Molecular Pathogenesis and Immune Evasion of Vesicular Stomatitis New Jersey Virus Inferred from Genes Expression Changes in Infected Porcine Macrophages
Abstract
1. Introduction
2. Results
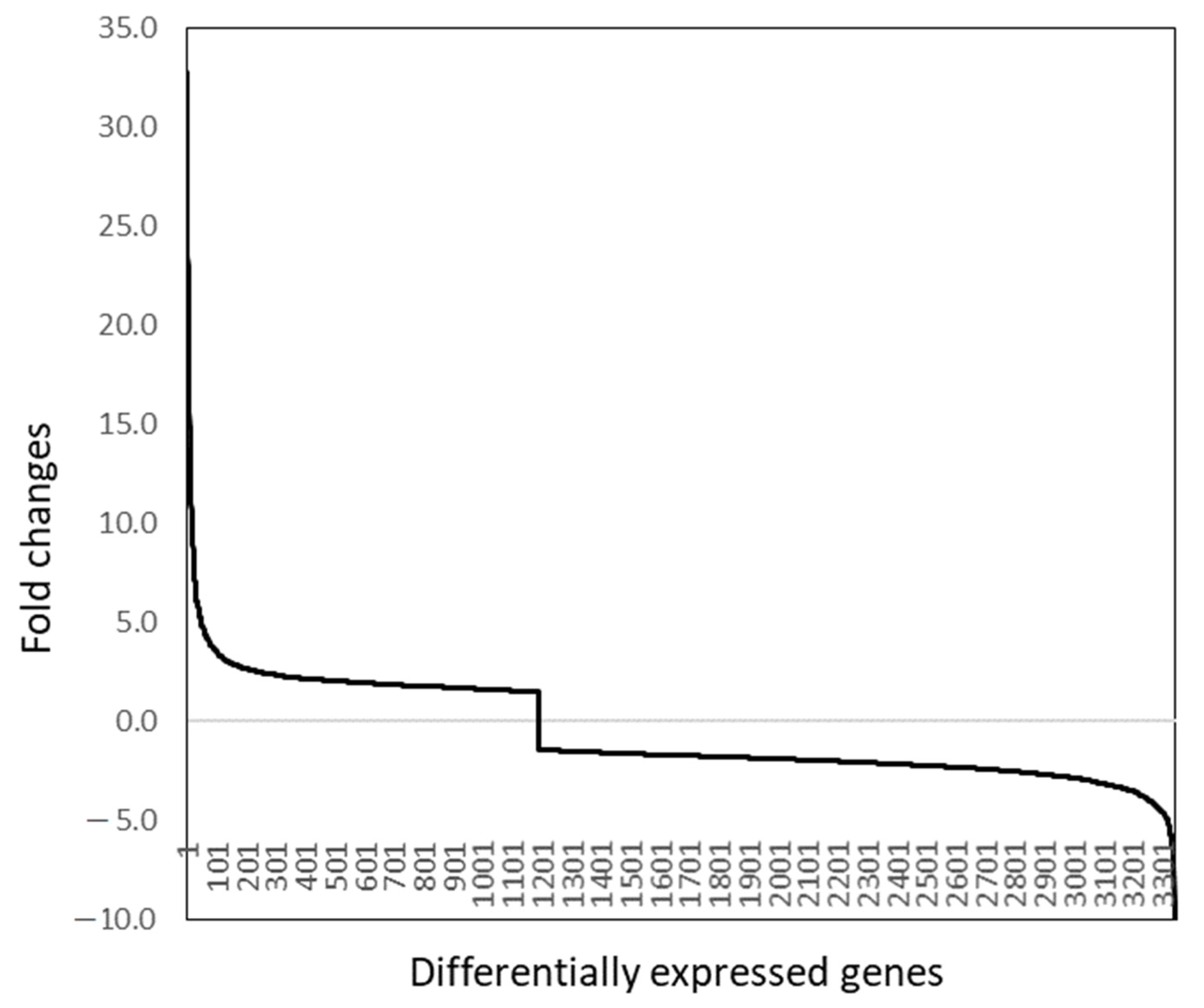
2.1. Differential Gene Expression
2.2. Pathway Analyses
2.3. Interferon Expression and Signaling
2.4. Immune Signaling Pathways
2.5. Cytokines, Chemokines, and Receptors
2.6. Apoptosis, Autophagy, and Unfold Protein Response
2.7. Host mRNA Transcription, Modification, and Stability
2.8. Inflammation-Related Genes
3. Discussion
4. Materials and Methods
4.1. Cell Culture of Macrophages and Viruses
4.2. RNA Isolation
4.3. DNA Microarray Analysis
4.4. Statistical and Bioinformatic Analyses of Microarray Data
4.5. Pathway Analyses
4.6. Biological Inference
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wagner, R.R.; Rose, J.K. Rhabdoviridae: The viruses and their replication. In Fields’ Virology, 3rd ed.; Fields, B.N., Knipe, D.M., Howley, P.M., Chanock, R.M., Hirsh, M.S., Melnick, J.L., Monath, T.P., Roizman, B., Straus, S.E., Eds.; Lippincott-Raven: Philadelphia, PA, USA, 1996; Volume 2, pp. 1121–1136. [Google Scholar]
- Dietzgen, R.G. Morphology. Genome organization, transcription and replication of rhabdoviruses. In Rhabdoviruses: Molecular Taxonomy, Evolution, Genomics, Ecology, Host-Vector Interactions, Cytopathology and Control; Dietzgen, R.G., Kuzmin, I.V., Eds.; Caister Academic Press: Poole, UK, 2012. [Google Scholar]
- Spiropoulou, C.F.; Nichol, S.T. A small highly basic protein is encoded in overlapping frame within the P gene of vesicular stomatitis virus. J. Virol. 1993, 67, 3103–3110. [Google Scholar] [CrossRef]
- Rodríguez, L.L. Emergence and re-emergence of vesicular stomatitis in the United States. Virus Res. 2002, 85, 211–219. [Google Scholar] [CrossRef]
- Mead, D.G.; Gray, E.W.; Noblet, R.; Murphy, M.D.; Howerth, E.W.; Stallknecht, D.E. Biological transmission of vesicular stomatitis virus (New Jersey serotype) by Simulium vittatum (Diptera: Simuliidae) to domestic swine (Sus scrofa). J. Med. Entomol. 2004, 41, 78–82. [Google Scholar] [CrossRef]
- Finkelshtein, D.; Werman, A.; Novick, D.; Barak, S.; Rubinstein, M. LDL receptor and its family members serve as the cellular receptors for vesicular stomatitis virus. Proc. Natl. Acad. Sci. USA 2013, 110, 7306–7311. [Google Scholar] [CrossRef] [PubMed]
- Hastie, E.; Cataldi, M.; Marriott, I.; Grdzelishvili, V.Z. Understanding and altering cell tropism of vesicular stomatitis virus. Virus Res. 2013, 176, 16–32. [Google Scholar] [CrossRef] [PubMed]
- Publicover, J.; Ramsburg, E.; Robek, M.; Rose, J.K. Rapid pathogenesis induced by a vesicular stomatitis virus matrix protein mutant: Viral pathogenesis is linked to induction of tumor necrosis factor alpha. J. Virol. 2006, 80, 7028–7036. [Google Scholar] [CrossRef]
- Iannacone, M.; Moseman, E.A.; Tonti, E.; Bosurgi, L.; Junt, T.; Henrickson, S.E.; Whelan, S.P.; Guidotti, L.G.; von Andrian, U.H. Subcapsular sinus macrophages prevent CNS invasion on peripheral infection with a neurotropic virus. Nature 2010, 465, 1079–1083. [Google Scholar] [CrossRef] [PubMed]
- Scherer, C.F.; O’Donnell, V.; Golde, W.T.; Gregg, D.; Estes, D.M.; Rodriguez, L.L. Vesicular stomatitis New Jersey virus (VSNJV) infects keratinocytes and is restricted to lesion sites and local lymph nodes in the bovine, a natural host. Vet. Res. 2007, 38, 375–390. [Google Scholar] [CrossRef]
- Sun, G.; Fang, X.; Wu, H.; Zhou, X.; Ke, Y.; Sun, T. Porcine monocyte-derived dendritic cells can be differentially activated by vesicular stomatitis virus and its matrix protein mutants. Vet. Microbiol. 2018, 219, 30–39. [Google Scholar] [CrossRef]
- Velazquez-Salinas, L.; Pauszek, S.J.; Stenfeldt, C. Increased Virulence of an Epidemic Strain of Vesicular Stomatitis Virus Is Associated With Interference of the Innate Response in Pigs. Front. Microbiol. 2018, 9, 1891. [Google Scholar] [CrossRef]
- Velazquez-Salinas, L.; Pauszek, S.J.; Holinka, L.G.; Gladue, D.P.; Rekant, S.; Bishop, E.A. A Single Amino Acid Substitution in the Matrix Protein (M51R) of Vesicular Stomatitis New Jersey Virus Impairs Replication in Cultured Porcine Macrophages and Results in Significant Attenuation in Pigs. Front. Microbiol. 2020, 11, 1123. [Google Scholar] [CrossRef]
- Faul, E.J.; Lyles, D.S.; Schnell, M.J. Interferon response and viral evasion by members of the family rhabdoviridae. Viruses 2009, 1, 832–851. [Google Scholar] [CrossRef] [PubMed]
- Rieder, M.; Conzelmann, K.K. Rhabdovirus evasion of the interferon system. J. Interferon Cytokine Res. 2009, 29, 499–509. [Google Scholar] [CrossRef]
- Jayakar, H.R.; Whitt, M.A. Identification of two additional translation products from the matrix (M) gene that contribute to vesicular stomatitis virus cytopathology. J. Virol. 2002, 76, 8011–8018. [Google Scholar] [CrossRef]
- Kopecky, S.A.; Willingham, M.C.; Lyles, D.S. Matrix protein and another viral component contribute to induction of apoptosis in cells infected with vesicular stomatitis virus. J. Virol. 2001, 75, 12169–12181. [Google Scholar] [CrossRef]
- Black, B.L.; Lyles, D.S. Vesicular stomatitis virus matrix protein inhibits host cell-directed transcription of target genes in vivo. J. Virol. 1992, 66, 4058–4064. [Google Scholar] [CrossRef]
- Yuan, H.; Yoza, B.K.; Lyles, D.S. Inhibition of host RNA polymerase II-dependent transcription by vesicular stomatitis virus results from inactivation of TFIID. Virology 1998, 251, 383–392. [Google Scholar] [CrossRef]
- von Kobbe, C.; van Deursen, J.M.; Rodrigues, J.P.; Sitterlin, D.; Bachi, A.; Wu, X.; Wilm, M.; Carmo-Fonseca, M.; Izaurralde, E. Vesicular stomatitis virus matrix protein inhibits host cell gene expression by targeting the nucleoporin Nup98. Mol. Cell. 2000, 6, 1243–1252. [Google Scholar] [CrossRef]
- Rajani, K.R.; Pettit, K.E.L.; McKenzie, M.O.; Horita, D.A.; Chou, J.W.; Lyles, D.S. Complexes of vesicular stomatitis virus matrix protein with host Rae1 and Nup98 involved in inhibition of host transcription. PLoS Pathog. 2012, 8, e1002929. [Google Scholar] [CrossRef] [PubMed]
- Pan, W.; Song, D.; He, W.; Lu, H.; Lan, Y.; Tong, J.; Gao, F.; Zhao, K. The matrix protein of vesicular stomatitis virus inhibits host-directed transcription of target genes via interaction with the TFIIH subunit p8. Vet. Microbiol. 2017, 208, 82–88. [Google Scholar] [CrossRef]
- Petersen, J.M.; Her, L.S.; Varvel, V.; Lund, E.; Dahlberg, J.E. The matrix protein of vesicular stomatitis virus inhibits nucleocytoplasmic transport when it is in the nucleus and associated with nuclear pore complexes. Mol. Cell. Biol. 2000, 20, 8590–8601. [Google Scholar] [CrossRef] [PubMed]
- Varble, A.J.; Ried, C.D.; Hammond, W.J.; Marquis, K.A.; Woodruff, M.C.; Ferran, M.C. The vesicular stomatitis virus matrix protein inhibits NF-κB activation in mouse L929 cells. Virology 2016, 499, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.; McKenzie, M.O.; Puckett, S.; Hojnacki, M.; Poliquin, L.; Lyles, D.S. Ability of the matrix protein of vesicular stomatitis virus to suppress beta interferon gene expression is genetically correlated with the inhibition of host RNA and protein synthesis. J. Virol. 2003, 77, 4646–4657. [Google Scholar] [CrossRef] [PubMed]
- Kandasamy, R.K.; Vladimer, G.; Snijder, B. A time-resolved molecular map of the macrophage response to VSV infection. NPJ Syst. Biol. Appl. 2016, 2, 16027. [Google Scholar] [CrossRef]
- Russell, T.M. Theses: Transcriptome-Wide Analysis of VSV Strains with Varying Ability to Block NF-κB. Master’s Thesis, Rochester Institute of Technology, Rochester, NY, USA, 2018. Available online: https://scholarworks.rit.edu/theses/9951/ (accessed on 26 July 2021).
- Franken, L.; Schiwon, M.; Kurts, C. Macrophages: Sentinels and regulators of the immune system. Cell Microbiol. 2016, 18, 475–487. [Google Scholar] [CrossRef]
- Dantzer, R. Cytokine, sickness behavior, and depression. Immunol. Allergy Clin. N. Am. 2009, 29, 247–264. [Google Scholar] [CrossRef]
- Zhou, Q.; Lavorgna, A.; Bowman, M.; Hiscott, J.; Harhaj, E.W. Aryl Hydrocarbon Receptor Interacting Protein Targets IRF7 to Suppress Antiviral Signaling and the Induction of Type I Interferon. J. Biol. Chem. 2015, 290, 14729–14739. [Google Scholar] [CrossRef] [PubMed]
- Yamada, T.; Horimoto, H.; Kameyama, T.; Hayakawa, S.; Yamato, H.; Dazai, M.; Takada, A.; Kida, H.; Bott, D.; Zhou, A.C.; et al. Constitutive aryl hydrocarbon receptor signaling constrains type I interferon-mediated antiviral innate defense. Nat. Immunol. 2016, 17, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Labzin, L.; Schmidt, S.V.; Masters, S.L.; Beyer, M.; Krebs, W.; Klee, K.; Stahl, R.; Lütjohann, D.; Schultze, J.L.; Latz, E.; et al. ATF3 Is a Key Regulator of Macrophage IFN Responses. J. Immunol. 2015, 195, 4446–4455. [Google Scholar] [CrossRef]
- Köröskényi, K.; Kiss, B.; Szondy, Z. Adenosine A2A receptor signaling attenuates LPS-induced pro-inflammatory cytokine formation of mouse macrophages by inducing the expression of DUSP1. Biochim. Biophys. Acta 2016, 1863, 1461–1471. [Google Scholar] [CrossRef]
- Ray, N.; Kuwahara, M.; Takada, Y.; Maruyama, K.; Kawaguchi, T.; Tsubone, H.; Ishikawa, H.; Matsuo, K. c-Fos suppresses systemic inflammatory response to endotoxin. Int. Immunol. 2006, 18, 671–677. [Google Scholar] [CrossRef]
- Ning, F.; Li, X.; Yu, L.; Zhang, B.; Zhao, Y.; Liu, Y.; Zhao, B.; Shang, Y.; Hu, X. Hes1 attenuates type I IFN responses via VEGF-C and WDFY1. J. Exp. Med. 2019, 216, 1396–1410. [Google Scholar] [CrossRef]
- Keller, A.D.; Maniatis, T. Identification and characterization of a novel repressor of beta-interferon gene expression. Genes Dev. 1991, 5, 868–879. [Google Scholar] [CrossRef]
- Mora-López, F.; Pedreño-Horrillo, N.; Delgado-Pérez, L.; Brieva, J.A.; Campos-Caro, A. Transcription of PRDM1, the master regulator for plasma cell differentiation, depends on an SP1/SP3/EGR-1 GC-box. Eur. J. Immunol. 2008, 38, 2316–2324. [Google Scholar] [CrossRef]
- Das, T.; Chen, Z.; Hendriks, R.W.; Kool, M. A20/Tumor Necrosis Factor α-Induced Protein 3 in Immune Cells Controls Development of Autoinflammation and Autoimmunity: Lessons from Mouse Models. Front. Immunol. 2018, 9, 104. [Google Scholar] [CrossRef] [PubMed]
- Griffith, J.W.; Sokol, C.L.; Luster, A.D. Chemokines and chemokine receptors: Positioning cells for host defense and immunity. Annu. Rev. Immunol. 2014, 32, 659–702. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, T.; Holler, N.; Micheau, O.; Martinon, F.; Tinel, A.; Hofmann, K.; Tschopp, J. Bcl-rambo, a novel Bcl-2 homologue that induces apoptosis via its unique C-terminal extension. J. Biol. Chem. 2001, 276, 19548–19554. [Google Scholar] [CrossRef]
- Singh, P.; Ravanan, P.; Talwar, P. Death Associated Protein Kinase 1 (DAPK1): A Regulator of Apoptosis and Autophagy. Front. Mol. Neurosci. 2016, 9, 46. [Google Scholar] [CrossRef] [PubMed]
- García-Domingo, D.; Ramírez, D.; González de Buitrago, G.; Martínez-A, C. Death inducer-obliterator 1 triggers apoptosis after nuclear translocation and caspase upregulation. Mol. Cell. Biol. 2003, 23, 3216–3225. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Li, J.; Zhou, Q.; Yang, T.; Li, Y.; Zhang, Y.; Wang, J.; Jiao, Z. SGK1 inhibits PM2.5-induced apoptosis and oxidative stress in human lung alveolar epithelial A549 cells. Biochem. Biophys. Res. Commun. 2018, 496, 1291–1295. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Edelstein, L.C.; Gélinas, C. The Rel/NF-kappaB family directly activates expression of the apoptosis inhibitor Bcl-x(L). Mol. Cell. Biol. 2000, 20, 2687–2695. [Google Scholar] [CrossRef]
- Gu, C.; Castellino, A.; Chan, J.Y.; Chao, M.V. BRE: A modulator of TNF-alpha action. FASEB J. 1998, 12, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Akilov, O.E.; Wu, M.X.; Ustyugova, I.V.; Falo, L.D., Jr.; Geskin, L.J. Resistance of Sézary cells to TNF-α-induced apoptosis is mediated in part by a loss of TNFR1 and a high level of the IER3 expression. Exp. Dermatol. 2012, 21, 287–292. [Google Scholar] [CrossRef]
- Dunlop, E.A.; Seifan, S.; Claessens, T.; Behrends, C.; Kamps, M.A.; Rozycka, E.; Kemp, A.J.; Nookala, R.K.; Blenis, J.; Coull, B.J.; et al. FLCN, a novel autophagy component, interacts with GABARAP and is regulated by ULK1 phosphorylation. Autophagy 2014, 10, 1749–1760. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wang, G.; Hu, J.S.; Zhang, G.Q.; Chen, H.Z.; Yuan, Y.; Li, Y.L.; Lv, X.J.; Tian, F.Y.; Pan, S.H.; et al. RB1CC1-enhanced autophagy facilitates PSCs activation and pancreatic fibrogenesis in chronic pancreatitis. Cell Death Dis. 2018, 9, 952. [Google Scholar] [CrossRef] [PubMed]
- Morgan, N.E.; Cutrona, M.B.; Simpson, J.C. Multitasking Rab Proteins in Autophagy and Membrane Trafficking: A Focus on Rab33b. Int. J. Mol. Sci. 2019, 20, 3916. [Google Scholar] [CrossRef]
- Luo, S.; Rubinsztein, D.C. BCL2L11/BIM: A novel molecular link between autophagy and apoptosis. Autophagy 2013, 9, 104–105. [Google Scholar] [CrossRef]
- He, G.; Xu, W.; Tong, L.; Li, S.; Su, S.; Tan, X.; Li, C. Gadd45b prevents autophagy and apoptosis against rat cerebral neuron oxygen-glucose deprivation/reperfusion injury. Apoptosis 2016, 21, 390–403. [Google Scholar] [CrossRef] [PubMed]
- Mehrbod, P.; Ande, S.R.; Alizadeh, J.; Rahimizadeh, S.; Shariati, A.; Malek, H.; Hashemi, M.; Glover, K.K.M.; Sher, A.A.; Coombs, K.M.; et al. The roles of apoptosis, autophagy and unfolded protein response in arbovirus, influenza virus, and HIV infections. Virulence 2019, 10, 376–413. [Google Scholar] [CrossRef]
- Chen, Y.; Brandizzi, F. IRE1: ER stress sensor and cell fate executor. Trends Cell Biol. 2013, 23, 547–555. [Google Scholar] [CrossRef]
- Novoa, I.; Zeng, H.; Harding, H.P.; Ron, D. Feedback inhibition of the unfolded protein response by GADD34-mediated dephosphorylation of eIF2alpha. J. Cell. Biol. 2001, 153, 1011–1022. [Google Scholar] [CrossRef]
- Mazan-Mamczarz, K.; Lal, A.; Martindale, J.L.; Kawai, T.; Gorospe, M. Translational repression by RNA-binding protein TIAR. Mol. Cell. Biol. 2006, 26, 2716–2727. [Google Scholar] [CrossRef] [PubMed]
- Schaljo, B.; Kratochvill, F.; Gratz, N.; Sadzak, I.; Sauer, I.; Hammer, M.; Vogl, C.; Strobl, B.; Muller, M.; Blackshear, P.J.; et al. Tristetraprolin is required for full anti-inflammatory response of murine macrophages to IL-10. J. Immunol. 2009, 183, 1197–1206. [Google Scholar] [CrossRef] [PubMed]
- Önal, U.; Valenzuela-Sánchez, F.; Vandana, K.E.; Rello, J. Mid-Regional Pro-Adrenomedullin (MR-proADM) as a Biomarker for Sepsis and Septic Shock: Narrative Review. Healthcare 2018, 6, 110. [Google Scholar] [CrossRef] [PubMed]
- Kawahara, K.; Hohjoh, H.; Inazumi, T.; Tsuchiya, S.; Sugimoto, Y. Prostaglandin E2-induced inflammation: Relevance of prostaglandin E receptors. Biochim. Biophys. Acta 2015, 1851, 414–421. [Google Scholar] [CrossRef]
- Wei, W.; Jiao, Y.; Postlethwaite, A.; Stuart, J.M.; Wang, Y.; Sun, D.; Gu, W. Dual-specificity phosphatases 2: Surprising positive effect at the molecular level and a potential biomarker of diseases. Genes Immunity 2013, 14, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ruan, Z.; Wang, S.; Yu, W.; Deng, F. LncRNA MALAT1 aggravates inflammation response through regulating PTGS2 by targeting miR-26b in myocardial ischemia-reperfusion injury. Int. J. Cardiol. 2019, 288, 122. [Google Scholar] [CrossRef] [PubMed]
- Bohlson, S.S.; O’Conner, S.D.; Hulsebus, H.J.; Ho, M.M.; Fraser, D.A. Complement, c1q, and c1q-related molecules regulate macrophage polarization. Front. Immunol. 2014, 5, 402. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Tan, B.; Yan, Y.; Ma, X.; Zhang, N.; Zhang, Z.; Liu, M.; Qian, M.; Du, B. Extracellular UDP and P2Y6 function as a danger signal to protect mice from vesicular stomatitis virus infection through an increase in IFN-β production. J. Immunol. 2014, 193, 4515–4526. [Google Scholar] [CrossRef] [PubMed]
- Yue, Y.; Huang, W.; Liang, J.; Guo, J.; Ji, J.; Yao, Y.; Zheng, M.; Cai, Z.; Lu, L.; Wang, J. IL4I1 Is a Novel Regulator of M2 Macrophage Polarization That Can Inhibit T Cell Activation via L-Tryptophan and Arginine Depletion and IL-10 Production. PLoS ONE 2015, 10, e0142979. [Google Scholar]
- Mielke, L.A.; Elkins, K.L.; Wei, L. Tumor progression locus 2 (Map3k8) is critical for host defense against Listeria monocytogenes and IL-1 beta production. J. Immunol. 2009, 183, 7984–7993. [Google Scholar] [CrossRef] [PubMed]
- Chae, J.J.; Wood, G.; Richard, K.; Jaffe, H.; Colburn, N.T.; Masters, S.L. The familial Mediterranean fever protein, pyrin, is cleaved by caspase-1 and activates NF-kappaB through its N-terminal fragment. Blood 2008, 112, 1794–1803. [Google Scholar] [CrossRef] [PubMed]
- Ko, C.Y.; Chang, W.C.; Wang, J.M. Biological roles of CCAAT/Enhancer-binding protein delta during inflammation. J. Biomed. Sci. 2015, 22, 6. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Tang, B.; Zhang, Z.; Xu, D.; Ma, G. DUSP6 Inhibitor (E/Z)-BCI Hydrochloride Attenuates Lipopolysaccharide-Induced Inflammatory Responses in Murine Macrophage Cells via Activating the Nrf2 Signaling Axis and Inhibiting the NF-kappaB Pathway. Inflammation 2019, 42, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Hamada, M.; Tsunakawa, Y.; Jeon, H.; Yadav, M.K.; Takahashi, S. Role of MafB in macrophages. Exp. Anim. 2020, 69, 19-0076. [Google Scholar] [CrossRef]
- Ma, Q.; Liu, Y.; Chen, L. JIP3 deficiency attenuates cardiac hypertrophy by suppression of JNK pathway. Biochem. Biophys. Res. Commun. 2018, 503, 1–7. [Google Scholar] [CrossRef]
- Kotrys, A.V.; Cysewski, D.; Czarnomska, S.D.; Pietras, Z.; Borowski, L.S.; Dziembowski, A.; Szczesny, R.J. Quantitative proteomics revealed C6orf203/MTRES1 as a factor preventing stress-induced transcription deficiency in human mitochondria. Nucleic Acids Res. 2019, 47, 7502–7517. [Google Scholar] [CrossRef]
- Blatteis, C.M.; Li, S.; Li, Z.; Feleder, C.; Perlik, V. Cytokines, PGE2 and endotoxic fever: A re-assessment. Prostaglandins Other Lipid Mediat. 2005, 76, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Soares, D.M.; Hiratsuka Veiga-Souza, F.; Fabrício, A.S.; Javier Miñano, F.; Petto Souza, G.E. CCL3/macrophage inflammatory protein-1alpha induces fever and increases prostaglandin E2 in cerebrospinal fluid of rats: Effect of antipyretic drugs. Brain Res. 2006, 1109, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Soares, D.M.; Machado, R.R.; Yamashiro, L.H.; Melo, M.C.; Souza, G.E. Cytokine-induced neutrophil chemoattractant (CINC)-1 induces fever by a prostaglandin-dependent mechanism in rats. Brain Res. 2008, 1233, 79–88. [Google Scholar] [CrossRef]
- Lachmann, H.J. Periodic fever syndromes. Best Pract. Res. Clin. Rheumatol. 2017, 31, 596–609. [Google Scholar] [CrossRef] [PubMed]
- Chesnokova, V.; Melmed, S. Leukemia inhibitory factor mediates the hypothalamic pituitary adrenal axis response to inflammation. Endocrinology 2000, 141, 4032–4040. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Daniel, J.A.; Whitlock, B.K.; Marks, D.L.; Gard, J.A.; Sartin, J.L. Leukemia inhibitory factor as a mediator of lipopolysaccharide effects on appetite and selected hormones and metabolites. J. Anim. Sci. 2016, 94, 2789–2797. [Google Scholar] [CrossRef] [PubMed]
- Kalinski, P. Regulation of immune responses by prostaglandin E2. J. Immunol. 2012, 188, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Sander, W.J.; O’Neill, H.G.; Pohl, C.H. Prostaglandin E2 As a Modulator of Viral Infections. Front. Physiol. 2017, 8, 89. [Google Scholar] [CrossRef]
- Dwivedi, P.; Greis, K.D. Granulocyte colony-stimulating factor receptor signaling in severe congenital neutropenia, chronic neutrophilic leukemia, and related malignancies. Exp. Hematol. 2017, 46, 9–20. [Google Scholar] [CrossRef]
- Stegelmeier, A.A.; van Vloten, J.P.; Mould, R.C.; Klafuric, E.M.; Minott, J.A.; Wootton, S.K.; Bridle, B.W.; Karimi, K. Myeloid Cells during Viral Infections and Inflammation. Viruses 2019, 11, 168. [Google Scholar] [CrossRef]
- Wajant, H.; Siegmund, D. TNFR1 and TNFR2 in the Control of the Life and Death Balance of Macrophages. Front. Cell Dev. Biol. 2019, 7, 91. [Google Scholar] [CrossRef]
- Sánchez-Jiménez, C.; Izquierdo, J.M. T-cell intracellular antigens in health and disease. Cell Cycle. 2015, 14, 2033–2043. [Google Scholar] [CrossRef]
- Rojas, J.M.; Avia, M.; Martín, V.; Sevilla, N. IL-10: A Multifunctional Cytokine in Viral Infections. J. Immunol. Res. 2017, 2017, 6104054. [Google Scholar] [CrossRef]
- Said, E.A.; Dupuy, F.P.; Trautmann, L.; Zhang, Y.; Shi, Y.; El-Far, M.; Hill, B.J.; Noto, A.; Ancuta, P.; Peretz, Y.; et al. Programmed death-1-induced interleukin-10 production by monocytes impairs CD4+ T cell activation during HIV infection. Nat. Med. 2010, 16, 452–459. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.A.; Schnyder-Candrian, S.; Schnyder, B.; Quesniaux, V.; Poli, V.; Stewart, C.L.; Ryffel, B. Endogenous leukemia inhibitory factor attenuates endotoxin response. Lab. Invest. 2005, 85, 276–284. [Google Scholar] [CrossRef]
- Davis, S.M.; Collier, L.A.; Winford, E.D.; Leonardo, C.C.; Ajmo, C.T.; Foran, E.A.; Kopper, T.J.; Gensel, J.C.; Pennypacker, K.R. Leukemia inhibitory factor modulates the peripheral immune response in a rat model of emergent large vessel occlusion. J. Neuroinflammation. 2018, 15, 288. [Google Scholar] [CrossRef] [PubMed]
- Metcalfe, S. LIF in the regulation of T-cell fate and as a potential therapeutic. Genes Immunity 2011, 12, 157–168. [Google Scholar] [CrossRef] [PubMed]
- Takahara, T.; Fukuyama, Y.; Saito, S.; Ogino, T.; Miyajima, N.; Kohase, M. Il-1, EGF, and HGF suppress the antiviral activity of interferon in primary monkey hepatic parenchymal cells. Jpn. J. Infect. Dis. 1999, 52, 458. [Google Scholar] [CrossRef]
- Kato, H.; Takeuchi, O.; Sato, S.; Yoneyama, M.; Yamamoto, M.; Matsui, K.; Uematsu, S.; Jung, A.; Kawai, T.; Ishii, K.J.; et al. Differential roles of MDA5 and RIG-I helicases in the recognition of RNA viruses. Nature 2006, 441, 101–105. [Google Scholar] [CrossRef]
- Meylan, E.; Curran, J.; Hofmann, K.; Moradpour, D.; Binder, M.; Bartenschlager, R.; Tschopp, J. Cardif is an adaptor protein in the RIG-I antiviral pathway and is targeted by hepatitis C virus. Nature 2005, 437, 1167–1172. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.Y.; Chen, W.; Wei, B.; Shan, Y.F.; Wang, C. IFN-induced TPR protein IFIT3 potentiates antiviral signaling by bridging MAVS and TBK1. J. Immunol. 2011, 187, 2559–2568. [Google Scholar] [CrossRef]
- Georgel, P.; Jiang, Z.; Kunz, S.; Janssen, E.; Mols, J.; Hoebe, K.; Bahram, S.; Oldstone, M.B.; Beutler, B. Vesicular stomatitis virus glycoprotein G activates a specific antiviral Toll-like receptor 4-dependent pathway. Virology 2007, 362, 304–313. [Google Scholar] [CrossRef]
- de Marcken, M.; Dhaliwal, K.; Danielsen, A.C.; Gautron, A.S.; Dominguez-Villar, M. TLR7 and TLR8 activate distinct pathways in monocytes during RNA virus infection. Sci. Signal. 2019, 12, eaaw1347. [Google Scholar] [CrossRef] [PubMed]
- Solmaz, G.; Puttur, F.; Francozo, M.; Lindenberg, M.; Guderian, M.; Swallow, M.; Duhan, V.; Khairnar, V.; Kalinke, U.; Ludewig, B.; et al. TLR7 Controls VSV Replication in CD169+ SCS Macrophages and Associated Viral Neuroinvasion. Front. Immunol. 2019, 10, 466. [Google Scholar] [CrossRef]
- Honda, K.; Takaoka, A.; Taniguchi, T. Type I interferon [corrected] gene induction by the interferon regulatory factor family of transcription factors. Immunity 2006, 25, 349–360. [Google Scholar] [CrossRef] [PubMed]
- Marié, I.; Durbin, J.E.; Levy, D.E. Differential viral induction of distinct interferon-alpha genes by positive feedback through interferon regulatory factor-7. EMBO J. 1998, 17, 6660–6669. [Google Scholar] [CrossRef]
- Lagos, D.; Pollara, G.; Henderson, S.; Gratrix, F.; Fabani, M.; Milne, R.S.; Gotch, F.; Boshoff, C. miR-132 regulates antiviral innate immunity through suppression of the p300 transcriptional co-activator. Nat. Cell. Biol. 2010, 12, 513–519. [Google Scholar] [CrossRef]
- Zhang, F.; Lin, X.; Yang, X.; Lu, G.; Zhang, Q.; Zhang, C. MicroRNA-132-3p suppresses type I IFN response through targeting IRF1 to facilitate H1N1 influenza A virus infection. Biosci. Rep. 2019, 39, BSR20192769. [Google Scholar] [CrossRef]
- Chan, S.W. The unfolded protein response in virus infections. Front. Microbiol. 2014, 5, 518. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, J.; Reis e Sousa, C.; Schito, M.; Hieny, S.; Wells, T.; Huffnagle, G.B.; Sher, A. CCR5 provides a signal for microbial induced production of IL-12 by CD8 alpha+ dendritic cells. Nat. Immunol. 2000, 1, 83–87. [Google Scholar] [CrossRef]
- Shaheen, Z.R.; Christmann, B.S.; Stafford, J.D.; Moran, J.M.; Buller, R.M.L.; Corbett, J.A. CCR5 is a required signaling receptor for macrophage expression of inflammatory genes in response to viral double-stranded RNA. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2019, 316, R525–R534. [Google Scholar] [CrossRef] [PubMed]
- Polzin, M.; McCanless, J.; Owen, S.; Sizemore, D.; Lucero, E.; Fuller, R.; Neufeld, H.S.; Seals, D.F.; Ahmed, M. Oncolytic vesicular stomatitis viruses selectively target M2 macrophages. Virus Res. 2020, 284, 197991. [Google Scholar] [CrossRef]
- Ma, Y.; Wei, Y.; Zhang, X.; Zhang, Y.; Cai, H.; Zhu, Y.; Shilo, K.; Oglesbee, M.; Krakowka, S.; Whelan, S.P.; et al. mRNA cap methylation influences pathogenesis of vesicular stomatitis virus in vivo. J. Virol. 2014, 88, 2913–2926. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, M.; Jing, Q.; Georgel, P.; New, L.; Chen, J.; Mols, J.; Kang, Y.J.; Jiang, Z.; Du, X.; Cook, R.; et al. Hypersusceptibility to vesicular stomatitis virus infection in Dicer1-deficient mice is due to impaired miR24 and miR93 expression. Immunity 2007, 27, 123–134. [Google Scholar] [CrossRef] [PubMed]
- Connor, J.H.; Lyles, D.S. Inhibition of host and viral translation during vesicular stomatitis virus infection. eIF2 is responsible for the inhibition of viral but not host translation. J. Biol. Chem. 2005, 280, 13512–13519. [Google Scholar] [CrossRef] [PubMed]
- Baltzis, D.; Qu, L.K.; Papadopoulou, S.; Blais, J.D.; Bell, J.C.; Sonenberg, N.; Koromilas, A.E. Resistance to vesicular stomatitis virus infection requires a functional cross talk between the eukaryotic translation initiation factor 2alpha kinases PERK and PKR. J. Virol. 2004, 78, 12747–12761. [Google Scholar] [CrossRef]
- Martinez, I.; Rodriguez, L.L.; Jimenez, C.; Pauszek, S.J.; Wertz, G.W. Vesicular stomatitis virus glycoprotein is a determinant of pathogenesis in swine, a natural host. J. Virol. 2003, 77, 8039–8047. [Google Scholar] [CrossRef]
- Martinez, I.; Wertz, G.W. Biological differences between vesicular stomatitis virus Indiana and New Jersey serotype glycoproteins: Identification of amino acid residues modulating pH-dependent infectivity. J. Virol. 2005, 79, 3578–3585. [Google Scholar] [CrossRef][Green Version]
- Morozov, I.; Davis, A.S.; Ellsworth, S.; Trujillo, J.D.; McDowell, C.; Shivanna, V.; Dasen, E.J.; Nichols, R.; Martin, B.K.; Monath, T.P.; et al. Comparative evaluation of pathogenicity of three isolates of vesicular stomatitis virus (Indiana serotype) in pigs. J. Gen. Virol. 2019, 100, 1478–1490. [Google Scholar] [CrossRef]
- Zsak, L.; Lu, Z.; Kutish, G.F.; Neilan, J.G.; Rock, D.L. An African swine fever virus virulence-associated gene NL-S with similarity to the herpes simplex virus ICP34.5 gene. J. Virol. 1996, 70, 8865–8871. [Google Scholar] [CrossRef]
- Velazquez-Salinas, L.; Pauszek, S.J.; Verdugo-Rodriguez, A.; Rodriguez, L.L. Complete Genome Sequences of Two Vesicular Stomatitis New Jersey Viruses Representing the 2012 U.S. Epidemic Strain and Its Closest Relative Endemic Strain from Southern Mexico. Genome Announc. 2018, 6, e00049-18. [Google Scholar] [CrossRef]
- Zhu, J.J.; Ramanathan, P.; Bishop, E.A.; O’Donnell, V.; Gladue, D.P.; Borca, M.V. Mechanisms of African swine fever virus pathogenesis and immune evasion inferred from gene expression changes in infected swine macrophages. PLoS ONE 2019, 14, e0223955. [Google Scholar] [CrossRef]
- Huang, X.; Madan, A. CAP3: A DNA sequence assembly program. Genome Res. 1999, 9, 868–877. [Google Scholar] [CrossRef] [PubMed]
- Smyth, G.; Gentleman, R.; Carey, V.; Dudoit, S.; Irizarry, R.; Huber, W. Limma: Linear Models for Microarray Data, Bioinformatics and Computational Biology Solutions Using R and Bioconductor; Springer: New York, NY, USA, 2005; pp. 397–420. [Google Scholar]
| Pathway Analysis | Count | Benjamini | |
|---|---|---|---|
| DEGs with at Least 2-Fold Differential Expression | GO_0007249: I-kappa B kinase/NF-kappa B signaling | 23 | 8.2 × 105 |
| GO_0016567: protein ubiquitination | 62 | 0.026 | |
| GO_0035666: TRIF-dependent toll-like receptor signaling pathway | 12 | 0.036 | |
| GO_0045944: positive regulation of transcription by RNA polymerase II | 135 | 0.045 | |
| KEGG_hsa04668: TNF signaling pathway | 34 | 6.4 × 107 | |
| KEGG_hsa04620: Toll-like receptor signaling pathway | 33 | 1.0 × 106 | |
| KEGG_hsa04064: NF-kappa B signaling pathway | 28 | 5.4 × 106 | |
| KEGG_hsa04622: RIG-I-like receptor signaling pathway | 21 | 5.7 × 104 | |
| KEGG_hsa04621: NOD-like receptor signaling pathway | 16 | 0.011 | |
| KEGG_hsa04144: Endocytosis | 43 | 0.012 | |
| KEGG_hsa05160: Hepatitis C | 27 | 0.022 | |
| KEGG_hsa05169: Epstein-Barr virus infection | 25 | 0.026 | |
| KEGG_hsa04210: Apoptosis | 16 | 0.029 | |
| KEGG_hsa05220: Chronic myeloid leukemia | 17 | 0.043 | |
| KEGG_hsa04140: Regulation of autophagy | 9 | 0.050 | |
| REACTOME_HSA-5357786: TNFR1-induced proapoptotic signaling | 8 | 0.039 | |
| DEGs with at Least 4-Fold Differential Expression | GO_0006954: inflammatory response | 19 | 1.2 × 105 |
| GO_0006915: apoptotic process | 20 | 5.4 × 104 | |
| GO_0045944: positive regulation of transcription by RNA polymerase II | 25 | 0.003 | |
| GO_0006955: immune response | 15 | 0.009 | |
| GO_0043065: positive regulation of apoptotic process | 12 | 0.019 | |
| GO_0071222: cellular response to lipopolysaccharide | 8 | 0.020 | |
| GO_0051897: positive regulation of protein kinase B signaling | 7 | 0.021 | |
| GO_0042981: regulation of apoptotic process | 10 | 0.022 | |
| GO_0070373: negative regulation of ERK1 and ERK2 cascade | 6 | 0.026 | |
| GO_2001244: positive regulation of intrinsic apoptotic signaling pathway | 5 | 0.029 | |
| GO_0030593: neutrophil chemotaxis | 6 | 0.036 | |
| GO_0051384: response to glucocorticoid | 6 | 0.037 | |
| GO_0070098: chemokine-mediated signaling pathway | 6 | 0.047 | |
| KEGG_hsa04060: Cytokine–cytokine receptor interaction | 15 | 3.8 × 105 | |
| KEGG_hsa04668: TNF signaling pathway | 11 | 4.7 × 105 | |
| KEGG_hsa04064: NF-kappa B signaling pathway | 7 | 0.016 | |
| KEGG_hsa04621: NOD-like receptor signaling pathway | 6 | 0.020 | |
| KEGG_hsa04620: Toll-like receptor signaling pathway | 7 | 0.027 | |
| Reactome-HSA-380108: Chemokine receptors bind chemokines | 7 | 0.003 |
| Group | Gene | EXP | EP/M | FDR | EP/EN | FDR |
|---|---|---|---|---|---|---|
| IFN and Signaling | IFNA17 | 77 | −1.9 | 0.01 | −1.1 | 0.96 |
| IFNB | 179 | 6.2 | 0.04 | −2.1 | 0.79 | |
| IFNAR1 | 3774 | −2.0 | 0.01 | 1.0 | 0.97 | |
| IFNAR2 | 2223 | −2.9 | 0.03 | −1.2 | 0.90 | |
| IFNGR1 | 1000 | −2.7 | 0.02 | −1.2 | 0.92 | |
| Ten Typical Interferon Stimulated Genes | IFI44L | 955 | 1.1 | 0.88 | 1.2 | 0.82 |
| IFIH1 | 107 | −1.1 | 0.92 | −1.0 | 1.00 | |
| IFIT1 | 231 | 1.7 | 0.52 | −1.4 | 0.89 | |
| IFIT2 | 420 | −2.4 | 0.23 | 1.0 | 0.99 | |
| IFIT3 | 3298 | −1.6 | 0.27 | 1.2 | 0.89 | |
| IFIT5 | 364 | −2.0 | 0.10 | 1.4 | 0.80 | |
| ISG20 | 580 | 1.2 | 0.91 | 1.3 | 0.96 | |
| MX1 | 3882 | −1.2 | 0.90 | −1.0 | 0.99 | |
| MX2 | 1330 | −1.5 | 0.56 | 1.2 | 0.94 | |
| OAS1 | 155 | −1.1 | 0.95 | 1.1 | 0.98 | |
| IFN Expression Inhibitors | AHR | 193 | 6.1 | 0.01 | −1.0 | 0.98 |
| ATF3 | 1432 | 8.6 | 0.05 | −1.6 | 0.91 | |
| DUSP1 | 2208 | 13.8 | 0.01 | −1.6 | 0.88 | |
| EGR1 | 891 | 13.4 | 0.01 | −2.1 | 0.79 | |
| FOS | 1993 | 22.9 | 0.01 | −1.7 | 0.90 | |
| HES1 | 218 | 10.6 | 0.02 | −1.2 | 0.97 | |
| PRDM1 | 796 | 32.8 | 0.01 | −1.9 | 0.86 |
| Pathway | Gene | EXP | EP/M | FDR | EP/EN | FDR |
|---|---|---|---|---|---|---|
| MAPK | ATF2 | 300 | −2.4 | 0.01 | 1.3 | 0.75 |
| MAP2K5 | 1804 | −1.7 | 0.02 | 1.0 | 0.99 | |
| MAPK14/p38 | 539 | −3.2 | 0.03 | 1.0 | 1.00 | |
| MAPK4 | 176 | −2.8 | 0.02 | 1.4 | 0.79 | |
| MAP3K18 | 2279 | −4.3 | 0.00 | 1.1 | 0.98 | |
| NFκB | CARD6 | 404 | −2.6 | 0.01 | 1.1 | 0.95 |
| IKBKB | 907 | −2.2 | 0.01 | −1.0 | 0.99 | |
| IRAK1 | 5234 | −3.5 | 0.00 | −1.0 | 0.98 | |
| NLK/NEMO | 170 | −3.3 | 0.01 | 1.2 | 0.88 | |
| TAB1 | 1817 | −2.2 | 0.03 | 1.1 | 0.98 | |
| TAB2 | 416 | −2.7 | 0.00 | 1.1 | 0.91 | |
| TAK1 | 440 | −2.1 | 0.01 | 1.2 | 0.80 | |
| NFKBIA | 10873 | 7.9 | 0.01 | −1.2 | 0.95 | |
| NFKBID | 1182 | 4.2 | 0.03 | −1.6 | 0.81 | |
| TNFAIP3/A20 | 799 | 8.3 | 0.00 | −1.4 | 0.88 | |
| RIG-I | IRF5 | 3796 | −2.1 | 0.01 | −1.1 | 0.95 |
| MAVS | 452 | −2.1 | 0.03 | −1.1 | 0.95 | |
| TBK1 | 459 | −2.0 | 0.05 | −1.1 | 0.97 | |
| Toll-like Receptor | BTK | 4636 | −2.0 | 0.01 | 1.2 | 0.82 |
| TLR1 | 361 | −2.8 | 0.02 | 1.2 | 0.93 | |
| TLR2 | 11817 | −3.8 | 0.00 | −1.1 | 0.94 | |
| TLR4 | 543 | −3.8 | 0.01 | 1.0 | 0.99 | |
| TICAM2/TRIF | 129 | −2.8 | 0.02 | 1.3 | 0.84 | |
| TLR6 | 143 | −3.3 | 0.01 | 1.2 | 0.91 | |
| TLR7 | 293 | 1.7 | 0.03 | 1.0 | 0.99 |
| Group | Gene | EXP | EP/M | FDR | EP/EN | FDR |
|---|---|---|---|---|---|---|
| Cytokines | CSF3 | 750 | 4.0 | 0.05 | −1.3 | 0.93 |
| IL1A | 698 | 13.9 | 0.02 | −1.9 | 0.87 | |
| IL1B | 1793 | 7.7 | 0.13 | −1.7 | 0.92 | |
| IL10 | 1109 | 11.5 | 0.00 | −1.9 | 0.76 | |
| IL27 | 318 | 3.8 | 0.01 | −1.9 | 0.67 | |
| TNF | 2641 | 23.4 | 0.01 | −1.7 | 0.87 | |
| TNFSF9/CD137L | 369 | 5.2 | 0.02 | −2.4 | 0.66 | |
| TNFSF11 | 729 | −4.5 | 0.02 | 1.2 | 0.94 | |
| AREG | 258 | 17.5 | 0.01 | −1.6 | 0.91 | |
| HBEGF | 673 | 4.7 | 0.04 | −1.3 | 0.94 | |
| LIF | 217 | 12.9 | 0.01 | −1.9 | 0.79 | |
| VEGFA | 384 | 5.7 | 0.03 | −1.6 | 0.86 | |
| Cytokine Receptors | IL1R2 | 219 | 2.9 | 0.04 | −1.3 | 0.88 |
| IL17RA | 4899 | −1.7 | 0.02 | 1.0 | 0.98 | |
| IL20RB | 92 | 2.7 | 0.03 | −1.4 | 0.80 | |
| LTBR | 8211 | −3.5 | 0.01 | 1.1 | 0.95 | |
| TNFRSF1A | 3943 | −2.3 | 0.01 | −1.0 | 1.00 |
| Group | Gene | EXP | EP/M | FDR | EP/EN | FDR |
|---|---|---|---|---|---|---|
| CCLs | CCL3 | 2336 | 7.4 | 0.01 | −1.8 | 0.80 |
| CCL4 | 3028 | 29.1 | 0.00 | −2.1 | 0.79 | |
| CCL5 | 6487 | 3.1 | 0.06 | −1.4 | 0.88 | |
| CCL5_v | 385 | 23.0 | 0.01 | −1.6 | 0.90 | |
| CCL20 | 412 | 17.7 | 0.01 | −1.4 | 0.94 | |
| ELR+ CXCLs | CXCL1 | 1791 | 6.4 | 0.03 | −1.1 | 0.98 |
| CXCL2 | 3008 | 21.2 | 0.00 | −1.9 | 0.81 | |
| CXCL3 | 2388 | 6.8 | 0.02 | −1.5 | 0.90 | |
| CCL/CXCL Receptors | CCR5 | 246 | −2.8 | 0.02 | −1.0 | 1.00 |
| CCR7 | 206 | 4.5 | 0.00 | −1.3 | 0.84 | |
| CCRL2 | 1839 | −1.8 | 0.02 | 1.1 | 0.94 | |
| CX3CR1 | 129 | −2.2 | 0.02 | 1.1 | 0.92 | |
| CXCR4 | 1060 | 4.3 | 0.02 | −1.1 | 0.98 |
| Group | Gene | EXP | EP/MM | FDR | EP/EN | FDR |
|---|---|---|---|---|---|---|
| Apoptosis and Death Receptor Signaling | BCL2L13 | 1167 | −2.0 | 0.01 | 1.2 | 0.77 |
| CASP8 | 337 | −2.1 | 0.02 | 1.1 | 0.90 | |
| DAPK1 | 246 | −2.2 | 0.01 | 1.1 | 0.96 | |
| DIDO1 | 162 | −2.1 | 0.02 | 1.3 | 0.75 | |
| BIRC3/cIAP2 | 656 | 3.5 | 0.01 | −1.2 | 0.90 | |
| REL | 100 | 4.8 | 0.02 | −2.4 | 0.66 | |
| SGK1 | 2392 | 4.1 | 0.01 | −1.4 | 0.86 | |
| BRE | 184 | 2.9 | 0.05 | −2.0 | 0.68 | |
| FADD | 145 | −2.2 | 0.04 | −1.0 | 1.00 | |
| IER3 | 988 | 5.6 | 0.02 | −1.5 | 0.87 | |
| RIPK1 | 1864 | −2.1 | 0.01 | −1.1 | 0.91 | |
| TRADD | 3504 | −2.1 | 0.03 | −1.0 | 0.98 | |
| Autophagy | ATG3 | 2041 | −1.8 | 0.03 | 1.1 | 0.92 |
| ATG4B | 1154 | −2.8 | 0.01 | 1.0 | 0.99 | |
| ATG5 | 524 | −2.1 | 0.05 | 1.2 | 0.88 | |
| ATG9A | 977 | −2.2 | 0.00 | 1.1 | 0.96 | |
| ATG16L1 | 351 | −2.3 | 0.01 | −1.3 | 0.72 | |
| ATG16L2 | 1146 | −2.1 | 0.00 | −1.1 | 0.95 | |
| ATG101 | 1026 | −2.7 | 0.01 | −1.1 | 0.95 | |
| FLCN | 771 | −4.8 | 0.01 | −1.1 | 0.97 | |
| RAB33B | 241 | −3.0 | 0.00 | 1.4 | 0.70 | |
| RB1CC1 | 147 | −1.9 | 0.03 | 1.1 | 0.97 | |
| ULK1 | 1083 | −1.8 | 0.03 | −1.1 | 0.96 | |
| BCL2L11/BIM | 152 | 4.3 | 0.00 | −1.6 | 0.71 | |
| GADD45B | 649 | 22.6 | 0.00 | −1.6 | 0.86 | |
| UPR | ERN1 | 146 | −2.6 | 0.02 | 1.0 | 0.99 |
| PPP1R15A | 850 | 7.0 | 0.01 | −1.5 | 0.85 | |
| XBP1 | 4634 | −6.1 | 0.01 | 1.1 | 0.98 |
| Group | Gene | EXP | EP/M | FDR | EP/EN | FDR |
|---|---|---|---|---|---|---|
| mRNA transcription | CDK7 | 359 | −3.1 | 0.01 | 1.2 | 0.91 |
| GTF2A1 | 534 | −2.5 | 0.00 | 1.3 | 0.72 | |
| GTF2B | 1429 | −2.2 | 0.05 | 1.2 | 0.92 | |
| GTF2E1 | 176 | −2.2 | 0.02 | 1.1 | 0.97 | |
| MNAT1 | 217 | −1.7 | 0.03 | 1.2 | 0.84 | |
| RPAP3 | 161 | −1.6 | 0.05 | 1.0 | 0.99 | |
| TAF1C | 481 | −3.1 | 0.03 | −1.2 | 0.94 | |
| TAF7 | 716 | −2.7 | 0.01 | 1.2 | 0.89 | |
| TAF11 | 882 | −3.2 | 0.03 | 1.1 | 0.97 | |
| TBP | 1191 | −1.8 | 0.01 | 1.2 | 0.92 | |
| TCEANC2 | 130 | −2.6 | 0.01 | 1.3 | 0.75 | |
| TCF20 | 348 | −2.2 | 0.03 | −1.0 | 0.98 | |
| TFCP2 | 248 | −1.9 | 0.01 | 1.1 | 0.91 | |
| mRNA processing | CMTR2 | 180 | −3.5 | 0.01 | 1.3 | 0.83 |
| DICER1 | 1024 | −2.4 | 0.02 | −1.1 | 0.98 | |
| MIR132 | 78 | 3.3 | 0.03 | −2.7 | 0.54 | |
| TIAL1 | 93 | −3.7 | 0.04 | −1.3 | 0.88 | |
| ZFP36/TTP | 5049 | 4.5 | 0.03 | −2.0 | 0.74 |
| Group | Gene | EXP | EP/M | FDR | EP/EN | FDR |
|---|---|---|---|---|---|---|
| Inflammation mediator | ADM | 331 | 5.9 | 0.01 | −1.3 | 0.90 |
| DUSP2 | 2264 | 3.8 | 0.01 | −1.0 | 0.99 | |
| MALAT1 | 125 | 6.0 | 0.01 | −1.7 | 0.75 | |
| PTGS2 | 300 | 15.6 | 0.02 | −1.3 | 0.95 | |
| Macrophage activation | C5AR1 | 10355 | −3.0 | 0.01 | 1.1 | 0.94 |
| IL4I1 | 297 | 3.6 | 0.01 | −1.2 | 0.89 | |
| P2RY1 | 505 | −7.3 | 0.00 | 1.1 | 0.96 | |
| P2RY6 | 290 | −2.6 | 0.05 | 1.1 | 0.97 | |
| Immune stimulators | MAP3K8 | 779 | 10.0 | 0.00 | −1.5 | 0.85 |
| MEFV | 1158 | 6.7 | 0.03 | −1.7 | 0.85 | |
| CEBPD | 2210 | −9.3 | 0.02 | −1.1 | 0.99 | |
| DUSP6 | 4285 | −6.3 | 0.01 | 1.0 | 1.00 | |
| MAFB | 3002 | −10.0 | 0.00 | −1.3 | 0.91 | |
| MAPK8IP3/JIP3 | 1932 | −5.8 | 0.01 | 1.0 | 1.00 | |
| MTRES1 | 1804 | −9.7 | 0.00 | 1.2 | 0.93 |
| Pathogenesis | Mechanism Inferred from Differentially Expressed Genes |
|---|---|
| Systemic | Fever: ↑ CCLs [3, 4, 5], CXCLs [1, 2, 3], IL1A, PGTS2, TNF |
| Anorexia: ↑ LIF, PGTS2 | |
| Systemic infection restriction: ↑ IFNB, VSV sensitive to IFN inhibition | |
| Local Tissue | Immune cell infiltration: ↑ CCLs [3, 4, 5, 20], CXCLs [1, 2, 3], PTGS2 |
| Inflammation: ↑ ADM, PGTS2 | |
| Vasodilatation: ↑ PGTS2 | |
| Necroptosis/apoptosis: ↑ TNF, ↓ TIAL1 | |
| Infected/Non-infected Cells | ↓ General immune response: ↑ IL10 |
| ↓ Interferon response: ↑ AREG, HBEGF, VEGF, IL1A | |
| ↓ MΦ, neutrophils, Th1, CTL, NK cell activities: ↑ PGE/PGTS2 | |
| ↓ Th17 response: ↑ LIF; ↓ IL17RA | |
| Infected Cells | ↓ IFNB production: ↑ AHR, ATF3, DUSP1, FOS, HES1, PRDM1; ↓ ATF2, XBP1 |
| ↓ MAPK signaling: ↓ MAPK4, MAPK14/p38, MAP3K18 | |
| ↓ RIG-I signaling: ↓ IRF5, MAVS, TBK1 | |
| ↓ NFκB signaling: ↑ NFKBIA, NFKBID, A20; ↓ TNFSF11, 7 DEGs | |
| ↓ TLR4 signaling: ↓ BTK, TICAM2, TLR4 | |
| ↓ Interferon signaling: ↓ IFNAR1, IFNAR2, IFNGR1, ↑ ATF3 | |
| ↓ Apoptosis and/or autophagy: ↑ GADD45B, ↓ 18 DEGs (Table 6) | |
| ↓ TNF signaling: ↓ FADD, RIPK1, TNFRSF1A, TRADD; ↑ BRE, IER3 | |
| ↓ Unfolded protein response: ↓ ERN1, XBP1, ↑ GADD34 | |
| ↓ AT-rich (cytokine) mRNA stability: ↑ ZFP36 | |
| ↓ Host mRNA cap-methylation/translation: ↓ CMTR2 | |
| ↓ Host transcription: ↓ 13 DEGs involved in RNA transcription (Table 7) | |
| ↓ MΦ M1 activation: ↓C5AR1, CCR5, IL17RA, Y2RY1, Y2RY6; ↑IL4I1, TNFSF9 | |
| ↑ VSV replication (↓ ISG expression): ↑MIR132 | |
| ↑ VSV replication (unknown mechanisms): ↓ DICER1, ↑ TLR7 | |
| ↑ VSV protein synthesis via eIF2α dephosphorylation: ↑ GADD34 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Velazquez-Salinas, L.; Canter, J.A.; Zhu, J.J.; Rodriguez, L.L. Molecular Pathogenesis and Immune Evasion of Vesicular Stomatitis New Jersey Virus Inferred from Genes Expression Changes in Infected Porcine Macrophages. Pathogens 2021, 10, 1134. https://doi.org/10.3390/pathogens10091134
Velazquez-Salinas L, Canter JA, Zhu JJ, Rodriguez LL. Molecular Pathogenesis and Immune Evasion of Vesicular Stomatitis New Jersey Virus Inferred from Genes Expression Changes in Infected Porcine Macrophages. Pathogens. 2021; 10(9):1134. https://doi.org/10.3390/pathogens10091134
Chicago/Turabian StyleVelazquez-Salinas, Lauro, Jessica A. Canter, James J. Zhu, and Luis L. Rodriguez. 2021. "Molecular Pathogenesis and Immune Evasion of Vesicular Stomatitis New Jersey Virus Inferred from Genes Expression Changes in Infected Porcine Macrophages" Pathogens 10, no. 9: 1134. https://doi.org/10.3390/pathogens10091134
APA StyleVelazquez-Salinas, L., Canter, J. A., Zhu, J. J., & Rodriguez, L. L. (2021). Molecular Pathogenesis and Immune Evasion of Vesicular Stomatitis New Jersey Virus Inferred from Genes Expression Changes in Infected Porcine Macrophages. Pathogens, 10(9), 1134. https://doi.org/10.3390/pathogens10091134







