% |
| ESBL | 44% | 78% | ||
| PHOSFOMYCIN | 3.30% | 42% | 9.30% | |
| AMINOGLICOSIDES | 10% | 27.40% | 20% | 87% |
| IMIPENEM | 3% | 33% | 14% | 100% |
| TRIMETHOPRIM/Sulfamethoxazole | 29% | 43% | 87% | |
| PIPERICILLIN/TAZOBACTAM | 16% | |||
| TOBRAMICIN | 100% | |||
| (B) | ||||
| COMMUNITY | E. coli | K. pneumoniae | P. aeruginosa | A. baumannii Complex |
| PENICILLIN/INHIBITOR | 29% | 44% | ||
| CIPROFLOXACIN | 35% | 56% | 26% | 50% |
| ESBL | 32% | 52% | ||
| PHOSFOMYCIN | 5% | 16% | 40% | |
| AMINOGLYCOSIDES | 6.20% | 47% | 7.3% | 0 |
| IMIPENEM | 0 | 4% | 0 | 100% |
| TRIMETHOPRIM/Sulfamethoxazole | 28% | 30% | 0 | |
| PIPERICILLIN/TAZOBACTAM | 24% | |||
| TOBRAMICIN | 0 | |||
| (A) | |||||
|---|---|---|---|---|---|
| Gram-Negative Resistance | |||||
| Nosocomial | Community | ||||
| aminoglycosides | 19% | 7.3% | |||
| penicillin/inhibitor | 45% | 31% | |||
| phosfomycin | 28% | 13% | |||
| imipenem | 19% | 23% | |||
| trimethoprim/Sulfamethoxazole | 36% | 29% | |||
| ciprofloxacin | 44% | 42% | |||
| (B) | |||||
| E. coli | K. pneumoniae | P. aeruginosa | |||
| Aminoglycosydes | OR 1.141 p = 0.503 | OR 2.14 p = 0.0001 | OR 1.58 p = 0.406 | ||
| Penicillin/Inhibitor | OR 1.04 p = 0.692 | OR 2.40 p ˂ 0.0001 | OR 0.48 p = 0.256 | ||
| Phosfomycin | OR 1.211 p = 0.694 | OR 1.03 p = 0.916 | OR 2.5 p = 0.183 | ||
| Imipenem | OR 1.302 p = 0.8717 | OR 11.6 p = 0.0008 | OR 0.37 p = 0.463 | ||
| Trimethoprim/Sulfamethoxazole | OR 1.142 p = 0.395 | OR 1.84 p = 0.0036 | NA | ||
| Ciprofloxacin | OR 1.07 p = 0.629 | OR 1.93 p = 0.0008 | OR 0.537 p = 0.174 | ||
| (C) | |||||
| Klebsiella pneumoniae | |||||
| 2019 | 2020 | 2021 | 2022 | ||
| Aminoglycosides | OR 2.34 (CI 95% 1.1646–4.721) p = 0.0170 | OR 2 (IC 95% 0.8341–4.470) p = 0.1244 | OR 3.5 (IC 95% 1.3105–9.161) p = 0.0122 | OR 2 (IC 95% 0.8388–3.688) p = 0.1350 | |
| Penicillin/Inhibitor | OR 1.7 (IC 95% 0.9691–2.8937) p = 0.0647 | OR 3 (IC 95% 1.236–6.450) p = 0.0137 | OR 2.4 (IC 95% 1.2580–4.450) p = 0.0075 | OR 4 (IC 95% 1.9624–6.923) p ˂ 0.0001 | |
| Ciprofloxacin | OR 1.8 (IC 95% 0.8509–3.9918) p = 0.1210 | OR 3 (IC 95% 0.9426–6.851) p = 0.0653 | OR 3 (IC 95%1.2751–6.178) p = 0.0104 | OR 1.52 (IC 95% 0.7490–3.095) p = 0.2454 | |
| ESBL | OR 2.6 (IC 95% 1.1807–5.6576) p = 0.0175 | OR 3 (IC 95% 1.2061–7.422) p = 0.0181 | OR 2.2 (IC 95% 1.1250–4.325) p = 0.0213 | OR 3.1 (IC 95% 1.6288–6.0663) p = 0.0006 | |
| Phosfomycin | OR 0.9 (IC 95% 0.4109–1.94434) p = 0.7766 | OR 0.24 (IC 95% 0.0340–1.727) p = 0.1572 | OR 1.8 (IC 95% 0.5118–6.869) p = 0.3427 | OR 1.1 (IC 95% 0.2451–4.573) p = 0.9390 | |
| Imipenem | OR 8.2 (IC 95% 1.8226–36.726) p = 0.0063 | OR 6 (IC 95% 0.2815–113.337) p = 0.2578 | OR 8 (IC 95% 0.4417–140.495) p = 0.1603 | OR 6 (IC 95% 0.3155–106.331) p = 0.2368 | |
| Trimethoprim/ Sulfamethoxazole | OR 3.14 (IC 95% 1.2805–7.697) p = 0.0124 | OR 2.3 (IC 95% 0.8538–6.3436) p = 0.0987 | OR 1.3 (IC 95% 0.5623–2.8937) p = 0.5302 | OR 2 (IC 95% 0.8840–3.7561) p = 0.1040 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trinchera, M.; Midiri, A.; Mancuso, G.; Lagrotteria, M.A.; De Ani, C.A.; Biondo, C. A Four-Year Study of Antibiotic Resistance, Prevalence and Biofilm-Forming Ability of Uropathogens Isolated from Community- and Hospital-Acquired Urinary Tract Infections in Southern Italy. Pathogens 2025, 14, 59. https://doi.org/10.3390/pathogens14010059
Trinchera M, Midiri A, Mancuso G, Lagrotteria MA, De Ani CA, Biondo C. A Four-Year Study of Antibiotic Resistance, Prevalence and Biofilm-Forming Ability of Uropathogens Isolated from Community- and Hospital-Acquired Urinary Tract Infections in Southern Italy. Pathogens. 2025; 14(1):59. https://doi.org/10.3390/pathogens14010059
Chicago/Turabian StyleTrinchera, Marilena, Angelina Midiri, Giuseppe Mancuso, Maria Antonietta Lagrotteria, Carmelo Antonio De Ani, and Carmelo Biondo. 2025. "A Four-Year Study of Antibiotic Resistance, Prevalence and Biofilm-Forming Ability of Uropathogens Isolated from Community- and Hospital-Acquired Urinary Tract Infections in Southern Italy" Pathogens 14, no. 1: 59. https://doi.org/10.3390/pathogens14010059
APA StyleTrinchera, M., Midiri, A., Mancuso, G., Lagrotteria, M. A., De Ani, C. A., & Biondo, C. (2025). A Four-Year Study of Antibiotic Resistance, Prevalence and Biofilm-Forming Ability of Uropathogens Isolated from Community- and Hospital-Acquired Urinary Tract Infections in Southern Italy. Pathogens, 14(1), 59. https://doi.org/10.3390/pathogens14010059






