Adherence to Anti-Malarial Treatment in Malaria Endemic Areas of Bangladesh
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting and Population
2.2. Sample Size
2.3. Adherence Definition
2.4. Sampling Strategy
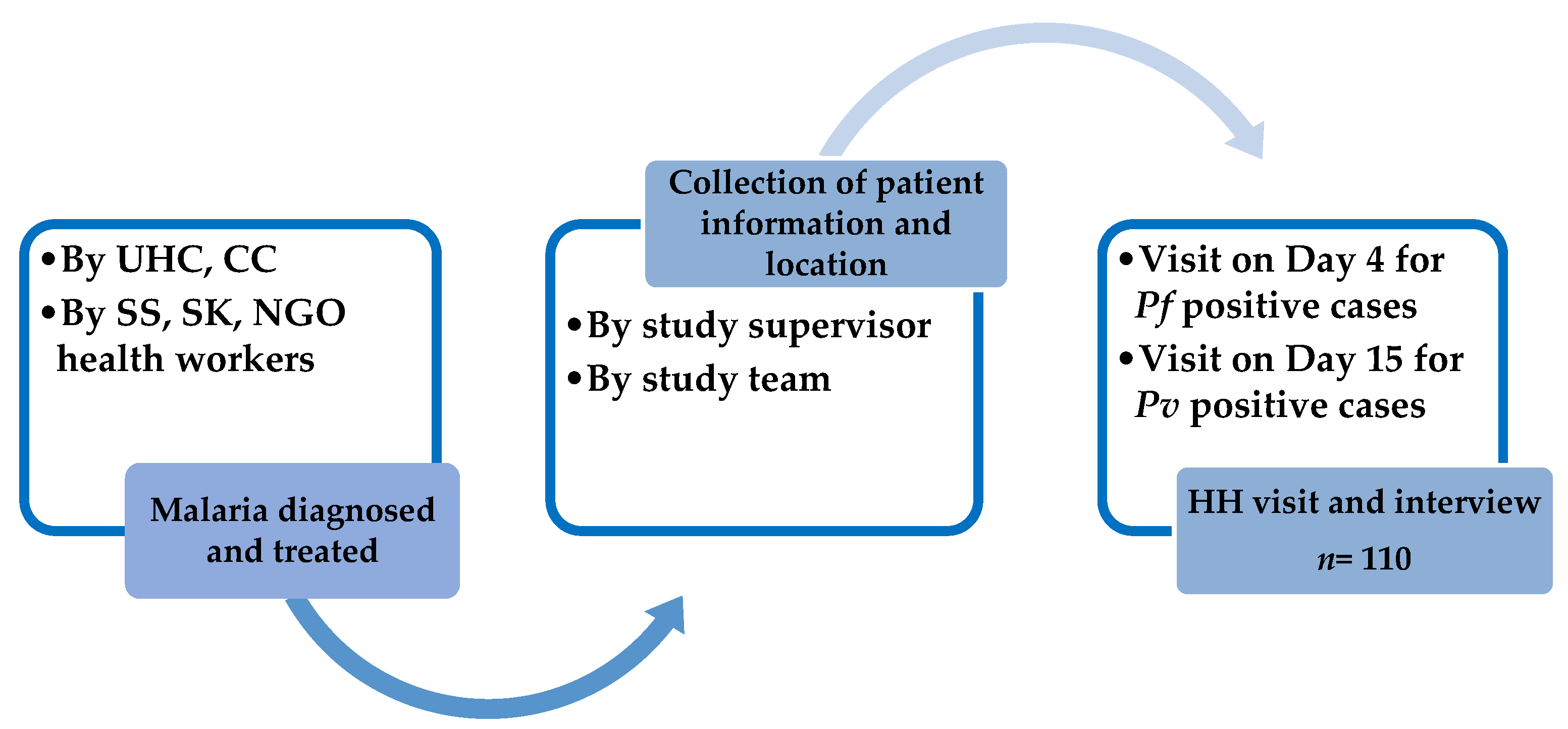
2.5. Data Collection and Analysis Procedures
2.6. Ethical Approval and Informed Consent
3. Results
3.1. Demographic Characteristics
3.2. Level of Adherence
3.3. Reasons for Nonadherence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rougeron, V.; Elguero, E.; Arnathau, C.; Hidalgo, B.A.; Durand, P.; Houze, S.; Berry, A.; Zakeri, S.; Haque, R.; Alam, M.S.; et al. Human Plasmodium vivax diversity, population structure and evolutionary origin. PLoS Neglected Trop. Dis. 2020, 14, e0008072. [Google Scholar] [CrossRef] [PubMed]
- Sato, S. Plasmodium—A brief introduction to the parasites causing human malaria and their basic biology. J. Physiol. Anthr. 2021, 40, 1. [Google Scholar] [CrossRef] [PubMed]
- Sazed, S.A.; Kibria, M.G.; Alam, M.S. An Optimized Real-Time qPCR Method for the Effective Detection of Human Malaria Infections. Diagnostics 2021, 11, 736. [Google Scholar] [CrossRef] [PubMed]
- Matthews, H.; Duffy, C.W.; Merrick, C.J. Checks and balances? DNA replication and the cell cycle in Plasmodium. Parasites Vectors 2018, 11, 216. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.-H.; Moss, E.L.; Park, D.J.; Ndiaye, D.; Mboup, S.; Volkman, S.K.; Sabeti, P.C.; Wirth, D.F.; Neafsey, D.E.; Hartl, D.L. Malaria life cycle intensifies both natural selection and random genetic drift. Proc. Natl. Acad. Sci. USA 2013, 110, 20129–20134. [Google Scholar] [CrossRef] [PubMed]
- Directorate General of Health Services; Government of the People’s Republic of Bangladesh. Health Bulletin 2020; Government of the People’s Republic of Bangladesh: Dhaka, Bangladesh, 2022. [Google Scholar]
- Haque, U.; Ahmed, S.M.; Hossain, S.; Huda, M.; Hossain, A.; Alam, M.S.; Mondal, D.; Khan, W.A.; Khalequzzaman, M.; Haque, R. Malaria prevalence in endemic districts of Bangladesh. PLoS ONE 2009, 4, e6737. [Google Scholar] [CrossRef]
- Alam, M.S.; Chakma, S.; Khan, A.W.; Glass, G.E.; Mohon, A.N.; Elahi, R.; Norris, L.C.; Podder, M.P.; Ahmed, S.; Haque, R.; et al. Diversity of anopheline species and their Plasmodium infection status in rural Bandarban, Bangladesh. Parasites Vectors 2012, 5, 150. [Google Scholar] [CrossRef]
- Rahman, W.; Chotivanich, K.; Silamut, K.; Tanomsing, N.; Hossain, A.; Faiz, M.A.; Dondorp, A.M.; Maude, R.J. Plasmodium malariae in Bangladesh. Trans. R. Soc. Trop. Med. Hyg. 2010, 104, 78–80. [Google Scholar] [CrossRef]
- Starzengruber, P.; Fuehrer, H.-P.; Ley, B.; Thriemer, K.; Swoboda, P.; Habler, V.E.; Jung, M.; Graninger, W.; A Khan, W.; Haque, R.; et al. High prevalence of asymptomatic malaria in south-eastern Bangladesh. Malar. J. 2014, 13, 16. [Google Scholar] [CrossRef]
- Saeheng, T.; Na-Bangchang, K. Prediction of improved antimalarial chemotherapy of artesunate-mefloquine in combination with mefloquine sensitive and resistant Plasmodium falciparum malaria. PLoS ONE 2023, 18, e0282099. [Google Scholar] [CrossRef]
- Sinha, I.; Abu Sayeed, A.; Uddin, D.; Wesolowski, A.; Zaman, S.I.; Faiz, M.A.; Ghose, A.; Rahman, M.R.; Islam, A.; Karim, M.J.; et al. Mapping the travel patterns of people with malaria in Bangladesh. BMC Med. 2020, 18, 45. [Google Scholar] [CrossRef] [PubMed]
- National Malaria Control Program. Malaria Treatment Regimen 2016; Ministry of Health and Family Welfare, Government of the People’s Republic of Bangladesh: Dhaka, Bangladesh, 2016. [Google Scholar]
- Noedl, H.; Se, Y.; Sriwichai, S.; Schaecher, K.; Teja-Isavadharm, P.; Smith, B.; Rutvisuttinunt, W.; Bethell, D.; Surasri, S.; Fukuda, M.M.; et al. Artemisinin Resistance in Cambodia: A Clinical Trial Designed to Address an Emerging Problem in Southeast Asia. Clin. Infect. Dis. 2010, 51, e82–e89. [Google Scholar] [CrossRef] [PubMed]
- Lek, D.; Rachmat, A.; Harrison, D.; Chin, G.; Chaoratanakawee, S.; Saunders, D.; Menard, D.; Rogers, W.O. Efficacy of three anti-malarial regimens for uncomplicated Plasmodium falciparum malaria in Cambodia, 2009–2011: A randomized controlled trial and brief review. Malar. J. 2022, 21, 259. [Google Scholar] [CrossRef] [PubMed]
- Imwong, M.; Dhorda, M.; Tun, K.M.; Thu, A.M.; Phyo, A.P.; Proux, S.; Suwannasin, K.; Kunasol, C.; Srisutham, S.; Duanguppama, J.; et al. Molecular epidemiology of resistance to antimalarial drugs in the Greater Mekong subregion: An observational study. Lancet Infect. Dis. 2020, 20, 1470–1480. [Google Scholar] [CrossRef] [PubMed]
- Khamsiriwatchara, A.; Sudathip, P.; Sawang, S.; Vijakadge, S.; Potithavoranan, T.; Sangvichean, A.; Satimai, W.; Delacollette, C.; Singhasivanon, P.; Lawpoolsri, S.; et al. Artemisinin resistance containment project in Thailand. (I): Implementation of electronic-based malaria information system for early case detection and individual case management in provinces along the Thai-Cambodian border. Malar. J. 2012, 11, 247. [Google Scholar] [CrossRef] [PubMed]
- Na-Bangchang, K.; Ruengweerayut, R.; Mahamad, P.; Ruengweerayut, K.; Chaijaroenkul, W. Declining in efficacy of a three-day combination regimen of mefloquine-artesunate in a multi-drug resistance area along the Thai-Myanmar border. Malar. J. 2010, 9, 273. [Google Scholar] [CrossRef]
- Rovira-Vallbona, E.; Kattenberg, J.H.; Van Hong, N.; Guetens, P.; Imamura, H.; Monsieurs, P.; Chiheb, D.; Erhart, A.; Phuc, B.Q.; Xa, N.X.; et al. Molecular surveillance of Plasmodium falciparum drug-resistance markers in Vietnam using multiplex amplicon sequencing (2000–2016). Sci. Rep. 2023, 13, 13948. [Google Scholar] [CrossRef]
- Commons, R.J.; A Simpson, J.; Thriemer, K.; Hossain, M.S.; Douglas, N.M.; Humphreys, G.S.; Sibley, C.H.; Guerin, P.J.; Price, R.N. Risk of Plasmodium vivax parasitaemia after Plasmodium falciparum infection: A systematic review and meta-analysis. Lancet Infect. Dis. 2019, 19, 91–101. [Google Scholar] [CrossRef]
- Douglas, N.M.; Lampah, D.A.; Kenangalem, E.; Simpson, J.A.; Poespoprodjo, J.R.; Sugiarto, P.; Anstey, N.M.; Price, R.N. Major Burden of Severe Anemia from Non-Falciparum Malaria Species in Southern Papua: A Hospital-Based Surveillance Study. PLoS Med. 2013, 10, e1001575. [Google Scholar] [CrossRef]
- Hossain, M.S.; Commons, R.J.; Douglas, N.M.; Thriemer, K.; Alemayehu, B.H.; Amaratunga, C.; Anvikar, A.R.; Ashley, E.A.; Asih, P.B.S.; Carrara, V.I.; et al. The risk of Plasmodium vivax parasitaemia after P. falciparum malaria: An individual patient data meta-analysis from the WorldWide Antimalarial Resistance Network. PLoS Med. 2020, 17, e1003393. [Google Scholar] [CrossRef]
- Bruxvoort, K.; Goodman, C.; Kachur, S.P.; Schellenberg, D. How Patients Take Malaria Treatment: A Systematic Review of the Literature on Adherence to Antimalarial Drugs. PLoS ONE 2014, 9, e84555. [Google Scholar] [CrossRef] [PubMed]
- Yeung, S.; White, N.J. How do patients use antimalarial drugs? A review of the evidence. Trop. Med. Int. Health 2005, 10, 121–138. [Google Scholar] [CrossRef] [PubMed]
- Rathmes, G.; Rumisha, S.F.; Lucas, T.C.D.; Twohig, K.A.; Python, A.; Nguyen, M.; Nandi, A.K.; Keddie, S.H.; Collins, E.L.; Rozier, J.A.; et al. Global estimation of anti-malarial drug effectiveness for the treatment of uncomplicated Plasmodium falciparum malaria 1991–2019. Malar. J. 2020, 19, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Ribera, J.M.; Hausmann-Muela, S.; Gryseels, C.; Grietens, K.P. Re-imagining adherence to treatment from the “other side”: Local interpretations of adverse anti-malarial drug reactions in the Peruvian Amazon. Malar. J. 2016, 15, 1–7. [Google Scholar] [CrossRef]
- Duarte, E.C.; Gyorkos, T.W. Self-reported compliance with last malaria treatment and occurrence of malaria during follow-up in a Brazilian Amazon population. Trop. Med. Int. Health 2003, 8, 518–524. [Google Scholar] [CrossRef] [PubMed]
- A Pereira, E.; Ishikawa, E.A.; Fontes, C.J. Adherence to Plasmodium vivax malaria treatment in the Brazilian Amazon Region. Malar. J. 2011, 10, 355. [Google Scholar] [CrossRef] [PubMed]
- Khanam, F.; Hossain, M.B.; Chowdhury, T.R.; Rahman, M.S.; Kabir, M.; Naher, S.; Islam, M.A.; Rahman, M. Exploring the gap between coverage, access, and utilization of long-lasting insecticide-treated nets (LLINs) among the households of malaria endemic districts in Bangladesh. Malar. J. 2018, 17, 455. [Google Scholar] [CrossRef]
- Rahman, M.; Dondorp, A.M.; Day, N.P.; Lindegardh, N.; Imwong, M.; Faiz, M.; Bangali, A.M.; Kamal, A.M.; Karim, J.; Kaewkungwal, J.; et al. Adherence and efficacy of supervised versus non-supervised treatment with artemether/lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria in Bangladesh: A randomised controlled trial. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 861–867. [Google Scholar] [CrossRef]
- Haldar, K.; Alam, M.S.; Koepfli, C.; Lobo, N.F.; Phru, C.S.; Islam, M.N.; Faiz, A.; Khan, W.A.; Haque, R. Bangladesh in the era of malaria elimination. Trends Parasitol. 2023, 39, 760–773. [Google Scholar] [CrossRef]
- Charan, J.; Biswas, T. How to calculate sample size for different study designs in medical research? Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef]
- Fogg, C.; Musabe, J.; Namiiro, P.; Kiguli, J.; Checchi, F.; Biraro, S.; Piola, P.; Bajunirwe, F.; Guthmann, J.-P.; Kyomugisha, A. Adherence to a six-dose regimen of artemether-lumefantrine for treatment of uncomplicated Plasmodium falciparum malaria in uganda. Am. J. Trop. Med. Hyg. 2004, 71, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Gerstl, S.; Namagana, A.; Palacios, L.; Mweshi, F.; Aprile, S.; Lima, A. High adherence to malaria treatment: Promising results of an adherence study in South Kivu, Democratic Republic of the Congo. Malar. J. 2015, 14, 414. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines for Malaria, 3 June 2022; World Health Organization: Geneve, Switzerland, 2022. [Google Scholar]
- Simba, D.O.; Kakoko, D.; Tomson, G.; Premji, Z.; Petzold, M.; Mahindi, M.; Gustafsson, L.L. Adherence to artemether/lumefantrine treatment in children under real-life situations in rural Tanzania. Trans. R. Soc. Trop. Med. Hyg. 2012, 106, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Tun, Z.W.; Lin, Z.; Wai, K.; Lin, K.; Oung, M.T.; Kyaw, T.T. Adherence to the recommended regimen of artemether-lumefantrine for treatment of uncomplicated falciparum malaria in Myanmar. Myanmar Health Sci. Res. J. 2012, 24, 51–55. [Google Scholar]
- Reilley, B.; Abeyasinghe, R.; Pakianathar, M.V. Barriers to prompt and effective treatment of malaria in northern Sri Lanka. Trop. Med. Int. Health 2002, 7, 744–749. [Google Scholar] [CrossRef] [PubMed]
- Rishikesh, K.; Saravu, K. Primaquine treatment and relapse in Plasmodium vivax malaria. Pathog. Glob. Health 2016, 110, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Thriemer, K.; Ley, B.; von Seidlein, L. Towards the elimination of Plasmodium vivax malaria: Implementing the radical cure. PLoS Med. 2021, 18, e1003494. [Google Scholar] [CrossRef] [PubMed]
- Kathirvel, S.; Tripathy, J.P.; Tun, Z.M.; Patro, B.K.; Singh, T.; Bhalla, A.; Devnani, M.; Wilkinson, E. Physicians’ compliance with the National Drug Policy on Malaria in a tertiary teaching hospital, India, from 2010 to 2015: A mixed method study. Trans. R. Soc. Trop. Med. Hyg. 2017, 111, 62–70. [Google Scholar] [CrossRef]
- Solari-Soto, L.; Mendoza-Requena, D.; Llanos-Cuentas, A. Ensayo clínico del tratamiento de la malaria vivax con esquema acortado de primaquina comparado con el esquema tradicional. Rev. Soc. Peru. Med. Interna 2002, 15, 197–199. [Google Scholar]
- Onyango, O.E.; Ayodo, G.; A Watsierah, C.; Were, T.; Okumu, W.; Anyona, S.B.; Raballah, E.; Okoth, J.M.; Gumo, S.; Orinda, O.G.; et al. Factors associated with non-adherence to Artemisinin-based combination therapy (ACT) to malaria in a rural population from holoendemic region of western Kenya. BMC Infect. Dis. 2012, 12, 143. [Google Scholar] [CrossRef]
- Banek, K.; Lalani, M.; Staedke, S.G.; Chandramohan, D. Adherence to artemisinin-based combination therapy for the treatment of malaria: A systematic review of the evidence. Malar. J. 2014, 13, 7. [Google Scholar] [CrossRef] [PubMed]
- Goller, J.L.; Ringwald, P.; Jolley, D.; Biggs, B.-A. Regional differences in the response of plasmodium vivax malaria to primaquine as anti-relapse therapy. Am. J. Trop. Med. Hyg. 2007, 76, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Laver, S.M.; Wetzels, J.; Behrens, R.H. Knowledge of malaria, risk perception, and compliance with prophylaxis and personal and environmental preventive measures in travelers exiting Zimbabwe from Harare and Victoria Falls International airport. J. Travel Med. 2006, 8, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Krause, G.; Sauerborn, R. Comprehensive community effectiveness of health care. A study of malaria treatment in children and adults in rural Burkina Faso. Ann. Trop. Paediatr. 2000, 20, 273–282. [Google Scholar] [CrossRef]
- Gebrekidan, M.G.; Gebremedhin, G.B.; Gebregiorgis, Y.S.; Gezehegn, A.A.; Weldearegay, K.T. Artemether–lumefantrin treatment adherence among uncomplicated Plasmodium falciparum malaria patients, visiting public health facilities in AsgedeTsimbla district, Tigray, Ethiopia: A cross-sectional study. Antimicrob. Resist. Infect. Control 2020, 9, 184. [Google Scholar] [CrossRef]
- Mace, K.E.; Mwandama, D.; Jafali, J.; Luka, M.; Filler, S.J.; Sande, J.; Ali, D.; Kachur, S.P.; Mathanga, D.P.; Skarbinski, J. Adherence to Treatment with Artemether-Lumefantrine for Uncomplicated Malaria in Rural Malawi. Clin. Infect. Dis. 2011, 53, 772–779. [Google Scholar] [CrossRef]
| Characteristics | Pf Patient n (%) | Pv Patient n (%) | Total n (%) |
|---|---|---|---|
| Upazila | |||
| Alikadam | 36 (46.7) | 15 (45.5) | 51 (46.3) |
| Lama | 30 (39.0) | 10 (30.3) | 40 (36.4) |
| Thanchi | 5 (6.5) | 3 (9.1) | 8 (7.3) |
| Chakaria | 6 (7.8) | 5 (15.1) | 11 (10.0) |
| Sex | |||
| Male | 56 (72.7) | 28 (84.9) | 84 (76.4) |
| Female | 21 (27.3) | 5 (15.1) | 26 (23.6) |
| Age, year | |||
| 11–17 Years | 30 (39.0) | 7 (21.2) | 37 (33.6) |
| 18 Years and above | 47 (61.0) | 26 (78.8) | 73 (66.4) |
| Median (IQR) | 24 (14–38) | 22 (18–28) | 22 (15–36) |
| Ethnicity | |||
| Mro | 37 (48.0) | 5 (15.1) | 42 (38.2) |
| Tripura | 15 (19.5) | 5 (15.1) | 20 (18.2) |
| Chakma | 0 (0.0) | 2 (6.1) | 2 (1.8) |
| Marma | 6 (7.8) | 2 (6.1) | 8 (7.3) |
| Tangchangya | 3 (3.9) | 2 (6.1) | 5 (4.6) |
| Bengali | 16 (20.8) | 17 (51.5) | 33 (30.0) |
| Education | |||
| No formal education | 34 (44.2) | 8 (24.2) | 42 (38.2) |
| Primary | 25 (32.5) | 9 (27.3) | 34 (30.9) |
| Secondary | 15 (19.5) | 11 (33.3) | 26 (23.6) |
| College/Graduate | 3 (3.9) | 5 (15.2) | 8 (7.3) |
| Occupation | |||
| Farming/Jhum Cultivation | 34 (44.2) | 8 (24.2) | 42 (38.2) |
| Own business | 3 (3.9) | 3 (9.1) | 6 (5.4) |
| Student | 22 (28.6) | 11 (33.3) | 33 (30.0) |
| Daily labour | 7 (9.1) | 6 (18.2) | 13 (11.8) |
| Housewife | 4 (5.2) | 0 (0.0) | 4 (3.6) |
| Other | 7 (9.1) | 5 (15.2) | 12 (10.9) |
| Family Size (members) | |||
| ≤4 | 16 (20.8) | 14 (42.4) | 30 (27.3) |
| ≥5 | 61 (79.2) | 19 (57.6) | 80 (72.7) |
| Respondent | |||
| Patient Self | 50 (64.9) | 25 (75.8) | 75 (68.2) |
| Family member/Responsible for the child | 27 (35.1) | 8 (24.2) | 35 (31.8) |
| Adherence Level | Nonadherent (NA) | Probably Adherent (PA) | Total | p-Value |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Plasmodium falciparum | 3 (3.9) | 74 (96.1) | 77 | 0.05 |
| Plasmodium vivax | 5 (15.1) | 28 (84.9) | 33 | |
| Total | 8 (7.3) | 102 (92.7) | 110 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hossain, M.S.; Matin, M.A.; Ferdous, N.-E.N.; Hasan, A.; Sazed, S.A.; Neogi, A.K.; Chakma, S.; Islam, M.A.; Khan, A.A.; Haque, M.E.; et al. Adherence to Anti-Malarial Treatment in Malaria Endemic Areas of Bangladesh. Pathogens 2023, 12, 1392. https://doi.org/10.3390/pathogens12121392
Hossain MS, Matin MA, Ferdous N-EN, Hasan A, Sazed SA, Neogi AK, Chakma S, Islam MA, Khan AA, Haque ME, et al. Adherence to Anti-Malarial Treatment in Malaria Endemic Areas of Bangladesh. Pathogens. 2023; 12(12):1392. https://doi.org/10.3390/pathogens12121392
Chicago/Turabian StyleHossain, Mohammad Sharif, Mohammad Abdul Matin, Nur-E Naznin Ferdous, Anamul Hasan, Saiful Arefeen Sazed, Amit Kumer Neogi, Sumit Chakma, Md. Atiqul Islam, Afsana Alamgir Khan, Md. Ekramul Haque, and et al. 2023. "Adherence to Anti-Malarial Treatment in Malaria Endemic Areas of Bangladesh" Pathogens 12, no. 12: 1392. https://doi.org/10.3390/pathogens12121392
APA StyleHossain, M. S., Matin, M. A., Ferdous, N.-E. N., Hasan, A., Sazed, S. A., Neogi, A. K., Chakma, S., Islam, M. A., Khan, A. A., Haque, M. E., Islam, S., Islam, M. N., Khan, W. A., Islam, M. A., Haque, R., & Alam, M. S. (2023). Adherence to Anti-Malarial Treatment in Malaria Endemic Areas of Bangladesh. Pathogens, 12(12), 1392. https://doi.org/10.3390/pathogens12121392







