A Three-Case Series of Thrombotic Deaths in Patients over 50 with Comorbidities Temporally after modRNA COVID-19 Vaccination
Abstract
:1. Introduction
2. Case Series
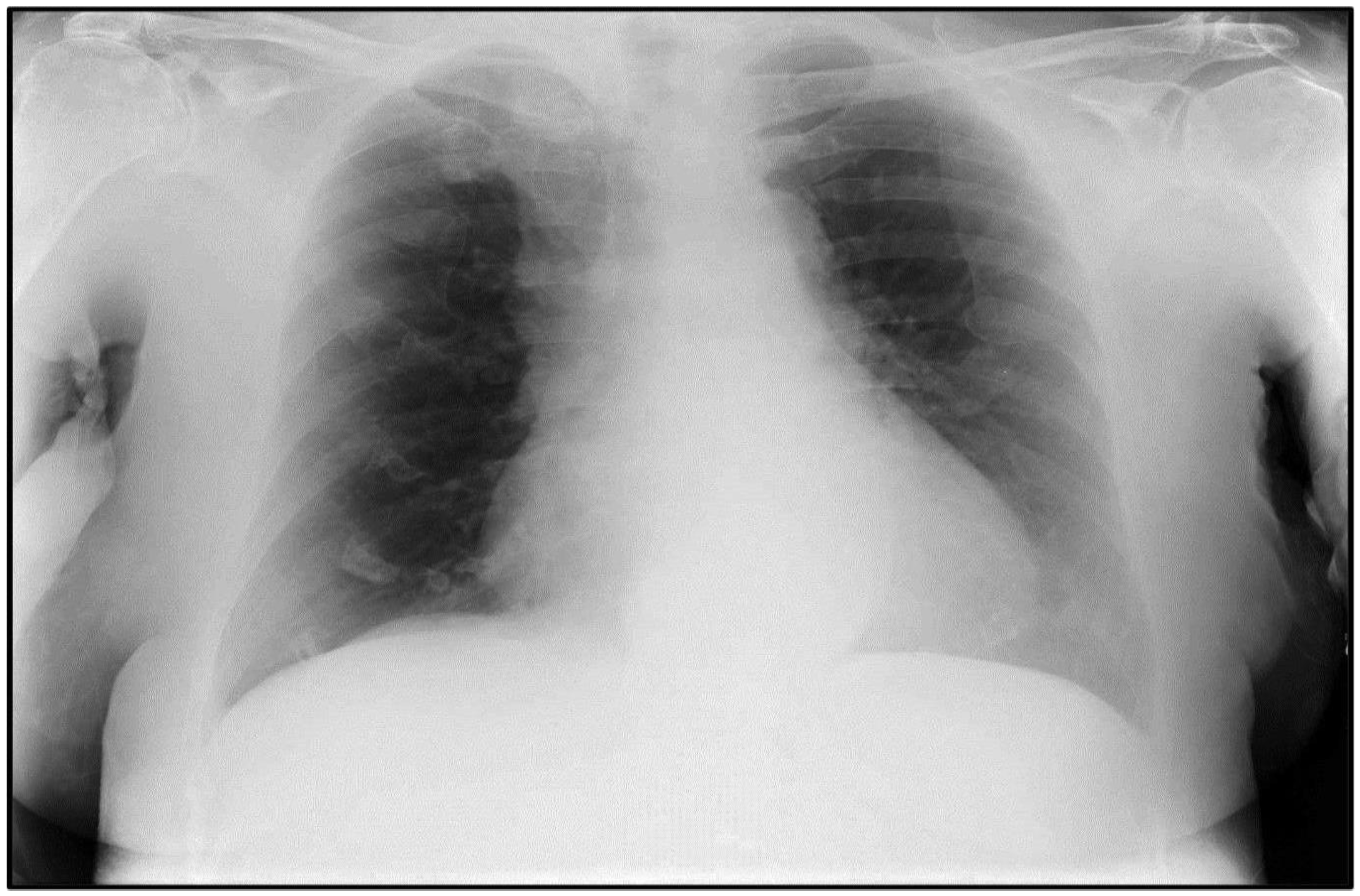
2.1. Case #1
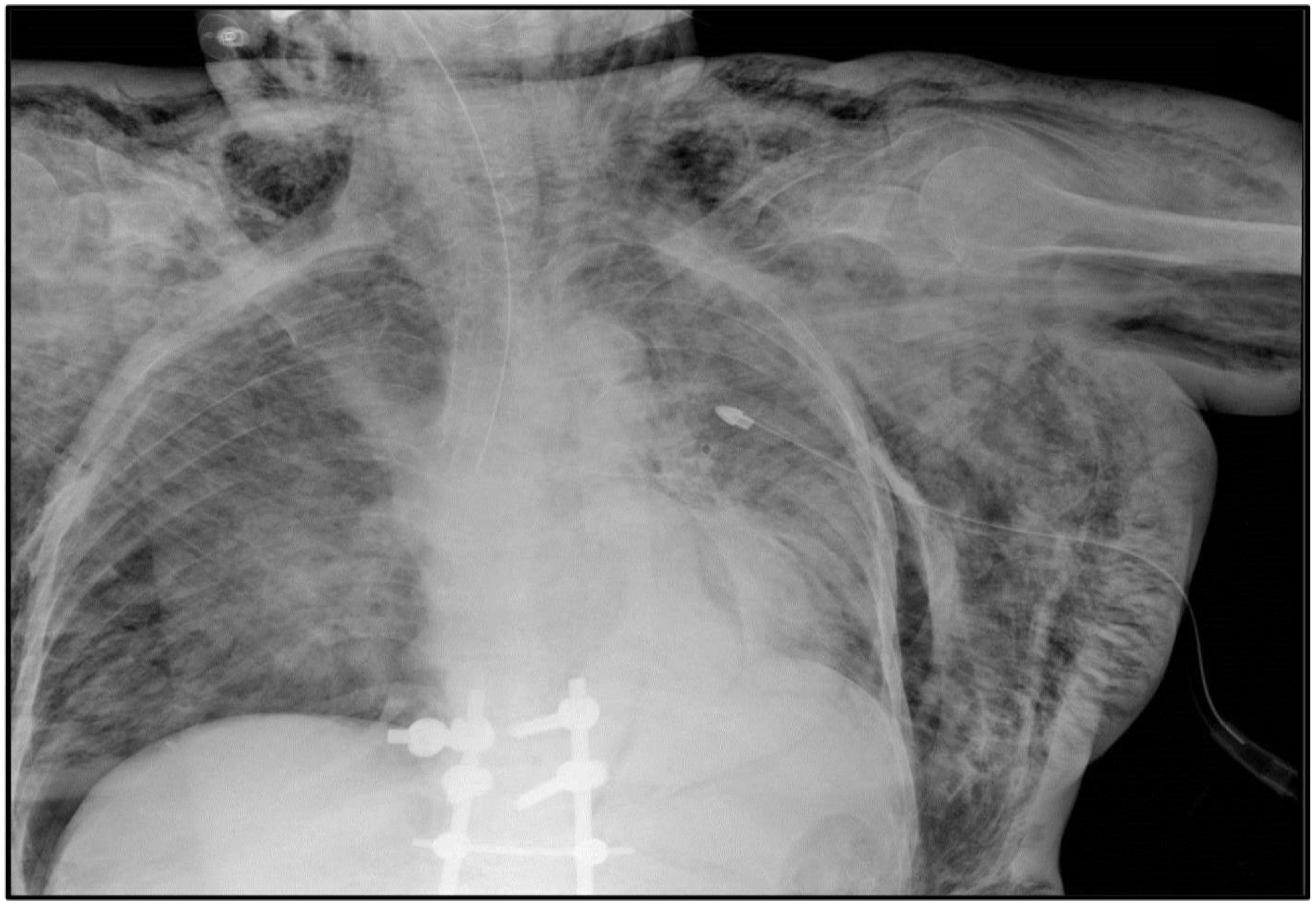
2.2. Case #2
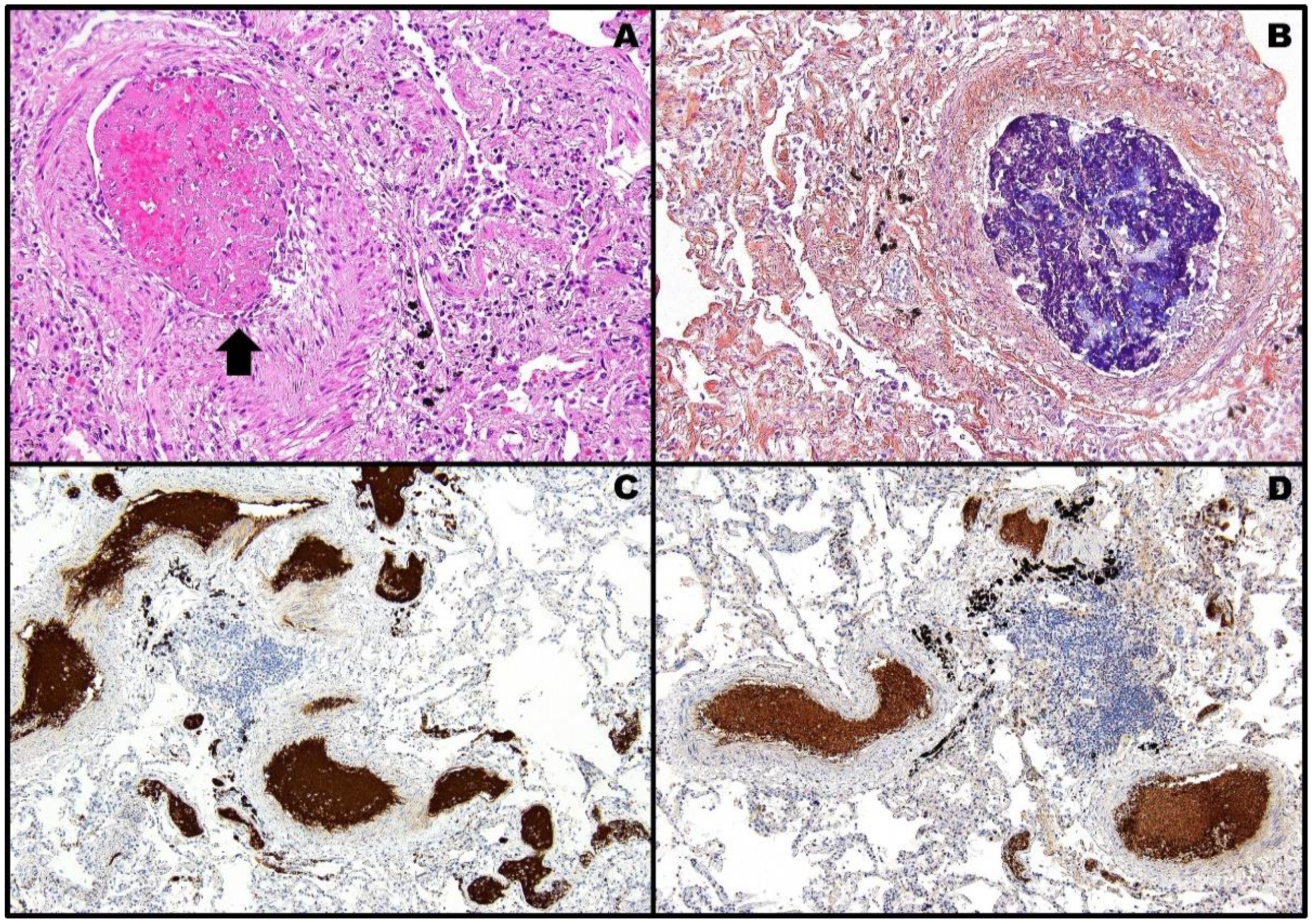
2.3. Case #3
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roncati, L.; Roncati, M. Emergency use authorization (EUA), conditional marketing authorization (CMA), and the precautionary principle at the time of COVID-19 pandemic. J. Public Health Policy 2021, 42, 518–521. [Google Scholar] [CrossRef]
- Greinacher, A.; Thiele, T.; Warkentin, T.E.; Weisser, K.; Kyrle, P.A.; Eichinger, S. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N. Engl. J. Med. 2021, 384, 2092–2101. [Google Scholar] [CrossRef] [PubMed]
- Schultz, N.H.; Sørvoll, I.H.; Michelsen, A.E.; Munthe, L.A.; Lund-Johansen, F.; Ahlen, M.T.; Wiedmann, M.; Aamodt, A.H.; Skattør, T.H.; Tjønnfjord, G.E.; et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N. Engl. J. Med. 2021, 384, 2124–2130. [Google Scholar] [CrossRef] [PubMed]
- Scully, M.; Singh, D.; Lown, R.; Poles, A.; Solomon, T.; Levi, M.; Goldblatt, D.; Kotoucek, P.; Thomas, W.; Lester, W. Pathologic antibodies to platelet factor 4 after ChAdOx1 nCoV-19 vaccination. N. Engl. J. Med. 2021, 384, 2202–2211. [Google Scholar] [CrossRef] [PubMed]
- Oldenburg, J.; Klamroth, R.; Langer, F.; Albisetti, M.; von Auer, C.; Ay, C.; Korte, W.; Scharf, R.E.; Pötzsch, B.; Greinacher, A. Diagnosis and management of vaccine-related thrombosis following AstraZeneca COVID-19 vaccination: Guidance statement from the GTH. Hamostaseologie 2021, 41, 184–189. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Vaxzevria (Previously COVID-19 Vaccine AstraZeneca): EPAR—Product Information. Annex I—Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/vaxzevria-previously-covid-19-vaccine-astrazeneca-epar-product-information_en.pdf (accessed on 18 January 2022).
- Norwegian Institute of Public Health. Norwegian Institute of Public Health’s Recommendation about AstraZeneca Vaccine. Available online: https://www.fhi.no/en/news/2021/astrazeneca-vaccine-removed-from-coronavirus-immunisation-programme-in-norw/ (accessed on 15 April 2021).
- Danish Health Authority. Denmark Continues Its Vaccine Rollout without the COVID-19 Vaccine from AstraZeneca. Available online: https://www.sst.dk/en/english/news/2021/denmark-continues-its-vaccine-rollout-without-the-covid-19-vaccine-from-astrazeneca (accessed on 14 April 2021).
- Muir, K.L.; Kallam, A.; Koepsell, S.A.; Gundabolu, K. Thrombotic thrombocytopenia after Ad26.COV2.S vaccination. N. Engl. J. Med. 2021, 384, 1964–1965. [Google Scholar] [CrossRef] [PubMed]
- America Society of Hematology. COVID-19 Resources—Vaccine-Induced Immune Thrombotic Thrombocytopenia. Available online: https://www.hematology.org/covid-19/vaccine-induced-immune-thrombotic-thrombocytopenia (accessed on 28 January 2022).
- Platton, S.; Bartlett, A.; MacCallum, P.; Makris, M.; McDonald, V.; Singh, D.; Scully, M.; Pavord, S. Evaluation of laboratory assays for anti-platelet factor 4 antibodies after ChAdOx1 nCOV-19 vaccination. J. Thromb. Haemost. 2021, 19, 2007–2013. [Google Scholar] [CrossRef]
- Franchini, M.; Liumbruno, G.M.; Pezzo, M. COVID-19 vaccine-associated immune thrombosis and thrombocytopenia (VITT): Diagnostic and therapeutic recommendations for a new syndrome. Eur. J. Haematol. 2021, 107, 173–180. [Google Scholar] [CrossRef]
- Eisman, R.; Surrey, S.; Ramachandran, B.; Schwartz, E.; Poncz, M. Structural and functional comparison of the genes for human platelet factor 4 and PF4alt. Blood 1990, 76, 336–344. [Google Scholar] [CrossRef] [Green Version]
- Warkentin, T.E. Drug-induced immune-mediated thrombocytopenia—From purpura to thrombosis. N. Engl. J. Med. 2007, 356, 891–893. [Google Scholar] [CrossRef] [Green Version]
- European Medicines Agency. COVID-19 Vaccine Janssen: EPAR—Product Information. Annex I—Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/covid-19-vaccine-janssen-epar-product-information_en.pdf (accessed on 20 January 2022).
- Roncati, L.; Corsi, L. Nucleoside-modified messenger RNA COVID-19 vaccine platform. J. Med. Virol. 2021, 93, 4054–4057. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Comirnaty: EPAR—Product Information. Annex I—Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/comirnaty-epar-product-information_en.pdf (accessed on 20 January 2022).
- McKeigue, P.M.; Burgul, R.; Bishop, J.; Robertson, C.; McMenamin, J.; O’Leary, M.; McAllister, D.A.; Colhoun, H.M. Association of cerebral venous thrombosis with recent COVID-19 vaccination: Case-crossover study using ascertainment through neuroimaging in Scotland. BMC Infect. Dis. 2021, 21, 1275. [Google Scholar] [CrossRef] [PubMed]
- Finsterer, J.; Nics, S. Venous sinus thrombosis after the second jab of a mRNA-based SARS-CoV-2 vaccine. Brain Hemorrhages 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Yagi, Y.; Asami, Y.; Kyoya, M.; Yokota, T. Cerebral venous sinus thrombosis after mRNA-based COVID-19 vaccination. Neurol. Sci. 2022, 43, 41–43. [Google Scholar] [CrossRef] [PubMed]
- Cheng, N. Cerebral venous sinus thrombosis after Pfizer-BioNTech COVID-19 (BNT162b2) vaccination. J. Clin. Neurol. 2021, 17, 573–575. [Google Scholar] [CrossRef] [PubMed]
- Zakaria, Z.; Sapiai, N.A.; Ghani, A.R.I. Cerebral venous sinus thrombosis 2 weeks after the first dose of mRNA SARS-CoV-2 vaccine. Acta Neurochir. 2021, 163, 2359–2362. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, Y.; Kimihira, L.; Nagasawa, H.; Seo, K.; Wada, M. Cerebral venous sinus thrombosis after BNT162b2 mRNA COVID-19 vaccination. Cureus 2021, 13, e18775. [Google Scholar] [CrossRef]
- Fan, B.E.; Shen, J.Y.; Lim, X.R.; Tu, T.M.; Chang, C.C.R.; Khin, H.S.W.; Koh, J.S.; Rao, J.P.; Lau, S.L.; Tan, G.B.; et al. Cerebral venous thrombosis post BNT162b2 mRNA SARS-CoV-2 vaccination: A black swan event. Am. J. Hematol. 2021, 96, E357–E361. [Google Scholar] [CrossRef]
- Dias, L.; Soares-Dos-Reis, R.; Meira, J.; Ferrão, D.; Soares, P.R.; Pastor, A.; Gama, G.; Fonseca, L.; Fagundes, V.; Carvalho, M. Cerebral venous thrombosis after BNT162b2 mRNA SARS-CoV-2 vaccine. J. Stroke Cerebrovasc. Dis. 2021, 30, 105906. [Google Scholar] [CrossRef]
- Al-Maqbali, J.S.; Al Rasbi, S.; Kashoub, M.S.; Al Hinaai, A.M.; Farhan, H.; Al Rawahi, B.; Al Alawi, A.M. A 59-year-old woman with extensive deep vein thrombosis and pulmonary thromboembolism 7 days following a first dose of the Pfizer-BioNTech BNT162b2 mRNA COVID-19 vaccine. Am. J. Case Rep. 2021, 22, e932946. [Google Scholar] [CrossRef]
- Al-Ahmad, M.; Al Rasheed, M.; Altourah, L.; Rodriguez-Bouza, T.; Shalaby, N. Isolated thrombosis after COVID-19 vaccination: Case series. Int. J. Hematol. 2022, 115, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Bilotta, C.; Perrone, G.; Adelfio, V.; Spatola, G.F.; Uzzo, M.L.; Argo, A.; Zerbo, S. COVID-19 vaccine-related thrombosis: A systematic review and exploratory analysis. Front. Immunol. 2021, 12, 729251. [Google Scholar] [CrossRef] [PubMed]
- Abbattista, M.; Martinelli, I.; Peyvandi, F. Comparison of adverse drug reactions among four COVID-19 vaccines in Europe using the EudraVigilance database: Thrombosis at unusual sites. J. Thromb. Haemost. 2021, 19, 2554–2558. [Google Scholar] [CrossRef] [PubMed]
- Shimazawa, R.; Ikeda, M. Potential adverse events in Japanese women who received tozinameran (BNT162b2, Pfizer-BioNTech). J. Pharm. Policy Pract. 2021, 14, 46. [Google Scholar] [CrossRef]
- Ferner, R.E.; Stevens, R.J.; Anton, C.; Aronson, J.K. Spontaneous reporting to regulatory authorities of suspected adverse drug reactions to COVID-19 vaccines over time: The effect of publicity. Drug Saf. 2022, 45, 137–144. [Google Scholar] [CrossRef]
- Lee, S.; Sankhala, K.K.; Bose, S.; Gallemore, R.P. Combined central retinal artery and vein occlusion with ischemic optic neuropathy after COVID-19 vaccination. Int. Med. Case Rep. J. 2022, 15, 7–14. [Google Scholar] [CrossRef]
- Tanaka, H.; Nagasato, D.; Nakakura, S.; Tanabe, H.; Nagasawa, T.; Wakuda, H.; Imada, Y.; Mitamura, Y.; Tabuchi, H. Exacerbation of branch retinal vein occlusion post SARS-CoV-2 vaccination: Case reports. Medicine 2021, 100, e28236. [Google Scholar] [CrossRef]
- Hinton, J.; Briosa, E.; Gala, A.; Corbett, S. mRNA COVID-19 vaccine-related anaphylactoid reaction and coronary thrombosis. Mayo Clin. Proc. 2021, 96, 3182–3183. [Google Scholar] [CrossRef]
- Hippisley-Cox, J.; Patone, M.; Mei, X.W.; Saatci, D.; Dixon, S.; Khunti, K.; Zaccardi, F.; Watkinson, P.; Shankar-Hari, M.; Doidge, J.; et al. Risk of thrombocytopenia and thromboembolism after COVID-19 vaccination and SARS-CoV-2 positive testing: Self-controlled case series study. BMJ 2021, 374, n1931. [Google Scholar] [CrossRef]
- Malayala, S.V.; Papudesi, B.N.; Sharma, R.; Vusqa, U.T.; Raza, A. A case of idiopathic thrombocytopenic purpura after booster dose of BNT162b2 (Pfizer-BioNtech) COVID-19 vaccine. Cureus 2021, 13, e18985. [Google Scholar] [CrossRef]
- De Bruijn, S.; Maes, M.B.; De Waele, L.; Vanhoorelbeke, K.; Gadisseur, A. First report of a de novo iTTP episode associated with a mRNA-based anti-COVID-19 vaccination. J. Thromb. Haemost. 2021, 19, 2014–2018. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Anayama, M.; Sumi, M.; Kobayashi, H. Immune thrombocytopenia after BNT162b2 mRNA COVID-19 vaccination. Rinsho Ketsueki 2021, 62, 1688–1693. [Google Scholar] [CrossRef] [PubMed]
- Waqar, S.H.B.; Khan, A.A.; Memon, S. Thrombotic thrombocytopenic purpura: A new menace after COVID BNT162b2 vaccine. Int. J. Hematol. 2021, 114, 626–629. [Google Scholar] [CrossRef] [PubMed]
- Shibata, K.; Tanaka, H.; Otani, A.; Kubo, M.; Hasegawa, A.; Amano, I. Development of thrombocytopenic purpura following BNT162b2 mRNA COVID-19 vaccination. Rinsho Ketsueki 2021, 62, 1519–1521. [Google Scholar] [CrossRef] [PubMed]
- Okada, Y.; Sakai, R.; Sato-Fitoussi, M.; Nodera, M.; Yoshinaga, S.; Shibata, A.; Kurasawa, T.; Kondo, T.; Amano, K. Potential triggers for thrombocytopenia and/or hemorrhage by the BNT162b2 vaccine, Pfizer-BioNTech. Front. Med. 2021, 8, 751598. [Google Scholar] [CrossRef] [PubMed]
- Sumi, T.; Nagahisa, Y.; Matsuura, K.; Sekikawa, M.; Yamada, Y.; Nakata, H.; Chiba, H. Lung squamous cell carcinoma with hemoptysis after vaccination with tozinameran (BNT162b2, Pfizer-BioNTech). Thorac. Cancer 2021, 12, 3072–3075. [Google Scholar] [CrossRef] [PubMed]
- Fueyo-Rodriguez, O.; Valente-Acosta, B.; Jimenez-Soto, R.; Neme-Yunes, Y.; Inclán-Alarcón, S.I.; Trejo-Gonzalez, R.; García-Salcido, M.Á. Secondary immune thrombocytopenia supposedly attributable to COVID-19 vaccination. BMJ Case Rep. 2021, 14, e242220. [Google Scholar] [CrossRef]
- Lee, E.J.; Cines, D.B.; Gernsheimer, T.; Kessler, C.; Michel, M.; Tarantino, M.D.; Semple, J.W.; Arnold, D.M.; Godeau, B.; Lambert, M.P.; et al. Thrombocytopenia following Pfizer and Moderna SARS-CoV-2 vaccination. Am. J. Hematol. 2021, 96, 534–537. [Google Scholar] [CrossRef]
- Bhan, C.; Bheesham, N.; Shakuntulla, F.; Sharma, M.; Sun, C.; Weinstein, M. An unusual presentation of acute deep vein thrombosis after the Moderna COVID-19 vaccine—A case report. Ann. Transl. Med. 2021, 9, 1605. [Google Scholar] [CrossRef]
- Su, P.H.; Yu, Y.C.; Chen, W.H.; Lin, H.C.; Chen, Y.T.; Cheng, M.H.; Huang, Y.M. Case report: Vaccine-induced immune thrombotic thrombocytopenia in a pancreatic cancer patient after vaccination with messenger RNA-1273. Front. Med. 2021, 8, 772424. [Google Scholar] [CrossRef]
- Syed, K.; Chaudhary, H.; Donato, A. Central venous sinus thrombosis with subarachnoid hemorrhage following a mRNA COVID-19 vaccination: Are these reports merely co-incidental? Am. J. Case Rep. 2021, 22, e933397. [Google Scholar] [CrossRef] [PubMed]
- Andraska, E.A.; Kulkarni, R.; Chaudhary, M.; Sachdev, U. Three cases of acute venous thromboembolism in females after vaccination for coronavirus disease 2019. J. Vasc. Surg. Venous Lymphat. Disord. 2022, 10, 14–17. [Google Scholar] [CrossRef] [PubMed]
- Pishko, A.M.; Cuker, A. Thrombosis after vaccination with messenger RNA-1273: Is this vaccine-induced thrombosis and thrombocytopenia or thrombosis with thrombocytopenia syndrome? Ann. Intern. Med. 2021, 174, 1468–1469. [Google Scholar] [CrossRef] [PubMed]
- Osmanodja, B.; Schreiber, A.; Schrezenmeier, E.; Seelow, E. First diagnosis of thrombotic thrombocytopenic purpura after SARS-CoV-2 vaccine—Case report. BMC Nephrol. 2021, 22, 411. [Google Scholar] [CrossRef]
- Smadja, D.M.; Yue, Q.Y.; Chocron, R.; Sanchez, O.; Lillo-Le Louet, A. Vaccination against COVID-19: Insight from arterial and venous thrombosis occurrence using data from VigiBase. Eur. Respir. J. 2021, 58, 2100956. [Google Scholar] [CrossRef]
- Favaloro, E.J.; Pasalic, L.; Lippi, G. Antibodies against platelet factor 4 and their associated pathologies: From HIT/HITT to spontaneous HIT-like syndrome, to COVID-19, to VITT/TTS. Antibodies 2022, 11, 7. [Google Scholar] [CrossRef]
- Thiele, T.; Ulm, L.; Holtfreter, S.; Schönborn, L.; Kuhn, S.O.; Scheer, C.; Warkentin, T.E.; Bröker, B.M.; Becker, K.; Aurich, K.; et al. Frequency of positive anti-PF4/polyanion antibody tests after COVID-19 vaccination with ChAdOx1 nCoV-19 and BNT162b2. Blood 2021, 138, 299–303. [Google Scholar] [CrossRef]
- See, I.; Lale, A.; Marquez, P.; Streiff, M.B.; Wheeler, A.P.; Tepper, N.K.; Woo, E.J.; Broder, K.R.; Edwards, K.M.; Gallego, R.; et al. Case series of thrombosis with thrombocytopenia syndrome after COVID-19 vaccination-United States, December 2020 to August 2021. Ann. Intern. Med. 2022, in press. [Google Scholar] [CrossRef]
- Schönborn, L.; Thiele, T.; Kaderali, L.; Günther, A.; Hoffmann, T.; Seck, S.E.; Selleng, K.; Greinacher, A. Most anti-PF4 antibodies in vaccine-induced immune thrombotic thrombocytopenia are transient. Blood 2022, 139, 1903–1907. [Google Scholar] [CrossRef]
- Ueland, T.; Hausberg, I.; Mørtberg, T.V.; Dahl, T.B.; Lerum, T.V.; Michelsen, A.; Ranheim, T.; Nezvalova Henriksen, K.; Dyrhol-Riise, A.M.; Holme, P.A.; et al. Anti-PF4/polyanion antibodies in COVID-19 patients are associated with disease severity and pulmonary pathology. Platelets 2022, in press. [Google Scholar] [CrossRef]
- Roncati, L.; Ligabue, G.; Nasillo, V.; Lusenti, B.; Gennari, W.; Fabbiani, L.; Malagoli, C.; Gallo, G.; Giovanella, S.; Lupi, M.; et al. A proof of evidence supporting abnormal immunothrombosis in severe COVID-19: Naked megakaryocyte nuclei increase in the bone marrow and lungs of critically ill patients. Platelets 2020, 31, 1085–1089. [Google Scholar] [CrossRef] [PubMed]
- Roncati, L.; Corsi, L.; Barbolini, G. Abnormal immunothrombosis and lupus anticoagulant in a catastrophic COVID-19 recalling Asherson’s syndrome. J. Thromb. Thrombolysis 2021, 52, 1043–1046. [Google Scholar] [CrossRef] [PubMed]
- Østergaard, L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: Consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol. Rep. 2021, 9, e14726. [Google Scholar] [CrossRef] [PubMed]
- Solari, D.; Alberio, L.; Ribi, C.; Grandoni, F.; Stalder, G. Autoimmune hemolytic anemia and pulmonary embolism: An association to consider. TH Open 2021, 5, e8–e13. [Google Scholar] [CrossRef] [PubMed]
- Ungprasert, P.; Tanratana, P.; Srivali, N. Autoimmune hemolytic anemia and venous thromboembolism: A systematic review and meta-analysis. Thromb. Res. 2015, 136, 1013–1017. [Google Scholar] [CrossRef]
- Boyer, N.L.; Niven, A.; Edelman, J. Tacrolimus-associated thrombotic microangiopathy in a lung transplant recipient. BMJ Case Rep. 2013, 2013, bcr2012007351. [Google Scholar] [CrossRef] [Green Version]
- Cortina, G.; Trojer, R.; Waldegger, S.; Schneeberger, S.; Gut, N.; Hofer, J. De novo tacrolimus-induced thrombotic microangiopathy in the early stage after renal transplantation successfully treated with conversion to everolimus. Pediatr. Nephrol. 2015, 30, 693–697. [Google Scholar] [CrossRef]
- Wattanakit, K.; Cushman, M.; Stehman-Breen, C.; Heckbert, S.R.; Folsom, A.R. Chronic kidney disease increases risk for venous thromboembolism. J. Am. Soc. Nephrol. 2008, 19, 135–140. [Google Scholar] [CrossRef] [Green Version]
- Wattanakit, K.; Cushman, M. Chronic kidney disease and venous thromboembolism: Epidemiology and mechanisms. Curr. Opin. Pulm. Med. 2009, 15, 408–412. [Google Scholar] [CrossRef] [Green Version]
- Mathieson, P.; Reckless, I.; Ferrett, C. Secondary spontaneous pneumothorax: A rare complication of pulmonary embolism. BMJ Case Rep. 2012, 2012, bcr-2012-006860. [Google Scholar] [CrossRef] [Green Version]
- Manenti, A.; Roncati, L.; Melegari, G. Deepening pathology of SARS-CoV-2 pneumonia explains lung ventilation complications. Ann. Thorac. Surg. 2021, 113, 1389. [Google Scholar] [CrossRef] [PubMed]
- United States Centers for Disease Control and Prevention. Safety of COVID-19 Vaccines. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/safety-of-vaccines.html (accessed on 14 February 2022).
- European Medicines Agency. COVID-19 Vaccines Safety Update. Available online: https://www.ema.europa.eu/en/documents/covid-19-vaccine-safety-update/covid-19-vaccines-safety-update-17-february-2022_en.pdf (accessed on 17 February 2022).
- Agenzia Italiana del Farmaco. Rapporto Annuale Sulla Sicurezza Dei Vaccini Anti-COVID-19. Available online: https://www.aifa.gov.it/documents/20142/1315190/Rapporto_annuale_su_sicurezza_vaccini%20anti-COVID-19.pdf (accessed on 11 February 2022).


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roncati, L.; Manenti, A.; Corsi, L. A Three-Case Series of Thrombotic Deaths in Patients over 50 with Comorbidities Temporally after modRNA COVID-19 Vaccination. Pathogens 2022, 11, 435. https://doi.org/10.3390/pathogens11040435
Roncati L, Manenti A, Corsi L. A Three-Case Series of Thrombotic Deaths in Patients over 50 with Comorbidities Temporally after modRNA COVID-19 Vaccination. Pathogens. 2022; 11(4):435. https://doi.org/10.3390/pathogens11040435
Chicago/Turabian StyleRoncati, Luca, Antonio Manenti, and Lorenzo Corsi. 2022. "A Three-Case Series of Thrombotic Deaths in Patients over 50 with Comorbidities Temporally after modRNA COVID-19 Vaccination" Pathogens 11, no. 4: 435. https://doi.org/10.3390/pathogens11040435
APA StyleRoncati, L., Manenti, A., & Corsi, L. (2022). A Three-Case Series of Thrombotic Deaths in Patients over 50 with Comorbidities Temporally after modRNA COVID-19 Vaccination. Pathogens, 11(4), 435. https://doi.org/10.3390/pathogens11040435







