Cautious Optimism Building: What HIE Managers Think About Adding Artificial Intelligence to Improve Patient Matching
Abstract
1. Introduction
Could you imagine the horror, you are going under anesthesia for a surgery 5, 4, 3, 2 and as you are going under you hear them say the wrong patient’s name. Thankfully they caught it, but could you imagine waking up in that panic!
HIE Patient Matching—The Challenges
By not having a universal patient identifier, we are all building our own proprietary matching programs. When you think of it that’s not efficient, when you think about interoperability, we’re all starting from a different point based on maturity levels.
2. Literature Review
2.1. The History of HIEs
2.2. Patient Matching—Sources of Value
We are finally getting those benefits of early investment, our grants, it is paying off with what we are now doing, able to do, and deliver to our stakeholders. We are seeing, they are seeing it.
2.3. Patient Matching—The Challenges
It’s a Sisyphean effort. You know, once you open that queue you’ve got 92,000 matches to review. It just feels like all of this effort. It’s difficult to see in any sort of tangible way how it is positively, you know, affecting you or positively influencing the data. The data, it never stops.
2.4. Patient Matching Techniques—The Current State
3. This Study
3.1. Interview Protocol
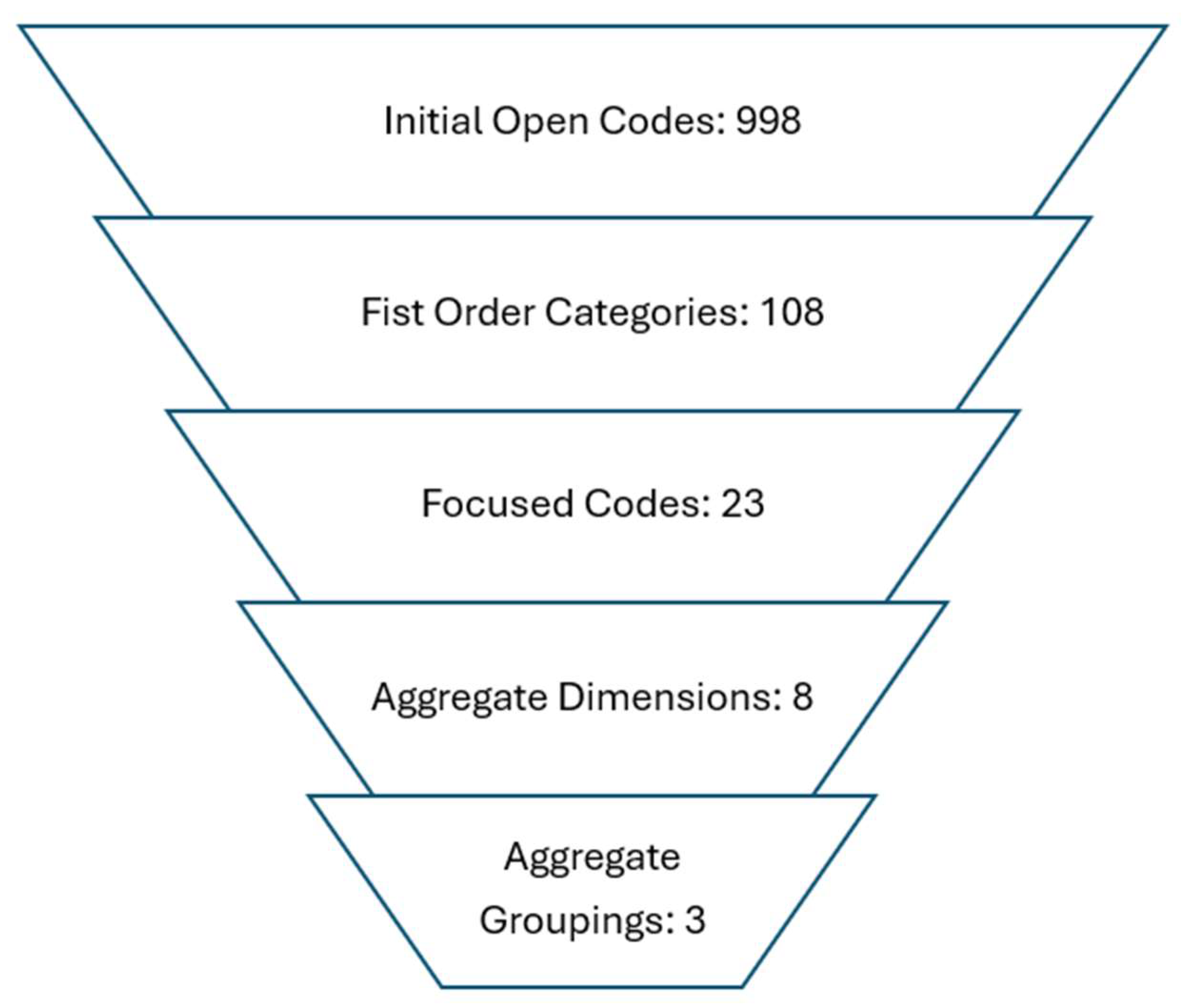
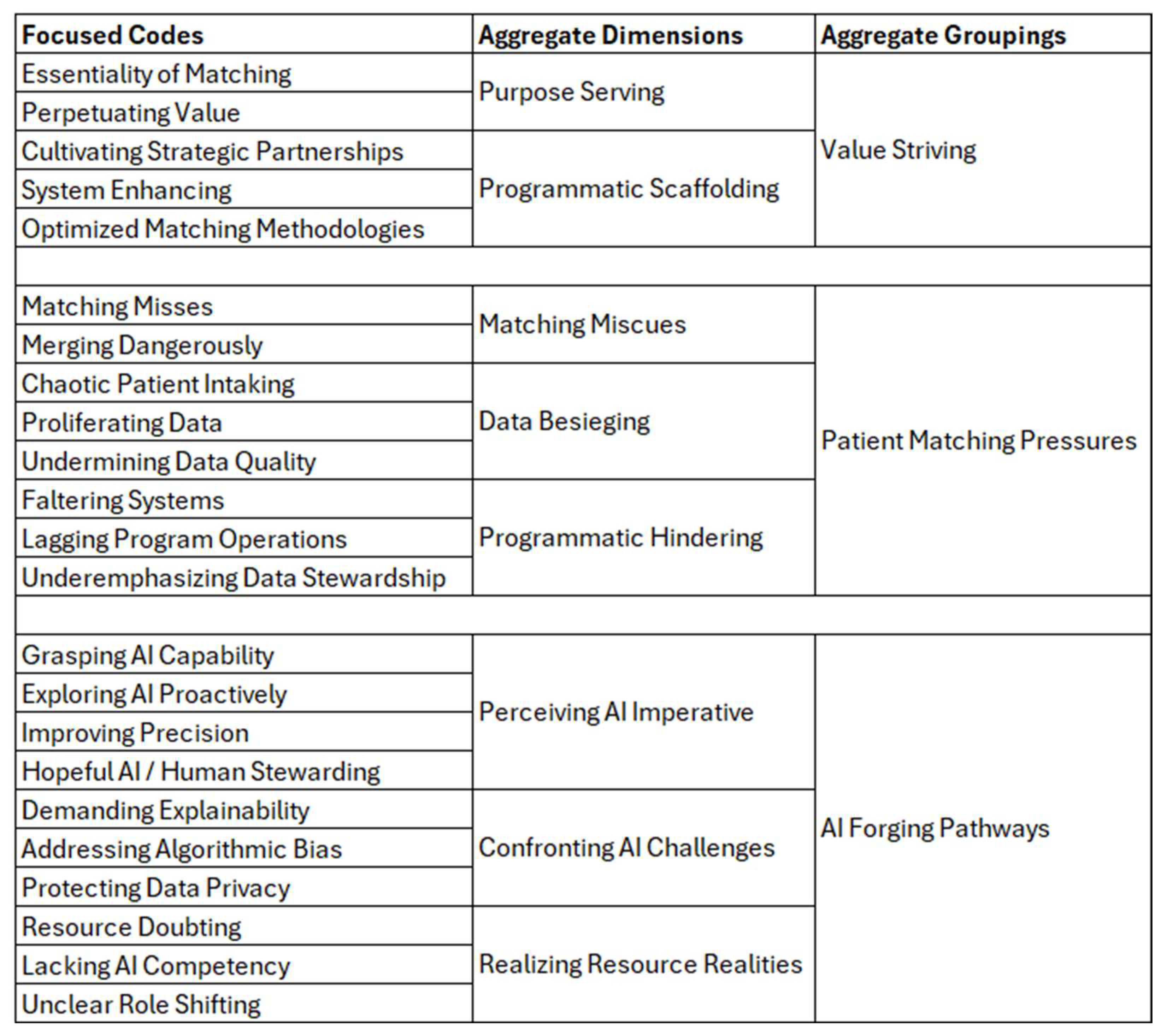
3.2. Data Analysis
4. Findings
4.1. Grounded Theory Overview
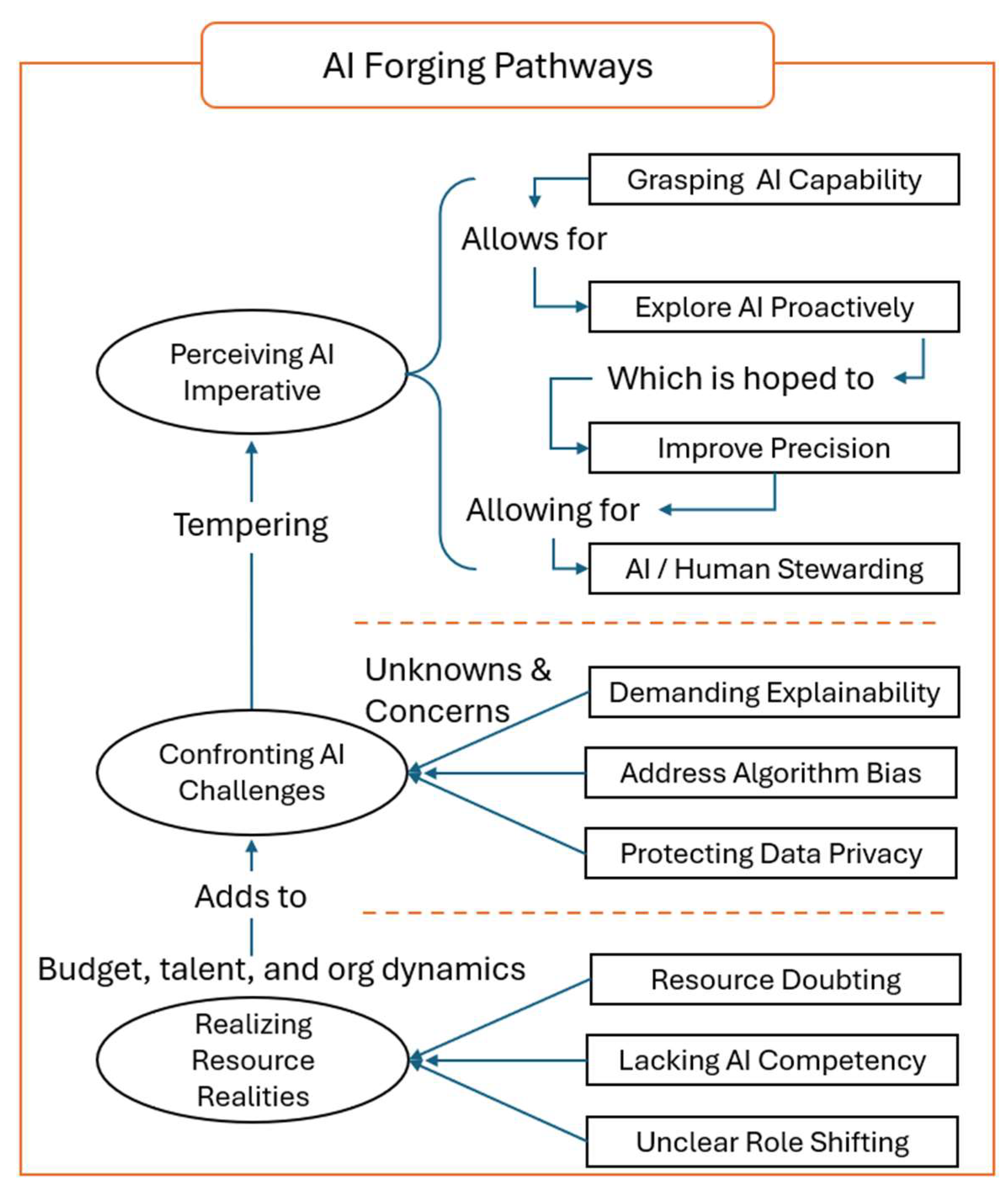
4.2. AI Forging Pathways—A Preview
4.2.1. Perceiving AI Imperative
We can’t deny AI has really a kind of bright future I can see in the HIEs and healthcare sector for sure. It’s coming and we have to prepare, there is a buzz, and conversations are happening more and more.
Perceiving AI Imperative
Not every customer understands what AI can produce for them right now, its early, training, talent, they are not really set up. So, it will require some time for the customers to understand what they require certain prototypes and AI use cases they even have, what AI to use.
Exploring AI Proactively
I think there’s tremendous opportunity in that field of AI. We haven’t defined a specific application that we’re pursuing, but we do think about using it for natural language processing and code normalization. It would make sense to utilize some machine learning in the algorithmic matching process. Especially where we have humans looking at records and making decisions. Conversations are started and we are testing.
Improving Precision
We have been dealing with the last mile problem in patient matching for years, it’s that final percentage of records that just won’t resolve. Our hope with AI is that its predictive power, its ability to learn from millions of data points and spot patterns, will finally help in this regard, more testing to do and trust is a big part of it, but this is how we are thinking to utilize AI.
Hopeful AI/Human Stewarding
We need a collaborative effort of AI and human. The idea of getting all this technology is to increase efficiency and reduce the cost, and have the human do more strategy, enable more cognition as a tool. Let the computers handle the mundane and volume-based tasks, this is evident for manual review, humans cannot keep up, let AI handle the bulk load.
4.2.2. Confronting AI Challenges
Demanding Explainability
When an AI system makes a decision about patient matching, we need to know why, it boils down to a few things, it’s about patient safety and data integrity. If we cannot understand why the AI made a specific match we compromise our ability to build trust with clinicians using the system.
Addressing Algorithmic Bias
Algorithmic bias is a critical ethical challenge that AI introduces into an HIE network, you learn from your data, and data from one part of the HIE might be demographically different from another part of the state, or better yet nationally. AI is a huge help to the industry, but we need guardrails and trust, we don’t want to inadvertently create a different set of divides within our communities.
Protecting Data Privacy
AI does introduce a whole new layer of privacy concerns for us in the HIE space to worry about. We are taking precautions, but how do we know others are, it is a scary time, we need regulation around this, we need business agreements to have AI protections.
4.2.3. Realizing Resource Realities
Resource Doubting
So, I think there’s a place for AI, absolutely. But it’s not something that we’ve embraced yet, and I think ultimately our implementation of AI is probably going to depend a lot on budget. There’re limited resources in my HIE. AI would be great, but I have to balance operations, there’s tech costs, talent costs, training to think about.
Lacking AI Competency
The reality is our HIE runs pretty lean and exploring and/or introducing AI into our environment adds an entirely new dimension of talent needs. This is a significant challenge when your operational model is built around constraints or talent deficiencies in the industry, most of us are non-profits. We simply cannot effectively integrate AI or truly leverage its potential within our HIE at this time.
Unclear Role Shifting
What I think if AI comes to fruition isn’t just the AI itself, it’s the change management. How it will change what our people actually do, and will staff be ready for that, it’s a new paradigm for all levels, boards, leaders, staff. What do we let AI handle, what do our people handle, tasks aren’t going to be the same. We’ll need new roles we haven’t even defined yet.
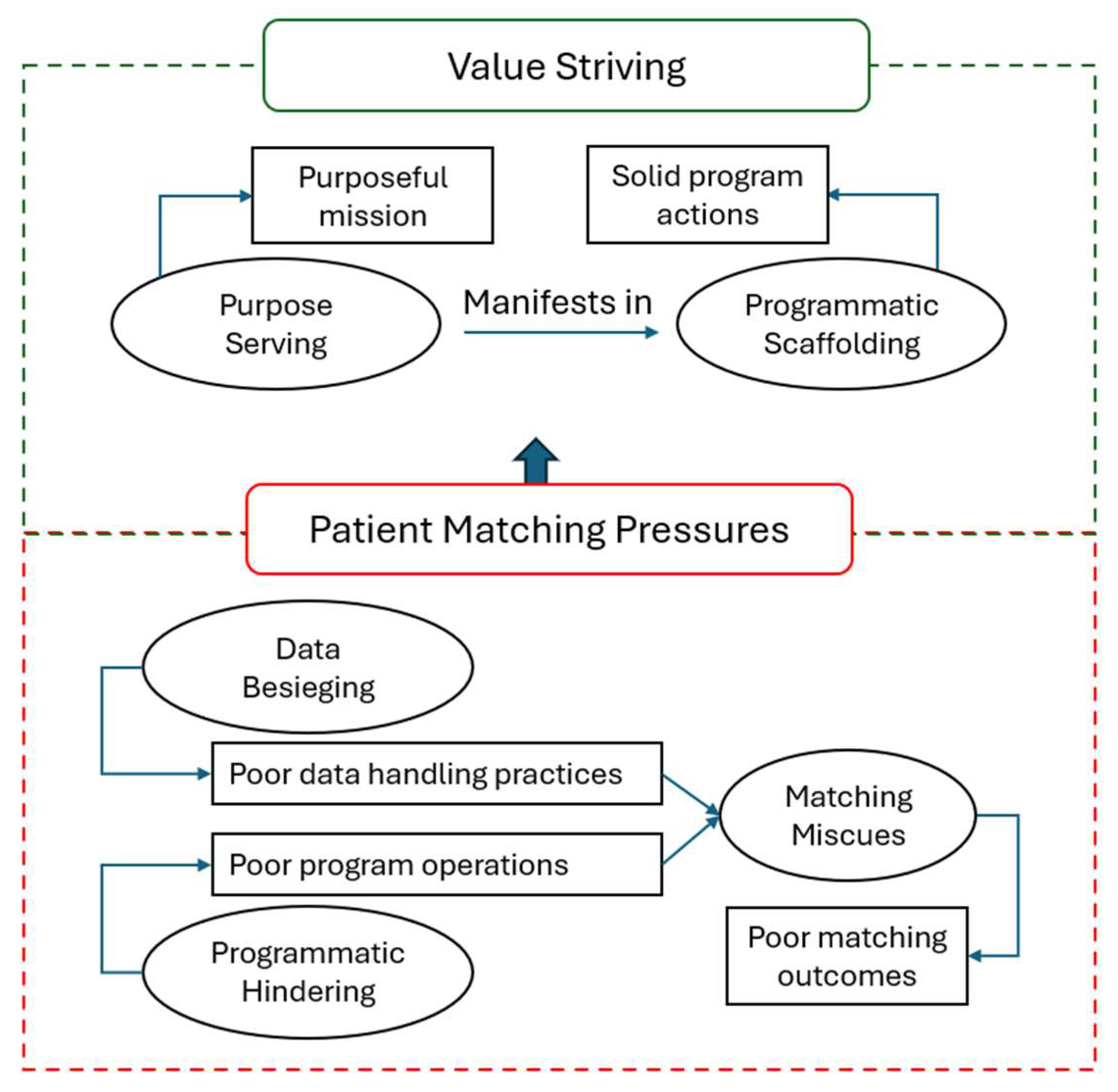
4.3. Value Striving
4.3.1. Purpose Serving
Some HIEs have always been ahead of their time. They were the first organizations to really think about how to move data at scale and how to build infrastructure to do so. And they’re all oftentimes just swimming upstream against policy and or you know, I’ll call it supply chain alignments in a world where most of the care continuum was to not make it easy for digital information to flow and to share. Some of these HIEs have been a beacon of light.
Essentiality of Matching
When I came to HIE I realized, because it’s a critical component of how the records are queried, stored, or used to match patients. And it was a huge problem for HIE in general if you couldn’t match. We had a tremendous number of patient records and if you could not match, what’s the sense of collecting these records.
Perpetuating Value
The value of HIE is this comprehensive view into the member as they’ve moved to multiple different provider types over the years and you know the acutely sick have many visits, right? They’re seeing specialists, they are seeing primary care providers, they are getting admitted into various hospitals and hospital systems. So, the MPI is the is like the one thing that brings all of that together for us. Otherwise, you know, you don’t have the complete picture of a patient.
4.3.2. Programmatic Scaffolding
Cultivating Strategic Partnerships
You guys are the people that hold the strings here when it comes to providing healthcare services to people, I need your help to fix this. So, we basically got around the table, enlisting community experts to solve issues and there was a coalition of healthcare stakeholders assembled to do just that.
System Enhancing
We’ve seen over the last years more and more focus on governance. So, on data governance and being aware of not just setting standards from a national level, but setting standards from an organizational level of saying, you know, these are minimum data standards we’re adhering to, and we are making the technology work groups actually adhere to them.
Optimized Matching Methodologies
But the approach what we have taken most is we have taken more like the hybrid approach, and we can combine algorithms, and we can do reviews, we want to push up scores, you know the most.
4.4. Patient Matching Pressures
4.4.1. Matching Miscues
We haven’t done it right in most cases, and when we can’t match a patient to their records or we make errors, we haven’t helped the patient, we haven’t equipped the doctor with the tools to get at that data in a way that gives them clarity.
Matching Misses
The expense of repeated medical care due to duplicate records costs about a thousand $950 per patient per inpatient stay and then over $1700 per emergency department visit. We know that 35% of all rejected claims result from inaccurate patient identification, which costs the average hospital 2.5 million, and the US [healthcare] system over 6.7 billion annually.
Merging Dangerously
If it’s not connected or it’s improperly overlaid or merged, it’s just, I think, a patient safety issue and with the exchange just growing and growing. You can’t control it after it’s gone on. So, if you’re using someone’s information and they’re not the right person or it’s not the right person’s information.
4.4.2. Data Besieging
I’m challenged by, you know, examples where organizations were, you know, told or informed about bad matches, false positives right and chose not to do anything about it. I’ve always struggled in that kind of a dynamic because of the impacts across, it hurts everyone. I would rather the outcome be correct than you know, sort of a head in the sand approach.
Chaotic Patient Intaking
Everybody has their own set of intake protocols, right? So, registration for, you know, for me at Hospital A has 15 different fields that I have to answer, you know, patient questionnaire, but if I go to Hospital B, maybe it’s 25, so there is no consistency from the start. This complicates things.
Proliferating Data
You know you could have person X, being a record, B, record, C, record, E, record. But you have to be careful about building a bridge across these sources, like you could have accidentally created a new person. That is an agglomeration now, it is way bigger now. It’s not just matching two records from A and B source. You could be matching against 20 records, 30 sources. So, the false positive avoidance is pretty important.
Undermining Data Quality
Some HIEs just absorb as much data as they can and some HIEs will actually put a little bit of governance upfront and be like hey I’m not going to take a sin record Right? If it’s not, if it’s a name and date of birth. That’s not enough. If you have a policy where you can enforce data quality standards at the source, that’s helpful for an HIE. But the fact remains we don’t see that and when someone lets bad data through, and we’ve seen it, it’s out there, and it’s not getting changed.
4.4.3. Programmatic Hindering
Just the amount of infrastructure and people you need to be able to support it. It is a lot, right? So that’s been kind of like. And it’s an activity that really needs to be enterprise wide and it’s not, it misses in many ways, from tech to process, and we’ve seen this in the HIEs we support in the state, there is varying emphasis on technology programs.
Faltering Systems
But if you can’t get good connectivity, if you can’t connect and others are down, you can’t get the data you need, you can’t communicate reliably and can’t find the person or if it is the same person from place to place.
Lagging Program Operations
I had been given the task to maintain the MPI when I came on 4 years ago, it had been started, I want to say 2017 … and never looked at. So, it hadn’t been tuned, it hadn’t been, you know, nothing was identified like nothing was working so what purpose was it serving?
Underemphasizing Data Stewardship
We get 15 million messages a month on average. So that’s a whole bunch of maybes that we’re still we can’t handle it like. There’s we cannot. There’s “no I could hire full time person to be their dedicated job just to do the human intervention, and that person wouldn’t be able to complete them all in a day, month, year.”
4.5. Grounded Theory Summary
5. Discussion
I’d say, it might be a little bit of a black box, so we don’t know exactly what they’re doing. So, I think that’s kind of always a big open question for me of what and how the algorithms are doing it.
If I’m going down an AI path, I need the AI to be transparent enough, that when we do quality control, we understand why it did what it did. Where I know what the calculation is, judge, the outcomes so that when I’m looking at an identity later I can systematically explain why that match was made.
We worry about this whole algorithmic bias issue of just because your model performs really well on the data you’ve trained it on does not mean it will perform really well on everybody’s data across every healthcare system across everything, right? That’s where they tend to make their mistakes, in the extreme cases on data you haven’t seen.
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Albarak, Mashel, and Rami Bahsoon. 2018. Prioritizing technical debt in database normalization using portfolio theory and data quality metrics. Paper presented at the 2018 International Conference on Technical Debt, Gothenburg, Sweden, May 27–28. [Google Scholar]
- Al Braiki, Atif, Hamed Ali Al Hashemi, Robert Denson, Sanji de Sylva, Ehab M. Fikry, Rahul Goyal, Bisera Lakinska, and Niam Yaraghi. 2024. Beyond Borders: Evaluating the Impact of Health Information Exchange on Resource Utilization in the United Arab Emirates—A Longitudinal Study. Information Systems Frontiers 27: 731–42. [Google Scholar] [CrossRef]
- Allen, Mike. 2004. Bush Touts Plan for Electronic Medicine. Washington Post, May 27. [Google Scholar]
- Barnett, Michael L., Asaf Bitton, Jeff Souza, and Bruce E. Landon. 2021. Trends in outpatient care for Medicare beneficiaries and implications for primary care, 2000 to 2019. Annals of Internal Medicine 174: 1658–65. [Google Scholar] [CrossRef]
- Benk, Michaela, Sophie Kerstan, Florian von Wangenheim, and Andrea Ferrario. 2024. Twenty-four years of empirical research on trust in AI: A bibliometric review of trends, overlooked issues, and future directions. AI & Society 40: 2083–106. [Google Scholar]
- Bloomrosen, Meryl, and Eta S. Berner. 2022. Findings from the 2022 Yearbook Section on Health Information Exchange. Yearbook of Medical Informatics 31: 215–18. [Google Scholar] [CrossRef]
- Borna, Sahar, Michael J. Maniaci, Clifton R. Haider, Karla C. Maita, Ricardo A. Torres-Guzman, Francisco R. Avila, Julianne J. Lunde, Jordan D. Coffey, Bart M. Demaerschalk, and Antonio J. Forte. 2023. Artificial intelligence models in health information exchange: A systematic review of clinical implications. Healthcare 11: 2584. [Google Scholar] [CrossRef]
- Bosh, Karin A., Joseph R. Coyle, Nicole W. Muriithi, Chitra Ramaswamy, Weilin Zhou, Antoine D. Brantley, Lauren J. Stockman, Lindsey VanderBusch, Emily F. Westheimer, Tian Tang, and et al. 2018. Linking HIV and viral hepatitis surveillance data: Evaluating a standard, deterministic matching algorithm using data from 6 US health jurisdictions. American Journal of Epidemiology 187: 2415–22. [Google Scholar] [CrossRef] [PubMed]
- Bouhaddou, Omar, Jamie Bennett, Tim Cromwell, Graham Nixon, Jennifer Teal, Mike Davis, Robert Smith, Linda Fischetti, David Parker, Zachary Gillen, and et al. 2011. The department of Veterans Affairs, department of defense, and Kaiser permanente nationwide health information network exchange in San Diego: Patient selection, consent, and identity matching. AMIA Annual Symposium Proceedings 2011: 135. [Google Scholar] [PubMed]
- Charmaz, Kathy. 2006. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. Thousand Oaks: SAGE Publications. Available online: https://books.google.com/books?id=v1qP1KbXz1AC (accessed on 1 March 2025).
- Charmaz, Kathy. 2014. Constructing grounded theory (introducing qualitative methods series). In Constructing Grounded Theory. Los Angeles: Sage. [Google Scholar]
- Chassin, Mark R., and Elise C. Becher. 2002. The wrong patient. Annals of Internal Medicine 136: 826–33. [Google Scholar] [CrossRef]
- Cox, Shelley, Rohan Martin, Piyali Somaia, and Karen Smith. 2012. The development of a data-matching algorithm to define the ‘case patient’. Australian Health Review 37: 54–59. [Google Scholar] [CrossRef]
- Deng, Yu, Lacey P. Gleason, Adam Culbertson, Xiaotian Chen, Elmer V. Bernstam, Theresa Cullen, Ramkiran Gouripeddi, Christopher Harle, David F. Hesse, Jacob Kean, and et al. 2023. Evolving availability and standardization of patient attributes for matching. Health Affairs Scholar 1: qxad047. [Google Scholar] [CrossRef] [PubMed]
- Eden, Karen B., Annette M. Totten, Steven Z. Kassakian, Paul N. Gorman, Marian S. McDonagh, Beth Devine, Mary Pappas, Mark Daeges, Sandra Woods, and William R. Hersh. 2016. Barriers and facilitators to exchanging health information: A systematic review. International Journal of Medical Informatics 88: 44–51. [Google Scholar] [CrossRef]
- Everson, Jordan, Keith E. Kocher, and Julia Adler-Milstein. 2016. Health information exchange associated with improved emergency department care through faster accessing of patient information from outside organizations. Journal of the American Medical Informatics Association 24: e103–e110. [Google Scholar] [CrossRef]
- Fichman, Robert G., and Chris F. Kemerer. 1999. The illusory diffusion of innovation: An examination of assimilation gaps. Information Systems Research 10: 255–75. [Google Scholar] [CrossRef]
- Furukawa, Michael F., Vaishali Patel, Dustin Charles, Matthew Swain, and Farzad Mostashari. 2013. Hospital electronic health information exchange grew substantially in 2008–12. Health Affairs 32: 1346–54. [Google Scholar] [CrossRef]
- Gefen, David, and Paul A. Pavlou. 2012. The Boundaries of Trust and Risk: The Quadratic Moderating Role of Institutional Structures. Information Systems Research 23: 940–59. [Google Scholar] [CrossRef]
- Gefen, David, Arik Ragowsky, Brian Leffew, and Rene Riedl. 2025. The Importance of Distrust in Trusting Digital Workers. Communications of ACM 68: 42–49. [Google Scholar] [CrossRef]
- Gefen, David, Ofir Ben-Assuli, Mark Stehr, Bruce Rosen, and Yaron Denekamp. 2019. Governmental intervention in Hospital Information Exchange (HIE) diffusion: A quasi-experimental ARIMA interrupted time series analysis of monthly HIE patient penetration rates. European Journal of Information Systems 28: 627–45. [Google Scholar] [CrossRef]
- Godlove, Tim, and Adrian W. Ball. 2015. Patient matching within a health information exchange. Perspectives in Health Information Management 12: 1g. [Google Scholar] [PubMed]
- Gopal, Gayatri, Clemens Suter-Crazzolara, Luca Toldo, and Werner Eberhardt. 2019. Digital transformation in healthcare–architectures of present and future information technologies. Clinical Chemistry and Laboratory Medicine (CCLM) 57: 328–35. [Google Scholar] [PubMed]
- Grannis, Shaun J., Huiping Xu, Joshua R. Vest, Suranga Kasthurirathne, Na Bo, Ben Moscovitch, Rita Torkzadeh, and Josh Rising. 2019. Evaluating the effect of data standardization and validation on patient matching accuracy. Journal of the American Medical Informatics Association 26: 447–56. [Google Scholar] [CrossRef]
- Grannis, Shaun J., Jennifer L. Williams, Suranga Kasthuri, Molly Murray, and Huiping Xu. 2022. Evaluation of real-world referential and probabilistic patient matching to advance patient identification strategy. Journal of the American Medical Informatics Association 29: 1409–15. [Google Scholar] [CrossRef]
- Greer, Melody L. 2020. 4294 Patient Matching Errors and Associated Safety Events. Journal of Clinical and Translational Science 4: 42. [Google Scholar] [CrossRef]
- Grote, Thomas., and Philipp Berens. 2020. On the ethics of algorithmic decision-making in healthcare. Journal of Medical Ethics 46: 205–11. [Google Scholar] [CrossRef] [PubMed]
- Hagger-Johnson, Gareth, Katie Harron, Harvey Goldstein, Robert Aldridge, and Ruth Gilbert. 2017. Probabilistic linking to enhance deterministic algorithms and reduce linkage errors in hospital administrative data. Journal of Innovation in Health Informatics 24: 891. [Google Scholar] [CrossRef] [PubMed]
- Halevy, Alon Y. 2011. Game-changing interoperability for healthcare: Bringing semantically harmonized clinical information into provider workflows from disparate health information technologies. Paper presented at the 2011 8th International Conference & Expo on Emerging Technologies for a Smarter World, Hauppauge, NY, USA, November 2–3. [Google Scholar]
- HealthIT.gov. 2022. National Trends in Hospital and Physician Adoption of Electronic Health Records. Assistant Secretary for Technology Policy. Available online: https://www.healthit.gov/data/quickstats/national-trends-hospital-and-physician-adoption-electronic-health-records (accessed on 1 March 2025).
- Heath, Michele L., Radha Appan, and Naveen Gudigantala. 2017. Exploring Health Information Exchange (HIE) Through Collaboration Framework: Normative Guidelines for IT Leadership of Healthcare Organizations. Information Systems Management 34: 137–56. [Google Scholar] [CrossRef]
- Hersh, William R., Annette M. Totten, Karen B. Eden, Beth Devine, Paul Gorman, Steven Z. Kassakian, Susan S. Woods, Monica Daeges, Miranda Pappas, and Marian S. McDonagh. 2015. Outcomes from health information exchange: Systematic review and future research needs. JMIR Medical Informatics 3: e5215. [Google Scholar] [CrossRef]
- Holmgren, A. Jay, and Julia Adler-Milstein. 2017. Health information exchange in US hospitals: The current landscape and a path to improved information sharing. Journal of Hospital Medicine 12: 193–98. [Google Scholar] [CrossRef]
- Holzinger, Andreas, Georg Langs, Helmut Denk, Kurt Zatloukal, and Heimo Müller. 2019. Causability and explainability of artificial intelligence in medicine. Wiley Interdisciplinary Reviews: Data Mining and Knowledge Discovery 9: e1312. [Google Scholar]
- Hripcsak, George, Meryl Bloomrosen, Patricia Flatley Brennan, Christopher G. Chute, Jim Cimino, Don E. Detmer, Margo Edmunds, Peter J. Embi, Melissa M. Goldstein, William E. Hammond, and et al. 2013. Health data use, stewardship, and governance: Ongoing gaps and challenges: A report from AMIA’s 2012 Health Policy Meeting. Journal of the American Medical Informatics Association 21: 204–11. [Google Scholar] [CrossRef]
- Hulsen, Tim. 2020. Sharing is caring—Data sharing initiatives in healthcare. International Journal of Environmental Research and Public Health 17: 3046. [Google Scholar] [CrossRef]
- IEEE. 2024. A Transdisciplinary Framework for Effective and Reliable Continuum of Care. In A Transdisciplinary Framework for Effective and Reliable Continuum of Care. Piscataway: IEEE, pp. 1–37. [Google Scholar]
- Janakiraman, Ramkumar, Eunho Park, Emre M. Demirezen, and Subodha Kumar. 2023. The effects of health information exchange access on healthcare quality and efficiency: An empirical investigation. Management Science 69: 791–811. [Google Scholar] [CrossRef]
- Just, Beth H., David Marc, Megan Munns, and Ryan Sandefer. 2016. Why patient matching is a challenge: Research on master patient index (MPI) data discrepancies in key identifying fields. Perspectives in Health Information Management 13: 1e. [Google Scholar]
- Kaelber, David C., and David W. Bates. 2007. Health information exchange and patient safety. Journal of Biomedical Informatics 40: S40–S45. [Google Scholar] [CrossRef]
- Kash, Bita A., Juha Baek, Elise Davis, Tiffany Champagne-Langabeer, and James R. Langabeer, II. 2017. Review of successful hospital readmission reduction strategies and the role of health information exchange. International Journal of Medical Informatics 104: 97–104. [Google Scholar] [CrossRef]
- Kohn, Linda T., Janet M. Corrigan, and Molla S. Donaldson. 2000. To Err is Human: Building a Safer Health System. In To Err is Human: Building a Safer Health System. Edited by Linda T. Kohn, Janet M. Corrigan and Molla S. Donaldson. Washington, DC: Donaldson National Academies Press (US). [Google Scholar] [CrossRef]
- Kuperman, Gilad. J. 2011. Health-information exchange: Why are we doing it, and what are we doing? Journal of the American Medical Informatics Association 18: 678–82. [Google Scholar] [CrossRef]
- Lammers, Emily J., Julia Adler-Milstein, and Keith E. Kocher. 2014. Does Health Information Exchange Reduce Redundant Imaging? Evidence From Emergency Departments. Medical Care 52: 227–34. [Google Scholar] [CrossRef]
- Liao, Joshua M., and Danny Chu. 2012. The state of health information exchange. Journal of Health & Medical Informatics 3: 1–2. [Google Scholar]
- McDonald, Clement J. 1981. Action-Oriented Decisions in Ambulatory Medicine. Chicago: Year Book Medical Publishers Chicago. [Google Scholar]
- McDonald, Clement J., J. Marc Overhage, William M. Tierney, Paul R. Dexter, Douglas K. Martin, Jeffrey G. Suico, Atif Zafar, Gunther Schadow, Lonnie Blevins, Tull Glazener, and et al. 1999. The Regenstrief Medical Record System: A quarter century experience. International Journal of Medical Informatics 54: 225–53. [Google Scholar] [CrossRef]
- Menachemi, Nir, Saurabh Rahurkar, Christopher A. Harle, and Joshua R. Vest. 2018. The benefits of health information exchange: An updated systematic review. Journal of the American Medical Informatics Association 25: 1259–65. [Google Scholar] [CrossRef]
- Pai, Dinesh R., Balaraman Rajan, and Subhajit Chakraborty. 2022. Do EHR and HIE deliver on their promise? Analysis of Pennsylvania acute care hospitals. International Journal of Production Economics 245: 108398. [Google Scholar] [CrossRef]
- Parker, Carol J., and Julia Adler-Milstein. 2016. Errors related to health information exchange. In Safety of Health IT: Clinical Case Studies. Berlin/Heidelberg: Springer, pp. 153–65. [Google Scholar]
- Prakash, Ashish V., and Saini Das. 2021. Medical practitioner’s adoption of intelligent clinical diagnostic decision support systems: A mixed-methods study. Information & Management 58: 1–24. [Google Scholar]
- Rahurkar, Saurabh, Joshua R. Vest, and Nir Menachemi. 2015. Despite The Spread of Health Information Exchange, There Is Little Evidence of Its Impact on Cost, Use, and Quality of Care. Health Affairs 34: 477–83. [Google Scholar] [CrossRef] [PubMed]
- Riplinger, Lauren, Jordi Piera-Jiménez, and Julie P. Dooling. 2020. Patient identification techniques–approaches, implications, and findings. Yearbook of medical informatics 29: 81–86. [Google Scholar] [CrossRef]
- Rosenthal, Sarah, Julia Adler-Milstein, and Vaishali Patel. 2024. Public Health Data Exchange Through Health Information Exchange Organizations: National Survey Study. JMIR Public Health and Surveillance 10: e64969. [Google Scholar] [CrossRef]
- Rudin, Robert S., Aneesa Motala, Carolyn L. Goldzweig, and Paul G. Shekelle. 2014. Usage and effect of health information exchange: A systematic review. Annals of Internal Medicine 161: 803–11. [Google Scholar] [CrossRef]
- Sandeep, MM, Lavanya Vilvanathan, and Janarthanan Balakrishnan. 2025. Leveraging AI in recruitment: Enhancing intellectual capital through resource-based view and dynamic capability framework. Journal of Intellectual Capital 26: 404–25. [Google Scholar] [CrossRef]
- Shaban-Nejad, Arash, Martin Michalowski, and David L. Buckeridge. 2018. Health intelligence: How artificial intelligence transforms population and personalized health. NPJ Digital Medicine 1: 53. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, Jason S., Farzad Mostashari, George Hripcsak, Nicholas Soulakis, and Gilad Kuperman. 2011. Using health information exchange to improve public health. American Journal of Public Health 101: 616–23. [Google Scholar] [CrossRef]
- Shen, Nelson, Thérèse Bernier, Lydia Sequeira, John Strauss, Michelle P. Silver, Abigail Carter-Langford, and David Wiljer. 2019. Understanding the patient privacy perspective on health information exchange: A systematic review. International Journal of Medical Informatics 125: 1–12. [Google Scholar] [CrossRef]
- Sherifi, Dasantila. 2019. Impact. In Portable Health Records in a Mobile Society. Edited by Egondu R. Onyejekwe, Jon Rokne and Cory L. Hall. Berlin and Heidelberg: Springer International Publishing, pp. 227–32. [Google Scholar] [CrossRef]
- Slager, Staci, Julie Beckstrom, Charlene Weir, Guilherme Del Fiol, and Benjamin S. Brooke. 2017. Information exchange between providers during transitions of surgical care: Communication, documentation and sometimes both. In Building Capacity for Health Informatics in the Future. Amsterdam: IOS Press, pp. 303–8. [Google Scholar]
- Sonko, Sedat S., Adebusuyi O. Adewusi, Obiajulu C. Obi, Shedrack Onwusinkwue, and Akoh Atadoga. 2024. A critical review towards artificial general intelligence: Challenges, ethical considerations, and the path forward. World Journal of Advanced Research and Reviews 21: 1262–68. [Google Scholar] [CrossRef]
- Sragow, Howard M., Eileen Bidell, Douglas Mager, and Shaun Grannis. 2020. Universal patient identifier and interoperability for detection of serious drug interactions: Retrospective study. JMIR Medical Informatics 8: e23353. [Google Scholar] [CrossRef] [PubMed]
- Swain, Michael, Dustin Charles, Vaishali Patel, and Talisha Searcy. 2015. Health information exchange among US non-federal acute care hospitals: 2008–14. ONC Data Brief 24: 1–12. [Google Scholar]
- Thornton, Sidney N., and Shannon K. Hood. 2005. Reducing duplicate patient creation using a probabilistic matching algorithm in an open-access community data sharing environment. Paper presented at the AMIA Annual Symposium Proceedings, Washington, DC, USA, October 22–26. [Google Scholar]
- Torres, Gretchen W., Karen Swietek, Petry S. Ubri, Rachel F. Singer, Kristina H. Lowell, and Wilhelmine Miller. 2014. Building and strengthening infrastructure for data exchange: Lessons from the beacon communities. eGEMs 2: 1092. [Google Scholar] [CrossRef][Green Version]
- Vest, Joshua R., and Larry D. Gamm. 2010. Health information exchange: Persistent challenges and new strategies. Journal of the American Medical Informatics Association: JAMIA 17: 288. [Google Scholar] [CrossRef]
- Wiens, Jenna, Suchi Saria, Mark Sendak, Marzyeh Ghassemi, Vincent X. Liu, Finale Doshi-Velez, Kenneth Jung, Katherine Heller, David Kale, and Mohammed Saeed. 2019. Do no harm: A roadmap for responsible machine learning for health care. Nature Medicine 25: 1337–40. [Google Scholar] [CrossRef]
- Wu, Huixin, and Elizabeth M. LaRue. 2017. Linking the health data system in the US: Challenges to the benefits. International Journal of Nursing Sciences 4: 410–17. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Yan, Lincoln R. Sheets, Yin-Wu Chen, Zon-Yin Shae, Jeffrey J. P. Tsai, and Chi-Ren Shyu. 2020. A Patient-Centric Health Information Exchange Framework Using Blockchain Technology. IEEE Journal of Biomedical and Health Informatics 24: 2169–76. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Licciardello, T.R.; Gefen, D.; Nag, R. Cautious Optimism Building: What HIE Managers Think About Adding Artificial Intelligence to Improve Patient Matching. Soc. Sci. 2025, 14, 579. https://doi.org/10.3390/socsci14100579
Licciardello TR, Gefen D, Nag R. Cautious Optimism Building: What HIE Managers Think About Adding Artificial Intelligence to Improve Patient Matching. Social Sciences. 2025; 14(10):579. https://doi.org/10.3390/socsci14100579
Chicago/Turabian StyleLicciardello, Thomas R., David Gefen, and Rajiv Nag. 2025. "Cautious Optimism Building: What HIE Managers Think About Adding Artificial Intelligence to Improve Patient Matching" Social Sciences 14, no. 10: 579. https://doi.org/10.3390/socsci14100579
APA StyleLicciardello, T. R., Gefen, D., & Nag, R. (2025). Cautious Optimism Building: What HIE Managers Think About Adding Artificial Intelligence to Improve Patient Matching. Social Sciences, 14(10), 579. https://doi.org/10.3390/socsci14100579








