First Molecular Detection and Genotype Identification of Toxoplasma gondii in Chickens from Farmers’ Markets in Fujian Province, Southeastern China
Abstract
:1. Introduction
2. Materials and Methods
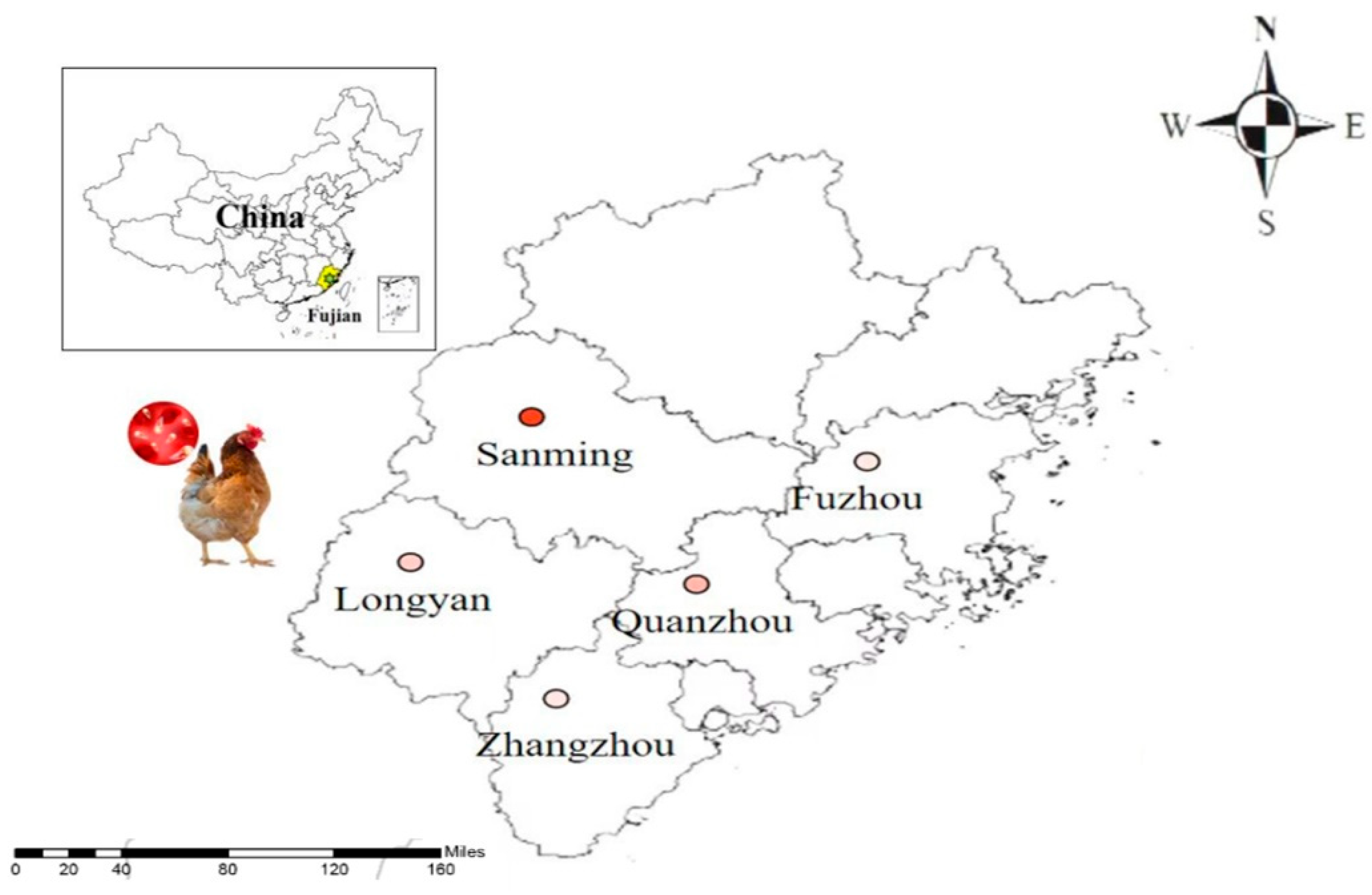
2.1. Geographical Features of Fujian
2.2. Sample Collection
2.3. Extraction and Detection of Tissue DNA
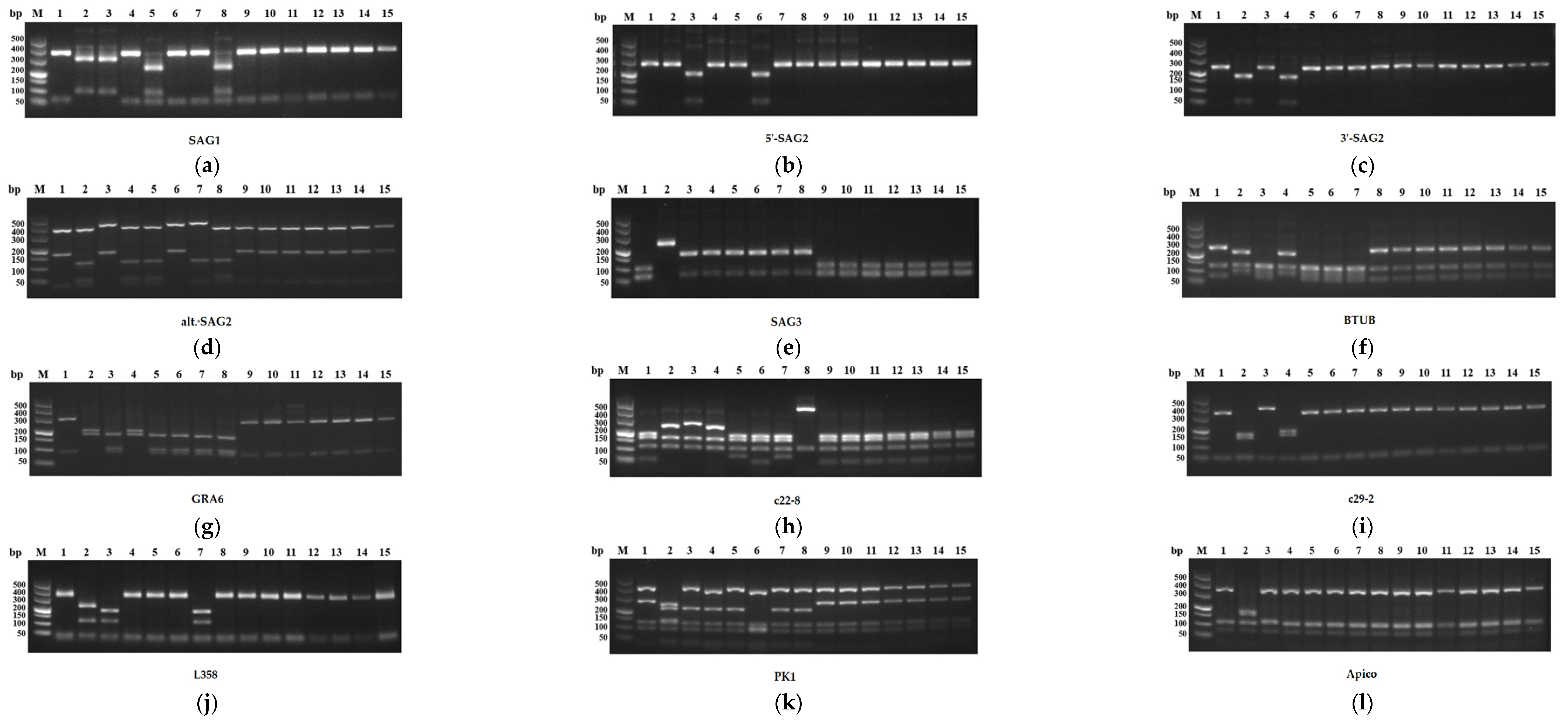
2.4. Genetic Characterization of T. gondii
2.5. Data and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Montoya, J.G.; Liesenfeld, O. Toxoplasmosis. Lancet 2004, 363, 1965–1976. [Google Scholar] [CrossRef]
- Chikweto, A.; Sharma, R.N.; Tiwari, K.P.; Verma, S.K.; Calero-Bernal, R.; Jiang, T.; Su, C.; Kwok, O.C.; Dubey, J.P. Isolation and RFLP Genotyping of Toxoplasma gondii in Free-Range Chickens (Gallus domesticus) in Grenada, West Indies, Revealed Widespread and Dominance of Clonal Type III Parasites. J. Parasitol. 2017, 103, 52–55. [Google Scholar] [CrossRef]
- Dasa, T.T.; Geta, T.G.; Yalew, A.Z.; Abebe, R.M.; Kele, H.U. Toxoplasmosis infection among pregnant women in Africa: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0254209. [Google Scholar] [CrossRef]
- Holland, G.N. Ocular toxoplasmosis: A global reassessment. Part I: Epidemiology and course of disease. Am. J. Ophthalmol. 2003, 136, 973–988. [Google Scholar] [CrossRef]
- Jiang, T.; Shwab, E.K.; Martin, R.M.; Gerhold, R.W.; Rosenthal, B.M.; Dubey, J.P.; Su, C. A partition of Toxoplasma gondii genotypes across spatial gradients and among host species, and decreased parasite diversity towards areas of human settlement in North America. Int. J. Parasitol. 2018, 48, 611–619. [Google Scholar] [CrossRef]
- Jones, J.L.; Dubey, J.P. Foodborne Toxoplasmosis. Clin. Infect. Dis. 2012, 55, 845–851. [Google Scholar] [CrossRef]
- Dubey, J.P. Toxoplasma gondii infections in chickens (Gallus domesticus): Prevalence, clinical disease, diagnosis and public health significance. Zoonoses Public Health 2010, 57, 60–73. [Google Scholar] [CrossRef]
- Goodwin, M.A.; Dubey, J.P.; Hatkin, J. Toxoplasma gondii peripheral neuritis in chickens. J. Vet. Diagn. Investig. 1994, 6, 382–385. [Google Scholar] [CrossRef]
- Must, K.; Hytönen, M.K.; Orro, T.; Lohi, H.; Jokelainen, P. Toxoplasma gondii seroprevalence varies by cat breed. PLoS ONE 2017, 12, e0184659. [Google Scholar] [CrossRef]
- Rodrigues, F.T.; Moreira, F.A.; Coutinho, T.; Dubey, J.P.; Cardoso, L.; Lopes, A.P. Antibodies to Toxoplasma gondii in slaughtered free-range and broiler chickens. Vet. Parasitol. 2019, 271, 51–53. [Google Scholar] [CrossRef]
- Almeria, S.; Dubey, J.P. Foodborne transmission of Toxoplasma gondii infection in the last decade. An overview. Res. Vet. Sci. 2021, 135, 371–385. [Google Scholar] [CrossRef]
- Smith, N.C.; Goulart, C.; Hayward, J.A.; Kupz, A.; Miller, C.M.; van Dooren, G.G. Control of human toxoplasmosis. Int. J. Parasitol. 2021, 51, 95–121. [Google Scholar] [CrossRef]
- Maani, S.; Rezanezhad, H.; Solhjoo, K.; Kalantari, M.; Erfanian, S. Genetic characterization of Toxoplasma gondii isolates from human spontaneous aborted fetuses in Jahrom, southern Iran. Microb. Pathog. 2021, 161, 105217. [Google Scholar] [CrossRef]
- Ivović, V.; Vujanić, M.; Živković, T.; Klun, I.; Djurković-Djaković, O. Molecular detection and genotyping of Toxoplasma gondii from clinical samples. In Toxoplasmosis: Recent Advances; InTech: Rijeka, Croatia, 2012; pp. 1–18. [Google Scholar]
- Dubey, J.P.; Pena, H.F.J.; Cerqueira-Cézar, C.K.; Murata, F.H.A.; Kwok, O.C.H.; Yang, Y.R.; Gennari, S.M.; Su, C. Epidemiologic significance of Toxoplasma gondii infections in chickens (Gallus domesticus): The past decade. Parasitology 2020, 147, 1263–1289. [Google Scholar] [CrossRef]
- Wu, Z.H.; Zhuo, B.M.; Qiu, H.H.; Ma, M.; Chen, H.Y.; Zhong, H. Investigation on seroprevalence of Toxoplasma gondii infections among neonates in Fujian Province. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi 2020, 33, 71–73. (In Chinese) [Google Scholar]
- Su, C.; Shwab, E.K.; Zhou, P.; Zhu, X.Q.; Dubey, J.P. Moving towards an integrated approach to molecular detection and identification of Toxoplasma gondii. Parasitology 2010, 137, 1–11. [Google Scholar] [CrossRef]
- Nie, L.B.; Gong, Q.L.; Wang, Q.; Zhang, R.; Shi, J.F.; Yang, Y.; Li, J.M.; Zhu, X.Q.; Shi, K.; Du, R. Prevalence of Toxoplasma gondii infection in chickens in China during 1993–2021: A systematic review and meta-analysis. Parasitol. Res. 2022, 121, 287–301. [Google Scholar] [CrossRef]
- Wang, M.; Ye, Q.; Zhang, N.Z.; Zhang, D.L. Seroprevalence of Toxoplasma gondii infection in food-producing animals in northwest China. Chin. J. Zoonoses 2016, 32, 608–612. (In Chinese) [Google Scholar]
- Chen, X.; Sun, P.; Chen, J.; Tan, Q.; Li, J.; Liu, X.; Xiao, Q.; Li, H.; Zhao, X.; Zhao, N.; et al. Epidemiological investigation and reinfection evaluation of Toxoplasma gondii in chickens in Shandong Province, China. Exp. Parasitol. 2022, 238, 108276. [Google Scholar] [CrossRef]
- Rajendran, C.; Keerthana, C.M.; Anilakumar, K.R.; Satbige, A.S.; Gopal, S. Development of B1 Nested PCR for Assessing the Prevalence of Zoonotic Protozoan Disease Agent Toxoplasma gondii among Food Animals from Karnataka State, Southern India. J. Microbiol. Lab. Sci. 2018, 1, 101. [Google Scholar]
- Mahami-Oskouei, M.; Morad, M.; Fallah, E.; Hamidi, F.; Asl Rahnamaye Akbari, N. Molecular Detection and Genotyping of Toxoplasma gondii in Chicken, Beef, and Lamb Meat Consumed in Northwestern Iran. Iran. J. Parasitol. 2017, 12, 38–45. [Google Scholar] [PubMed]
- Gonçalves, I.N.; Uzêda, R.S.; Lacerda, G.A.; Moreira, R.R.; Araújo, F.R.; Oliveira, R.H.; Corbellini, L.G.; Gondim, L.F. Molecular frequency and isolation of cyst-forming coccidia from free ranging chickens in Bahia State, Brazil. Vet. Parasitol. 2012, 190, 74–79. [Google Scholar] [CrossRef] [PubMed]
- El-Massry, A.; Mahdy, O.A.; El-Ghaysh, A.; Dubey, J.P. Prevalence of Toxoplasma gondii antibodies in sera of turkeys, chickens, and ducks from Egypt. J. Parasitol. 2000, 86, 627–628. [Google Scholar] [CrossRef] [PubMed]
- Mose, J.M.; Kagira, J.M.; Karanja, S.M.; Ngotho, M.; Kamau, D.M.; Njuguna, A.N.; Maina, N.W. Detection of Natural Toxoplasma gondii Infection in Chicken in Thika Region of Kenya Using Nested Polymerase Chain Reaction. BioMed Res. Int. 2016, 2016, 7589278. [Google Scholar] [CrossRef]
- Sun, H.C.; Fu, Y.; Yuan, X.F.; Li, J.X.; Xu, L.H.; Zhang, J.N.; Yu, B.; Huang, J.; Qi, M.; Shi, T.Y. Molecular Detection and Genotyping of Toxoplasma gondii from Pigs for Human Consumption in Zhejiang and Jiangsu Provinces, Eastern China. Foodborne Pathog. Dis. 2022, 19, 686–692. [Google Scholar] [CrossRef] [PubMed]
- Dumètre, A.; Dardé, M.L. How to detect Toxoplasma gondii oocysts in environmental samples? FEMS Microbiol. Rev. 2003, 27, 651–661. [Google Scholar] [CrossRef]
- Ruiz, A.; Frenkel, J.K. Intermediate and transport hosts of Toxoplasma gondii in Costa Rica. Am. J. Trop. Med. Hyg. 1980, 29, 1161–1166. [Google Scholar] [CrossRef]
- Khan, M.B.; Khan, S.; Rafiq, K.; Khan, S.N.; Attaullah, S.; Ali, I. Molecular identification of Toxoplasma gondii in domesticated and broiler chickens (Gallus domesticus) that possibly augment the pool of human toxoplasmosis. PLoS ONE 2020, 15, e0232026. [Google Scholar] [CrossRef]
- Zrelli, S.; Amairia, S.; Jebali, M.; Gharbi, M. Molecular detection of Toxoplasma gondii in Tunisian free-range chicken meat and their offal. Parasitol. Res. 2022, 121, 3561–3567. [Google Scholar] [CrossRef]
- Pan, M.; Lyu, C.; Zhao, J.; Shen, B. Sixty Years (1957–2017) of Research on Toxoplasmosis in China-An Overview. Front. Microbiol. 2017, 8, 1825. [Google Scholar] [CrossRef]
- Zhou, P.; Zhang, H.; Lin, R.Q.; Zhang, D.L.; Song, H.Q.; Su, C.; Zhu, X.Q. Genetic characterization of Toxoplasma gondii isolates from China. Parasitol. Int. 2009, 58, 193–195. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.X.; Lou, Z.Z.; Huang, S.Y.; Zhou, D.H.; Jia, W.Z.; Su, C.; Zhu, X.Q. Genetic characterization of Toxoplasma gondii from Qinghai vole, Plateau pika and Tibetan ground-tit on the Qinghai-Tibet Plateau, China. Parasites Vectors 2013, 6, 291. [Google Scholar] [CrossRef] [PubMed]
- Nie, D.P.; Jia, Y.X.; Chen, L.J.; You, Y.X.; Li, W.; Shen, L.J. Genotypes of Toxoplasma gondii isolates from HIV positive patients in Yunnan Province. Chin. J. Parasitol. Parasit. Dis. 2013, 31, 410–411. (In Chinese) [Google Scholar]
- Wang, L.; Chen, H.; Liu, D.; Huo, X.; Gao, J.; Song, X.; Xu, X.; Huang, K.; Liu, W.; Wang, Y.; et al. Genotypes and mouse virulence of Toxoplasma gondii isolates from animals and humans in China. PLoS ONE 2013, 8, e53483. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.M.; Huang, S.Y.; Miao, Q.; Jiang, H.H.; Yang, J.F.; Su, C.; Zhu, X.Q.; Zou, F.C. Genetic characterization of Toxoplasma gondii from cats in Yunnan Province, Southwestern China. Parasites Vectors 2014, 7, 178. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Nie, H.; Zhang, L.X.; Wang, H.Y.; Yin, C.C.; Su, C.; Zhu, X.Q.; Zhao, J.L. Genetic characterization of Toxoplasma gondii isolates from pigs in China. J. Parasitol. 2010, 96, 1027–1029. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.H.; Qin, S.Y.; Wang, W.; He, B.; Hu, T.S.; Wu, J.M.; Fan, Q.S.; Tu, C.C.; Liu, Q.; Zhu, X.Q. Prevalence and genetic characterization of Toxoplasma gondii infection in bats in southern China. Vet. Parasitol. 2014, 203, 318–321. [Google Scholar] [CrossRef]
- Miao, Q.; Huang, S.Y.; Qin, S.Y.; Yu, X.; Yang, Y.; Yang, J.F.; Zhu, X.Q.; Zou, F.C. Genetic characterization of Toxoplasma gondii in Yunnan black goats (Capra hircus) in southwest China by PCR-RFLP. Parasites Vectors 2015, 8, 57. [Google Scholar] [CrossRef]
- Zhang, X.X.; Huang, S.Y.; Zhang, Y.G.; Zhang, Y.; Zhu, X.Q.; Liu, Q. First report of genotyping of Toxoplasma gondii in free-living Microtus fortis in Northeastern China. J. Parasitol. 2014, 100, 692–694. [Google Scholar] [CrossRef]
- Huang, S.Y.; Cong, W.; Zhou, P.; Zhou, D.H.; Wu, S.M.; Xu, M.J.; Zou, F.C.; Song, H.Q.; Zhu, X.Q. First report of genotyping of Toxoplasma gondii isolates from wild birds in China. J. Parasitol. 2012, 98, 681–682. [Google Scholar] [CrossRef]
- Dubey, J.P.; Navarro, I.T.; Graham, D.H.; Dahl, E.; Freire, R.L.; Prudencio, L.B.; Sreekumar, C.; Vianna, M.C.; Lehmann, T. Characterization of Toxoplasma gondii isolates from free range chickens from Paraná, Brazil. Vet. Parasitol. 2003, 117, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Dubey, J.P.; Gomez-Marin, J.E.; Bedoya, A.; Lora, F.; Vianna, M.C.; Hill, D.; Kwok, O.C.; Shen, S.K.; Marcet, P.L.; Lehmann, T. Genetic and biologic characteristics of Toxoplasma gondii isolates in free-range chickens from Colombia, South America. Vet. Parasitol. 2005, 134, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Aspinall, T.V.; Marlee, D.; Hyde, J.E.; Sims, P.F. Prevalence of Toxoplasma gondii in commercial meat products as monitored by polymerase chain reaction—Food for thought? Int. J. Parasitol. 2002, 32, 1193–1199. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.V.D.; Mendona, A.D.O.; Pezerico, S.B.; Domingues, P.F.; Langoni, H. Genotyping of Toxoplasma gondii strains detected in pork sausage. Parasitol. Latinoam. 2005, 60, 65–68. [Google Scholar]
- Fallah, E.; Hajizadeh, M.; Farajnia, S.; Khanmahammadi, M. SAG2 locus genotyping of Toxoplasma gondii in meat products of East Azerbaijan Province, North West of Iran During 2010–2011. Afr. J. Biotechnol. 2011, 10, 13631–13635. [Google Scholar]
| Areas | No. Tested | No. Positive | Infection Rate |
|---|---|---|---|
| Zhangzhou | 182 | 2 | 1.1% |
| Sanming | 95 | 16 | 16.8% |
| Quanzhou | 100 | 8 | 8.0% |
| Fuzhou | 100 | 1 | 1.0% |
| Longyan | 100 | 5 | 5.0% |
| Total | 577 | 32 | 5.5% |
| Areas | Postive/Tissue | Tissue Type | |||
|---|---|---|---|---|---|
| Heart | Liver | Lung | Muscle | ||
| Zhangzhou | 2 (2 × 4) | 2/2 | 0/2 | 1/2 | 0/2 |
| Sanming | 16 (16 × 4) | 4/16 | 6/16 | 11/16 | 0/16 |
| Quanzhou | 8 (8 × 4) | 2/8 | 3/8 | 5/8 | 3/8 |
| Fuzhou | 1 (1 × 4) | 0/1 | 0/1 | 1/1 | 0/1 |
| Longyan | 5 (5 × 4) | 3/5 | 0/5 | 4/5 | 0/5 |
| Total | 32 (32 × 4) | 11/32 (34.4%) | 9/32 (28.1%) | 22/32 (68.8%) | 3/32 (9.4%) |
| Strain Designation | Host | Area | SAG1 | 5′-SAG2 | 3′-SAG2 | alt. SAG2 | SAG3 | BTUB | GRA6 | c22-8 | c29-2 | L358 | PK1 | Apico | Genotypes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GT1 | Goat | United States | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Reference, Type Ⅰ, ToxoDB #10 |
| PGT | Sheep | United States | II/III | II | II | II | II | II | II | II | II | II | II | II | Reference, Type II, ToxoDB #1 |
| CTG | Cat | United States | II/III | III | III | III | III | III | III | III | III | III | III | III | Reference, Type III, ToxoDB #2 |
| TgCgCa1 | Cougar | Canada | Ⅰ | II | II | II | III | II | II | II | u-1 | Ⅰ | u-2 | Ⅰ | Reference, ToxoDB #66 |
| MAS | Human | France | u-1 | Ⅰ | Ⅰ | II | III | III | III | u-1 | Ⅰ | Ⅰ | III | Ⅰ | Reference, ToxoDB #17 |
| TgCatBr5 | Cat | United States | Ⅰ | III | III | III | III | III | III | Ⅰ | Ⅰ | Ⅰ | u-1 | Ⅰ | Reference, ToxoDB #19 |
| TgCatBr64 | Cat | Brazil | Ⅰ | Ⅰ | Ⅰ | u-1 | III | III | III | u-1 | Ⅰ | III | III | Ⅰ | Reference, ToxoDB #111 |
| TgRsCr1 | Toucan | Costa Rica | u-1 | Ⅰ | Ⅰ | II | III | Ⅰ | III | u-2 | Ⅰ | Ⅰ | III | Ⅰ | Reference, ToxoDB #52 |
| ZZC18 (lung) | Chicken | Fujian, China | I | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | ToxoDB #10 |
| ZZC19 (heart) | Chicken | Fujian, China | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | ToxoDB #10 |
| SMC20 (lung) | Chicken | Fujian, China | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | ToxoDB #10 |
| SMC22 (lung) | Chicken | Fujian, China | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | ToxoDB #10 |
| SMC30 (lung) | Chicken | Fujian, China | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | ToxoDB #10 |
| SMC31 (liver) | Chicken | Fujian, China | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | ToxoDB #10 |
| QZC68 (lung) | Chicken | Fujian, China | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | Ⅰ | ToxoDB #10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chu, M.-J.; Huang, L.-Y.; Miao, W.-Y.; Song, Y.-F.; Lin, Y.-S.; Li, S.-A.; Zhou, D.-H. First Molecular Detection and Genotype Identification of Toxoplasma gondii in Chickens from Farmers’ Markets in Fujian Province, Southeastern China. Pathogens 2023, 12, 1243. https://doi.org/10.3390/pathogens12101243
Chu M-J, Huang L-Y, Miao W-Y, Song Y-F, Lin Y-S, Li S-A, Zhou D-H. First Molecular Detection and Genotype Identification of Toxoplasma gondii in Chickens from Farmers’ Markets in Fujian Province, Southeastern China. Pathogens. 2023; 12(10):1243. https://doi.org/10.3390/pathogens12101243
Chicago/Turabian StyleChu, Meng-Jie, Li-Yuan Huang, Wen-Yuan Miao, Ya-Fei Song, Ying-Sheng Lin, Si-Ang Li, and Dong-Hui Zhou. 2023. "First Molecular Detection and Genotype Identification of Toxoplasma gondii in Chickens from Farmers’ Markets in Fujian Province, Southeastern China" Pathogens 12, no. 10: 1243. https://doi.org/10.3390/pathogens12101243
APA StyleChu, M.-J., Huang, L.-Y., Miao, W.-Y., Song, Y.-F., Lin, Y.-S., Li, S.-A., & Zhou, D.-H. (2023). First Molecular Detection and Genotype Identification of Toxoplasma gondii in Chickens from Farmers’ Markets in Fujian Province, Southeastern China. Pathogens, 12(10), 1243. https://doi.org/10.3390/pathogens12101243






