UVC-Based Air Disinfection Systems for Rapid Inactivation of SARS-CoV-2 Present in the Air
Abstract
1. Introduction
2. Results
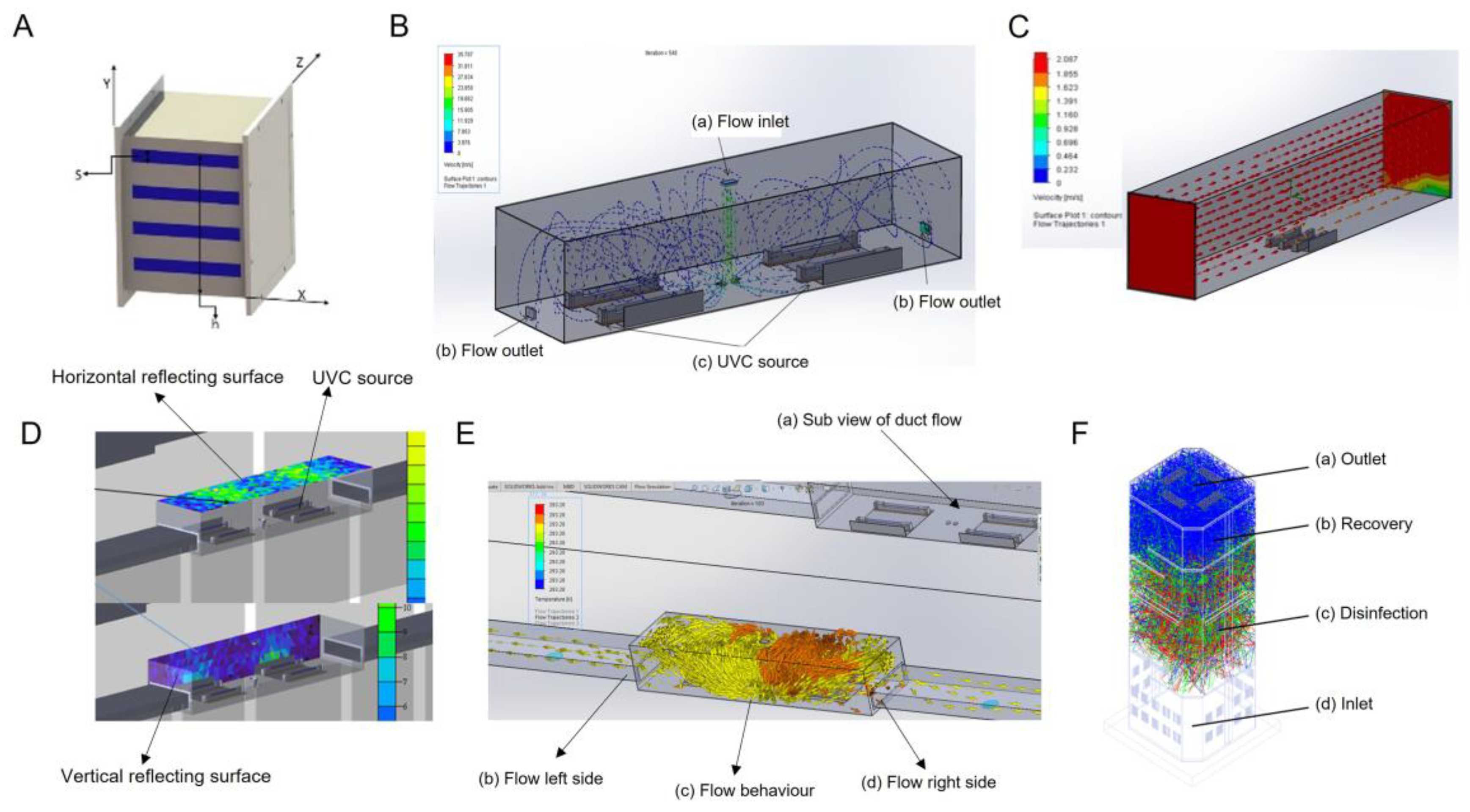
2.1. Design of Ultraviolet C (UVC) Disinfection System
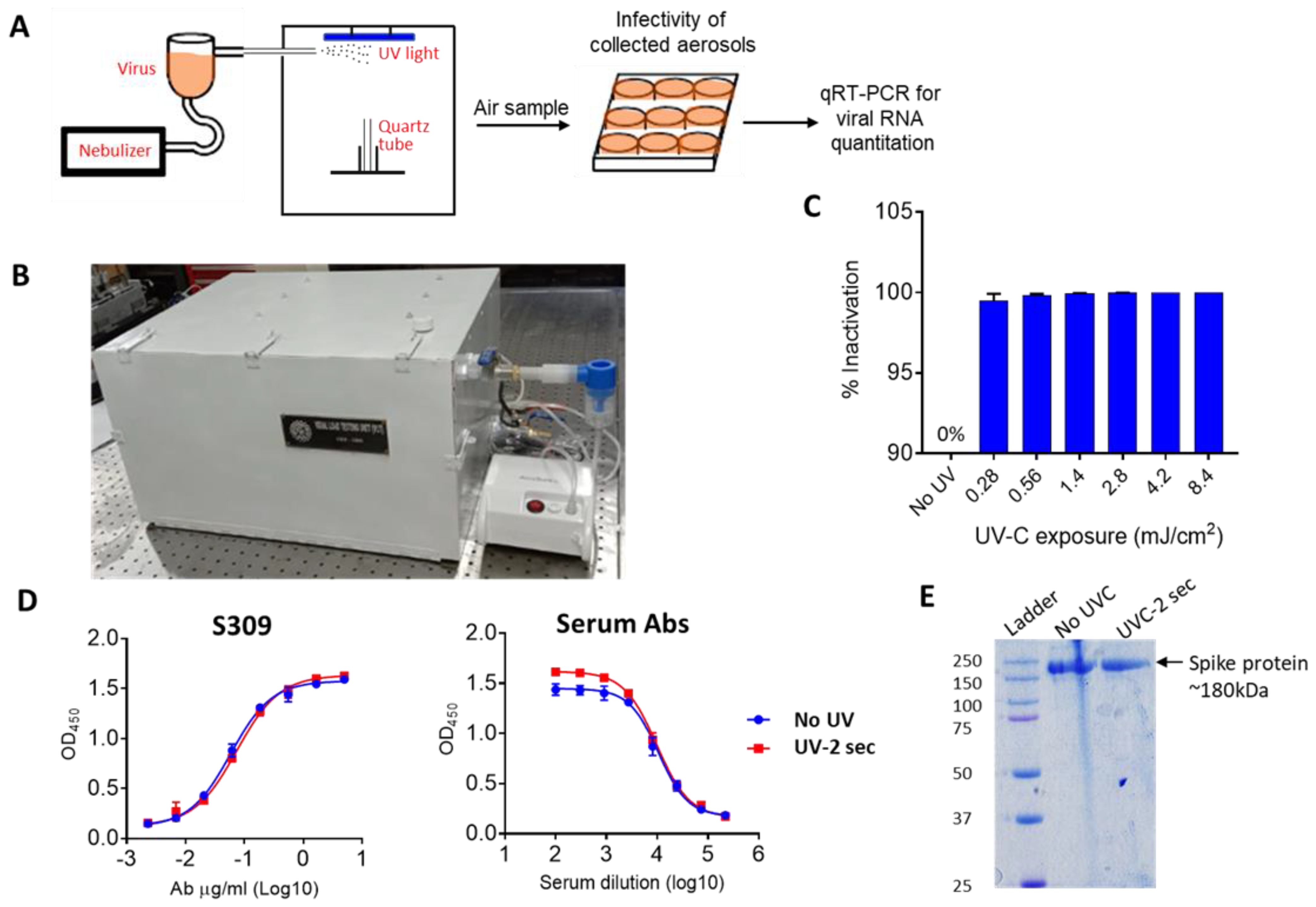
2.2. Design of a Stand-Alone System to Measure the Effect of UVC on SAS-CoV-2 Survival in Air
2.3. UVC Air Disinfection System Efficiently Inactivates Aerosolized SARS-CoV-2
2.4. Testing the Efficiency of Stand-Alone UVC Air Disinfection System against SARS-CoV-2 Virus
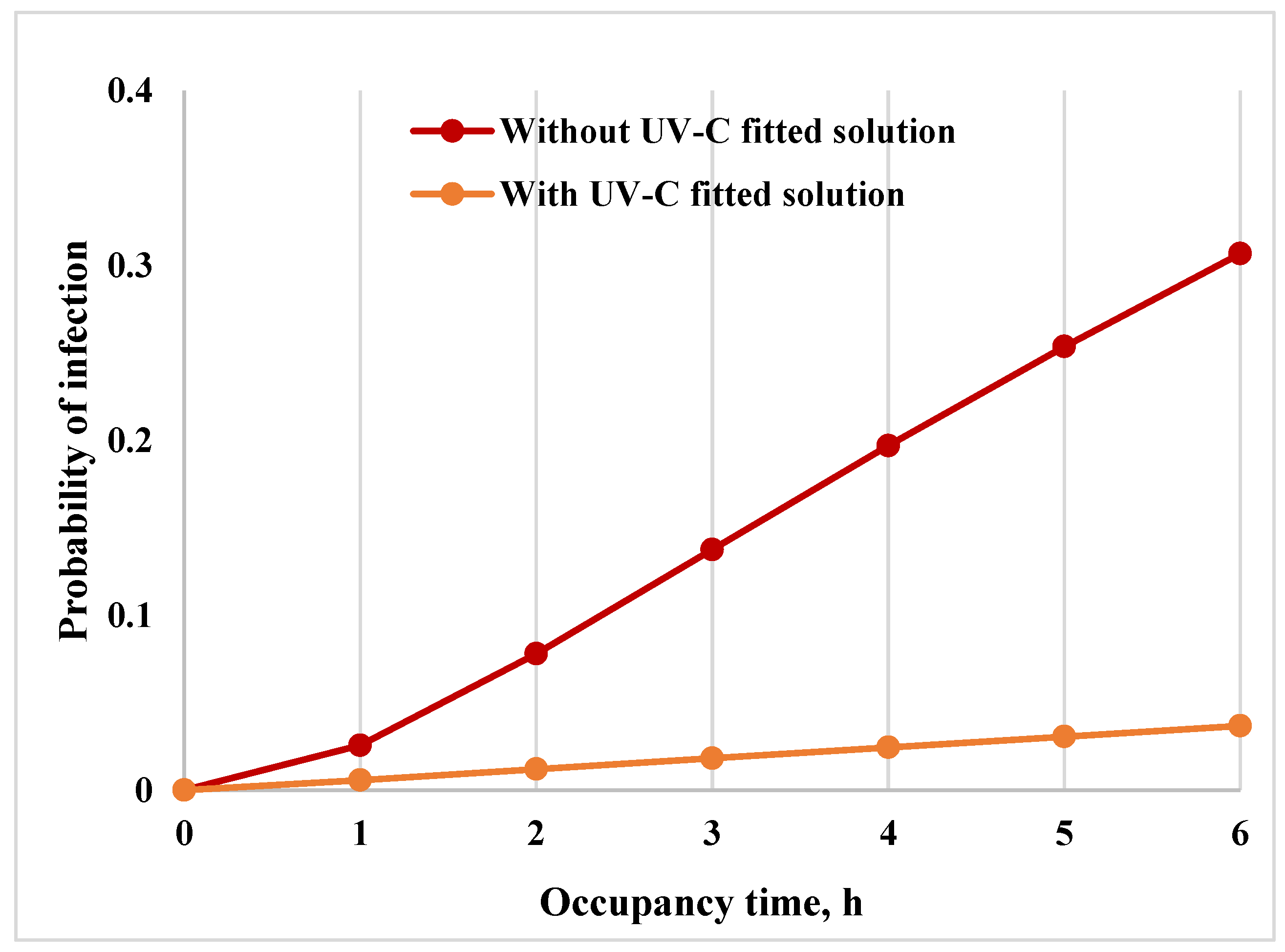
2.5. Risk Analysis of Infection and Reduction of Risk
3. Materials and Methods
3.1. Design of UVC Disinfection System
3.2. SARS-CoV-2 Virus Preparation
3.3. Aerosol Generation, Sample Collection and Infection of Cells by Aerosol Samples
3.4. Quantitative Real-Time PCR (qRT-PCR)
3.5. SARS-CoV-2 Spike Protein Expression
3.6. Antibody (S309) Expression and Purification
3.7. SDS-PAGE
3.8. Enzyme-Linked Immunosorbent Assay (ELISA)
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- Goralnick, E.; Kaufmann, C.; Gawande, A.A. Mass-Vaccination Sites—An Essential Innovation to Curb the COVID-19 Pandemic. N. Engl. J. Med. 2021, 384, e67. [Google Scholar] [CrossRef] [PubMed]
- Theuring, S.; Thielecke, M.; van Loon, W.; Hommes, F.; Hulso, C.; von der Haar, A.; Korner, J.; Schmidt, M.; Bohringer, F.; Mall, M.A.; et al. SARS-CoV-2 infection and transmission in school settings during the second COVID-19 wave: A cross-sectional study, Berlin, Germany, November 2020. Euro Surveill. 2021, 26, 210084. [Google Scholar] [CrossRef] [PubMed]
- Thornton, G.M.; Fleck, B.A.; Dandnayak, D.; Kroeker, E.; Zhong, L.; Hartling, L. The impact of heating, ventilation and air conditioning (HVAC) design features on the transmission of viruses, including the 2019 novel coronavirus (COVID-19): A systematic review of humidity. PLoS ONE 2022, 17, e0275654. [Google Scholar] [CrossRef] [PubMed]
- Nardell, E.A. Air Disinfection for Airborne Infection Control with a Focus on COVID-19: Why Germicidal UV is Essential(dagger). Photochem. Photobiol. 2021, 97, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Berry, G.; Parsons, A.; Morgan, M.; Rickert, J.; Cho, H. A review of methods to reduce the probability of the airborne spread of COVID-19 in ventilation systems and enclosed spaces. Environ. Res. 2022, 203, 111765. [Google Scholar] [CrossRef] [PubMed]
- Mantelli, M.; Dos Santos, L.; de Fraga, L.; Miotto, G.; Bergamin, A.; Cardoso, E.; Serrano, M.; Maffei, R.; Prestes, E.; Netto, J.; et al. Autonomous Environment Disinfection Based on Dynamic UV-C Irradiation Map. IEEE Robot. Autom. Lett. 2022, 7, 4789–4796. [Google Scholar] [CrossRef]
- Maquart, M.; Marlet, J. Rapid SARS-CoV-2 inactivation by mercury and LED UV-C lamps on different surfaces. Photochem. Photobiol. Sci. 2022, 21, 2243–2247. [Google Scholar] [CrossRef]
- Fischer, R.J.; Port, J.R.; Holbrook, M.G.; Yinda, K.C.; Creusen, M.; Ter Stege, J.; de Samber, M.; Munster, V.J. UV-C Light Completely Blocks Aerosol Transmission of Highly Contagious SARS-CoV-2 Variants WA1 and Delta in Hamsters. Environ. Sci. Technol. 2022, 56, 12424–12430. [Google Scholar] [CrossRef]
- Brooks, J.T.; Butler, J.C.; Redfield, R.R. Universal Masking to Prevent SARS-CoV-2 Transmission-The Time Is Now. JAMA 2020, 324, 635–637. [Google Scholar] [CrossRef]
- Hijnen, W.A.; Beerendonk, E.F.; Medema, G.J. Inactivation credit of UV radiation for viruses, bacteria and protozoan (oo)cysts in water: A review. Water Res. 2006, 40, 3–22. [Google Scholar] [CrossRef] [PubMed]
- Storm, N.; McKay, L.G.A.; Downs, S.N.; Johnson, R.I.; Birru, D.; de Samber, M.; Willaert, W.; Cennini, G.; Griffiths, A. Rapid and complete inactivation of SARS-CoV-2 by ultraviolet-C irradiation. Sci. Rep. 2020, 10, 22421. [Google Scholar] [CrossRef] [PubMed]
- Schuit, M.A.; Larason, T.C.; Krause, M.L.; Green, B.M.; Holland, B.P.; Wood, S.P.; Grantham, S.; Zong, Y.; Zarobila, C.J.; Freeburger, D.L.; et al. SARS-CoV-2 inactivation by ultraviolet radiation and visible light is dependent on wavelength and sample matrix. J. Photochem. Photobiol. B 2022, 233, 112503. [Google Scholar] [CrossRef] [PubMed]
- Freeman, S.; Kibler, K.; Lipsky, Z.; Jin, S.; German, G.K.; Ye, K. Systematic evaluating and modeling of SARS-CoV-2 UVC disinfection. Sci. Rep. 2022, 12, 5869. [Google Scholar] [CrossRef] [PubMed]
- Ma, B.; Gundy, P.M.; Gerba, C.P.; Sobsey, M.D.; Linden, K.G. UV Inactivation of SARS-CoV-2 across the UVC Spectrum: KrCl* Excimer, Mercury-Vapor, and Light-Emitting-Diode (LED) Sources. Appl. Environ. Microbiol. 2021, 87, e0153221. [Google Scholar] [CrossRef]
- Biasin, M.; Bianco, A.; Pareschi, G.; Cavalleri, A.; Cavatorta, C.; Fenizia, C.; Galli, P.; Lessio, L.; Lualdi, M.; Tombetti, E.; et al. UV-C irradiation is highly effective in inactivating SARS-CoV-2 replication. Sci. Rep. 2021, 11, 6260. [Google Scholar] [CrossRef] [PubMed]
- Douki, T.; Court, M.; Sauvaigo, S.; Odin, F.; Cadet, J. Formation of the main UV-induced thymine dimeric lesions within isolated and cellular DNA as measured by high performance liquid chromatography-tandem mass spectrometry. J. Biol. Chem. 2000, 275, 11678–11685. [Google Scholar] [CrossRef]
- Cadet, J.; Sage, E.; Douki, T. Ultraviolet radiation-mediated damage to cellular DNA. Mutat. Res. 2005, 571, 3–17. [Google Scholar] [CrossRef]
- Moharir, S.C.; Thota, S.C.; Goel, A.; Thakur, B.; Tandel, D.; Reddy, S.M.; Vodapalli, A.; Singh Bhalla, G.; Kumar, D.; Singh Naruka, D.; et al. Detection of SARS-CoV-2 in the air in Indian hospitals and houses of COVID-19 patients. J. Aerosol. Sci. 2022, 164, 106002. [Google Scholar] [CrossRef]
- Chia, P.Y.; Coleman, K.K.; Tan, Y.K.; Ong, S.W.X.; Gum, M.; Lau, S.K.; Lim, X.F.; Lim, A.S.; Sutjipto, S.; Lee, P.H.; et al. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat. Commun. 2020, 11, 2800. [Google Scholar] [CrossRef] [PubMed]
- Cherrie, J.W.; Cherrie, M.P.C.; Smith, A.; Holmes, D.; Semple, S.; Steinle, S.; Macdonald, E.; Moore, G.; Loh, M. Contamination of Air and Surfaces in Workplaces with SARS-CoV-2 Virus: A Systematic Review. Ann. Work Expo. Health 2021, 65, 879–892. [Google Scholar] [CrossRef] [PubMed]
- Prussin, A.J., 2nd; Schwake, D.O.; Lin, K.; Gallagher, D.L.; Buttling, L.; Marr, L.C. Survival of the Enveloped Virus Phi6 in Droplets as a Function of Relative Humidity, Absolute Humidity, and Temperature. Appl. Environ. Microbiol. 2018, 84, e00551-18. [Google Scholar] [CrossRef] [PubMed]
- Matson, M.J.; Yinda, C.K.; Seifert, S.N.; Bushmaker, T.; Fischer, R.J.; van Doremalen, N.; Lloyd-Smith, J.O.; Munster, V.J. Effect of Environmental Conditions on SARS-CoV-2 Stability in Human Nasal Mucus and Sputum. Emerg. Infect. Dis. 2020, 26, 2276–2278. [Google Scholar] [CrossRef]
- Geng, Y.; Wang, Y. Stability and transmissibility of SARS-CoV-2 in the environment. J. Med. Virol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Oswin, H.P.; Haddrell, A.E.; Otero-Fernandez, M.; Mann, J.F.S.; Cogan, T.A.; Hilditch, T.G.; Tian, J.; Hardy, D.A.; Hill, D.J.; Finn, A.; et al. The dynamics of SARS-CoV-2 infectivity with changes in aerosol microenvironment. Proc. Natl. Acad. Sci. USA 2022, 119, e2200109119. [Google Scholar] [CrossRef] [PubMed]
- Verreault, D.; Moineau, S.; Duchaine, C. Methods for sampling of airborne viruses. Microbiol. Mol. Biol. Rev. 2008, 72, 413–444. [Google Scholar] [CrossRef] [PubMed]
- Corman, V.M.; Landt, O.; Kaiser, M.; Molenkamp, R.; Meijer, A.; Chu, D.K.; Bleicker, T.; Brunink, S.; Schneider, J.; Schmidt, M.L.; et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020, 25, 2000045. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, A.R.; Leili, M.; Azarian, G.; Poormohammadi, A. Sampling and detection of corona viruses in air: A mini review. Sci. Total Environ. 2020, 740, 140207. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Hsieh, C.L.; Goldsmith, J.A.; Schaub, J.M.; DiVenere, A.M.; Kuo, H.C.; Javanmardi, K.; Le, K.C.; Wrapp, D.; Lee, A.G.; Liu, Y.; et al. Structure-based design of prefusion-stabilized SARS-CoV-2 spikes. Science 2020, 369, 1501–1505. [Google Scholar] [CrossRef]
- Pinto, D.; Park, Y.J.; Beltramello, M.; Walls, A.C.; Tortorici, M.A.; Bianchi, S.; Jaconi, S.; Culap, K.; Zatta, F.; De Marco, A.; et al. Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody. Nature 2020, 583, 290–295. [Google Scholar] [CrossRef]
- Aganovic, A.; Bi, Y.; Cao, G.; Drangsholt, F.; Kurnitski, J.; Wargocki, P. Estimating the impact of indoor relative humidity on SARS-CoV-2 airborne transmission risk using a new modification of the Wells-Riley model. Build. Environ. 2021, 205, 108278. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.rehva.eu/fileadmin/content/documents/Downloadable_documents/REHVA_COVID-19_Ventilation_Calculator_user_guide_V2.0.pdf (accessed on 1 December 2022).
- Buonanno, G.; Morawska, L.; Stabile, L. Quantitative assessment of the risk of airborne transmission of SARS-CoV-2 infection: Prospective and retrospective applications. Environ. Int. 2020, 145, 106112. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://pusprajbhatt.files.wordpress.com/2017/12/india-national-building-code-nbc-2016-vol-2.pdf (accessed on 1 December 2022).
- Diapouli, E.; Chaloulakou, A.; Koutrakis, P. Estimating the concentration of indoor particles of outdoor origin: A review. J. Air Waste Manag. Assoc. 2013, 63, 1113–1129. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://indico.fnal.gov/event/10650/attachments/3160/3783/ParticleDepositionRates_Thatcher_et_al_2002.pdf (accessed on 1 December 2022).
- Fears, A.C.; Klimstra, W.B.; Duprex, P.; Hartman, A.; Weaver, S.C.; Plante, K.C.; Mirchandani, D.; Plante, J.A.; Aguilar, P.V.; Fernandez, D.; et al. Comparative dynamic aerosol efficiencies of three emergent coronaviruses and the unusual persistence of SARS-CoV-2 in aerosol suspensions. medRxiv 2020. [Google Scholar] [CrossRef]
- Harcourt, J.; Tamin, A.; Lu, X.; Kamili, S.; Sakthivel, S.K.; Murray, J.; Queen, K.; Tao, Y.; Paden, C.R.; Zhang, J.; et al. Severe Acute Respiratory Syndrome Coronavirus 2 from Patient with Coronavirus Disease, United States. Emerg. Infect. Dis. 2020, 26, 1266–1273. [Google Scholar] [CrossRef]
- Jain, A.; Grover, V.; Singh, C.; Sharma, A.; Das, D.K.; Singh, P.; Thakur, K.G.; Ringe, R.P. Chlorhexidine: An effective anticovid mouth rinse. J. Indian Soc. Periodontol. 2021, 25, 86–88. [Google Scholar] [CrossRef]
- Matsuyama, S.; Nao, N.; Shirato, K.; Kawase, M.; Saito, S.; Takayama, I.; Nagata, N.; Sekizuka, T.; Katoh, H.; Kato, F.; et al. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc. Natl. Acad. Sci. USA 2020, 117, 7001–7003. [Google Scholar] [CrossRef]
- Ahmed, S.; Khan, M.S.; Gayathri, S.; Singh, R.; Kumar, S.; Patel, U.R.; Malladi, S.K.; Rajmani, R.S.; van Vuren, P.J.; Riddell, S.; et al. A Stabilized, Monomeric, Receptor Binding Domain Elicits High-Titer Neutralizing Antibodies against All SARS-CoV-2 Variants of Concern. Front. Immunol. 2021, 12, 765211. [Google Scholar] [CrossRef]
- Setlow, R.B.; Setlow, J.K. Evidence that ultraviolet-induced thymine dimers in DNA cause biological damage. Proc. Natl. Acad. Sci. USA 1962, 48, 1250–1257. [Google Scholar] [CrossRef]
- Goes, L.R.; Siqueira, J.D.; Garrido, M.M.; Alves, B.M.; Pereira, A.; Cicala, C.; Arthos, J.; Viola, J.P.B.; Soares, M.A.; Force, I.C.-T. New infections by SARS-CoV-2 variants of concern after natural infections and post-vaccination in Rio de Janeiro, Brazil. Infect. Genet. Evol. 2021, 94, 104998. [Google Scholar] [CrossRef] [PubMed]
- Mizrahi, B.; Lotan, R.; Kalkstein, N.; Peretz, A.; Perez, G.; Ben-Tov, A.; Chodick, G.; Gazit, S.; Patalon, T. Correlation of SARS-CoV-2-breakthrough infections to time-from-vaccine. Nat. Commun. 2021, 12, 6379. [Google Scholar] [CrossRef] [PubMed]
- Chalkidis, A.; Jampaiah, D.; Aryana, A.; Wood, C.D.; Hartley, P.G.; Sabri, Y.M.; Bhargava, S.K. Mercury-bearing wastes: Sources, policies and treatment technologies for mercury recovery and safe disposal. J. Environ. Manag. 2020, 270, 110945. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, O.; Padilla, I.; Tayibi, H.; Lopez-Delgado, A. Concerns on liquid mercury and mercury-containing wastes: A review of the treatment technologies for the safe storage. J. Environ. Manag. 2012, 101, 197–205. [Google Scholar] [CrossRef] [PubMed]

| S. No | Parameters | In-Duct UVC Disinfection Systems for HVAC Buildings | In-Duct UVC Disinfection Systems for HVAC Buses | Stand-alone UVC Disinfection System |
|---|---|---|---|---|
| i. | Flow rate (CFM) | >30,000 | <3000 | <300 |
| ii. | Applicable space(ft2) | >1000 | <350 (customizable) | <150 |
| iii. | Shape and size | Rectangular >300 mm | Rectangular <300 mm | Rectangular <1500 mm |
| iv. | Wattage (W) | >100 | <100 | <70 |
| v. | Weight | <2.5 Kg | <1.2 Kg | <3.0 Kg |
| vi. | UVC source (nm) | 254 | 254 | 254 |
| vii. | Length of the delivery duct (m) | >10 | <2 | <0.5 |
| viii. | Exposure time (s) | 1.1 | 1.14 | 1.1 |
| ix. | Dosage | >1.6 mJ/cm2 | >1.3 mJ/cm2 | >1.3 mJ/cm2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garg, H.; Ringe, R.P.; Das, S.; Parkash, S.; Thakur, B.; Delipan, R.; Kumar, A.; Kulkarni, K.; Bansal, K.; Patil, P.B.; et al. UVC-Based Air Disinfection Systems for Rapid Inactivation of SARS-CoV-2 Present in the Air. Pathogens 2023, 12, 419. https://doi.org/10.3390/pathogens12030419
Garg H, Ringe RP, Das S, Parkash S, Thakur B, Delipan R, Kumar A, Kulkarni K, Bansal K, Patil PB, et al. UVC-Based Air Disinfection Systems for Rapid Inactivation of SARS-CoV-2 Present in the Air. Pathogens. 2023; 12(3):419. https://doi.org/10.3390/pathogens12030419
Chicago/Turabian StyleGarg, Harry, Rajesh P. Ringe, Supankar Das, Suraj Parkash, Bhuwaneshwar Thakur, Rathina Delipan, Ajay Kumar, Kishor Kulkarni, Kanika Bansal, Prabhu B. Patil, and et al. 2023. "UVC-Based Air Disinfection Systems for Rapid Inactivation of SARS-CoV-2 Present in the Air" Pathogens 12, no. 3: 419. https://doi.org/10.3390/pathogens12030419
APA StyleGarg, H., Ringe, R. P., Das, S., Parkash, S., Thakur, B., Delipan, R., Kumar, A., Kulkarni, K., Bansal, K., Patil, P. B., Alam, T., Balam, N. B., Meena, C. S., Thakur, K. G., Kumar, A., & Kumar, A. (2023). UVC-Based Air Disinfection Systems for Rapid Inactivation of SARS-CoV-2 Present in the Air. Pathogens, 12(3), 419. https://doi.org/10.3390/pathogens12030419









