Inferred Causal Mechanisms of Persistent FMDV Infection in Cattle from Differential Gene Expression in the Nasopharyngeal Mucosa
Abstract
1. Introduction
2. Results
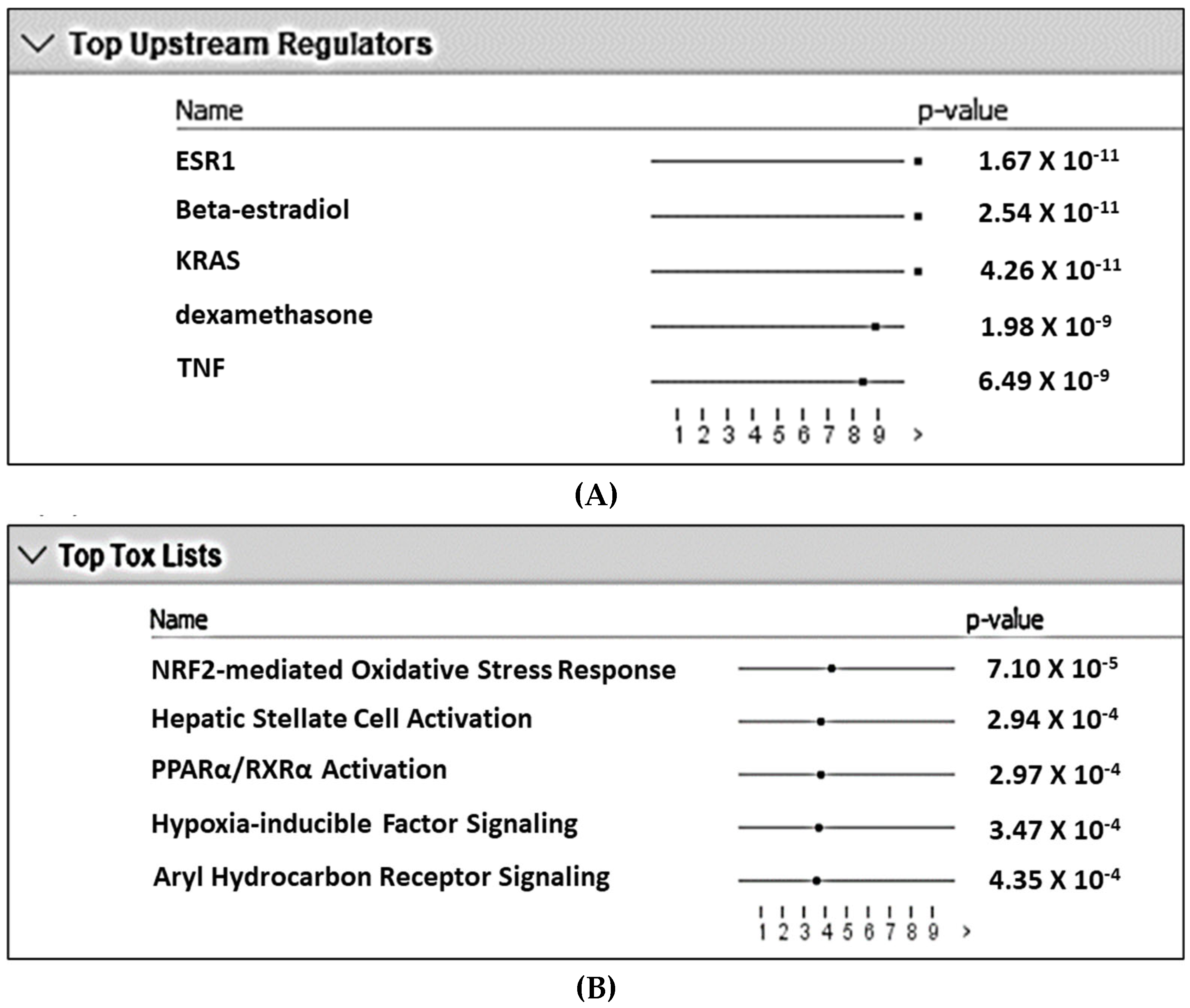
2.1. Pathway and Gene Ontology Term Analysis
2.2. AHR and HIF1α Signaling
2.3. NFκB Signaling
2.4. Wnt Signaling
2.5. Cytokines and Cytokine Receptors
2.6. Chemokines and Chemokine Receptors
2.7. T-Cell-Associated Factors
2.8. Myeloid Cell-Associated Factors
2.9. Innate Immunity
3. Discussion
4. Materials and Methods
4.1. Study Design and Gene Expression Data
4.2. Statistical Analysis
4.3. Pathway Analysis
4.4. Biological Inferences
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arzt, J.; Pacheco, J.M.; Rodriguez, L.L. The early pathogenesis of foot-and-mouth disease in cattle after aerosol inoculation. Vet. Pathol. 2010, 47, 1048–1063. [Google Scholar] [CrossRef]
- Arzt, J.; Juleff, N.; Zhang, Z.; Rodriguez, L.L. The pathogenesis of foot-and-mouth disease I: Viral pathways in cattle. Transbound. Emerg. Dis. 2011, 58, 291–304. [Google Scholar] [CrossRef] [PubMed]
- Burrows, R. Studies on the carrier state of cattle exposed to foot-and-mouth disease virus. Epidemiol. Infect. 1966, 64, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Burrows, R. The persistence of foot-and-mouth disease virus in sheep. Epidemiol. Infect. 1968, 66, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Moonen, P.; Schrijver, R. Carriers of foot-and-mouth disease virus: A review. Vet. Q. 2000, 22, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Stenfeldt, C.; Eschbaumer, M.; Rekant, S.I.; Pacheco, J.M.; Smoliga, G.R.; Hartwig, E.J.; Rodriguez, L.L.; Arzt, J. The foot-and-mouth disease carrier state divergence in cattle. J. Virol. 2016, 90, 6344–6364. [Google Scholar] [CrossRef] [PubMed]
- Bertram, M.R.; Vu, L.T.; Pauszek, S.J.; Brito, B.P.; Hartwig, E.J.; Smoliga, G.R.; Hoang, B.H.; Phuong, N.T.; Stenfeldt, C.; Fish, I.H.; et al. Lack of transmission of foot-and-mouth disease virus from persistently infected cattle to naïve cattle under field conditions in Vietnam. Front. Vet. Sci. 2018, 5, 174. [Google Scholar] [CrossRef]
- Stenfeldt, C.; Pacheco, J.M.; Smoliga, G.R.; Bishop, E.; Pauszek, S.J.; Hartwig, E.J.; Rodriguez, L.L.; Arzt, J. Detection of foot-and-mouth disease virus RNA and capsid protein in lymphoid tissues of convalescent pigs does not indicate existence of a carrier state. Transbound. Emerg. Dis. 2016, 63, 152–164. [Google Scholar] [CrossRef]
- Zhang, Z.D.; Kitching, R.P. The localization of persistent foot and mouth disease virus in the epithelial cells of the soft palate and pharynx. J. Comp. Pathol. 2001, 124, 89–94. [Google Scholar] [CrossRef]
- Pacheco, J.M.; Smoliga, G.R.; O’Donnell, V.; Brito, B.P.; Stenfeldt, C.; Rodriguez, L.L.; Arzt, J. Persistent foot-and-mouth disease virus infection in the nasopharynx of cattle; tissue-specific distribution and local cytokine expression. PLoS ONE 2015, 10, e0125698. [Google Scholar] [CrossRef]
- Stenfeldt, C.; Hartwig, E.J.; Smoliga, G.R.; Palinski, R.; Silva, E.B.; Bertram, M.R.; Fish, I.H.; Pauszek, S.J.; Arzt, J. Contact challenge of cattle with foot-and-mouth disease virus validates the role of the nasopharyngeal epithelium as the site of primary and persistent infection. Msphere 2018, 3, e00493-18. [Google Scholar] [CrossRef] [PubMed]
- Stenfeldt, C.; Arzt, J. The carrier conundrum; a review of recent advances and persistent gaps regarding the carrier state of Foot-and-mouth disease virus. Pathogens 2020, 9, 167. [Google Scholar] [CrossRef] [PubMed]
- Ilott, M.C.; Salt, J.S.; Gaskell, R.M.; Kitching, R.P. Dexamethasone inhibits virus production and the secretory IgA response in oesophageal-pharyngeal fluid in cattle persistently infected with foot-and-mouth disease virus. Epidemiol. Infect. 1997, 118, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.J.; Arzt, J.; Puckette, M.C.; Smoliga, G.R.; Pacheco, J.M.; Rodriguez, L.L. Mechanisms of foot-and-mouth disease virus tropism inferred from differential tissue gene expression. PLoS ONE 2013, 8, e64119. [Google Scholar] [CrossRef] [PubMed]
- Eschbaumer, M.; Stenfeldt, C.; Smoliga, G.R.; Pacheco, J.M.; Rodriguez, L.L.; Li, R.W.; Zhu, J.; Arzt, J. Transcriptomic analysis of persistent infection with foot-and-mouth disease virus in cattle suggests impairment of apoptosis and cell-mediated immunity in the nasopharynx. PLoS ONE 2016, 11, e0162750. [Google Scholar] [CrossRef]
- Stenfeldt, C.; Eschbaumer, M.; Smoliga, G.R.; Rodriguez, L.L.; Zhu, J.J.; Arzt, J. Clearance of a persistent picornavirus infection is associated with enhanced pro-apoptotic and cellular immune responses. Sci. Rep. 2017, 7, 17800–17814. [Google Scholar] [CrossRef]
- Zhu, J.J.; Stenfeldt, C.; Bishop, E.A.; Canter, J.A.; Eschbaumer, M.; Rodriguez, L.L.; Arzt, J. Mechanisms of maintenance of foot-and-mouth disease virus persistence inferred from genes differentially expressed in nasopharyngeal epithelia of virus carriers and non-carriers. Front. Vet. Sci. 2020, 7, 340. [Google Scholar] [CrossRef]
- Wagage, S.; Hunter, C.A. Interrelated roles for the aryl hydrocarbon receptor and hypoxia inducible factor-1α in the immune response to infection. Curr. Immunol. Rev. 2015, 11, 43–54. [Google Scholar] [CrossRef][Green Version]
- Gutiérrez-Vázquez, C.; Quintana, F.J. Regulation of the immune response by the aryl hydrocarbon receptor. Immunity 2018, 48, 19–33. [Google Scholar] [CrossRef]
- Sun, S.C. The non-canonical NF-κB pathway in immunity and inflammation. Nat. Rev. Immunol. 2017, 17, 545–558. [Google Scholar] [CrossRef]
- Bruhs, A.; Haarmann-Stemmann, T.; Frauenstein, K.; Krutmann, J.; Schwarz, T.; Schwarz, A. Activation of the arylhydrocarbon receptor causes immunosuppression primarily by modulating dendritic cells. J. Invest. Dermatol. 2015, 135, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Lahoti, T.S.; Boyer, J.A.; Kusnadi, A.; Gulsum, M.E.; Murray, I.A.; Perdew, G.H. Aryl hydrocarbon receptor activation synergistically induces lipopolysaccharide-mediated expression of proinflammatory chemokine (c-c motif) ligand 20. Toxicol. Sci. 2013, 1, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Innocentin, S.; Withers, D.R.; Roberts, N.A.; Gallagher, A.R.; Grigorieva, E.F.; Willhelm, C.; Veldhoen, M. Exogenous stimuli maintain intraepithelial lymphocytes via aryl hydrocarbon receptor activation. Cell 2011, 147, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, K.; Maekawa, Y.; Kataoka, K.; Ishifune, C.; Nishida, J.; Arimochi, H.; Kitamura, A.; Yoshimoto, T.; Tomita, S.; Nagahiro, S.; et al. The ARNT–STAT3 axis regulates the differentiation of intestinal intraepithelial TCRαβ+ CD8αα+ cells. Nat. Commun. 2013, 4, 2112. [Google Scholar] [CrossRef] [PubMed]
- Apetoh, L.; Quintana, F.J.; Pot, C.; Joller, N.; Xiao, S.; Kumar, D.; Burns, E.J.; Sherr, D.H.; Weiner, H.L.; Kuchroo, V.K. The aryl hydrocarbon receptor interacts with c-Maf to promote the differentiation of type 1 regulatory T cells induced by IL-27. Nat. Immunol. 2010, 11, 854–861. [Google Scholar] [CrossRef]
- Longhi, M.S.; Vuerich, M.; Kalbasi, A.; Kenison, J.E.; Yeste, A.; Csizmadia, E.; Vaughn, B.; Feldbrugge, L.; Mitsuhashi, S.; Wegiel, B.; et al. Bilirubin suppresses Th17 immunity in colitis by upregulating CD39. JCI Insight 2017, 2, e92791. [Google Scholar] [CrossRef]
- DiNatale, B.C.; Schroeder, J.C.; Francey, L.J.; Kusnadi, A.; Perdew, G.H. Mechanistic insights into the events that lead to synergistic induction of interleukin 6 transcription upon activation of the aryl hydrocarbon receptor and inflammatory signaling. J. Biol. Chem. 2010, 285, 24388–24397. [Google Scholar] [CrossRef]
- Cibrian, D.; Saiz, M.L.; de la Fuente, H.; Sánchez-Díaz, R.; Moreno-Gonzalo, O.; Jorge, I.; Ferrarini, A.; Vázquez, J.; Punzón, C.; Fresno, M.; et al. CD69 controls the uptake of L-tryptophan through LAT1-CD98 and AhR-dependent secretion of IL-22 in psoriasis. Nat. Immunol. 2016, 17, 985–996. [Google Scholar] [CrossRef]
- Tajima, H.; Tajiki-Nishino, R.; Watanabe, Y.; Kurata, K.; Fukuyama, T. Activation of aryl hydrocarbon receptor by benzo [a] pyrene increases interleukin 33 expression and eosinophil infiltration in a mouse model of allergic airway inflammation. J. Appl. Toxicol. 2020, 40, 1545–1553. [Google Scholar] [CrossRef]
- D’Ignazio, L.; Bandarra, D.; Rocha, S. NF-κB and HIF crosstalk in immune responses. FEBS J. 2016, 283, 413–424. [Google Scholar] [CrossRef]
- Papandreou, I.; Cairns, R.A.; Fontana, L.; Lim, A.L.; Denko, N.C. HIF-1 mediates adaptation to hypoxia by actively downregulating mitochondrial oxygen consumption. Cell Metab. 2006, 3, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W.; Tchernyshyov, I.; Semenza, G.L.; Dang, C.V. HIF-1-mediated expression of pyruvate dehydrogenase kinase: A metabolic switch required for cellular adaptation to hypoxia. Cell Metab. 2006, 3, 177–185. [Google Scholar] [CrossRef]
- Foxler, D.E.; Bridge, K.S.; James, V.; Webb, T.M.; Mee, M.; Wong, S.C.K.; Feng, Y.; Constantin-Teodosiu, D.; Petursdottir, T.E.; Bjornsson, J.; et al. The LIMD1 protein bridges an association between the prolyl hydroxylases and VHL to repress HIF-1 activity. Nat. Cell Biol. 2012, 14, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.C.; Quintin, J.; Cramer, R.A.; Shepardson, K.M.; Saeed, S.; Kumar, V.; Giamarellos-Bourboulis, E.J.; Matens, J.H.A.; Rao, N.A.; Aghajanirefah, A.; et al. mTOR-and HIF-1α–mediated aerobic glycolysis as metabolic basis for trained immunity. Science 2014, 345, 1250684. [Google Scholar] [CrossRef] [PubMed]
- Uche, U.U.; Piccirillo, A.R.; Kataoka, S.; Grebinoski, S.J.; D’Cruz, L.M.; Kane, L.P. PIK3IP1/TrIP restricts activation of T cells through inhibition of PI3K/Akt. J. Exp. Med. 2018, 215, 3165–3179. [Google Scholar] [CrossRef]
- Howie, D.; Waldmann, H.; Cobbold, S. Nutrient sensing via mTOR in T Cells maintains a tolerogenic microenvironment. Front. Immunol. 2014, 5, 409. [Google Scholar] [CrossRef]
- Goncharov, T.; Niessen, K.; de Almagro, M.C.; Izrael-Tomasevic, A.; Fedorova, A.V.; Varfolomeev, E.; Arnott, D.; Deshayes, K.; Kirkpatrivk, D.S.; Vucic, D. OTUB1 modulates c-IAP1 stability to regulate signaling pathways. EMBO J. 2013, 32, 1103–1114. [Google Scholar] [CrossRef]
- Peng, Y.; Xu, R.; Zheng, X. HSCARG negatively regulates the cellular antiviral RIG-I like receptor signaling pathway by inhibiting TRAF3 ubiquitination via recruiting OTUB1. PLoS Pathog. 2014, 10, e1004041. [Google Scholar] [CrossRef]
- Häcker, H.; Tseng, P.H.; Karin, M. Expanding TRAF function: TRAF3 as a tri-faced immune regulator. Nat. Rev. Immunol. 2011, 11, 457–468. [Google Scholar] [CrossRef]
- Huang, S.; Lu, W.; Ge, D.; Meng, N.; Li, Y.; Su, L.; Zhang, S.; Zhang, Y.; Zhao, B.; Miao, J. A new microRNA signal pathway regulated by long noncoding RNA TGFB2-OT1 in autophagy and inflammation of vascular endothelial cells. Autophagy 2015, 11, 2172–2183. [Google Scholar] [CrossRef]
- van Delft, M.A.; Huitema, L.F.; Tas, S.W. The contribution of NF-κB signalling to immune regulation and tolerance. Eur. J. Clin. Investig. 2015, 45, 529–539. [Google Scholar] [CrossRef]
- Micheli, L.; Leonardi, L.; Conti, F.; Maresca, G.; Colazingari, S.; Mattei, E.; Lira, S.A.; Farioli-Vecchioli, S.; Caruso, M.; Tirone, F. PC4/Tis7/IFRD1 stimulates skeletal muscle regeneration and is involved in myoblast differentiation as a regulator of MyoD and NF-kappaB. J. Biol. Chem. 2011, 286, 5691–5707. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.R.; Gonzales, N.; Aronowski, J. Pleiotropic role of PPARγ in intracerebral hemorrhage: An intricate system involving Nrf2, RXR, and NF-κB. CNS Neurosci. Ther. 2015, 21, 357–366. [Google Scholar] [CrossRef]
- Shalom-Barak, T.; Liersemann, J.; Memari, B.; Flechner, L.; Devor, C.E.; Bernardo, T.M.; Kim, S.; Matsumoto, N.; Friedman, S.L.; Evans, R.M.; et al. Ligand-dependent corepressor (LCoR) is a rexinoid-inhibited peroxisome proliferator-activated receptor γ-retinoid X receptor α coactivator. Mol. Cell Biol. 2018, 38, e00107–e00117. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, Z.; Chai, L.; Che, Y.; Min, S.; Yang, R. Identification and characterization of a unique leucine-rich repeat protein (LRRC33) that inhibits Toll-like receptor-mediated NF-κB activation. Biochem. Biophys. Res. Commun. 2013, 434, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Li, S.Z.; Zhang, H.H.; Liang, J.B.; Song, Y.; Jin, B.X.; Xing, N.N.; Fan, G.C.; Du, R.L.; Zhang, X.D. Nemo-like kinase (NLK) negatively regulates NF-kappa B activity through disrupting the interaction of TAK1 with IKKβ. Biochim. Biophys. Acta. 2014, 1843, 1365–1372. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jian, J.; Li, G.; Hettinghouse, A.; Liu, C. Progranulin: A key player in autoimmune diseases. Cytokine 2018, 101, 48–55. [Google Scholar] [CrossRef]
- Shahraz, A.; Kopatz, J.; Mathy, R.; Kappler, J.; Winter, D.; Kapoor, S.; Schütza, V.; Scheper, T.; Gieselmann, V.; Neumann, H. Anti-inflammatory activity of low molecular weight polysialic acid on human macrophages. Sci. Rep. 2015, 5, 16800. [Google Scholar] [CrossRef]
- Abdul-Sater, A.A.; Edilova, M.I.; Clouthier, D.L.; Mbanwi, A.; Kremmer, E.; Watts, T.H. The signaling adaptor TRAF1 negatively regulates Toll-like receptor signaling and this underlies its role in rheumatic disease. Nat. Immunol. 2017, 18, 26–35. [Google Scholar] [CrossRef]
- Jane-wit, D.; Surovtseva, Y.V.; Qin, L.; Li, G.; Liu, R.; Clark, P.; Manes, T.D.; Wang, C.; Kashgarian, M.; Kirkiles-Smith, N.C.; et al. Complement membrane attack complexes activate noncanonical NF-κB by forming an Akt+ NIK+ signalosome on Rab5+ endosomes. Proc. Natl. Acad. Sci. USA 2015, 112, 9686–9691. [Google Scholar] [CrossRef]
- Koliesnik, I.O.; Andreas, N.; Romanov, V.S.; Sreekantapuram, S.; Krljanac, B.; Haenold, R.; Weih, F. RelB regulates Th17 differentiation in a cell-intrinsic manner. Immunobiology 2018, 223, 191–199. [Google Scholar] [CrossRef]
- Suryawanshi, A.; Tadagavadi, R.K.; Swafford, D.; Manicassamy, S. Modulation of inflammatory responses by Wnt/β-Catenin signaling in dendritic cells: A novel immunotherapy target for autoimmunity and cancer. Front. Immunol. 2016, 7, 460. [Google Scholar] [CrossRef] [PubMed]
- Manicassamy, S.; Reizis, B.; Ravindran, R.; Nakaya, H.; Salazar-Gonzalez, R.M.; Wang, Y.C.; Pulendran, B. Activation of b-catenine in dendritic cells regulates immunity versus tolerance in the intestine. Science 2010, 329, 849–853. [Google Scholar] [CrossRef] [PubMed]
- Martin-Orozco, E.; Sanchez-Fernandez, A.; Ortiz-Parra, I.; Ayala-San Nicolas, M. WNT signaling in tumors: The way to evade drugs and immunity. Front. Immunol. 2019, 10, 2854. [Google Scholar] [CrossRef] [PubMed]
- Hunter, C.A.; Jones, S.A. IL-6 as a keystone cytokine in health and disease. Nat. Immunol. 2015, 16, 448–457. [Google Scholar] [CrossRef]
- Burkholder, B.; Huang, R.Y.; Burgess, R.; Luo, S.; Jones, V.S.; Zang, W.; Lv, Z.; Gao, C.; Wang, B.; Zhang, Y.; et al. Tumor-induced perturbations of cytokines and immune cell networks. Biochim. Biophys. Acta. 2014, 1845, 182–201. [Google Scholar] [CrossRef]
- McGeachy, M.J.; Cua, D.J. The link between IL-23 and Th17 cell-mediated immune pathologies. Semin. Immunol. 2007, 19, 372–376. [Google Scholar] [CrossRef]
- Cruikshank, W.W.; Kornfeld, H.; Center, D.M. Interleukin-16. J. Leukoc. Biol. 2000, 67, 757–766. [Google Scholar] [CrossRef]
- Skundric, D.S.; Cruikshank, W.W.; Montgomery, P.C.; Lisak, R.P.; Tse, H.Y. Emerging role of IL-16 in cytokine-mediated regulation of multiple sclerosis. Cytokine 2015, 75, 234–248. [Google Scholar] [CrossRef]
- Matsumoto, Y.; Fujita, T.; Hirai, I.; Sahara, H.; Torigoe, T.; Ezoe, K.; Saito, T.; Cruikshank, W.W.; Yotsuyanagi, T.; Sato, N. Immunosuppressive effect on T cell activation by interleukin-16-and interleukin-10-cDNA-double-transfected human squamous cell line. Burns 2009, 35, 383–389. [Google Scholar] [CrossRef]
- Bézie, S.; Picarda, E.; Ossart, J.; Tesson, L.; Usual, C.; Renaudin, K.; Anegon, I.; Guillonneau, C. IL-34 is a Treg-specific cytokine and mediates transplant tolerance. J. Clin. Investig. 2015, 125, 3952–3964. [Google Scholar] [CrossRef] [PubMed]
- Guillonneau, C.; Bézie, S.; Anegon, I. Immunoregulatory properties of the cytokine IL-34. Cell Mol. Life Sci. 2017, 74, 2569–2586. [Google Scholar] [CrossRef] [PubMed]
- Foucher, E.D.; Blanchard, S.; Preisser, L.; Garo, E.; Ifrah, N.; Guardiola, P.; Delneste, Y.; Jeannin, P. IL-34 induces the differentiation of human monocytes into immunosuppressive macrophages. antagonistic effects of GM-CSF and IFNγ. PLoS ONE 2013, 8, e56045. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Pan, G.; Tang, C.; Li, Z.; Zheng, D.; Wei, X.; Wu, Z. IL-34 inhibits acute rejection of rat liver transplantation by inducing Kupffer cell M2 polarization. Transplantation 2018, 102, e265–e274. [Google Scholar] [CrossRef] [PubMed]
- Boulakirba, S.; Pfeifer, A.; Mhaidly, R.; Obba, S.; Goulard, M.; Schmitt, T.; Chaintreuil, P.; Calleja, A.; Furstoss, N.; Orange, F.; et al. IL-34 and CSF-1 display an equivalent macrophage differentiation ability but a different polarization potential. Sci. Rep. 2018, 8, 256. [Google Scholar] [CrossRef] [PubMed]
- Sidhu-Varma, M.; Shih, D.Q.; Targan, S.R. Differential levels of Tl1a affect the expansion and function of regulatory T cells in modulating murine colitis. Inflamm. Bowel Dis. 2016, 22, 548–559. [Google Scholar] [CrossRef]
- Valatas, V.; Kolios, G.; Bamias, G. TL1A (TNFSF15) and DR3 (TNFRSF25): A co-stimulatory system of cytokines with diverse functions in gut mucosal immunity. Front. Immunol. 2019, 10, 583. [Google Scholar] [CrossRef]
- Liu, H.; Rohowsky-Kochan, C. Interleukin-27-mediated suppression of human Th17 cells is associated with activation of STAT1 and suppressor of cytokine signaling protein 1. J. Interferon Cytokine Res. 2011, 31, 459–469. [Google Scholar] [CrossRef]
- Aparicio-Siegmund, S.; Garbers, C. The biology of interleukin-27 reveals unique pro- and anti-inflammatory functions in immunity. Cytokine Growth Factor Rev. 2015, 26, 579–586. [Google Scholar] [CrossRef]
- Yoshida, H.; Hunter, C.A. The immunobiology of interleukin-27. Annu. Rev. Immunol. 2015, 33, 417–443. [Google Scholar] [CrossRef]
- Mascanfroni, I.D.; Yeste, A.; Vieira, S.M.; Burns, E.J.; Patel, B.; Sloma, I.; Wu, Y.; Mayo, L.; Ben-Hamo, R.; Efroni, S.; et al. IL-27 acts on DCs to suppress the T cell response and autoimmunity by inducing expression of the immunoregulatory molecule CD39. Nat. Immunol. 2013, 14, 1054–1063. [Google Scholar] [CrossRef] [PubMed]
- Pot, C.; Jin, H.; Awasthi, A.; Lie, S.M.; Lai, C.Y.; Madan, R.; Sharpe, A.H.; Karp, C.L.; Miaw, S.C.; Ho, I.C.; et al. Cutting edge: IL-27 induces the transcription factor c-Maf, cytokine IL-21, and the costimulatory receptor ICOS that coordinately act together to promote differentiation of IL-10-producing Tr1 cells. J. Immunol. 2009, 183, 797–801. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S. The role of transforming growth factor β in T helper 17 differentiation. Immunology. 2018, 155, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Morianos, I.; Papadopoulou, G.; Semitekolou, M.; Xanthou, G. Activin-A in the regulation of immunity in health and disease. J. Autoimmun. 2019, 104, 102314. [Google Scholar] [CrossRef]
- Angkasekwinai, P.; Park, H.; Wang, Y.H.; Wang, Y.H.; Chang, S.H.; Corry, D.B.; Liu, Y.J.; Zhu, Z.; Dong, C. Interleukin 25 promotes the initiation of proallergic type 2 responses. J. Exp. Med. 2007, 204, 1509–1517. [Google Scholar] [CrossRef]
- Bulek, K.; Swaidani, S.; Qin, J.; Lu, Y.; Gulen, M.F.; Herjan, T.; Min, B.; Kastelein, R.A.; Aronica, M.; Kosz-Vnenchak, M.; et al. The essential role of single Ig IL-1 receptor-related molecule/toll IL-1R8 in regulation of Th2 immune response. J. Immunol. 2009, 182, 2601–2609. [Google Scholar] [CrossRef]
- Hsieh, S.L.; Lin, W.W. Decoy receptor 3: An endogenous immunomodulator in cancer growth and inflammatory reactions. J. Biomed. Sci. 2017, 24, 39. [Google Scholar] [CrossRef]
- Mueller, A.M.; Pedré, X.; Killian, S.; David, M.; Steinbrecher, A. The decoy receptor 3 (DcR3, TNFRSF6B) suppresses Th17 immune responses and is abundant in human cerebrospinal fluid. J. Neuroimmunol. 2009, 209, 57–64. [Google Scholar] [CrossRef]
- Kurts, C.; Carbone, F.R.; Krummel, M.F.; Koch, K.M.; Miller, J.F.; Heath, W.R. Signaling through CD30 protects against autoimmune diabetes mediated by CD8 T cells. Nature 1999, 398, 341–344. [Google Scholar] [CrossRef]
- Menzies-Gow, A.; Ying, S.; Sabroe, I.; Stubbs, V.L.; Soler, D.; Williams, T.J.; Kay, A.B. Eotaxin (CCL11) and eotaxin-2 (CCL24) induce recruitment of eosinophils, basophils, neutrophils, and macrophages as well as features of early- and late-phase allergic reactions following cutaneous injection in human atopic and nonatopic volunteers. J. Immunol. 2002, 169, 2712–2718. [Google Scholar] [CrossRef]
- Li, W.; Liu, L.; Gomez, A.; Zhang, J.; Ramadan, A.; Zhang, Q.; Choi, S.W.; Zhang, P.; Greenson, J.K.; Liu, C.; et al. Proteomics analysis reveals a Th17-prone cell population in presymptomatic graft-versus-host disease. JCI Insight 2016, 1, e86660. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.Y.; Eri, R.; Lyons, A.B.; Grimm, M.C.; Korner, H. CC Chemokine ligand 20 and its cognate receptor CCR6 in mucosal T cell immunology and inflammatory bowel disease: Odd couple or axis of evil? Front. Immunol. 2013, 4, 194. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.Y.S.; Körner, H. The CCR6-CCL20 axis in humoral immunity and T-B cell immunobiology. Immunobiology 2019, 224, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Meiron, M.; Zohar, Y.; Anunu, R.; Wildbaum, G.; Karin, N. CXCL12 (SDF-1alpha) suppresses ongoing experimental autoimmune encephalomyelitis by selecting antigen-specific regulatory T cells. J. Exp. Med. 2008, 205, 2643–2655. [Google Scholar] [CrossRef] [PubMed]
- Comito, G.; Giannoni, E.; Segura, C.P.; Barcellos-de-Souza, P.; Raspollini, M.R.; Baroni, G.; Lanciotti, M.; Serni, S.; Chiarugi, P. Cancer-associated fibroblasts and M2-polarized macrophages synergize during prostate carcinoma progression. Oncogene 2014, 33, 2423–2431. [Google Scholar] [CrossRef]
- Lim, K.; Hyun, Y.M.; Lambert-Emo, K.; Capece, T.; Bae, S.; Miller, R.; Topham, D.J.; Kim, M. Neutrophil trails guide influenza-specific CD8+ T cells in the airways. Science 2015, 349, aaa4352. [Google Scholar] [CrossRef]
- Zhong, J.; Rajagopalan, S. Dipeptidyl peptidase-4 regulation of SDF-1/CXCR4 axis: Implications for cardiovascular disease. Front. Immunol. 2015, 6, 477. [Google Scholar] [CrossRef]
- Ansel, K.M.; Ngo, V.N.; Hyman, P.L.; Luther, S.A.; Förster, R.; Sedgwick, J.D.; Browning, J.L.; Lipp, M.; Cyster, J.G. A chemokine-driven positive feedback loop organizes lymphoid follicles. Nature 2000, 406, 309–314. [Google Scholar] [CrossRef]
- Kurth, I.; Willimann, K.; Schaerli, P.; Hunziker, T.; Clark-Lewis, I.; Moser, B. Monocyte selectivity and tissue localization suggests a role for breast and kidney-expressed chemokine (BRAK) in macrophage development. J. Exp. Med. 2001, 194, 855–861. [Google Scholar] [CrossRef]
- Lu, J.; Chatterjee, M.; Schmid, H.; Beck, S.; Gawaz, M. CXCL14 as an emerging immune and inflammatory modulator. J. Inflamm. 2016, 13, 1–8. [Google Scholar] [CrossRef]
- Cereijo, R.; Gavaldà-Navarro, A.; Cairó, M.; Quesada-López, T.; Villarroya, J.; Morón-Ros, S.; Sánchez-Infantes, D.; Peyrou, M.; Iglesias, R.; Mampel, T.; et al. CXCL14, a brown adipokine that mediates brown-fat-to-macrophage communication in thermogenic adaptation. Cell Metab. 2018, 28, 750–763. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.T.; Liu, S.P.; Lin, C.H.; Lee, S.W.; Hsu, C.Y.; Sytwu, H.K.; Hsieh, C.H.; Shyu, W.C. A crucial role of CXCL14 for promoting regulatory T cells activation in stroke. Theranostics 2017, 7, 855–875. [Google Scholar] [CrossRef] [PubMed]
- Rajasekaran, G.; Dinesh Kumar, S.; Nam, J.; Jeon, D.; Kim, Y.; Lee, C.W.; Park, I.S.; Shin, S.Y. Antimicrobial and anti-inflammatory activities of chemokine CXCL14-derived antimicrobial peptide and its analogs. Biochim. Biophys. Acta. Biomembr. 2019, 1861, 256–267. [Google Scholar] [CrossRef] [PubMed]
- Tanegashima, K.; Suzuki, K.; Nakayama, Y.; Tsuji, K.; Shigenaga, A.; Otaka, A.; Hara, T. CXCL14 is a natural inhibitor of the CXCL12-CXCR4 signaling axis. FEBS Lett. 2013, 587, 1731–1735. [Google Scholar] [CrossRef] [PubMed]
- Tanegashima, K.; Tsuji, K.; Suzuki, K.; Shigenaga, A.; Otaka, A.; Hara, T. Dimeric peptides of the C-terminal region of CXCL14 function as CXCL12 inhibitors. FEBS Lett. 2013, 587, 3770–3775. [Google Scholar] [CrossRef]
- Ramos, C.D.; Canetti, C.; Souto, J.T.; Silva, J.S.; Hogaboam, C.M.; Ferreira, S.H.; Cunha, F.Q. MIP-1alpha[CCL3] acting on the CCR1 receptor mediates neutrophil migration in immune inflammation via sequential release of TNF-alpha and LTB4. J. Leukoc Biol. 2005, 78, 167–177. [Google Scholar] [CrossRef]
- Griffith, J.W.; Sokol, C.L.; Luster, A.D. Chemokines and chemokine receptors: Positioning cells for host defense and immunity. Annu. Rev. Immunol. 2014, 32, 659–702. [Google Scholar] [CrossRef]
- Castellino, F.; Huang, A.Y.; Altan-Bonnet, G.; Stoll, S.; Scheinecker, C.; Germain, R.N. Chemokines enhance immunity by guiding naive CD8+ T cells to sites of CD4+ T cell-dendritic cell interaction. Nature 2006, 440, 890–895. [Google Scholar] [CrossRef]
- Ye, J.; Kohli, L.L.; Stone, M.J. Characterization of binding between the chemokine eotaxin and peptides derived from the chemokine receptor CCR3. J. Biol. Chem. 2000, 275, 27250–27257. [Google Scholar] [CrossRef]
- Collins, P.J.; McCully, M.L.; Martínez-Muñoz, L.; Santiago, C.; Wheeldon, J.; Caucheteux, S.; Thelen, S.; Cecchinato, V.; Laufer, J.M.; Purvanov, V.; et al. Epithelial chemokine CXCL14 synergizes with CXCL12 via allosteric modulation of CXCR4. FASEB J. 2017, 31, 3084–3097. [Google Scholar] [CrossRef]
- Janssens, R.; Struyf, S.; Proost, P. Pathological roles of the homeostatic chemokine CXCL12. Cytokine Growth Factor Rev. 2018, 44, 51–68. [Google Scholar] [CrossRef] [PubMed]
- Lei, Y.; Takahama, Y. XCL1 and XCR1 in the immune system. Microbes Infect. 2012, 14, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; Moon, S.J.; Lee, S.W. Lineage re-commitment of CD4CD8αα intraepithelial lymphocytes in the gut. BMB Rep. 2016, 49, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Lederman, S.; Yellin, M.J.; Krichevsky, A.; Belko, J.; Lee, J.J.; Chess, L. Identification of a novel surface protein on activated CD4+ T cells that induces contact-dependent B cell differentiation (help). J. Exp. Med. 1992, 175, 1091–1101. [Google Scholar] [CrossRef]
- Flanagan, K.; Fitzgerald, K.; Baker, J.; Regnstrom, K.; Gardai, S.; Bard, F.; Mocci, S.; Seto, P.; You, M.; Larochelle, C.; et al. Laminin-411 is a vascular ligand for MCAM and facilitates TH17 cell entry into the CNS. PLoS ONE 2012, 7, e40443. [Google Scholar] [CrossRef]
- Kohlhaas, S.; Garden, O.A.; Scudamore, C.; Turner, M.; Okkenhaug, K.; Vigorito, E. Cutting edge: The Foxp3 target miR-155 contributes to the development of regulatory T cells. J. Immunol. 2009, 182, 2578–2582. [Google Scholar] [CrossRef]
- Lu, L.F.; Thai, T.H.; Calado, D.P.; Chaudhry, A.; Kubo, M.; Tanaka, K.; Loeb, G.B.; Lee, H.; Yoshimura, A.; Rajewski, K.; et al. Foxp3-dependent microRNA155 confers competitive fitness to regulatory T cells by targeting SOCS1 protein. Immunity 2009, 30, 80–91. [Google Scholar] [CrossRef]
- Escobar, T.M.; Kanellopoulou, C.; Kugler, D.G.; Kilaru, G.; Nguyen, C.K.; Nagarajan, V.; Bhairavabhotla, R.K.; Northrup, D.; Zahr, R.; Burr, P.; et al. miR-155 activates cytokine gene expression in Th17 cells by regulating the DNA-binding protein Jarid2 to relieve polycomb-mediated repression. Immunity 2014, 40, 865–879. [Google Scholar] [CrossRef]
- Yao, R.; Ma, Y.L.; Liang, W.; Li, H.; Ma, Z.; Yu, X.; Liao, Y. MicroRNA-155 modulates Treg and Th17 cells differentiation and Th17 cell function by targeting SOCS1. PLoS ONE 2012, 7, e46082. [Google Scholar] [CrossRef]
- Cui, G.; Qin, X.; Wu, L.; Zhang, Y.; Sheng, X.; Yu, Q.; Sheng, H.; Xi, B.; Zhang, J.Z.; Zang, Y.Q. Liver X receptor (LXR) mediates negative regulation of mouse and human Th17 differentiation. J. Clin. Investig. 2011, 121, 658–670. [Google Scholar] [CrossRef]
- Martin, P.; Gomez, M.; Lamana, A.; Cruz-Adalia, A.; Ramirez-Huesca, M.; Ursa, M.A.; Yanez-Mo, M.; Sanchez-Madrid, F. CD69 association with Jak3/Stat5 proteins regulates Th17 cell differentiation. Mol. Cell Biol. 2010, 30, 4877–4889. [Google Scholar] [CrossRef]
- Zeng, H.; Zhang, R.; Jin, B.; Chen, L. Type 1 regulatory T cells: A new mechanism of peripheral immune tolerance. Cell Mol Immunol. 2015, 12, 566–571. [Google Scholar] [CrossRef]
- Arce-Sillas, A.; Álvarez-Luquín, D.D.; Tamaya-Domínguez, B.; Gomez-Funtes, S.; Trejo-Garcia, A.; Melo-Salas, M.; Cárdenas, G.; Rodriguez-Ramirez, J.; Adalid-Peralta, L. Regulatory T Cells: Molecular actions on effector cells in immune regulation. J. Immunol. Res. 2016, 2016, 1720827. [Google Scholar] [CrossRef]
- Rueda, C.M.; Jackson, C.M.; Chougnet, C.A. Regulatory T-cell-mediated suppression of conventional T-cells and dendritic cells by different cAMP intracellular pathways. Front. Immunol. 2016, 7, 216. [Google Scholar] [CrossRef]
- Wherry, E.J.; Kurachi, M. Molecular and cellular insights into T cell exhaustion. Nat. Rev. Immunol. 2015, 15, 486–499. [Google Scholar] [CrossRef]
- Jones, A.; Bourque, J.; Kuehm, L.; Opejin, A.; Teague, R.M.; Gross, C.; Hawiger, D. Immunomodulatory functions of BTLA and HVEM govern induction of extrathymic regulatory T cells and tolerance by dendritic cells. Immunity 2016, 45, 1066–1077. [Google Scholar] [CrossRef]
- Aksoylar, H.I.; Lampe, K.; Barnes, M.J.; Plas, D.R.; Hoebe, K. Loss of immunological tolerance in Gimap5-deficient mice is associated with loss of Foxo in CD4+ T cells. J. Immunol. 2012, 188, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Endale, M.; Aksoylar, H.I.; Hoebe, K. Central role of gimap5 in maintaining peripheral tolerance and T cell homeostasis in the gut. Mediat. Inflamm. 2015, 2015, 436017. [Google Scholar] [CrossRef] [PubMed]
- Patterson, A.R.; Bolcas, P.; Lampe, K.; Cantrell, R.; Ruff, B.; Lewkowich, I.; Hogan, S.P.; Janssen, E.M.; Bleesing, J.; Hershey, G.K.K.; et al. Loss of GTPase of immunity-associated protein 5 (Gimap5) promotes pathogenic CD4+ T-cell development and allergic airway disease. J. Allergy Clin. Immunol. 2019, 143, 245–257. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Mao, L.; Xiao, F.; Liao, Z.; Yin, J.; Li, W.; Sun, M.; Liu, M.; Ji, X.; Liu, C.; et al. Interferon-stimulated genes inhibit caprine parainfluenza virus type 3 replication in Madin-Darby bovine kidney cells. Vet. Microbiol. 2020, 241, 108573. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Liang, S.; Zhong, Z.; Wen, J.; Li, W.; Wang, L.; Xu, J.; Zhong, F.; Li, X. Soluble CD83 inhibits human monocyte differentiation into dendritic cells in vitro. Cell Immunol. 2014, 292, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Nakano-Yokomizo, T.; Tahara-Hanaoka, S.; Nakahashi-Oda, C.; Nabekura, T.; Tchao, N.K.; Kadosaki, M.; Totsuka, N.; Kurita, N.; Nakamagoe, K.; Tamaoka, A.; et al. The immunoreceptor adapter protein DAP12 suppresses B lymphocyte-driven adaptive immune responses. J. Exp. Med. 2011, 208, 1661–1671. [Google Scholar] [CrossRef] [PubMed]
- Gasiorowski, R.E.; Ju, X.; Hart, D.N.; Clark, G.J. CD300 molecule regulation of human dendritic cell functions. Immunol. Lett. 2013, 149, 93–100. [Google Scholar] [CrossRef]
- Lopez Robles, M.D.; Pallier, A.; Huchet, V.; Le Texier, L.; Remy, S.; Braudeau, V.; Delbos, L.; Moreau, A.; Louvet, C.; Brosseau, C.; et al. Cell-surface C-type lectin-like receptor CLEC-1 dampens dendritic cell activation and downstream Th17 responses. Blood Adv. 2017, 1, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.H.; Faunce, D.E.; Stacey, M.; Terajewicz, A.; Nakamura, T.; Zhang-Hoover, J.; Kerley, M.; Mucenski, M.L.; Gordon, S.; Stein-Streilein, J. The macrophage F4/80 receptor is required for the induction of antigen-specific efferent regulatory T cells in peripheral tolerance. J. Exp. Med. 2005, 201, 1615–1625. [Google Scholar] [CrossRef]
- Yoshida, R. MHC class I recognition by monocyte-/macrophage-specific receptors. Adv. Immunol. 2014, 124, 207–247. [Google Scholar] [CrossRef]
- Wang, J.; Sun, J.; Liu, L.N.; Flies, D.B.; Nie, X.; Toki, M.; Zhang, J.; Song, C.; Zarr, M.; Zhou, X.; et al. Siglec-15 as an immune suppressor and potential target for normalization cancer immunotherapy. Nat. Med. 2019, 25, 656–666. [Google Scholar] [CrossRef]
- Freeman, G.J.; Casasnovas, J.M.; Umetsu, D.T.; DeKruyff, R.H. TIM genes: A family of cell surface phosphatidylserine receptors that regulate innate and adaptive immunity. Immunol. Rev. 2010, 235, 172–189. [Google Scholar] [CrossRef]
- Albackerk, L.A.; Karisola, P.; Chang, Y.J.; Umetsu, S.E.; Zhou, M.; Akbari, O.; Kobayashi, N.; Baumgarth, N.; Freeman, G.J.; Umetsu, D.T.; et al. TIM-4, a receptor for phosphatidylserine, controls adaptive immunity by regulating the removal of antigen-specific T cells. J. Immunol. 2010, 185, 6839–6849. [Google Scholar] [CrossRef]
- Round, J.L.; Lee, S.M.; Li, J.; Tran, G.; Jabri, B.; Chatila, T.A.; Mazmanian, S.K. The Toll-like receptor 2 pathway establishes colonization by a commensal of the human microbiota. Science 2011, 332, 974–977. [Google Scholar] [CrossRef]
- Xiong, Y.; Pennini, M.; Vogel, S.N.; Medvedev, A.E. IRAK4 kinase activity is not required for induction of endotoxin tolerance but contributes to TLR2-mediated tolerance. J. Leukoc. Biol. 2013, 94, 291–300. [Google Scholar] [CrossRef]
- Manoharan, I.; Hong, Y.; Suryawanshi, A.; Angus-Hill, M.L.; Sun, Z.; Mellor, A.L.; Munn, D.H.; Manicassamy, S. TLR2-dependent activation of beta-catenin pathway in dendritic cells induces regulatory responses and attenuates autoimmune inflammation. J. Immunol. 2014, 193, 4203–4213. [Google Scholar] [CrossRef] [PubMed]
- Bhaskaran, N.; Cohen, S.; Zhang, Y.; Weinberg, A.; Pandiyan, P. TLR-2 signaling promotes IL-17A production in CD4+ CD25+ Foxp3+ regulatory cells during oropharyngeal candidiasis. Pathogens 2015, 4, 90–110. [Google Scholar] [CrossRef] [PubMed]
- Choteau, L.; Vancraeyneste, H.; Le Roy, D.; Dubuquoy, L.; Romani, L.; Jouault, T.; Poulain, D.; Sendid, B.; Calandra, T.; Roger, T.; et al. Role of TLR1, TLR2 and TLR6 in the modulation of intestinal inflammation and Candida albicans elimination. Gut Pathog. 2017, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Schröder, J.M.; Harder, J. Human beta-defensin-2. Int. J. Biochem. Cell Biol. 1999, 31, 645–651. [Google Scholar] [CrossRef]
- Chen, W.; Liu, Z.; Zhang, Q.; Yan, Q.; Jing, S. Induction and antiviral activity of human β-defensin 3 in intestinal cells with picornavirus infection. Acta Virol. 2018, 62, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Gaggero, S.; Bruschi, M.; Petretto, A.; Parodi, M.; Del Zotto, G.; Lavarello, C.; Prato, C.; Santucci, L.; Barbuto, A.; Bottino, C.; et al. Nidogen-1 is a novel extracellular ligand for the NKp44 activating receptor. Oncoimmunology 2018, 7, e1470730. [Google Scholar] [CrossRef] [PubMed]
- Turner, A.; Li, L.C.; Pilli, T.; Qian, L.; Wiley, E.L.; Setty, S.; Christov, K.; Ganesh, L.; Maker, A.V.; Li, P.; et al. MADD knock-down enhances doxorubicin and TRAIL induced apoptosis in breast cancer cells. PLoS ONE 2013, 8, e56817. [Google Scholar] [CrossRef]
- Zhu, J.J.; Canter, J.A.; Rodriguez, L.L.; Arzt, J. A novel bovine CXCL15 gene in the GRO chemokine gene cluster. Vet. Immunol. Immunopathol. 2020, 220, 109990. [Google Scholar] [CrossRef]
- Schönrich, G.; Raftery, M.J. Neutrophil extracellular traps go viral. Front. Immunol. 2016, 7, 366. [Google Scholar] [CrossRef]
- Pruett, J.H.; Fisher, W.F.; DeLoach, J.R. Effects of dexamethasone on selected parameters of the bovine immune system. Vet. Res. Commun. 1987, 11, 305–323. [Google Scholar] [PubMed]
- Jain, N.C.; Vegad, J.L.; Shrivastava, A.B.; Jain, N.K.; Garg, U.K.; Kolte, G.N. Haematological changes in buffalo calves inoculated with Escherichia coli endotoxin and corticosteroids. Res. Vet. Sci. 1989, 47, 305–308. [Google Scholar] [CrossRef]
- Thanasak, J.; Jorritsma, R.; Hoek, A.; Noordhuizen, J.P.; Rutten, V.P.; Müller, K.E. The effects of a single injection of dexamethasone-21-isonicotinate on the lymphocyte functions of dairy cows at two weeks post-partum. Vet. Res. 2004, 35, 103–112. [Google Scholar] [CrossRef][Green Version]
- Veldhoen, M.; Hirota, K.; Westendorf, A.M.; Buer, J.; Dumoutier, L.; Renauld, J.C.; Stockinger, B. The aryl hydrocarbon receptor links TH17-cell-mediated autoimmunity to environmental toxins. Nature 2008, 453, 106–109. [Google Scholar] [CrossRef]
- Veldhoen, M.; Hirota, K.; Christensen, J.; O’Garra, A.; Stockinger, B. Natural agonists for aryl hydrocarbon receptor in culture medium are essential for optimal differentiation of Th17 T cells. J. Exp. Med. 2009, 206, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Quintana, F.J.; Basso, A.S.; Iglesias, A.H.; Korn, T.; Farez, M.F.; Bettelli, E.; Caccamo, M.; Oukka, M.; Weiner, H.L. Control of T(reg) and T(H)17 cell differentiation by the aryl hydrocarbon receptor. Nature. 2008, 453, 65–71. [Google Scholar] [CrossRef]
- Singh, N.P.; Singh, U.P.; Rouse, M.; Zhang, J.; Chatterje, S.; Nagarkatti, P.S.; Nagarkatti, M. Dietary indoles suppress delayed-type hypersensitivity by inducing a switch from proinflammatory Th17 cells to anti-inflammatory regulatory T cells through regulation of microRNA. J. Immunol. 2016, 196, 1108–1122. [Google Scholar] [CrossRef] [PubMed]
- Hammerschmidt-Kamper, C.; Biljes, D.; Merches, K.; Steiner, I.; Daldrup, T.; Bol-Schoenmakers, M.; Pieters, R.H.H.; Esser, C. Indole-3-carbinol, a plant nutrient and AhR-Ligand precursor, supports oral tolerance against OVA and improves peanut allergy symptoms in mice. PLoS ONE 2017, 12, e0180321. [Google Scholar] [CrossRef]
- Cervantes-Barragan, L.; Chai, J.N.; Tianero, M.D.; Di Luccia, B.; Ahern, P.P.; Merriman, J.; Cortez, V.S.; Caparon, M.G.; Donia, M.S.; Gilfillan, S.; et al. Lactobacillus reuteri induces gut intraepithelial CD4+ CD8αα+ T cells. Science 2017, 357, 806–810. [Google Scholar] [CrossRef]
- Schiering, C.; Wincent, E.; Metidji, A.; Iseppon, A.; Li, Y.; Potocnik, A.J.; Omenetti, S.; Henderson, C.J.; Wolf, C.R.; Nebert, D.W.; et al. Feedback control of AHR signalling regulates intestinal immunity. Nature 2017, 542, 242–245. [Google Scholar] [CrossRef]
- Mezrich, J.D.; Fechner, J.H.; Zhang, X.; Johnson, B.P.; Burlingham, W.J.; Bradfield, C.A. An interaction between kynurenine and the aryl hydrocarbon receptor can generate regulatory T cells. J. Immunol. 2010, 185, 3190–3198. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.; Kimura, A.; Nakahama, T.; Chinen, I.; Masuda, K.; Nohara, K.; Fujii-Kuriyama, Y.; Kishimoto, T. Aryl hydrocarbon receptor negatively regulates dendritic cell immunogenicity via a kynurenine-dependent mechanism. Proc. Natl. Acad. Sci. USA 2010, 107, 19961–19966. [Google Scholar] [CrossRef] [PubMed]
- Quintana, F.J.; Murugaiyan, G.; Farez, M.F.; Mitsdoerffer, M.; Tukpah, A.M.; Burns, E.J.; Weiner, H.L. An endogenous aryl hydrocarbon receptor ligand acts on dendritic cells and T cells to suppress experimental autoimmune encephalomyelitis. Proc. Natl. Acad. Sci. USA 2010, 107, 20768–20773. [Google Scholar] [CrossRef]
- Platzer, B.; Richter, S.; Kneidinger, D.; Waltenberger, D.; Woisetschläger, M.; Strobl, H. Aryl hydrocarbon receptor activation inhibits in vitro differentiation of human monocytes and Langerhans dendritic cells. J. Immunol. 2009, 183, 66–74. [Google Scholar] [CrossRef]
- Jurado-Manzano, B.B.; Zavala-Reyes, D.; Turrubiartes-Martínez, E.A.; Portales-Pérez, D.P.; González-Amaro, R.; Layseca-Espinosa, E. FICZ generates human tDCs that induce CD4+ CD25high Foxp3+ Treg-like cell differentiation. Immunol. Lett. 2017, 190, 84–92. [Google Scholar] [CrossRef]
- Shinde, R.; McGaha, T.L. The aryl hydrocarbon receptor: Connecting immunity to the microenvironment. Trends Immunol. 2018, 39, 1005–1020. [Google Scholar] [CrossRef] [PubMed]
- Swedenborg, E.; Pongratz, I. AhR and ARNT modulate ER signaling. Toxicology 2010, 268, 132–138. [Google Scholar] [CrossRef]
- Göttel, M.; Le Corre, L.; Dumont, C.; Schrenk, D.; Chagnon, M.C. Estrogen receptor α and aryl hydrocarbon receptor cross-talk in a transfected hepatoma cell line (HepG2) exposed to 2,3,7,8-tetrachlorodibenzo-p-dioxin. Toxicol. Rep. 2014, 1, 1029–1036. [Google Scholar] [CrossRef]
- Helle, J.; Bader, M.I.; Keiler, A.M.; Zierau, O.; Vollmer, G.; Chittur, S.V.; Tenniswood, M.; Kretzschmar, G. Cross-talk in the female rat mammary gland: Influence of aryl hydrocarbon receptor on estrogen receptor signaling. Environ. Health Perspect. 2016, 124, 601–610. [Google Scholar] [CrossRef]
- Vorrink, S.U.; Domann, F.E. Regulatory crosstalk and interference between the xenobiotic and hypoxia sensing pathways at the AhR-ARNT-HIF1α signaling node. Chem. Biol. Interact. 2014, 218, 82–88. [Google Scholar] [CrossRef]
- Shi, L.Z.; Wang, R.; Huang, G.; Vogel, P.; Neale, G.; Green, D.R.; Chi, H. HIF1alpha-dependent glycolytic pathway orchestrates a metabolic checkpoint for the differentiation of TH17 and Treg cells. J. Exp. Med. 2011, 208, 1367–1376. [Google Scholar] [CrossRef] [PubMed]
- Dang, E.V.; Barbi, J.; Yang, H.Y.; Jinasena, D.; Yu, H.; Zheng, Y.; Bordman, Z.; Fu, J.; Kim, Y.; Yen, H.R.; et al. Control of T(H)17/T(reg) balance by hypoxia-inducible factor 1. Cell 2011, 146, 772–784. [Google Scholar] [CrossRef] [PubMed]
- Gagliani, N.; Amezcua Vesely, M.C.; Iseppon, A.; Brockmann, L.; Xu, H.; Palm, N.W.; de Zoete, M.R.; Licona-Limón, P.; Paiva, R.S.; Ching, T.; et al. Th17 cells transdifferentiate into regulatory T cells during resolution of inflammation. Nature 2015, 523, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Vogel, C.F.; Khan, E.M.; Leung, P.S.; Gershwin, M.E.; Chang, W.L.; Wu, D.; Haarmann-Stemmann, T.; Hoffmann, A.; Denison, M.S. Cross-talk between aryl hydrocarbon receptor and the inflammatory response: A role for nuclear factor-κB. J. Biol. Chem. 2014, 289, 1866–1875. [Google Scholar] [CrossRef]
- Liu, P.C.; Phillips, M.A.; Matsumura, F. Alteration by 2,3,7,8-Tetrachlorodibenzo-p-dioxin of CCAAT/enhancer binding protein correlates with suppression of adipocyte differentiation in 3T3-L1 cells. Mol. Pharmacol. 1996, 49, 989–997. [Google Scholar]
- Borland, M.G.; Krishnan, P.; Lee, C.; Albrecht, P.P.; Shan, W.; Bility, M.T.; Marcus, C.B.; Lin, J.M.; Amin, S.; Gonzalez, F.J.; et al. Modulation of aryl hydrocarbon receptor (AHR)-dependent signaling by peroxisome proliferator-activated receptor β/δ (PPARβ/δ) in keratinocytes. Carcinogenesis 2014, 35, 1602–1612. [Google Scholar] [CrossRef]
- Phan, A.T.; Goldrath, A.W. Hypoxia-inducible factors regulate T cell metabolism and function. Mol. Immunol. 2015, 68, 527–535. [Google Scholar] [CrossRef]
- Tian, Y.; Ke, S.; Denison, M.S.; Rabson, A.B.; Gallo, M.A. Ah receptor and NF-kappaB interactions, a potential mechanism for dioxin toxicity. J. Biol. Chem. 1999, 274, 510–515. [Google Scholar] [CrossRef]
- Amatya, N.; Garg, A.V.; Gaffen, S.L. IL-17 Signaling: The Yin and the Yang. Trends Immunol. 2017, 38, 310–322. [Google Scholar] [CrossRef]
- Cella, M.; Colonna, M. Aryl hydrocarbon receptor: Linking environment to immunity. Semin. Immunol. 2015, 27, 310–314. [Google Scholar] [CrossRef]
- Marinelli, L.; Martin-Gallausiaux, C.; Bourhis, J.M.; Béguet-Crespel, F.; Blottière, H.M.; Lapaque, N. Identification of the novel role of butyrate as AhR ligand in human intestinal epithelial cells. Sci. Rep. 2019, 9, 643. [Google Scholar] [CrossRef] [PubMed]
- Garrison, P.M.; Rogers, J.M.; Brackney, W.R.; Denison, M.S. Effects of histone deacetylase inhibitors on the Ah receptor gene promoter. Arch. Biochem. Biophys. 2000, 374, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.H. Immune regulation by microbiome metabolites. Immunology 2018, 154, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Jin, U.H.; Cheng, Y.; Park, H.; Davidson, L.A.; Callaway, E.S.; Chapkin, R.S.; Jayaraman, A.; Asante, A.; Allred, C.; Weaver, E.A.; et al. Short chain fatty acids enhance aryl hydrocarbon (Ah) responsiveness in mouse colonocytes and Caco-2 human colon cancer cells. Sci. Rep. 2017, 7, 10163. [Google Scholar] [CrossRef] [PubMed]
- Salt, J.S.; Mulcahy, G.; Kitching, R.P. Isotype-specific antibody responses to foot-and-mouth disease virus in sera and secretions of ‘carrier’and ‘non-carrier’cattle. Epidemiol. Infect. 1996, 117, 349–360. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Parida, S.; Anderson, J.; Cox, S.J.; Barnett, P.V.; Paton, D.J. Secretory IgA as an indicator of oro-pharyngeal foot-and-mouth disease virus replication and as a tool for post vaccination surveillance. Vaccine 2006, 24, 1107–1116. [Google Scholar] [CrossRef]
- Smyth, G.K. Limma: Linear models for microarray data. In Bioinformatics and Computational Biology Solutions Using R and Bioconductor; Gentleman, R., Carey, V.J., Huber, W., Irizarry, R.A., Dudoit, S., Eds.; Statistics for Biology and Health; Springer: New York, NY, USA, 2015. [Google Scholar]
| Pathway | Function | Term | p Value |
|---|---|---|---|
| GOTERM_BP | Immunity | GO:0006955~immune response | 0.007 |
| Gene expression | GO:0000184~mRNA nonsense-mediated decay | 0.039 | |
| GO:0006364~rRNA processing | 0.042 | ||
| GO:0006412~translation | 0.044 | ||
| GO:0006413~translational initiation | 0.045 | ||
| KEGG | Immunity | hsa05166: Human T-cell leukemia virus-I infection hsa04062: Chemokine signaling pathway hsa05100: Bacterial invasion of epithelial cells hsa04670: Leukocyte transendothelial migration hsa04666: Fc gamma R-mediated phagocytosis hsa04662: B cell receptor signaling pathway hsa05169: Epstein-Barr virus infection | 1.96 × 10−4 0.002 0.004 0.016 0.021 0.025 0.042 |
| Gene expression | hsa04151: PI3K-Akt signaling pathway hsa04064: NF-kappa B signaling pathway hsa04066: HIF-1 signaling pathwayhsa04310: Wnt signaling pathway | 0.030 0.043 0.044 0.047 |
| Group | Gene | ESI | p | FDR | Fold | Function |
|---|---|---|---|---|---|---|
| Transcription factors | AHR | 296 | 0.04 | 8.1 | Activated by AHR ligands | |
| ARNT | 56 | 0.99 | 1.00 | 1.0 | Dimerize with AHR and HIF1A | |
| ARNTL | 495 | 0.05 | 0.30 | 6.5 | ||
| ARNTL2 | 61 | 0.72 | 0.93 | 1.1 | ||
| HIF1A | 4537 | 0.05 | −1.8 | Activated by eATP, hypoxia, TCR | ||
| AHR target genes | B7H4 | 2468 | 0.04 | 5.0 | Immune inhibitory receptor | |
| CD8A | 1601 | 0.05 | 9.8 | CD8αα, inhibit TCR signaling | ||
| CD39 | 327 | 0.00 | 14.5 | Adenosine-mediated immune suppression | ||
| CD39_l 1 | 1029 | 0.11 | 4.5 | |||
| CYP1A1 | 176 | 0.24 | 3.1 | Metabolism of AHR ligands | ||
| CYP1A2 | 4255 | 0.31 | 3.4 | |||
| CYP1B1 | 48 | 0.03 | 2.4 | |||
| CCL20 | 2161 | 0.03 | 18.7 | Recruit Th17 to epithelia | ||
| IL6 | 74 | 0.01 | 2.5 | Th→Th17 differentiation | ||
| IL23A | 1393 | 0.07 | 9.1 | |||
| IL33 | 578 | 0.04 | 0.27 | 4.3 | ↑ 2 Treg differentiation and function | |
| STAT3 | 3206 | 0.00 | 20.3 | Th17 and Treg cell differentiation | ||
| HIF1A target genes | ACSS3 | 197 | 0.00 | 0.00 | 9.6 | ↑ Fatty acid metabolism |
| PDK1 | 153 | 0.00 | −37.6 | ↓ Pyruvate metabolism via tricarboxylic acid cycle (TCA) | ||
| PDK1_l 1 | 506 | 0.01 | 0.15 | −2.9 | ||
| Genes regulating HIF1A signaling and expression | AKT1 | 2544 | 0.06 | 2.9 | AKT signaling | |
| AKT2 | 1402 | 0.05 | 2.3 | |||
| HIF1AN | 1901 | 0.04 | 0.26 | 1.9 | HIF1A inhibitor | |
| LIMD1 | 29 | 0.05 | 1.7 | ↑ HIF1A degradation | ||
| VHL | 3998 | 0.03 | 0.22 | 2.1 | ||
| PIK3IP1 | 183 | 0.08 | 15.1 | ↓ AKT-mTOR signaling | ||
| TSC1 | 3501 | 0.04 | 2.1 | |||
| PIAS2 | 540 | 0.01 | 10.4 | Inhibitor of STATs | ||
| PIAS3 | 1536 | 0.01 | 0.12 | 3.8 | ||
| PIAS4 | 4885 | 0.01 | 0.13 | 2.0 |
| Group | Gene | ESI | p | FDR | Fold | Function |
|---|---|---|---|---|---|---|
| Canonical pathway | IKBKB/IKKβ | 318 | 0.03 | −3.2 | Predominant IKK catalytic unit | |
| IKBIP | 1973 | 0.07 | −7.5 | IKKβ interacting protein | ||
| NOD2 | 504 | 0.08 | −6.1 | Bind muramyl dipeptide | ||
| OTUB1 | 2939 | 0.07 | −3.3 | Stimulator via stabilizing c-IAP | ||
| TGFB2_OT1 | 266 | 0.00 | −8.6 | Activate NFKB RELA | ||
| IFRD2 | 14,949 | 0.03 | 2.2 | Deacetylation of RELA | ||
| IL1R2 | 1265 | 0.01 | 0.17 | 4.8 | Decoy receptor of IL1R1 | |
| LCOR | 896 | 0.00 | 36.3 | Act with PPARG to ↓ NFkB signaling Inhibit TLR signaling | ||
| LRRC33 | 89 | 0.00 | 8.1 | |||
| MAP3K2 | 2846 | 0.05 | −7.9 | MAPK signaling Inhibitor of NFKB1 and RELA Disrupt TAK1 and IKKβ interaction | ||
| NFKBIA | 25,742 | 0.01 | 2.0 | |||
| NLK | 375 | 0.01 | 17.5 | |||
| PGRN | 4870 | 0.02 | 3.8 | Inhibit TNF signaling, ↑ Treg | ||
| SIGLEC11 | 191 | 0.00 | 16.6 | Suppress LPS signaling | ||
| TRAF1 | 373 | 0.00 | 11.2 | Inhibit TLR signaling | ||
| Non-canonical pathway | TNFRSF1B | 8298 | 0.01 | 0.17 | 3.8 | TNF receptor 2 |
| MAP3K14/NIK | 2846 | 0.05 | 0.32 | 4.3 | Kinase of non-canonical pathway | |
| NFKB2/p100 | 2376 | 0.03 | 4.5 | Transcription factors of non-canonical pathway | ||
| RELB | 11,156 | 0.05 | 4.2 | |||
| TNFSF8/CD30L | 350 | 0.07 | 0.35 | 2.9 | Receptors and ligands of non-canonical pathway | |
| TNFRSF8/CD30 | 40 | 0.09 | 2.0 | |||
| LTB | 10,635 | 0.08 | 9.3 | |||
| LTBR | 4407 | 0.03 | 14.4 | |||
| CD40LG | 251 | 0.01 | 0.12 | 11.3 | ||
| CD40 | 1488 | 0.05 | 8.6 | |||
| RANKL/TNFSF11 | 163 | 0.02 | 0.21 | 3.8 | ||
| CD27/TNFRSF7 | 556 | 0.01 | 9.9 | |||
| OTUB1 | 2939 | 0.07 | −3.3 | Inhibitor via stabilizing TRAF3 |
| Gene | ESI | p | FDR | Fold |
|---|---|---|---|---|
| WNT4 | 225 | 0.05 | 5.7 | |
| WNT5A | 285 | 0.09 | 4.2 | |
| WNT7A | 107 | 0.01 | 4.2 | |
| WNT10B | 39 | 0.04 | 1.7 | |
| WNT16 | 53 | 0.00 | 6.5 | |
| WNT3 | 81 | 0.02 | 0.21 | 2.9 |
| Group | Gene | ESI | p | FDR | Fold | Biological Activity and Expressing Cells 1 |
|---|---|---|---|---|---|---|
| Cytokines | IL6 | 74 | 0.01 | 2.5 | Stimulate Th → Th17 differentiation | |
| IL16 | 3000 | 0.03 | 7.2 | ↑ CD4+ cells, ↑ immune tolerance | ||
| IL23A | 1393 | 0.07 | 9.1 | Stimulate Th → Th17 differentiation | ||
| IL34 | 178 | 0.02 | 4.4 | Mφ → M2/MDSC and Th → Treg | ||
| TNFSF15 | 313 | 0.07 | 20.8 | Activate T cells, Treg expansion | ||
| IL17A | 161 | 0.70 | 0.92 | 1.4 | Cytokines produced by Th17 cells | |
| IL17F | 227 | 0.13 | 0.47 | −2.1 | ||
| IL22 | 16 | 0.24 | 0.56 | 1.1 | ||
| IL10 | 127 | 0.95 | 0.99 | 1.1 | Immune inhibitory cytokine | |
| IL21 | 184 | 0.02 | 0.17 | 3.3 | Act with IL27 and AHR to ↑ Tr1 IL-10 family, delimit Th17 response | |
| IL24 | 2804 | 0.02 | 0.17 | 6.7 | ||
| IL33 | 578 | 0.04 | 0.27 | 4.3 | Inhibit Th17 activity | |
| IL36A | 212 | 0.01 | 0.15 | 3.7 | Synergize IL17A | |
| TGFB1 | 223 | 0.26 | 0.64 | 1.7 | ||
| TGFB2 | 151 | 0.16 | 0.52 | 2.2 | Th17, Treg, and Tr1 differentiation | |
| TGFB3 | 130 | 0.07 | 0.35 | 2.0 | ||
| (MMP9) | 871 | 0.00 | 37.5 | Activate TGFβ to ↑ tolerogenic DC/MDSC | ||
| Cytokine Receptors | ACVR1B | 793 | 0.05 | 10.2 | Stimulate Th2 and Treg differentiation | |
| ACVR2B | 108 | 0.05 | −3.9 | |||
| IL17RB | 121 | 0.00 | 15.6 | Stimulate Th2 differentiation | ||
| IL18RAP | 118 | 0.06 | 2.9 | IL-18 signaling | ||
| IL27RA | 47,894 | 0.02 | 1.9 | ↓ Th2, Th17, Treg; ↑ Th1, Tr1, ↑ CD39 | ||
| sIL10RB | 2425 | 0.06 | 12.0 | IL10 and IFNλ signaling | ||
| SIGIRR | 1700 | 0.02 | −9.2 | Inhibit signaling of IL-1 cytokines | ||
| TGFBR3 | 87 | 0.01 | 2.5 | Th17, Treg, and Tr1 differentiation | ||
| TNFRSF6B | 907 | 0.06 | 5.2 | Suppress IL17 production and FAS | ||
| TNFRSF8 | 40 | 0.09 | 2.0 | Inhibit CD8+ effector cells |
| Group | Gene | ESI | p | FDR | Fold | Biological Activity and Expressing Cells 1 |
|---|---|---|---|---|---|---|
| Chemokines | CCL3 | 907 | 0.05 | −4.5 | Recruit Mφ, NK, CD8+ T cells, neutrophils | |
| CCL11 | 1074 | 0.03 | 26.7 | Recruit eosinophils, mast cells, Th2 | ||
| CCL14 | 54 | 0.01 | 2.4 | Recruit CD4+CD146+CCR5+ Th17 cells | ||
| CCL19 | 829 | 0.01 | 0.12 | 2.9 | Recruit DC, T, and B cells via CCR7 | |
| CCL20 | 2161 | 0.03 | 18.7 | Recruit Th17, B cells, and DC to epithelia | ||
| CCL28 | 436 | 0.02 | 0.19 | 4.5 | IgA-expressing cells | |
| CXCL12 | 487 | 0.00 | 13.9 | Recruit CD8+ T cells; Th1 → Tr1, Mφ → M2 | ||
| (DPP4) | 1283 | 0.01 | 10.6 | Convert CXCL12 to antagonist Recruit B cells and Tfh cells | ||
| CXCL13 | 77 | 0.06 | 2.6 | |||
| CXCL14 | 2727 | 0.04 | 34.3 | Recruit myeloid and B cells, promote Treg | ||
| CXCL15 | 525 | 0.01 | 0.14 | −6.3 | Recruit neutrophils | |
| ELR+CXCLs 2 | 2530 | n/a | −3.2 | Recruit neutrophil > Mo, NK, CD8+ T cells | ||
| Chemokine Receptors | CCR1 | 1159 | 0.03 | 4.5 | Mo, Mφ, neutrophil, Th1, DC | |
| CCR2 | 171 | 0.01 | 0.11 | 4.4 | Mo, Mφ, Th1, iDC, basophil, NK | |
| CCR3 | 76 | 0.02 | 0.19 | 8.1 | Eosinophil > basophil, mast cell | |
| CCR5 | 153 | 0.34 | 2.2 | Mφ, Th1, NK, Treg, CD8+ T, DC, neutrophil | ||
| CCR6 | 1976 | 0.06 | 0.03 | 6.9 | Th17 > iDC, γδ T, NKT, NK, Treg, Tfh cells naive T and B, mDC, Tcm cells | |
| CCR7 | 1213 | 0.01 | 16.5 | |||
| CXCR1/2 | 311 | 0.24 | −1.5 | neutrophil > Mo, NK, CD8+ T, mast cell | ||
| CXCR4 | 7857 | 0.03 | 0.31 | 2.4 | CXCL12 and CXCL14 receptor | |
| ACKR3 | 685 | 0.10 | −4.4 | Bind and degrade CXCL12 | ||
| XCR1 | 629 | 0.05 | 0.07 | −4.0 | CD8+ dendritic cell cross-presentation |
| Group | Gene | ESI | p | FDR | Fold | Biological Activity and Expressing Cells 1 |
|---|---|---|---|---|---|---|
| CD4+ or CD8+ cells | CD4 | 58 | 0.02 | 0.19 | 3.3 | T helper cell marker |
| CD5 | 6619 | 0.09 | 3.0 | BTLA → ↑ CD5 to ↑ Treg differentiation | ||
| CD8A | 1601 | 0.05 | 9.8 | Form CD8αα dimer, high on CD4+ IEL | ||
| CD8B | 120 | 0.08 | 0.39 | −2.8 | CD8αβ, CD8+ cytotoxic T cells | |
| CD40L | 251 | 0.01 | 0.12 | 11.3 | Primarily on activated CD4+ T cells | |
| TGFBR3 | 87 | 0.01 | 2.5 | Th17, Treg, and Tr1 differentiation, Zhang | ||
| ThPOK | 3191 | 0.02 | 4.0 | CD4+ T cell transcription factor | ||
| Th17 cells | CD146 | 118 | 0.01 | 2.6 | Expressed on a Th17 subset Highly expressed in Th17 and Treg cells | |
| MIR155 | 219 | 0.00 | 8.1 | |||
| RORC | 723 | 0.03 | 0.23 | 6.3 | TH17 transcription factor Inhibit Th17 differentiation Inhibit Th17 differentiation | |
| CD69 | 268 | 0.01 | 0.13 | 2.3 | ||
| LXRA | 1717 | 0.03 | 10.1 | |||
| STAT5A | 11,302 | 0.03 | 1.8 | Inhibit Th17 differentiation | ||
| TNFRSF6B | 907 | 0.06 | 5.2 | Suppress IL17 production | ||
| Regulatory T cells | CD49B | 216 | 0.14 | 0.49 | 1.9 | Tr1 marker |
| FOXP3 | 218 | 0.34 | 0.73 | −1.1 | FOXP3+ Treg transcription factor | |
| GITR | 88 | 0.05 | 0.31 | 1.6 | TNFRSF18 on Treg cells ↑ Tr1 but ↓ Th17 differentiation | |
| IRF4 | 12,334 | 0.01 | 0.11 | 2.5 | ||
| LAG3 | 214 | 0.02 | 0.20 | 2.5 | Tr1 marker | |
| TNFRSF9 | 176 | 0.01 | 0.11 | 8.8 | Non-specific Tr1 marker | |
| ADCY4 | 1005 | 0.01 | 36.2 | Immune suppression by ↑ cAMP to activate PKA | ||
| ADCY6 | 498 | 0.01 | 0.12 | 4.7 | ||
| BTLA | 80 | 0.06 | 7.4 | Th cell inhibitory receptor | ||
| GIMAP5 | 205 | 0.02 | 0.03 | 22.4 | Immune tolerance, expressed in T cells |
| Gene | ESI | FDR | Fold | Biological Activity and Expressing Cells 1 |
|---|---|---|---|---|
| CD83 | 11,022 | 0.10 | 3.5 | Suppressive on several immune cells |
| CD300D | 154 | 0.04 | 2.7 | Macrophage suppressive receptor |
| CLEC1A | 149 | 0.04 | 9.0 | DC receptor, ↓ Th17 response |
| EMR1 | 84 | 0.06 | 2.4 | Mφ induce antigen specific Treg cells |
| MFSD6 | 2626 | 0.03 | −4.1 | MHC-I restricted killing by Mφ |
| SIGLEC11 | 191 | 0.00 | 16.6 | Suppress LPS signaling in macrophages |
| SIGLEC15 | 190 | 0.01 | 2.1 | Suppress Ag-specific T cell responses |
| TIMD4 | 5266 | 0.01 | 8.8 | Remove apoptotic and T effector cells |
| TLR2 | 100 | 0.06 | 11.9 | Promote immune tolerance |
| Group | Gene | ESI | FDR | Fold | Functions |
|---|---|---|---|---|---|
| Defensin | DEFB1 | 516 | 0.07 | −3.4 | Antimicrobial defensin |
| DEFB4B | 8363 | 0.00 | 10.8 | Anti-Gram - bacteria | |
| DEFB103A | 3069 | 0.00 | −10.7 | Anti-Gram - & + bacteria | |
| DEFB13 | 2339 | 0.74 | −1.80 | Beta-defensin 13 | |
| EDB | 2559 | 0.24 | −4.8 | Enteric beta-defensin | |
| LAP | 30,838 | 0.27 | −2.1 | Lingual antimicrobial peptide | |
| TAP | 23,613 | 0.28 | −3.2 | Tracheal antimicrobial peptide | |
| NK cell cytotoxicity | KMT2E | 443 | 0.57 | 1.6 | NCR2 ligand |
| MADD | 397 | 0.01 | 9.7 | ↓ TRAIL-induced apoptosis | |
| NID1 | 346 | 0.04 | 8.9 | Inhibit NK cell cytotoxicity |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, J.J.; Stenfeldt, C.; Bishop, E.A.; Canter, J.A.; Eschbaumer, M.; Rodriguez, L.L.; Arzt, J. Inferred Causal Mechanisms of Persistent FMDV Infection in Cattle from Differential Gene Expression in the Nasopharyngeal Mucosa. Pathogens 2022, 11, 822. https://doi.org/10.3390/pathogens11080822
Zhu JJ, Stenfeldt C, Bishop EA, Canter JA, Eschbaumer M, Rodriguez LL, Arzt J. Inferred Causal Mechanisms of Persistent FMDV Infection in Cattle from Differential Gene Expression in the Nasopharyngeal Mucosa. Pathogens. 2022; 11(8):822. https://doi.org/10.3390/pathogens11080822
Chicago/Turabian StyleZhu, James J., Carolina Stenfeldt, Elizabeth A. Bishop, Jessica A. Canter, Michael Eschbaumer, Luis L. Rodriguez, and Jonathan Arzt. 2022. "Inferred Causal Mechanisms of Persistent FMDV Infection in Cattle from Differential Gene Expression in the Nasopharyngeal Mucosa" Pathogens 11, no. 8: 822. https://doi.org/10.3390/pathogens11080822
APA StyleZhu, J. J., Stenfeldt, C., Bishop, E. A., Canter, J. A., Eschbaumer, M., Rodriguez, L. L., & Arzt, J. (2022). Inferred Causal Mechanisms of Persistent FMDV Infection in Cattle from Differential Gene Expression in the Nasopharyngeal Mucosa. Pathogens, 11(8), 822. https://doi.org/10.3390/pathogens11080822







