The Mediating Effect of Psychological Resilience between Individual Social Capital and Mental Health in the Post-Pandemic Era: A Cross-Sectional Survey over 300 Family Caregivers of Kindergarten Children in Mainland China
Abstract
1. Introduction
1.1. Social Capital and Mental Health
1.2. Psychological Resilience and Mental Health
1.3. The Mediation Role of Psychological Resilience between Social Capital and Mental Health
1.4. The Current Study
2. Materials and Methods
2.1. Participants and Sampling
2.2. Measurements
2.2.1. Personal Social Capital Scale
2.2.2. Depression Anxiety Stress Scales
2.2.3. Connor–Davidson Resilience Scale
2.3. Data Analysis
3. Results
3.1. Characteristics of Participants
3.2. Correlations among Main Variables
3.3. Influencing Factors of Mental Health Outcomes
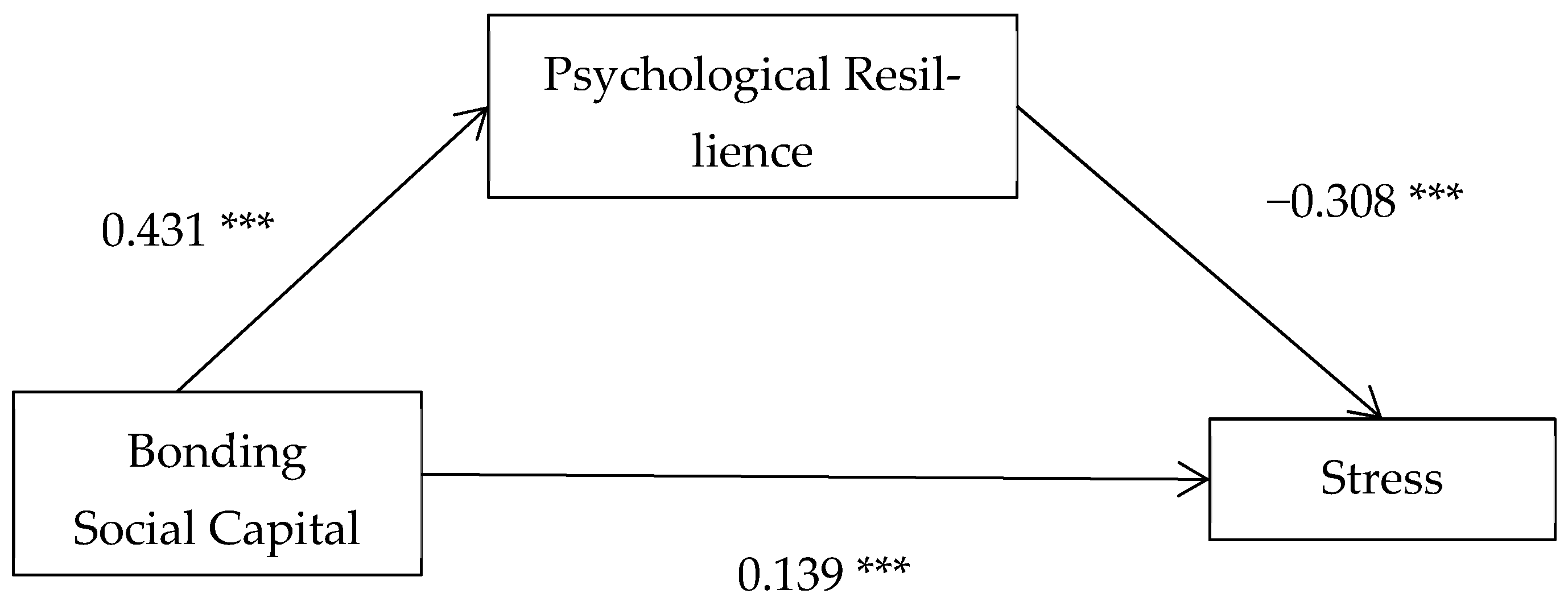
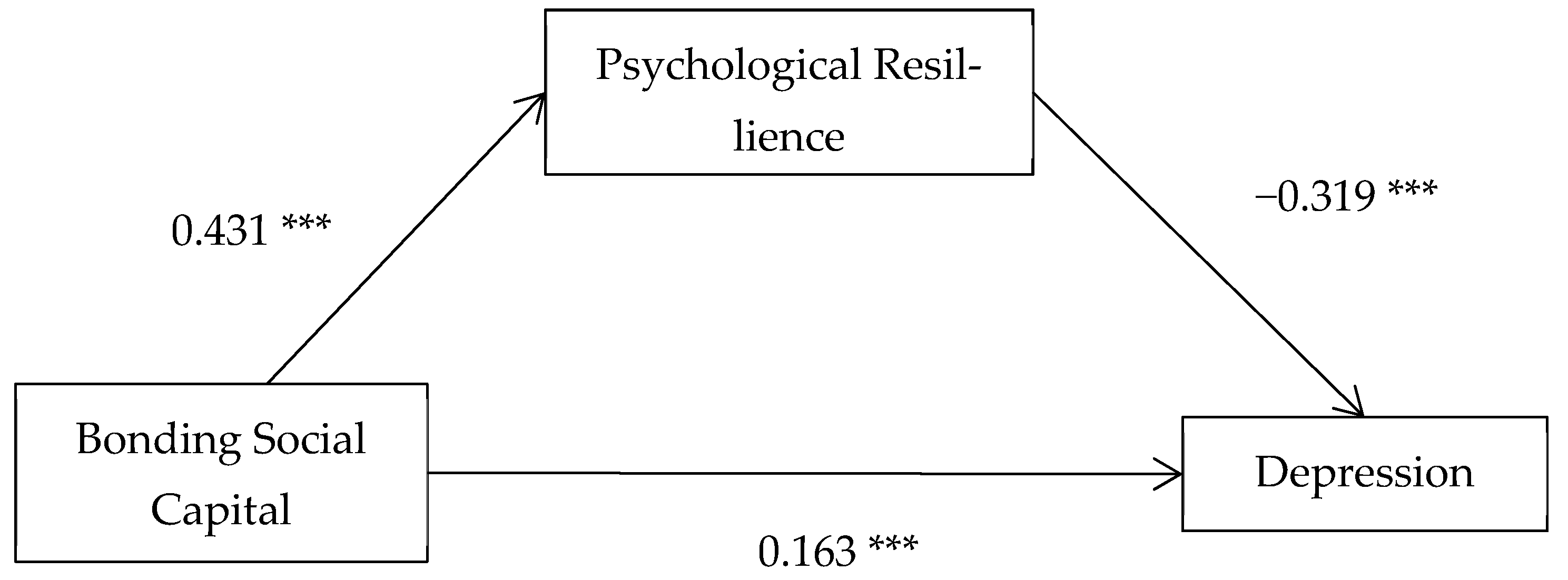
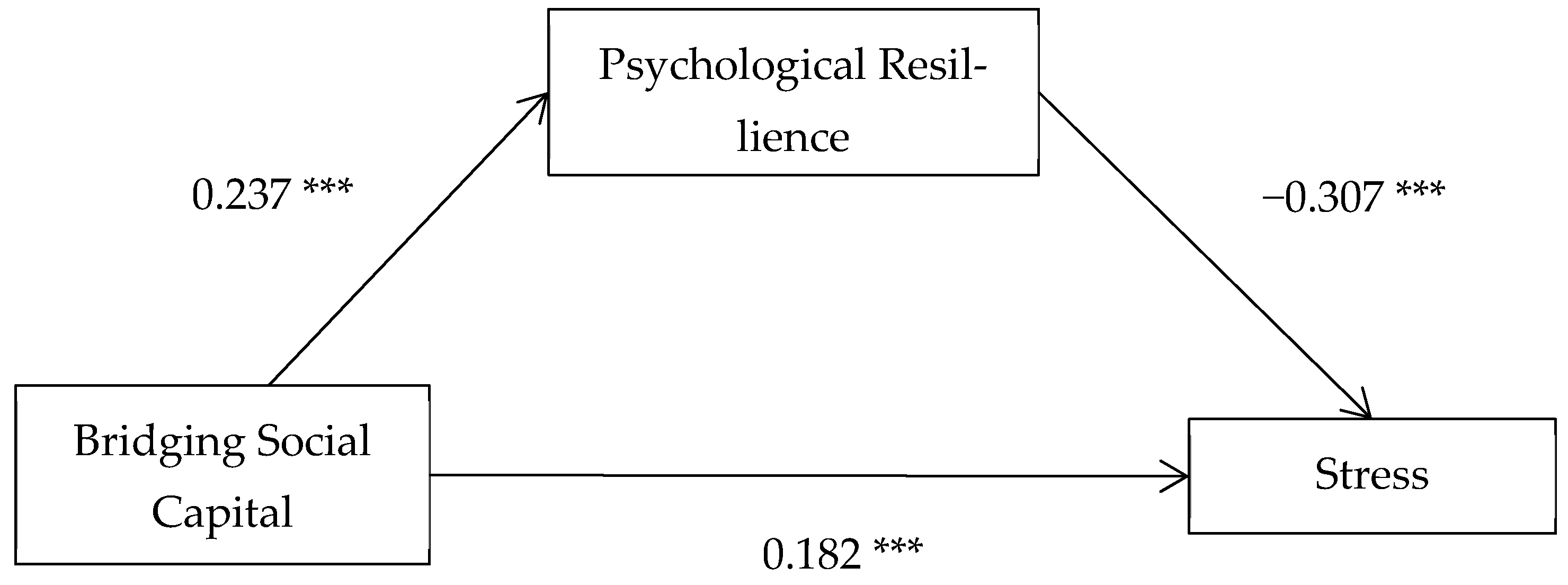
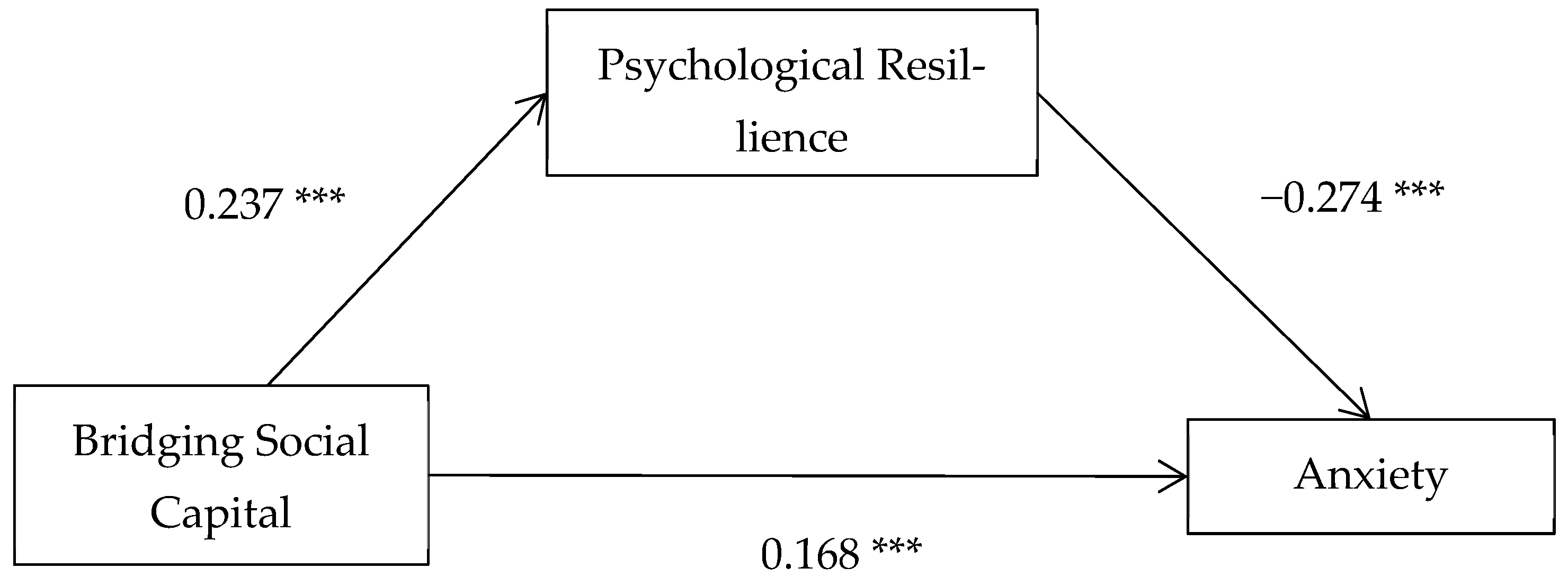
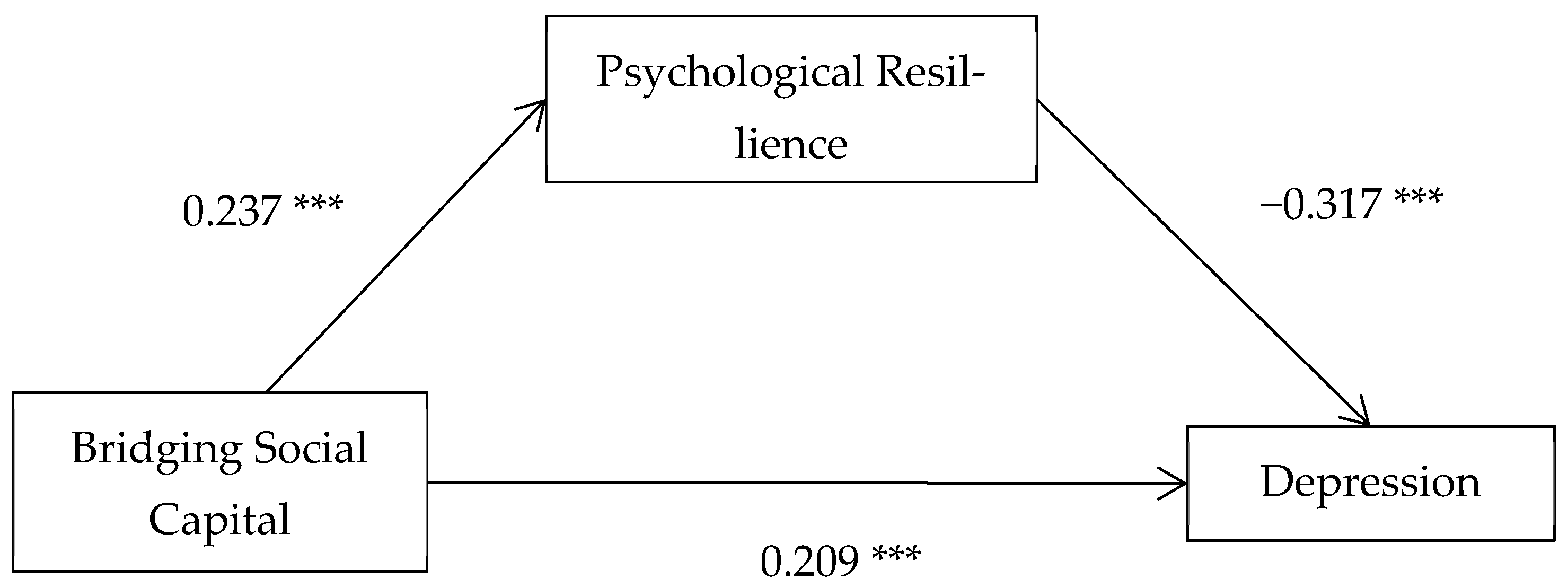
3.4. Mediation Analysis
4. Discussion
4.1. Social Capital and Mental Health
4.2. Psychological Resilience and Mental Health
4.3. Social Capital and Psychological Resilience
4.4. Mediating Role of Psychological Resilience
5. Implications
6. Limitation and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aburn, Gemma, Merryn Gott, and Karen Hoare. 2016. What is resilience? An integrative review of the empirical literature. Journal of Advanced Nursing 72: 980–1000. [Google Scholar] [CrossRef] [PubMed]
- Adelinejad, Fatemeh, Mirtaher Mousavi, and Alireza Mohseni Tabrizi. 2022. The effect of social capital on the mental health of the university students during the COVID-19 pandemic with the mediation of the resilience variable. Health in Emergencies and Disasters Quarterly 8: 27–38. [Google Scholar] [CrossRef]
- Aldrich, Daniel P. 2012. Building Resilience: Social Capital in Post-Disaster Recovery. Chicago: University of Chicago Press. [Google Scholar]
- Aldrich, Daniel P., and Michelle A. Meyer. 2015. Social capital and community resilience. American Behavioral Scientist 59: 254–69. [Google Scholar] [CrossRef]
- Ali, Afia, Michael King, Andre Strydom, and Angela Hassiotis. 2016. Self-reported stigma and its association with socio-demographic factors and physical disability in people with intellectual disabilities: Results from a cross-sectional study in England. Social Psychiatry and Psychiatric Epidemiology 51: 465–74. [Google Scholar] [CrossRef]
- Antony, Martin M., Peter J. Bieling, Brian J. Cox, Murray W. Enns, and Richard P. Swinson. 1998. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment 10: 176–81. [Google Scholar] [CrossRef]
- Archuleta, Adrian J., and Christina R. Miller. 2011. Validity evidence for the translated version of the Personal Social Capital Scale. Journal of the Society for Social Work and Research 2: 39–53. [Google Scholar] [CrossRef]
- Barrett, Patrick, Beatrice Hale, and Mary Butler. 2014. Family Care and Social Capital: Transitions in Informal Care. Berlin/Heidelberg: Springer, p. 170. [Google Scholar]
- Bassett, Emma, and Spencer Moore. 2013. Mental Health and Social Capital: Social Capital as a Promising Initiative to Improving the Mental Health of Communities. London: InTech. [Google Scholar] [CrossRef]
- Bourdieu, P. 2008. The Forms of Capital (1986). In Readings in Economic Sociology, 2nd ed. Edited by Nicole Woolsey Biggart. New York: John Wiley & Sons, pp. 280–91. [Google Scholar]
- Brodaty, Henry, and Marika Donkin. 2009. Family caregivers of people with dementia. Dialogues in Clinical Neuroscience 11: 217–28. [Google Scholar] [CrossRef]
- Calvano, Claudia, Lara Engelke, Jessica Di Bella, Jana Kindermann, Babette Renneberg, and Sibylle M. Winter. 2021. Families in the COVID-19 pandemic: Parental stress, parent mental health and the occurrence of adverse childhood experiences—Results of a representative survey in Germany. European Child and Adolescent Psychiatry 31: 1–13. [Google Scholar] [CrossRef] [PubMed]
- Campbell-Sills, Laura, and Murray B. Stein. 2007. Psychometric analysis and refinement of the connor–davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies 20: 1019–28. [Google Scholar] [CrossRef] [PubMed]
- Chadda, Rakesh K. 2014. Caring for the family caregivers of persons with mental illness. Indian Journal of Psychiatry 56: 221–27. [Google Scholar] [CrossRef]
- Chan, Sally Wai-Chi. 2011. Family caregiving in dementia: The Asian perspective of a global problem. Dementia and Geriatric Cognitive Disorders 30: 469–78. [Google Scholar] [CrossRef]
- Chen, Sue-Hsien, Jing-Long Huang, Kuo-Wei Yeh, and Yun-Fang Tsai. 2015. The stress of caring for children with asthma: A qualitative study of primary caregivers. Journal of Nursing Research 23: 298–307. [Google Scholar] [CrossRef]
- Chen, Xiaoyun, Yixuan Mao, Linghua Kong, Guopeng Li, Minglan Xin, Fenglan Lou, and Ping Li. 2016. Resilience moderates the association between stigma and psychological distress among family caregivers of patients with schizophrenia. Personality and Individual Differences 96: 78–82. [Google Scholar] [CrossRef]
- Chen, Xinguang, Bonita Stanton, Jie Gong, Xiaoyi Fang, and Xiaoming Li. 2009. Personal Social Capital Scale: An instrument for health and behavioural research. Health Education Research 24: 306–17. [Google Scholar] [CrossRef] [PubMed]
- Chen, Xinguang, Mengting Gao, Yayun Xu, Yan Wang, and Shiyue Li. 2018. Associations between personal social capital and depressive symptoms: Evidence from a probability sample of urban residents in China. International Journal of Social Psychiatry 64: 767–77. [Google Scholar] [CrossRef]
- Cheng, Chang, Daifeng Dong, Jiayue He, Xue Zhong, and Shuqiao Yao. 2020. Psychometric properties of the 10-item Connor–Davidson Resilience Scale (CD-RISC-10) in Chinese undergraduates and depressive patients. Journal of Affective Disorders 261: 211–20. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Marcus Y. L., Xinlin Yang, F. H. T. Wong, J. H. Li, and J. Li. 2013. Caregiving of children with intellectual disabilities in China—An examination of affiliate stigma and the cultural thesis. Journal of Intellectual Disability Research 57: 1117–29. [Google Scholar] [CrossRef]
- Connor, Kathryn M., and Jonathan R. T. Davidson. 2003. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depression and Anxiety 18: 76–82. [Google Scholar] [CrossRef] [PubMed]
- Costa, Ana Carla dos Santos, Vaishnavi Menon, Rachana Phadke, Kartik Dapke, Adriana Viola Miranda, Shoaib Ahmad, Mohammad Yasir Essar, and Hashim Talib Hashim. 2022. Mental health in the post COVID-19 era: Future perspectives. Einstein 20: eCE6760. [Google Scholar] [CrossRef] [PubMed]
- Dai, Xianhua, and Nian Gu. 2021. The impact of social capital on mental health: Evidence from the China family panel survey. International Journal of Environmental Research and Public Health 19: 190. [Google Scholar] [CrossRef] [PubMed]
- Ding, Xiuxiu, Mingming Liang, Qiuxia Song, Wanying Su, Ning Li, Haixia Liu, Yile Wu, Xianwei Guo, Hao Wang, Jian Zhang, and et al. 2023. Development of psychological resilience and associations with emotional and behavioral health among preschool left-behind children. Social Psychiatry and Psychiatric Epidemiology 58: 467–76. [Google Scholar] [CrossRef]
- Dominguez, Silvia, and Tammi Arford. 2010. It is all about who you know: Social capital and health in low-income communities. Health Sociology Review 19: 114–29. [Google Scholar] [CrossRef]
- Drouin, Michelle, Brandon T. McDaniel, Jessica Pater, and Tammy Toscos. 2020. How parents and their children used social media and technology at the beginning of the COVID-19 pandemic and associations with anxiety. Cyberpsychology, Behavior, and Social Networking 23: 727–36. [Google Scholar] [CrossRef]
- Eberl, Andreas. 2020. The effect of informal caregiving on social capital investments. Social Science Research 85: 102319. [Google Scholar] [CrossRef] [PubMed]
- Ehsan, Annahita, Hannah Sophie Klaas, Alexander Bastianen, and Dario Spini. 2019. Social capital and health: A systematic review of systematic reviews. SSM-Population Health 8: 100425. [Google Scholar] [CrossRef]
- Ferlander, Sara, Andrew Stickley, Olga Kislitsyna, Tanya Jukkala, Per Carlson, and Ilkka Henrik Makine. 2016. Social capital–a mixed blessing for women? A cross-sectional study of different forms of social relations and self-rated depression in Moscow. BMC Psychology 4: 1–12. [Google Scholar] [CrossRef]
- Furukawa, Hidetoshi, and Chieko Greiner. 2020. Developing a social capital scale for family caregivers of people with dementia. Geriatric Nursing 41: 740–46. [Google Scholar] [CrossRef] [PubMed]
- Gao, Mengting, Chenchang Xiao, Xuan Zhang, Shiyue Li, and Hong Yan. 2018. Social capital and PTSD among PLWHA in China: The mediating role of resilience and internalized stigma. Psychology, Health & Medicine 23: 698–706. [Google Scholar] [CrossRef]
- Gazzaz, Arwa Z., Richard M. Carpiano, Denise M. Laronde, and Jolanta Aleksejuniene. 2022. Parental psychosocial factors, unmet dental needs and preventive dental care in children and adolescents with special health care needs: A stress process model. BMC Oral Health 22: 282. [Google Scholar] [CrossRef] [PubMed]
- Giesbrecht, Melissa, Faye Wolse, Valorie A. Crooks, and Kelli Stajduhar. 2015. Identifying socio-environmental factors that facilitate resilience among Canadian palliative family caregivers: A qualitative case study. Palliative & Supportive Care 13: 555–65. [Google Scholar] [CrossRef]
- Gong, X., X. Y. Xie, R. Xu, and Y. J. Luo. 2010. Depression-Anxiety-Stress Scale Chinese Simplified Edition (DASS-21) test report among Chinese college students. Chinese Journal of Clinical Psychology 4: 443–46. [Google Scholar] [CrossRef]
- Graber, Rebecca, Florence Pichon, and Elizabeth Carabine. 2015. Psychological Resilience. London: Overseas Development Institute. [Google Scholar]
- Granek, L., Z. R. S. Rosenberg-Yunger, D. Dix, R. J. Klaassen, L. Sung, J. Cairney, and A. F. Klassen. 2014. Caregiving, single parents and cumulative stresses when caring for a child with cancer. Child: Care, Health and Development 40: 184–94. [Google Scholar] [CrossRef]
- Hayes, Andrew F. 2018. Partial, conditional, and moderated moderated mediation: Quantification, inference, and interpretation. Communication Monographs 85: 4–40. [Google Scholar] [CrossRef]
- He, Beiting, Ran An, and John Berry. 2019. Psychological adjustment and social capital: A qualitative investigation of Chinese expatriates. Cross Cultural & Strategic Management 26: 67–92. [Google Scholar] [CrossRef]
- He, Fei, Rong Cao, Ziqi Feng, Hao Guan, and Jiaxi Peng. 2013. The impacts of dispositional optimism and psychological resilience on the subjective well-being of burn patients: A structural equation modelling analysis. PLoS ONE 8: e82939. [Google Scholar] [CrossRef]
- Herrmann-Pillath, Carsten. 2010. Social capital, Chinese style: Individualism, relational collectivism and the cultural embeddedness of the institutions–performance link. China Economic Journal 2: 325–50. [Google Scholar] [CrossRef]
- Horiuchi, Shiro, Yusuke Kanazawa, Takahisa Suzuki, and Hiroki Takikawa. 2013. Who gains resources from which social capital? A mathematical review. In Social Capital: Theory, Measurement and Outcomes. Hauppauge: Nova Publishers, pp. 1–27. [Google Scholar]
- Hue, Ming-tak, and Ngar-sze Lau. 2015. Promoting well-being and preventing burnout in teacher education: A pilot study of a mindfulness-based programme for pre-service teachers in Hong Kong. Teacher Development 19: 381–401. [Google Scholar] [CrossRef]
- Jamison, Jesslyn M., Dominique Egger, Christian E. Vazquez, Megan J. McBride, Sydney N. Pauling, Katherine E. Hess, Esther J. Calzada, and Sarah Kate Bearman. 2023. Mental health trajectories of Latinx female caregivers and young children during COVID-19: A longitudinal analysis. Journal of Child and Family Studies 32: 571–85. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Dongdong, Yajie Yan, Han Zhou, and Quan Wang. 2022. The association between personal social capital and health-related quality of life among Chinese older people: A cross-sectional study. Frontiers in Nutrition 9: 995729. [Google Scholar] [CrossRef] [PubMed]
- Khaksar, Seyed Mohammad Sadegh, Tahereh Maghsoudi, and Suzanne Young. 2019. Social capital, psychological resilience and job burnout in hazardous work environments. Labour & Industry: A Journal of the Social and Economic Relations of Work 29: 155–80. [Google Scholar] [CrossRef]
- Lai, Daniel WL, and Caroline Thomson. 2011. The impact of perceived adequacy of social support on caregiving burden of family caregivers. Families in Society 92: 99–106. [Google Scholar] [CrossRef]
- Lee, Vivian, Carly Albaum, Paula Tablon Modica, Farah Ahmad, Jan Willem Gorter, Nazilla Khanlou, and Carly McMorris. 2021. The impact of COVID-19 on the mental health and well-being of caregivers of autistic children and youth: A scoping review. Autism Research 14: 2477–94. [Google Scholar] [CrossRef]
- Leng, Anli, Caifen Xu, Stephen Nicholas, Jennifer Nicholas, and Jian Wang. 2019. Quality of life in caregivers of a family member with serious mental illness: Evidence from China. Archives of Psychiatric Nursing 33: 23–29. [Google Scholar] [CrossRef] [PubMed]
- Lewis, Joanne M., Michelle DiGiacomo, Tim Luckett, Patricia M. Davidson, and David C. Currow. 2013. A social capital framework for palliative care: Supporting health and well-being for people with life-limiting illness and their carers through social relations and networks. Journal of Pain and Symptom Management 45: 92–103. [Google Scholar] [CrossRef] [PubMed]
- Li, Chunkai, Shan Jiang, and Xiaotong Fang. 2020. Effects of multi-dimensional social capital on mental health of children in poverty: An empirical study in Mainland China. Journal of Health Psychology 25: 853–67. [Google Scholar] [CrossRef] [PubMed]
- Li, Ting, and Qiang Xie. 2022. Effects of college students’ perceived stress on anxiety in the time of COVID-19: The chain mediation role of psychological resilience and regulatory emotional self-efficacy. International Journal of Mental Health Promotion 24: 263–76. [Google Scholar] [CrossRef]
- Li, Yawen, Ling Xu, Iris Chi, and Ping Guo. 2014. Participation in productive activities and health outcomes among older adults in urban China. The Gerontologist 54: 784–96. [Google Scholar] [CrossRef] [PubMed]
- Lin, Fang-Yi, Jiin-Ru Rong, and Tzu-Ying Lee. 2013. Resilience among caregivers of children with chronic conditions: A concept analysis. Journal of Multidisciplinary Healthcare 6: 323–33. [Google Scholar] [CrossRef] [PubMed]
- Liu, Yujun, M. Courtney Hughes, Karen A. Roberto, and Jyoti Savla. 2022. Physical and mental health of family caregivers of older parents and grandchildren in China. Aging and Health Research 2: 100052. [Google Scholar] [CrossRef]
- Liu, Yujun, Rong Fu, Karen A. Roberto, and Jyoti Savla. 2019. Depressive symptoms among adult children caregivers in China: Moderating effects of working status and gender. Aging & Mental Health 23: 1391–99. [Google Scholar] [CrossRef]
- Lovibond, Peter F., and Sydney H. Lovibond. 1995. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy 33: 335–43. [Google Scholar] [CrossRef]
- Lu, Nan, Shicun Xu, and Jingyue Zhang. 2021. Community social capital, family social capital, and self-rated health among older rural Chinese adults: Empirical evidence from rural northeastern China. International Journal of Environmental Research and Public Health 18: 5516. [Google Scholar] [CrossRef]
- Mandelbaum, Jennifer, Spencer Moore, Patricia P. Silveira, Michael J. Meaney, Robert D. Levitan, and Laurette Dubé. 2020. Does social capital moderate the association between children’s emotional overeating and parental stress? A cross-sectional study of the stress-buffering hypothesis in a sample of mother-child dyads. Social Science & Medicine 257: 112082. [Google Scholar] [CrossRef]
- Masten, Ann S. 2001. Ordinary magic: Resilience processes in development. American Psychologist 56: 227. [Google Scholar] [CrossRef]
- Wen, Ming, and Danhua Lin. 2012. Child development in rural China: Children left behind by their migrant parents and children of nonmigrant families. Child Development 83: 120–36. [Google Scholar] [CrossRef]
- Moore, Spencer, and Ichiro Kawachi. 2017. Twenty years of social capital and health research: A glossary. Journal Epidemiol Community Health 71: 513–17. [Google Scholar] [CrossRef]
- Moussa, Miriam Taouk, Peter F. Lovibond, and Roy E. Laube. 2016. Psychometric Properties 1 Psychometric Properties of a Chinese Version of the 21-Item Depression Anxiety Stress Scales (DASS 21). Sydney: Transcultural Mental Health Centre, Cumberland Hospital. [Google Scholar]
- Newman, Kristine, Angel He Wang, Arthur Ze Yu Wang, and Dalia Hanna. 2019. The role of internet-based digital tools in reducing social isolation and addressing support needs among informal caregivers: A scoping review. BMC Public Health 19: 1–12. [Google Scholar] [CrossRef]
- Oh, Hyunsung, and Soo Kyung Park. 2020. Gender and stress-buffering of social capital toward depression among precarious workers in South Korea. Work 66: 53–62. [Google Scholar] [CrossRef]
- Ong, Anthony D., Cindy S. Bergeman, Toni L. Bisconti, and Kimberly A. Wallace. 2006. Psychological resilience, positive emotions, and successful adaptation to stress in later life. Journal of Personality and Social Psychology 91: 730. [Google Scholar] [CrossRef]
- Palacio G, Carolina, Alicia Krikorian, María José Gómez-Romero, and Joaquín T. Limonero. 2020. Resilience in caregivers: A systematic review. American Journal of Hospice and Palliative Medicine 37: 648–58. [Google Scholar] [CrossRef]
- Panter-Brick, Catherine, and James F. Leckman. 2013. Editorial commentary: Resilience in child development–interconnected pathways to well-being. Journal of Child Psychology and Psychiatry 54: 333–36. [Google Scholar] [CrossRef]
- Papastavrou, Evridiki, Panayiota Andreou, Nicos Middleton, Haritini Tsangari, and Savvas Papacostas. 2015. Dementia caregiver burden association with community participation aspect of social capital. Journal of Advanced Nursing 71: 2898–910. [Google Scholar] [CrossRef]
- Penning, Margaret J., and Zheng Wu. 2016. Caregiver stress and mental health: Impact of caregiving relationship and gender. The Gerontologist 56: 1102–13. [Google Scholar] [CrossRef]
- Poortinga, Wouter. 2006. Social relations or social capital? Individual and community health effects of bonding social capital. Social Science & Medicine 63: 255–70. [Google Scholar] [CrossRef]
- Putnam, Robert D. 2000. Bowling Alone: The Collapse and Revival of American Community. New York: Simon and Schuster. [Google Scholar]
- Que, Jianyu, Lin Lu, and Le Shi. 2019. Development and challenges of mental health in China. General Psychiatry 32: 1–4. [Google Scholar] [CrossRef]
- Richardson, Jane C., and Carolyn A. Chew-Graham. 2016. Resilience and well-being. In Mental Health and Older People: A Guide for Primary Care Practitioners. Cham: Springer, pp. 9–17. [Google Scholar]
- Roberts, Emily, and Kristopher M. Struckmeyer. 2018. The impact of respite programming on caregiver resilience in dementia care: A qualitative examination of family caregiver perspectives. INQUIRY: The Journal of Health Care Organization, Provision, and Financing 55: 0046958017751507. [Google Scholar] [CrossRef]
- Rogers, Shannon H., and Patricia M. Jarema. 2015. A brief history of social capital research. In Social Capital at the Community Level: An Applied Interdisciplinary Perspective. Edited by John M. Halstead and Steven C. Deller. London: Routledge, pp. 14–30. [Google Scholar]
- Rosenberg, John P., Debbie Horsfall, Rosemary Leonard, and Kerrie Noonan. 2015. Informal caring networks for people at end of life: Building social capital in Australian communities. Health Sociology Review 24: 29–37. [Google Scholar] [CrossRef]
- Roth, Adam R. 2020. Informal caregiving and social capital: A social network perspective. Research on Aging 42: 272–80. [Google Scholar] [CrossRef]
- Roxas, Hernan Banjo, and Fara Azmat. 2014. Community social capital and entrepreneurship: Analyzing the links. Community Development 45: 135–50. [Google Scholar] [CrossRef]
- Rutter, Michael. 1985. Resilience in the face of adversity: Protective factors and resistance to psychiatric disorder. The British Journal of Psychiatry 147: 598–611. [Google Scholar] [CrossRef]
- Salehi, Asiyeh, Carolyn Ehrlich, Elizabeth Kendall, and Adem Sav. 2019. Bonding and bridging social capital in the recovery of severe mental illness: A synthesis of qualitative research. Journal of Mental Health 28: 331–39. [Google Scholar] [CrossRef]
- Salehi, Asiyeh, Neil Harris, Elisabeth Coyne, and Bernadette Sebar. 2014. Trust and quality of life: A cross-sectional study of young women. International Journal of Social Psychiatry 61: 506–14. [Google Scholar] [CrossRef]
- Santini, Ziggi Ivan, Ai Koyanagi, Stefanos Tyrovolas, Catherine Mason, and Josep Maria Haro. 2015. The association between social relationships and depression: A systematic review. Journal of Affective Disorders 175: 53–65. [Google Scholar] [CrossRef]
- Sartorius, Norman. 2003. Social capital and mental health. Current Opinion in Psychiatry 16: S101–5. [Google Scholar] [CrossRef]
- Smith, Bruce W., Jeanne Dalen, Kathryn Wiggins, Erin Tooley, Paulette Christopher, and Jennifer Bernard. 2008. The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine 15: 194–200. [Google Scholar] [CrossRef]
- Southwick, S. M., L. Sippel, J. Krystal, D. Charney, L. Mayes, and R. Pietrzak. 2016. Why are some individuals more resilient than others: The role of social support. World Psychiatry 15: 77. [Google Scholar] [CrossRef]
- Su, Irene J., Hao Liu, Ai Li, and Jing-Fang Chen. 2021. Investigation into the psychological resilience of family caregivers burdened with in-home treatment of patients with bipolar disorder. Journal of Affective Disorders Reports 3: 100059. [Google Scholar] [CrossRef]
- Sun, Qian, and Nan Lu. 2020. Social capital and mental health among older adults living in urban China in the context of COVID-19 pandemic. International Journal of Environmental Research and Public Health 17: 7947. [Google Scholar] [CrossRef]
- Süss, Hannah, and Ulrike Ehlert. 2020. Psychological resilience during the perimenopause. Maturitas 131: 48–56. [Google Scholar] [CrossRef]
- Teahan, Áine, Attracta Lafferty, Eilish McAuliffe, Amanda Phelan, Liam O’Sullivan, Diarmuid O’Shea, and Gerard Fealy. 2018. Resilience in family caregiving for people with dementia: A systematic review. International Journal of Geriatric Psychiatry 33: 1582–95. [Google Scholar] [CrossRef]
- Toledano-Toledano, Filiberto, David Luna, José Moral de la Rubia, Silvia Martínez Valverde, Carlos Alberto Bermúdez Morón, Marcela Salazar García, and Mario José Vasquez Pauca. 2021. Psychosocial factors predicting resilience in family caregivers of children with cancer: A cross-sectional study. International Journal of Environmental Research and Public Health 18: 748. [Google Scholar] [CrossRef]
- Toledano-Toledano, Filiberto, José Moral de la Rubia, Yunier Broche-Pérez, Miriam Teresa Domínguez-Guedea, and Víctor Granados-García. 2019. The measurement scale of resilience among family caregivers of children with cancer: A psychometric evaluation. BMC Public Health 19: 1–14. [Google Scholar] [CrossRef] [PubMed]
- Tong, Huijuan, Feng Qiu, and Ling Fan. 2022. Characterising common challenges faced by parental caregivers of children with type 1 diabetes mellitus in mainland China: A qualitative study. BMJ Open 12: 1–9. [Google Scholar] [CrossRef] [PubMed]
- Trail, Thomas, Esther Friedman, Carolyn M. Rutter, and Terri Tanielian. 2020. The relationship between engagement in online support groups and social isolation among military caregivers: Longitudinal questionnaire study. Journal of Medical Internet Research 22: e16423. [Google Scholar] [CrossRef]
- Villalonga-Olives, E., T. R. Wind, and I. Kawachi. 2017. The dark side of social capital: A systematic review of the negative health effects of social capital. Social Science & Medicine 194: 105–27. [Google Scholar] [CrossRef]
- Vinkers, Christiaan H., Marian Joëls, Yuri Milaneschi, René S. Kahn, Brenda W. J. H. Penninx, and Marco P. M. Boks. 2014. Stress exposure across the life span cumulatively increases depression risk and is moderated by neuroticism. Depression and Anxiety 31: 737–45. [Google Scholar] [CrossRef]
- Wang, Peigang, Xinguang Chen, Jie Gong, and Angela J. Jacques-Tiura. 2014. Reliability and validity of the personal social capital scale 16 and personal social capital scale 8: Two short instruments for survey studies. Social Indicators Research 119: 1133–48. [Google Scholar] [CrossRef]
- Wei, Wenjing, Rongrong Yang, Jie Zhang, Haili Chen, Jinghua Ye, Qiru Su, Jianxiang Liao, and Zhitian Xiao. 2022. The mediating roles of family resilience and social support in the relationship between illness severity and depressive symptoms among primary caregivers of children with epilepsy in China. Frontiers in Neurology 13: 831899. [Google Scholar] [CrossRef]
- Wind, Tim R., and Ivan H. Komproe. 2012. The mechanisms that associate community social capital with post-disaster mental health: A multilevel model. Social Science and Medicine 75: 1715–20. [Google Scholar] [CrossRef]
- Windle, Gill. 2011. What is resilience? A review and concept analysis. Reviews in Clinical Gerontology 21: 152–69. [Google Scholar] [CrossRef]
- Wu, Qiaobing, Bill Tsang, and Holly Ming. 2012. Contributions of family and neighbourhood factors to the mental health of migrant children in China: Implications for policy and services. International Journal of Adolescence and Youth 17: 113–29. [Google Scholar] [CrossRef]
- Wu, Qiaobing, Bill Tsang, and Holly Ming. 2014. Social capital, family support, resilience and educational outcomes of Chinese migrant children. British Journal of Social Work 44: 636–56. [Google Scholar] [CrossRef]
- Wu, Qiaobing, Deping Lu, and Mi Kang. 2015. Social capital and the mental health of children in rural China with different experiences of parental migration. Social Science & Medicine 132: 270–77. [Google Scholar] [CrossRef]
- Xu, Ling, Yiwei Liu, Hui He, Noelle L. Fields, Dorothea L. Ivey, and Chen Kan. 2021. Caregiving intensity and caregiver burden among caregivers of people with dementia: The moderating roles of social support. Archives of Gerontology and Geriatrics 94: 104334. [Google Scholar] [CrossRef]
- Ye, Zeng Jie, Hong Zhong Qiu, Peng Fei Li, Peng Chen, Mu Zi Liang, Mei Ling Liu, Yuan Liang Yu, Shu Ni Wang, and Xiao Ming Quan. 2017. Validation and application of the Chinese version of the 10-item Connor-Davidson Resilience Scale (CD-RISC-10) among parents of children with cancer diagnosis. European Journal of Oncology Nursing 27: 36–44. [Google Scholar] [CrossRef]
- Zhong, Yaqin, Jian Wang, and Stephen Nicholas. 2020. Social support and depressive symptoms among family caregivers of older people with disabilities in four provinces of urban China: The mediating role of caregiver burden. BMC Geriatrics 20: 1–10. [Google Scholar] [CrossRef]
- Zhou, Ting, Chunli Yi, Xuxia Zhang, and Yuyin Wang. 2014. Factors impacting the mental health of the caregivers of children with asthma in China: Effects of family socioeconomic status, symptoms control, proneness to shame, and family functioning. Family Process 53: 717–30. [Google Scholar] [CrossRef]
- Zhou, Ting, Yiting Wang, and Chunli Yi. 2018. Affiliate stigma and depression in caregivers of children with Autism Spectrum Disorders in China: Effects of self-esteem, shame and family functioning. Psychiatry Research 264: 260–65. [Google Scholar] [CrossRef]
- Zimmerman, Marc A., Sarah A. Stoddard, Andria B. Eisman, Cleopatra H. Caldwell, Sophie M. Aiyer, and Alison Miller. 2013. Adolescent resilience: Promotive factors that inform prevention. Child Development Perspectives 7: 215–20. [Google Scholar] [CrossRef]


| N (Mean) | % (SD) | |
|---|---|---|
| Age | 37.68 | 5.5 |
| Gender | ||
| Father | 128 | 38.7 |
| Mother | 203 | 61.3 |
| Marital status | ||
| Married | 318 | 96.1 |
| Divorce | 13 | 3.9 |
| Educational level | ||
| Junior Secondary | 15 | 4.5 |
| Senior Secondary | 95 | 28.7 |
| Tertiary Education (Non-degree/Sub-degree) | 118 | 35.6 |
| Tertiary Education (Bachelor’s degree) | 95 | 28.7 |
| Tertiary Education (Postgraduate degree) | 8 | 2.4 |
| Personal income (RMB) | ||
| ≤3000 | 9 | 2.7 |
| 3001–5000 | 121 | 36.6 |
| 5001–10,000 | 170 | 51.4 |
| >10,000 | 31 | 9.4 |
| Employment status | ||
| Employed | 317 | 95.8 |
| Unemployed | 14 | 4.2 |
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Bonding | 1 | |||||
| 2. Bridging | 0.659 ** | 1 | ||||
| 3. Resilience | 0.325 ** | 0.208 ** | 1 | |||
| 4. Stress | 0.009 | 0.191 ** | −0.548 ** | 1 | ||
| 5. Anxiety | 0.021 | 0.181 ** | −0.489 ** | 0.876 ** | 1 | |
| 6. Depression | 0.034 | 0.208 ** | −0.497 ** | 0.857 ** | 0.912 ** | 1 |
| Stress | Anxiety | Depression | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |||||||
| β | p | β | p | β | p | β | p | β | p | β | p | |
| Gender | 0.121 | 0.019 | 0.04 | 0.339 | 0.101 | 0.047 | 0.031 | 0.485 | 0.11 | 0.029 | 0.039 | 0.360 |
| Age | 0.259 | 0.000 *** | 0.129 | 0.003 ** | 0.301 | 0.000 *** | 0.186 | 0.000 *** | 0.291 | 0.000 *** | 0.171 | 0.000 *** |
| Marital status | −0.08 | 0.090 | −0.04 | 0.354 | −0.08 | 0.123 | −0.04 | 0.409 | −0.05 | 0.259 | −0.010 | 0.802 |
| Educational level | −0.2 | 0.000 *** | −0.05 | 0.247 | −0.17 | 0.000 *** | −0.05 | 0.321 | −0.18 | 0.000 *** | −0.046 | 0.291 |
| Personal income | 0.107 | 0.037 | 0.117 | 0.005 ** | 0.118 | 0.020 * | 0.127 | 0.004 * | 0.187 | 0.000 *** | 0.197 | 0.000 *** |
| Employment status | 0.009 | 0.848 | 0.042 | 0.289 | −0.01 | 0.919 | 0.024 | 0.557 | −0.03 | 0.523 | 0.000 | 0.995 |
| Bonding | −0.02 | 0.688 | −0.02 | 0.716 | −0.043 | 0.459 | ||||||
| Bridging | 0.321 | 0.000 *** | 0.291 | 0.000 *** | 0.328 | 0.000 *** | ||||||
| Psychological Resilience | −0.57 | 0.000 *** | −0.5 | 0.000 *** | −0.514 | 0.000 *** | ||||||
| R2 | 0.132 | 0.439 | 0.149 | 0.389 | 0.167 | 0.429 | ||||||
| F for R2 change | 9.46 *** | 67.326 *** | 10.898 *** | 48.353 *** | 12.469 *** | 56.512 *** | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feng, J.; Cai, P.; Guan, X.; Li, X.; He, L.; Fung, K.-k.; Mai, Z. The Mediating Effect of Psychological Resilience between Individual Social Capital and Mental Health in the Post-Pandemic Era: A Cross-Sectional Survey over 300 Family Caregivers of Kindergarten Children in Mainland China. Soc. Sci. 2024, 13, 122. https://doi.org/10.3390/socsci13020122
Feng J, Cai P, Guan X, Li X, He L, Fung K-k, Mai Z. The Mediating Effect of Psychological Resilience between Individual Social Capital and Mental Health in the Post-Pandemic Era: A Cross-Sectional Survey over 300 Family Caregivers of Kindergarten Children in Mainland China. Social Sciences. 2024; 13(2):122. https://doi.org/10.3390/socsci13020122
Chicago/Turabian StyleFeng, Juxiong, Pengpeng Cai, Xin Guan, Xuhong Li, Langjie He, Kwok-kin Fung, and Zheyuan Mai. 2024. "The Mediating Effect of Psychological Resilience between Individual Social Capital and Mental Health in the Post-Pandemic Era: A Cross-Sectional Survey over 300 Family Caregivers of Kindergarten Children in Mainland China" Social Sciences 13, no. 2: 122. https://doi.org/10.3390/socsci13020122
APA StyleFeng, J., Cai, P., Guan, X., Li, X., He, L., Fung, K.-k., & Mai, Z. (2024). The Mediating Effect of Psychological Resilience between Individual Social Capital and Mental Health in the Post-Pandemic Era: A Cross-Sectional Survey over 300 Family Caregivers of Kindergarten Children in Mainland China. Social Sciences, 13(2), 122. https://doi.org/10.3390/socsci13020122







