Lessons Learned from an Experience with Vancomycin-Intermediate Staphylococcus aureus Outbreak in a Newly Built Secondary Hospital in Korea
Abstract
1. Introduction
2. Results
2.1. Clinical Characteristics of Subjects with Vancomycin-Intermediate Staphylococcus aureus Isolates
2.2. Microbiological Characteristics of Vancomycin-Intermediate Staphylococcus aureus
2.3. Amount of Vancomycin Used and Changes in the Vancomycin Minimum Inhibitory Concentration for Staphylococcus aureus
3. Discussion
4. Materials and Methods
4.1. Setting
4.2. Outbreak and Intervention
4.3. Laboratory Tests for Staphylococcus aureus
4.4. Vancomycin Consumption and the Vancomycin Minimum Inhibitory Concentrations of Staphylococcus aureus Isolates
4.5. Case Definition
4.6. Ethics
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Globally, T.D.-R.I. Final Report and Recommendations the Review on Antimicrobial Resistance Chaired by Jim O’neill. 2016. Available online: https://www.biomerieuxconnection.com/wp-content/uploads/2018/04/Tackling-Drug-Resistant-Infections-Globally_-Final-Report-and-Recommendations.pdf (accessed on 24 October 2020).
- Ena, J.; Dick, R.W.; Jones, R.N.; Wenzel, R.P. The epidemiology of intravenous vancomycin usage in a university hospital: A 10-year study. JAMA 1993, 269, 598–602. [Google Scholar] [CrossRef]
- Hiramatsu, K.; Hanaki, H.; Ino, T.; Yabuta, K.; Oguri, T.; Tenover, F. Methicillin-resistant Staphylococcus aureus clinical strain with reduced vancomycin susceptibility. J. Antimicrob. Chemother. 1997, 40, 135–136. [Google Scholar] [CrossRef] [PubMed]
- Tenover, F.C.; Biddle, J.W.; Lancaster, M.V. Increasing resistance to vancomycin and other glycopeptides in Staphylococcus aureus. Emerg. Infect. Dis. 2001, 7, 327. [Google Scholar] [CrossRef]
- Aref, S.; Masoud, D.; Taati, M.M.; Somayeh, Y.; Davood, D.-S. Global prevalence and distribution of vancomycin resistant, vancomycin intermediate and heterogeneously vancomycin intermediate Staphylococcus aureus clinical isolates: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 1–20. [Google Scholar]
- Park, J.W.; Lee, H.; Kim, J.W.; Kim, B. Characterization of infections with vancomycin-intermediate Staphylococcus aureus (VISA) and Staphylococcus aureus with reduced vancomycin susceptibility in South Korea. Sci. Rep. 2019, 9, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Korea Centers for Disease Control and Prevention. Infectious Disease Portal. Available online: http://www.kdca.go.kr/npt/biz/npp/ist/bass/bassDissStatsMain.do (accessed on 26 October 2020).
- de Lassence, A.; Hidri, N.; Timsit, J.-F.; Joly-Guillou, M.-L.; Thiery, G.; Boyer, A.; Lable, P.; Blivet, A.; Kalinowski, H.; Martin, Y. Control and outcome of a large outbreak of colonization and infection with glycopeptide-intermediate Staphylococcus aureus in an intensive care unit. Clin. Infect. Dis. 2006, 42, 170–178. [Google Scholar] [CrossRef][Green Version]
- Sakai, Y.; Qin, L.; Miura, M.; Masunaga, K.; Tanamachi, C.; Iwahashi, J.; Kida, Y.; Takasu, O.; Sakamoto, T.; Watanabe, H. Successful infection control for a vancomycin-intermediate Staphylococcus aureus outbreak in an advanced emergency medical service centre. J. Hosp. Infect. 2016, 92, 385–391. [Google Scholar] [CrossRef]
- Cosgrove, S.; Carroll, K.; Perl, T. Staphylococcus aureus with reduced susceptibility to vancomycin. Clin. Infect. Dis. 2004, 39, 539–545. [Google Scholar] [CrossRef]
- Gardete, S.; Tomasz, A. Mechanisms of vancomycin resistance in Staphylococcus aureus. J. Clin. Invest. 2014, 124, 2836–2840. [Google Scholar] [CrossRef]
- Kim, M.-N.; Hwang, S.H.; Pyo, Y.-J.; Mun, H.-M.; Pai, C.H. Clonal Spread of Staphylococcus aureus Heterogeneously Resistant to Vancomycin in a University Hospital in Korea. J. Clin. Microbiol. 2002, 40, 1376–1380. [Google Scholar] [CrossRef]
- Kim, J.W.; Kang, G.S.; Yoo, J.I.; Kim, H.S.; Lee, Y.S.; Yu, J.-Y.; Lee, K.-J.; Park, C.; Kim, I.-H. Molecular Typing and Resistance Profiles of Vancomycin-Intermediate Staphylococcus aureus in Korea: Results from a National Surveillance Study, 2007–2013. Ann. Clin. Microbiol. 2016, 19, 88–96. [Google Scholar] [CrossRef][Green Version]
- Kim, E.S.; Song, J.S.; Lee, H.J.; Choe, P.G.; Park, K.H.; Cho, J.H.; Park, W.B.; Kim, S.-H.; Bang, J.-H.; Kim, D.-M. A survey of community-associated methicillin-resistant Staphylococcus aureus in Korea. J. Antimicrob. Chemother. 2007, 60, 1108–1114. [Google Scholar] [CrossRef] [PubMed]
- Harbarth, S.; Dharan, S.; Liassine, N.; Herrault, P.; Auckenthaler, R.; Pittet, D. Randomized, placebo-controlled, double-blind trial to evaluate the efficacy of mupirocin for eradicating carriage of methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 1999, 43, 1412–1416. [Google Scholar] [CrossRef] [PubMed]
- Laupland, K.B.; Conly, J.M. Treatment of Staphylococcus aureus colonization and prophylaxis for infection with topical intranasal mupirocin: An evidence-based review. Clin. Infect. Dis. 2003, 37, 933–938. [Google Scholar] [CrossRef]
- Chang, W.; Ma, X.; Gao, P.; Lv, X.; Lu, H.; Chen, F. Vancomycin MIC creep in methicillin-resistant Staphylococcus aureus (MRSA) isolates from 2006 to 2010 in a hospital in China. Ind. J. Med. Microbiol. 2015, 33, 262. [Google Scholar] [CrossRef] [PubMed]
- Yeh, Y.-C.; Yeh, K.-M.; Lin, T.-Y.; Chiu, S.-K.; Yang, Y.-S.; Wang, Y.-C.; Lin, J.-C. Impact of vancomycin MIC creep on patients with methicillin-resistant Staphylococcus aureus bacteremia. J. Microbiol. Immun. Infect. 2012, 45, 214–220. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Howden, B.P.; Peleg, A.Y.; Stinear, T.P. The evolution of vancomycin intermediate Staphylococcus aureus (VISA) and heterogenous-VISA. Infect. Genet. Evol. 2014, 21, 575–582. [Google Scholar] [CrossRef]
- Wayne, P.; Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. 29th ed. CLSI Supplement M100. 2019. Available online: https://www.techstreet.com/mss/products/preview/2031512 (accessed on 24 October 2020).
- Walters, M.; Lonsway, D.; Rasheed, K.; Albrecht, V.; McAllister, S.; Limbago, B.; Kallen, A. Investigation and Control of Vancomycin-resistant Staphylococcus aureus: A Guide for Health Departments and Infection Control Personnel. Available online: http://www.cdc.gov/hai/pdfs/VRSA-Investigation-Guide-05_12_2015.pdf (accessed on 26 October 2020).
- Enright, M.C.; Day, N.P.; Davies, C.E.; Peacock, S.J.; Spratt, B.G. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones ofStaphylococcus aureus. J. Clin. Microbiol. 2000, 38, 1008–1015. [Google Scholar] [CrossRef]
- Oliveira, D.C.; de Lencastre, H. Multiplex PCR strategy for rapid identification of structural types and variants of the mec element in methicillin-resistant Staphylococcus aureus. Antimicrob. Agent. Chemother. 2002, 46, 2155–2161. [Google Scholar] [CrossRef]
- Harmsen, D.; Claus, H.; Witte, W.; Rothgänger, J.; Claus, H.; Turnwald, D.; Vogel, U. Typing of methicillin-resistant Staphylococcus aureus in a university hospital setting by using novel software for spa repeat determination and database management. J. Clin. Microbiol. 2003, 41, 5442–5448. [Google Scholar] [CrossRef] [PubMed]
- Koreen, L.; Ramaswamy, S.V.; Graviss, E.A.; Naidich, S.; Musser, J.M.; Kreiswirth, B.N. spa typing method for discriminating among Staphylococcus aureus isolates: Implications for use of a single marker to detect genetic micro-and macrovariation. J. Clin. Microbiol. 2004, 42, 792–799. [Google Scholar] [CrossRef] [PubMed]
- WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index 2020. Available online: https://www.whocc.no/atc_ddd_index (accessed on 28 October 2020).
- Horan, T.C.; Andrus, M.; Dudeck, M.A. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am. J. Infect. Contr. 2008, 36, 309–332. [Google Scholar] [CrossRef] [PubMed]
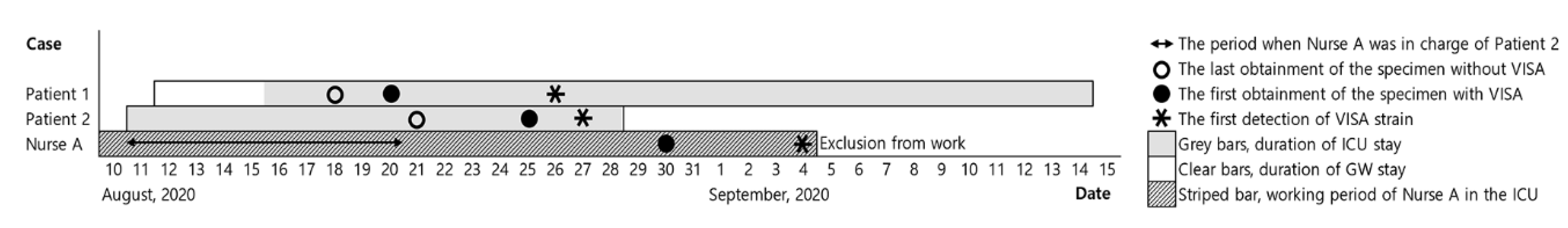


| Variable | Patient 1 | Patient 2 | Nurse A |
|---|---|---|---|
| Clinical characteristics | |||
| Age (years) | 66 | 46 | 34 |
| Sex | Male | Male | Female |
| Specimen | Sputum | Sputum | Nasal cavity |
| Diagnosis on ICU admission | Acute myeloid leukaemia, pneumonia | Intracerebral haemorrhage, hypertension | None |
| Risk factors associated with VISA | Previous vancomycin use, indwelling medical devices | Indwelling medical devices | None |
| Case definition | Presence of infection | Colonisation | Colonisation |
| Outcome | Died | Died | Decolonisation |
| Antimicrobial resistance profiles of VISA | |||
| Ciprofloxacin | ≥8 | ≥8 | ≥8 |
| Clindamycin | ≥8 | ≥8 | ≥8 |
| Erythromycin | ≥8 | ≥8 | ≥8 |
| Telithromycin | ≥4 | ≥4 | ≥4 |
| Gentamicin | ≥16 | ≥16 | ≥16 |
| Mupirocin | 4 | 4 | 4 |
| Oxacillin | ≥4 | ≥4 | ≥4 |
| Penicillin G | ≥0.5 | ≥0.5 | ≥0.5 |
| Quinupristin/dalfopristin | 0.5 | 0.5 | ≤0.25 |
| Rifampicin | ≤0.5 | ≤0.5 | ≤0.5 |
| Trimethoprim/Sulfamethoxazole | ≤10 | ≤10 | ≤10 |
| Tetracycline | ≥16 | ≥16 | ≥16 |
| Tigecycline | 1 | 0.5 | 0.5 |
| Nitrofurantoin | 32 | 32 | ≤16 |
| Teicoplanin | 16 | 8 | 8 |
| Vancomycin | 4 | 4 | 4 |
| Linezolid | 4 | 4 | 2 |
| Molecular features of VISA | |||
| MLST | ST5 | ST5 | ST5 |
| SCCmec type | II | II | II |
| spa type | t2460 | t2460 | t2460 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.H.; Kim, Y.C.; Kim, H.; Lee, H.M.; Lee, J.H.; Kim, D.A.; Kim, C.; Park, J.Y.; Park, Y.S. Lessons Learned from an Experience with Vancomycin-Intermediate Staphylococcus aureus Outbreak in a Newly Built Secondary Hospital in Korea. Pathogens 2021, 10, 564. https://doi.org/10.3390/pathogens10050564
Kim MH, Kim YC, Kim H, Lee HM, Lee JH, Kim DA, Kim C, Park JY, Park YS. Lessons Learned from an Experience with Vancomycin-Intermediate Staphylococcus aureus Outbreak in a Newly Built Secondary Hospital in Korea. Pathogens. 2021; 10(5):564. https://doi.org/10.3390/pathogens10050564
Chicago/Turabian StyleKim, Min Hyung, Yong Chan Kim, Heejung Kim, Hyuk Min Lee, Ju Hyun Lee, Da Ae Kim, Chanhee Kim, Jin Young Park, and Yoon Soo Park. 2021. "Lessons Learned from an Experience with Vancomycin-Intermediate Staphylococcus aureus Outbreak in a Newly Built Secondary Hospital in Korea" Pathogens 10, no. 5: 564. https://doi.org/10.3390/pathogens10050564
APA StyleKim, M. H., Kim, Y. C., Kim, H., Lee, H. M., Lee, J. H., Kim, D. A., Kim, C., Park, J. Y., & Park, Y. S. (2021). Lessons Learned from an Experience with Vancomycin-Intermediate Staphylococcus aureus Outbreak in a Newly Built Secondary Hospital in Korea. Pathogens, 10(5), 564. https://doi.org/10.3390/pathogens10050564






