HIV Pretreatment Drug Resistance Trends in Mexico City, 2017–2020
Abstract
:1. Introduction
2. Results
2.1. Characteristics of the Study Participants
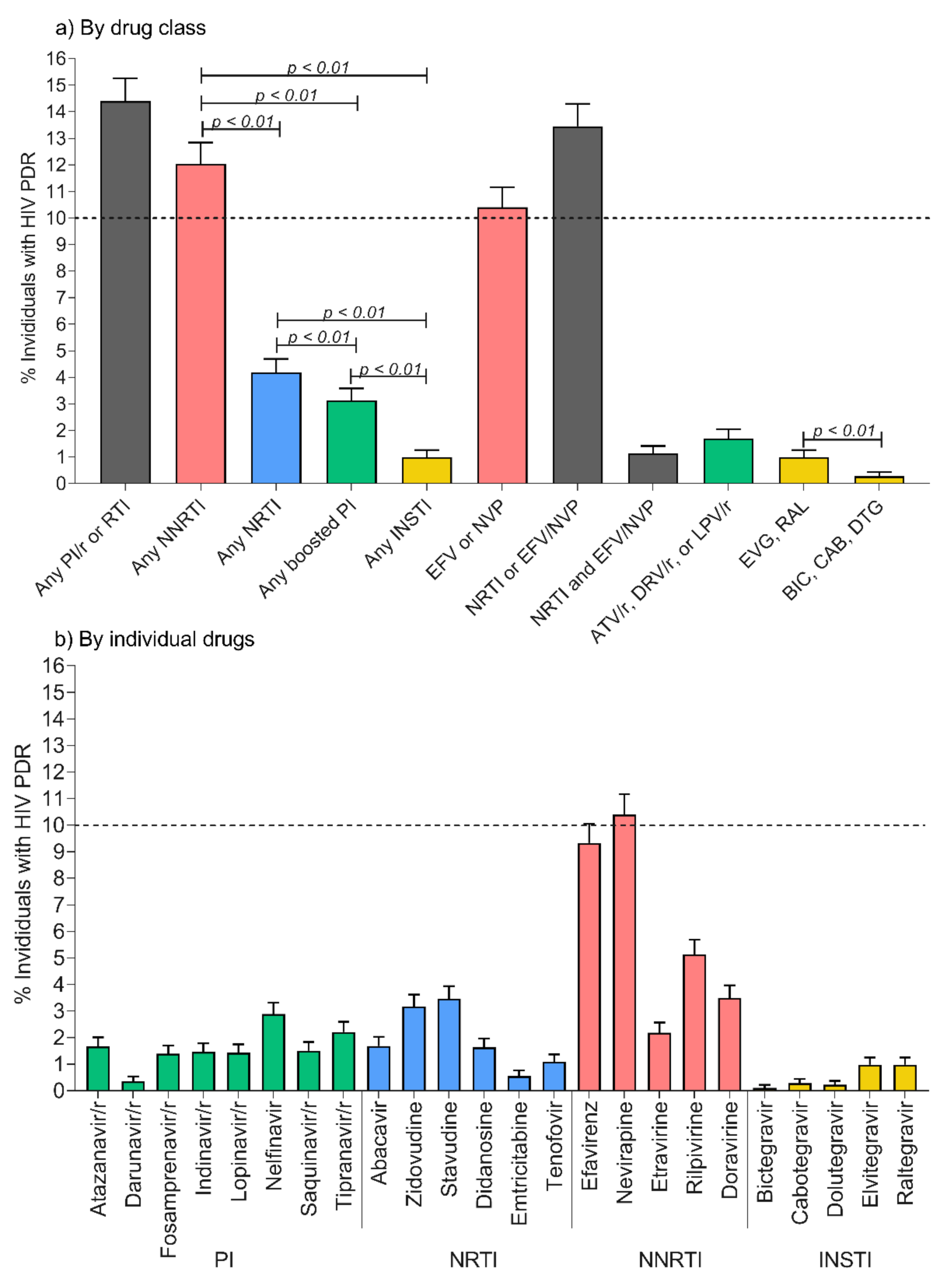
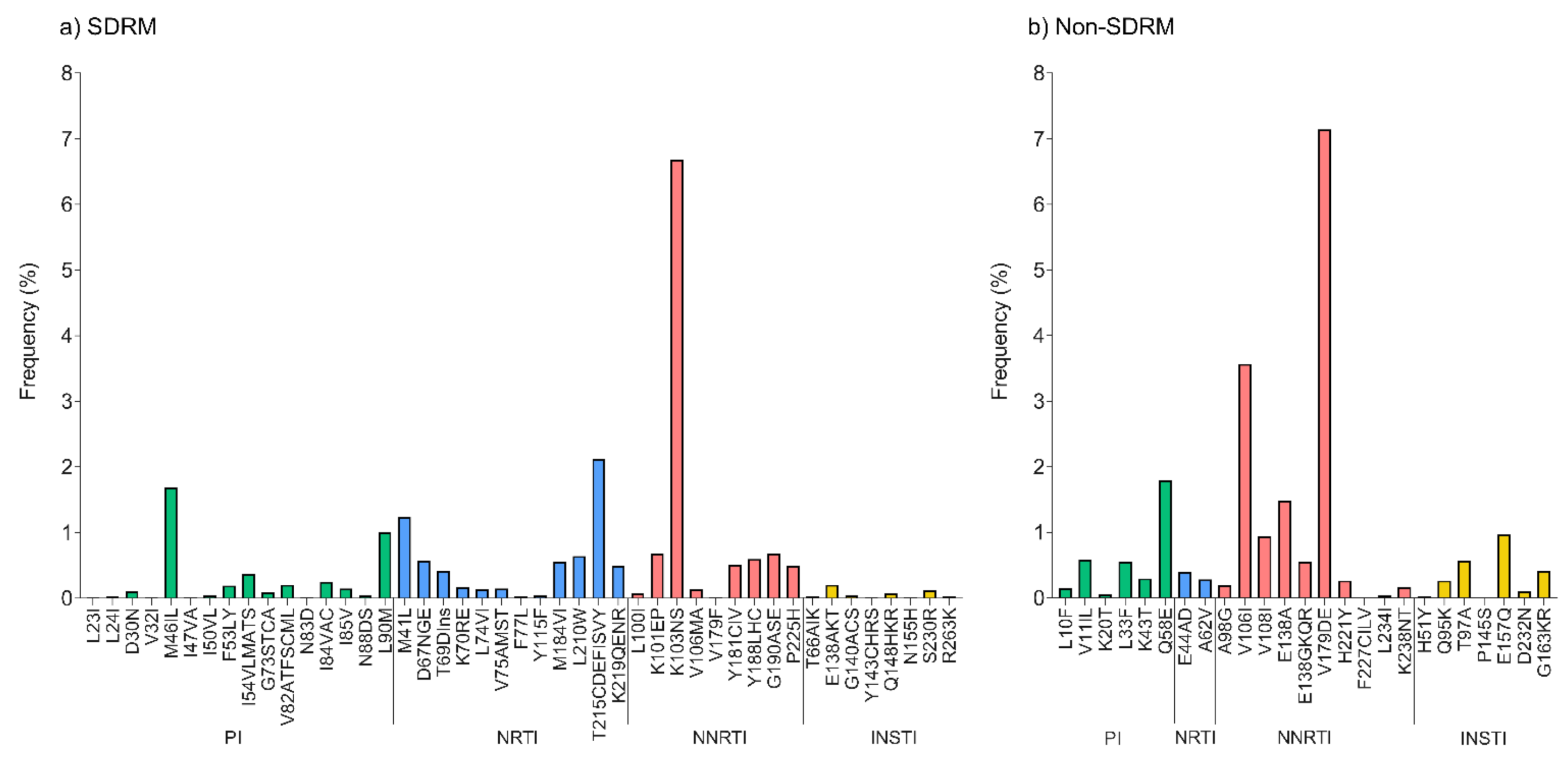
2.2. Overall Estimations of Pretreatment Drug Resistance
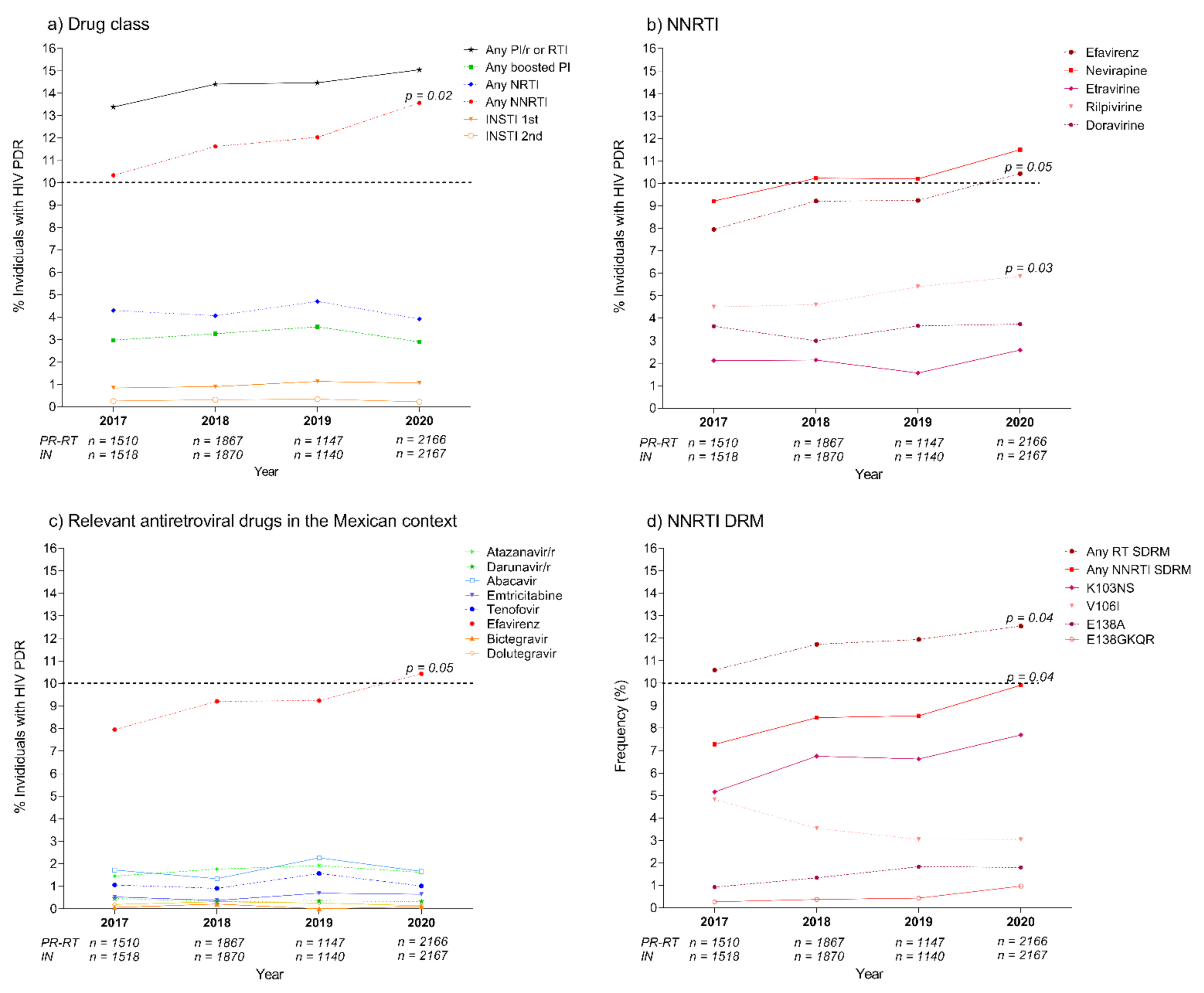
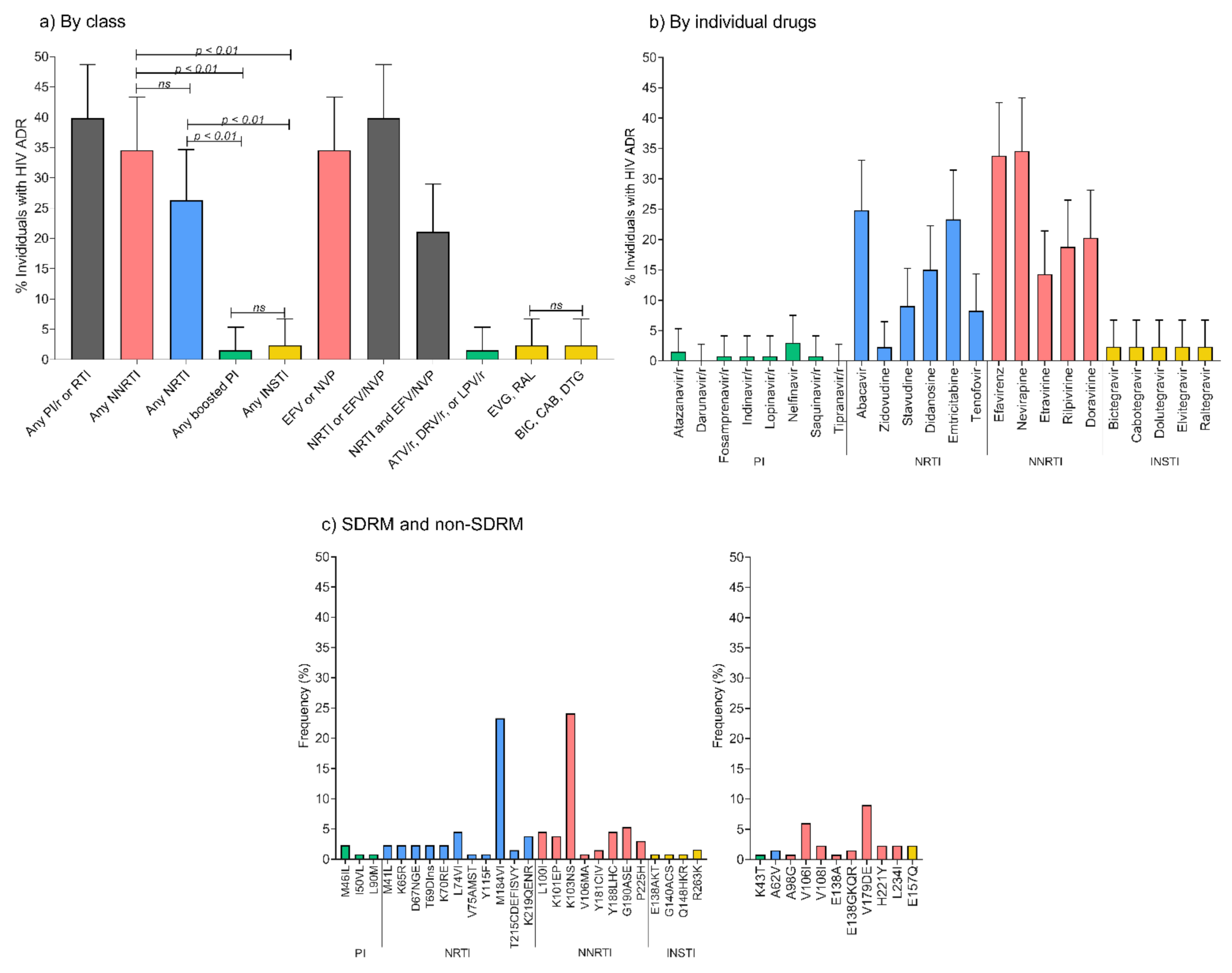
2.3. Pretreatment Drug Resistance Trends across the Study Period
2.4. Associations of Pretreatment Drug Resistance with Epidemiological Variables
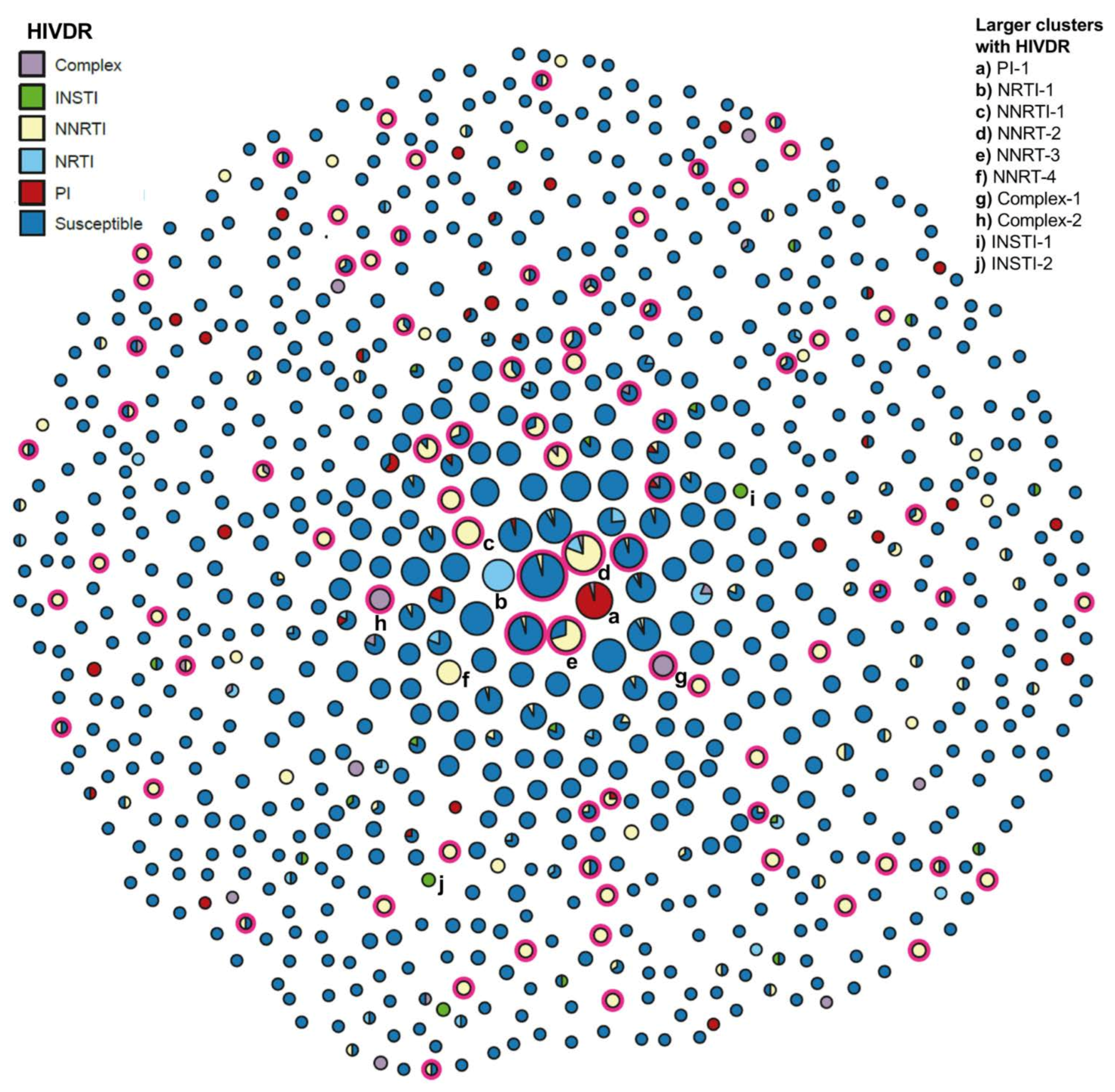
2.5. Analysis of HIV PDR Transmission within Mexico City’s HIV Genetic Network
2.6. Characteristics and Prevalence of Acquired Drug Resistance in Mexico City, 2020
3. Discussion
4. Materials and Methods
4.1. Study Population
4.2. HIV Amplification and Sequencing
4.3. HIV Drug Resistance Assessment
4.4. Associations between Pretreatment Drug Resistance and Epidemiological Variables
4.5. HIV Transmission Network Inference
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Palella, F.J.; Loveless, M.O.; Holmberg, S.D. Declining Morbidity and Mortality among Patients with Advanced Human Immunodeficiency Virus Infection. N. Engl. J. Med. 1998, 338, 853–860. [Google Scholar] [CrossRef]
- Eaton, J.W.; Johnson, L.F.; Salomon, J.A.; Bärnighausen, T.; Bendavid, E.; Bershteyn, A.; Bloom, D.E.; Cambiano, V.; Fraser, C.; Hontelez, J.A.C.; et al. HIV Treatment as Prevention: Systematic Comparison of Mathematical Models of the Potential Impact of Antiretroviral Therapy on HIV Incidence in South Africa. PLoS Med. 2012, 9, e1001245. [Google Scholar] [CrossRef]
- WHO. HIV Data and Statistics. Available online: https://www.who.int/teams/control-of-neglected-tropical-diseases/yaws/diagnosis-and-treatment/hiv (accessed on 28 October 2021).
- WHO. HIV Drug Resistance Report. 2019. Available online: https://www.who.int/publications/i/item/WHO-CDS-HIV-19.21 (accessed on 28 October 2021).
- WHO. Surveillance of HIV Drug Resistance in Adults Initiating Antiretroviral Therapy Pretreatment HIV Drug Resistance. Concept Note. 2014. Available online: https://www.who.int/publications/i/item/9789241507196 (accessed on 18 November 2021).
- Gupta, R.K.; Gregson, J.; Parkin, N.; Haile-Selassie, H.; Tanuri, A.; Andrade Forero, L.; Kaleebu, P.; Watera, C.; Aghokeng, A.; Mutenda, N.; et al. HIV-1 Drug Resistance before Initiation or Re-Initiation of First-Line Antiretroviral Therapy in Low-Income and Middle-Income Countries: A Systematic Review and Meta-Regression Analysis. Lancet Infect. Dis. 2018, 18, 346–355. [Google Scholar] [CrossRef] [Green Version]
- WHO. Consolidated Guidelines on HIV Prevention, Testing, Treatment, Service Delivery and Monitoring: Recommendations for a Public Health Approach. Available online: https://www.who.int/publications-detail-redirect/9789240031593 (accessed on 28 October 2021).
- Ávila-Ríos, S.; García-Morales, C.; Matías-Florentino, M.; Romero-Mora, K.A.; Tapia-Trejo, D.; Quiroz-Morales, V.S.; Reyes-Gopar, H.; Ji, H.; Sandstrom, P.; Casillas-Rodríguez, J.; et al. Pretreatment HIV-Drug Resistance in Mexico and Its Impact on the Effectiveness of First-Line Antiretroviral Therapy: A Nationally Representative 2015 WHO Survey. Lancet HIV 2016, 3, e579–e591. [Google Scholar] [CrossRef]
- Ávila-Ríos, S.; García-Morales, C.; Valenzuela-Lara, M.; Chaillon, A.; Tapia-Trejo, D.; Pérez-García, M.; López-Sánchez, D.M.; Maza-Sánchez, L.; del Arenal-Sánchez, S.J.; Paz-Juárez, H.E.; et al. HIV-1 Drug Resistance before Initiation or Re-Initiation of First-Line ART in Eight Regions of Mexico: A Sub-Nationally Representative Survey. J. Antimicrob. Chemother. 2019, 74, 1044–1055. [Google Scholar] [CrossRef]
- García-Morales, C.; Tapia-Trejo, D.; Quiroz-Morales, V.S.; Navarro-Álvarez, S.; Barrera-Arellano, C.A.; Casillas-Rodríguez, J.; Romero-Mora, K.A.; Gómez-Palacio-Schjetnan, M.; Murakami-Ogasawara, A.; Ávila-Ríos, S.; et al. HIV Pretreatment Drug Resistance Trends in Three Geographic Areas of Mexico. J. Antimicrob. Chemother. 2017, 72, 3149–3158. [Google Scholar] [CrossRef]
- Secretaría de Salud, Centro Nacional para la Prevencion y el Control del VIH y el SIDA. Guia de Manejo Antirretroviral de las Personas que Viven con el VIH/SIDA. CENSIDA: Mexico City, Mexico, 2021; ISBN 9789707210127. [Google Scholar]
- Secretaría de Salud, Centro Nacional para la Prevención y el Control del VIH y el SIDA. Boletín de Atención Integral de Personas que Viven con VIH; CENSIDA: Mexico City, Mexico, 2021. Available online: https://www.gob.mx/censida/articulos/boletin-de-diagnostico-y-tratamiento-antirretroviral-censida?idiom=es (accessed on 28 October 2021).
- Anstett, K.; Brenner, B.; Mesplede, T.; Wainberg, M.A. HIV Drug Resistance against Strand Transfer Integrase Inhibitors. Retrovirology 2017, 14, 36. [Google Scholar] [CrossRef] [PubMed]
- Paton, N.I.; Musaazi, J.; Kityo, C.; Walimbwa, S.; Hoppe, A.; Balyegisawa, A.; Kaimal, A.; Mirembe, G.; Tukamushabe, P.; Ategeka, G.; et al. Dolutegravir or Darunavir in Combination with Zidovudine or Tenofovir to Treat HIV. N. Engl. J. Med. 2021, 385, 330–341. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Rodríguez, A. Clínicas Especializadas Condesa. Epidemiologic Response to HIV/AIDS and HCV in Mexico City, 2020. 2021. Available online: http://condesadf.mx/pdf/Respuesta2020_cdmx17feb21OK.pdf (accessed on 28 October 2021).
- Dávila-Conn, V.; García-Morales, C.; Matías-Florentino, M.; López-Ortiz, E.; Paz-Juárez, H.E.; Beristain-Barreda, Á.; Cárdenas-Sandoval, M.; Tapia-Trejo, D.; López-Sánchez, D.; Becerril-Rodríguez, M.; et al. Characteristics and Growth of the Genetic HIV Transmission Network of Mexico City during 2020. JIAS 2021, 24, e25836. [Google Scholar] [CrossRef] [PubMed]
- Matías-Florentino, M.; Chaillon, A.; Ávila-Ríos, S.; Mehta, S.R.; Paz-Juárez, H.E.; Becerril-Rodríguez, M.A.; del Arenal-Sánchez, S.J.; Piñeirúa-Menéndez, A.; Ruiz, V.; Iracheta-Hernández, P.; et al. Pretreatment HIV Drug Resistance Spread within Transmission Clusters in Mexico City. J. Antimicrob. Chemother. 2020, 75, 656–667. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Wagar, N.; DeVos, J.R.; Rottinghaus, E.; Diallo, K.; Nguyen, D.B.; Bassey, O.; Ugbena, R.; Wadonda-Kabondo, N.; McConnell, M.S.; et al. Optimization of a Low Cost and Broadly Sensitive Genotyping Assay for HIV-1 Drug Resistance Surveillance and Monitoring in Resource-Limited Settings. PLoS ONE 2011, 6, e28184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Laethem, K.; Schrooten, Y.; Covens, K.; Dekeersmaeker, N.; De Munter, P.; Van Wijngaerden, E.; Van Ranst, M.; Vandamme, A.-M. A Genotypic Assay for the Amplification and Sequencing of Integrase from Diverse HIV-1 Group M Subtypes. J. Virol. Methods 2008, 153, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Public Health Agency of Canada. HyDRA Web. Available online: https://hydra.canada.ca/ (accessed on 1 July 2021).
- Parkin, N.T.; Avila-Rios, S.; Bibby, D.F.; Brumme, C.J.; Eshleman, S.H.; Harrigan, P.R.; Howison, M.; Hunt, G.; Ji, H.; Kantor, R.; et al. Multi-Laboratory Comparison of Next-Generation to Sanger-Based Sequencing for HIV-1 Drug Resistance Genotyping. Viruses 2020, 12, 694. [Google Scholar] [CrossRef] [PubMed]
- BC Centre for Excellence in HIV/AIDS. Recall. Available online: https://recall.bccfe.ca/ (accessed on 28 October 2021).
- WHO. WHO/HIV ResNet HIV Drug Resistance Quality Control Tool. Available online: https://sequenceqc-dev.bccfe.ca/who_qc (accessed on 28 October 2021).
- Stanford University. HIV Drug Resistance Database. Available online: https://hivdb.stanford.edu/ (accessed on 28 October 2021).
- WHO. WHO/HIV ResNet HIV Drug Resistance Laboratory Operational Framework. 2017. Available online: https://www.who.int/publications-detail-redirect/978-92-4-000987-5 (accessed on 28 October 2021).
- WHO HIV ResNet. Available online: https://www.who.int/groups/who-hivresnet (accessed on 28 October 2021).
- REGA HIV-1 Subtyping Tool. Available online: http://dbpartners.stanford.edu:8080/RegaSubtyping/stanford-hiv/typingtool/ (accessed on 19 November 2021).
- Kosakovsky Pond, S.L.; Weaver, S.; Leigh Brown, A.J.; Wertheim, J.O. HIV-TRACE (TRAnsmission Cluster Engine): A Tool for Large Scale Molecular Epidemiology of HIV-1 and Other Rapidly Evolving Pathogens. Mol. Biol. Evol. 2018, 35, 1812–1819. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Total Number of Observations b n = 6661 | With PDR to Any Drug c,d n = 957 | p Value | With PDR to EFV/NVP d n = 690 | p Value | |
|---|---|---|---|---|---|
| Gender, n (%) Cisgender Women Cisgender Men Transgender Women Transgender Men Missing | 267 (4.0) 6234 (93.6) 51 (0.8) 3 (0.0) 106 (1.6) | 32 (12.0) 907 (14.5) 6 (11.8) 0 (0.0) 12 (11.3) | 0.14 0.06 0.39 0.62 0.23 | 24 (9.0) 653 (10.5) 4 (7.8) 0 (0.0) 9 (8.5) | 0.26 0.13 0.38 0.72 0.33 |
| Age (years) e Median (IQR) | 28 (24–35) | 28 (24–34) | 0.09 | 28 (24–34) | 0.30 |
| State of residence, n (%) Mexico City Mexico State Other Missing | 4223 (63.4) 967 (14.5) 90 (1.4) 1381 (20.7) | 621 (14.7) 142 (14.7) 9 (10.0) 185 (13.4) | 0.16 0.40 0.15 0.13 | 448 (10.6) 107 (11.1) 5 (5.6) 130 (9.4) | 0.20 0.23 0.08 0.10 |
| HIV subtype, n (%) B Non-B | 6577 (98.7) 84 (1.3) | 946 (14.4) 11 (13.1) | 0.44 | 680 (11.6) 10 (11.9) | 0.37 |
| Viral load (log RNA copies/mL) f Median (range) | 4.8 (4.25–5–31) | 4.7 (4.2–5.3) | 0.02 * | 4.7 (4.2–5.3) | 0.03 * |
| CD4+ T cell count (cells/mm3), n g Median (IQR) | 249 (120–395) | 250 (123–407) | 0.22 | 254 (129–405) | 0.16 |
| CD4+ T cell count category, n (%) <200 cells/mm3 200–500 cells/mm3 >500 cells/mm3 Missing | 2323 (34.87) 2721 (40.8) 809 (12.2) 808 (12.1) | 334 (14.4) 389 (14.3) 129 (15.9) 105 (13.0) | 0.51 0.46 0.10 0.13 | 240 (10.3) 285 (10.5) 94 (11.6) 71 (8.8) | 0.50 0.41 0.12 0.06 |
| CD4+ T cell %, n h Median (IQR) | 15 (9–21) | 15 (9–22) | 0.27 | 15 (10–22) | 0.14 |
| Total Number of Observations b n = 1348 | With PDR to Any Drug c,d n = 215 (15.9%) | p Value | With PDR to EFV/NVP d n = 158 (11.7%) | p Value | |
|---|---|---|---|---|---|
| Gender, n (%) Cisgender Women Cisgender Men Transgender Women Transgender Men | 85 (6.3) 1234 (91.5) 28 (2.1) 1 (0.1) | 13 (15.3) 196 (15.9) 6 (21.4) 0 (0.0) | 0.50 0.46 0.28 0.84 | 9 (10.6) 145 (11.8) 4 (14.3) 0 (0.0) | 0.45 0.53 0.42 0.88 |
| Age (years) Median (IQR) | 29 (25–36) | 29 (25–35) | 0.54 | 30 (25–35) | 0.81 |
| Prior ARV exposure, n (%) No Yes Missing | 1145 (84.9) 141 (10.5) 62 (4.6) | 164 (14.3) 41 (29.1) 10 (16.4) | <0.01 * <0.01 * 0.88 | 115 (10.0) 35 (24.8) 8 (13.1) | <0.01 * <0.01 * 0.72 |
| State of residence, n (%) Mexico City Mexico State Other | 1035 (76.8) 279 (20.7) 33 (2.5) | 180 (17.4) 32 (11.5) 3 (9.1) | <0.01 * 0.01 * 0.20 | 134 (13.0) 23 (8.2) 1 (3.0) | <0.01 * 0.02 * 0.08 |
| HIV subtype, n (%) B Non-B | 1330 (98.7) 18 (1.3) | 211 (15.8) 4 (22.1) | 0.51 | 155 (11.6) 3 (16.8) | 0.35 |
| Viral load (log RNA copies/mL) Median (range) | 4.6 (4.1–5.2) | 4.6 (4.0–5.1) | 0.22 | 4.6 (3.9–5.1) | 0.20 |
| CD4+ T cell count (cells/mm3) Median (IQR) | 173 (78–291) | 154 (71–281) | 0.15 | 152 (84–284) | 0.38 |
| CD4+ T cell count category, n (%) <200 cells/mm3 200–500 cells/mm3 >500 cells/mm3 Missing | 757 (56.2) 529 (39.2) 60 (4.4) 2 (0.2) | 137 (18.1) 70 (13.2) 8 (13.3) 0 (0.0) | <0.01 * 0.02 * 0.36 0.70 | 102 (13.5) 51 (9.6) 5 (8.3) 0 (0.0) | 0.01 0.03 * 0.28 0.78 |
| CD4+ T cell % Median (IQR) | 13 (7–19) | 12 (7–18) | 041 | 14 (8–19) | 0.48 |
| Sexual risk category, n (%) Heterosexual cis women Heterosexual cis men Cisgender MSM Transgender women Missing | 78 (5.8) 172 (12.8) 888 (65.9) 31 (2.3) 179 (13.3) | 11 (14.1) 20 (11.6) 139 (15.6) 6 (19.3) 39 (21.8) | 0.39 0.06 0.36 0.37 0.02 * | 8 (10.3) 12 (7.0) 105 (11.8) 3 (9.7) 30 (16.8) | 0.42 0.02 * 0.47 0.50 0.02 * |
| Marital status, n (%) Single Married Domestic partnership Other Missing | 958 (71.1) 46 (3.4) 173 (12.8) 29 (2.2) 142 (10.5) | 153 (16.0) 7 (15.2) 20 (11.6) 3 (10.3) 32 (22.5) | 0.53 0.54 0.05 0.29 0.02 * | 115 (12.0) 3 (6.5) 13 (7.5) 2 (6.9.6) 25 (17.6) | 0.34 0.19 0.04 * 0.32 0.02 * |
| Education, n (%) Illiterate Elementary High School Technician Degree Postgraduate Missing | 7 (0.5) 59 (4.4) 587 (43.5) 64 (4.7) 440 (32.6) 44 (3.26) 147 (10.91) | 1 (14.3) 11 (18.6) 86 (14.6) 10 (15.6) 69 (15.7) 5 (11.4) 33 (22.4) | 0.69 0.33 0.14 0.55 0.46 0.27 0.02 * | 1 (14.3) 8 (13.6) 56 (9.5) 9 (14.1) 54 (12.3) 4 (9.1) 26 (17.7) | 0.58 0.38 0.02 * 0.33 0.36 0.40 0.02 * |
| Self-identified social class, n (%) Low Middle High Missing | 477 (35.4) 717 (53.2) 2 (0.2) 152 (11.3) | 74 (15.5) 108 (15.1) 1 (50.0) 32 (21.0) | 0.40 0.19 0.29 0.05 | 50 (10.5) 83 (11.6) 0 (0.0) 25 (16.4) | 0.17 0.46 0.77 0.04 * |
| Indigenous languages spoken, n (%) No Yes Missing | 1156 (85.7) 40 (3.0) 152 (11.3) | 177 (15.3) 6 (15.0) 32 (21.0) | 0.07 0.54 0.05 | 130 (11.2) 3 (7.5) 25 (16.4) | 0.11 0.29 0.04 * |
| Other sexually transmitted infections, n (%) No Yes Preferred not to answer Missing | 633 (47.0) 426 (31.6) 58 (4.3) 231 (17.1) | 91 (14.4) 72 (16.9) 10 (17.2) 42 (18.2) | 0.08 0.28 0.45 0.17 | 72 (11.4) 48 (11.3) 5 (8.6) 33 (14.3) | 0.38 0.40 0.31 0.11 |
| Role in anal sex, n (%) Receptive Insertive/Receptive Insertive Missing | 319 (23.6) 474 (35.3) 223 (16.5) 332 (24.6) | 49 (15.4) 76 (16.0) 32 (14.4) 58 (17.5) | 0.41 0.50 0.27 0.22 | 35 (11.0) 64 (13.5) 17 (7.7) 42 (12.6) | 0.36 0.08 0.02 * 0.30 |
| Circumcision, n (%) No Yes Missing | 807 (59.9) 240 (17.8) 301 (22.3) | 131 (16.2) 28 (11.7) 56 (18.6) | 0.39 0.03 * 0.09 | 97 (12.0) 20 (8.3) 41 (13.6) | 0.37 0.04 * 0.14 |
| Injectable drug use, n (%) No Yes Missing | 1143 (84.8) 49 (3.6) 156 (11.6) | 170 (14.9) 13 (26.5) 32 (20.5) | <0.01 * 0.04 * 0.06 | 123 (10.8) 10 (20.4) 25 (16.0) | <0.01 * 0.05 0.05 |
| Venues for sex, n (%) At home At partner’s home Venues for sex Multiple Missing | 519 (38.5) 290 (21.5) 93 (6.9) 111 (8.2) 335 (24.8) | 82 (15.8) 48 (16.5) 14 (15.0) 12 (10.8) 59 (17.6) | 0.48 0.40 0.47 0.07 0.19 | 62 (11.9) 36 (12.4) 8 (8.6) 8 (7.2) 44 (13.1) | 0.45 0.37 0.22 0.07 0.20 |
| Resistance to Any ARV a | Resistance to NNRTI a | |||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | p Value | aOR | 95% CI | p Value | |
| Age (years) b | 1.0 | 1.0–1.0 | 0.07 | 1.0 | 1.0–1.0 | 0.1 |
| Sexual risk category c Heterosexual cis men Heterosexual cis women Cisgender MSM Transgender women Missing | Ref. 1.1 1.5 1.9 2.8 | 0.5–2.5 0.9–2.4 0.7–5.4 1.1–7.0 | 0.8 0.2 0.2 0.03 * | Ref. 1.3 1.9 1.5 3.2 | 0.5–3.5 1.0–3.5 0.4–5.7 1.1–9.3 | 0.6 0.1 0.6 0.03 * |
| Injectable drug use No Yes Missing | Ref. 1.7 0.9 | 0.9–3.7 0.4–2.0 | 0.07 0.7 | Ref. 1.8 1.0 | 0.8–3.8 0.4–2.6 | 0.1 1.0 |
| CD4+ T cell count category 200–499 cells/mm3 <200 cells/mm3 ≥500 cells/mm3 | Ref. 1.6 1.0 | 1.2–2.2 0.4–2.1 | 0.005 * 0.9 | Ref. 1.6 0.8 | 1.1–2.4 0.3–2.1 | 0.01 * 0.6 |
| Viral load (log copies/mL) b | 0.9 | 0.7–1.1 | 0.2 | 0.9 | 0.7–1.1 | 0.2 |
| Prior ARV exposure No Yes Missing | Ref. 2.7 0.9 | 1.7–4.1 0.4–1.8 | 0.001 * 0.7 | Ref. 3.4 1.0 | 2.1–5.3 0.4–2.2 | 0.001 * 0.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Morales, C.; Tapia-Trejo, D.; Matías-Florentino, M.; Quiroz-Morales, V.S.; Dávila-Conn, V.; Beristain-Barreda, Á.; Cárdenas-Sandoval, M.; Becerril-Rodríguez, M.; Iracheta-Hernández, P.; Macías-González, I.; et al. HIV Pretreatment Drug Resistance Trends in Mexico City, 2017–2020. Pathogens 2021, 10, 1587. https://doi.org/10.3390/pathogens10121587
García-Morales C, Tapia-Trejo D, Matías-Florentino M, Quiroz-Morales VS, Dávila-Conn V, Beristain-Barreda Á, Cárdenas-Sandoval M, Becerril-Rodríguez M, Iracheta-Hernández P, Macías-González I, et al. HIV Pretreatment Drug Resistance Trends in Mexico City, 2017–2020. Pathogens. 2021; 10(12):1587. https://doi.org/10.3390/pathogens10121587
Chicago/Turabian StyleGarcía-Morales, Claudia, Daniela Tapia-Trejo, Margarita Matías-Florentino, Verónica Sonia Quiroz-Morales, Vanessa Dávila-Conn, Ángeles Beristain-Barreda, Miroslava Cárdenas-Sandoval, Manuel Becerril-Rodríguez, Patricia Iracheta-Hernández, Israel Macías-González, and et al. 2021. "HIV Pretreatment Drug Resistance Trends in Mexico City, 2017–2020" Pathogens 10, no. 12: 1587. https://doi.org/10.3390/pathogens10121587
APA StyleGarcía-Morales, C., Tapia-Trejo, D., Matías-Florentino, M., Quiroz-Morales, V. S., Dávila-Conn, V., Beristain-Barreda, Á., Cárdenas-Sandoval, M., Becerril-Rodríguez, M., Iracheta-Hernández, P., Macías-González, I., García-Mendiola, R., Guzmán-Carmona, A., Zarza-Sánchez, E., Cruz, R. A., González-Rodríguez, A., Reyes-Terán, G., & Ávila-Ríos, S. (2021). HIV Pretreatment Drug Resistance Trends in Mexico City, 2017–2020. Pathogens, 10(12), 1587. https://doi.org/10.3390/pathogens10121587






