Preventive Treatment for Household Contacts of Drug-Susceptible Tuberculosis Patients
Abstract
:1. Introduction
1.1. Risk of TB among Household Contacts
1.2. Impact and Cost-Effectiveness of TB Prevention among Household Contacts
1.3. WHO Recommendations for Screening and Treatment of TB Infection in Household Contacts
1.4. Country TPT Guidelines and Policies
1.5. TPT Regimens
1.6. TPT Durability
1.7. TPT Completion and Adherence among Household Contacts
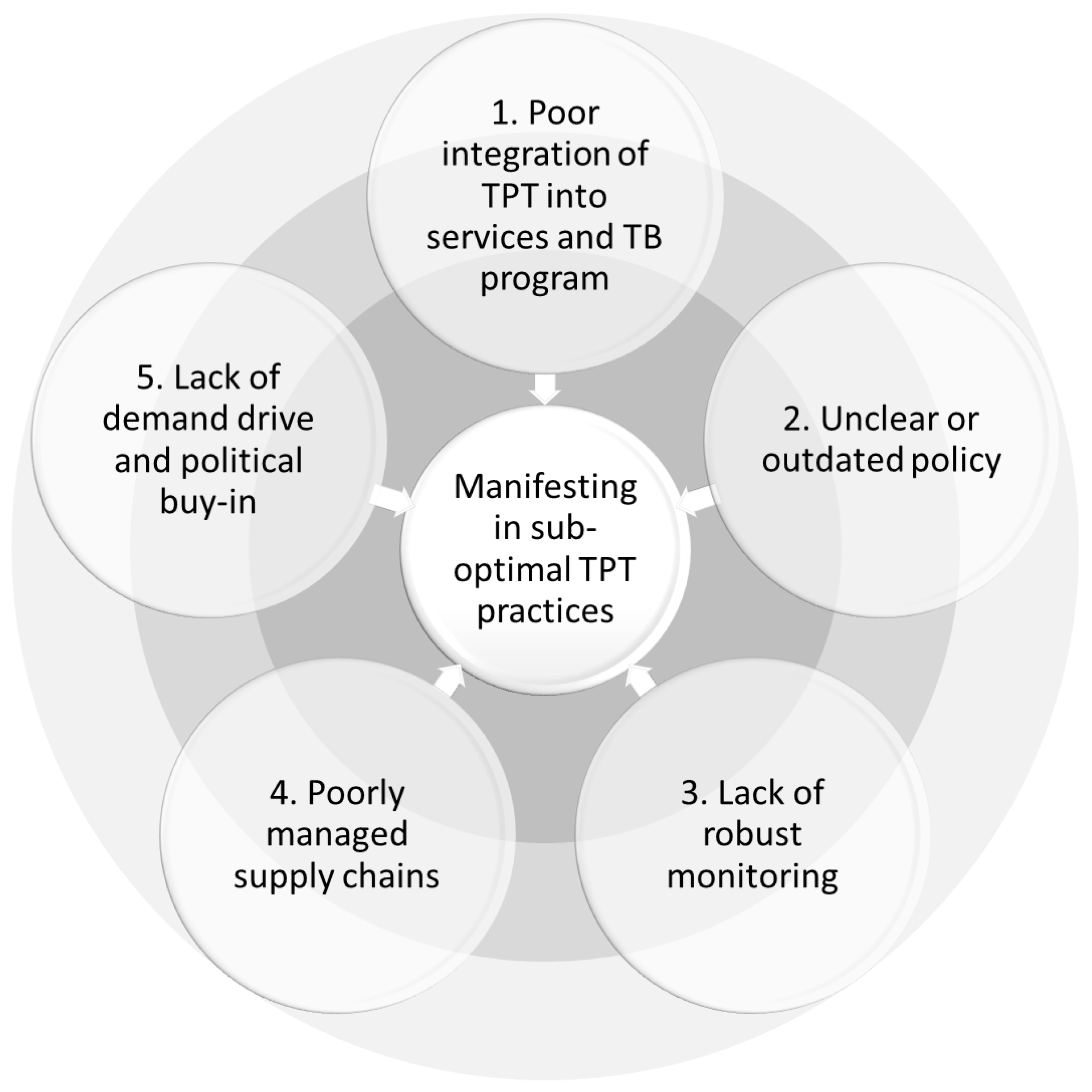
2. Policy-to-Implementation Gap
2.1. Conceptual Mapping of Challenges to TPT Delivery among Household Contacts
2.2. Driver 1—Poor Integration of TPT into TB Service Delivery Specifically and Primary Care Generally
2.3. Driver 2—Unclear or Outdated Policy and Lack of Appropriate Provider Training
2.4. Driver 3—A Lack of Robust TPT Monitoring Systems with an Over-Focus on Total TPT Initiations rather than Treatment Completions
2.5. Driver 4—Poorly Managed Supply Chains
2.6. Driver 5—A Lack of Demand Drive, Political Buy-In, and Civil Society/Activism for TPT Services
3. Future Directions: How Do We Close the Policy-to-Implementation Gap?
3.1. TPT Regimens and Availability
3.2. TB Infection Testing
3.3. Approaches to Contact Screening and Investigation
3.4. Models of Care for TPT Provision to Household Contacts
3.5. Expanding TPT Services
4. Monitoring and Evaluation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Tuberculosis Report 2021; World Health Organization: Geneva, Switzerland, 2021.
- World Health Organization. Latent Tuberculosis Infection: Updated and Consolidated Guidelines for Programmatic Management; World Health Organization: Geneva, Switzerland, 2018.
- United Nations. Political Declaration of the High-Level Meeting of the General Assembly on the Fight Against Tuberculosis. In United to End Tuberculosis: An Urgent Global Response to a Global Epidemic; United Nations: New York, NY, USA, 2019. [Google Scholar]
- Majumdar, S.S.; Triasih, R.; Graham, S.M. Scaling up tuberculosis preventive therapy for contacts in high transmission settings. Lancet Glob. Health 2020, 8, e617–e618. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for South-East Asia. A Situational Analysis of Programmatic Management of TB Preventive Treatment in the WHO South-East Asia Region; World Health Organization, Regional Office for South-East Asia: New Delhi, India, 2020.
- World Health Organization. Global Tuberculosis Report 2021: Supplementary Material; World Health Organization: Geneva, Switzerland, 2022. Available online: https://apps.who.int/iris/handle/10665/360605 (accessed on 26 September 2022).
- Di Gennaro, F.; Gualano, G.; Timelli, L.; Vittozzi, P.; Di Bari, V.; Libertone, R.; Cerva, C.; Pinnarelli, L.; Nisii, C.; Ianniello, S.; et al. Increase in Tuberculosis Diagnostic Delay during First Wave of the COVID-19 Pandemic: Data from an Italian Infectious Disease Referral Hospital. Antibiotics 2021, 10, 272. [Google Scholar] [CrossRef] [PubMed]
- Houben, R.M.G.J.; Dodd, P.J. The Global Burden of Latent Tuberculosis Infection: A Re-estimation Using Mathematical Modelling. PLoS Med. 2016, 13, e1002152. [Google Scholar] [CrossRef] [Green Version]
- Cohen, A.; Mathiasen, V.D.; Schön, T.; Wejse, C. The global prevalence of latent tuberculosis: A systematic review and meta-analysis. Eur. Respir. J. 2019, 54, 1900655. [Google Scholar] [CrossRef]
- Velen, K.; Shingde, R.V.; Ho, J.; Fox, G.J. The effectiveness of contact investigation among contacts of tuberculosis patients: A systematic review and meta-analysis. Eur. Respir. J. 2021, 58, 2100266. [Google Scholar] [CrossRef] [PubMed]
- Kendall, E.A.; Shrestha, S.; Dowdy, D.W. The Epidemiological Importance of Subclinical Tuberculosis. A Critical Reappraisal. Am. J. Respir. Crit. Care Med. 2021, 203, 168–174. [Google Scholar] [CrossRef]
- Mendelsohn, S.C.; Fiore-Gartland, A.; Penn-Nicholson, A.; Mulenga, H.; Mbandi, S.K.; Borate, B.; Hadley, K.; Hikuam, C.; Musvosvi, M.; Bilek, N.; et al. Validation of a host blood transcriptomic biomarker for pulmonary tuberculosis in people living with HIV: A prospective diagnostic and prognostic accuracy study. Lancet Glob. Health 2021, 9, e841–e853. [Google Scholar] [CrossRef]
- Jo, Y.; Gomes, I.; Flack, J.; Salazar-Austin, N.; Churchyard, G.; Chaisson, R.E.; Dowdy, D.W. Cost-effectiveness of scaling up short course preventive therapy for tuberculosis among children across 12 countries. eClinicalMedicine 2021, 31, 100707. [Google Scholar] [CrossRef] [PubMed]
- Mandalakas, A.M.; Hesseling, A.C.; Gie, R.P.; Schaaf, H.S.; Marais, B.J.; Sinanovic, E. Modelling the cost-effectiveness of strategies to prevent tuberculosis in child contacts in a high-burden setting. Thorax 2013, 68, 247–255. [Google Scholar] [CrossRef] [Green Version]
- Kendall, E.A.; Hussain, H.; Kunkel, A.; Kubiak, R.W.; Trajman, A.; Menzies, R.; Drain, P.K. Isoniazid or rifampicin preventive therapy with and without screening for subclinical TB: A modeling analysis. BMC Med. 2021, 19, 315. [Google Scholar] [CrossRef]
- Doan, T.N.; Fox, G.J.; Meehan, M.T.; Scott, N.; Ragonnet, R.; Viney, K.; Trauer, J.M.; McBryde, E.S. Cost-effectiveness of 3 months of weekly rifapentine and isoniazid compared with other standard treatment regimens for latent tuberculosis infection: A decision analysis study. J. Antimicrob. Chemother. 2019, 74, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Oxlade, O.; Boon, S.D.; Menzies, D.; Falzon, D.; Lane, M.Y.; Kanchar, A.; Zignol, M.; Matteelli, A. TB preventive treatment in high- and intermediate-incidence countries: Research needs for scale-up. Int. J. Tuberc. Lung Dis. 2021, 25, 823–831. [Google Scholar] [CrossRef] [PubMed]
- Shepardson, D.; Marks, S.M.; Chesson, H.; Kerrigan, A.; Holland, D.P.; Scott, N.; Tian, X.; Borisov, A.S.; Shang, N.; Heilig, C.M.; et al. Cost-effectiveness of a 12-dose regimen for treating latent tuberculous infection in the United States. Int. J. Tuberc. Lung Dis. 2013, 17, 1531–1537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.W.; Yang, S.F.; Yeh, Y.P.; Tsao, T.C.; Tsao, S.M. Impacts of 12-dose regimen for latent tuberculosis infection: Treatment completion rate and cost-effectiveness in Taiwan. Medicine 2016, 95, e4126. [Google Scholar] [CrossRef] [PubMed]
- Pease, C.; Alvarez, G.; Mallick, R.; Patterson, M.; Finn, S.; Habis, Y.; Schwartzman, K.; Kilabuk, E.; Mulpuru, S.; Zwerling, A. Cost-effectiveness analysis of 3 months of weekly rifapentine and isoniazid compared to isoniazid monotherapy in a Canadian arctic setting. BMJ Open 2021, 11, e047514. [Google Scholar] [CrossRef]
- Smieja, M.; Marchetti, C.; Cook, D.; Smaill, F.M. Isoniazid for preventing tuberculosis in non-HIV infected persons. Cochrane Database Syst. Rev. 1999, 1999, CD001363. [Google Scholar] [CrossRef]
- Harries, A.D.; Kumar, A.M.V.; Satyanarayana, S.; Takarinda, K.C.; Timire, C.; Dlodlo, R.A. Treatment for latent tuberculosis infection in low- and middle-income countries: Progress and challenges with implementation and scale-up. Expert Rev. Respir. Med. 2020, 14, 195–208. [Google Scholar] [CrossRef]
- Martinson, N.A.; Barnes, G.L.; Moulton, L.H.; Msandiwa, R.; Hausler, H.; Ram, M.; McIntyre, J.A.; Gray, G.E.; Chaisson, R.E. New Regimens to Prevent Tuberculosis in Adults with HIV Infection. N. Engl. J. Med. 2011, 365, 11–20. [Google Scholar] [CrossRef] [Green Version]
- Sterling, T.R.; Scott, N.A.; Miro, J.M.; Calvet, G.; La Rosa, A.; Infante, R.; Chen, M.P.; Benator, D.A.; Gordin, F.; Benson, C.A.; et al. Three months of weekly rifapentine and isoniazid for treatment of Mycobacterium tuberculosis infection in HIV-coinfected persons. AIDS 2016, 30, 1607–1615. [Google Scholar] [CrossRef] [Green Version]
- Sterling, T.R.; Villarino, M.E.; Borisov, A.S.; Shang, N.; Gordin, F.; Bliven-Sizemore, E.; Hackman, J.; Hamilton, C.D.; Menzies, D.; Kerrigan, A.; et al. Three Months of Rifapentine and Isoniazid for Latent Tuberculosis Infection. N. Engl. J. Med. 2011, 365, 2155–2166. [Google Scholar] [CrossRef]
- Villarino, M.E.; Scott, N.A.; Weis, S.E.; Weiner, M.; Conde, M.B.; Jones, B.; Nachman, S.; Oliveira, R.; Moro, R.N.; Shang, N.; et al. Treatment for preventing tuberculosis in children and adolescents: A randomized clinical trial of a 3-month, 12-dose regimen of a combination of rifapentine and isoniazid. JAMA Pediatr. 2015, 169, 247–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Churchyard, G.; Cardenas, V.; Chihota, V.; Mngadi, K.; Sebe, M.; Brumskine, W.; Martinson, N.; Yimer, G.; Wang, S.-H.; Garcia-Basteiro, A.L.; et al. Annual Tuberculosis Preventive Therapy for Persons With HIV Infection: A Randomized Trial. Ann. Intern. Med. 2021, 174, 1367–1376. [Google Scholar] [CrossRef] [PubMed]
- Dooley, K.E.; Savic, R.; Gupte, A.; Marzinke, M.A.; Zhang, N.; Edward, V.A.; Wolf, L.; Sebe, M.; Likoti, M.; Fyvie, M.J.; et al. Once-weekly rifapentine and isoniazid for tuberculosis prevention in patients with HIV taking dolutegravir-based antiretroviral therapy: A phase 1/2 trial. Lancet HIV 2020, 7, e401–e409. [Google Scholar] [CrossRef]
- Alsdurf, H.; Hill, P.C.; Matteelli, A.; Getahun, H.; Menzies, D. The cascade of care in diagnosis and treatment of latent tuberculosis infection: A systematic review and meta-analysis. Lancet Infect. Dis. 2016, 16, 1269–1278. [Google Scholar] [CrossRef]
- Szkwarko, D.; Hirsch-Moverman, Y.; Du Plessis, L.; Du Preez, K.; Carr, C.; Mandalakas, A.M. Child contact management in high tuberculosis burden countries: A mixed-methods systematic review. PLoS ONE 2017, 12, e0182185. [Google Scholar] [CrossRef] [Green Version]
- Unitaid. Landmark Deal Secures Significant Discount on Price of Medicine to Prevent TB; Unitaid: Geneva, Switzerland, 2019. [Google Scholar]
- Unitaid. Partners Announce Reduced Price for Patient-Friendly Tuberculosis Preventive Treatments; Unitaid: Geneva, Switzerland, 2022. [Google Scholar]
- World Health Organization. WHO Operational Handbook on Tuberculosis. In Module 1: Prevention—Tuberculosis Preventive Treatment; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. Rapid Communication: TB Antigen-Based Skin Tests for the Diagnosis of TB Infection; WHO/UCN/TB/2022.1; World Health Organization: Geneva, Switzerland, 2022.
- Scriba, T.J.; Fiore-Gartland, A.; Penn-Nicholson, A.; Mulenga, H.; Mbandi, S.K.; Borate, B.; Mendelsohn, S.C.; Hadley, K.; Hikuam, C.; Kaskar, M.; et al. Biomarker-guided tuberculosis preventive therapy (CORTIS): A randomised controlled trial. Lancet Infect. Dis. 2021, 21, 354–365. [Google Scholar] [CrossRef]
- Fox, G.J.; Nguyen, C.B.; Nguyen, T.A.; Tran, P.T.; Marais, B.J.; Graham, S.M.; Nguyen, B.H.; Velen, K.; Dowdy, D.W.; Mason, P.; et al. Levofloxacin versus placebo for the treatment of latent tuberculosis among contacts of patients with multidrug-resistant tuberculosis (the VQUIN MDR trial): A protocol for a randomised controlled trial. BMJ Open 2020, 10, e033945. [Google Scholar] [CrossRef] [Green Version]
- Onozaki, I.; Law, I.; Sismanidis, C.; Zignol, M.; Glaziou, P.; Floyd, K. National tuberculosis prevalence surveys in Asia, 1990-2012: An overview of results and lessons learned. Trop Med. Int. Health 2015, 20, 1128–1145. [Google Scholar] [CrossRef]
- Drain, P.K.; Bajema, K.L.; Dowdy, D.; Dheda, K.; Naidoo, K.; Schumacher, S.G.; Ma, S.; Meermeier, E.; Lewinsohn, D.M.; Sherman, D.R. Incipient and Subclinical Tuberculosis: A Clinical Review of Early Stages and Progression of Infection. Clin. Microbiol. Rev. 2018, 31. [Google Scholar] [CrossRef] [Green Version]
- Lebina, L.; Martinson, N. A cluster randomized trial of targeted universal testing for TB in clinics. In Proceedings of the Conference on Retroviruses and Opportunistic Infections 2021, online, 6–10 March 2021. [Google Scholar]
- Shapiro, A.E.; Variava, E.; Rakgokong, M.H.; Moodley, N.; Luke, B.; Salimi, S.; Chaisson, R.E.; Golub, J.E.; Martinson, N.A. Community-based Targeted Case Finding for Tuberculosis and HIV in Household Contacts of Patients with Tuberculosis in South Africa. Am. J. Respir. Crit. Care Med. 2012, 185, 1110–1116. [Google Scholar] [CrossRef]
- Kweza, P.F.; Van Schalkwyk, C.; Abraham, N.; Uys, M.; Claassens, M.; Medina-Marino, A. Estimating the magnitude of pulmonary tuberculosis patients missed by primary health care clinics in South Africa. Int. J. Tuberc. Lung Dis. 2018, 22, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Gajee, R.; Sebokolodi, L.; Makura, C.; Modi, S.; Khumalo, Z.; Gilbert, L. The impact of a quality improvement project to improve TB Screening in the West Rand District. In Proceedings of the South Africa 5th SA TB Conference, Durban, South Africa, 12–15 June 2018. [Google Scholar]
- Department of Health. TB Screening and Testing: Standard Operating Procedure; Department of Health: Pretoria, South Africa, 2022.
- Aurum Institute Community and Universal Testing for Tuberculosis Among Contacts. Available online: https://wwwisrctncom/ISRCTN10003903 (accessed on 27 September 2022).
- Sekandi, J.N.; Dobbin, K.; Oloya, J.; Okwera, A.; Whalen, C.C.; Corso, P.S. Cost-Effectiveness Analysis of Community Active Case Finding and Household Contact Investigation for Tuberculosis Case Detection in Urban Africa. PLoS ONE 2015, 10, e0117009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hussain, H.; Malik, A.; Ahmed, J.F.; Siddiqui, S.; Amanullah, F.; Creswell, J.; Tylleskär, T.; Robberstad, B. Cost-effectiveness of household contact investigation for detection of tuberculosis in Pakistan. BMJ Open 2021, 11, e049658. [Google Scholar] [CrossRef]
- Martinson, N.A.; Lebina, L.; Webb, E.L.; Ratsela, A.; Varavia, E.; Kinghorn, A.; Lala, S.G.; E Golub, J.; Bosch, Z.; Motsomi, K.P.; et al. Household contact tracing with intensified tuberculosis and HIV screening in South Africa: A cluster randomised trial. Clin. Infect. Dis. 2021. [Google Scholar] [CrossRef]
- Hirsch-Moverman, Y.; Howard, A.A.; Mantell, J.E.; Lebelo, L.; Frederix, K.; Wills, A.; Hesseling, A.C.; Nachman, S.; Maama, L.B.; El-Sadr, W.M. Improving child tuberculosis contact identification and screening in Lesotho: Results from a mixed-methods cluster-randomized implementation science study. PLoS ONE 2021, 16, e0248516. [Google Scholar] [CrossRef]
- Egere, U.; Sillah, A.; Togun, T.; Kandeh, S.; Cole, F.; Jallow, A.; Able-Thomas, A.; Hoelscher, M.; Heinrich, N.; Hill, P.C.; et al. Isoniazid preventive treatment among child contacts of adults with smear-positive tuberculosis in The Gambia. Public Health Action 2016, 6, 226–231. [Google Scholar] [CrossRef] [Green Version]
- Kay, A.W.; Sandoval, M.; Mtetwa, G.; Mkhabela, M.; Ndlovu, B.; Devezin, T.; Sikhondze, W.; Vambe, D.; Sibanda, J.; Dube, G.S.; et al. Vikela Ekhaya: A Novel, Community-based, Tuberculosis Contact Management Program in a High Burden Setting. Clin. Infect. Dis. 2022, 74, 1631–1638. [Google Scholar] [CrossRef]
- Vasiliu, A.; Salazar-Austin, N.; Trajman, A.; Lestari, T.; Mtetwa, G.; Bonnet, M.; Casenghi, M. Child Contact Case Management—A Major Policy-Practice Gap in High-Burden Countries. Pathogens 2021, 11, 1. [Google Scholar] [CrossRef]
- Johns Hopkins University. Community Initiated Preventive Therapy for TB (CHIP-TB Trial). 2021. Available online: Clinicaltrials.gov (accessed on 8 September 2022).
- Verver, S.; Warren, R.; Munch, Z.; Richardson, M.; van der Spuy, G.; Borgdorff, M.W.; A Behr, M.; Beyers, N.; van Helden, P.D. Proportion of tuberculosis transmission that takes place in households in a high-incidence area. Lancet 2004, 363, 212–214. [Google Scholar] [CrossRef]
- Egere, U.; Togun, T.; Sillah, A.; Mendy, F.; Otu, J.; Hoelscher, M.; Heinrich, N.; Hill, P.C.; Kampmann, B. Identifying children with tuberculosis among household contacts in The Gambia. Int. J. Tuberc. Lung Dis. 2017, 21, 46–52. [Google Scholar] [CrossRef]
- Hoang, T.T.T.; Nguyen, V.N.; Dinh, N.S.; Thwaites, G.; Nguyen, T.A.; Van Doorn, H.R.; Cobelens, F.; Wertheim, H.F.L. Active contact tracing beyond the household in multidrug resistant tuberculosis in Vietnam: A cohort study. BMC Public Health 2019, 19, 241. [Google Scholar] [CrossRef]

| WHO-Recommended TPT Regimen | Target Population | Regimen Duration and Frequency | Child-Friendly Formulation | Regimen Advantages | Regimen Disadvantages |
|---|---|---|---|---|---|
| 1HP | Adolescents of 13 years and older and adults with and without HIV | 28 days | Available in the next 2–5 years |
|
|
| 3HP | Children of 2 years and older, adolescents, and adults | 12 weekly doses | Available in the next 2–5 years |
|
|
| 3RH | Persons of all ages with and without HIV | 90 daily doses | Currently available as dispersible FDC for children of <25 kg |
|
|
| 4R | Persons of all ages with and without HIV | 120 daily doses | Can be compounded into syrup, not readily available in LMICs |
|
|
| 6–9H | Persons of all ages with and without HIV | 180–270 daily doses | Dispersible tablet available |
|
|
| Indicator | Definition | Calculation | Notes |
|---|---|---|---|
| Contact investigation coverage | Percentage of contacts of bacteriologically confirmed pulmonary TB who are evaluated for TB disease | Numerator: number of contacts of bacteriologically confirmed pulmonary TB disease who completed evaluation for TB disease (+/− TB infection) Denominator: number of contacts of bacteriologically confirmed pulmonary TB disease (+/− TB infection) | Denominator may be estimated using TB notifications and demographic data |
| TPT coverage | Percentage of TPT-eligible contacts who initiate TPT | Numerator: number of individuals initiated on TPT Denominator: number of TPT-eligible individuals | This can be calculated separately using TPT indication (household contact, PLHIV, etc.) and by age (<5 years old, 5–14 years old, 15+ years old, etc.) |
| TPT completion | Percentage of individuals who initiated and completed TPT | Numerator: number of individuals completing TPT Denominator: number of individuals initiating TPT | This can be calculated separately using TPT indication (household contact, PLHIV, etc.) and by age (<5 years old, 5–14 years old, 15+ years old, etc.) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salazar-Austin, N.; Mulder, C.; Hoddinott, G.; Ryckman, T.; Hanrahan, C.F.; Velen, K.; Chimoyi, L.; Charalambous, S.; Chihota, V.N. Preventive Treatment for Household Contacts of Drug-Susceptible Tuberculosis Patients. Pathogens 2022, 11, 1258. https://doi.org/10.3390/pathogens11111258
Salazar-Austin N, Mulder C, Hoddinott G, Ryckman T, Hanrahan CF, Velen K, Chimoyi L, Charalambous S, Chihota VN. Preventive Treatment for Household Contacts of Drug-Susceptible Tuberculosis Patients. Pathogens. 2022; 11(11):1258. https://doi.org/10.3390/pathogens11111258
Chicago/Turabian StyleSalazar-Austin, Nicole, Christiaan Mulder, Graeme Hoddinott, Theresa Ryckman, Colleen F. Hanrahan, Kavindhran Velen, Lucy Chimoyi, Salome Charalambous, and Violet N Chihota. 2022. "Preventive Treatment for Household Contacts of Drug-Susceptible Tuberculosis Patients" Pathogens 11, no. 11: 1258. https://doi.org/10.3390/pathogens11111258
APA StyleSalazar-Austin, N., Mulder, C., Hoddinott, G., Ryckman, T., Hanrahan, C. F., Velen, K., Chimoyi, L., Charalambous, S., & Chihota, V. N. (2022). Preventive Treatment for Household Contacts of Drug-Susceptible Tuberculosis Patients. Pathogens, 11(11), 1258. https://doi.org/10.3390/pathogens11111258







