The Role of Risk Communication in Shaping Health-Protective Behavior Amid the COVID-19 Pandemic in Thailand
Abstract
:1. Introduction
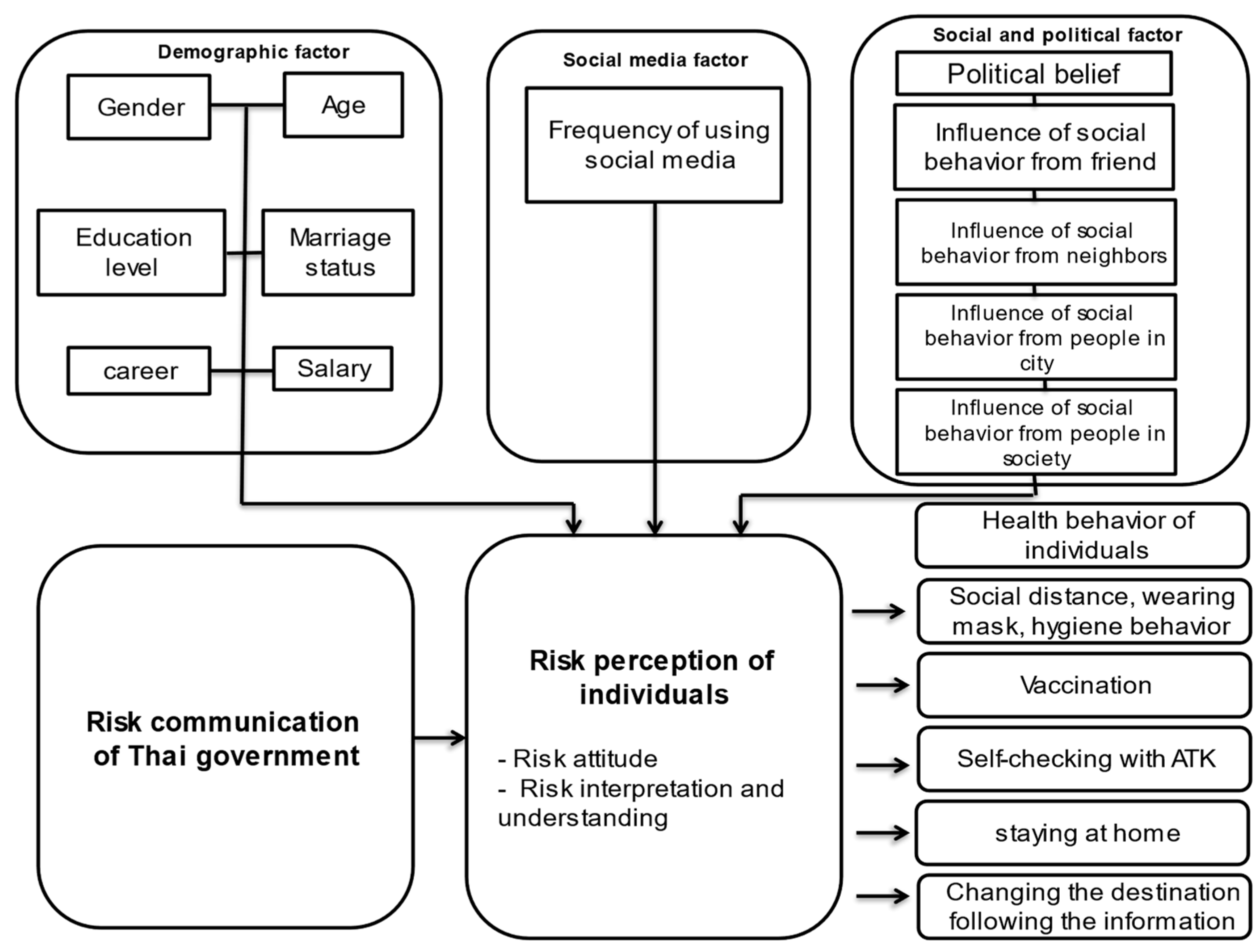
2. Theoretical Background
| Variables | Definition of Variables |
|---|---|
| Risk communication process of the Thai government | Sender of risk communication who represents the source of information. |
| Demographic variables | These are the independent variables in this research. |
| Social media variables and social and political variables | Modifying factor for analyzing environmental factors to represent a cue for action that can influence an individual’s perception of risk and their behavior. These are independent variables in this research. |
| Individual perception of risk | Perception is related to the knowledge and belief of an individual and can lead to healthy behavior. It is represented by independent and dependent variables in this research. |
| Healthy behavior of individuals | The likelihood of an action is the result of an individual’s risk perception and the risk communication process. This is a dependent variable in this research. |
3. Materials and Methods
3.1. Questionnaire
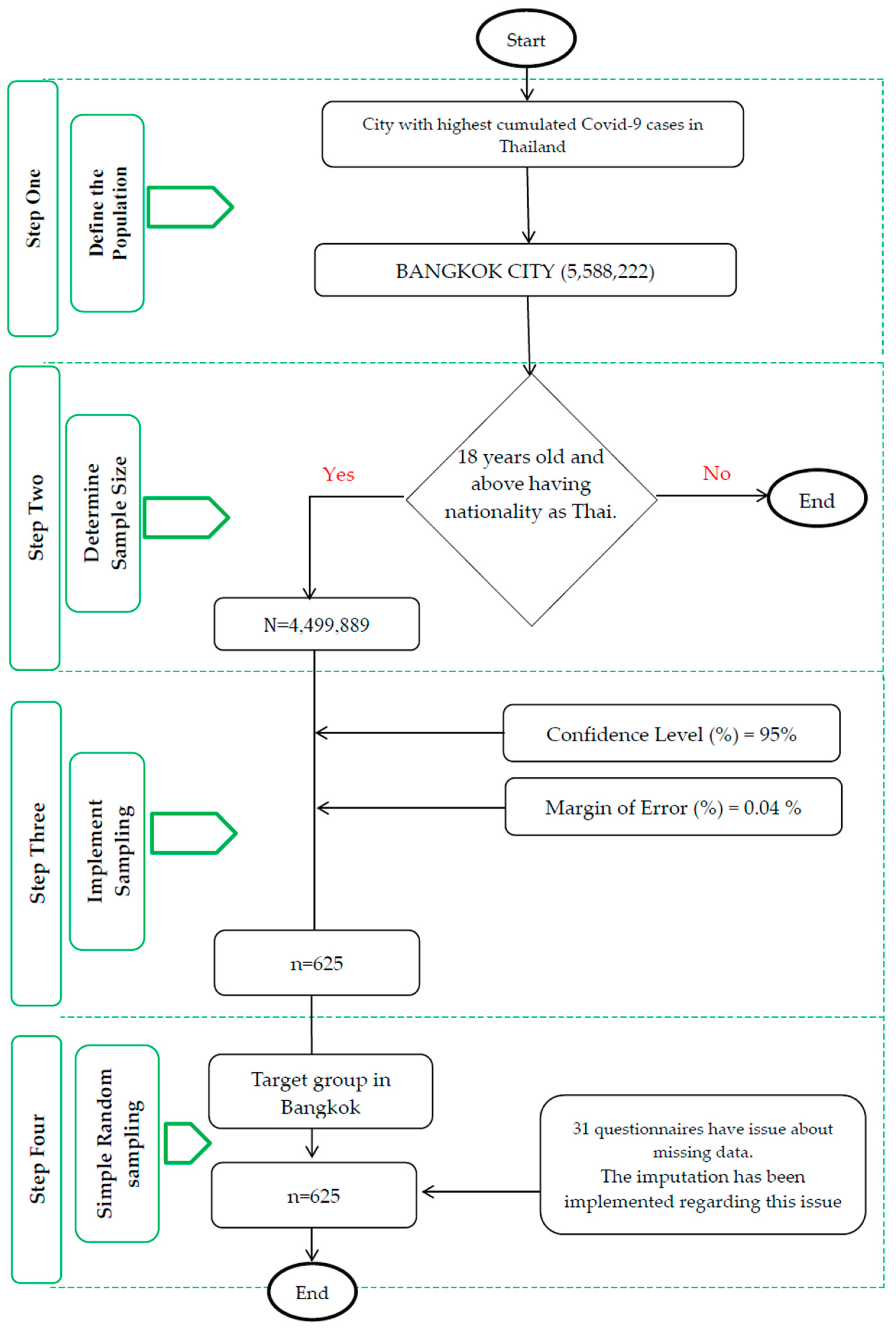
3.2. Data Sampling
3.3. Data Analysis
4. Results
4.1. Descriptive Results
4.2. The Distributions of the Measures Used in This Study
4.2.1. Demographic Factors
4.2.2. Social Media Factor
4.2.3. Social and Cultural Factors
4.2.4. Health-Protective Behavior of Individuals
5. Discussion
6. Study Limitation
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abraham, Charles, and Paschal Sheeran. 2015. The health belief model. In Predicting and Changing Health Behaviour: Research and Practice with Social Cognition Models. Edited by Mark Conner and Paul Norman. New York: McGraw-Hill Education (UK), pp. 30–69. [Google Scholar]
- Arslanca, Tufan, Cihan Fidan, Mine Daggez, and Polat Dursun. 2021. Knowledge, preventive behaviors and risk perception of the COVID-19 pandemic: A cross-sectional study in Turkish health care workers. PLoS ONE 16: e0250017. [Google Scholar] [CrossRef] [PubMed]
- Barriors, John, and Yael Hochberg. 2020. Risk Perception Through the Lens of Politics in the Time of the COVID-19 Pandemic. Chicago: Becker Friedman Institute. [Google Scholar]
- Becker, Marshall, and Irwin Rosenstock. 1984. Compliance with medical advice. In Health Care and Human Behavior. Edited by A. Steptoe and A. Matthews. London: Academic Press, pp. 135–52. [Google Scholar]
- Berg, Siv Hilde, Jane K. O’hara, Marie Therese Shortt, Henriette Thune, Kolbjørn Kallesten Brønnick, Daniel Adrian Lungu, Jo Røislien, and Siri Wiig. 2021. Health authorities’ health risk communication with the public during pandemics: A rapid scoping review. BMC Public Health 21: 1–23. [Google Scholar] [CrossRef]
- Bier, Vicki. 2001. On the state of the art: Risk communication to the public. Reliability Engineering & System Safety 71: 139–50. [Google Scholar] [CrossRef]
- Choi, Doo-Hun, Woohyun Yoo, Ghee-Young Noh, and Keeho Park. 2017. The impact of social media on risk perceptions during the MERS outbreak in South Korea. Computers in Human Behavior 72: 422–31. [Google Scholar] [CrossRef]
- Farrag, Nesrine Saad, and Abdel-Hady El-Gilany. 2021. Risk communication in COVID-19 pandemic: A note for health-care workers. International Journal of Health & Allied Sciences 10: 227. [Google Scholar] [CrossRef]
- Frewer, Lynn. 2004. The public and effective risk communication. Toxicology Letters 1–3: 391–97. [Google Scholar] [CrossRef] [PubMed]
- González-Padilla, Daniel, and Leonardo Tortolero-Blanco. 2020. Social media influence in the COVID-19 Pandemic. International Brazilian Journal of Urology 46: 120–24. [Google Scholar] [CrossRef]
- Heydari, Seyed Taghi, Leila Zarei, Ahmad Kalateh Sadati, Najmeh Moradi, Maryam Akbari, Gholamhossin Mehralian, and Kamran Bagheri Lankarani. 2021. The effect of risk communication on preventive and protective behaviours during the COVID-19 outbreak: Mediating role of risk perception. BMC Public Health 21: 1–11. [Google Scholar] [CrossRef]
- Hooker, Claire, Adam Capon, and Julie Leask. 2017. Communicating about risk: Strategies for situations where public concern is high, but the risk is low. Public Health Research & Practice 27: e2711709. [Google Scholar] [CrossRef]
- McComas, Katherine. 2006. Defining Moments in Risk Communication Research: 1996–2005. Journal of Health Communication 11: 75–91. [Google Scholar] [CrossRef]
- Ministry of Public Health. 2021. Strategic Plan: COVID-19. January. Available online: https://ddc.moph.go.th/viralpneumonia/eng/file/main/en_Thailand%20Covid-19%20plan_MOPH_2021.pdf (accessed on 25 June 2023).
- Mullainathan, Sendhil, and Andrei Shleifer. 2005. The Market for News. American Economic Review 95: 1031–53. [Google Scholar] [CrossRef]
- Namwat, Chawetsan, Rapeepong Suphanchaimat, Natthaprang Nittayasoot, and Sopon Iamsirithaworn. 2020. Thailand’s response against Coronavirus disease 2019: Challenges and lessons learned. Outbreak, Surveillance, Investigation & Response (OSIR) Journal 13: 33–37. [Google Scholar] [CrossRef]
- Office of Risk Communication and Health Behavior Development, Ministry of Public Health. 2020. Diseases and Health Hazards in Crisis (Crisis Risk Communication). Bangkok: Department of Disease Control, Ministry of Public Health. [Google Scholar]
- Osterrieder, Anne, Giulia Cuman, Wirichada Pan-Ngum, Phaik Kin Cheah, Phee-Kheng Cheah, Pimnara Peerawaranun, Margherita Silan, Miha Orazem, Ksenija Perkovic, Urh Groselj, and et al. 2021. Economic and social impacts of COVID-19 and public health measures: Results from an anonymous online survey in Thailand, Malaysia, the UK, Italy and Slovenia. BMJ Open 11: e046863. [Google Scholar] [CrossRef]
- Ounsaneha, Weerawat, Orapin Laosee, Thunwadee Tachapattaworakul Suksaroj, and Cheerawit Rattanapan. 2023. Preventive Behaviors and Influencing Factors among Thai Residents in Endemic Areas during the Highest Epidemic Peak of the COVID-19 Outbreak. International Journal of Environmental Research and Public Health 20: 2525. [Google Scholar] [CrossRef] [PubMed]
- Passa, L. 2021. Three sets of questions projecting Thai government response to the emerging COVID-19 pandemic through mass media communications. PSDS Journal of Development Studies 4: 98–131. [Google Scholar]
- Radwan, Ahmed Farouk, and Sheren Ali Mousa. 2021. Government Communication Strategies during Coronavirus Pandemic: United Arab Emirates Lessons. Journal of Health Management 22: 516–27. [Google Scholar] [CrossRef]
- Rattay, Petra, Niels Michalski, Olga Maria Domanska, Anna Kaltwasser, Freia De Bock, Lothar H. Wieler, and Susanne Jordan. 2021. Differences in risk perception, knowledge and protective behaviour regarding COVID-19 by education level among women and men in Germany. Results from the COVID-19 Snapshot Monitoring (COSMO) study. PLoS ONE 16: e0251694. [Google Scholar] [CrossRef] [PubMed]
- Renn, Ortwin. 2008. Risk Communication: Insights and Requirements for Designing Successful Communication Programs on Health and Environmental Hazards, in Risk and Crisis Communication. London: Routledge, Boca Raton: CRC Press, Abingdon: Taylor & Francis Group, pp. 81–99. [Google Scholar]
- Reyna, Valerie F., Wendy L. Nelson, Paul K. Han, and Nathan F. Dieckmann. 2009. How numeracy influences risk comprehension and medical decision making. Psychological Bulletin 135: 943–73. [Google Scholar] [CrossRef]
- Rezaei, Mansour, Nader Rajabi Gilan, Ali Almasi, Mehdi Khezeli, Fatemeh Jamshidi Nazar, Zahra Jorjoran Shushtari, Yahya Salimi, Farid Najafi, Neda Sarabi, Shahram Saeidi, and et al. 2022. The role of risk perception, risk communication, and demographic factors in COVID-19 preventive behaviors: An online survey in Iran. Osong Public Health and Research Perspectives 13: 282–89. [Google Scholar] [CrossRef]
- Rogers, Brooke, and Julia Pearce. 2013. Risk communication, risk perception and behavior as foundations of effective national security practices. In Strategic Intelligence Management. Oxford: Butterworth-Heinemann, pp. 66–74. [Google Scholar]
- Ropeik, David, and Paul Slovic. 2003. Risk communication: A neglected tool in protecting public health. Risk in Perspective 2: 1–4. [Google Scholar]
- Savadori, Lucia, and Marco Lauriola. 2021. Risk Perception and Protective Behaviors During the Rise of the COVID-19 Outbreak in Italy. Frontiers in Psychology 11: 577331. [Google Scholar] [CrossRef]
- Schneider, Claudia R., Sarah Dryhurst, John Kerr, Alexandra LJ Freeman, Gabriel Recchia, David Spiegelhalter, and Sander van der Linden. 2021. COVID-19 risk perception: A longitudinal analysis of its predictors and associations with health protective behaviours in the United Kingdom. Journal of Risk Research 24: 294–313. [Google Scholar] [CrossRef]
- Sirilak, Supakit. 2020. COVID-19 Infodemic management: Thailand experience. Paper Presented at 75th Session of the General Assembly of the United Nations. Available online: https://www.who.int/docs/default-source/coronaviruse/risk-comms-updates/thailand-unga-presentation-infodemic-thailand-21sep2020-final.pdf?sfvrsn=d757509e_6 (accessed on 22 July 2023).
- Sund, Björn, Mikael Svensson, and Henrik Andersson. 2017. Demographic determinants of incident experience and risk perception: Do high-risk groups accurately perceive themselves as high-risk? Journal of Risk Research 20: 99–117. [Google Scholar] [CrossRef]
- The Cabinet of the Royal Thai Government. 2016. Thailand National Strategic Plan for Emerging Infectious Diseases 2017–2021. December 7. Available online: https://ddc.moph.go.th/uploads/ckeditor2//eidnationplan20172022_en_270660.pdf (accessed on 20 June 2023).
- Thummapol, Onouma, Sanitnarathorn Pannawit, Thongma Sichon, Srithumsuk Werayuth, and Tunthanongsakkul Donlaporn. 2021. What influences thai community-dwelling older adults to undertake health protective behaviors in the time of covid-19 pandemic? a structural equation modeling analysis. Naresuan University Journal 30: 87–98. [Google Scholar]
- Tsoy, Diana, Tanin Tirasawasdichai, and Konstantin Ivanovich Kurpayanidi. 2021. Role of Social Media in Shaping Public Risk Perception during COVID-19 Pandemic: A Theoretical Review. International Journal of Management Science and Business Administration 7: 35–41. [Google Scholar] [CrossRef]
- Tuler, Seth, Uma Langkulsen, Caron Chess, and Nuntavarn Vichit-Vadakan. 2012. Health, and environmental risk communication in Thailand: An analysis of agency staff’s perspectives on risk communication with external stakeholders. Austrian Journal of South-East Asian Studies 5: 52–73. [Google Scholar]
- Wahlberg, Anders A. F., and Lennart Sjoberg. 2000. Risk perception and the media. Journal of Risk Research 3: 31–55. [Google Scholar] [CrossRef]
- Zeballos Rivas, Diana Reyna, Marinalda Lidia Lopez Jaldin, Blanca Nina Canaviri, Luisa Fabiola Portugal Escalante, Angela M. C. Alanes Fernández, and Juan Pablo Aguilar Ticona. 2021. Social media exposure, risk perception, preventive behaviors and attitudes during the COVID-19 epidemic in La Paz, Bolivia: A cross sectional study. Plosone 16: e0245859. [Google Scholar] [CrossRef]
| Factor | N | Percent |
|---|---|---|
| Gender | ||
| 285 | 45.6 |
| 340 | 54.4 |
| Age | ||
| 201 | 32.2 |
| 111 | 17.8 |
| 94 | 15.0 |
| 104 | 16.6 |
| 115 | 18.4 |
| Education level | ||
| 21 | 3.4 |
| 80 | 12.8 |
| 423 | 67.7 |
| 101 | 16.2 |
| Occupation | ||
| 64 | 10.2 |
| 86 | 13.8 |
| 86 | 13.8 |
| 338 | 54.1 |
| 23 | 3.7 |
| 1 | 0.2 |
| 27 | 4.3 |
| Marital status | ||
| 379 | 60.6 |
| 20 | 3.2 |
| 162 | 25.9 |
| 24 | 3.8 |
| 30 | 4.8 |
| 10 | 1.6 |
| Salary level | ||
| 70 | 11.2 |
| 217 | 34.7 |
| 233 | 37.3 |
| 95 | 15.2 |
| 10 | 1.6 |
| Topic | Detail | Study Distribution | ||||||
|---|---|---|---|---|---|---|---|---|
| Strongly Disagree | Disagree | Medium | Agree | Strongly Agree | Mean | Median | ||
| Attitude about risk communication | Risk communication about hygiene | 30 (4.8%) | 10 (1.6%) | 228 (36.5%) | 296 (47.4%) | 61 (9.8%) | 3.56 | 4 |
| Risk communication about social distancing | 26 (4.2%) | 74 (11.8%) | 264 (42.2%) | 220 (35.2%) | 41 (6.6%) | 3.28 | 3 | |
| Risk communication about staying at home | 86 (13.8%) | 110 (17.6%) | 268 (42.9%) | 140 (22.4%) | 21 (3.4%) | 2.84 | 3 | |
| Risk communication about vaccination | 91 (14.6%) | 95 (15.2%) | 338 (54.1%) | 100 (16%) | 1 (0.2%) | 2.72 | 3 | |
| Risk communication about the daily number of COVID-19 patients | 96 (15.4%) | 119 (19%) | 299 (47.8%) | 100 (16%) | 11 (1.8%) | 2.70 | 3 | |
| Health-protective behavior | Wearing a mask, social distancing, and hygienic behavior | - | - | 91 (14.6%) | 330 (52.8%) | 204 (32.6%) | 4.18 | 4 |
| Staying at home | - | 10 (1.6%) | 126 (20.2%) | 353 (56.5%) | 136 (21.8%) | 3.98 | 4 | |
| Changing the destination according to the information | - | 30 (4.8%) | 136 (21.8%) | 332 (53.1%) | 127 (20.3%) | 3.89 | 4 | |
| Self-checking with ATK | 20 (3.2%) | 20 (3.2%) | 158 (25.3%) | 305 (48.8%) | 122 (19.5%) | 3.78 | 4 | |
| Vaccination | 47 (7.5%) | 74 (11.8%) | 111 (17.8%) | 276 (44.2%) | 117 (18.7%) | 3.55 | 4 | |
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p-Value | df | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Regression | Residual | |||
| (Constant) | 2.093 | 0.119 | 17.655 | 0.000 | 6 | 619 | |
| Gender | −0.098 | 0.029 | −0.127 | −3.311 | 0.001 | ||
| Age | −0.005 | 0.012 | −0.020 | −0.409 | 0.683 | ||
| Salary level | −0.055 | 0.018 | −0.133 | −2.963 | 0.003 | ||
| Occupation | −0.144 | 0.054 | −0.114 | −2.675 | 0.008 | ||
| Marital status | −0.030 | 0.039 | −0.039 | −0.780 | 0.436 | ||
| Education level | −0.147 | 0.024 | −0.251 | −6.258 | 0.000 | ||
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p-Value | df | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Regression | Residual | |||
| (Constant) | 1.319 | 0.053 | 24.806 | 0.000 | 1 | 624 | |
| Exposing to social media | −0.058 | 0.021 | −0.111 | −2.781 | 0.006 | ||
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p-Value | df | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Regression | Residual | |||
| (Constant) | 1.681 | 0.064 | 26.288 | 0.000 | 1 | 624 | |
| Exposing to social media | −0.145 | 0.025 | −0.226 | −5.799 | 0.000 | ||
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p-Value | df | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Regression | Residual | |||
| (Constant) | 1.465 | 0.070 | 20.947 | 0.000 | 1 | 624 | |
| Exposing to social media | 0.004 | 0.027 | 0.006 | 0.137 | 0.891 | ||
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p-Value | df | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Regression | Residual | |||
| (Constant) | 1.312 | 0.055 | 23.801 | 0.000 | 2 | 623 | |
| Political belief | −0.071 | 0.029 | −0.169 | −2.462 | 0.014 | ||
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p-Value | df | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Regression | Residual | |||
| (Constant) | 1.536 | 0.070 | 21.825 | 0.000 | 4 | 621 | |
| Social behavior observation (friend) | −0.083 | 0.022 | −0.210 | −3.839 | 0.000 | ||
| Social behavior observation (neighbors) | 0.087 | 0.017 | 0.239 | 4.978 | 0.000 | ||
| Social behavior observation (people in the same city) | 0.044 | 0.025 | 0.102 | 1.746 | 0.081 | ||
| Social behavior observation (people in the same society) | −0.132 | 0.022 | -0.287 | −6.095 | 0.000 | ||
| Model | Unstandardized Coefficients | Standardized Coefficients | t | p-Value | df | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Regression | Residual | |||
| Wearing a mask, social distancing, and hygienic behavior | −0.121 | 0.069 | −0.070 | −1.745 | 0.081 | 1 | 624 |
| Vaccination | 0.320 | 0.119 | 0.107 | 2.681 | 0.008 | ||
| Self-checking with ATK | 0.036 | 0.095 | 0.015 | 0.381 | 0.704 | ||
| Staying at home | −0.099 | 0.073 | −0.054 | −1.361 | 0.174 | ||
| Changing one’s destination according to the information | −0.204 | 0.081 | −0.100 | −2.518 | 0.012 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Termmee, S.; Wang, B. The Role of Risk Communication in Shaping Health-Protective Behavior Amid the COVID-19 Pandemic in Thailand. Soc. Sci. 2023, 12, 551. https://doi.org/10.3390/socsci12100551
Termmee S, Wang B. The Role of Risk Communication in Shaping Health-Protective Behavior Amid the COVID-19 Pandemic in Thailand. Social Sciences. 2023; 12(10):551. https://doi.org/10.3390/socsci12100551
Chicago/Turabian StyleTermmee, Suphunnika, and Bing Wang. 2023. "The Role of Risk Communication in Shaping Health-Protective Behavior Amid the COVID-19 Pandemic in Thailand" Social Sciences 12, no. 10: 551. https://doi.org/10.3390/socsci12100551
APA StyleTermmee, S., & Wang, B. (2023). The Role of Risk Communication in Shaping Health-Protective Behavior Amid the COVID-19 Pandemic in Thailand. Social Sciences, 12(10), 551. https://doi.org/10.3390/socsci12100551







