Selective COVID-19 Coinfections in Diabetic Patients with Concomitant Cardiovascular Comorbidities Are Associated with Increased Mortality
Abstract
:1. Introduction
2. Results
2.1. Influence of Coinfections and Comorbidities in Overall COVID-19 Case Fatality Rates
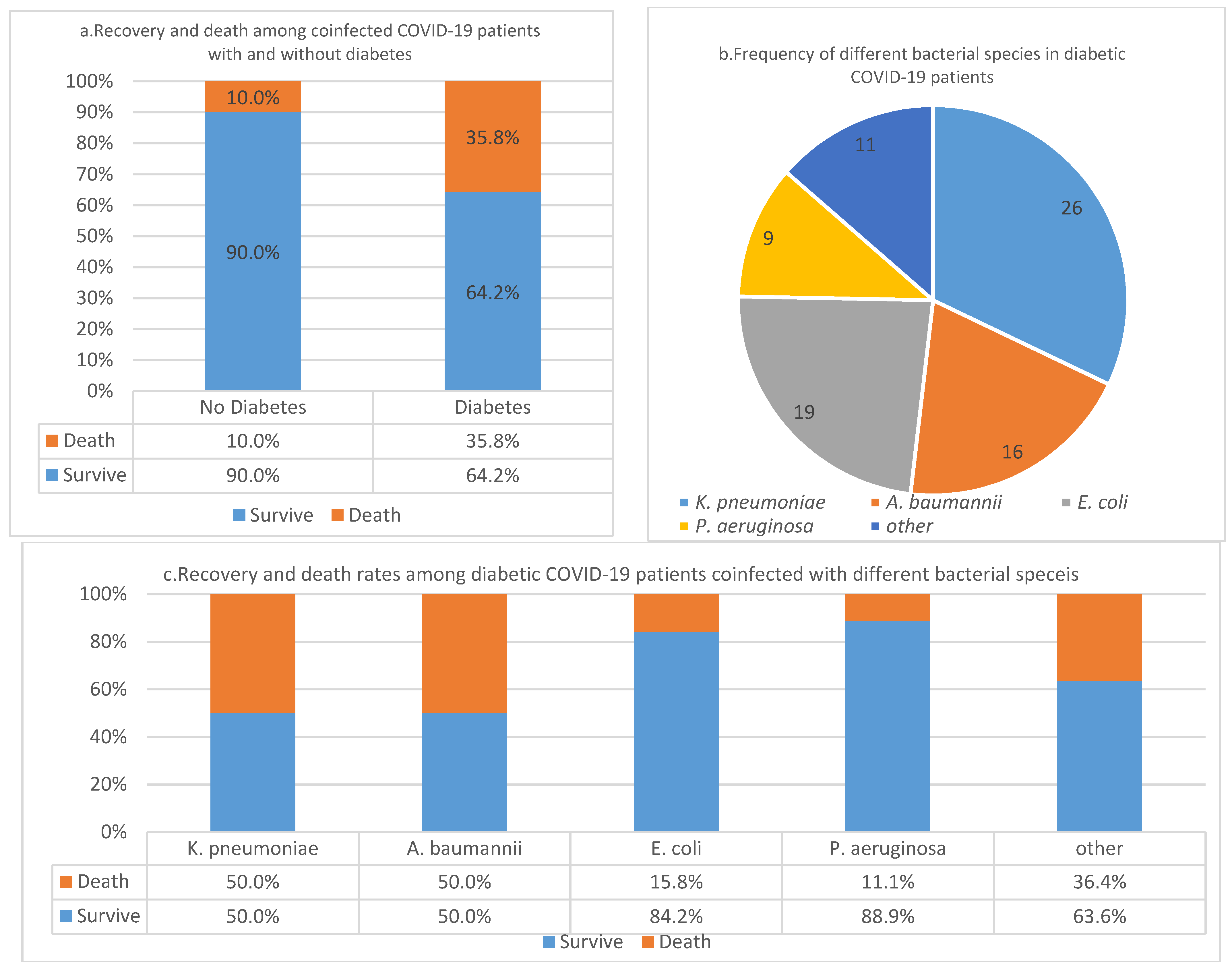
2.2. Diabetes
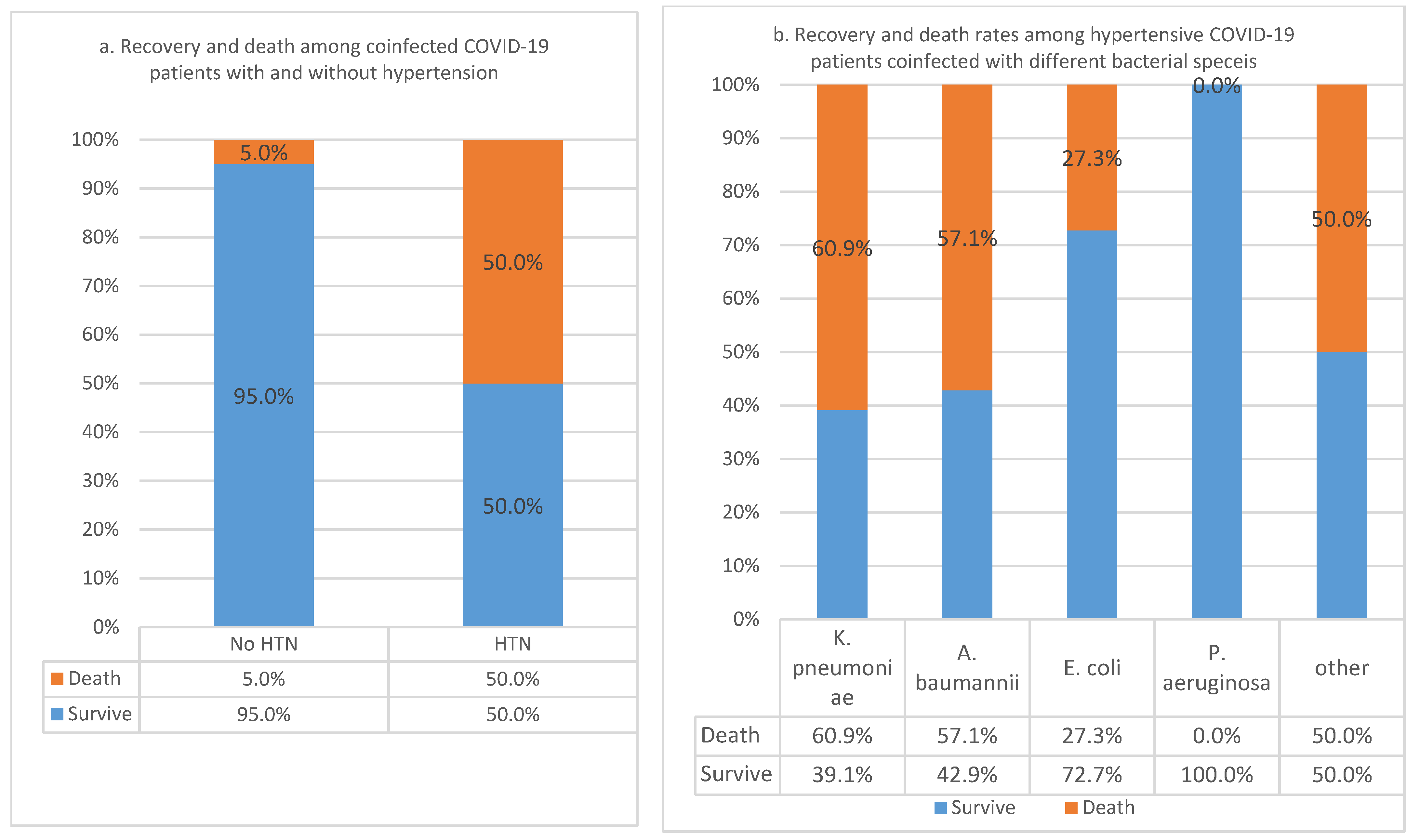
2.3. Hypertension (HTN)
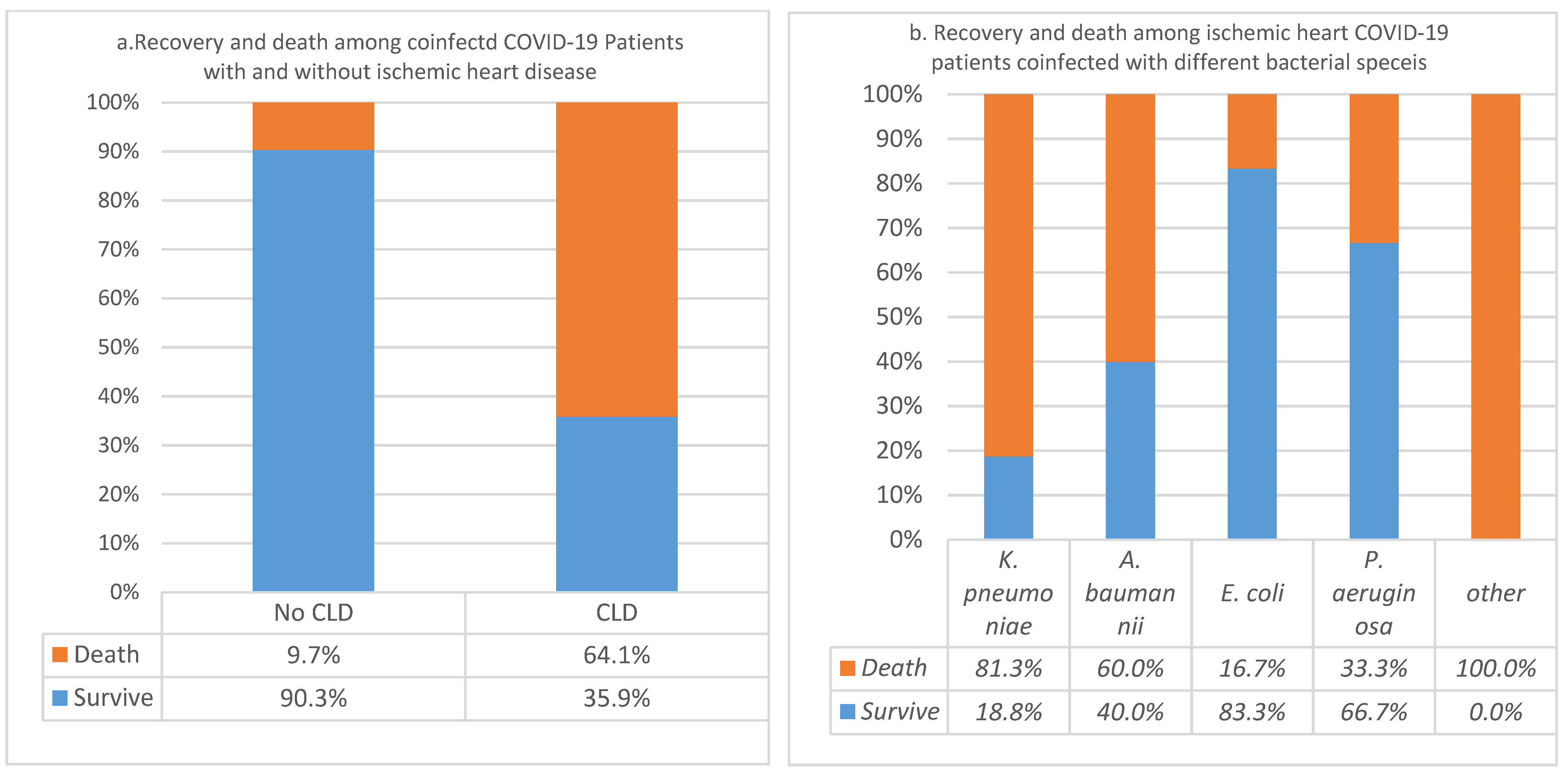
2.4. Ischemic Heart Disease (IHD)
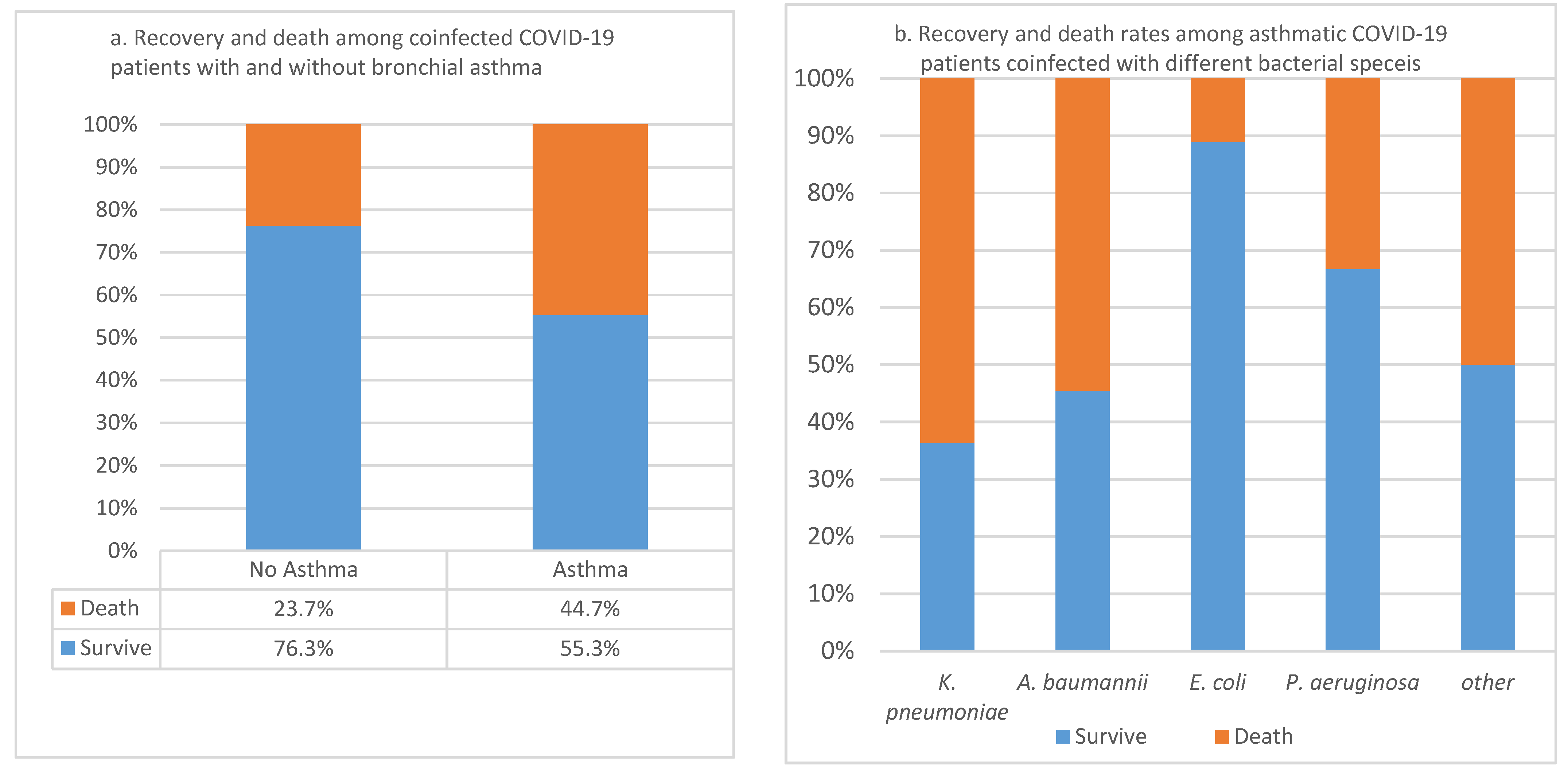
2.5. Bronchial Asthma
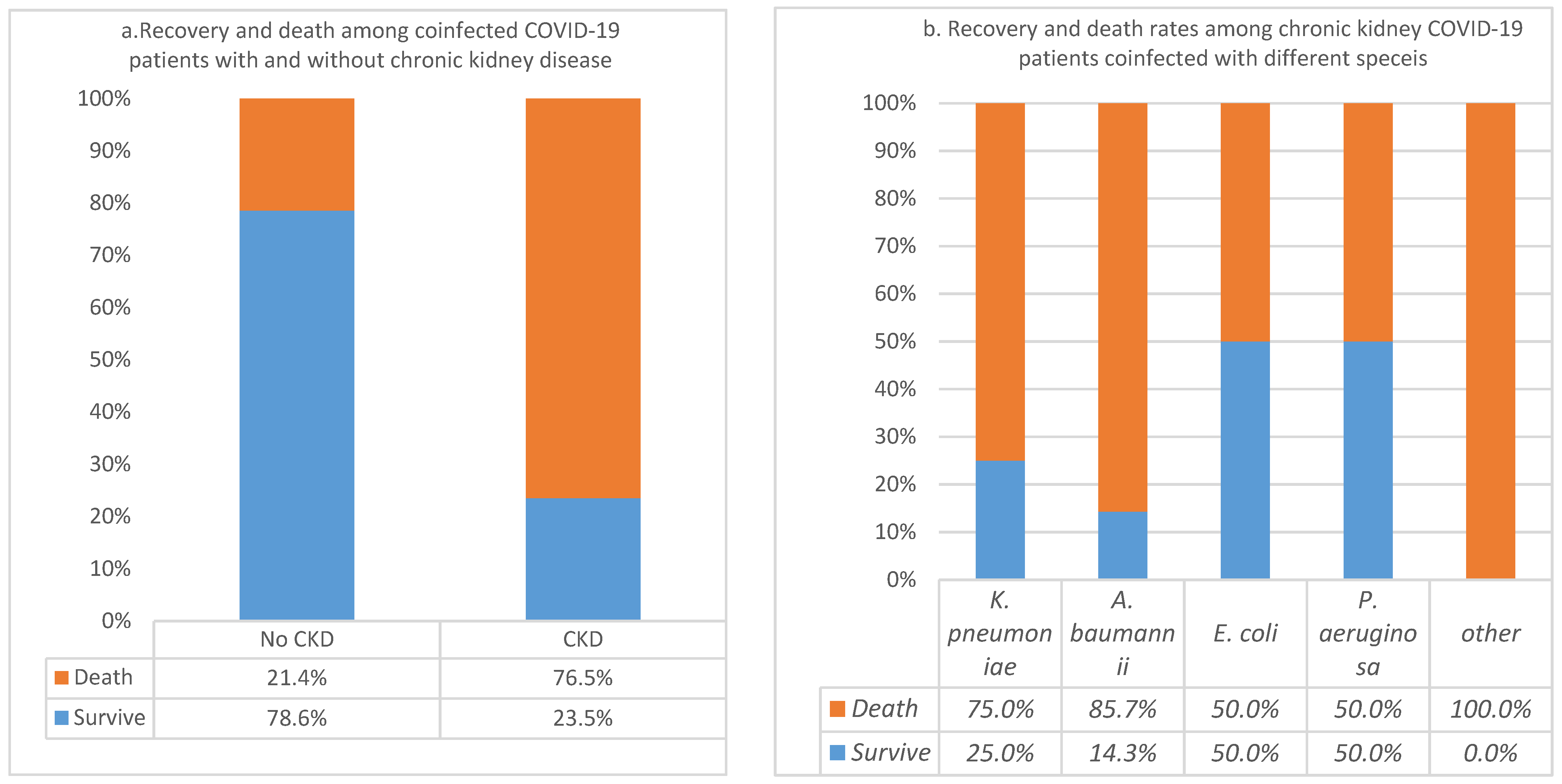
2.6. Chronic Kidney Disease (CKD)
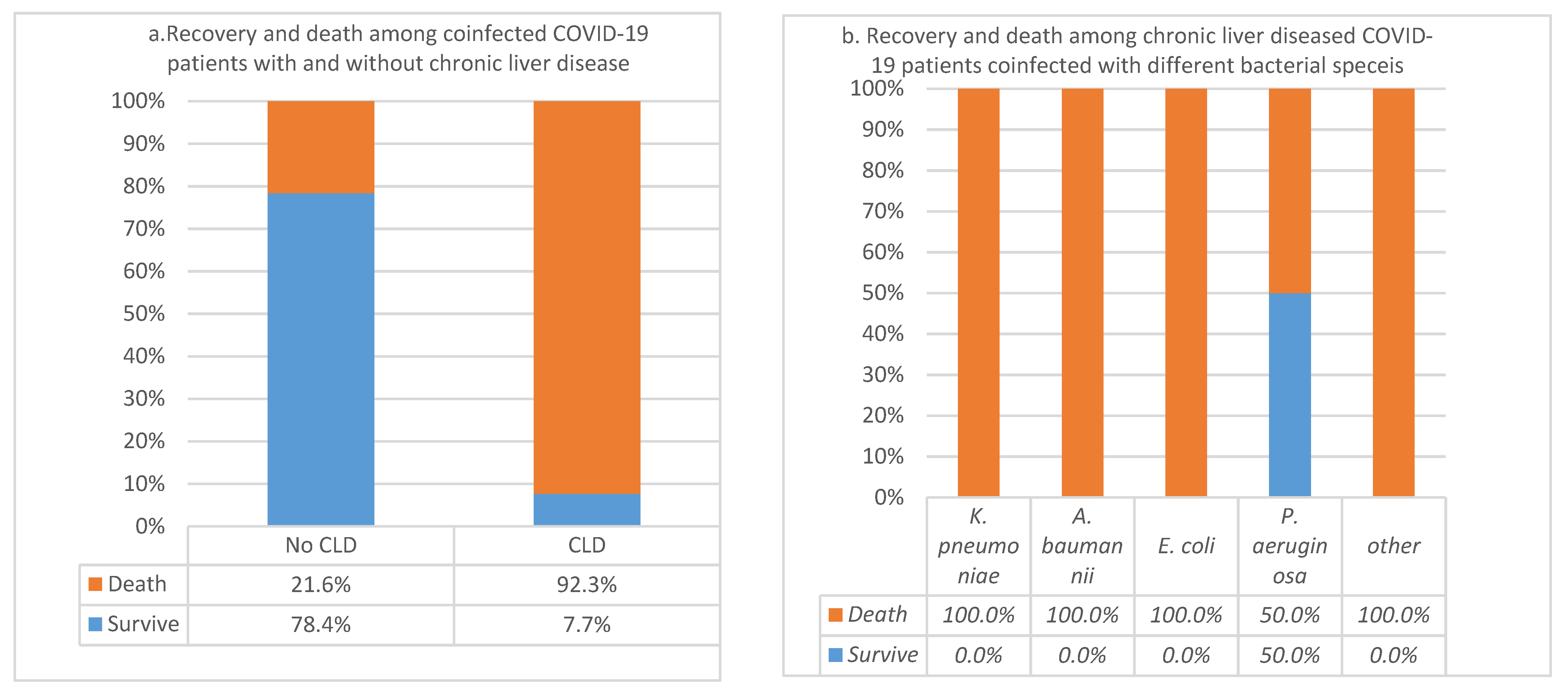
2.7. Chronic Liver Disease CLD
3. Discussion
4. Materials and Methods
4.1. Study Descriptions, Hospital, Data Acquisitions, and Statistical Analysis
4.2. Work Environment
4.3. Diagnostic Clinical Microbiological Data
4.4. Standard Definitions of Resistances
4.5. Criteria for Sampling Coinfection and/or Superinfection
4.6. Statistical Analysis of the Data
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Torjesen, I. COVID-19: Omicron May Be More Transmissible than Other Variants and Partly Resistant to Existing Vaccines, Scientists Fear. BMJ 2021, 375, n2943. [Google Scholar] [CrossRef] [PubMed]
- Said, K.B.; Alsolami, A.; Fathuldeen, A.; Alshammari, F.; Alhiraabi, W.; Alaamer, S.; Alrmaly, H.; Aldamadi, F.; Aldakheel, D.F.; Moussa, S.; et al. In-Silico Pangenomics of SARS-CoV-2 Isolates Reveal Evidence for Subtle Adaptive Expression Strategies, Continued Clonal Evolution, and Sub-Clonal Emergences, Despite Genome Stability. Microbiol. Res. 2021, 12, 204–233. [Google Scholar] [CrossRef]
- Scully, M.; Singh, D.; Lown, R.; Poles, A.; Solomon, T.; Levi, M.; Goldblatt, D.; Kotoucek, P.; Thomas, W.; Lester, W. Pathologic Antibodies to Platelet Factor 4 after ChAdOx1 NCoV-19 Vaccination. N. Engl. J. Med. 2021, 384, 2202–2211. [Google Scholar] [CrossRef]
- Greinacher, A.; Thiele, T.; Warkentin, T.E.; Weisser, K.; Kyrle, P.A.; Eichinger, S. Thrombotic Thrombocytopenia after ChAdOx1 NCov-19 Vaccination. N. Engl. J. Med. 2021, 384, 2092–2101. [Google Scholar] [CrossRef] [PubMed]
- McCrae, K.R. Thrombotic Thrombocytopenia Due to SARS-CoV-2 Vaccination. Clevel. Clin. J. Med. 2021, 33. [Google Scholar] [CrossRef] [PubMed]
- Welsh, K.J.; Baumblatt, J.; Chege, W.; Goud, R.; Nair, N. Thrombocytopenia Including Immune Thrombocytopenia after Receipt of MRNA COVID-19 Vaccines Reported to the Vaccine Adverse Event Reporting System (VAERS). Vaccine 2021, 39, 3329–3332. [Google Scholar] [CrossRef] [PubMed]
- Saudagar, V.; Patil, S.; Goh, S.; Pothiawala, S. Vigilance Regarding Immune Thrombocytopenic Purpura after COVID-19 Vaccine. Ir. J. Med. Sci. 2021, 191, 919–920. [Google Scholar] [CrossRef] [PubMed]
- Aran, D.; Beachler, D.C.; Lanes, S.; Overhage, J.M. Prior Presumed Coronavirus Infection Reduces COVID-19 Risk: A Cohort Study. J. Infect. 2020, 81, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Calcagno, A.; Ghisetti, V.; Burdino, E.; Trunfio, M.; Allice, T.; Boglione, L.; Bonora, S.; di Perri, G. Co-Infection with Other Respiratory Pathogens in COVID-19 Patients. Clin. Microbiol. Infect. 2021, 27, 297–298. [Google Scholar] [CrossRef] [PubMed]
- Boschiero, M.N.; Duarte, A.; Palamim, C.V.C.; Alvarez, A.E.; Mauch, R.M.; Marson, F.A.L. Frequency of Respiratory Pathogens Other than SARS-CoV-2 Detected during COVID-19 Testing. Diagn. Microbiol. Infect. Dis. 2022, 102, 115576. [Google Scholar] [CrossRef] [PubMed]
- Langford, B.J.; So, M.; Raybardhan, S.; Leung, V.; Westwood, D.; MacFadden, D.R.; Soucy, J.P.R.; Daneman, N. Bacterial Co-Infection and Secondary Infection in Patients with COVID-19: A Living Rapid Review and Meta-Analysis. Clin. Microbiol. Infect. 2020, 26, 1622–1629. [Google Scholar] [CrossRef]
- Lai, C.C.; Wang, C.Y.; Hsueh, P.R. Co-Infections among Patients with COVID-19: The Need for Combination Therapy with Non-Anti-SARS-CoV-2 Agents? J. Microbiol. Immunol. Infect. 2020, 53, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Spoto, S.; Valeriani, E.; Riva, E.; de Cesaris, M.; Tonini, G.; Vincenzi, B.; Locorriere, L.; Anguissola, G.B.; Pantano, A.L.; Brando, E.; et al. A Staphylococcus aureus Coinfection on a COVID-19 Pneumonia in a Breast Cancer Patient. Int. J. Gen. Med. 2020, 13, 729–733. [Google Scholar] [CrossRef]
- Genné, D.; Rossel, M.; Sarr, A.; Battilotti, F.; Rais, O.; Rego, R.O.M.; Voordouw, M.J. Competition between Strains of Borrelia afzelii in the Host Tissues and Consequences for Transmission to Ticks. ISME J. 2021, 15, 2390–2400. [Google Scholar] [CrossRef] [PubMed]
- Gandra, S.; Ram, S.; Levitz, S.M. The “Black Fungus” in India: The Emerging Syndemic of COVID-19-Associated Mucormycosis. Ann. Intern. Med. 2021, 174, 1301–1302. [Google Scholar] [CrossRef] [PubMed]
- Contou, D.; Claudinon, A.; Pajot, O.; Micaëlo, M.; Longuet Flandre, P.; Dubert, M.; Cally, R.; Logre, E.; Fraissé, M.; Mentec, H.; et al. Bacterial and Viral Co-Infections in Patients with Severe SARS-CoV-2 Pneumonia Admitted to a French ICU. Ann. Intensive Care 2020, 10, 119. [Google Scholar] [CrossRef]
- Alhazzani, W.; Møller, M.H.; Arabi, Y.M.; Loeb, M.; Gong, M.N.; Fan, E.; Oczkowski, S.; Levy, M.M.; Derde, L.; Dzierba, A.; et al. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). Crit. Care Med. 2020, 48, E440–E469. [Google Scholar] [CrossRef] [PubMed]
- Acharya, D.; Lee, K.; Lee, D.S.; Lee, Y.S.; Moon, S.S. Mortality Rate and Predictors of Mortality in Hospitalized COVID-19 Patients with Diabetes. Healthcare 2020, 8, 338. [Google Scholar] [CrossRef] [PubMed]
- Rastad, H.; Karim, H.; Ejtahed, H.S.; Tajbakhsh, R.; Noorisepehr, M.; Babaei, M.; Azimzadeh, M.; Soleimani, A.; Inanloo, S.H.; Shafiabadi Hassani, N.; et al. Risk and Predictors of In-Hospital Mortality from COVID-19 in Patients with Diabetes and Cardiovascular Disease. Diabetol. Metab. Syndr. 2020, 12, 57. [Google Scholar] [CrossRef] [PubMed]
- Alguwaihes, A.M.; Al-Sofiani, M.E.; Megdad, M.; Albader, S.S.; Alsari, M.H.; Alelayan, A.; Alzahrani, S.H.; Sabico, S.; Al-Daghri, N.M.; Jammah, A.A. Diabetes and COVID-19 among Hospitalized Patients in Saudi Arabia: A Single-Centre Retrospective Study. Cardiovasc. Diabetol. 2020, 19, 205. [Google Scholar] [CrossRef]
- Sheshah, E.; Sabico, S.; Albakr, R.M.; Sultan, A.A.; Alghamdi, K.S.; al Madani, K.; Alotair, H.A.; Al-Daghri, N.M. Prevalence of Diabetes, Management and Outcomes among COVID-19 Adult Patients Admitted in a Specialized Tertiary Hospital in Riyadh, Saudi Arabia. Diabetes Res. Clin. Pract. 2021, 172, 108538. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Shi, Z.; Zhang, Y.; Wang, C.; do Vale Moreira, N.C.; Zuo, H.; Hussain, A. Comorbid Diabetes and the Risk of Disease Severity or Death among 8807 COVID-19 Patients in China: A Meta-Analysis. Diabetes Res. Clin. Pract. 2020, 166, 108346. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Arora, A.; Sharma, P.; Anikhindi, S.A.; Bansal, N.; Singla, V.; Khare, S.; Srivastava, A. Is Diabetes Mellitus Associated with Mortality and Severity of COVID-19? A Meta-Analysis. Diabetes Metab. Syndr. 2020, 14, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Singh, R. Letter to the Editor in Response to the Article: “Is Diabetes Mellitus Associated with Mortality and Severity of COVID-19? A Meta-Analysis (Kumar et al.)”. Diabetes Metab. Syndr. 2020, 14, 937. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.E.; Bhattacharyya, R.; Miller, A.L. Diabetes Mellitus Increases the Risk of Hospital Mortality in Patients with COVID-19: Systematic Review with Meta-Analysis. Medicine 2020, 99, e22439. [Google Scholar] [CrossRef] [PubMed]
- van Niekerk, G.; van der Merwe, M.; Engelbrecht, A.M. Diabetes and Susceptibility to Infections: Implication for COVID-19. Immunology 2021, 164, 467–475. [Google Scholar] [CrossRef]
- Roganović, J. Downregulation of MicroRNA-146a in Diabetes, Obesity and Hypertension May Contribute to Severe COVID-19. Med. Hypotheses 2021, 146, 110448. [Google Scholar] [CrossRef] [PubMed]
- Abu-Farha, M.; Al-Mulla, F.; Thanaraj, T.A.; Kavalakatt, S.; Ali, H.; Abdul Ghani, M.; Abubaker, J. Impact of Diabetes in Patients Diagnosed With COVID-19. Front. Immunol. 2020, 11, 576818. [Google Scholar] [CrossRef] [PubMed]
- Petty, L.A.; Flanders, S.A.; Vaughn, V.M.; Ratz, D.; O’Malley, M.; Malani, A.N.; Washer, L.; Kim, T.; Kocher, K.E.; Kaatz, S.; et al. Risk Factors and Outcomes Associated with Community-Onset and Hospital-Acquired Coinfection in Patients Hospitalized for Coronavirus Disease 2019 (COVID-19): A Multihospital Cohort Study. Infect. Control. Hosp. Epidemiol. 2021, 1–10. [Google Scholar] [CrossRef]
- Adapa, S.; Chenna, A.; Balla, M.; Merugu, G.P.; Koduri, N.M.; Daggubati, S.R.; Gayam, V.; Naramala, S.; Konala, V.M. COVID-19 Pandemic Causing Acute Kidney Injury and Impact on Patients with Chronic Kidney Disease and Renal Transplantation. J. Clin. Med. Res. 2020, 12, 352–361. [Google Scholar] [CrossRef]
- Naicker, S.; Yang, C.W.; Hwang, S.J.; Liu, B.C.; Chen, J.H.; Jha, V. The Novel Coronavirus 2019 Epidemic and Kidneys. Kidney Int. 2020, 97, 824. [Google Scholar] [CrossRef]
- Ma, Y.; Diao, B.; Lv, X.; Zhu, J.; Liang, W.; Liu, L.; Bu, W.; Cheng, H.; Zhang, S.; Yang, L.; et al. 2019 Novel Coronavirus Disease in Hemodialysis (HD) Patients: Report from One HD Center in Wuhan, China. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors Associated with COVID-19-Related Death Using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef]
- Ioannou, G.N.; Locke, E.; Green, P.; Berry, K.; O’Hare, A.M.; Shah, J.A.; Crothers, K.; Eastment, M.C.; Dominitz, J.A.; Fan, V.S. Risk Factors for Hospitalization, Mechanical Ventilation, or Death Among 10 131 US Veterans With SARS-CoV-2 Infection. JAMA Netw. Open 2020, 3, e2022310. [Google Scholar] [CrossRef] [PubMed]
- Pirola, C.J.; Sookoian, S. SARS-CoV-2 Virus and Liver Expression of Host Receptors: Putative Mechanisms of Liver Involvement in COVID-19. Liver Int. Off. J. Int. Assoc. Study Liver 2020, 40, 2038–2040. [Google Scholar] [CrossRef] [PubMed]
- de Smet, V.; Verhulst, S.; van Grunsven, L.A. Single Cell RNA Sequencing Analysis Did Not Predict Hepatocyte Infection by SARS-CoV-2. J. Hepatol. 2020, 73, 993–995. [Google Scholar] [CrossRef] [PubMed]
- Brann, D.H.; Tsukahara, T.; Weinreb, C.; Lipovsek, M.; van den Berge, K.; Gong, B.; Chance, R.; Macaulay, I.C.; Chou, H.J.; Fletcher, R.B.; et al. Non-Neuronal Expression of SARS-CoV-2 Entry Genes in the Olfactory System Suggests Mechanisms Underlying COVID-19-Associated Anosmia. Sci. Adv. 2020, 6. [Google Scholar] [CrossRef] [PubMed]
- Butowt, R.; von Bartheld, C.S. Anosmia in COVID-19: Underlying Mechanisms and Assessment of an Olfactory Route to Brain Infection. Neurosci. Rev. J. Bringing Neurobiol. Neurol. Psychiatry 2020, 27, 582–603. [Google Scholar] [CrossRef]
- Cantuti-Castelvetri, L.; Ojha, R.; Pedro, L.D.; Djannatian, M.; Franz, J.; Kuivanen, S.; van der Meer, F.; Kallio, K.; Kaya, T.; Anastasina, M.; et al. Neuropilin-1 Facilitates SARS-CoV-2 Cell Entry and Infectivity. Science 2020, 370, 856–860. [Google Scholar] [CrossRef] [PubMed]
- Desforges, M.; le Coupanec, A.; Stodola, J.K.; Meessen-Pinard, M.; Talbot, P.J. Human Coronaviruses: Viral and Cellular Factors Involved in Neuroinvasiveness and Neuropathogenesis. Virus Res. 2014, 194, 145–158. [Google Scholar] [CrossRef] [PubMed]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial Cell Infection and Endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Cox, M.J.; Loman, N.; Bogaert, D.; O’Grady, J. Co-Infections: Potentially Lethal and Unexplored in COVID-19. Lancet Microbe 2020, 1, e11. [Google Scholar] [CrossRef]
- Tee, L.Y.; Alhamid, S.M.; Tan, J.L.; di Oo, T.; Chien, J.; Galinato, P.; Tan, S.Y.; Humaira, S.; Fong, R.K.C.; Puar, T.H.; et al. COVID-19 and Undiagnosed Pre-Diabetes or Diabetes Mellitus Among International Migrant Workers in Singapore. Front. Public Health 2020, 8, 584249. [Google Scholar] [CrossRef]
- Logette, E.; Lorin, C.; Favreau, C.; Oshurko, E.; Coggan, J.S.; Casalegno, F.; Sy, M.F.; Monney, C.; Bertschy, M.; Delattre, E.; et al. A Machine-Generated View of the Role of Blood Glucose Levels in the Severity of COVID-19. Front. Public Health 2021, 9, 695139. [Google Scholar] [CrossRef]
- Al-Rubeaan, K.; Almashouq, M.K.; Youssef, A.M.; AlQumaidi, H.; al Derwish, M.; Ouizi, S.; Al-Shehri, K.; Masoodi, S.N. All-Cause Mortality among Diabetic Foot Patients and Related Risk Factors in Saudi Arabia. PLoS ONE 2017, 12, e0188097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brownrigg, J.R.W.; Davey, J.; Holt, P.J.; Davis, W.A.; Thompson, M.M.; Ray, K.K.; Hinchliffe, R.J. The Association of Ulceration of the Foot with Cardiovascular and All-Cause Mortality in Patients with Diabetes: A Meta-Analysis. Diabetologia 2012, 55, 2906–2912. [Google Scholar] [CrossRef]
- Chammas, N.K.; Hill, R.L.R.; Edmonds, M.E. Increased Mortality in Diabetic Foot Ulcer Patients: The Significance of Ulcer Type. J. Diabetes Res. 2016, 2016, 2879809. [Google Scholar] [CrossRef] [Green Version]
- Al-Rubeaan, K.; Youssef, A.M.; Ibrahim, H.M.; Al-Sharqawi, A.H.; AlQumaidi, H.; AlNaqeb, D.; Aburisheh, K.H. All-Cause Mortality and Its Risk Factors among Type 1 and Type 2 Diabetes Mellitus in a Country Facing Diabetes Epidemic. Diabetes Res. Clin. Pract. 2016, 118, 130–139. [Google Scholar] [CrossRef]
- Abbott, C.A.; Garrow, A.P.; Carrington, A.L.; Morris, J.; van Ross, E.R.; Boulton, A.J. Foot Ulcer Risk Is Lower in South-Asian and African-Caribbean Compared with European Diabetic Patients in the UK: The North-West Diabetes Foot Care Study. Diabetes Care 2005, 28, 1869–1875. [Google Scholar] [CrossRef] [Green Version]
- Paczosa, M.K.; Mecsas, J. Klebsiella pneumoniae: Going on the Offense with a Strong Defense. Microbiol. Mol. Biol. Rev. MMBR 2016, 80, 629. [Google Scholar] [CrossRef] [Green Version]
- Hu, X.; Lee, J.S.; Pianosi, P.T.; Ryu, J.H. Aspiration-Related Pulmonary Syndromes. Chest 2015, 147, 815–823. [Google Scholar] [CrossRef] [PubMed]
- Chusri, S.; Chongsuvivatwong, V.; Silpapojakul, K.; Singkhamanan, K.; Hortiwakul, T.; Charernmak, B.; Doi, Y. Clinical Characteristics and Outcomes of Community and Hospital-Acquired Acinetobacter baumannii Bacteremia. J. Microbiol. Immunol. Infect. 2019, 52, 796–806. [Google Scholar] [CrossRef] [PubMed]
- Dijkshoorn, L.; Nemec, A.; Seifert, H. An Increasing Threat in Hospitals: Multidrug-Resistant Acinetobacter baumannii. Nat. Rev. Microbiol. 2007, 5, 939–951. [Google Scholar] [CrossRef] [PubMed]
- Rangel, K.; Chagas, T.P.G.; De-Simone, S.G. Acinetobacter baumannii Infections in Times of COVID-19 Pandemic. Pathogens 2021, 10, 1006. [Google Scholar] [CrossRef] [PubMed]
- Nebreda-Mayoral, T.; Miguel-Gómez, M.A.; March-Rosselló, G.A.; Puente-Fuertes, L.; Cantón-Benito, E.; Martínez-García, A.M.; Muñoz-Martín, A.B.; Orduña-Domingo, A. Bacterial/Fungal Infection in Hospitalized Patients with COVID-19 in a Tertiary Hospital in the Community of Castilla y León, Spain. Enferm. Infecc. Y Microbiol. Clin. 2020. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.; Cockerill, F., III; Eliopoulos, G.; Jenkins, S.; Lewis, I.I.J.; Limbago, B.; Nicolau, D.; Patel, R.; Powell, M.; Richter, S.; et al. Performance Standards for Antimicrobial Susceptibility Testing, 26th ed.; Clinical Laboratory Standards Institute: Wayne, PA, USA, 2016; pp. 52–60. [Google Scholar]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-Resistant, Extensively Drug-Resistant and Pandrug-Resistant Bacteria: An International Expert Proposal for Interim Standard Definitions for Acquired Resistance. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC; Ncezid; DHQP. Bloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-Central Line Associated Bloodstream Infection). National Healthcare Safety Network 2022; pp. BSI 4-1–BSI 4-48. Available online: https://www.cdc.gov/nhsn/pdfs/pscmanual/4psc_clabscurrent.pdf (accessed on 12 January 2022).
| Deaths in Total and Diabetic Coinfections | Concomitant Heart Comorbidities | Supportive and Clinical Characteristics | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Major coinfecting bacteria | Total Death per major coinfections | Deaths per coinfections with diabetes | Asthma | Hypertension | Chronic Kidney Diseases | Chronic Liver Diseases | Heart Failure | Ischemic Heart Disease | Patient Age Range | Infilt CXR? | Steps in High Oxygen Intervention Requirments before Death | ICU | LALC | ||
| 0–20 Year Old | 21– 49 Year Old | Seniors >50 Year | |||||||||||||
| K. pneumoniae (MDR) | 14 | 13 (93%) | 7 (50%) | 13 (93%) | 3 (21%) | 5 (36%) | 2 (14%) | 12 (86%) | 0 | 1 | 13 | Yes | All were initially ventilated, then required intubation and high oxygenation (>4 L on avg) | Yes | <5 |
| A. baumannii (XDR) | 11 | 8 (73%) | 5 (45.5%) | 7 (64%) | 5 (45.5%) | 2 (18%) | 0 | 6 (54.5% | 0 | 2 | 9 | Yes | All, except one, required initial ventilation, then required intubation and high oxygenation (>4 L on avg) | Yes | <5 |
| E. coli (MDR) | 3 | 3 | 1 | 3 | 1 | 1 | 0 | 1 | 0 | 0 | 3 | Yes | Only these three patients were intubated with high oxygenation before death | Yes | <5 |
| Totals | 28 | 24 (85.7%) | 13 (46.4%) | 23 (82%) | 9 (32%) | 8 (28.5%) | 2 (7%) | 19 (68%) | 0 | 3 (10.7%) | 25 (89%) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Said, K.B.; Alsolami, A.; Alshammari, F.; Alreshidi, F.S.; Fathuldeen, A.; Alrashid, F.; Bashir, A.I.; Osman, S.; Aboras, R.; Alshammari, A.; et al. Selective COVID-19 Coinfections in Diabetic Patients with Concomitant Cardiovascular Comorbidities Are Associated with Increased Mortality. Pathogens 2022, 11, 508. https://doi.org/10.3390/pathogens11050508
Said KB, Alsolami A, Alshammari F, Alreshidi FS, Fathuldeen A, Alrashid F, Bashir AI, Osman S, Aboras R, Alshammari A, et al. Selective COVID-19 Coinfections in Diabetic Patients with Concomitant Cardiovascular Comorbidities Are Associated with Increased Mortality. Pathogens. 2022; 11(5):508. https://doi.org/10.3390/pathogens11050508
Chicago/Turabian StyleSaid, Kamaleldin B., Ahmed Alsolami, Fawwaz Alshammari, Fayez Saud Alreshidi, Anas Fathuldeen, Fawaz Alrashid, Abdelhafiz I. Bashir, Sara Osman, Rana Aboras, Abdulrahman Alshammari, and et al. 2022. "Selective COVID-19 Coinfections in Diabetic Patients with Concomitant Cardiovascular Comorbidities Are Associated with Increased Mortality" Pathogens 11, no. 5: 508. https://doi.org/10.3390/pathogens11050508
APA StyleSaid, K. B., Alsolami, A., Alshammari, F., Alreshidi, F. S., Fathuldeen, A., Alrashid, F., Bashir, A. I., Osman, S., Aboras, R., Alshammari, A., Alshammari, T., Alharbi, S. F., & on behalf of the Ha’il COM Research Unit Group. (2022). Selective COVID-19 Coinfections in Diabetic Patients with Concomitant Cardiovascular Comorbidities Are Associated with Increased Mortality. Pathogens, 11(5), 508. https://doi.org/10.3390/pathogens11050508






