Abstract
Mesocarnivores are small- or mid-sized carnivore species that display a variety of ecologies and behaviours. In Europe, wild mesocarnivores are represented by the red fox (Vulpes vulpes), the golden jackal (Canis aureus), the European wildcat (Felis silvestris), the Mustelidae of the genera Meles, Martes, Mustela, Lutra, the invasive species of raccoon dog (Nyctereutes procyonoides), raccoons (Procyon lotor), and American mink (Neogale vison). These abundant animals thrive in various habitats and often develop their activity close to human settlements. Thus, they may play an important role in the introduction, maintenance, and transmission of major parasitic zoonoses and promote bridging infections with domestic animals. Against this background, this article reports and discusses some of the most important endoparasites of wild mesocarnivores living in Europe, on the basis of their actual role as reservoirs, spreaders, or sentinels. The data derived from epizootiological studies in different European countries, and the proven or speculated implications of the detected endoparasites in human and domestic animals’ health, are discussed. Through older and recent literature review, the state-of-the-art knowledge on the occurrence and prevalence of the parasites under consideration is presented, showing further, warranted investigations and the need for surveillance and vigilance.
1. Introduction
The role of wild animals in the emergence and re-emergence of diseases, some of zoonotic concern, has been appreciated relatively recently [1]. It is typical that of all wildlife-derived zoonoses, those caused by viruses and bacteria gain most of the attention, probably because they may lead to dramatic epidemiological situations, epidemics, and pandemics. On the other hand, wildlife-derived zoonotic parasitoses usually cause less spectacular dispersion among populations, often remain asymptomatic, and due to their ways of transmission and complex life cycles, do not cause epidemics or pandemics. This may be why wildlife-associated zoonotic parasites receive less scientific and administrative attention and effort, in the frame of One Health alerts, approaches, and strategies [1]. However, human infections with parasites originating from wildlife have been identified and can be characterised as food-borne, vector-borne, and environment-borne.
Similarly, bridging infections between wild and domestic animals is a recognised phenomenon that seems to be occurring more often in recent years [2,3]. Such infections are influenced by climate change, land-use change, and novel human activities. Human exploitation of the environment led to a dissolution of natural barriers that used to function as disease control. As a result, wildlife, domestic animals, and humans share zones of sympatric habitats, where bridging infections may occur [4].
In Europe, such sympatric interactions often involve small- and mid-sized (<15 kg body weight) carnivore species, referred to by the term “mesocarnivores”. Mesocarnivores are represented by a much higher number of different species compared with large carnivores and display a variety of ecologies and behaviours. For example, these species can be solitary to highly social, may have a strictly carnivorous or an omnivorous diet and many of them are generalists regarding their habitat selection, thus they often live in close proximity to humans, occupying the top of the food chain, with no other animal species acting as a competitor. Their relatively small size and flexibility in thriving in various habitats result in the abundance of mesocarnivores in practically all kinds of environments [5]. Accordingly, wild mesocarnivores often develop their activity in proximity to humanised environments, and this has become more common in recent years, clearly because of the land-use changes, and the overall destruction and fragmentation of wild habitats and ecosystems, forcing wild animals closer to suburban and urban areas and, practically, to a territorial expansion or adaptation. This phenomenon is further enhanced by the introduction and proliferation of allochthonous species, such as the raccoon, the common racoon dog, and the American mink, which are among the most widespread invasive carnivores in Europe [6].
The expansion and proliferation of mesocarnivores results, among other things, in bridging infections and transmission of parasites of wildlife origin to humans and domestic animals [1]. For example, Baylisascaris procyonis, a parasite of raccoons, is a recognised zoonotic nematode of emerging medical importance, and Echinococcus multilocularis, a taeniid of foxes, has infected humans with an increasing trend in Europe in recent years [1,7]. Similarly, these interactions lead to spillover parasitoses between related animal species, as evidenced in the case of Angiostrongylus vasorum, passing from its main host, the foxes, to sympatric dogs, and Troglostrongylus brevior which is common in domestic cats living in sympatry with wildcats, i.e., the natural definitive host of the parasite (Figure 1) [2,3].
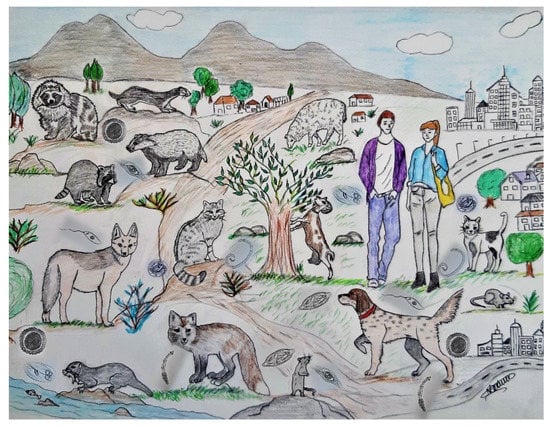
Figure 1.
Wild mesocarnivores, domestic animals, and humans in sympatric settings can lead to the transmission of important zoonotic parasites and to bridging infections between wild and domestic animals.
This review aims to explore the role of wild mesocarnivores as reservoirs and bridge hosts of important emerging parasites in Europe, taking into consideration the distribution, biology, and behaviour of these animals, and providing some basic information about the impact of the parasites on human and domestic animals’ health.
The topic is approached on an animal-group or animal-species basis. Starting with the family of Canidae, arguably the most abundant species, the red fox (Vulpes vulpes), the golden jackal (Canis aureus), and the invasive common raccoon dog (Nyctereutes procyonoides) are addressed. The family Procionidae is represented by the invasive raccoon (Procyon lotor) and Felidae by the widespread European wildcat (Felis silvestris). Finally, from the family Mustelidae, the prolific genera Meles, Martes, Mustela, Lutra, and the invasive American mink (Neogale vison), are approached under the scope of the present article. A list of the parasites discussed and mentioned in each animal species in this article is presented in Table 1.

Table 1.
The parasites discussed and reported in this article for each mesocarnivore species in Europe.
Some ideas on future strategies, based on surveillance and monitoring, regarding the prevention of further emergence of wildlife-derived parasitic zoonoses, are discussed.
2. Canidae
In Europe, the wild mesocarnivore members of the family Canidae consist of the red fox (Vulpes vulpes), the golden jackal (Canis aureus), and the raccoon dog (Nyctereutes procyonoides) [8]. The red fox and Golden jackal are indigenous species in Europe, with differences in the areas of origin and distribution. On the other hand, the raccoon dog is an alien species brought from Russia during the first half of the 20th century which then spread rapidly into many European countries (see File S1) [9,10].
2.1. Red Fox (Vulpes vulpes)
The red fox (from now on “fox”) is a very adaptable species with a generalist diet, high reproductive potential, and social flexibility [11]. These characteristics, in combination with the success of rabies control [12], allowed an increase in the fox population from the 1990s and a geographical expansion from traditionally endemic areas of central Europe to the east (i.e., western Russia and the Baltic states) and other European regions (see File S1) [13,14]. Alongside this, over time, there has been a progressive urbanisation of fox populations due to the fragmentation of their habitats, followed by easy adaptation to suburban and urban environments [15]. Typically, synurbic foxes reach higher population densities when compared with animals in wild habitats, favoured by sufficient and seasonally stable food of anthropogenic origin (e.g., waste or pet food) [16]. In urban and peri-urban areas, the frequency of contact between foxes, humans, and pets has changed from sporadic to constant, significantly increasing the chances of parasite transmission [17,18]. Parasites shared by foxes, pets, and humans in Europe have been previously reviewed [19,20]. Foxes represent the natural reservoir for various endoparasites traditionally showing a wildlife cycle, transmitted by the faecal–oral route or via intermediate hosts [20,21]. On the other hand, they act as dead-end hosts for some foodborne human infections, as in Europe fox meat is generally not consumed. However, they may represent an excellent indicator for the circulation of food-borne parasites, being nonspecific predators/scavengers, and widespread, contributing to the maintenance of parasites’ life cycle in wild settings [22,23].
In addition, they may be excellent sentinels of vector-borne diseases (VBDs), mainly because of their proximity to urban or agricultural settings and frequent exposure to different arthropod vectors (e.g., ticks, mosquitos, sand flies) for which they represent a good blood meal source [19,24,25].
2.1.1. Leishmania infantum: The Role of the Red Fox Is Still Unclear
Leishmaniosis is a severe parasitic disease caused in Europe by the kinetoplastid protozoon L. infantum, transmitted by sand flies of the genus Phlebotomus [26]. The role of several wild canid species as potential primary or secondary reservoirs has been investigated due to their close phylogenetic relationship with the main reservoir, the dog.
A consistent exposition to Leishmania infection was demonstrated in fox populations in Europe, by serology and molecular surveys, with prevalence ranging widely [27]. The lowest prevalence values were detected in France (9–15%) [28,29] and Georgia (2.6%) [30] and the highest in the highly endemic regions of the Mediterranean Basin, i.e., Italy (6–50%) [31,32,33,34], Greece (59.5%) [35], and Spain (12–74%) [36], usually in line with those recorded in dogs in the same areas. However, the rates of parasite detection in the skin of foxes vary greatly, from 0% to 34% in highly endemic areas [32,33] and are much lower if compared to deep organs (i.e., spleen, bone marrow, or lymph nodes). These findings lead to the speculation that foxes might be less capable of infecting phlebotomine vectors than dogs, as dogs’ skin shows positive rates similar to or even higher than deep organs [37]. However, further studies are needed to elucidate the role of foxes in the epidemiology of L. infantum.
Entomological surveys conducted in Europe showed that foxes act as a good blood source for Phlebotomus pernicious, and frequently share an ecosystem with rabbits and hares that are proven amplifier hosts of the parasite [38,39]. However, to date, there have been no investigations regarding the infectiousness of foxes to sandflies (xenodiagnosis). In fact, studies carried out in Brazil showed that Lutzomia longipalpis (the main vector of Leishmania chagasi in the New World) did not become infected after blood meals on infected crab-eating fox (Cerdocyon thous) [40].
Most studies on foxes indicate that infected animals do not present any clinical signs. However, in Greece, the majority of the animals examined (63.8%) showed at least two to three clinical signs compatible with canine leishmaniosis (CanL), including low weight, dermatitis, skin lesions, alopecia, splenomegaly, enlargement of lymph nodes, and onychogryphosis [35].
2.1.2. Babesia spp. and Hepatozoon spp.: The Red Fox as a Competent Reservoir
Red foxes have been identified as reservoirs for tick-borne pathogens (TBPs), including hemoprotozoan organisms of the genera Babesia and Hepatozoon [41].
In Europe, Babesia canis is the main species infecting dogs, and although it has also been reported in foxes, these animals do not seem to act as a reservoir of the parasite [42]. A second species causing babesiosis in dogs, i.e., Babesia vogeli, was also reported in red foxes in France [43].
However, red foxes have been proposed as the natural host of Babesia vulpes (syn. B. microti-like piroplasm, Babesia sp. “Spanish dog”, Theileria annae) [44,45], due to their high infection rates and the absence of clinical signs in most of the cases. The effective tick vector of B. vulpes is still unknown [46], but Ixodes hexagonus, a triphasic hard tick with esophilic behaviour, has been speculated as a potential vector [47].
The highest prevalences of fox infection with B. vulpes in Europe are recorded in Portugal and Spain, where 68% to 100% of animals are infected, depending on the sample nature (blood or bone marrow) and the analysed geographic area [48,49]. The presence of B. vulpes at high prevalence was also described in Germany (46.5%) [50], Austria (50.7%) [51], and Italy (5–69.2%) [52,53], while in other countries, the prevalence is lower, e.g., 20.7% in Romania [54], 20% in Hungary [55], 32% in Bosnia and Herzegovina, [51], 30.7% in Poland [46], and 5% in Croatia [56]. The pathogenic consequences of B. vulpes in red foxes have not been thoroughly studied. However, enlargement of both kidneys and the spleen has been observed in necropsied infected foxes [46].
Hepatozoon canis is commonly detected in European fox populations. Hepatozoon infection is acquired through the ingestion of an infected ixodid tick. In southern Europe, Rhipicephalus sanguineus sensu lato (s.l.), widely distributed and strongly associated with dog presence, is considered the main vector of the parasite [57]. However, in areas where R. sanguineus s.l. is not endemic (e.g., Austria, Slovakia, Germany, Poland), the role of alternative species, e.g., Ixodes ricinus and Dermacentor reticulatus as competent vectors has been speculated [42]. Alternative routes of H. canis transmission are transplacental, proven in both foxes and dogs [51], and the consumption of infected prey carrying H. canis tissue cysts [58].
A high prevalence of H. canis has been detected in fox populations from central and southern Italy (50%) [34,52], Germany (45.2%) [50], and Poland (44.7%) [46], with higher values in Portugal (75.6%) [59], Serbia (61.2%) [60], and the Czech Republic (95%) [61], while lower rates were recorded in Bosnia and Herzegovina (38.6%) [51], Croatia (23%) [56], Austria (18.5%) [62], Slovakia (17.1%) [63], and Hungary (8%) [64]. Hepatozoonosis in foxes, similar to dogs, generally develops as a subclinical infection; however, a slightly enlarged spleen and liver may be observed [46].
2.1.3. Dirofilaria immitis and Dirofilaria repens: Red Foxes Are Infected but Not Quite Infectious
The fox has been proven able to act as a definitive host for both Dirofilaria immitis and Dirofilaria repens (the causative agents of canine cardiopulmonary and subcutaneous dirofilariosis, respectively) but infections in foxes are generally regarded as an epiphenomenon of the dog infection in overlapping habitats [19]. Since foxes tend to show lower levels of heartworm infections (the burden of D. repens infection is more difficult to be estimated) and lower microfilaremia compared to dogs [65], it has been speculated that they are not an epidemiologically important host for competent vectors and thus they are of minor significance from an epidemiological and a public health perspective [66].
In the traditional endemic areas of southern Europe, infection in foxes is reported with prevalences between 1.5% and 30% for D. immitis and from 1.2% to 22% for D. repens [43]. However, the presence of filarial infections in low endemic areas, i.e., Hungary [67], Romania [68], Russia [69], and Serbia was also reported with prevalences between 0.3–8.5% and 0.7–6.4% for D. immitis and D. repens, respectively [70].
To date, the clinical impact of these two major filarids in foxes is unknown and deserves future investigation.
2.1.4. Thelazia callipaeda: Red Foxes as an Important Source of Infection
Thelazia callipaeda is a vector-borne zoonotic nematode with the zoophilic fruitfly Phortica variegata as the only confirmed vector in Europe [71]. Thelazia callipaeda lives in the conjunctival sac and associated tissues of a relatively large spectrum of hosts, including carnivores, lagomorphs, and humans [72].
The importance of foxes in the epidemiology of T. callipaeda in different habitat types across Europe has been documented by the high prevalence of infection and the speculated frequent contact of foxes with the vector, favoured by the co-occurrence of the seasonality and crepuscular activity of P. variegata and fox activity patterns [51,73,74].
Thelazia callipaeda is endemic in fox populations of Italy, France, and Switzerland, but has also been expanding to various hosts in regions of Portugal, Greece, and Balkan areas [51,75,76]. The prevalence rates vary within large limits, from low, i.e., 5.1% and 5.7% in northern Italy and Switzerland, respectively, [77,78] to medium, i.e., 27.7% and 29.4% in Bosnia and Herzegovina, and Romania, respectively, [51,74] and high, i.e., 49.3% in southern Italy [79]. The occurrence of a unique genetic haplotype (h-1) of T. callipaeda in all specimens examined from foxes and pets suggests that this parasite circulates among domestic and wild carnivores in all areas where it has been reported [72].
The zoonotic potential of T. callipaeda is of concern mainly in rural areas of southeast Asia [80,81], however, ophthalmologists and general physicians should be particularly alert to possible human cases in all areas where the infection is known in foxes and other hosts [82]. In fact, sporadic human cases in Europe have been diagnosed in endemic countries, i.e, Italy, France [83], Spain [84], Serbia [85], Germany [86], Croatia [87], Portugal [88], and Hungary [89].
2.1.5. Toxoplasma gondii and Trichinella spp.: The Red Fox as a Sentinel of Occurrence
Toxoplasma gondii and Trichinella spp. are food-borne pathogens of worldwide importance in human and veterinary medicine. Foxes do not serve as a direct source of human infection in European countries; however, they represent an excellent sentinel for the circulation of these parasites, which are typically present in predatory and scavenger wild carnivores [90]. Furthermore, foxes may have an active role in the maintenance and propagation of these parasites in the sylvatic cycle.
Toxoplasma gondii (see Section 4.1.1) can infect foxes through ingestion of sporulated oocysts (e.g., via contamination of food, water, soil), but more frequently, via predation of infected prey harbouring tissue cysts. Vertical transmission has also been proposed, as in other hosts, but there is no clear evidence of this [91].
A high level of fox populations exposition to the parasite is documented as a result of the cumulative effect of consuming infected prey. The highest Toxoplasma seroprevalence in foxes is detected in central eastern countries reaching up to 35% in Austria [92], 75–85% in Germany [93], and 100% in the Czech Republic and Belgium [94,95].
Genotyping of T. gondii isolates in red foxes has been performed only in a few studies, showing that most of the isolates belong to the clonal type II or mixed clonal type II and III [93,96] that represent typical archetypal lineages of the anthropogenic food sources [97].
Only scarce information is available regarding the clinical impact of T. gondii in foxes; however, apparently red foxes tolerate T. gondii infection very well in the absence of immunocompromising factors (i.e., canine distemper virus (CDV), vulpine circovirus (FoxCV)), compared with other fox species, i.e., blue foxes (Vulpes lagopus). In fact, experimental studies demonstrated that when oocysts or tissue cysts of the highly pathogenic strains GT-1 or TC-1 are fed to red fox puppies, the animals do not develop any clinical signs [98], contrary to experimentally infected blue foxes (Vulpes lagopus), which develop severe clinical toxoplasmosis after parenteral infection with tachyzoites of the highly virulent RH strain [99].
Interestingly, recent studies suggest that T. gondii, due to its neurotropism and the predilection for specific sites, is able to manipulate intermediate host behaviour in order to enhance transmission (i.e., limbic system) [100] and to trigger aberrant behaviour in foxes. An association between toxoplasmosis and a range of aberrant behavioural traits known as “dopey fox syndrome” (DFS), was speculated [101].
Of the 12 nematode species that comprise the genus Trichinella, 4 (Trichinella spiralis, Trichinella britovi, Trichinella nativa, and Trichinella pseudospiralis) circulate in Europe, showing different host ranges, geographical distributions, ecology, and histopathological features (i.e., encapsulated/not-encapsulated larvae) [102]. Trichinella spp. Has a peculiar monoxenic life cycle: carnivorous, omnivorous, and occasionally herbivorous animals are identified as hosts of the parasite, whose transmission occurs through the ingestion of infected meat containing the first larval stage [102]. Adult nematodes in the intestine produce larvae which migrate within the skeletal and cardiac muscles, causing clinical disease in susceptible hosts (e.g., humans).
A wide range of carnivores can harbour infective larvae of Trichinella spp., but foxes are considered the main reservoir of the sylvatic cycle and reflect the parasite’s presence in the food web since they are cumulatively exposed to infection due to their food habits [103]. There is contradictory information in scientific papers regarding the distribution of Trichinella larvae in the muscles of naturally infected foxes; however, a number of studies showed that the highest infection intensity is usually recorded in muscles of the trunk and head (i.e., masticatory muscle, diaphragm, intercostal muscles, and tongue root muscles) [104].
The prevalence of Trichinella spp. in fox populations varies significantly in European countries, with the lowest values (0.9–5%) observed in southern and western Europe and the highest (up to 40%) in the endemic northeastern regions (i.e., Finland, Serbia, Romania, Bulgaria, and Russia) [105,106]. In most cases, T. britovi has been identified in foxes, and only sporadically T. spiralis, suggesting a major role of the fox as a reservoir of T. britovi (sylvatic cycle), and a lower importance in the epidemiology of T. spiralis in the domestic cycle [107].
2.1.6. Echinococcus multilocularis: The Red Fox Is the “Usual Suspect”
Echinococcus multilocularis is a small tapeworm of the Taeniidae family with a typical prey–predator life cycle [108] that develops predominantly in sylvatic environments and rural settlements. The adult parasite lives in the small intestine of wild carnivores (definitive hosts), producing mature proglottids with eggs that are released into the environment via the faeces. Small rodents of the family Arvicolidae and Muridae (e.g., Microtus arvalis; Apodemus spp.) act as intermediate hosts and become infected by ingesting (e.g., via food or water) the eggs of the parasite. The larval (metacestode) stage of the parasite, the alveolar cyst, develops in the liver and other internal organs of the intermediate host [108,109]. In Europe, the fox is considered the main definitive host of E. multilocularis, and together with raccoon dogs, is used as sentinel by the monitoring system of the EFSA Council [110].
Historically, endemic regions for E. multilocularis in Europe consisted of a ‘core’ area including southern Germany, eastern France, north-central Switzerland, eastern Italy, and western Austria, where prevalences in foxes ranges from 15–65% [7,111,112]. However, broad epidemiological studies reported a significant expansion of the parasite to northern and eastern countries, i.e., Denmark, Sweden, Lithuania, Estonia, and Poland [7,113], with peaks observed in Estonia (29.4%) [114], Latvia (35.6%) [115], and Lithuania (58%) [109].
Echinococcus multilocularis is the causative agent of alveolar echinococcosis (AE) in humans, a serious disease that can be fatal if left untreated [109]. The prevalence of human AE cases in Europe is approximately proportional to the prevalence of infection in the definitive hosts (mainly foxes) and displays a significantly increasing trend since 2010 [116]. Moreover, human cases of AE are being reported more frequently in urban areas, as a consequence of the urbanization of the E. multilocularis life cycle, due to the approach of foxes to the peri-urban/urban environment [19]. Although E. multilocularis prevalence in foxes in such environments is usually lower than in rural and wild settings, because foxes consume a lower proportion of intermediate hosts, the enlarging fox densities in urban settings may enhance the risk of bridging and zoonotic infections in these particular areas [117].
In Europe, surveys revealed that adult foxes, due to partial immunity acquired after exposure, display a lower prevalence of infection and lower worm burdens than foxes under one year of age, rendering young foxes the main drivers of infection spread [118]. This finding is different for T. gondii and Trichinella spp. for which adult animals show a higher prevalence of infection due to the long life of these parasites in host tissues that remain viable for many years (Trichinella spp.) or even lifelong (T. gondii) after the first infection of the host [119].
2.1.7. Angiostrongylus vasorum and Airway Capillarioses: Red Foxes Contribute to Their Expansion
The fox is considered the major reservoir host and spreader of Capillaria aerophila (syn. Eucoleus aerophilus) and Capillaria boehmi (syn. Eucoleus boehmi), the agents of the lung and nasal capillariosis, respectively, and Angiostrongylus vasorum, also known as French heartworm [19,21,120,121,122]. In the last two decades, these parasites have been recognised as emerging agents of disease in dogs in several European countries [122].
The capillarids of the airway are typical soil-transmitted nematodes, with a direct cycle: immature eggs are excreted with the faeces of the definitive hosts, and the infective L1 develops inside within 15–40 days for C. boehmi and 35–60 days for C. aerophila [123]. Infection is acquired through the ingestion of embryonated eggs, while earthworms are suggested to act as facultative intermediates or transport hosts [123].
Capillaria aerophila and C. boehmi share common patterns of transmission and thus are frequently detected in co-infections. Foxes show rates of positivity that vary a lot (from 4% to 100%) among different geographical European countries. More precisely, C. aerophila infection in foxes reaches 97% in Lithuania, 88.8% in Norway, 84% in Serbia, 76.2% in Poland, 75% in Germany, 66% in Hungary, and 65% in the Netherlands [124,125,126,127,128,129,130,131]. The Capillaria boehmi infection rate in foxes ranged from 8% in Hungary [130] to 30.7–51% in Italy and Norway [21,126,132], whereas the highest prevalence (90%) has been recorded in Serbia [127].
Few cases of human infection by C. aerophila mimicking the clinical and radiographic findings of pulmonary bronchial carcinoma have been described in Europe, i.e., Russia, Ukraine, France, and Serbia [127,133,134], where the prevalence of infection in foxes is high (up to 84%).
Angiostrongylus vasorum is a metastrongyloid nematode characterised by an indirect life cycle: definitive hosts (domestic dogs and wild canids) acquire the infection by the ingestion of infected gastropods harbouring the infective third-larval stage (L3) or of paratenic hosts, such as frogs, birds (e.g., Rana temporaria, Gallus gallus domesticus), and other small vertebrates [135,136,137].
Angiostrongylus vasorum was traditionally endemic in southwestern France, the UK, and Denmark [138], where infection in dogs was documented in isolated foci with only sporadic occurrence outside those areas. However, over the last 20 years, an expansion of the parasite’s geographical range and spreading to new geographical areas (e.g., Italy, Bulgaria, Slovakia, Poland, Serbia, Belgium, Romania) has been documented [122,139,140]. The decisive factors of this expansion include growing fox populations, the movement of dogs from endemic to non-endemic areas, and climate changes impacting the intermediate hosts’ epidemiology, as observed in other snail-borne diseases [141,142]. After the first detection of A. vasorum in British foxes [143] a number of epidemiological surveys were conducted in these animals and variable rates were recorded with higher prevalence found in central Italy (75–78%) [132,144] and north-eastern Switzerland (81.8%) [145], followed by Great Britain, Hungary, Norway, Poland, Republic of Ireland, Romania, Serbia, Slovakia, Spain, and the Netherlands, with rates up 43% [144].
Unlike dogs, in which A. vasorum infection may show a wide spectrum of clinical manifestations, ranging from no or minor clinical signs to life-threatening disease [146], foxes usually exhibit chronic infections with mild clinical signs that occur when concurrent infective diseases and high worm burdens are present [141,147]. However, fatal infections in foxes have been recently described [148].
2.1.8. Other Parasites
Foxes may harbour various parasites in addition to those mentioned above, which may be shared with pets and/or have zoonotic implications.
Foxes may get infected with cyst-forming parasites further than T. gondii by prey or carrion consumption, especially mice and deer; in fact, foxes may act both as intermediate and definitive host for Neospora caninum, despite the fact that to date, no active oocyst shedding has been described in foxes in Europe. Biomolecular and serological surveys showed low to moderate prevalences of N. caninum infection in foxes in Europe, lower than those recorded for T. gondii [95].
Low to medium rates of positivity for Cryptosporidium parvum and Giardia duodenalis have also been detected [149,150]. Foxes may also show patent infections through a wide range of tapeworms of the genus Taenia, especially those transmitted through predation of rodents or rabbits/hares, i.e., Taenia crassiceps, Taenia pisiformis [151,152], and Mesocestoides spp. [153]. On the other hand, Echinococcus granulosus s.l. is very rarely detected in foxes and usually with low burdens [19].
Foxes are also suitable definitive hosts for various species of trematodes. Among those, the most important in terms of frequency and public health implications are the meat-borne intestinal fluke Alaria alata [154] and the fish-borne liver fluke Opisthorchis felineus [90].
Typical soil-transmitted nematodes in dogs, e.g., Trichuris vulpis, Toxocara canis, and Uncinaria stenocephala may equally have foxes as natural hosts [20,155,156]. In contrast to the high prevalence observed for U. stenocephala, a scant detection of the other ancylostomatid, Ancylostoma caninum, is recorded [20].
Among the extra-intestinal parasites, Crenosoma vulpis and Capillaria plica are also being recorded at high prevalences in foxes [157] and a new species of the genus Spirocerca, i.e., Spirocerca vulpis, is emerging in foxes from Bosnia, Herzegovina, Italy, and Spain [158]. Interestingly, S. vulpis exhibits a different nodule location, focused on the stomach wall compared to the most known Spirocerca lupi, which mainly develops in the oesophagus and aorta of dogs and wolves [159].
2.2. Golden Jackal (Canis aureus)
At the beginning of the century, the population of the Golden jackal (from now on “jackal”), also known as the common or Asiatic jackal, Eurasian Golden jackal, or reed wolf [160,161], in Europe declined dramatically; however, a notable expansion started in the 1950s, allowing a progressive recolonisation in Europe [162,163]. Currently, stable, reproducing populations with high densities are being recorded in approximately 20 countries in central and eastern Europe, while in others, sporadic vagrant animals are observed (see File S1) [164]. The factors favouring the territorial expansion of jackals are unclear, but land use, climate change, and the lack of natural predators have been suggested [165].
The jackal has an opportunistic nutritional behaviour with an extremely varied diet consisting mostly of small mammals, birds, and their eggs, but is also a scavenger and is capable of using anthropogenic food sources [162]. This wide food spectrum, their relatively broad territorial mobility (from 1 to 20 km2), and their ability to adapt to novel habitats both in suburban and urban areas allow jackals to come into contact with animals that live in close proximity to humans, such as dogs and foxes [162]. With this in mind, taking into account that jackals act as hosts to a wide variety of canine and zoonotic parasites, it should be considered that they may play an important role in bridging infections to domestic animals and humans [162,166].
2.2.1. Dirofilaria immitis and Dirofilaria repens: Golden jackals Are Suitable Spreaders
Jackals are considered a potential wild reservoir of filaroids in endemic areas of Europe, particularly for D. immitis, as they are frequently found infected both in necropsies (adult worms) and in blood examinations (microfilariae), and excessive microfilaremia are recorded in up to 50% of infected animals [19,68,167]. On the contrary, D. repens has been found in the blood of jackals by molecular methods at a low prevalence (3%) [68].
In endemic areas, the spatial distribution and prevalence of D. immitis infection are similar to those recorded in dogs, suggesting that jackals might play a role in the transmission and the maintenance of the parasite comparable to dogs, i.e, the primary definitive host [68]. In fact, unlike dogs, jackals are out of any preventative control and represent a good blood source for Aedes albopictus and Culex pipiens complex mosquitoes, which are the most efficient vectors of D. immitis in Europe [68]. The highest prevalence of D. immitis infection in jackals is recorded in the Balkans and central European countries, e.g., Bulgaria, Serbia [168], Hungary [67], and Romania [68], where it reaches up to 35% of animals.
2.2.2. Other Parasites
Jackals can be exposed to several vector-borne pathogens that primarily affect dogs, suggesting the hypothesis of bridging infections. For instance, L. infantum, B. canis, and H. canis have been found at the margin of the endemic areas of CanL and canine babesiosis [162] and to date they are the only species isolates in jackals in Europe.
From the public health impact point of view, jackals should be considered a natural sylvatic reservoir of Trichinella spp. The most common species isolated in this animal species is T. britovi; however, in the Balkans T. spiralis has also been identified [169]. Since vagrant individuals may migrate for long distances, they may contribute to the introduction and spread of this parasite in neighbouring countries where Trichinella spp. is less prevalent (i.e., Greece, Italy, and northern Macedonia).
Jackals may also serve as the definitive host for both E. granulosus and E. multilocularis [109]. In fact, this wild canid frequently preys on rodents, including arvicolins and other easily available food sources, such as viscera and carrions that may promote infection with Echinococcus spp. [170]. In the European continent, the fox and the domestic dog remain the major definitive hosts of E. multilocularis and E. granulosus, respectively, (see Section 2.1.5) and jackals and other wild canids, i.e., the raccoon dog, have an inferior importance in the sylvatic and domestic life cycles of the parasites, in particular of E. granulosus [171]. However, they have been identified as definitive hosts for E. granulosus in Hungary, Bulgaria, and Italy [166]. There is a general agreement, that in central and eastern European regions where E. multilocularis prevalence is high in foxes, a correlated low to moderate infection prevalence (up to 5%) can be also observed in secondary definitive hosts such as jackals, raising a question on the role of this wild canid as an additional, albeit minor, reservoir and infection source for humans [109,172,173]. In fact, E. multilocularis was detected in jackals from Hungary, Serbia, Croatia, Austria, and Switzerland [166].
The presence of traditional soil-transmitted nematodes is described in jackal populations in Europe but with low to moderate prevalences compared to other wild canids (i.e., wolf, foxes, raccoon dogs) [162]. However, a relatively prevalent presence of tapeworms, i.e., Dipylidium caninum, Multiceps multiceps, and Mesocestoides spp. is documented [162]. A widely distributed trematode in jackals is A. alata, found in Russia and in the Balkans [174].
Finally, jackals have also been found to be infected with a wide range of extra-intestinal nematodes, i.e., A. vasorum, S. lupi, C. plica, C. aerophila, and T. callipaeda, but the reports are scant [162,175]. In Europe, T. callipaeda was found only in one jackal in Romania, with high intensity of infection (70 nematodes) [175]. The absence of similar findings in other areas is probably due to a lack of full post-mortem examination (e.g., when the eyes are damaged) and thus it cannot be excluded that jackals may act as a potential reservoir host of this parasite.
2.3. Raccoon Dog (Nyctereutes procyonoides)
The raccoon dog originates from east Asia and is one of the most successful invasive carnivores in Europe. It was introduced in the western Soviet Union for its fur in the middle of the 20th century [176,177]. The successful control of rabies from the 1990s, together with the high reproductive capacity and behavioural adaptation of this species, led to its successful establishment and expansion all over Europe (see File S1) [13,178]. One of the major threats arising from the growing and expanding population of raccoon dogs is linked to their role in maintaining and transmitting various parasites, some of high zoonotic concern, for which raccoon dogs may act as important definitive hosts in wild environments [13,179,180].
Trichinella spp., Echinococcus multilocularis and Other Parasites
The raccoon dog is a suitable indicator and a well-adapted host for all four species of the genus Trichinella circulating in Europe (see Section 2.1.5) [181], which can be detected in single or mixed infections. This wild canid plays an important role, especially in spreading T. spiralis and T. britovi through the sylvatic cycle in north-eastern European countries [182,183]. The prevalence of Trichinella infection in raccoon dogs varies widely between different European regions, from 0% in Denmark and Austria, to 1.9–4% in Germany, 33.2% in Finland, 35.5% in Lithuania, 32.5% in Latvia, and 57.5% in Estonia [176,184,185,186,187].
Although little information is available on the predilection of raccoon dog muscles to Trichinella infection, an experimental infection with T. spiralis and T. nativa showed that the highest larval loads were detected in the foreleg, eye, and tongue muscles of the animals [188].
The raccoon dog has been documented as an additional definitive host for E. multilocularis in Europe, as it is highly susceptible to this parasite [109,189,190]. With the exception of Slovakia, where E. multilocularis prevalence in raccoon dogs is ~27% [191], i.e., similar to that recorded in foxes [105], in countries of high endemicity (Germany, Poland, Czech Republic, Slovakia, Switzerland, Austria, and Lithuania), these animals are less frequently infected than foxes, with prevalences ranging from 1.6% to 8.2% [180,192]. The different feeding preferences of the raccoon dog (amphibians) compared to fox (rodents) could be the reason for the prevalence difference of such taenidae [178]. Actually, although the raccoon dog may act as a definitive host for E. multilocularis, there is no evidence that it could maintain the life cycle of the parasite in the absence of the main reservoir, i.e., the fox [189].
A parasite detected in raccoon dogs with an increasing frequency in some European countries is A. alata, with a prevalence from 30% in Austria [186] to 96.5% in Lithuania [151,178]. The adult stage of this trematode has been found in the intestine of raccoon dogs with little pathogenic relevance; however, the larval stage (mesocercariae) found in paratenic hosts, e.g., wild boars (Sus scrofa), is pathogenic and represents a problem of public health concern [193].
3. Procionidae
The mesocarnivores of the family Procionidae include several mammals native to North and South America [194]. The raccoon (Procyon lotor), represents the only procionid established as an alien species in several European countries and areas of the Caucasus [195].
3.1. Raccoon (Procyon lotor)
The raccoon was introduced into Europe and Asia in the early 20th century, where it was released for hunting purposes or escaped or was set free from captivity (i.e., fur farms, houses) [196]. Despite the fact that most of the raccoon populations in Europe do not reach high densities, over 100 animals per km2 have been detected in some peri-urban areas of Germany, i.e., the country hosting the largest population outside America [183,197]. Stable populations are currently developing in Spain and France and some newly established populations are present in many central, northern, and eastern European countries (see File S1) [198,199]. Te raccoon’s success as an introduced species is attributed to its adaptability to different environments, omnivorous feeding habits, high reproductive potential, and the lack of natural predators [199,200].
One of the major threats arising from the growing and expanding population of raccoons in Europe is related to pathogens that are transmittable to humans and domestic animals [200]. Raccoons in Europe seem to have an impoverished parasitic fauna compared with those of the North American populations, both in terms of species diversity and abundance of parasites, although they have acquired a few parasite taxa endemic in Europe [201]. In any case, raccoons represent a potential source of exotic parasite spillover to other wild animals, dogs, and humans.
Baylisascaris procyonis, Strongyloides procyonis and Other Parasites
Baylisascaris procyonis is an ascarid nematode, characterised by its particular zoonotic importance and severe implications for human health [202]. Raccoons and related procionids are the main hosts of this parasite, which can also develop to the adult stage in dogs [203]. It is a typical geohelminth, acquired through oral–faecal transmission from the environment. The infected host sheds millions of eggs daily that become infective (containing the third-stage larva, L3) in approximately 10–12 days and remain infective for months or years [204]. In Europe, B. procyonis infection in raccoons has been documented in over 70% of raccoons in central Germany [196,205] and in 33.3% in Italy at necropsy [206]. Raccoons infected with B. procyonis usually do not exhibit clinical signs [203]. However, heavy burdens have been associated with intestinal obstruction [207,208].
A wide range of mammals, including humans, may accidentally ingest infected eggs from the environment with subsequent health implications. Raccoons, adapted to peri-urban and urban areas, defecate at latrines close to their resting places in peri-domestic sites, e.g., barns, lofts, attics, chimneys, or garages [196]. This typical behaviour increases the risk of human and dog exposure to B. procyonis infection [209].
When humans accidentally ingest the infected eggs, L3 hatch and may start their plurivisceral migration, causing ocular and visceral larva migrans syndrome (OLM, VLM), which may become fatal when larvae invade the central nervous system (neural larva migrans syndrome, NLM), causing eosinophilic meningoencephalitis with progressive neurological disorders [210]. Human baylisacariosis is an emerging zoonosis, usually described in patients (often children) who had close contact with these animals [202,211]. In Europe, human baylisacariosis has been documented only once, in Germany, in a patient who had purchased a raccoon from a local zoo and presented with unilateral neuroretinitis syndrome [212].
Another parasite strongly associated with raccoons is Strongyloides procyonis, a threadworm infecting mainly the small intestine. The biology of S. procyonis is poorly known, and presumably similar to that of Strongyloides stercoralis, in which infective filariform larvae from the environment enter the host through transdermal penetration and follow the tracheal migration until they reach the small intestine where they mature into female adults that produce eggs through parthenogenesis. Larvae hatch from eggs directly in the intestinal mucosa, initiating autoinfective cycles with a remarkable persistence within the host [213].
The first descriptions of S. procyonis in raccoons are from North America [214], while to date, in Europe the parasite was found in raccoons in Poland [215] and recently in central Italy, where a parasitological investigation showed a prevalence of 26.9% [201]. Susceptibility of dogs to S. procyonis has been experimentally demonstrated [216], as well as that of humans, through a healthy volunteer who developed a short-lived intestinal infection [217]. However, S. procyonis in humans and dogs may be confused with the morphologically similar, most common species S. stercoralis [218], resulting in an overall underestimation of S. procyonis occurrence. Such an underestimation could also be favoured by the fact that the detection of parasitic females of S. procyonis is not easy, even after a thorough inspection of the mucosa scraped from the whole length of the intestine.
The emergence of this exotic parasite does not appear particularly alarming from a public health point of view, as it is known to cause at most mild dermatitis in humans [217]. However, the course of infection in immunocompromised individuals or animals remains unknown, as well as the impact on naïve native mesocarnivores (e.g., mustelids) that share habitats with raccoons. To properly assess the potential health threats to indigenous domestic and wild species, field surveys as well as laboratory characterisation of the sparsely known biology of S. procyonis are necessary.
Raccoons may also be rarely infected with other endoparasites shared with domestic and wild canids, i.e., Leishmania spp., D. immitis, T. gondii, and Trichinella spp., but their role in the transmission and epidemiology of these parasites is insignificant or still not well defined in Europe as in raccoons’ native countries.
4. Felidae
The wild members of the Felidae family in Europe are the Eurasian lynx (Lynx lynx), the Iberian lynx (Lynx pardinus), and the European wildcat (Felis silvestris) [219]. Both Lynx species are classified into the large carnivores of Europe [220], leaving the European wildcat the only representative of the family in the group of wild mesocarnivores [221].
4.1. European Wildcat (Felis silvestris)
The European wildcat (from now on “wildcat”) is widespread in Europe, with its largest population in the eastern-central, eastern, and south-eastern continent (see File S1) [222]. Although the species is assessed as least concern (LC) by the International Union for Conservation of Nature (IUCN), and despite the limited reliable data on the trends of its range and size, the populations are estimated to be declining in most areas, with an overall fragmented distribution [222]. The fragmentation and destruction of wildcat habitats are among the reasons for the observed declining population and results in forcing the animals closer to human settlements and domestic animals. This is an important drive for spreading wildcat parasites further from the sylvatic cycles to the margins of wild and humanised environments, rendering spillovers a realistic scenario [3]. Wildcats host a great number of different parasites [223,224,225,226], but in this article, some of the most important, in terms of bridging infections and public health, are presented.
4.1.1. Toxoplasma gondii: The European Wildcat Is a “Master of the Game”
Felids have the “privilege” of maintaining the circulation of the protozoan parasite T. gondii in nature as the only definitive hosts, developing the enteroepithelial phase of the parasite’s life cycle and shedding oocysts to the environment via their faeces [226]. Wildcats were confirmed as definitive hosts of T. gondii approximately 30 years after the discovery of the parasite’s lifecycle [227,228]. A great range of vertebrates serve as intermediate hosts, including humans, and interestingly the infection has even been documented in species living in environments where the definitive hosts are not present, e.g., in polar bears (Ursus maritimus) in the Arctic [229]. In intermediate hosts, but in felids as well, the parasite develops tissue cysts. Both definitive and intermediate hosts may be infected by three routes of transmission: by ingesting sporulated oocysts from the environment (soil, water), by consuming raw meat with tissue cysts, and vertically, i.e., transplacentally or lactogenically [230]. Toxoplasma infection is usually asymptomatic in felids, but clinical disease may occur in other animals and humans. Accordingly, T. gondii is an important abortive agent in small ruminants and the cause of neurological disorders in many other species [231]. Infections with occasionally fatal outcomes have been reported in many wildlife species, e.g., red foxes, mustelids and other carnivores [230], red squirrels [232], and lagomorphs [233]. In humans, clinical toxoplasmosis usually occurs in immunocompromised patients, and it is also detrimental in congenital infections, causing encephalitis, retinochoroiditis, multiple organ damage, and death [231].
Infection in wildcats in Europe has been documented in a number of surveys. A total of 5 out of 6, 3 out of 6, and all 23 examined wildcats were found T. gondii seropositive in southern Portugal, Spain, and Great Britain, respectively [234,235,236], while in a wider serosurvey in France, 75 out of 112 wildcats (67.0%), were found seropositive [237]. Molecular detection of the parasite was successful in 4 out of 12 wildcats examined in Germany [238]. According to a recent systematic review and meta-analysis of the literature, the wildcat is ranked only second to the lion (Panthera leo) in terms of T. gondii seroprevalence [239].
Among the spreaders of T. gondii in Europe, i.e., the felids, wildcats hold an important position because of their wide geographical dispersion, their proliferation in various environments, and their high frequency of infection due to their predatory nature. Although it was evidenced that wildcats are infected equally prevalently as stray rural cats in France [237], other studies show an impressively high, and in some cases universal infection of the examined sample [234,236]. This is not surprising, as wildcats are exclusively fed by prey and have no access to, nor preference for, human-made food, a behaviour resulting in a higher prevalence of parasitic infections and polyparasitism compared to domestic cats, even stray ones [240]. For this reason, wildcats hold a key role in the circulation of the parasite in sylvatic and rural-suburban environments and subsequently in the infection of other wild and domestic animals, and humans. The risk of human infection at the conjunction of the sylvatic and domestic cycles is enhanced by the fact that the market and the trend for game meat consumption is currently under development, as consumers turn to more healthy and natural food options [154]. Tissue cysts of T. gondii in the meat of wild animals, e.g., hares, cervids, and wild boars, is a source of human infection when consumed raw or undercooked, while it has also been evidenced that people handling game meat (evisceration, skinning) are also at risk of infection when proper hygiene measures are overlooked [91].
4.1.2. The Haemoparasites Hepatozoon spp., and Cytauxzoon spp.
The apicomplexan parasites Hepatozoon spp. and Cytauxzoon spp. are blood-associated TBPs that can infect wild and domestic felids. The feline hepatozoonosis and cytauxzoonosis vectors are unknown and various hard tick species may be involved [241]. Wildcats and stray domestic cats are more prevalently infected than domestic cats that live indoors, as they are more frequently exposed to tick vectors. In fact, wildcats are important for the maintenance of the sylvatic cycle of VBPs and likely play an important epizootiological role in spillover infections to domestic animals [241].
Feline hepatozoonosis is typically subclinical, but fatal myocarditis due to H. silvestris in a domestic cat has been recently reported [242]. Wildcats and domestic cats share two different Hepatozoon species (Hepatozoon felis and Hepatozoon silvestris [243,244,245]) while molecular and phylogenetic analysis support the hypothesis of a species-complex classification for H. felis [246,247]. Hepatozoon spp. is transmitted when the host ingests a tick containing the infective oocysts of the protozoan [248]. This particularity in transmission compared to the typical VBPs transmission, i.e., by a vector blood meal, is associated with the high prevalence of Hepatozoon infections in felids due to grooming behaviour, and also to infection through ingestion of parasite cystozoites in prey tissues [246,249]. Thus, because of their exclusively predatory lifestyle, wildcats are expected to be more frequently infected than domestic cats and are likely the source of bridging infections to domestic cats in areas of sympatry.
Cytauxzoonosis caused by Cytauxzoon felis was first described as a severe disease in domestic cats in the USA, while its natural host is the bobcat (Lynx rufus) [250]. Schizonts are formed in the macrophages of felids after their inoculation with Cytauxzoon spp. through a tick bite, resulting in multiple organ failure and clinical cytauxzoonosis in domestic cats [251]. In Europe, however, different parasite species exist and infections in domestic cats are generally less severe, although some heavy and even fatal cases have been reported [252]. Three species have been genetically described in wildcats in Europe (Cytauxzoon europaeus, Cytauxzoon otrantorum, and Cytauxzoon banethi [253]). The clinical importance of these parasites is still unclear, but the high prevalence of Cytauxzoon spp. in wildcats contradicts high pathogenicity in this animal species [252]. Recently, C. europaeus has also been identified in domestic cats in Europe and interestingly, the close genetic relationship between wildcat and domestic cat isolates observed leads to the hypothesis that spillover from the wild reservoirs to domestic cats has occurred [252].
4.1.3. Troglostrongylus brevior: A Lungworm of European wildcats Is Gaining a Prominent Place in Domestic Cat Parasitology
The gastropod-transmitted crenosomatid T. brevior inhabits the bronchi and bronchioles of felines (Felinae). It was first described in an African wildcat (Felis lybica, formerly Felis ocreata) and a jungle cat (Felis chaus, formerly Catolynx chaus) in the middle east [254]. In Europe, the parasite is very common in wildcats with recorded prevalences between 14.9% and 71.4% [226,255,256], while it has also been found in Eurasian lynx [256,257]. Due to the widely distributed populations and the high prevalence of infection in wildcats, these animals are considered the reservoir and the natural host of this parasite in Europe [3].
Troglostrongylus brevior gained particular scientific attention after 2012 when it was recognised as the agent of important, and occasionally fatal, parasitic disease in domestic cats [258]. The role of wildcats in the epizootiology of troglostrongylosis is critical, evidenced by the fact that the infection in domestic cats is reported mainly in areas of wildcat presence, i.e., south and eastern Europe. Thus, troglostrongylosis is considered a key example of a spillover infection from wildlife to domestic animals [3]. The clinical impact of troglostrongylosis in wildcats has not been clearly demonstrated, as the infection in these animals is often diagnosed post-mortem, or in mixed infection with other cardiopulmonary nematodes that likely worsen the clinical, imaging, gross pathology, and histopathology findings [226,244]. Nevertheless, troglostrongylosis in wildcats may have similar clinical impact as in domestic cats, where the disease has been better studied [259]. Accordingly, in cats T. brevior shows significant pathogenicity, probably due to its relatively large size and its location (bronchi and bronchioles), resulting in damage to large areas of the lungs [258]. Clinical signs include coughing, tachypnoea, and dyspnoea, abnormal respiratory auscultation sounds, and various non-specific signs, such as poor body condition, anorexia, and lethargy [259]. An important aspect related to the severity of troglostrongylosis is its ability for vertical transmission from queens to kittens [3], which often results in severe and even fatal infections in young cats that are more susceptive to troglostrongylosis than adults. Considering the importance of troglostrongylosis in veterinary medicine, it is essential to keep a vigilant eye on the distribution trends of T. brevior and include this infection in the differential diagnosis of respiratory disease in domestic cats, especially in the areas of wildcat geographic distribution.
4.1.4. Angiostrongylus chabaudi: A Wildcat-Specific Parasite
In contrast to T. brevior, A. chabaudi, a metastrongyloid, gastropod-transmitted nematode that inhabits the pulmonary arteries and the right chambers of the heart of wildcats [260] is characterised as a host-specific parasite. After the first description of its adult stage in a wildcat [261], the parasite came back to light six decades later, with the isolation of a few, immature parasites from two domestic cats in Italy [262,263]. Soon after, a patent infection was diagnosed post-mortem in a wildcat in Greece [260], and subsequently, additional single cases or epizootiological surveys were reported in Romania, Bulgaria, Bosnia and Herzegovina, Italy, and Greece [226,264,265,266,267], confirming that wildcats are the natural host of this parasite, with a prevalence that reaches up to 56.5% [226].
Evidence of the pathogenesis and clinical impact of angiostrongylosis in wildcats exists thanks to the results of post-mortem findings where A. chabaudi was present in a monospecific parasitosis of the cardiopulmonary system [260,265]. According to those reports, the lungs may be swollen and heavy with a cobblestone appearance. Significant hypertrophy and thickening of the arterial wall were ascribed to pulmonary hypertension caused by the presence of nematodes in the pulmonary arteries. Furthermore, the presence of eggs and migrating larvae was associated with a marked inflammation in the lung parenchyma, with coalescing granulomatous areas, alveolar collapse or emphysemas, and parenchymal haemorrhages [260,265]. Heavy lung lesions were also found in other cases of wildcat angiostrongylosis; however, mixed infection with other cardiopulmonary nematodes did not allow a clear picture of the specific impact of A. chabaudi [226,264]. Similarly, severe clinical disease and imaging findings have been described in a case of a wildcat hospitalisation, but the multiparasitism diagnosed in this animal renders the description of clinical angiostrongylosis impossible [244].
The gastropod-intermediate hosts of A. chabaudi are widespread [268,269] and at least some also transmit metastrongyloids that infect both wildcats and domestic cats, i.e., the common cat lungworm Aelurostrongylus abstrusus and T. brevior. However, despite the fact that all three parasites (i) have similar life cycles, (ii) common intermediate hosts, and (iii) circulate in areas where wildcats and domestic cats live in sympatry, to date, A. chabaudi is not incriminated for spillover from wildcats to domestic cats, and except the two cases in Italy [262,263], no other incidence of infection in domestic cats has ever been reported. It is important to note that lack of infection in cats has been practically confirmed by a great number of epizootiological surveys on cat parasites conducted in recent years in Europe, and especially by surveys targeting specifically the detection of Angiostrongylus spp. in domestic cats in areas where infected wildcats have been found [3,270,271]. However, in an environmentally and parasitologically changing world, it cannot be ruled out that eventually spillover infections of A. chabaudi from wildcats to domestic cats will occur [270]. Bridging infections between wildlife and domestic animals have been recently documented in the case of A. vasorum between foxes and dogs and of T. brevior between wildcats and domestic cats [3,270]. It is important to stress that parasites often cause a milder disease in their natural than in non-natural hosts, as has been evidenced by A. vasorum and C. felis, where the natural hosts, foxes and bobcats, respectively, develop a chronic, subclinical parasitosis while dogs and domestic cats, respectively, often suffer from a severe disease [250,270]. Accordingly, angiostrongylosis may appear more pathogenic in domestic cats as non-natural hosts of A. chabaudi. For all the above reasons, the scientific community and veterinary practitioners need to be alert for accurate and timely diagnosis of the infection in domestic cats, especially in the areas of Europe where the infection has been documented in wildcats.
4.1.5. Cylicospirura spp.: Could It Be a Concern for Domestic Cats?
The parasites of the genus Cylicospirura are spirurid nematodes that live in a ramified burrow inside nodules, formed in the course of this infection in the gastric wall of felids. The described species of the genus so far are Cylicospirura petrowi, Cylicospirura felineus, Cylicospirura subaequalis, Cylicospirura heydorni, Cylicospirura pardalis, and Cylicospirura advena, isolated from a number of different felid species, e.g., Panthera pardus, Panthera tigris tigris, L. rufus, Felis. concolor, and Felis catus in practically all continents [272]. In Europe, Cylicospirura spp. has been reported in lynx from Germany [273], in wildcats from Italy, Germany, Bulgaria, and Greece [223,225,226,274], and in a domestic cat in Italy [275].
The parasite’s life cycle is unknown, but from the analogy of other Spirocercidae it has been suggested that various insects and small vertebrates may serve as intermediate and paratenic hosts, respectively. Cylicospirurosis seems to remain usually subclinical; however, in some rare cases described in domestic cats, the infection is associated with chronic vomiting [275]. The lesions are restricted to the gastric wall where single or multiple nodules, with a central or subcentral mucosal pore, are formed [226]. Histologically, the nodules are characterised by dense sclerotic collagen with anastomosing bands and inflammatory infiltration around the parasites [275,276].
Based on case reports, it is clear that the parasite may infect domestic cats, albeit quite rarely [276]. For this reason, cylicospirurosis may be encountered as a bridging infection from wildlife to domestic animals more frequently in the future. Particularly in areas where the infection in wildcats has been documented in high prevalence, as in Greece (34.8%) [226], domestic cats may be under high infection pressure due to the environmental and climatic changes that bring wildlife closer to human settlements.
4.1.6. Other Parasites
Wildcats host a number of other parasites for which they may play a minor or no exceptional role when compared with other wild or domestic animals. Nevertheless, due to their lifestyle, wildcats are usually infected with a higher frequency with parasites that may infect equally successfully domestic cats. For example, it has been evidenced that wildcats may serve as definitive hosts of E. multilocularis [277], but Felidae seem less competent hosts than Canidae in this important zoonotic cestode [231], so they likely play a minor role in endemic areas. In this context, only immature worms were detected in 5% of the wildcats examined in Germany [223].
As rodents are the main prey of wildcats, parasites such as Taenia taeniaformis are very common in wildcats, showing a prevalence of up to 73.9% [226]. These animals are the main reservoir of this parasite, and although it does not have any zoonotic implications, it may cause clinical disease in felids via intestinal trauma and obstruction [226].
Among others, wildcats may also be important reservoirs for T. callipaeda [79,226] and for C. aerophila, the latter reaching prevalences of up to 33.8% of animals on the basis of post-mortem examinations [226].
5. Mustelidae
The family Mustelidae is comprised of small- to medium-sized animals, some of which are located in specific environments (e.g., water) and others are adapted to most habitat types, including urban settings [278]. This family is the largest and the most diverse of the Carnivora order. Mustelids are opportunistic predators feeding on various small mammals, fish, amphibians, birds, fruits, plants, or mushrooms [279]. They are well-known reservoirs of important pathogens for animals and humans as they harbour a wide diversity of viruses, protozoa, and helminths, playing an important role in spreading diseases. Although mustelids have a wide distribution in Europe and are in close contact with domestic animals, parasitological studies of these animals are limited and most of the time include incidental findings. In the last decade, some zoonotic and emerging diseases were detected for the first time in mustelid species [280,281], including the invasive species Neogale vison [282]. The absence of relevant studies in some countries could be related to a low research interest in this animal family or to the legally protected status of many mustelids.
5.1. The Eurasian Badger (Meles meles)
The Eurasian badger (from now on “badger”) is the biggest mustelid species in Europe with a wide distribution and stable population, classified as “least concerned” according to the IUCN (see File S1) [283]. Badger distribution and population density are correlated with their food resources, which mainly consist of cereals, earthworms, insects, and even rabbits depending on the local conditions [284]. Even though a negative correlation between human population density and badger density was reported [283], in some European countries the anthropogenic land-use change increased food resources for this animal species because of agriculture [285]. Badgers are mainly nocturnal animals that dig large burrows used as temporary shelter by many other animal species, such as foxes, other smaller mustelid species, or even lynx [284,286,287].
5.1.1. Giardia spp. and Leishmania infantum: Still a Lot to Discover Here
There are only a few published studies investigating Giardia spp. in badgers. Giardia duodenalis, was first reported in badgers in the UK in 2010 [288] in a group of cubs that was presented to a wildlife center. In that paper, the authors describe severe digestive illness, manifested by acute diarrhea and death among the badgers [288]. It is not clear if the clinical manifestations were related to giardiosis or to other pathogens. Although giardiosis could have clinical implications in badgers, G. duodenalis assemblage E identified in these cubs does not represent a zoonotic risk [288]. However, recently, infection by zoonotic G. duodenalis genotypes (assemblages A and B) was identified in 48.8% of Eurasian badgers from Italy [289], highlighting the role of badgers in the epidemiology and spreading of zoonotic genotypes. Giardia spp. was molecularly detected in a single animal in Poland, but none of the badgers examined in Spain were positive [290,291]. Even though badgers use latrines for defecation, precipitation can spread the parasite’s cysts into the surroundings, contaminating vegetables, fruits, and water, thus reaching other animal hosts and humans [289].
Leishmania infantum in Eurasian badgers has been investigated in Spain and Italy where the parasite was detected by PCR in 26% and 53.33% of the animals, respectively [53,292]. Additional studies were performed in different regions of Spain, but all with negative results [293,294,295]. It is clear that the infection is present in badgers, but it remains to be concluded if these animals represent reservoir hosts and can infect sandflies or not.
5.1.2. Cryptosporidium spp. and Toxoplasma gondii: Eurasian badgers Are Frequent Hosts
Cryptosporidiosis and giardiosis are two of the most prevalent parasitic diseases in both animals and humans, worldwide [296]. The genus Cryptosporidium includes approximately 30 species with more than 70 genotypes. Wild mammals can be infected with a wide range of species while humans are usually infected with C. hominis and C. parvum [291]. The typical route of infection is via water or food contaminated with oocysts [297]. The clinical presentation of the infection may vary from asymptomatic to acute or chronic digestive distress [298]. Although Cryptosporidium is an important and widespread parasite, limited data are available regarding its prevalence and distribution in wild mesocarnivores, especially in Mustelidae.
Cryptosporidium infection in badgers was detected for the first time in 15% of the animals examined in Great Britain, where C. parvum was morphometrically identified by copromicroscopy [299]. More recently, 2.9% of badgers examined by PCR in Spain harboured Cryptosporidium spp., including the zoonotic C. parvum and C. hominis [291]. Furthermore, 23.2% of the examined badgers in Italy tested positive for Cryptosporidium copro-antigen [289]. These results suggest that badgers could represent an important source of infection in their natural habitats as well as in urban and peri-urban areas. Molecular identification of Crypstoporidium spp. in positive badgers is essential in order to establish the actual zoonotic significance of the infection in this animal species.
Toxoplasma gondii is a well-studied parasite due to its effects on human health. Among all badger protists it is the most studied one, with high reported prevalences [235,300,301,302,303,304,305]. Between 2000 and 2010, seroprevalence over 70% was reported in badgers from the UK [300] and Spain [235,301]. In more recent studies in Portugal and Poland, 50% and 37.5% of the examined animals, respectively, were seropositive [302,306]. The infection in badgers has also been confirmed molecularly in the UK, Poland, Slovakia, and the European part of Turkey [303,304,305,306,307]. Although none of the badgers showed any clinical symptoms related to toxoplasmosis, some authors consider that anorexic and lethargic badgers or those showing an atypical behaviour should be tested for toxoplasmosis [300].
A survey in Poland confirmed that T. gondii prevalence in mustelids was significantly higher when compared to canids, rodents, and insectivores, which indicates that animals of the Mustelidae family are important reservoirs for T. gondii [305].
5.1.3. Trichinella spp., Angiostrongylus vasorum, Dirofilaria immitis, Thelazia callipaeda: Nematodes of Veterinary and Medical Importance can Infect Eurasian badgers
In some countries (e.g., Romania, Czech Republic, Croatia, Russia) badgers are tradi-tionally hunted for meat consumption or for their fat, used as a food supplement, thus in-fection by Trichinella spp. must be considered [308]. According to the International Trichinella Reference Centre (ITRC) [309], the species T. britovi, T. nativa, and T. pseudospiralis and 20 Trichinella isolates have been found in badgers. For example, T. britovi was identified in badgers from Latvia, Italy, and Romania, T. britovi and T. nativa in Estonia, and T. nativa and T. spiralis in Ukraine [310,311].
In a study performed between 2007 and 2014 in wild animals in Estonia, a large proportion (60%) of the badgers examined were found to be infected with Trichinella spp. This was a significantly higher prevalence than recordings taken between 1965 and 2000, which was 6.7% [312]. The infection prevalence in Latvia of 100% indicates that badgers could be more commonly infected than previously assumed and favour the transmission of Trichinella [313].
Most importantly, the risk of human infection may be considered high as badger meat is consumed in several European countries and no routine inspections are implemented as badger is not an official meat source for the population. Infection in humans due to consumption of badger meat has not been reported yet in European countries, probably due to culinary habits (eating thermally processed meat); however, such human infections have been recorded in other continents [314,315]. In Europe, one of the main sources of human infection is wild boar meat [7]. In their diet, wild boars include 5–88% animal matter, mainly small mammals, but larger mammals are sometimes also ingested as carrions [316,317,318]. There are no confirmed records of mustelid consumption by wild boar, but this is something that cannot be ruled out and thus it can be hypothesised that mustelids may play a role in Trichinella transmission to wild boar.
The canine cardiopulmonary nematode A. vasorum, was documented in badgers in Italy, Spain, and Norway by necropsy [319,320,321,322,323,324]. Angiostrongylus vasorum is a common parasite of red foxes, while badgers are typically infected with Angiostrongylus daskalovi, a different but morphologically similar species [324]. Thus, misidentifications should be taken into consideration and molecular confirmation of the identity should be considered. The role of mustelids in the transmission of A. vasorum and their role in the biology of canine angiostrongylosis has not yet been determined.
Although the occurrence of D. immitis microfilaraemia was documented in a badger by microscopical examination and molecular detection, which would normally signify a potential reservoir host, this isolated finding could be considered accidental and further research is needed (e.g., prevalence of infection, microfilaraemia duration) in order to establish the exact role of badgers in the transmission and maintenance of dirofilariosis in a given area [281].
Badgers are mostly nocturnal animals, thus not regularly exposed to the fruit fly vector of the eye worm T. callipaeda [79]. Nevertheless, the parasite was found in 1.8% of the examined badgers in Romania, confirming this animal species as a suitable host [280]. However, given the rarity of T. callipaeda in mustelids evidenced so far, the infection can be considered opportunistic in these animals in endemic areas.
5.2. Martens (Martes foina, Martes martes)
The genus Martes includes eight species of which only two, namely the stone or beech marten (Martes foina) and the pine marten (Martes martes), are present in Europe. Both species have stable populations [324] are adapted to various habitats, from coniferous to Mediterranean forests, and are well-adapted to human settlements, including urban and suburban areas of villages and even towns [325].
5.2.1. Beech marten (Martes foina)
The beech marten, also known as the stone marten, house marten, or white-breasted marten, has spread to south, central, and eastern Europe (see File S1), and prefers open areas. The species is common in urban areas, inhabiting attics, barns, garages, and other human-made enclosures [326].
Giardia spp., Leishmania infantum, Toxoplasma gondii: Badgers’ Proximity to Domestic Animals and Humans Is a Looming Risk
Giardia spp. infection in beech martens was investigated in Poland [290] with negative results and in Spain with 13% prevalence in PCR testing [291]. Considering the closeness of this animal species to human settlements, the risk of transmission to domestic animals and humans should be considered.
Several studies investigated the infection of L. infantum in stone martens in the endemic countries of Spain and Greece [292,293,294,295,327,328]. All studies performed in Spain were based on molecular detection of L. infantum DNA and revealed prevalences of up to 100%, but the only marten tested from Zakinthos island in Greece was negative [327]. However, the report from Greece is quite old and the method of diagnosis is not mentioned, thus a false negative result should be considered.
Muñoz-Madrid et al. [328] were the first to investigate mustelids as potential reservoir hosts of Leishmania in Spain, using a qPCR method from hair. Surprisingly, all three examined beech martens were found to be positive. Another study performed on 21 martens from Basque Country in northern Spain identified the infection with Leishmania in 6 animals (29%) [292]. More recently, in 2018 a study from the regions Murcia, Valencia, and Andalucia detected a 30% prevalence in 10 examined animals. In northwestern Spain, two out of the three examined beech martens were positive by PCR testing [294]. In four animals investigated in the Catalonia region by qPCR testing, a prevalence of 50% was found in DNA extracted from the liver and spleen [295].
These results, together with the fact that M. foina is commonly spotted in human settlements, could signify an important role of this animal in the epidemiology of L. infantum. However, it is not possible to draw any definite conclusion because there is no evidence of stone martens’ capacity to infect sandflies, thus further research on this matter would be elucidating.
Toxoplasma gondii infection in M. foina was detected in 18% of the tested animals in the Czech Republic by xenodiagnosis [329] and at a prevalence of 4.92% by PCR testing several years later [330]. In Spain, 85% of the tested beech martens were seropositive [235]. Furthermore, 57.1%, 66.7%, and 52.9% of the examined beech martens in Slovakia, Portugal, and Lithuania, respectively, were positive by PCR testing and serology, respectively, [236,304,331]. The high prevalence of T. gondii infection is likely related to beech martens’ main prey in winter, i.e., rodents [332]. Due to their proximity to peri-urban and urban areas, these animals can be an important source of infection for domestic cats or even urban rodents.
Thelazia callipaeda, Capillaria aerophila and Trichinella spp.: Beech Martens Are Additional Hosts of These Important Parasites
Studies on T. callipaeda in the abundant group of mustelids are still limited with scarce information on their role as reservoir hosts for this parasite [280,333]. In Europe, infection with T. callipaeda in beech martens was documented in Italy (13.60%) [79], Portugal (one case report) [334], and Romania (7.69%) [280]. The idea that wild animals act as reservoir hosts for T. callipaeda has been previously discussed [29]. Considering that beech martens are abundant, they may play an important role in maintaining and spreading the infection to domestic animals and humans [29].
Capillaria aerophila is a zoonotic lungworm that was identified in beech marten carcasses in Europe [310,335]. The contamination of the environment with high numbers of infective eggs raises the chances of transmission to dogs, cats, and even humans.
Trichinella spiralis and T. britovi were isolated from beech martens, which could represent a source of infection for other sylvatic animal species, but less so for humans as consumption of beech marten meat is not reported in European countries. Reported prevalences range between 4.8% and 50% for T. britovi in Italy [336], Slovakia [337], Serbia [338], and Romania [339]. Trichinella spiralis was identified in lower Silesia, Poland, in 15.3% of the examined animals [340]. The detection of the “domestic cycle” species T. spiralis in mustelids is attributed to the habitat loss and urbanisation of these wild animals. The transmission to domestic animals can be promoted by the presence of backyard pigs with free outdoor access [339].
5.2.2. Pine Marten (Martes martes)
The pine marten prefers woodlands with dense vegetation. It is found mainly in northeastern and central Europe, but some populations are present in parts of the Mediterranean (see File S1). Their presence was reported in some European cities. Their food is mainly based on small mammals, such as voles, mice, squirrels, birds, and amphibians [341]. Due to their feeding habits, they are very likely to be infected with food-borne parasites such as T. gondii. Several studies investigated the infection of European M. martes with T. gondii with moderate to high detected prevalences (17% to 100%) [235,304,305,306,329,330,331].
Similar to the other animal species of this genus, pine martens are important reservoirs for Trichinella in sylvatic and urban environments. In this animal species, trichinellosis was identified in a few European countries with varying prevalence (8.3–91.8%) [191,310,311,313,336,337,339,342,343,344,345,346,347,348,349,350]. The species T. britovi was mainly identified, while in two cases T. spiralis was detected and there is also a single report of T. nativa in a pine marten from Latvia, coinfected with T. britovi [313]. The presence of T. spiralis suggests an involvement of pine martens in the domestic cycle of the parasite and a possible important role of these animals in the epidemiology of infection. On the other hand, according to the reports, T. spiralis is scant, which could be related to a low susceptibility of martens in maintaining the infection [310,338]. Further large-scale studies are needed in order to establish the exact nature and role of mustelids in the life cycle of Trichinella.
5.3. The Genus Mustela: Abundant and Parasite Carier
The species of the genus Mustela are globally distributed, and their number continuously changes, now numbering more than 15 [324]. Among them, there are very abundant and population-stable species, such as the European polecat (Mustela putorius), or highly endangered species such as the European mink (Mustela lutreola) [351]. Food-borne parasitic infections are often detected in these small and fit animals that feed on rodents, lagomorphs, and other vertebrate and invertebrate hosts [352]. As expected, they are important reservoirs for T. gondii. The majority of studies investigated the infection in polecats, a species that inhabits many European countries and is known to live near farms or other human settlements and revealed infection rates of up to 100% in the UK [303], Spain [235], Portugal [236], Poland [305], and Slovakia [304]. Furthermore, T. gondii was detected in the brain of 25% of weasels (Mustela nivalis) from the Czech Republic [329].
Trichinella britovi and T. spiralis were identified in the genus Mustela only in eastern Europe with low prevalence rates [337,353,354]. Small mustelids can be important reservoirs as they represent a possible source of food for wild boar. However, as previously mentioned, it is hard to verify the exact origin of hair and bones detected in the stomach of wild animals, thus more studies are needed in order to confirm the role of mustelids in the transmission and maintenance of trichinelosis.
Finally, infection with A. vasorum was reported in a polecat from Denmark [335] and in one ermine (Mustela erminea) from the UK [355], suggesting that these animals could play a role in the maintenance of this parasite in an area.
5.4. Eurasian otter (Lutra lutra): Their Water Affiliation May Be Decisive for Its Epidemiological Impact
The Eurasian otter (from now on “otter”) is a semiaquatic mammal present in most parts of Europe. Thanks to conservation efforts, declining otter populations are now in a process of recovery (see File S1) [356]. Otters live in a wide variety of aquatic habitats and although they are elusive, they can be found close to human settlements [357].
The affiliation of otters with water renders them a potentially important animal for the dissemination of parasites such as Giardia spp. and Cryptosporidium, for which water (drinking, recreational) is important source of infection. Giardia spp. was found in 1 out of 33 otters in Denmark [358] while both Giardia and Cryptosporidium were found 3.9% and 6.8% of the otters examined in northwest Spain, respectively [359], but no information about the zoonotic potential of these infections is available as no genetic characterisation of the parasites was performed.
As expected, otters are also infected with T. gondii through their prey and also because the parasite oocysts are transferred from the soil and are accumulated in the aquatic habitats by precipitation and agricultural water runoff [360]. In this sense, otters can be utilised as sentinels for T. gondii load in a given area [361]. In fact, Toxoplasma seropositivity in otters has been documented from 25.5% to 100% depending, among others factors, on the sample size [236,360,361], indicating that otters play an important role in the maintenance and circulation of the parasite.
The otter has occasionally been found as infected with D. immitis [168,362,363]. However, its factual reservoir role is unknown, as microfilaraemia was documented in only one case [168,362,363]. Further investigations are needed to clarify the role of otters as a source of infection for dogs and other hosts in the same area.
5.5. The American Mink (Neogale vison): An Invasive Species Claims Its Role in Parasite Epidemiology in Europe
The American mink is native to North America, and it was introduced in Europe as a fur animal. Due to the fact that some animals escaped or were intentionally released in nature, the species has now a stable population in some parts of Europe (see File S1) [364]. The American mink is distributed mostly along streams and lakes, but it is also often detected in swamps and marshes. It is a strictly carnivorous species that feeds on fish, amphibians, crustaceans, and some small mammals [365,366], and it is an important reservoir host for many zoonotic pathogens, including parasites.
American minks were found serologically or molecularly positive for T. gondii in the UK, Poland, and Denmark, reaching a prevalence of up to 78.8% in Spain [17,303,306,367,368,369]. Infection with Cryptosporidium was detected in animals from Ireland, Spain, and the Czech Republic with prevalences of 6.17%, 24.20%, and 6%, respectively. Taking into consideration that both T. gondii and Cryptosporidium are often water transmitted and that American minks prefer habitats close to water, it may be speculated that these animals are important spreaders of the parasites.
The zoonotic parasite L. infantum was detected by PCR testing in DNA extracted from the liver and spleen of one mink from Spain [295], suggesting that these animals may represent an additional reservoir host species in endemic areas.
Finally, the nematode of emerging veterinary concern, A. vasorum, was found in 1.16% of the American minks examined in Denmark [335], the zoonotic C. aerophila in 11–15% of the animals in Lithuania [370,371], and the important food-borne nematode Trichinella spp. in Ukraine and Poland in 3.3% and 25 of the animals, respectively [282,310,340].
6. Conclusions
According to the expanding relative literature, mesocarnivores hold an important and in some cases critical role as reservoirs and bridge hosts of important emerging parasites in Europe. These animals host parasites that may be introduced into the areas where they expand or in which they invade and can be transmitted to sympatric domestic animals. An important portion of these parasites have a proven or potential zoonotic importance and thus should be taken into consideration in human medicine and the One Health approach to public health, especially in the context of changing conditions due to climate change, land-use change, natural environment degradation, and rewilding of urban areas.
Continuing investigations and monitoring are warranted and necessary in order to elucidate further the occurrence, prevalence, and epidemiology of the parasites under consideration and to design strategies that would control and prevent the occurrence of important zoonoses and emerging bridging infections between wildlife, domestic animals, and humans.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/pathogens12020178/s1, File S1: Characteristics and geographical distribution of mesocarnivores in Europe.
Author Contributions
Conceptualisation F.V.; writing—original draft preparation, review and editing F.V., G.D. and A.D. All authors have read and agreed to the published version of the manuscript.
Funding
This article received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank Leonardo Brustenga for preparing the Supplementary Materials.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Polley, L. Navigating parasite webs and parasite flow: Emerging and re-emerging parasitic zoonoses of wildlife origin. Int. J. Parasitol. 2005, 35, 1279–1294. [Google Scholar]
- Morgan, E.R.; Modry, D.; Paredes-Esquivel, C.; Foronda, P.; Traversa, D. Angiostrongylosis in Animals and Humans in Europe. Pathogens 2021, 10, 1236. [Google Scholar]
- Traversa, D.; Morelli, S.; Di Cesare, A.; Diakou, A. Felid Cardiopulmonary Nematodes: Dilemmas Solved and New Questions Posed. Pathogens 2021, 10, 30. [Google Scholar]
- Daszak, P.; Cunningham, A.A.; Hyatt, A.D. Anthropogenic environmental change and the emergence of infectious diseases in wildlife. Acta Trop. 2001, 78, 103–116. [Google Scholar] [CrossRef]
- Roemer, G.W.; Gompper, M.E.; Van Valkenburgh, B. The ecological role of the mammalian mesocarnivore. BioScience 2009, 59, 165–173. [Google Scholar]
- Tedeschi, L.; Biancolini, D.; Capinha, C.; Rondinini, C.; Essl, F. Introduction, spread, and impacts of invasive alien mammal species in Europe. Mammal Rev. 2022, 52, 252–266. [Google Scholar] [CrossRef]
- EFSA (European Food Safety Authority); ECDC (European Centre for Disease Prevention and Control). The European Union One Health 2019 Zoonoses Report. EFSA J. 2021, 19, e6406. [Google Scholar]
- Sillero-Zubiri, C.; Hoffmann, M.; Macdonald, D.W. Canids: Foxes, Wolves, Jackalsand Dogs, Status Survey and Conservation Action Plan; IUCN/SSC Canid Specialist Group: Gland, Switzerland; Cambridge, UK, 2004; p. 430. [Google Scholar]
- Helle, E.; Kauhala, K. Distribution history and present status of the raccoon dog in Finland. Holarct. Ecol. 1991, 14, 278–286. [Google Scholar]
- Kauhala, K.; Saeki, M. Nyctereutes procyonoides. IUCN RedList Threat. Species 2016, e.T14925A85658776. Available online: https://dx.doi.org/10.2305/IUCN.UK.2016-1.RLTS.T14925A85658776.en (accessed on 27 December 2022).
- Criado-Fornelio, A.; Martín-Pérez, T.; Verdú-Expósito, C.; Reinoso-Ortiz, S.A.; Pérez-Serrano, J. Molecular epidemiology of parasitic protozoa and Ehrlichia canis in wildlife in Madrid (central Spain). Parasitol. Res. 2018, 117, 2291–2298. [Google Scholar]
- Duscher, G.G.; Fuehrer, H.P.; Kübber-Heiss, A. Fox on the run—Molecular surveillance of fox blood and tissue for the occurrence of tick-borne pathogens in Austria. Parasit. Vectors 2014, 7, 521. [Google Scholar]
- Laurimaa, L.; Moks, E.; Soe, E.; Valdmann, H.; Saarma, U. Echinococcus multilocularis and other zoonotic parasites in red foxes in Estonia. Parasitology 2016, 143, 1450–1458. [Google Scholar] [CrossRef]
- Hoffmann, M.; Sillero-Zubiri, C. Vulpes vulpes amended version of 2016 assessment. IUCN Red List. Threat. Species 2021, e.T23062A193903628. Available online: https://dx.doi.org/10.2305/IUCN.UK.2021-1.RLTS.T23062A193903628.en (accessed on 27 December 2022).
- Janko, J.; Schröder, W.; Linke, S.; König, A. Space use and resting site selection of red foxes (Vulpes vulpes) living near villages and small towns in southern Germany. Acta Theriol. 2012, 57, 245–250. [Google Scholar] [CrossRef]
- Contesse, P.; Hegglin, D.; Gloor, S.; Bontadina, F.; Deplazes, P. Original investigation: The diet of urban foxes (Vulpes vulpes) and the availability of anthropogenic food in the city of Zurich, Switzerland. Mamm. Biol. 2004, 69, 81–95. [Google Scholar] [CrossRef]
- Plumer, L.; Davison, J.; Saarma, U. Rapid urbanization of red foxes in Estonia: Distribution, behaviour, attacks on domestic animals, and health-risks related to zoonotic diseases. PLoS ONE 2014, 9, e115124. [Google Scholar] [CrossRef]
- André, M.R. Diversity of Anaplasma and Ehrlichia/Neoehrlichia Agents in Terrestrial Wild Carnivores Worldwide: Implications for Human and Domestic Animal Health and Wildlife Conservation. Front. Vet. Sci. 2018, 23, 293. [Google Scholar] [CrossRef]
- Otranto, D.; Cantacessi, C.; Dantas-Torres, F.; Brianti, E.; Pfeffer, M.; Genchi, C.; Guberti, V.; Capelli, G.; Deplazes, P. The role of wild canids and felids in spreading parasites to dogs and cats in Europe. Part II: Helminths and arthropods. Vet. Parasitol. 2015, 213, 24–37. [Google Scholar] [CrossRef]
- Otranto, D.; Deplazes, P. Zoonotic nematodes of wild carnivores. Int. J. Parasitol. Parasites Wildl. 2019, 9, 370–383. [Google Scholar]
- Veronesi, F.; Morganti, G.; Di Cesare, A.; Lepri, E.; Cassini, R.; Zanet, S.; Deni, D.; Chiari, M.; Ferroglio, E. Eucoleus boehmi infection in red fox (Vulpes vulpes) from Italy. Vet. Parasitol. 2014, 206, 232–239. [Google Scholar]
- Dell’Arte, G.L.; Laaksonen, T.; Norrdahl, K.; Korpimaki, E. Variation in the diet composition of a generalist predator, the red fox, in relation to season and density of main prey. Acta Oecologica 2007, 31, 276–281. [Google Scholar]
- Kidawa, D.; Kowalczyk, R. The effects of sex, age, season and habitat on diet of the red fox Vulpes vulpes in northeastern Poland. Acta Theriol. 2011, 56, 209–218. [Google Scholar]
- Aguirre, A.A. Wild canids as sentinels of ecological health: A conservation medicine perspective. Parasit. Vectors 2009, 8 (Suppl. S1), S7. [Google Scholar]
- Medkour, H.; Laidoudi, Y.; Lafri, I.; Davoust, B.; Mekroud, A.; Bitam, I.; Mediannikov, O. Canine vector-borne protozoa: Molecular and serological investigation for Leishmania spp., Trypanosoma spp., Babesia spp., and Hepatozoon spp. in dogs from Northern Algeria. Vet. Parasitol. Reg. Stud. Rep. 2020, 19, 100353. [Google Scholar] [CrossRef]
- Campino, L.; Pratlong, F.; Abranches, P.; Rioux, J.-A.; Santos-Gomes, G.; Alves-Pires, C.; Cortes, S.; Ramada, J.; Cristovao, J.M.; Afonso, M.O.; et al. Leishmaniasis in Portugal: Enzyme polymorphism of Leishmania infantum based on the identification of 213 strains. Trop. Med. Int. Health 2006, 11, 1708–1714. [Google Scholar]
- Azami-Conesa, I.; Gómez-Muñoz, M.T.; Martínez-Díaz, R.A. A Systematic Review (1990–2021) of Wild Animals Infected with Zoonotic Leishmania. Microorganisms 2021, 9, 1101. [Google Scholar] [CrossRef]
- Rioux, J.A.; Albaret, J.L.; Houin, R.; Dedet, J.; Lanotte, G. Ecologie des leishmanioses dans le sud de la France. 2. Les reservoirs selvatiques. Infestation spontanee de renard (Vulpes vulpes L.). Ann. Parasito. Hum. Comp. 1968, 43, 421–428. [Google Scholar]
- Davoust, B.; Mary, C.; Marié, J.L. Detection of Leishmania in red foxes (Vulpes vulpes) from southeastern France using realtime quantitative PCR. J. Wildl. Dis. 2014, 50, 130–132. [Google Scholar] [CrossRef]
- Babuadze, G.; Alvar, J.; Argaw, D.; de Koning, H.P.; Iosava, M.; Kekelidze, M.; Tsertsvadze, N.; Tsereteli, D.; Chakhunashvili, G.; Mamatsashvili, T.; et al. Epidemiology of visceral leishmaniasis in Georgia. PLoS Negl. Trop. Dis. 2014, 8, e2725. [Google Scholar] [CrossRef]
- Mancianti, F.; Mignone, W.; Galestri, F. Serologic survey for leishmaniasis in free-living red foxes (Vulpes vulpes) in Italy. J. Wildl. Dis. 1994, 30, 454–456. [Google Scholar]
- Dipineto, L.; Manna, L.; Baiano, A.; Gala, M.; Fioretti, A.; Gravino, A.E.; Menna, L.F. Presence of Leishmania infantum in red foxes (Vulpes vulpes) in southern Italy. J. Wildl. Dis. 2007, 43, 518–520. [Google Scholar]
- Verin, R.; Polia, A.; Ariti, G.; Nardoni, S.; Bertucelli, M.; Mancianti, F. Detection of Leishmania infantum DNA in tissue of free-ranging red foxes (Vulpes vulpes) in Central Italy. Eur. J. Wild. Res. 2010, 56, 689–692. [Google Scholar] [CrossRef]
- Sgroi, G.; Iatta, R.; Veneziano, V.; Bezerra-Santos, M.A.; Lesiczka, P.; Hrazdilová, K.; Annoscia, G.; D’Alessio, N.; Golovchenko, M.; Rudenko, N.; et al. Molecular survey on tick-borne pathogens and Leishmania infantum in red foxes (Vulpes vulpes) from southern Italy. Ticks Tick Borne Dis. 2021, 12, 101669. [Google Scholar]
- Karayiannis, S.; Ntais, P.; Messaritakis, I.; Tsirigotakis, N.; Dokianakis, E.; Antoniou, M. Detection of Leishmania infantum in red foxes (Vulpes vulpes) in Central Greece. Parasitology 2015, 142, 1574–1578. [Google Scholar]
- Criado-Fornelio, A.; Gutierrez-Garcia, L.; Rodriguez-Caabeiro, F.; Reus-Garcia, E.; Roldan-Soriano, M.A.; Diaz-Sanchez, M.A. A parasitological survey of wild red foxes (Vulpes vulpes) from the province of Guadalajara, Spain. Vet. Parasitol. 2000, 92, 245–251. [Google Scholar]
- Solano-Gallego, L.; Morell, P.; Arboix, M.; Alberola, J.; Ferrer, L. Prevalence of Leishmania infantum infection in dogs living in an area of canine leishmaniasis endemicity using PCR on several tissues and serology. J. Clin. Microbiol. 2001, 39, 560–563. [Google Scholar] [CrossRef]
- Molina, R.; Jiménez, M.I.; Cruz, I.; Iriso, A.; Martín-Martín, I.; Sevillano, O. The hare (Lepus granatensis) as potential sylvatic reservoir of Leishmania infantum in Spain. Vet. Parasitol. 2012, 190, 268–271. [Google Scholar] [CrossRef]
- Jiménez, M.; González, E.; Martín-Martín, I.; Hernández, S.; Molina, R. Could wild rabbits (Oryctolagus cuniculus) be reservoirs for Leishmania infantum in the focus of Madrid, Spain? Vet. Parasitol. 2014, 202, 296–300. [Google Scholar]
- Courtenay, O.; Carson, C.; Calvo-Bado, L.; Garcez, L.M.; Quinnell, R.J. Heterogeneities in Leishmania infantum infection: Using skin parasite burdens to identify highly infectious dogs. PLoS Negl. Trop. Dis. 2014, 8, e2583. [Google Scholar] [CrossRef]
- Ilie, M.; Imre, M.; Imre, K.; Hot, I.; Morariu, S.; Sorescu, D. Occurrence of Hepatozoon spp. in red foxes (Vulpes vulpes) in Romania. Parasit. Vectors 2014, 7, O33. [Google Scholar] [CrossRef]
- Mierzejewska, E.J.; Pawełczyk, A.; Radkowski, M.; Welc-Falęciak, R.; Bajer, A. Pathogens vectored by the tick, Dermacentor reticulatus, in endemic regions and zones of expansion in Poland. Parasit. Vectors 2015, 8, 49. [Google Scholar]
- Medkour, H.; Laidoudi, Y.; Marié, J.L.; Fenollar, F.; Davoust, B.; Mediannikov, O. Molecular investigation of vector-borne pathogens in red foxes (Vulpes vulpes) from southern France. J. Wildl. Dis. 2020, 56, 837–850. [Google Scholar]
- Baneth, G.; Florin-Christensen, M.; Cardoso, L.; Schnittger, L. Reclassification of Theileria annae as Babesia vulpes sp. nov. Parasit. Vectors 2015, 8, 207. [Google Scholar]
- Baneth, G.; Cardoso, L.; Brilhante-Simões, P.; Schnittger, L. Establishment of Babesia vulpes n. sp. (Apicomplexa: Babesiidae), a piroplasmid species pathogenic for domestic dogs. Parasit. Vectors 2019, 12, 129. [Google Scholar] [CrossRef]
- Mierzejewska, E.J.; Dwużnik, D.; Koczwarska, J.; Stańczak, Ł.; Opalińska, P.; Krokowska-Paluszak, M.; Wierzbicka, A.; Górecki, G.; Bajer, A. The red fox (Vulpes vulpes), a possible reservoir of Babesia vulpes, B. canis and Hepatozoon canis and its association with the tick Dermacentor reticulatus occurrence. Ticks Tick Borne Dis. 2021, 12, 101551. [Google Scholar] [CrossRef]
- Camacho, A.T.; Pallas, E.; Gestal, J.J.; Guitián, F.J.; Olmeda, A.S.; Telford, S.R.; Spielman, A. Ixodes hexagonus is the main candidate as vector of Theileria annae in northwest Spain Vet. Parasitol. 2003, 112, 157–163. [Google Scholar]
- Cardoso, L.; Cortes, H.C.E.; Reis, A.; Rodrigues, P.; Simões, M.; Lopes, A.P.; Vila-Viçosa, M.J.; Talmi-Frank, D.; Eyal, O.; Solano-Gallego, L.; et al. Prevalence of Babesia microti-like infection in red foxes (Vulpes vulpes) from Portugal. Vet. Parasitol. 2013, 19, 90–95. [Google Scholar]
- Checa, R.; López-Beceiro, A.M.; Montoya, A.; Barrera, J.P.; Ortega, N.; Gálvez, R.; Marino, V.; González, J.; Olmeda, Á.S.; Fidalgo, L.E.; et al. Babesia microti-like piroplasm (syn. Babesia vulpes) infection in red foxes (Vulpes vulpes) in NW Spain (Galicia) and its relationship with Ixodes hexagonus. Vet. Parasitol. 2018, 252, 22–28. [Google Scholar] [CrossRef]
- Najm, N.A.; Meyer-Kayser, E.; Hoffmann, L.; Pfister, K.; Silaghi, C. Hepatozoon canis in German red foxes (Vulpes vulpes) and their ticks: Molecular characterization and the phylogenetic relationship to other Hepatozoon spp. Parasitol. Res. 2014, 113, 2679–2685. [Google Scholar] [CrossRef]
- Hodžić, A.; Alić, A.; Fuehrer, H.P.; Harl, J.; Wille-Piazzai, W.; Duscher, G.G. A molecular survey of vector-borne pathogens in red foxes (Vulpes vulpes) from Bosnia and Herzegovina. Parasit. Vectors 2015, 8, 88. [Google Scholar] [CrossRef]
- Ebani, V.V.; Rocchigiani, G.; Nardoni, S.; Bertelloni, F.; Vasta, V.; Papini, R.A.; Verin, R.; Poli, A.; Mancianti, F. Molecular detection of tick-borne pathogens in wild red foxes (Vulpes vulpes) from Central Italy. Acta Trop. 2017, 172, 197–200. [Google Scholar] [CrossRef]
- Battisti, E.; Zanet, S.; Khalili, S.; Trisciuoglio, A.; Hertel, B.; Ferroglio, E. Molecular Survey on Vector-Borne Pathogens in Alpine Wild Carnivorans. Front. Vet. Sci. 2020, 27, 1. [Google Scholar]
- Daskalaki, A.A.; Ionică, A.M.; Deak, G.; Gherman, C.M.; D’Amico, G.; Păstrav, I.R.; Matei, I.A.; Domșa, C.; Mihalca, A.D. Environmental factors influencing the distribution of “Theileria annae” in red foxes, Vulpes vulpes in Romania. Ticks Tick Borne Dis. 2018, 9, 660–664. [Google Scholar]
- Farkas, R.; Takács, N.; Hornyák, Á.; Nachum-Biala, Y.; Hornok, S.; Baneth, G. First report on Babesia cf. microti infection of red foxes (Vulpes vulpes) from Hungary. Parasit. Vectors 2015, 8, 55. [Google Scholar] [CrossRef]
- Deždek, D.; Vojta, L.; Ćurković, S.; Lipej, Z.; Mihaljević, Ž.; Cvetnić, Ž.; Beck, R. Molecular detection of Theileria annae and Hepatozoon canis in foxes (Vulpes vulpes) in Croatia. Vet. Parasitol. 2010, 172, 333–336. [Google Scholar] [CrossRef]
- Giannelli, A.; Ramos, R.A.; Dantas-Torres, F.; Mencke, N.; Baneth, G.; Otranto, D. Experimental evidence against transmission of Hepatozoon canis by Ixodes ricinus. Ticks Tick Borne Dis. 2013, 4, 391–394. [Google Scholar] [CrossRef]
- Baneth, G. Perspectives on canine and feline hepatozoonosis. Vet. Parasitol. 2011, 181, 3–11. [Google Scholar] [CrossRef]
- Cardoso, L.; Cortes, H.C.; Eyal, O.; Reis, A.; Lopes, A.P.; Vila-Viçosa, M.J.; Rodrigues, P.A.; Baneth, G. Molecular and histopathological detection of Hepatozoon canis in red foxes (Vulpes vulpes) from Portugal. Parasit. Vectors 2014, 7, 113. [Google Scholar] [CrossRef]
- Juwaid, S.; Sukara, R.; Penezić, A.; Mihaljica, D.; Veinović, G.; Kavallieratos, N.G.; Ćirović, D.; Tomanović, S. First evidence of tick-borne protozoan pathogens, Babesia sp. and Hepatozoon canis, in red foxes (Vulpes vulpes) in Serbia. Acta Vet. Hung. 2019, 67, 70–80. [Google Scholar] [CrossRef]
- Mitková, B.; Hrazdilová, K.; Steinbauer, V.; D’Amico, G.; Mihalca, A.D.; Modrý, D. Autochthonous Hepatozoon infection in hunting dogs and foxes from the Czech Republic. Parasitol. Res. 2016, 115, 4167–4171. [Google Scholar]
- Hodžić, A.; Mrowietz, N.; Cézanne, R.; Bruckschwaiger, P.; Punz, S.; Habler, V.E.; Tomsik, V.; Lazar, J.; Duscher, G.G.; Glawischnig, W.; et al. Occurrence and diversity of arthropod-transmitted pathogens in red foxes (Vulpes vulpes) in western Austria, and possible vertical (transplacental) transmission of Hepatozoon canis. Parasitol. 2018, 145, 335–344. [Google Scholar] [CrossRef]
- Miterpáková, M.; Komjáti-Nagyová, M.; Hurníková, Z.; Víchová, B. Retrospective molecular study on canine hepatozoonosis in Slovakia—Does infection risk for dogs really exist? Ticks Tick Borne Dis. 2017, 8, 567–573. [Google Scholar] [CrossRef]
- Farkas, R.; Solymosi, N.; Takács, N.; Hornyák, Á.; Hornok, S.; Nachum-Biala, Y.; Baneth, G. First molecular evidence of Hepatozoon canis infection in red foxes and Golden jackals from Hungary. Parasit. Vectors 2014, 7, 303. [Google Scholar]
- Gomes-de-Sá, S.; Santos-Silva, S.; Moreira, A.S.; Barradas, P.F.; Amorim, I.; Cardoso, L.; Mesquita, J.R. Dirofilaria immitis antigenemia and microfilaremia in Iberian wolves and red foxes from Portugal. Parasit. Vectors 2022, 15, 119. [Google Scholar]
- Simón, F.; Siles-Lucas, M.; Morchón, R.; González-Miguel, J.; Mellado, I.; Carretón, E.; Montoya-Alonso, J.A. Human and animal dirofilariasis: The emergence of a zoonotic mosaic. Clin. Microbiol. Rev. 2012, 25, 507–544. [Google Scholar]
- Tolnai, Z.; Széll, Z.; Sproch, Á.; Szeredi, L.; Sréter, T. Dirofilaria immitis: An emerging parasite in dogs, red foxes and Golden jackals in Hungary. Vet. Parasitol. 2014, 203, 339–342. [Google Scholar]
- Ionică, A.M.; Matei, I.A.; D’Amico, G.; Ababii, J.; Daskalaki, A.A.; Sándor, A.D.; Enache, D.V.; Gherman, C.M.; Mihalca, A.D. Filarioid infections in wild carnivores: A multispecies survey in Romania. Parasit. Vectors 2017, 10, 332. [Google Scholar]
- Kravchenko, V.; Itin, G.; Kartashev, V.; Ermakov, A.; Kartashov, S.; Diosdado, A.; González-Miguel, J.; Simón, F. Dirofilaria immitis and D. repens in sylvatic reservoirs of Krasnodar Krai (Russian Federation). Vet. Parasitol. Reg. Stud. Rep. 2016, 6, 35–38. [Google Scholar] [CrossRef]
- Potkonjak, A.; Rojas, A.; Gutiérrez, R.; Nachum-Biala, Y.; Kleinerman, G.; Savić, S.; Polaček, V.; Pušić, I.; Harrus, S.; Baneth, G. Molecular survey of Dirofilaria species in stray dogs, red foxes and Golden jackals from Vojvodina, Serbia. Comp. Immunol. Microbiol. Infect. Dis. 2020, 68, 101409. [Google Scholar] [CrossRef]
- Otranto, D.; Cantacessi, C.; Testini, G.; Lia, R.P. Phortica variegata as an intermediate host of Thelazia callipaeda under natural conditions: Evidence for pathogen transmission by a male arthropod vector. Int. J. Parasitol. 2006, 36, 1167–1173. [Google Scholar]
- Otranto, D.; Mendoza-Roldan, J.A.; Dantas-Torres, F. Thelazia callipaeda. Trends Parasitol. 2020, 4922, 301–306. [Google Scholar] [CrossRef]
- Otranto, D.; Dantas-Torres, F. Transmission of the eyeworm Thelazia callipaeda: Between fantasy and reality. Parasit. Vectors 2015, 8, 273. [Google Scholar] [CrossRef]
- Ionică, A.M.; Deak, G.; Mate, I.A.; D’Amico, G.; Cotuţiu, V.D.; Gherman, C.M.; Mihalca, A.D. Thelazia callipaeda, an endemic parasite of red foxes (Vulpes vulpes) in Western Romania. J. Wildl. Dis. 2018, 54, 829–833. [Google Scholar]
- Diakou, A. Thelazia callipaeda: Vigilance is the best course of action. Vet. Rec. 2017, 181, 344–345. [Google Scholar] [CrossRef]
- Maia, C.; Catarino, A.; Almeida, B.; Ramos, C.; Campino, L. Cardoso Emergence of Thelazia callipaeda infection in dogs and cats from east-central Portugal. Transbound. Emerg. Dis. 2016, 63, 416–421. [Google Scholar]
- Otranto, D.; Ferroglio, E.; Lia, R.P.; Traversa, D.; Rossi, L. Current status and epidemiological observation of Thelazia callipaeda (Spirurida, Thelaziidae) in dogs, cats and foxes in Italy: A “coincidence” or a parasitic disease of the Old Continent? Vet. Parasitol. 2007, 116, 315–325. [Google Scholar]
- Malacrida, F.; Hegglin, D.; Bacciarini, L.; Otranto, D.; Nägeli, F.; Nägeli, C.; Bernasconi, C.; Scheu, U.; Balli, A.; Marenco, M.; et al. Emergence of canine ocular thelaziosis caused by Thelazia callipaeda in southern Switzerland. Vet. Parasitol. 2008, 157, 321–327. [Google Scholar]
- Otranto, D.; Dantas Torres, F.; Mallia, E.; Di Geronimo, P.M.; Brianti, E.; Testini, G.; Traversa, D.; Lia, R.P. Thelazia callipaeda (Spirurida, Thelaziidae) in wild animals: Report of new host species and ecological implications. Vet. Parasitol. 2009, 166, 262–267. [Google Scholar]
- Shen, J.; Gasser, R.B.; Chu, D.; Wang, Z.; Yuan, X.; Cantacessi, C.; Otranto, D. Human thelaziosis—A neglected parasitic disease of the eye. J. Parasitol. 2006, 92, 872–876. [Google Scholar]
- Otranto, D.; Dutto, M. Human thelaziasis Europe. Emerg. Infect. Dis. 2008, 14, 647–649. [Google Scholar] [CrossRef]
- Sargo, R.; Loureiro, F.; Catarino, A.L.; Valente, J.; Silva, F.; Cardoso, L.; Otranto, D.; Maia, C. First report of Thelazia callipaeda in red foxes (Vulpes vulpes) from Portugal. JZVM 2014, 45, 458–460. [Google Scholar]
- Otranto, D.; Dantas-Torres, F.; Brianti, E.; Traversa, D.; Petrić, D.; Genchi, C.; Capelli, G. Vector-borne helminths of dogs and humans in Europe. Parasit. Vectors. 2013, 6, 16. [Google Scholar] [CrossRef]
- Fuentes, I.; Montes, I.; Saugar, J.M.; Latrofa, S.; Gárate, T.; Otranto, D. Thelaziosis in humans, a zoonotic infection, Spain, 2011. Emerg. Infect Dis. 2012, 18, 2073–2075. [Google Scholar]
- Tasić-Otašević, S.; Gabrielli, S.; Trenkić-Božinović, M.; Petrović, A.; Gajić, B.; Colella, V.; Momčilović, S.; Cancrini, G.; Otranto, D. Eyeworm infections in dogs and in a human patient in Serbia: A One Health approach is needed. Comp. Immunol. Microbiol. Infect. Dis. 2016, 45, 20–22. [Google Scholar] [CrossRef]
- Dolff, S.; Kehrmann, J.; Eisermann, P.; Dalbah, S.; Tappe, D.; Rating, P. Case report: Thelazia callipaeda eye infection: The first human case in Germany. Am. J. Trop. Med. Hyg. 2020, 102, 350–351. [Google Scholar] [CrossRef]
- Paradžik, M.T.; Samardžić, K.; Živičnjak, T.; Martinković, F.; Janjetović, Ž.; Miletić-Medved, M. Thelazia callipaeda—First human case of thelaziosis in Croatia. Wien. Klin. Wochenschr. 2016, 128, 221–223. [Google Scholar]
- Morgado, A.C.T.; do Vale, B.; Ribeiro, P.; Coutinho, T.; Santos-Silva, S.; de Sousa Moreira, A.; Rodrigues, F.T.; Coelho, A.C.; Lopes, A.P.; Mesquita, J.R. First report of human Thelazia callipaeda infection in Portugal. Acta Trop. 2022, 231, 106436. [Google Scholar]
- Juhász, H.; Thury, G.; Szécsényi, M.; Tóth-Molnár, E.; Burián, K.; Deim, Z.; Terhes, G. Human Thelaziosis Caused by Thelazia callipaeda Eyeworm, Hungary. Emerg. Infect. Dis. 2022, 28, 2559–2561. [Google Scholar] [CrossRef]
- Pozio, E.; Zarlenga, D.S. New pieces of the Trichinella puzzle. Int. J. Parasitol. 2013, 43, 983–997. [Google Scholar] [CrossRef]
- Tenter, A.M.; Heckeroth, A.R.; Weiss, L.M. Toxoplasma gondii: From animals to humans. Int. J. Parasitol. 2000, 30, 1217–1258. [Google Scholar]
- Wanha, K.; Edelhofer, R.; Gabler-Eduardo, C.; Prosl, H. Prevalence of antibodies against Neospora caninum and Toxoplasma gondii in dogs and foxes in Austria. Vet. Parasitol. 2005, 128, 189–193. [Google Scholar] [CrossRef]
- Herrmann, D.C.; Maksimov, P.; Maksimov, A.; Sutor, A.; Schwarz, S.; Jaschke, W.; Schliephake, A.; Denzin, N.; Conraths, F.J.; Schares, G. Toxoplasma gondii in foxes and rodents from the German Federal States of Brandenburg and Saxony-Anhalt: Seroprevalence and genotypes. Vet. Parasitol. 2012, 185, 78–85. [Google Scholar] [CrossRef]
- Buchton, D.; Maley, S.W.; Pastoret, P.P.; Brochier, B.; Innes, E.A. Examination of red foxes (Vulpes vulpes) from Belgium for antibody to Neospora caninum and Toxoplasma gondii. Vet. Rec. 1997, 141, 308–309. [Google Scholar]
- Bártová, E.; Slezáková, R.; Nágl, I.; Sedlák, K.N. Neospora caninum and Toxoplasma gondii antibodies in red foxes (Vulpes vulpes) in the Czech Republic. Ann. Agric. Environ. Med. 2016, 23, 84–86. [Google Scholar] [CrossRef]
- Aubert, D.; Ajzenberg, D.; Richomme, C.; Gilot-Fromont, E.; Terrier, M.E.; de Gevigney, C.; Game, Y.; Maillard, D.; Gibert, P.; Dardé, M.L.; et al. Molecular and biological characteristics of Toxoplasma gondii isolates from wildlife in France. Vet. Parasitol. 2010, 171, 346–349. [Google Scholar] [CrossRef]
- Uzelac, A.; Ćirović, D.; Penezić, A.; Ćirković, V.; Djurković-Djaković, O. Detection and genotyping of Toxoplasma gondii in wild canids in Serbia. Parasitol. Int. 2019, 73, 101973. [Google Scholar] [CrossRef]
- Dubey, J.P.; Storandt, S.T.; Kwok, O.C.; Thulliez, P.; Kazacos, K.R. Toxoplasma gondii antibodies in naturally exposed wild coyotes, red foxes, and gray foxes and serologic diagnosis of Toxoplasmosis in red foxes fed T. gondii oocysts and tissue cysts. J. Parasitol. 1999, 85, 240–343. [Google Scholar] [CrossRef]
- Bjerkås, I. Neuropathology and host-parasite relationship of acute experimental toxoplasmosis of the blue fox (Alopex lagopus). Vet. Pathol. 1990, 27, 381–390. [Google Scholar]
- Webster, J.P. Rats, cats, people and parasites: The impact of latent toxoplasmosis on behaviour. Microbes Infect. 2001, 3, 1037–1345. [Google Scholar]
- Milne, G.; Fujimoto, C.; Bean, T.; Peters, H.J.; Hemmington, M.; Taylor, C.; Fowkes, R.C.; Martineau, H.M.; Hamilton, C.M.; Walker, M.; et al. Infectious Causation of Abnormal Host Behavior: Toxoplasma gondii and Its Potential Association With Dopey Fox Syndrome. Front. Psychiatry 2020, 11, 513536. [Google Scholar] [CrossRef]
- Gottstein, B.; Pozio, E.; Nöckler, K. Epidemiology, diagnosis, treatment, and control of trichinellosis. Clin. Microbiol. Rev. 2009, 22, 127–145. [Google Scholar] [CrossRef]
- De Craeye, S.; Speybroeck, N.; Ajzenberg, D.; Dardé, M.L.; Collinet, F.; Tavernier, P.; Van Gucht, S.; Dorny, P.; Dierick, K. Toxoplasma gondii and Neospora caninum in wildlife: Common parasites in Belgian foxes and Cervidae? Vet. Parasitol. 2011, 178, 64–69. [Google Scholar]
- Kapel, C.M.; Webster, P.; Gamble, H.R. Muscle distribution of sylvatic and domestic Trichinella larvae in production animals and wildlife. Vet Parasitol. 2005, 132, 101–105. [Google Scholar]
- EFSA. The EU summary report on trends and sources of zoonoses, zoonotic agents and food-borne outbreaks in 2013. EFSA J. 2013, 13, 3991. [Google Scholar]
- Bilska-Zając, E.; Różycki, M.; Grądziel-Krukowska, K.; Bełcik, A.; Mizak, I.; Karamon, J.; Sroka, J.; Zdybel, J.; Cencek, T. Diversity of Trichinella species in relation to the host species and geographical location. Vet. Parasitol. 2020, 279, 109052. [Google Scholar]
- Imre, K.; Pozio, E.; Tonanzi, D.; Sala, C.; Ilie, M.S.; Imre, M.; Morar, A. The red fox (Vulpes vulpes) plays a minor role in the epidemiology of the domestic cycle of Trichinella in Romania. Vet. Parasitol. 2015, 212, 448–450. [Google Scholar] [CrossRef]
- Eckert, J.; Deplazes, P. Alveolar echinococcosis in humans: The current situation in central Europe and the need for countermeasures. Parasitol Today 1999, 15, 315–319. [Google Scholar] [CrossRef]
- Oksanen, A.; Siles-Lucas, M.; Karamon, J.; Possenti, A.; Conraths, F.J.; Romig, T.; Wysocki, P.; Mannocci, A.; Mipatrini, D.; La Torre, G. The geographical distribution and prevalence of Echinococcus multilocularis in animals in the European Union and adjacent countries: A systematic review and meta-analysis. Parasit. Vectors 2016, 9, 519. [Google Scholar] [CrossRef]
- EFSA AHAW Panel (EFSA Panel on Animal Health and Welfare). Scientific opinion on Echinococcus multilocularis infection in animals. EFSA J. 2015, 13, 129. [Google Scholar]
- Citterio, C.V.; Obber, F.; Trevisiol, K.; Dellamaria, D.; Celva, R.; Bregoli, M. Echinococcus multilocularis and other cestodes in red foxes (Vulpes vulpes) of northeast Italy, 2012–2018. Parasit Vectors 2021, 14, 29. [Google Scholar]
- Obber, F.; Celva, R.; Da Rold, G.; Trevisiol, K.; Ravagnan, S.; Danesi, P. A highly endemic area of Echinococcus multilocularis identified through a comparative re-assessment of prevalence in the red fox (Vulpes vulpes), Alto Adige (Italy). PLoS ONE 2022, 17, e0268045. [Google Scholar]
- Davidson, R.K.; Romig, T.; Jenkins, E.; Tryland, M.; Robertson, L. The impact of globalization on thedistribution of Echinococcus multilocularis. Trends Parasitol. 2012, 28, 239–247. [Google Scholar] [CrossRef]
- Moks, E.; Saarma, U.; Valdmann, H. Echinococcus multilocularis in Estonia. Emerg. Infect. Dis. 2005, 11, 1973–1974. [Google Scholar] [CrossRef]
- Bagrade, G.; Snabel, V.; Romig, T.; Ozolins, J.; Huettner, M.; Miterpakova, M.; Sevcova, D.; Dubinsky, P. Echinococcus multilocularis is a frequent parasite of red foxes (Vulpes vulpes) in Latvia. Helminthologia 2008, 45, 157–161. [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC). Echinococcosis: Annual Epidemiological Report for 2016; ECDC: Stockholm, Sweden, 2018. [Google Scholar]
- Mackenstedt, U.; Jenkins, D.; Romig, T. The role of wildlife in the transmission of parasitic zoonoses in peri-urban and urban areas. Int. J. Parasitol Parasites Wildl. 2015, 4, 71–79. [Google Scholar]
- Hofer, S.; Gloor, S.; Müller, U.; Mathis, A.; Hegglin, D.; Deplazes, P. High prevalence of Echinococcus multilocularis in urban red foxes (Vulpes vulpes) and voles (Arvicola terrestris) in the city of Zürich, Switzerland. Parasitology 2000, 120, 135–142. [Google Scholar] [CrossRef]
- Bruschi, F.; Pozio, E. Trichinella britovi. Trends Parasitol. 2020, 36, 227–228. [Google Scholar]
- Latrofa, M.S.; Lia, R.P.; Giannelli, A.; Colella, V.; Santoro, M.; D’Alessio, N.; Campbell, B.E.; Parisi, A.; Dantas-Torres, F.; Mutafchiev, Y.; et al. Crenosoma vulpis in wild and domestic carnivores from Italy: A morphological and molecular study. Parasitol. Res. 2015, 114, 3611–3617. [Google Scholar]
- Koch, J.; Willesen, J.L. Canine pulmonary angiostrongylosis: An update. Vet. J. 2009, 179, 348–359. [Google Scholar] [CrossRef]
- Traversa, D.; Di Cesare, A.; Conboy, G. Canine and feline cardiopulmonary parasitic nematodes in Europe: Emerging and underestimated. Parasit. Vectors 2010, 3, 62. [Google Scholar] [CrossRef]
- Conboy, G. Helminth parasites of the canine and feline respiratory tract. Vet. Clin. N. Am. Small. Anim. Pract. 2009, 39, 1109–1126. [Google Scholar]
- Saeed, C.; Maddox-Hyttel, J.; Monrad, C.M. Kapel Helminths of red foxes (Vulpes vulpes) in Denmark. Vet. Parasitol. 2006, 139, 168–179. [Google Scholar]
- Al-Sabi, M.N.S.; Halasa, T.; Kapel, C.M.O. Infections with cardiopulmonary and intestinal helminths and sarcoptic mange in red foxes from two different localities in Denmark. Acta Parasitol. 2014, 59, 98–107. [Google Scholar]
- Davidson, R.K.; Gjerde, B.; Vikøren, T.; Lillehaug, A.; Handeland, K. Prevalence of Trichinella larvae and extra-intestinal nematodes in Norwegian red foxes (Vulpes vulpes). Vet. Parasitol. 2006, 136, 307–316. [Google Scholar] [CrossRef]
- Lalosevic, V.; Lalosevic, D.; Capo, I.; Simin, V.; Galfi, A.; Traversa, D. High infection rate of zoonotic Eucoleus aerophilus infection in foxes from Serbia. Parasite 2013, 20, 3. [Google Scholar]
- Karamon, J.; Dąbrowska, J.; Kochanowski, M.; Samorek-Pieróg, M.; Sroka, J.; Różycki, M.; Cencek, T. Prevalence of intestinal helminths of red foxes (Vulpes vulpes) in central Europe (Poland): A significant zoonotic threat. Parasit. Vectors 2018, 11, 436. [Google Scholar] [CrossRef]
- Schug, K.; Krämer, F.; Schaper, R.; Hirzmann, J.; Failing, K.; Hermosilla, C.; Taubert, A. Prevalence survey on lungworm (Angiostrongylus vasorum, Crenosoma vulpis, Eucoleus aerophilus) infections of wild red foxes (Vulpes vulpes) in central Germany. Parasit. Vectors 2018, 11, 85. [Google Scholar]
- Sréter, T.; Széll, Z.; Marucci, G.; Pozio, E.; Varga, I. Extraintestinal nematode infections of red foxes (Vulpes vulpes) in Hungary. Vet. Parasitol. 2003, 115, 329–334. [Google Scholar]
- Franssen, F.; Deksne, G.; Esíte, Z.; Havelaar, A.; Swart, A.; van der Giessen, J. Trend analysis of Trichinella in a red fox population from a low endemic area using a validated artificial digestion and sequential sieving technique. Vet. Res. 2014, 45, 120. [Google Scholar]
- Magi, M.; Guardone, L.; Prati, M.C.; Mignone, W.; Macchioni, F. Extraintestinal nematodes of the red fox Vulpes vulpes in north-west Italy. J. Helminthol. 2015, 89, 506–511. [Google Scholar]
- Di Cesare, A.; Castagna, G.; Otranto, D.; Meloni, S.; Milillo, P.; Latrofa, M.S.; Paoletti, B.; Bartolini, R.; Traversa, D. Molecular detection of Capillaria aerophila, an agent of canine and feline pulmonary capillariosis. J. Clin. Microbiol. 2012, 5, 1958–1963. [Google Scholar]
- Lalosevic, D.; Lalosevic, V.; Klem, I.; Stanojev-Jovanovic, D.; Pozio, E. Pulmonary capillariasis miming bronchial carcinoma. Am. J. Trop. Med. Hyg. 2008, 78, 14–16. [Google Scholar] [CrossRef]
- Bolt, G.; Monrad, J.; Frandsen, F.; Henriksen, P.; Dietz, H.H. The common frog (Rana temporaria) as a potential paratenic and intermediate host for Angiostrongylus vasorum. Parasitol. Res. 1993, 79, 428–430. [Google Scholar] [CrossRef]
- Bolt, G.; Monrad, J.; Henriksen, P.; Dietz, H.; Koch, J.; Bindseil, E.; Jensen, A. The fox (Vulpes vulpes) as a reservoir for canine angiostrongylosis in Denmark. Field survey and experimental infections. Acta Vet. Scand. 1992, 33, 357–362. [Google Scholar] [CrossRef]
- Mozzer, L.R.; Lima, W.S. Gallus gallus domesticus: Paratenic host of Angiostrongylus vasorum. Vet. Parasitol. 2015, 207, 81–84. [Google Scholar]
- Morgan, E.R.; Jefferies, R.; Krajewski, M.; Ward, P.; Shaw, S.E. Canine pulmonary angiostrongylosis: The influence of climate on parasite distribution. Parasitol. Int. 2009, 58, 406–410. [Google Scholar]
- Taylor, C.S.; Garcia Gato, R.; Learmount, J.; Aziz, N.A.; Montgomery, C.; Rose, H. Increased prevalence and geographic spread of the cardiopulmonary nematode Angiostrongylus vasorum in fox populations in Great Britain. Parasitology 2015, 142, 1190–1195. [Google Scholar] [CrossRef]
- Deak, G.; Gherman, C.M.; Ionică, A.M.; Vezendan, A.D.; D’Amico, G.; Matei, I.A.; Daskalaki, A.A.; Marian, I.; Damian, A.; Cozma, V.; et al. Angiostrongylus vasorum in Romania: An extensive survey in red foxes, Vulpes vulpes. Parasit. Vectors 2017, 12, 33. [Google Scholar]
- Morgan, E.R.; Tomlinson, A.; Hunter, S.; Nichols, T.; Roberts, E.; Fox, M.T.; Taylor, M.A. Angiostrongylus vasorum and Eucoleus aerophilus in foxes (Vulpes vulpes) in Great Britain. Vet. Parasitol. 2008, 154, 4857. [Google Scholar] [CrossRef]
- Traversa, D.; Di Cesare, A.; Meloni, S.; Frangipane di Regalbono, A.; Milillo, P.; Pampurini, F.; Venco, L. Canine angiostrongylosis in Italy: Occurrence of Angiostrongylus vasorum in dogs with compatible clinical pictures. Parasitol. Res. 2013, 112, 24732480. [Google Scholar]
- Simpson, V.R. Angiostrongylus vasorum infection in foxes (Vulpes vulpes) in Cornwall. Vet. Rec. 1996, 139, 443–445. [Google Scholar]
- Tieri, E.E.; Saletti, M.A.; D’Angelo, A.R.; Parisciani, G.; Pelini, S.; Cocco, A.; Di Teodoro, G.; Di Censo, E.; D’Alterio, N.; Latrofa, M.S.; et al. Angiostrongylus vasorum in foxes (Vulpes vulpes) and wolves (Canis lupus italicus) from Abruzzo region, Italy. Int. J. Parasitol. Parasites Wildl. 2021, 15, 184–194. [Google Scholar] [CrossRef]
- Gillis-Germitsch, N.; Tritten, L.; Hegglin, D.; Deplazes, P.; Schnyder, M. Conquering Switzerland: The emergence of Angiostrongylus vasorum in foxes over three decades and its rapid regional increase in prevalence contrast with the stable occurrence of lungworms. Parasitology 2020, 147, 1071–1079. [Google Scholar]
- Morelli, S.; Gori, F.; Colombo, M.; Traversa, D.; Sarrocco, G.; Simonato, G.; Nespeca, C.; Di Cesare, A.; Frangipane di Regalbono, A.; Veronesi, F.; et al. Simultaneous Exposure to Angiostrongylus vasorum and Vector-Borne Pathogens in Dogs from Italy. Pathogens 2021, 10, 1200. [Google Scholar]
- Santoro, M.; D’Alessio, N.; Di Prisco, F.; Neola, B.; Restucci, B.; Pagano, T.B.; Veneziano, V. Angiostrongylus vasorum infection in red foxes (Vulpes vulpes) in southern Italy. Acta Parasitol. 2015, 60, 356–359. [Google Scholar]
- Eleni, C.; Grifoni, G.; Di Egidio, A.; Meoli, R.; De Liberato, C. Pathological findings of Angiostrongylus vasorum infection in red foxes (Vulpes vulpes) from Central Italy, with the first report of a disseminated infection in this host species. Parasitol. Res. 2014, 113, 1247–1250. [Google Scholar]
- Hamnes, I.S.; Gjerde, B.K.; Forberg, T.; Robertson, L.J. Occurrence of Giardia and Cryptosporidium in Norwegian red foxes (Vulpes vulpes). Vet. Parasitol. 2007, 143, 347–353. [Google Scholar] [CrossRef]
- Papini, R. Giardia and Cryptosporidium in Red Foxes (Vulpes vulpes): Screening for Coproantigens in a Population of Central Italy and Mini-Review of the Literature. Mac. Vet. Rev. 2019, 42, 101–106. [Google Scholar]
- Bružinskaitė-Schmidhalter, R.; Šarkūnas, M.; Malakauskas, A.; Mathis, A.; Torgerson, P.; Deplazes, P. Helminths of red foxes (Vulpes vulpes) and raccoon dogs (Nyctereutes procyonoides) in Lithuania. Parasitology 2012, 139, 120–127. [Google Scholar]
- Vergles, A.; Rataj, J.; Posedi, D.; Zele, G. Vengušt Intestinal parasites of the red fox (Vulpes vulpes) in Slovenia. Acta Vet. Hung. 2013, 61, 454–462. [Google Scholar]
- Hrčkova, G.; Miterpáková, M.; O’Connor, A.; Snábel, V.; Olson, P.D. Molecular and morphological circumscription of Mesocestoides tapeworms from red foxes (Vulpes vulpes) in central Europe. Parasitology 2011, 138, 638–647. [Google Scholar]
- Korpysa-Dzirba, W.; Różycki, M.; Bilska-Zając, E.; Karamon, J.; Sroka, J.; Bełcik, A.; Wasiak, M.; Cencek, T. Alaria alata in Terms of Risks to Consumers’ Health. Foods 2021, 10, 1614. [Google Scholar]
- Reperant, L.A.; Hegglin, D.; Fischer, C.; Kohler, L.; Weber, J.M.; Deplazes, P. Influence of urbanization on the epidemiology of intestinal helminths of the red fox (Vulpes vulpes) in Geneva, Switzerland. Parasitol. Res. 2007, 101, 605–611. [Google Scholar]
- Borecka, A.; Gawor, J.; Zięba, F. A survey of intestinal helminths in wild carnivores from the Tatra National Park, southern Poland. Ann. Parasitol. 2013, 59, 169–172. [Google Scholar]
- Aleksić, J.; Stepanović, P.; Dimitrijević, S.; Gajić, B.; Bogunović, D.; Davidov, I.; Aleksić-Agelidis, A.; Ilić, T. Capillaria plica in Red Foxes (Vulpes vulpes) from Serbia: Epidemiology and Diagnostic Approaches to Urinary Capillariosis in Domestic Carnivores. Acta Parasit. 2020, 65, 954–962. [Google Scholar]
- Rojas, A.; Sanchis-Monsonís, G.; Alić, A.; Hodžić, A.; Otranto, D.; Yasur-Landau, D.; Martínez-Carrasco, C.; Baneth, G. Spirocerca vulpis sp. nov. (Spiruridae: Spirocercidae): Description of a new nematode species of the red fox, Vulpes vulpes (Carnivora: Canidae). Parasitology 2018, 21, 1–12. [Google Scholar]
- Sanchis-Monsonis, G.; Tizzani, P.; Ruiz de Ybanez, R.; Rojas, A.; Baneth, G.; Martínez-Carrasco, C. Spirocercosis in Red Foxes (Vulpes vulpes) from the Valencian Community (Eastern Spain). In Proceedings of the XX Congreso de la Sociedad Española de Parasitología, La Laguna, Tenerife, Spain, 19–21 July 2017. [Google Scholar]
- Jhala, Y.V.; Moehlman, P.D. Golden jackal Canis aureus Linnaeus, 1758. Least Concern. In Status Survey and Conservation Action Plan. Canids: Foxes, Wolves, Jackals and Dogs; IUCN: Gland, Switzerland; Cambridge, UK, 2004; pp. 156–161. [Google Scholar]
- Koepfli, K.P.; Pollinger, J.; Godinho, R.; Robinson, J.; Lea, A.; Hendricks, S.; Schweizer, R.M. Genome-wide evidence reveals that African and Eurasian Golden jackals are distinct species. Curr Biol. 2015, 25, 2158–2165. [Google Scholar]
- Gherman, C.M.; Mihalca, A.D. A synoptic overview of Golden jackal parasites reveals high diversity of species. Parasit. Vectors 2017, 10, 419. [Google Scholar]
- Hoffmann, M.; Arnold, J.; Duckworth, J.W.; Jhala, Y.; Kamler, J.F.; Krofel, M. Canis aureus (errata version published in 2020). IUCN Red List. Threat. Species 2018, e.T118264161A163507876. Available online: https://dx.doi.org/10.2305/IUCN.UK.2018-2.RLTS.T118264161A163507876.en (accessed on 27 December 2022).
- Trouwborst, A.; Krofel, M.; Linnell, J.D.C. Legal implications of range expansions in a terrestrial carnivore: The case of the Golden jackal (Canis aureus) in Europe. Biodivers Conserv. 2015, 24, 2593–2610. [Google Scholar]
- Arnold, J.; Humer, A.; Heltai, M.; Murariu, D.; Spassov, N.; Hackländer, K. Current status and distribution of golden jackals Canis aureus in Europe. Mamm Rev. 2012, 42, 1–11. [Google Scholar] [CrossRef]
- Frey, C.F.; Basso, W.U.; Zürcher-Giovannini, S.; Marti, I.; Borel, S.; Guthruf, S.; Gliga, D.; Lundström-Stadelmann, B.; Origgi, F.C.; Ryser-Degiorgis, M.P. The Golden jackal (Canis aureus): A new host for Echinococcus multilocularis and Trichinella britovi in Switzerland. Schweiz. Arch. Tierheilkd 2022, 164, 71–78. [Google Scholar]
- Ćircović, D.; Penezić, A.; Pavlović, I.; Kulišić, Z.; Ćosić, N.; Burazerović, J.; Maletić, V. First records of Dirofilaria repens in wild canids from the region of Central Balkan. Acta Vet. Hung. 2014, 62, 481–488. [Google Scholar] [CrossRef]
- Penezić, A.; Selaković, S.; Pavlović, I.; Ćirović, D. First findings and prevalence of adult heartworms (Dirofilaria immitis) in wild carnivores from Serbia. Parasitol. Res. 2014, 113, 3281–3285. [Google Scholar]
- Zivojinovic, M.; Sofronic-Milosavljevic, L.J.; Cvetkovic, J.; Pozio, E.; Interisano, M.; Plavsic, B.; Radojicic, S.; Kulisic, Z. Trichinella infections in different host species of an endemic district of Serbia. Vet. Parasitol. 2013, 194, 136–138. [Google Scholar]
- Lanszki, J.; Heltai, M.; Szabó, L. Feeding habits and trophic niche overlap between sympatric Golden jackal (Canis aureus) and red fox (Vulpes vulpes) in the Pannonian ecoregion (Hungary). Can. J. Zool. 2006, 84, 1647–1656. [Google Scholar]
- Balog, T.; Nagy, G.; Halász, T.; Csányi, E.; Zomborsszky, Z.; Csivincsik, Á. The occurrence of Echinococcus spp. in Golden jackal (Canis aureus) in southwestern Hungary: Should we need to rethink its expansion? Parasitol. Int. 2021, 80, 102214. [Google Scholar]
- Széll, Z.; Marucci, G.; Pozio, E.; Sréter, T. Echinococcus multilocularis and Trichinella spiralis in Golden jackals (Canis aureus) of Hungary. Vet. Parasitol. 2013, 197, 393–396. [Google Scholar]
- Lalošević, D.; Lalošević, V.; Simin, V.; Miljević, M.; Čabrilo, B.; Bjelić Čabrilo, O. Spreading of multilocular echinococcosis in southern Europe: The first record in foxes and jackals in Serbia, Vojvodina Province. Eur. J. Wildl. Res. 2016, 62, 793–796. [Google Scholar] [CrossRef]
- Florijančić, T.; Ozimec, S.; Bošković, I.; Degmečić, D.; Urošević, B.; Nekvapil, N. Survey on sylvatic parasitosis in Podunavlje Region of Croatia. In Modern Aspects of Sustainable Management of Game Population, Proceedings of the International Symposium on Hunting, Zemun, Serbia, 22–24 June 2012; University of Belgrade, Faculty of Agriculture: Zemun, Serbia, 2012. [Google Scholar]
- Mihalca, A.D.; Ionică, A.M.; D’Amico, G.; Daskalaki, A.A.; Deak, G.; Matei, I.A. Thelazia callipaeda in wild carnivores from Romania: New host and geographical records. Parasit. Vectors. 2016, 9, 350. [Google Scholar]
- Lavrov, N.P. Results of raccoon dog introductions in different parts of the soviet union. Tr. Kafedr. Biol. MGZPI. 1971, 29, 101–160. [Google Scholar]
- Kauhala, K.; Saeki, M. Raccoon dog Nyctereutes procyonoides. In Canids: Foxes, Wolves, Jackals and Dogs: Status Survey and Conservation Action Plan; Sillero-Zubiri, C., Hoffmann, M., Macdonald, D.W., Eds.; IUCN Publication Services: Cambridge, UK, 2004; pp. 136–142. [Google Scholar]
- Al-Sabi, M.N.; Chriél, M.; Jensen, T.; Enemark, H. Endoparasites of the raccoon dog (Nyctereutes procyonoides) and the red fox (Vulpes vulpes) in Denmark 2009–2012—A comparative study. Int. J. Parasitol. Parasites Wildl. 2013, 17, 144–151. [Google Scholar] [CrossRef]
- Deplazes, P.; Hegglin, D.; Gloor, S.; Romig, T. Wilderness in the city: The urbanization of Echinococcus multilocularis. Trends Parasitol. 2004, 20, 77–84. [Google Scholar] [CrossRef]
- Kauhala, K.; Kowalczyk, R. Invasion of the raccoon dog Nyctereutes procyonoides in Europe: History of colonization, features behind its success, and threats to native fauna. Curr. Zool. 2011, 57, 584–598. [Google Scholar] [CrossRef]
- Oivanen, L.; Kapel, C.M.; Pozio, E.; La Rosa, G.; Mikkonen, T.; Sukura, A. Associations between Trichinella Species and Host Species in Finland. J. Parasitol. 2002, 88, 84–88. [Google Scholar]
- Cabaj, W.; Moskwa, B.; Pastusiak, K.; Bień, J. Włośnica u zwierząt wolno żyjących stałym zagrożeniem zdrowia ludzi w Polsce. Kosmos 2005, 54, 95–103. [Google Scholar]
- Osten-Sacken, N.; Solarczyk, P. Trichinella spiralis in road-killed raccoon dogs (Nyctereutes procyonoides) in western Poland. Ann. Parasitol. 2016, 62, 77–79. [Google Scholar]
- Cybulska, A.; Kornacka, A.; Moskwa, B. The occurrence and muscle distribution of Trichinella britovi in raccoon dogs (Nyctereutes procyonoides) in wildlife in the Głęboki Bród Forest District, Poland. Int. J. Parasitol. Parasites Wildl. 2019, 9, 149–153. [Google Scholar]
- Mayer-Scholl, A.; Reckinger, S.; Schulze, C.; Nöckler, K. Study on the occurrence of Trichinella spp. in raccoon dogs in Brandenburg, Germany. Vet. Parasitol. 2016, 231, 102–105. [Google Scholar] [CrossRef]
- Duscher, T.; Hodžić, A.; Glawischnig, W.; Duscher, G. The raccoon dog (Nyctereutes procyonoides) and the raccoon (Procyon lotor)—Their role and impact of maintaining and transmitting zoonotic diseases in Austria, Central Europe. Parasitol. Res. 2017, 116, 1411–1416. [Google Scholar]
- Kärssin, A.; Häkkinen, L.; Niin, E.; Peik, K.; Vilem, A.; Jokelainen, P. Lassen Trichinella spp. biomass has increased in raccoon dogs (Nyctereutes procyonoides) and red foxes (Vulpes vulpes) in Estonia. Parasit. Vectors 2017, 10, 609. [Google Scholar]
- Mikkonen, L.; Oivanen, A.; Näreaho, H.; Helin, A. Sukura Predilection muscles and physical condition of raccoon dog (Nyctereutes procyonoides) experimentally infected with Trichinella spiralis and Trichinella nativa. Acta Vet. Scand. 2001, 42, 441–452. [Google Scholar]
- Kapel, C.M.O.; Torgerson, P.; Thompson, R.; Deploy, P. Reproductive potential of Echinococcus multilocularis in experimentally infected foxes, dogs, raccoon dogs and cats. Int. J. Parasitol. 2006, 36, 79–86. [Google Scholar]
- Romig, T.; Deplazes, P.; Jenkins, D.; Giraudoux, P.; Massolo, A.; Craig, P.S.; Wassermann, M.; Takahashi, K.; de la Rue, M. Ecology and life cycle patterns of Echinococcus species. In Echinococcus and Echinococcosis, Part A; Thompson, R.C.A., Deplazes, P., Lymbery, A.J., Eds.; Elsevier: Amsterdam, The Netherlands, 2017; Volume 95, pp. 213–314. [Google Scholar]
- Hurníková, Z.; Miterpáková, M.; Chovancová, B. The important zoonoses in the protected areas of the Tatra National Park (TANAP). Wiad Parazytol. 2009, 55, 395–398. [Google Scholar]
- Machnicka-Rowińska, B.; Rocki, B.; Dziemian, E.; Kołodziej-Sobocińska, M. Raccoon dog (Nyctereutes procyonoides)—The new host of Echinococcus multilocularis in Poland. Wiad. Parazytol. 2002, 48, 65–68. [Google Scholar]
- Möhl, K.; Grosse, K.; Hamedy, A.; Wüste, T.; Kabelitz, P.; Lücker, E. Biology of Alaria spp. and human exposition risk to Alaria mesocercariae-a review. Parasitol. Res. 2009, 105, 1–15. [Google Scholar]
- Nowak, R.M. Walker’s Carnivores of the World, 1st ed.; The Johns Hopkins University Press: Baltimore, MD, USA, 2005; p. 313. [Google Scholar]
- Salgado, I. Is the raccoon (Procyon lotor) out of control in Europe? Biodivers. Conserv. 2018, 27, 2243–2256. [Google Scholar]
- Bauer, C. Baylisascariosis—Infections of animals and humans with ‘unusual’ roundworms. Vet. Parasitol. 2013, 193, 404–412. [Google Scholar] [CrossRef]
- Fischer, M.L.; Hochkirch, A.; Heddergott, M.; Schulze, C.; Anheyer-Behmenburg, H.E.; Lang, J.; Michler, F.U.; Hohmann, U.; Ansorge, H.; Hoffmann, L.; et al. Historical invasion records can be misleading: Genetic evidence for multiple introductions of invasive raccoons (Procyon lotor) in Germany. PLoS ONE 2015, 10, e0125441. [Google Scholar]
- Beltrán-Beck, B.; García, F.; Gortázar, C. Raccoons in Europe: Disease hazards due to the establishment of an invasive species. Eur. J. Wildl. Res. 2012, 58, 5–15. [Google Scholar] [CrossRef]
- Al-Sabi, M.N.S.; Chriél, M.; Hansen, M.S.; Enemark, H.L. Baylisascaris procyonis in wild raccoons (Procyon lotor) in Denmark. Vet. Parasitol. Reg. Stud. Rep. 2015, 1, 55–58. [Google Scholar]
- Rosatte, R.C. Management of raccoons (Procyon lotor) in Ontario, Canada: Do human intervention and disease have significant impact on raccoon populations? In Proceedings of the 1st Euro-American Mammal Congress Mammalia, Santiago de Composte, Spain, 19–24 July 2000. [Google Scholar]
- Romeo, C.; Cafiso, A.; Fesce, E.; Martínez-Rondán, F.J.; Panzeri, M.; Martinoli, A. Lost and found: Helminths infecting invasive raccoons introduced to Italy. Parasitol. Int. 2021, 86, 102354. [Google Scholar]
- French, S.K.; Pearl, D.L.; Shirose, L.; Peregrine, A.S.; Jardine, C.M. Demographic and environmental factors associated with Baylisascaris procyonis infection of raccoons (Procyon lotor) in Ontario, Canada. J. Wildl. Dis. 2020, 56, 328–337. [Google Scholar]
- Kazacos, K.R. Baylisascaris procyonis and related species. In Parasitic Diseases of Wild Mammals, 2nd ed.; Samuel, W.M., Pybus, M.J., Kocan, A.A., Eds.; Iowa State University Press: Ames, IA, USA, 2008; pp. 301–341. [Google Scholar]
- Kazacos, K.R.; Jelicks, L.A.; Tanowitz, H.B. Baylisascaris larva migrans. In Handbook of Clinical Neurology, 1st ed.; Garcia, H.H., Tanowitz, H.B., Del Brutto, O.H., Eds.; Elsevier: Amsterdam, The Netherlands, 2013; pp. 251–262. [Google Scholar]
- Rentería-Solís, Z.; Birka, S.; Schmäschke, R.; Król, N.; Obiegala, A. First detection of Baylisascaris procyonis in wild raccoons (Procyon lotor) from Leipzig, Saxony, Eastern Germany. Parasitol. Res. 2018, 117, 3289–3292. [Google Scholar]
- Lombardo, A.; Brocherel, G.; Donnini, C.; Fichi, G.; Mariacher, A.; Diaconu, E.L.; Carfora, V.; Battisti, A.; Cappai, N.; Mattioli, L.; et al. First report of the zoonotic nematode Baylisascaris procyonis in non-native raccoons (Procyon lotor) from Italy. Parasit. Vectors 2022, 15, 24. [Google Scholar]
- Stone, W.S. Intestinal obstruction in raccoons caused by the ascarid Baylisascaris Procyonis. NY Fish Game J. 1983, 30, 117–118. [Google Scholar]
- Carlson, B.L.; Nielsen, S. Jejunal obstruction due to Baylisascaris procyonis in a raccoon. J. Am. Vet. Med. Assoc. 1984, 185, 1396–1397. [Google Scholar]
- Page, K.; Beasley, J.C.; Olson, Z.H.; Smyser, T.J.; Downey, M.; Kellner, K.F. Reducing Baylisascaris procyonis roundworm larvae in raccoon latrines. Emerg. Infect. Dis. 2011, 17, 90–93. [Google Scholar] [CrossRef]
- Sorvillo, F.; Ash, L.R.; Berlin, O.G.W.; Yatabe, J.; Degiorgio, C.; Morse, S.A. Baylisascaris procyonis: An emerging helminthic zoonosis. Emerg. Infect. Dis. 2002, 8, 355–359. [Google Scholar] [CrossRef]
- Gavin, P.J.; Kazacos, K.R.; Shulman, S.T. Baylisascariasis. Clin. Microbiol. Rev. 2005, 18, 703–718. [Google Scholar] [CrossRef]
- Küchle, M.; Knorr, H.L.J.; Medenblik-Frysch, S.; Weber, A.; Bauer, C.; Naumann, G.O.H. Diffuse unilateral subacute neuroretinitis syndrome in a German most likely caused by the raccoon roundworm, Baylisascaris procyonis. Graefe’s Arch. Clin. Exp. Ophthalmol. 1993, 231, 48–51. [Google Scholar]
- Schad, G.A. Morphology and life history of Strongylides stercoralis. In Strongyloidiasis: A Major Roundworm Infection of Man; Grove, D.I., Ed.; Taylor and Francis: London, UK, 1989; pp. 85–104. [Google Scholar]
- Little, M.D. Comparative Morphology of Six Previously Described and Seven New Species of Strongyloides (Nematoda). Ph.D. Thesis, Tulane University, New Orleans, LA, USA, 1961. [Google Scholar]
- Popiołek, M.; Staśkiewicz, J.; Bartoszewicz, M.; Okarma, H.; Smalec, B.; Zalewski, A. Helminth parasites of an introduced invasive carnivore species, the raccoon (Procyon lotor L.), from the Warta Mouth National Park (Poland). J. Parasitol. 2011, 97, 357–360. [Google Scholar]
- Little, M.D. Comparative morphology of six species of Strongyloides (Nematoda) and redefinition of the genus. J. Parasitol. 1966, 52, 69–84. [Google Scholar] [CrossRef]
- Little, M.D. Dermatitis in a human volunteer infected with Strongyloides of nutria and raccoon. Am. J. Trop. Med. Hyg. 1965, 14, 1007–1009. [Google Scholar] [CrossRef]
- Speare, R. Identification of species of Strongyloides. In Strongyloidiasis: A Major Roundworm Infection of Man; Grove, D.I., Ed.; Taylor and Francis: London, UK, 1989; pp. 11–83. [Google Scholar]
- Kitchener, A.C.; Breitenmoser-Würsten, C.; Eizirik, E.; Gentry, A.; Werdelin, L.; Wilting, A.; Yamaguchi, N.; Abramov, A.V.; Christiansen, P.; Driscoll, C.; et al. A revised taxonomy of the Felidae. The final report of the Cat Classification Task Force of the IUCN/SSC Cat Specialist Group. Cat News 2017, 11, 80. [Google Scholar]
- Boitani, L.; Linnell, J.D. Bringing large mammals back: Large carnivores in Europe. In Rewilding European Landscapes; Springer: Cham, Switzerland, 2015; pp. 67–84. [Google Scholar]
- Hunter, L.; Barrett, P. Wild Cats of the World, Reissue ed; Bloomsbury Wildlife: London, UK, 2019; p. 240. [Google Scholar]
- Gerngross, P.; Ambarli, H.; Angelici, F.M.; Anile, S.; Campbell, R.; Ferreras de Andres, P.; Gil-Sanchez, J.M.; Götz, M.; Jerosch, S.; Mengüllüoglu, D.; et al. Felis silvestris. IUCN Red List. Threat. Species 2022, e.T181049859A181050999. Available online: https://doi.org/10.2305/IUCN.UK.2022-1.RLTS.T181049859A181050999.en (accessed on 15 August 2022).
- Steeb, S. Postmortale Untersuchungen an der Europäischen Wildkatze (Felis silvestris silvestris SCHREBER, 1777). Ph.D. Thesis, Fachbereich Veterinärmedizin der Justus-Liebig-Universität Gießen, Belgrade, Serbia, 2015. Available online: http://geb.uni-giessen.de/geb/volltexte/2015/11349/ (accessed on 2 December 2022).
- Martinkovic, F.; Sindicic, M.; Lucinger, S.; Štimac, I.; Bujanic, M.; Živicnjak, T.; Jan, D.S.; Šprem, N.; Popovic, R.; Konjevic, D. Endoparasites of wildcats in Croatia. Vet. Arh. 2017, 87, 713–729. [Google Scholar]
- Napoli, E.; Anile, S.; Arrabito, C.; Scornavacca, D.; Mazzamuto, M.V.; Gaglio, G.; Otranto, D.; Giannetto, S.; Brianti, E. Survey on parasitic infections in wildcat (Felis silvestris silvestris Schreber, 1777) by scat collection. Parasitol. Res. 2016, 115, 255–261. [Google Scholar] [CrossRef]
- Diakou, A.; Migli, D.; Dimzas, D.; Morelli, S.; Di Cesare, A.; Youlatos, D.; Lymberakis, P.; Traversa, D. Endoparasites of European Wildcats (Felis silvestris) in Greece. Pathogens 2021, 10, 594. [Google Scholar] [CrossRef]
- Dubey, J.P. History of the discovery of the life cycle of Toxoplasma gondii. Int. J. Parasitol. 2009, 39, 877–882. [Google Scholar] [CrossRef]
- Lukesová, D.; Literák, I. Shedding of Toxoplasma gondii oocysts by Felidae in zoos in the Czech Republic. Vet. Parasitol. 1998, 74, 1–7. [Google Scholar] [CrossRef]
- Dubey, J.P.; Murata, F.; Cerqueira-Cézar, C.K.; Kwok, O.; Su, C. Epidemiologic and public health significance of Toxoplasma gondii infections in bears (Ursus spp.): A 50 year review including recent genetic evidence. J. Parasitol. 2021, 107, 519–528. [Google Scholar] [CrossRef]
- Dubey, J.P. Toxoplamosis of Humans and Animals, 2nd ed.; CRC Press: Beltsville, MD, USA, 2010. [Google Scholar]
- Morelli, S.; Diakou, A.; Di Cesare, A.; Colombo, M.; Traversa, D. Canine and Feline Parasitology: Analogies, Differences, and Relevance for Human Health. Clin. Microbiol. Rev. 2021, 34, e0026620. [Google Scholar] [CrossRef]
- Simpson, V.R.; Hargreaves, J.; Butler, H.M.; Davison, N.J.; Everest, D.J. Causes of mortality and pathological lesions observed post-mortem in red squirrels (Sciurus vulgaris) in Great Britain. BMC Vet. Res. 2013, 9, 1–14. [Google Scholar]
- Almeria, S.; Murata, F.H.A.; Cerqueira-Cézar, C.K.; Kwok, O.C.H.; Shipley, A.; Dubey, J.P. Epidemiological and Public Health Significance of Toxoplasma gondii Infection in Wild Rabbits and Hares: 2010–2020. Microorganisms 2021, 9, 597. [Google Scholar] [CrossRef]
- McOrist, S. Diseases of the European wildcat (Felis silvestris Schreber, 1777) in Great Britain. Rev. Sci. Et Tech. (Int. Off. Epizoot.) 1992, 11, 1143–1149. [Google Scholar] [CrossRef]
- Sobrino, R.; Cabezón, O.; Millán, J.; Pabón, M.; Arnal, M.C.; Luco, D.F.; Gortázar, C.; Dubey, J.P.; Almeria, S. Seroprevalence of Toxoplasma gondii antibodies in wild carnivores from Spain. Vet. Parasitol. 2007, 148, 187–192. [Google Scholar] [CrossRef]
- Waap, H.; Nunes, T.; Vaz, Y.; Leitão, A. Serological survey of Toxoplasma gondii and Besnoitia besnoiti in a wildlife conservation area in southern Portugal. Vet. Parasitol. Reg. Stud. Rep. 2016, 3, 7–12. [Google Scholar] [CrossRef]
- Afonso, E.; Germain, E.; Poulle, M.L.; Ruette, S.; Devillard, S.; Say, L.; Villena, I.; Aubert, D.; Gilot-Fromont, E. Environmental determinants of spatial and temporal variations in the transmission of Toxoplasma gondii in its definitive hosts. Int. J. Parasitol. Parasites Wildl. 2013, 2, 278–285. [Google Scholar] [CrossRef]
- Herrmann, D.C.; Wibbelt, G.; Götz, M.; Conraths, F.J.; Schares, G. Genetic characterisation of Toxoplasma gondii isolates from European beavers (Castor fiber) and European wildcats (Felis silvestris silvestris). Vet. Parasitol. 2013, 191, 108–111. [Google Scholar] [CrossRef]
- Hatam-Nahavandi, K.; Calero-Bernal, R.; Rahimi, M.T.; Pagheh, A.S.; Zarean, M.; Dezhkam, A.; Ahmadpour, E. Toxoplasma gondii infection in domestic and wild felids as public health concerns: A systematic review and meta-analysis. Sci Rep. 2021, 11, 9509. [Google Scholar] [CrossRef]
- Diakou, A.; Morelli, S. Challenging the 9 lives: Parasites of cats and wildcats. In Proceedings of the XXXII Congresso SoIPa, Napoli, Italy, 27–30 June 2022; p. 41. [Google Scholar]
- Unterköfler, M.S.; Harl, J.; Barogh, B.S.; Spergser, J.; Hrazdilová, K.; Müller, F.; Jeschke, D.; Anders, O.; Steinbach, P.; Ansorge, H.; et al. Molecular analysis of blood-associated pathogens in European wildcats (Felis silvestris silvestris) from Germany. Int. J. Parasitol. Parasites Wildl. 2022, 19, 128–137. [Google Scholar] [CrossRef]
- Kegler, K.; Nufer, U.; Alic, A.; Posthaus, H.; Olias, P.; Basso, W. Fatal infection with emerging apicomplexan parasite Hepatozoon silvestris in a domestic cat. Parasites Vectors 2018, 11, 428. [Google Scholar] [CrossRef]
- Hodžić, A.; Alić, A.; Prašović, S.; Otranto, D.; Baneth, G.; Duscher, G.G. Hepatozoon silvestris sp. nov.: Morphological and molecular characterization of a new species of Hepatozoon (Adeleorina: Hepatozoidae) from the European wild cat (Felis silvestris silvestris). Parasitology 2017, 144, 650–661. [Google Scholar] [CrossRef]
- Diakou, A.; Dimzas, D.; Astaras, C.; Savvas, I.; Di Cesare, A.; Morelli, S.; Neofitos, Κ.; Migli, D.; Traversa, D. Clinical investigations and treatment outcome in a European wildcat (Felis silvestris silvestris) infected by cardio-pulmonary nematodes. Vet. Parasitol. RSR 2020, 19, 100357. [Google Scholar] [CrossRef]
- Grillini, M.; Simonato, G.; Tessarin, C.; Dotto, G.; Traversa, D.; Cassini, R.; Marchiori, E.; Frangipane di Regalbono, A. Cytauxzoon sp. and Hepatozoon spp. in Domestic Cats: A Preliminary Study in North-Eastern Italy. Pathogens 2021, 10, 1214. [Google Scholar] [CrossRef]
- Morelli, S.; Diakou, A.; Traversa, D.; Di Gennaro, E.; Simonato, G.; Colombo, M.; Dimzas, D.; Grillini, M.; Frangipane di Regalbono, A.; Beugnet, F.; et al. First record of Hepatozoon spp. in domestic cats in Greece. Ticks Tick-Borne Dis. 2021, 12, 101580. [Google Scholar] [CrossRef]
- Hornok, S.; Boldogh, S.A.; Takács, N.; Kontschán, J.; Szekeres, S.; Sós, E.; Sándor, A.D.; Wang, Y.; Tuska-Szalay, B. Molecular epidemiological study on ticks and tick-borne protozoan parasites (Apicomplexa: Cytauxzoon and Hepatozoon spp.) from wild cats (Felis silvestris), Mustelidae and red squirrels (Sciurus vulgaris) in central Europe, Hungary. Parasit. Vectors 2022, 15, 174. [Google Scholar] [CrossRef]
- Smith, T.G. The genus Hepatozoon (Apicomplexa: Adeleina). J. Parasitol. 1996, 82, 565–585. [Google Scholar]
- Baneth, G.; Sheiner, A.; Eyal, O.; Hahn, S.; Beaufils, J.P.; Anug, Y.; Talmi-Frank, D. Redescription of Hepatozoon felis (Apicomplexa: Hepatozoidae) based on phylogenetic analysis, tissue and blood form morphology, and possible transplacental transmission. Parasites Vectors 2013, 6, 102. [Google Scholar]
- Wang, J.L.; Li, T.T.; Liu, G.H.; Zhu, X.Q.; Yao, C. Two Tales of Cytauxzoon felis Infections in Domestic Cats. Clin. Microbiol. Rev. 2017, 30, 861–885. [Google Scholar] [CrossRef]
- Sherrill, M.K.; Cohn, L.A. Cytauxzoonosis: Diagnosis and treatment of an emerging disease. J. Feline Med. Surg. 2015, 17, 940–948. [Google Scholar] [CrossRef]
- Willi, B.; Meli, M.L.; Cafarelli, C.; Gilli, U.O.; Kipar, A.; Hubbuch, A.; Riond, B.; Howard, J.; Schaarschmidt, D.; Regli, W.; et al. Cytauxzoon europaeus infections in domestic cats in Switzerland and in European wildcats in France: A tale that started more than two decades ago. Parasites Vectors 2022, 15, 19. [Google Scholar] [CrossRef]
- Panait, L.C.; Mihalca, A.D.; Modrý, D.; Juránková, J.; Ionică, A.M.; Deak, G.; Gherman, C.M.; Heddergott, M.; Hodžić, A.; Veronesi, F.; et al. Three new species of Cytauxzoon in European wild felids. Vet. Parasitol. 2021, 290, 109344. [Google Scholar] [CrossRef]
- Gerichter, C.B. Studies on the nematodes parasitic in the lungs of Felidae in Palestine. Parasitology 1949, 39, 251–262. [Google Scholar] [CrossRef]
- Falsone, L.; Brianti, E.; Gaglio, G.; Napoli, E.; Anile, S.; Mallia, E.; Giannelli, A.; Poglayen, G.; Giannetto, S.; Otranto, D. The European wildcats (Felis silvestris silvestris) as reservoir hosts of Troglostrongylus brevior (Strongylida: Crenosomatidae) lungworms. Vet. Parasitol. 2014, 205, 193–198. [Google Scholar] [CrossRef]
- Deak, G.; Ionică, A.M.; Pop, R.A.; Mihalca, A.D.; Gherman, C.M. New insights into the distribution of cardio-pulmonary nematodes in road-killed wild felids from Romania. Parasit. Vectors 2022, 15, 153. [Google Scholar] [CrossRef]
- Alić, A.; Traversa, D.; Duscher, G.G.; Kadrić, M.; Di Cesare, A.; Hodžić, A. Troglostrongylus brevior in an Eurasian lynx (Lynx lynx) from Bosnia and Herzegovina. Parasit. Vectors 2015, 8, 653. [Google Scholar] [CrossRef]
- Brianti, E.; Gaglio, G.; Giannetto, S.; Annoscia, G.; Latrofa, M.S.; Dantas-Torres, F.; Traversa, D.; Otranto, D. Troglostrongylus brevior and Troglostrongylus subcrenatus (Strongylida: Crenosomatidae) as agents of broncho-pulmonary infestation in domestic cats. Parasit. Vectors 2012, 5, 178. [Google Scholar] [CrossRef]
- Morelli, S.; Diakou, A.; Colombo, M.; Di Cesare, A.; Barlaam, A.; Dimzas, D.; Traversa, D. Cat Respiratory Nematodes: Current Knowledge, Novel Data and Warranted Studies on Clinical Features, Treatment and Control. Pathogens 2021, 10, 454. [Google Scholar] [CrossRef]
- Diakou, A.; Psalla, D.; Migli, D.; Di Cesare, A.; Youlatos, D.; Marcer, F.; Traversa, D. First evidence of the European wildcat (Felis silvestris silvestris) as definitive host of Angiostrongylus chabaudi. Parasitol. Res. 2016, 115, 1235–1244. [Google Scholar] [CrossRef]
- Biocca, E. Angiostrongylus chabaudi n. sp. parassita del cuore e dei vasi polmonari del gatto selvatico (Felis silvestris). R Accad Naz Lincei 1957, 22, 526–532. [Google Scholar]
- Varcasia, A.; Tamponi, C.; Brianti, E.; Cabras, P.A.; Boi, R.; Pipia, A.P.; Giannelli, A.; Otranto, D.; Scala, A. Angiostrongylus chabaudi Biocca, 1957: A new parasite for domestic cats? Parasit. Vectors 2014, 7, 588. [Google Scholar] [CrossRef]
- Traversa, D.; Lepri, E.; Veronesi, F.; Paoletti, B.; Simonato, G.; Diaferia, M.; Di Cesare, A. Metastrongyloid infection by Aelurostrongylus abstrusus, Troglostrongylus brevior and Angiostrongylus chabaudi in a domestic cat. Int. J. Parasitol. 2015, 45, 685–690. [Google Scholar]
- Stevanović, O.; Diakou, A.; Morelli, S.; Paraš, S.; Trbojević, I.; Nedić, D.; Sladojević, Ž.; Kasagić, D.; Di Cesare, A. Severe verminous pneumonia caused by natural mixed infection with Aelurostrongylus abstrusus and Angiostrongylus chabaudi in a European wildcat from western Balkan area. Acta Parasitol. 2019, 64, 411–417. [Google Scholar]
- Giannelli, A.; Kirkova, Z.; Abramo, F.; Latrofa, M.S.; Campbell, B.; Zizzo, N.; Cantacessi, C.; Dantas-Torres, F.; Otranto, D. Angiostrongylus chabaudi in felids: New findings and a review of the literature. Vet. Parasitol. 2016, 228, 188–192. [Google Scholar] [CrossRef]
- Gherman, C.M.; Ionica, A.M.; D’Amico, G.; Otranto, D.; Mihalca, A.D. Angiostrongylus chabaudi (Biocca, 1957) in wildcat (Felis silvestris silvestris, S.) from Romania. Parasitol. Res. 2016, 115, 2511–2517. [Google Scholar] [CrossRef]
- Veronesi, F.; Traversa, D.; Lepri, E.; Morganti, G.; Vercillo, F.; Grelli, D.; Cassini, R.; Marangi, M.; Iorio, R.; Ragni, B.; et al. Occurrence of lungworms in European wildcats (Felis silvestris silvestris) of central Italy. J. Wildl. Dis. 2016, 52, 270–278. [Google Scholar] [CrossRef]
- Dimzas, D.; Morelli, S.; Traversa, D.; Di Cesare, A.; Van Bourgonie, Y.R.; Breugelmans, K.; Backeljau, T.; Di Regalbono, A.F.; Diakou, A. Intermediate gastropod hosts of major feline cardiopulmonary nematodes in an area of wildcat and domestic cat sympatry in Greece. Parasit. Vectors. 2020, 13, 1–12. [Google Scholar] [CrossRef]
- Dimzas, D.; Di Cesare, A.; Morelli, S.; Iorio, R.; Backeljau, T.; Vanderheyden Lombal, A.; De Meyer, M.; Meganck, K.; Smitz, N.; Kassari, N.; et al. Angiostrongylus chabaudi natural infection in wild caught gastropods. In Proceedings of the 7th European Dirofilaria and Angiostrongylus Days, Madrid, Spain, 23–24 September 2022. [Google Scholar]
- Di Cesare, A.; Morelli, S.; Colombo, M.; Simonato, G.; Veronesi, F.; Marcer, F.; Diakou, A.; D’Angelosante, R.; Pantchev, N.; Psaralexi, E.; et al. Is angiostrongylosis a realistic threat for domestic cats? Front. Veter. Sci. 2020, 7, 195. [Google Scholar] [CrossRef]
- Györke, A.; Dumitrache, M.O.; Kalmár, Z.; Pastiu, A.I.; Mircean, V. Molecular survey of metastrongyloid lungworms in domestic cats (Felis silvestris catus) from Romania: A retrospective study (2008–2011). Pathogens 2020, 9, 80. [Google Scholar]
- Junker, K.; Lane, E.P.; McRee, A.E.; Foggin, C.; van Dyk, D.S.; Mutafchiev, Y. Two new species of Cylicospirura vevers, 1922 (Nematoda: Spirocercidae) from carnivores in southern Africa, with validation of the related genera Gastronodus Singh, 1934 and Skrjabinocercina Matschulsky, 1952. Folia Parasitol. 2013, 60, 339–352. [Google Scholar]
- Segeritz, L.; Anders, O.; Middelhoff, T.L.; Winterfeld, D.T.; Maksimov, P.; Schares, G.; Conraths, F.J.; Taubert, A.; Hermosilla, C. New Insights into Gastrointestinal and Pulmonary Parasitofauna of Wild Eurasian lynx (Lynx lynx) in the Harz Mountains of Germany. Pathogens 2021, 10, 1650. [Google Scholar] [CrossRef]
- Yanchev, Y.; Genov, T. The helminth fauna of the wild cat (Felis silvestris) in Bulgaria. Khelmintologiya 1978, 6, 81–101. [Google Scholar]
- Ibba, F.; Lepri, E.; Veronesi, F.; Di Cesare, A.; Paltrinieri, S. Gastric cylicospirurosis in a domestic cat from Italy. J. Feline Med. Surg. 2014, 16, 522–526. [Google Scholar] [CrossRef]
- Crossland, N.A.; Hanks, C.R.; Ferguson, J.A.; Kent, M.L.; Sanders, J.L.; Del Piero, F. First report of Cylicospirura felineus in a feral domestic shorthair cat in North America. JFMS Open Rep. 2015, 1, 2055116915593964. [Google Scholar] [CrossRef]
- Eckert, J.; Gemmell, M.A.; Meslin, F.X.; Pawlowski, Z.; World Organisation for Animal Health; World Health Organization. WHO/OIE Manual on Echinococcosis in Humans and Animals: A Public Health Problem of Global Concern. 2021. Available online: https://apps.who.int/iris/handle/10665/42427 (accessed on 2 December 2022).
- Stubbe, M. Martes foina (Erxleben, 1777)—Haus-, Steinmarder. In Handbuch der Säugetiere; Stubbe, M., Krapp, F., Eds.; Aula Verlag: Wiesbaden, Germany, 1993; pp. 427–479. [Google Scholar]
- Lanszki, J.; Heltai, M. Feeding habits of sympatric mustelids in an agricultural area of Hungary. Acta Zool. Acad. Sci. Hung. 2011, 57, 291–304. [Google Scholar]
- Ionică, A.M.; Deak, G.; D’Amico, G.; Stan, G.F.; Chișamera, G.B.; Constantinescu, I.C.; Adam, C.; Lefkaditis, M.; Gherman, C.M.; Mihalca, A.D. Thelazia callipaeda in mustelids from Romania with the European badger, Meles meles, as a new host for this parasite. Parasit. Vectors. 2019, 12, 1–6. [Google Scholar]
- Ionică, A.M.; Deak, G.; Boncea, R.; Gherman, C.M.; and Mihalca, A.D. The European Badger as a New Host for Dirofilaria immitis and an Update on the Distribution of the Heartworm in Wild Carnivores from Romania. Pathogens 2022, 11, 420. [Google Scholar] [CrossRef]
- Hurníková, Z.; Kołodziej-Sobocińska, M.; Dvorožňáková, E.; Niemczynowicz, A.; Zalewski, A. An invasive species as an additional parasite reservoir: Trichinella in introduced American mink (Neovison vison). Vet. Parasitol. 2016, 231, 106–109. [Google Scholar] [CrossRef]
- Kranz, A.; Abramov, A.V.; Herrero, J.; Maran, T. Meles meles. IUCN Red List. Threat. Species 2016, e.T29673A45203002. Available online: https://doi.org/10.2305/IUCN.UK.2016-1.RLTS.T29673A45203002.en (accessed on 2 December 2022).
- Piza-Roca, C.; Haye, M.L.; Jongejans, E. Environmental drivers of the distribution and density of the European badger (Meles meles): A review. Lutra 2014, 57, 87–109. [Google Scholar]
- Do Linh San, E.; Ferrari, N.; Weber, J.M. Ecology of European badgers (meles meles) in rural areas of Western Switzerland. In Middle-Sized Carnivores in Agricultural Landscapes; Nova Science Publishers NY: New York, NY, USA, 2011; pp. 83–104. [Google Scholar]
- Hancox, M. Dental anomalies in the Eurasian badger. J. Zool. 1988, 216, 606–608. [Google Scholar] [CrossRef]
- Sidorchuk, N.; Maslov, M.; Rozhnov, V. Role of badger setts in life of other carnivores. Stud. Ecol. Et Bioethicae 2015, 13, 81–95. [Google Scholar] [CrossRef]
- Barlow, A.M.; Mullineaux, E.; Wood, R.; Taweenan, W.; Wastling, J.M. Giardiosis in Eurasian badgers (Meles meles). Vet. Rec. 2010, 167, 1017. [Google Scholar] [CrossRef]
- Maestrini, M.; Berrilli, F.; Di Rosso, A.; Coppola, F.; Guadano Procesi, I.; Mariacher, A.; Perrucci, S. Zoonotic Giardia duodenalis Genotypes and Other Gastrointestinal Parasites in a Badger Population Living in an Anthropized Area of Central Italy. Pathogens 2022, 11, 906. [Google Scholar] [CrossRef]
- Stojecki, K.; Sroka, J.; Cacciò, S.M.; Cencek, T.; Dutkiewicz, J.; Kusyk, P. Prevalence and molecular typing of Giardia duodenalis in wildlife from eastern Poland. Folia Parasitol. 2015, 62, 1. [Google Scholar] [CrossRef]
- Mateo, M.; de Mingo, M.H.; de Lucio, A.; Morales, L.; Balseiro, A.; Espí, A.; Carmena, D. Occurrence and molecular genotyping of Giardia duodenalis and Cryptosporidium spp. in wild mesocarnivores in Spain. Vet. Parasitol. 2017, 235, 86–93. [Google Scholar]
- Del Río, L.; Chitimia, L.; Cubas, A.; Victoriano, I.; De la Rúa, P.; Gerrikagoitia, X.; Berriatua, E. Evidence for widespread Leishmania infantum infection among wild carnivores in L. infantum periendemic northern Spain. Prev. Vet. Med. 2014, 113, 430–435. [Google Scholar]
- Risueño, J.; Ortuño, M.; Pérez-Cutillas, P.; Goyena, E.; Maia, C.; Cortes, S.; Berriatua, E. Epidemiological and genetic studies suggest a common Leishmania infantum transmission cycle in wildlife, dogs and humans associated to vector abundance in Southeast Spain. Vet. Parasitol. 2018, 259, 61–67. [Google Scholar] [CrossRef]
- Oleaga, A.; Zanet, S.; Espí, A.; de Macedo, M.R.P.; Gortázar, C.; Ferroglio, E. Leishmania in wolves in northern Spain: A spreading zoonosis evidenced by wildlife sanitary surveillance. Vet. Parasitol. 2018, 255, 26–31. [Google Scholar]
- Alcover, M.M.; Ribas, A.; Guillén, M.C.; Berenguer, D.; Tomás-Pérez, M.; Riera, C.; Fisa, R. Wild mammals as potential silent reservoirs of Leishmania infantum in a Mediterranean area. Prev. Vet. Med. 2020, 175, 104874. [Google Scholar] [CrossRef]
- Thompson, R.C.; Ash, A. Molecular epidemiology of Giardia and Cryptosporidium infections. Infect. Genet. Evol. 2016, 40, 315–323. [Google Scholar]
- Cacciò, S.M.; Putignani, L. Epidemiology of human Cryptosporidiosis. In Cryptosporidium Parasite and Disease; Cacciò, S.M., Widmer, G., Eds.; Springer: Vienna, Austria, 2014; pp. 43–79. [Google Scholar]
- McKerr, C.; Chalmers, R.M.; Elwin, K.; Ayres, H.; Vivancos, R.; O’Brien, S.J.; Christley, R.M. Cross-sectional household transmission study of Cryptosporidium shows that C. hominis infections are a key risk factor for spread. BMC Inf. Dis. 2022, 22, 1–13. [Google Scholar]
- Sturdee, A.P.; Chalmers, R.M.; Bull, S.A. Detection of Cryptosporidium oocysts in wild mammals of mainland Britain. Vet. Parasitol. 1999, 80, 273–280. [Google Scholar]
- Anwar, A.; Knaggs, J.; Service, K.M.; McLaren, G.W.; Riordan, P.; Newman, C.; Delahay, R.J.; Cheesman, C.; Macdonald, D.W. Antibodies to Toxoplasma gondii in Eurasian badgers. J. Wild. Dis. 2006, 42, 179–181. [Google Scholar] [CrossRef]
- Millán, J.; Candela, M.G.; Palomares, F.; Cubero, M.J.; Rodríguez, A.; Barral, M.; de la Fuente, J.; Almería, S.; León-Vizcaíno, L. Disease threats to the endangered Iberian lynx (Lynx pardinus). Vet. J. 2009, 182, 114–124. [Google Scholar] [CrossRef]
- Lopes, A.P.; Sargo, R.; Rodrigues, M.; Cardoso, L. High seroprevalence of antibodies to Toxoplasma gondii in wild animals from Portugal. Parasitol. Res. 2011, 108, 1163–1169. [Google Scholar] [CrossRef]
- Burrells, A.; Bartley, P.M.; Zimmer, I.A.; Roy, S.; Kitchener, A.C.; Meredith, A.; Wright, S.E.; Innes, E.A.; Katzer, F. Evidence of the three main clonal Toxoplasma gondii lineages from wild mammalian carnivores in the UK. Parasitolology 2013, 140, 1768–1776. [Google Scholar]
- Turcekova, L.; Hurníková, Z.; Spisak, F.; Miterpáková, M.; Chovancová, B. Toxoplasma gondii in protected wildlife in the Tatra National Park (TANAP), Slovakia. Ann. Agric. Environ. Med. 2014, 21, 235–238. [Google Scholar]
- Sroka, J.; Karamon, J.; Wójcik-Fatla, A.; Dutkiewicz, J.; Bilska-Zajac, E.; Zajac, V.; Piotrowska, W.; Cencek, T. Toxoplasma gondii infection in selected species of free-living animals in Poland. Ann. Agric. Environ. Med. 2019, 26, 656–660. [Google Scholar] [CrossRef]
- Kornacka, A.; Cybulska, A.; Bień, J.; Goździk, K.; Moskwa, B. The usefulness of direct agglutination test, enzyme-linked immunosorbent assay and polymerase chain reaction for the detection of Toxoplasma gondii in wild animals. Vet. Parasitol. 2016, 228, 85–89. [Google Scholar]
- Karakavuk, M.; Aldemir, D.; Atalay Şahar, E.; Can, H.; Özdemir, H.G.; Değirmenci Döşkaya, A.; Gürüz, A.Y.; Döşkaya, M. Detection of Toxoplasma gondii in a Eurasian badger (Meles meles) Living in Wildlife Areas of Izmir, Turkey. Turkiye Parazitol Derg. 2018, 42, 237–239. [Google Scholar] [CrossRef]
- Máca, O. Molecular identification of Sarcocystis lutrae in the European otter (Lutra lutra) and the European badger (Meles meles) from the Czech Republic. Parasitol. Res. 2018, 117, 943–945. [Google Scholar] [CrossRef]
- Marucci, G.; Tonanzi, D.; Interisano, M.; Vatta, P.; Galati, F.; La Rosa, G. The International Trichinella Reference Centre data-base. Report on thirty-three years of activity and future perspectives. Food Waterborne Parasitol. 2022, 27, e00156. [Google Scholar] [CrossRef]
- Varodi, E.I.; Malega, A.M.; Kuzmin, Y.I.; Kornyushin, V.V. Helminths of wild predatory mammals of Ukraine. Nematodes. Vestn. Zool. 2017, 5, 187. [Google Scholar] [CrossRef]
- Järvis, T.; Miller, I.; Pozio, E. Epidemiological studies on animal and human trichinellosis in Estonia. Parasite 2001, 8, S86–S87. [Google Scholar]
- Kärssin, A.; Häkkinen, L.; Vilem, A.; Jokelainen, P.; Lassen, B. Trichinella spp. in wild boars (Sus scrofa), brown bears (Ursus arctos), Eurasian lynxes (Lynx lynx) and badgers (Meles meles) in Estonia, 2007–2014. Animals 2021, 11, 183. [Google Scholar]
- Deksne, G.; Segliņa, Z.; Jahundoviča, I.; Esīte, Z.; Bakasejevs, E.; Bagrade, G.; Kirjušina, M. High prevalence of Trichinella spp. in sylvatic carnivore mammals of Latvia. Vet. Par. 2016, 231, 118–123. [Google Scholar]
- Lee, H.C.; Kim, J.S.; Oh, H.Y.; Kim, J.H.; Kim, H.G.; Lee, M.S.; Kim, W.J.; Kim, H.T. A case of trichinosis caused by eating a wild badger. Korean J. Med. 1999, 1999, 134–138. [Google Scholar]
- Sohn, W.M.; Kim, H.M.; Chung, D.I.; Yee, S.T. The first human case of Trichinella spiralis infection in Korea. Korean J. Parasitol. 2000, 38, 111. [Google Scholar] [CrossRef]
- Giménez-Anaya, A.; Herrero, J.; Rosell, C.; Couto, S.; García-Serrano, A. Food habits of wild boars (Sus scrofa) in a Mediterranean coastal wetland. Wetlands 2008, 28, 197–203. [Google Scholar] [CrossRef]
- .Jędrzejewski, W.; Schmidt, K.; Miłkowski, L.; Jędrzejewska, B.; Okarma, H. Foraging by lynx and its role in ungulate mortality: The local (Białowieża Forest) and the Palaearctic viewpoints. Acta Theriol. 1993, 38, 385–403. [Google Scholar] [CrossRef]
- Hennig, R. Schwarzwild—Biologie, Verhalten, Hege und Jagd; BLV Verlagsgesellschaft: München, Germnay, 1998. [Google Scholar]
- Torres, J.; Miquel, J.; Motjé, M. Helminth parasites of the Eurasian badger (Meles meles L.) in Spain: A biogeographic approach. Parasitol. Res. 2001, 87, 259–263. [Google Scholar]
- Millán, J.; Sevilla, I.; Gerrikagoitia, X.; García-Pérez, A.L.; Barral, M. Helminth parasites of the Eurasian badger (Meles meles L.) in the Basque Country (Spain). Eur. J. Wildl. Res. 2004, 50, 37–40. [Google Scholar]
- Davidson, R.K.; Handeland, K.; Gjerde, B. The first report of Aelurostrongylus falciformis in Norwegian badgers (Meles meles). Acta Vet. Scand. 2006, 48, 1–4. [Google Scholar]
- Magi, M.; Guardone, L.; Dell’Omodarme, M.; Prati, M.; Mignone, W.; Torracca, B.; Monni, G.; Macchioni, F. Angiostrongylus vasorum in red foxes (Vulpes vulpes) and badgers (Meles meles) from Central and Northern Italy. Hystrix 2009, 20, 4442. [Google Scholar]
- Nagy, E.; Benedek, I.; Zsolnai, A.; Halász, T.; Csivincsik, Á.; Ács, V.; Nagy, G.; Tari, T. Habitat characteristics as potential drivers of the Angiostrongylus daskalovi infection in European badger (Meles meles) populations. Pathogens 2021, 10, 715. [Google Scholar]
- Tikhonov, A.; Cavallini, P.; Maran, T.; Krantz, A.; Herrero, J.; Giannatos, G.; Stubbe, M.; Libois, R.; Fernandes, M.; Yonzon, P.; et al. Martes foina (Mediterranean assessment). IUCN RedList Threat. Species 2010, e.T29672A9521091. Available online: https://www.iucnredlist.org/species/29672/9521091 (accessed on 27 December 2022).
- Virgós, E.; Zalewski, A.; Rosalino, L.M.; Mergey, M.; Aubrey, K.B.; Zielinski, W.J.; Buskirk, S.W. Habitat ecology of Martes species in Europe. In Biology and Conservation of Martens, Sables, and Fishers: A New Synthesis; Cornel University Press: New York, NY, USA, 2012; pp. 255–266. [Google Scholar]
- Abramov, A.V.; Kranz, A.; Herrero, J.; Choudhury, A.; Maran, T. Martes foina. IUCN Red List. Threat. Species 2016, e. T29672A45202514. Available online: https://www.researchgate.net/profile/Alexei-Abramov/publication/311304303_Martes_foina/links/58411cb008ae8e63e6213a1c/Martes-foina.pdf (accessed on 20 December 2022).
- Schnur, L.F. On the clinical manifestations and parasites of old world leishmaniases and Leishmania tropica causing visceral leishmaniasis. In Leishmaniasis; Springer: Boston, MA, USA, 1989; pp. 939–943. [Google Scholar]
- Muñoz-Madrid, R.; Belinchón-Lorenzo, S.; Iniesta, V.; Fernández-Cotrina, J.; Parejo, J.C.; Serrano, F.J.; Monroy, I.; Baz, V.; Gómez-Luque, A.; Gómez-Nieto, L.C. First detection of Leishmania infantum kinetoplast DNA in hair of wild mammals: Application of qPCR method to determine potential parasite reservoirs. Acta Trop. 2013, 128, 706–709. [Google Scholar]
- Hejlíček, K.; Literák, I.; Nezval, J. Toxoplasmosis in wild mammals from the Czech Republic. J. Wildl. Dis. 1997, 33, 480–485. [Google Scholar]
- Hůrková, L.; Modrý, D. PCR detection of Neospora. caninum, Toxoplasma gondii and Encephalitozoon cuniculi in brains of wild carnivores. Vet. Parasitol. 2006, 137, 150–154. [Google Scholar]
- Deksne, G.; Segliņa, Z.; Ligere, B.; Kirjušina, M. The Pine marten (Martes martes) and the Stone marten (Martes foina) as possible wild reservoirs of Toxoplasma gondii in the Baltic States. Vet. Parasitol. Reg. Stud. Rep. 2017, 9, 70–74. [Google Scholar]
- Baghli, A.; Engel, E.; Verhagen, R. Feeding habits and trophic niche overlap of two sympatric Mustelidae, the polecat Mustela putorius and the beech marten Martes foina. Z. Für Jagdwiss. 2002, 48, 217–225. [Google Scholar]
- do Vale, B.; Lopes, A.P.; da Conceição Fontes, M.; Silvestre, M.; Cardoso, L.; Coelho, A.C. Systematic review on infection and disease caused by Thelazia callipaeda in Europe: 2001–2020. Revue systématique de l’infection et de la maladie provoquées par Thelazia callipaeda en Europe (2001–2020). Parasite 2020, 27, 52. [Google Scholar] [CrossRef]
- Seixas, F.; Travassos, P.; Coutinho, T.; Lopes, A.P.; Latrofa, M.S.; dos Anjos Pires, M.; Otranto, D. The eyeworm Thelazia callipaeda in Portugal: Current status of infection in pets and wild mammals and case report in a beech marten (Martes foina). Vet. Parasitol. 2018, 252, 163–166. [Google Scholar]
- Lemming, L.; Jørgensen, A.C.; Nielsen, L.B.; Nielsen, S.T.; Mejer, H.; Chriél, M.; Petersen, H.H. Cardiopulmonary nematodes of wild carnivores from Denmark: Do they serve as reservoir hosts for infections in domestic animals? IJP-PW 2020, 13, 90–97. [Google Scholar]
- Remonti, L.; Balestrieri, A.; Domenis, L.; Banchi, C.; Lo Valvo, T.; Robetto, S.; Orusa, R. Red fox (Vulpes vulpes) cannibalistic behaviour and the prevalence of Trichinella britovi in NW Italian Alps. Parasitol. Res. 2005, 97, 431–435. [Google Scholar]
- Hurníková, Z.; Chovancová, B.; Bartková, D.; Dubinský, P. The role of wild carnivores in the maintenance of trichinellosis in the Tatras National Park, Slovakia. Helminthologia 2007, 44, 18–20. [Google Scholar] [CrossRef]
- Klun, I.; Ćosić, N.; Ćirović, D.; Vasilev, D.; Teodorović, V.; Djurković-Djaković, O. Trichinella spp. in wild mesocarnivores in an endemic setting. Acta Vet. Hung. 2019, 67, 34–39. [Google Scholar]
- Oltean, M.; Kalmár, Z.; Kiss, B.J.; Marinov, M.; Vasile, A.; Sándor, A.D.; Domşa, C.; Gherman, C.M.; Boireau, P.; Cozma, V.; et al. European muste-lids occupying pristine wetlands in the Danube Delta are infected with Trichinella likely derived from domesticated swine. J. Wildl. Dis. 2014, 50, 972–975. [Google Scholar]
- Piekarska, J.; Gorczykowski, M.; Kicia, M.; Pacon, J.; Soltysiak, Z.; Merta, D. Trichinella spp. (Nematoda) in free-living carnivores (Mammalia: Carnivora) from the Lower Silesia (Poland). Ann. Parasitol. 2016, 62 (Suppl.), 64. [Google Scholar]
- Herrero, J.; Kranz, A.; Skumatov, D.; Abramov, A.V.; Maran, T.; Monakhov, V.G. Martes martes. IUCN Red List Threat. Species 2016, e. T12848A45199169. Available online: https://www.researchgate.net/profile/Vladimir-Monakhov/publication/306105785_Martes_martes_Pine_Marten/links/57b1b98508ae95f9d8f4bbda/Martes-martes-Pine-Marten.pdf (accessed on 27 December 2022).
- Rossi, L.; Pozio, E.; Mignone, W.; Ercolini, C.; Dini, V. Epidemiology of sylvatic trichinellosis in north-western Italy. Rev. Sci. Et Tech. (Int. Off. Epizoot.) 1992, 11, 1039–1046. [Google Scholar]
- Pozio, E.; La Rosa, G.; Serrano, F.J.; Barrat, J.; Rossi, L. Environmental and human influence on the ecology of Trichinella spiralis and Trichinella britovi in Western Europe. Parasitology 1996, 113, 527–533. [Google Scholar]
- Senutaitė, J.; Grikienienė, J. Prevalence of Trichinella in muscles of some domestic and wild mammals in Lithuania and their impact on the organism. Acta Zool. Litu. 2001, 11, 395–404. [Google Scholar]
- Airas, N.; Saari, S.; Mikkonen, T.; Virtala, A.M.; Pellikka, J.; Oksanen, A.; Isomursu, M.; Kilpelä, S.S.; Lim, C.W.; Sukura, A. Sylvatic Trichinella spp. infection in Finland. J. Parasitol. 2010, 96, 67–76. [Google Scholar]
- Bakasejevs, E.; Daukšte, A.; Zolovs, M.; Zdanovska, A. Investigation of Trichinella in wildlife in Latgale region (Latvia). Acta Biol. Daugavp. 2012, 12, 1–5. [Google Scholar]
- Moskwa, B.; Goździk, K.; Bień, J.; Borecka, A.; Gawor, J.; Cabaj, W. First report of Trichinella pseudospiralis in Poland, in red foxes (Vulpes vulpes). Acta Parasitol. 2013, 58, 149–154. [Google Scholar] [CrossRef]
- Bērziņa, Z.; Stankevičiūtė, J.; Šidlauskas, G.; Bakasejevs, E.; Zdankovska, A.; Gackis, M. Trichinella sp. infection in Martens (Martes martes, Martes foina) in Latvia and Lithuania (Kaunas region). Rural Dev. 2013, 2013, 34. [Google Scholar]
- Badagliacca, P.; Di Sabatino, D.; Salucci, S.; Romeo, G.; Cipriani, M.; Sulli, N.; Morelli, D. The role of the wolf in endemic sylvatic Trichinella britovi infection in the Abruzzi region of Central Italy. Vet. Parasitol. 2016, 231, 124–127. [Google Scholar] [CrossRef]
- Cybulska, A.; Kornacka, A.; Skopek, R.; Moskwa, B. Trichinella britovi infection and muscle distribution in free-living martens (Martes spp.) from the Głęboki Bród Forest District, Poland. IJP-PAW 2020, 12, 176–180. [Google Scholar] [CrossRef]
- Maran, T.; Skumatov, D.; Gomez, A.; Põdra, M.; Abramov, A.V.; Dinets, V. Mustela lutreola. IUCN Red List. Threat. Species 2016. Available online: https://www.researchgate.net/profile/Alexei-Abramov/publication/307907972_Mustela_lutreola/links/5c17a24fa6fdcc494ffb2862/Mustela-lutreola.pdf (accessed on 2 December 2022).
- Santos, M.J.; Matos, H.M.; Baltazar, C.; Grilo, C.; Santos-Reis, M. Is Polecat (Mustela putorius). affected by ‘mediterraneity’? Mamm. Biol. 2009, 74, 448–455. [Google Scholar] [CrossRef]
- Shimalov, V.; Shimalov, V. Helminth fauna of the European polecat (Mustela putorius Linnaeus, 1758) in Belorussian Polesie. Parasitol. Res. 2002, 88, 259–260. [Google Scholar] [CrossRef]
- Boros, Z.; Ionică, A.M.; Deak, G.; Mihalca, A.D.; Chișamera, G.; Constantinescu, I.C.; Adam, C.; Gherman, C.M.; Cozma, V. Trichinella spp. Infection in European Polecats (Mustela Putorius Linnaeus, 1758) from Romania. Helminthologia 2021, 58, 323–327. [Google Scholar] [CrossRef]
- Simpson, V. Angiostrongylus vasorum infection in a stoat. Vet. Rec. 2010, 166, 182. [Google Scholar] [CrossRef]
- Loy, A.; Kranz, A.; Oleynikov, A.; Roos, A.; Savage, M.; Duplaix, N. Lutra lutra (amended versionof 2021 assessment). IUCN RedList. Threat. Species 2022, e.T12419A218069689. Available online: https://dx.doi.org/10.2305/IUCN.UK.2022-2.RLTS.T12419A218069689.en (accessed on 27 December 2022).
- El Alami, A.; Fattah, A.; Chait, A. A Survey of the Eurasian Otter Lutra lutra and Human-Otter Interaction in the Middle Oum Er Rbia River, Morocco. IUCN Otter Spec. Group Bull. 2020, 37, 219–231. [Google Scholar]
- Takeuchi-Storm, N.; Al-Sabi, M.N.S.; Chriel, M.; Enemark, H.L. Systematic examination of the cardiopulmonary, urogenital, muscular and gastrointestinal parasites of the Eurasian otters (Lutra lutra) in Denmark, a protected species recovering from a dramatic decline. Parasitol. Int. 2021, 84, 102418. [Google Scholar] [CrossRef]
- Méndez-Hermida, F.; Gómez-Couso, H.; Romero-Suances, R.; Ares-Mazás, E. Cryptosporidium and Giardia in wild otters (Lutra lutra). Vet. Parasitol. 2007, 144, 153–156. [Google Scholar] [CrossRef]
- Smallbone, W.A.; Chadwick, E.A.; Francis, J.; Guy, E.; Perkins, S.E.; Sherrard-Smith, E.; Cable, J. East-West Divide: Temperature and land cover drive spatial variation of Toxoplasma gondii infection in Eurasian otters (Lutra lutra) from England and Wales. Parasitology 2017, 144, 1433–1440. [Google Scholar] [CrossRef]
- Chadwick, E.A.; Cable, J.; Chinchen, A.; Francis, J.; Guy, E.; Kean, E.F.; Paul, S.C.; Perkins, S.E.; Sherrard-Smith, E.; Wilkinson, C.; et al. Seroprevalence of Toxoplasma gondii in the Eurasian otter (Lutra lutra) in England and Wales. Parasites Vectors 2013, 6, 75. [Google Scholar] [CrossRef]
- Torres, J.; Feliu, C.; Fernández-Morán, J.; Ruíz-Olmo, J.; Rosoux, R.; Santos-Reis, M.; Miquel, J.; Fons, R. Helminth parasites of the Eurasian otter Lutra lutra in southwest Europe. J. Helminthol. 2004, 78, 353–359. [Google Scholar] [CrossRef]
- Fusillo, R.; Romanucci, M.; Marcelli, M.; Massimini, M.; Della Salda, L. Health and Mortality Monitoring in Threatened Mammals: A First Post Mortem Study of Otters (Lutra lutra L.) in Italy. Animals 2022, 12, 609. [Google Scholar] [CrossRef]
- Hegyeli, Z.; Kecskés, A. The occurrence of wild-living American Mink Neovison vison in Transylvania, Romania. Small Carniv. Conserv. 2014, 51, 23–28. [Google Scholar]
- Bueno, F. Alimentacion del vison Americana (Mustela vison, Schreber) en el Rio Voltoya (Avila, Cuenca del Duero). Doñana Acta Vertebr. 1994, 215, 13. [Google Scholar]
- Mezzetto, D.; Dartora, F.; Mori, E. Feeding plasticity and temporal behaviour of the alien American mink in Europe. Acta Oecol. 2021, 110, 103700. [Google Scholar]
- Harrington, L.A.; Gelling, M.; Simpson, V.; Harrington, A.; Macdonald, D.W. Notes on the health status of free-living, non-native American mink, Neovison vison, in southern England. Eur. J. Wildl. Res. 2012, 58, 875–880. [Google Scholar]
- Ribas, M.P.; Almería, S.; Fernández-Aguilar, X.; De Pedro, G.; Lizarraga, P.; Alarcia-Alejos, O.; Molina-López, R.; Obón, E.; Gholipour, H.; Temiño, C.; et al. Tracking Toxoplasma gondii in freshwater ecosystems: Interaction with the invasive American mink (Neovison vison) in Spain. Parasitol. Res. 2018, 117, 2275–2281. [Google Scholar]
- Sengupta, M.E.; Pagh, S.; Stensgaard, A.S.; Chriel, M.; Petersen, H.H. Prevalence of Toxoplasma gondii and Cryptosporidium in feral and farmed American mink (Neovison vison) in Denmark. Acta Parasitol. 2021, 66, 1285–1291. [Google Scholar]
- Nugaraitė, D.; Mažeika, V.; Paulauskas, A. Helminths of mustelids (Mustelidae) in Lithuania. Biologija 2014, 60, 117–125. [Google Scholar] [CrossRef]
- Nugaraitė, D.; Mažeika, V.; Paulauskas, A. Helminths of mustelids with overlapping ecological niches: Eurasian otter (Linnaeus, 1758), American mink Schreber, 1777, and European polecat Linnaeus, 1758. Helminthologia 2019, 56, 66–74. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).