Abstract
Introduction: Acute kidney disease and chronic kidney disease are considered conditions that can increase the mortality and severity of COVID-19. However, few studies have investigated the impact of creatinine levels on COVID-19 progression in patients without a history of chronic kidney disease. The aim of the study was to assess the impact of creatinine levels at hospital admission on COVID-19 progression and mortality. Methods: We performed a multicenter, observational, retrospective study involving seventeen COVID-19 Units in the Campania region in southern Italy. All adult (≥18 years) patients, hospitalized with a diagnosis of SARS-CoV-2 infection confirmed by a positive reverse transcriptase-polymerase chain reaction on a naso-oropharyngeal swab, from 28 February 2020 to 31 May 2021, were enrolled in the CoviCamp cohort. Results: Evaluating inclusion/exclusion criteria, 1357 patients were included. Considering in-hospital mortality and creatinine value at admission, the best cut-off point to discriminate a death during hospitalization was 1.115 mg/dL. The logistic regression demonstrated that factors independently associated with mortality were age (OR 1.082, CI: 1.054–1.110), Charlson Comorbidity Index (CCI) (OR 1.341, CI: 1.178–1.526), and an abnormal creatinine value at admission, defined as equal to or above 1.12 mg/dL (OR 2.233, CI: 1.373–3.634). Discussion: In conclusion, our study is in line with previous studies confirming that the creatinine serum level can predict mortality in COVID-19 patients and defining that the best cut-off of the creatinine serum level at admission to predict mortality was 1.12 mg/dL.
1. Introduction
Since 2019, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has spread all over the world and caused a global crisis in healthcare and the economic and social sectors. [1]. The disease can cause severe illness, and it is characterized by a high mortality rate in certain groups [2,3]. Several studies have highlighted that different clinical conditions, such as diabetes, hypertension, chronic kidney disease, and dementia, can increase the mortality and severity of the disease [2,3]. Identifying high-risk patients shortly after admission allows for timely, supportive treatment [2,4,5].
Although the lungs are the most commonly affected organs by SARS-CoV-2, the kidneys are also frequently affected. In fact, acute kidney disease is a frequent complication of Coronavirus Disease-2019 (COVID-19), especially in patients with a severe disease [6,7]. The interplay between a hyperactive immune response, the cytopathic effects of the virus, and homeostatic reactions to balance the pulmonary hemodynamic response have been postulated to be the main cause of kidney damage [8]. As a predictor of poor outcome, creatinine levels at hospital admission may be a useful parameter to quickly identify high-risk COVID-19 patients who require intensive management [9,10]. To our knowledge, few studies have investigated the impact of creatinine levels on COVID-19 progression in patients without a history of chronic kidney disease [11].
Considering the study published earlier, the aim of this observational, retrospective study on a large cohort of COVID-19 patients hospitalized from February 2020 to May 2021 was to assess the impact of creatinine levels at hospital admission on COVID-19 disease progression and mortality in subjects without underlying chronic kidney disease.
2. Materials and Methods
2.1. Study Design and Setting
A multicenter, observational, retrospective study was performed, involving seventeen COVID-19 units in eight cities in the Campania region in southern Italy: Naples, Caserta, Salerno, Benevento, Avellino, Pozzuoli, Eboli, and Vallo della Lucania. Fifteen out of 17 were Infectious Disease Units, while the remaining 2 were sub-intensive care units; all these centers had collaborated in previous studies and were able to perform oxygen treatment and non-invasive ventilation (NIV).
All adult patients (≥18 years old) admitted from 28 February 2020 to 31 May 2021 with a diagnosis of SARS-CoV-2 confirmed by a positive reverse transcriptase-polymerase chain reaction (RT-PCR) on a naso-oropharyngeal swab were included in our CoviCamp cohort. From the CoviCamp cohort, we included in the present study all patients for whom a determination at admission of creatinine and severity of COVID-19 were available and who did not have chronic kidney disease (CKD). The exclusion criteria included minority age and lack of clinical data and/or of informed consent. No study protocol or guidelines regarding the criteria of hospitalization were shared among the centers involved in the study, and the patients were hospitalized following a decision by the physicians of each center.
The study was approved by the Ethics Committee of the University of Campania L. Vanvitelli, Naples (n°10877/2020). All procedures performed in this study were in accordance with the ethics standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethics standards. Informed consent was obtained from all participants included in the study.
This study was reported following the STROBE recommendations for an observational study (see Supplementary Data).
2.2. Variables and Definitions
All demographic and clinical data of patients with SARS-CoV2 infection enrolled in the cohort were collected in an electronic database. From this database we extrapolated the data for the present study.
The microbiological diagnosis of SARS-CoV-2 infection was defined as a positive RT-PCR test on a naso-oropharyngeal swab.
We divided the patients enrolled according to the clinical outcome of COVID-19 during hospitalization: mild, moderate, severe outcome, and death. Patients with mild infection did not need oxygen (O2) therapy and/or had a Modified Early Warning Score (MEWS) below 3 points during hospitalization. Patients with a moderate infection required non-invasive O2 therapy (excluding high-flow nasal cannula) and/or had a MEWS score equal to or above 3 points (≥3) during hospitalization. Patients with a severe infection needed management in an intensive care unit (ICU) and/or high-flow nasal cannula or invasive/non-invasive mechanical ventilation during hospitalization.
Patients were followed until negativity of SARS-CoV-2-RNA on naso-oropharyngeal swab and/or until they were discharged from hospital or died. The glomerular filtration rate (eGFR) was calculated using 2021 CKD-EPI [12]. Chronic Kidney Disease (CKD) was defined considering the diagnoses of CKD prior to hospitalization.
2.3. Statistical Analysis
For the descriptive analysis, categorical variables were presented as absolute numbers and their relative frequencies. Continuous variables were summarized as mean and standard deviation or as median and interquartile range (Q1–Q3). We performed a comparison of the patients who were discharged from hospital and those who died during hospitalization using Pearson chi-square or Fisher’s exact test for categorical variables and Student’s t test or Mann–Whitney tests for continuous variables. The same statistical analyses were performed to compare patients with different cut-offs of creatinine blood levels at admission. Odds ratios were calculated using binomial logistic regression; these analyses were performed only for parameters clinically relevant and for those that were statistically significant in univariate analysis. The receiver operating characteristic (ROC) curve and the Youden’s Index were used to determine the optimum cut-off point for possible effective variables on the patients’ outcomes. A p-value below 0.05 was considered statistically significant. Analyses were performed using STATA [13].
3. Results
During the study period, 2054 patients with a diagnosis of SARS-CoV-2 infection, confirmed by a positive RT-PCR on a naso-oropharyngeal swab, were hospitalized. Among them, 191 were excluded because they already suffered from CKD, and 506 were excluded for the lack of data on the creatinine value; thus, 1357 patients were included in the present study (Figure 1).
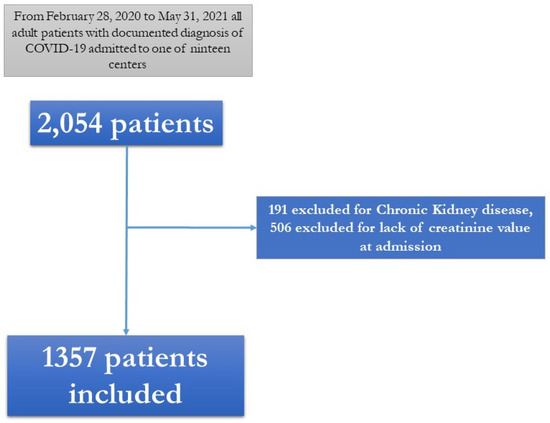
Figure 1.
Figure 1. Flow chart of patients included in the study.
The demographic and clinical characteristics of the 1357 patients included in the study are shown in Table 1, Table 2, Table 3 and Table 4. Eight hundred and twenty-six (60.9%) subjects were males, the median age was 62 years (Q1–Q3: 51–73 years), the median creatinine value at admission was 0.83 mg/dL (Q1–Q3: 0.7–1 mg/dL), and the median eGFR was 94 mL/min (Q1–Q3: 74–105 mL/min). No patients had received vaccination for SARS-CoV-2. A total of 641 (47.6%) patients had a mild outcome, 299 (22%) a moderate outcome, 308 (22.7%) a severe outcome, and 104 (7.7%) died (Table 3).

Table 1.
Demographic, clinical and laboratory data of the patients included at admission.

Table 2.
Comorbidity of patients included in our study.

Table 3.
Clinical outcome of patients included in our study.

Table 4.
Demographic, clinical and laboratory parameters in patients discharged or who died during hospitalization.
We compared the patients discharged (n = 1253) with those who died during hospital stay (n = 104) (Table 4). The patients who died during hospitalization were significantly older (p = 0.0001), with a higher CCI (p = 0.0001), higher rate of cardiovascular diseases (50 vs. 23.7%, p = 0.0001) and dementia (43 vs. 23%, p = 0.0001), had a shorter hospitalization stay (p = 0.0001), a lower P/F ratio (p = 0.0001), a lower median of days from symptom onset to hospital admission (p = 0.0001), and a higher creatinine value at admission (p = 0.0001) (Table 4 and see Supplementary Data). Other biochemical and clinical data are shown in Table 4.
Considering these data, we calculated the Area Under the Curve (AUC) for creatinine level at admission considering death during hospitalization as a status variable. The result was 0.647 (95% Confidence Interval (CI): 0.582–0.713; p < 0.001), with the best cut-off point of 1.115 mg/dL (sensitivity: 44.2%, specificity: 85.7%) demonstrating the direct correlation between death during hospitalization and creatinine levels at admission (see Supplementary Data).
Considering this cut-off, we defined two groups: a case group with a creatinine level equal to or higher than 1.12 mg/dL at admission (225 patients, 16.6%) and a control group with a creatinine level lower than 1.12 mg/dL at admission (1132 patients, 83.4%). The subjects in the case group were significantly older than those in the control group (p ≤ 0.001), had a higher median of CCI (p = 0.0001), and had more comorbidities, such as arterial hypertension (p = 0.001), cardio-vascular disease (p = 0.001), diabetes (p = 0.001), and COPD (Chronic obstructive pulmonary disease) (p = 0.001) (Table 5). There were no statistical differences between the case and control groups in the prevalence of chronic liver disease (p = 0.826), in median days from symptom onset to hospital admission (p = 0.696), and in median PaO2/FiO2 Ratio (P/F) at admission (p = 0.074) (Table 5). Moreover, the patients in the case group exhibited a higher rate of severe clinical outcome of COVID-19 (45.3% vs. 27.4%, p = 0.001) and of in-hospital mortality (20.4% vs. 5.1%, p = 0.001) (Table 5).

Table 5.
Demographic, clinical, and laboratory parameters in patients with creatinine at admission <1.12 and ≥1.12 mg/dL.
Lastly, the logistic regression demonstrated that the factors independently associated with mortality were age (OR 1.082, CI: 1.054–1.110), CCI (OR 1.341, CI: 1.178–1.526), and an abnormal creatinine value at admission, defined as equal to or above 1.12 mg/dL (OR 2.233, CI: 1.373–3.634) (Table 6)

Table 6.
Multivariable binomial logistic regression of parameters predictor of mortality.
4. Discussion
In this multicenter observational retrospective study, the aim was to assess the impact of creatinine levels at admission on disease progression and mortality in subjects without underlying chronic kidney disease. Compared to those with normal values, the patients with abnormal serum creatinine at hospital admission exhibited a higher severe COVID-19 rate and mortality rate; moreover, in the present large cohort of hospitalized COVID-19 patients, the best cut-off of creatinine serum levels at admission to predict mortality was 1.12 mg/dL.
Several studies have investigated the role of creatinine levels or renal function on COVID-19 clinical outcome and on mortality, demonstrating a significant association between high levels of creatinine and COVID-19 severity and mortality [8,10,11,14,15,16,17,18,19,20,21,22,23,24,25,26]. A systematic review performed by Izcovich and colleagues in 2020 aimed at identifying factors associated with a more severe COVID-19 presentation, which may help clinicians in the decision-making process of patients with COVID-19 [9]. Among the 207 studies included, the authors identified a serum creatinine increase as a prognostic factor for mortality increase (OR 1.14, 95% CI 1.02–1.28), but not for disease severity (OR 1.89, 95% CI 0.87–4.10) [9].
However, the majority of the published studies did not exclude or state that they were excluding patients with CKD, which does not allow us to know whether the creatinine value predicted the COVID-19 outcome in subjects without CKD, such as in the present study. A recent retrospective cohort study performed in Italy on 174 hospitalized patients with COVID-19 investigated the role of kidney dysfunction on COVID-19 severity and mortality, and examined in-depth the relationship between kidney function, age, and progression of COVID-19. The authors reported acute kidney impairment (AKI) in 10.2% of patients, and an overall mortality rate of 19.5% [14]. Patients with AKI presented a higher risk of mortality (OR 5.16, 95% CI 1.86–14.30) compared with non-AKI patients, especially in moderate–severe AKI (stages 2–3, aHR 8.43, 95% CI 2.96–24.02) compared to mild AKI (stage 1, aHR 1.90, 95% CI 0.62–5.82) [14]. Another predictor of mortality was age ≥ 70 years (aHR 6.2, 95% CI 1.80–21.40). However, the influence of baseline eGFR on clinical outcome decreased with age, and it did not seem to represent a risk factor for patients older than 70 years [14].
Another retrospective observational study, by Alfano et al., demonstrated that COVID-19 patients with decreased kidney function within 24 h from hospital admission were at high risk for AKI and in-hospital mortality [10]. The authors included 224 non-ICU patients, evaluated 24-h serum creatinine differences (ΔsCr), and stratified them in three groups: The first had stable kidney function (ΔsCr from –0.05 mg/dL up to +0.05 mg/dL), the second had decreased kidney function (ΔsCr higher than +0.05 mg/dL), and the last had improved kidney function (ΔsCr lower than −0.05 mg/dL). ΔsCr was a predictor of AKI (HR 7.9, p < 0.001) and mortality during hospitalization (HR 4.0, 95%, p < 0.001) [10]. A higher survival rate was observed in the first group, whereas the second one was associated with higher rates of both AKI and in-hospital mortality [10]. The regression analysis demonstrated that decreased kidney function was an independent risk factor for 30-day in-hospital mortality (HR 5.5, p = 0.04) [10].
To our knowledge, only one study investigated the role of creatinine serum levels in COVID-19 progression focusing only on patients without a history of CKD [11]. Chen et al. investigated the effect of abnormal renal function on prognosis of 1764 COVID-19 patients, considering not only serum creatinine values, but also cystatin C values, which is a more sensitive indicator of GFR compared with BUN (Blood Urea Nitrogen) and serum creatinine [11]. The authors demonstrated that elevated cystatin C levels were associated with a more severe clinical outcome (OR 2.449, p < 0.001), whereas elevated serum creatinine levels were independent predictors of death (OR 6.789, p 0.02) [11].
The creatinine value and renal function are very useful parameters not only in the evaluation and prognosis of patients with COVID-19, but also in antiviral treatment for SARS-CoV-2 infection. To date, remdesivir is the only antiviral approved in patients hospitalized for COVID-19 [27] and is not recommended for patients with eGFR < 30 mL/min [27]. However, recent observational studies and systematic reviews [28,29,30,31,32] reevaluate the impact of remdesivir in patients with reduced renal function or eGFR < 30 mL/min, suggesting that remdesivir can also be used in these patients if the potential benefits outweigh the risks [27].
Our study has several limitations. Firstly, it has a retrospective design. Secondly, we evaluated only patients with at least one value of creatinine serum at baseline, but we did not consider the trend of creatinine, nor blood urea nitrogen and/or cystatin C. Thirdly, we did not take into consideration other potential causes of increased values of serum creatinine, such as bacterial superinfection or dehydration caused by diarrhea. Fourthly, due to the historical period of our study, our cohort of patients did not include subjects who were vaccinated against SARS-CoV-2 and/or early treatments (antivirals or monoclonal antibodies). Moreover, our study did not account for the impact of different variants with a possible impact on the applicability of the findings to the vaccinated patients, which represents the majority of patients nowadays. On the other hand, the strengths of our study are the multicenter design and the sample size of the population.
In conclusion, our study is in line with previous studies in confirming that the creatinine serum level can predict mortality in COVID-19 patients and in defining that the best cut-off of creatinine serum levels at admission to predict mortality is 1.12 mg/dL. Despite the significant data, it should be noted that the study population had greater comorbidities and CCI compared to the control group, which, even if not statistically significant, may be clinically significant in determining an increase in creatinine and consequently with mortality and severity.
Despite the recent improvements in preventive and therapeutic measures, it is of paramount importance to find other examinations that can help clinicians to foresee the clinical progression of COVID-19. Although the studies are retrospective observational studies, they all demonstrate that the baseline creatinine level and its variations, especially in the first 24 h, seem to be a predictor of poor outcome and may be a useful parameter to identify high-risk patients requiring more careful attention.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/pathogens12080973/s1, Figure S1: Box plot of creatinine value grouped considering hospital discharge or death during hospitalization; Figure S2: ROC curve of creatinine levels considering death during hospitalization; Table S1: STROBE recommendations for an observational study; Table S2: Demographic, clinical and laboratory variable of patients grouped by outcome.
Author Contributions
N.C., A.R., C.M. and M.P. were involved in study concept and design, drafting of the manuscript,: P.M., I.G., C.M., E.A., V.S., V.E., V.G., R.P. (Roberto Parrella), G.C., E.M., A.M., C.C., G.D., G.R., M.G., A.P., L.O., R.P. (Raffaella Pisapia) and F.C., were involved in critical revision of the manuscript for important intellectual content; P.M., C.M., I.G., E.A., V.S., V.E., V.G., R.P. (Roberto Parrella), G.C., E.M., A.M., C.C., GDA, G.R., M.G., A.P., R.P. (Raffaella Pisapia), F.C. and L.O. were involved in the acquisition of data, analysis and interpretation of data, and in the critical revision of the manuscript; CoviCamp (Campania COVID-19 group) was involved in the enrolment of the patients. All authors contributed to data analysis and drafting or revising the article. They have agreed on the journal to which the article will be submitted, given final approval of the version to be published and agreed to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Funding
Notice for the acquisition of expressions of interest for the implementation of research and development services for the fight against COVID-19 (DGR no. 140 of 17 March 2020), Campania Region, Italy. Project: “Identification of demographic, clinical, virological, genetic, immunological and serological factors associated with unfavorable outcome in subjects with COVID-19”, [POR Campania FESR 2014-2020, Campania Region, grant number not applicable]. Notice for the acquisition of expressions of interest by Research Organizations for the realization of research, development, and innovation services for the fight against COVID-19 (DGR n. 504 of 10 November 2021)—Campania Region, Italy. Project: Impact of new variants, the use of early antiviral therapies and vaccination status on the clinical presentation of COVID-19: multicenter restrictive/prospective study. [POR Campania FESR 2014-2020, Campania Region, grant number not applicable].
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the University of Campania L. Vanvitelli, Naples (n°10877/2020, 11 May 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
Campania COVID-19 network: Nicola Coppola, Caterina Monari, Caterina Sagnelli, Paolo Maggi, Vincenzo Sangiovanni, Fabio Giuliano Numis, Ivan Gentile, Alfonso Masullo, Carolina Rescigno, Giosuele Calabria, Angelo Salomone Megna, Michele Gambardella, Elio Manzillo, Grazia Russo, Vincenzo Esposito, Giuseppina Dell’Aquila, Roberto Parrella, Rodolfo Punzi, Antonio Ponticiello, Mariantonietta Pisaturo, Enrico Allegorico, Raffaella Pisapia, Francesco Maria Fusco, Giovanni Porta, Margherita Macera, Federica Calò, Loredana Alessio, Cascone Angela, Caterina Monari, Onorato Lorenzo, Caterina Sagnelli, Stanzione Maria, Stornaiuolo Gianfranca, Anna Maria Rossomando, Mariana Di Lorenzo, Antonio Russo, Giorgio Bosso, Claudia Serra, Ferdinando Dello Vicario, Valentina Minerva, Giulia De Angelis, Stefania De Pascalis, Salvatore Martini, Paola Medusa, Ilaria Palma, Andrea Dell’Aquila, Nicola Carro, Roberta Astorri, Klodian Gjeloshi, Simona Imbriani, Carmen Ricozzi, Giovanni Di Caprio, Addolorata Masiello, Domenica Di Costanzo, Mariano Mazza, Vincenzo Bianco, Valeria Gentile, Antonio Riccardo Buonomo, Biagio Pinchera, Riccardo Scotto.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO Coronavirus (COVID-19) Dashboard|WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. (n.d.). Available online: https://covid19.who.int/ (accessed on 26 February 2022).
- Gallo Marin, B.; Aghagoli, G.; Lavine, K.; Yang, L.; Siff, E.J.; Chiang, S.S.; Salazar-Mather, T.P.; Dumenco, L.; Savaria, M.C.; Aung, S.N.; et al. Predictors of COVID-19 severity: A literature review. Rev. Med. Virol. 2021, 31, 1–10. [Google Scholar] [CrossRef]
- Pisaturo, M.; Calò, F.; Russo, A.; Camaioni, C.; Giaccone, A.; Pinchera, B.; Gentile, I.; Simeone, F.; Iodice, A.; Maggi, P.; et al. Dementia as Risk Factor for Severe Coronavirus Disease 2019: A Case-Control Study. Front. Aging Neurosci. 2021, 13, 698184. [Google Scholar] [CrossRef]
- Russo, A.; Pisaturo, M.; Palladino, R.; Maggi, P.; Numis, F.G.; Gentile, I.; Sangiovanni, V.; Esposito, V.; Punzi, R.; Calabria, G.; et al. Prognostic Value of Transaminases and Bilirubin Levels at Admission to Hospital on Disease Progression and Mortality in Patients with COVID-19—An Observational Retrospective Study. Pathogens 2022, 11, 652. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.D.; Ding, M.; Dong, X.; Zhang, J.J.; Kursat Azkur, A.; Azkur, D.; Gan, H.; Sun, Y.L.; Fu, W.; Li, W.; et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 2021, 76, 428–455. [Google Scholar] [CrossRef]
- Migliaccio, M.G.; Di Mauro, M.; Ricciolino, R.; Spiniello, G.; Carfora, V.; Verde, N.; Mottola, F.F.; Coppola, N.; Vanvitelli COVID-19 Group. Renal Involvement in COVID-19: A Review of the Literature. Infect. Drug Resist. 2021, 14, 895–903. [Google Scholar] [CrossRef] [PubMed]
- Ertuğlu, L.A.; Kanbay, A.; Afşar, B.; Afşar, R.E.; Kanbay, M. COVID-19 and acute kidney injury. Tuberk. Toraks 2020, 68, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Ye, Q. Kidney involvement in COVID-19 and its treatments. J. Med Virol. 2021, 93, 1387–1395. [Google Scholar] [CrossRef]
- Izcovich, A.; Ragusa, M.A.; Tortosa, F.; Marzio, M.A.L.; Agnoletti, C.; Bengolea, A.; Ceirano, A.; Espinosa, F.; Saavedra, E.; Sanguine, V.; et al. Prognostic factors for severity and mortality in patients infected with COVID-19: A systematic review. PLoS ONE 2020, 17, e0269291. [Google Scholar]
- Alfano, G.; Ferrari, A.; Fontana, F.; Mori, G.; Ligabue, G.; Giovanella, S.; Magistroni, R.; Meschiari, M.; Franceschini, E.; Menozzi, M.; et al. Twenty-four-hour serum creatinine variation is associated with poor outcome in the novel coronavirus disease 2019 (COVID-19) patients. Kidney Res. Clin. Pract. 2021, 40, 231–240. [Google Scholar] [CrossRef]
- Chen, S.; Li, J.; Liu, Z.; Chen, D.; Zhou, L.; Hu, D.; Li, M.; Long, W.; Huang, Y.; Huang, J.; et al. Comparing the Value of Cystatin C and Serum Creatinine for Evaluating the Renal Function and Predicting the Prognosis of COVID-19 Patients. Front. Pharmacol. 2021, 12, 587816. [Google Scholar] [CrossRef]
- Inker, L.A.; Eneanya, N.D.; Coresh, J.; Tighiouart, H.; Wang, D.; Sang, Y.; Crews, D.C.; Doria, A.; Estrella, M.M.; Froissart, M.; et al. New Creatinine- and Cystatin C-Based Equations to Estimate GFR without Race. N. Engl. J. Med. 2021, 385, 1737–1749. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC: College Station, TX, USA, 2019. [Google Scholar]
- La Porta, E.; Baiardi, P.; Fassina, L.; Faragli, A.; Perna, S.; Tovagliari, F.; Tallone, I.; Talamo, G.; Secondo, G.; Mazzarello, G.; et al. The role of kidney dysfunction in COVID-19 and the influence of age. Sci. Rep. 2022, 12, 8650. [Google Scholar] [CrossRef]
- Xia, T.; Zhang, W.; Xu, Y.; Wang, B.; Yuan, Z.; Wu, N.; Xiang, Y.; Li, C.; Shan, Y.; Xie, W.; et al. Early kidney injury predicts disease progression in patients with COVID-19: A cohort study. BMC Infect. Dis. 2021, 21, 1012. [Google Scholar] [CrossRef] [PubMed]
- Komaru, Y.; Doi, K. Does a slight change in serum creatinine matter in coronavirus disease 2019 (COVID-19) patients? Kidney Res. Clin. Pract. 2021, 40, 177–179. [Google Scholar] [CrossRef] [PubMed]
- Nadim, M.K.; Forni, L.G.; Mehta, R.L.; Connor, M.J., Jr.; Liu, K.D.; Ostermann, M.; Rimmelé, T.; Zarbock, A.; Bell, S.; Bihorac, A.; et al. COVID-19-associated acute kidney injury: Consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup. Nat. Rev. Nephrol. 2020, 16, 747–764. [Google Scholar] [CrossRef] [PubMed]
- Cei, F.; Chiarugi, L.; Brancati, S.; Montini, M.S.; Dolenti, S.; Di Stefano, D.; Beatrice, S.; Sellerio, I.; Messiniti, V.; Gucci, M.M.; et al. Early reduction of estimated Glomerular Filtration Rate (eGFR) predicts poor outcome in acutely ill hospitalized COVID-19 patients firstly admitted to medical regular wards (eGFR-COV19 study). Biomed. Pharmacother. 2022, 153, 113454. [Google Scholar] [CrossRef]
- Sami, R.; Soltaninejad, F.; Shayganfar, A.; Mirfendereski, S.; Mansourian, M.; Khademi, N.; Dehghan, M.; Khorrami, Z.; Jalali, S.; Mokhtari, Z. Severity of Disease and COVID-19 Complications During Hospital Stay: A Prospective Cohort Study. Arch. Iran. Med. 2022, 25, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Niculae, A.; Peride, I.; Nechita, A.M.; Petcu, L.C.; Tiglis, M.; Checherita, I.A. Epidemiological Characteristics and Mortality Risk Factors Comparison in Dialysis and Non-Dialysis CKD Patients with COVID-19-A Single Center Experience. J. Pers. Med. 2022, 12, 966. [Google Scholar] [CrossRef]
- Lin, Y.; Ma, B.; Yang, Y.; Chen, Y.; Huang, J.; Li, W.; Yu, X.; Liang, L. Impaired kidney function biomarkers and risk of severe COVID-19: Analysis of population-based cohort data. Mol. Genet. Genom. Med. 2022, 10, e2047. [Google Scholar] [CrossRef]
- Madaschi, S.; Resmini, E.; Bonfadini, S.; Massari, G.; Gamba, P.; Sandri, M.; Calza, S.; Cimino, E.; Zarra, E.; Dotti, S.; et al. Predictive markers for clinical outcomes in a cohort of diabetic patients hospitalized for COVID-19. Diabetol. Metab. Syndr. 2022, 14, 168. [Google Scholar] [CrossRef]
- Lombardi, C.; Roca, E.; Bigni, B.; Bertozzi, B.; Ferrandina, C.; Franzin, A.; Vivaldi, O.; Cottini, M.; D’Alessio, A.; Del Poggio, P.; et al. Immune and cellular damage biomarkers to predict COVID-19 mortality in hospitalized patients. Curr. Res. Immunol. 2021, 2, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, Z.; Faghih Dinevari, M.; Vahed, N.; Ebrahimi Bakhtavar, H.; Rahmani, F. Clinical and Laboratory Predictors of COVID-19-Related In-hospital Mortality; a Cross-sectional Study of 1000 Cases. Arch. Acad. Emerg. Med. 2022, 10, e49. [Google Scholar] [CrossRef] [PubMed]
- Cirillo, C.; Nakou, E.; Georgiopoulos, G.; Tountas, C.; Victor, K.; Marvaki, A.; Desai, N.; Fisher, R.; Ryan, M.; Demir, O.M.; et al. Predictors of in-hospital mortality in critically ill patients with COVID-19: A large dual tertiary centre study. BMJ Open 2022, 12, e059358. [Google Scholar] [CrossRef] [PubMed]
- Mirijello, A.; Piscitelli, P.; de Matthaeis, A.; Inglese, M.; D’Errico, M.M.; Massa, V.; Greco, A.; Fontana, A.; Copetti, M.; Florio, L.; et al. Low eGFR Is a Strong Predictor of Worse Outcome in Hospitalized COVID-19 Patients. J. Clin. Med. 2021, 10, 5224. [Google Scholar] [CrossRef]
- COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines; National Institutes of Health: Bethesda, MD, USA, 2021. Available online: https://www.covid19treatmentguidelines.nih.gov/ (accessed on 15 July 2023).
- Biancalana, E.; Chiriacò, M.; Sciarrone, P.; Mengozzi, A.; Mechelli, S.; Taddei, S.; Solini, A. Remdesivir, Renal Function and Short-Term Clinical Outcomes in Elderly COVID-19 Pneumonia Patients: A Single-Centre Study. Clin. Interv. Aging 2021, 16, 1037–1046. [Google Scholar] [CrossRef]
- Zhang, J.; Kummerfield, E.; Hultman, G.; Drawz, P.E.; Adam, T.J.; Simon, G.; Melton, G.B. Application of Causal Discovery Algorithms in Studying the Nephrotoxicity of Remdesivir Using Longitudinal Data from the EHR. AMIA Annu. Symp. Proc. 2023, 2022, 1227–1236. [Google Scholar]
- Li, X.; Zhou, L.; Gaggl, M.; Kinlaw, A.C.; Gou, Z.; Xu, Y.; Wei, J.; Wang, T. Remdesivir for COVID-19 and acute kidney injury: Disproportionality analysis of data from the U.S. Food and Drug Administration Adverse Event Reporting System. Int. J. Clin. Pharm. 2023, 45, 509–514. [Google Scholar] [CrossRef]
- Seethapathy, R.; Wang, Q.; Zhao, S.; Strohbehn, I.A.; Long, J.D.; Dinulos, J.E.; Harden, D.; Kadiyala, V.B.; Moreno, D.; Sise, M.E. Effect of remdesivir on adverse kidney outcomes in hospitalized patients with COVID-19 and impaired kidney function. PLoS ONE 2023, 18, e0279765. [Google Scholar] [CrossRef]
- Davoudi-Monfared, E.; Ahmadi, A.; Karimpour-Razkenari, E.; Shahrami, B.; Najmeddin, F.; Mojtahedzadeh, M. Remdesivir Administration in COVID-19 Patients with Renal Impairment: A Systematic Review. Am. J. Ther. 2022, 29, e520–e533. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).