Shielding without a Shield—Older People under COVID-19: A Comparison of Four Cities
Abstract
:1. Introduction
“Shielding is a term used to describe the protection of individuals at high risk of severe COVID-19 illness by separating them from the general population. When considering shielding, it is important to plan for socioeconomic impacts on the shielded, including psychosocial well-being, income generation, food access, and health service access. These are trade-offs that communities and individuals must weigh against the positive effects of shielding in the broader context of COVID-19 containment measures”.
Policies must take into account the most affected and least resilient. At a national level, this entails dedicated measures to address the needs and rights of women, older people, children, low-wage earners, persons with disabilities, and vulnerable groups. At a global level, it requires a comprehensive stimulus package amounting to at least ten percent of global GDP and massive support to developing countries in the form of an across-the-board debt standstill, debt restructuring, and greater support through international financial institutions.
The COVID-19 pandemic is causing untold fear and suffering for older people across the world. The fatality rate for older people is higher overall, and for those over 80, it is five times the global average. Beyond its immediate health impact, the pandemic is putting older people at greater risk of poverty, discrimination, and isolation. It is likely to have a particularly devastating impact on older people in developing countries.
2. Literature Review
2.1. Issues of Vulnerability
2.2. Disrupted Healthcare Services
2.3. Concept of Health Welfare Regime
2.4. Social Distancing and Its Psychological Resistance
- School closure;
- Workplace closures;
- Public event cancellation;
- Public transport closure;
- Restriction on internal movement;
- International travel controls;
2.5. Fear, Anxiety, and Depression due to Social Isolation
2.6. Mediating Effects of Digital Technology on Psychological Impacts
3. Methodology
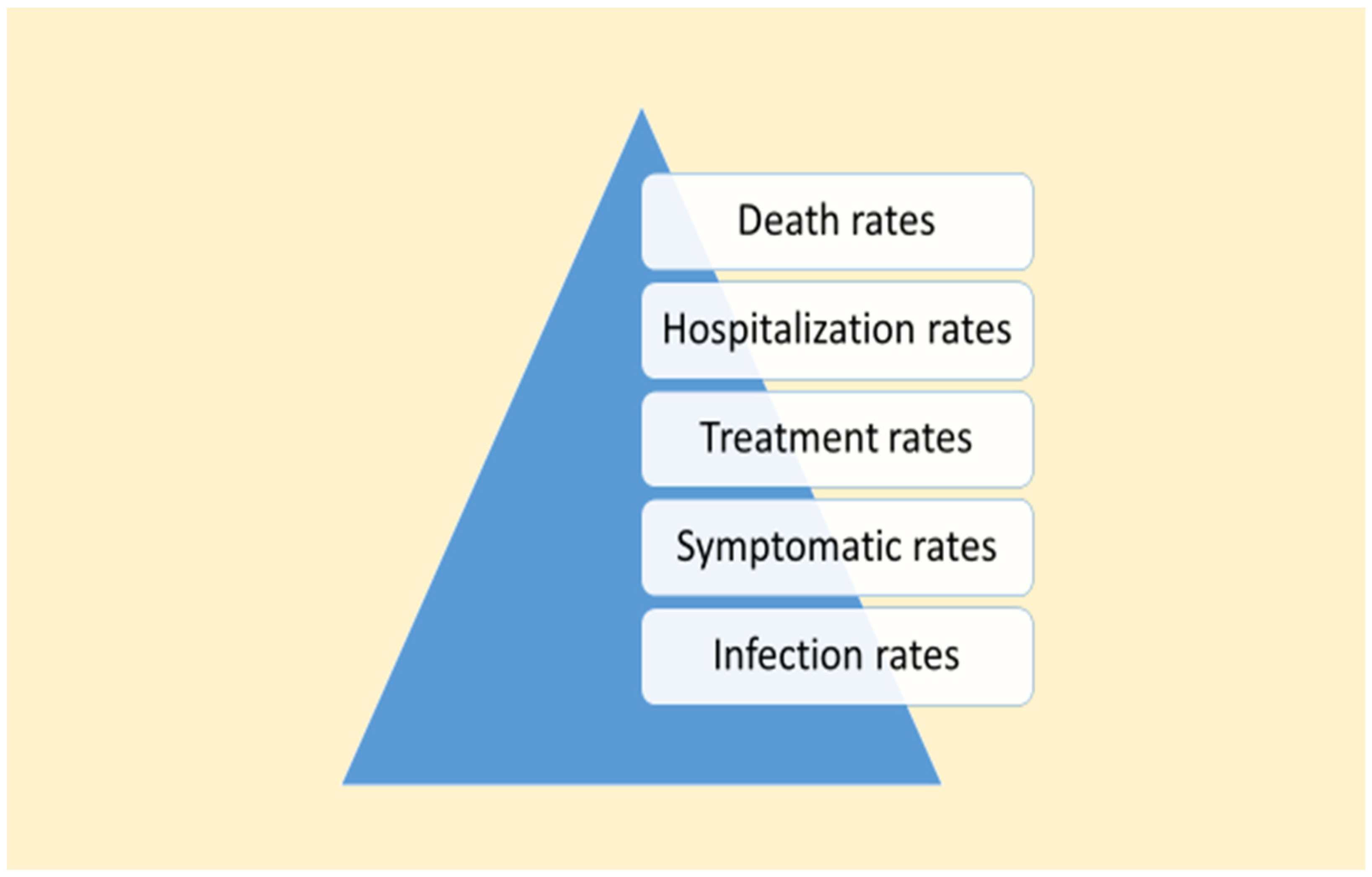
3.1. Framework of Study
3.2. Selection of Cities
3.3. Timeframe of Study
3.4. Quantitative and Qualitative Mix
4. Findings
4.1. Overall Deaths Caused by the Pandemic
4.2. China (Wuhan and Hong Kong)
4.3. Italy (Lombardy and Milan)
4.4. The United Kingdom (London)
4.5. Comparing COVID-19 Deaths
- (1)
- Although the case fatality rates of omicron were comparatively lower than its previous variants (Lorenzo-Redondo et al. 2022), the absolute number of deaths was higher in 2021 than in 2020 for Italy and the United Kingdom. The absolute number of deaths was higher in 2022 for Hong Kong and thus China, than the total in 2020 and 2021.
- (2)
- High infectivity of the omicron variant has led to a greater number of confirmed cases. This explained the higher crude death rates partially because proper vaccination and more experienced protection measures should have arguably lowered the death rate. Unfortunately, governments have not learned from the painful experiences of other cities. For example, larger death numbers were recorded in London in its second wave in 2021. A high number of deaths happening in Hong Kong as late as 2022 needs further analysis.
5. Mortality for Older People in the Four Cities
5.1. Wuhan
5.2. Milan
5.3. London
5.4. Hong Kong
5.5. Summary
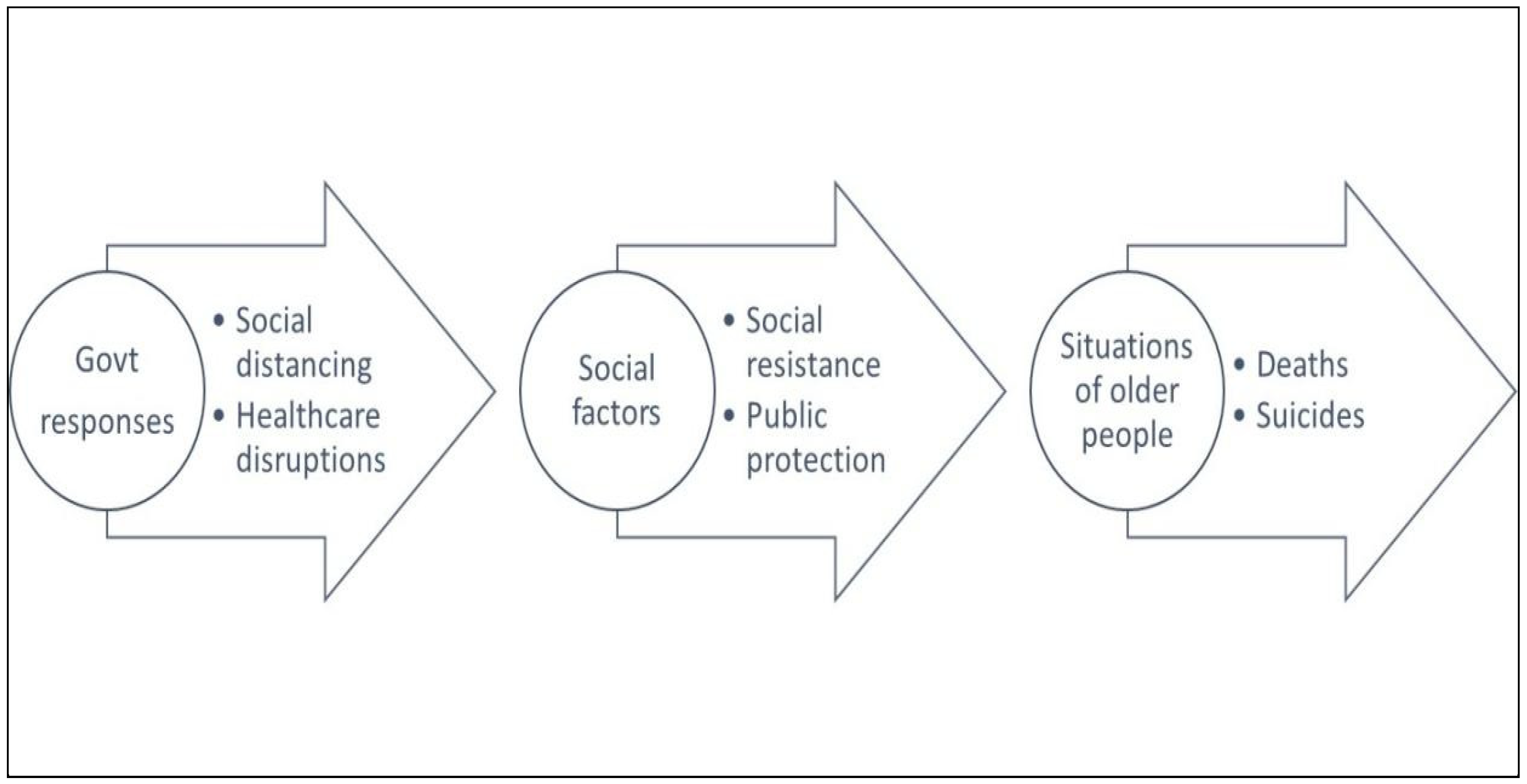
6. Government Responses and Disruptions of Essential Healthcare Services
6.1. Wuhan
6.2. Milan
6.3. London
6.4. Hong Kong
6.5. Summary
7. Psychological Impacts and Older People’s Resilience
7.1. Wuhan
- (a)
- It was a contagious disease that spread among social circles. For example, a choir, composed of mainly older singers, went for a picnic where tens of them became infected, and some of them died. In January 2020, Wuhan was celebrating the Chinese Lunar New Year, a time of family gatherings and feasts. Over dinners, COVID-19 quietly spread between family members. Normally, older people passed away due to weaker resistance, leaving behind their sons and daughters to live under long-term guilt and loss.
- (b)
- COVID-19 was a painful disease and death. It attacked the lungs of people and caused physical pain by making breathing difficult and sometimes impossible. Family members of the diseased knew well that the dying person was suffering under extreme physiological conditions.
- (c)
- COVID-19 caused sudden deaths. Family members sent their infected relatives to the hospitals and were not allowed to visit. They were not even allowed the chance to say farewell. When family members were informed of the deaths of their relatives, they could only pick up the ashes and remains of their loved ones from the Crematorium.
- (d)
- COVID-19 was a stigma-associated disease. It did not make life easier for the survivors. When they returned to the community after recovery and discharge, they were not welcome by neighbors. These reactions of the community could be described as a “sympathetic but scared” psychology. It was due to the lack of health knowledge about immunity after sickness and the fear of remained infectivity of the ex-patients.
7.2. Help Seeking, Coping, and Resilience of Older People
- (a)
- The Psychological Association of Hubei Province offered a 24-h hotline starting on 23 January 2020. Its President, Mr. Xiao J. X. remarked that older people under isolation and young people in identity formation deserved special psychological attention (Hubei Psychological Association 2020). However, in terms of age, 31% of their inquiries came from young people, 50% from middle-aged persons, and only 19% from older people. Older people were not used to seeking help from strangers and professionals.
- (b)
- Counselor Li Meng observed that at the beginning, most inquiries were about medical information. In the middle of February 2022, the tide changed. Psychological depression and pessimism began to dominate the consultations. One day she received five calls, all from older people who were living alone in Wuhan, as their sons or daughters worked in other cities. Mobility due to work among younger generations is a very common phenomenon in China. Physical “distancing” of intergeneration family members created a lot of worries, anxieties, and a sense of guilt during the epidemic.
- (c)
- Statistics showed that 50% of inquiries came from healthy populations, 30% from confirmed cases and their family members, 10% from people with mental health problems, and 5% from medical staff. The low call-in rate from medical staff who were under extreme work pressure showed that they were not used to seeking counseling help.
- (d)
- In late February, organized by the China Center for Disease Control, 300 psychological staff headed by psychiatrists from all over the country were sent to provide support to Wuhan patients and medical workers. Dr. Wang Z., a psychiatrist, talked about an old male patient who refused to be discharged because he worried that his son might reject his return to their house (qq.com 2020).
- (e)
- Dr. Wang also pointed out that people’s reactions to the coronavirus disease were different from earthquakes or fires because of its duration and scale. The communicable disease had no definite end and no boundary to whom it could kill. According to many counselors, the challenge of COVID-19 was its prolonged impact stage. It created anxiety and fear (ifeng.com 2020). It induced shame among the patients, a sense of guilt among their family members, and deep grief among the younger generations in the extended family.
- (f)
- Dr. Kong G. Y., a professor at the School of Psychology, Hua Zhong University, pointed out that “final accompaniment”, with parents or senior members of the family through the last section of life, is very important in both Chinese and western culture. Condolence is important for the expression of grief and the ventilation of sad feelings. However, it was not allowed during COVID-19. Furthermore, Dr. Kong admitted that the underlying psychological impacts of COVID-19 are beyond human knowledge because never were so many people, 10 million Wuhan residents, “locked down” for so long (from 23 January 2020, until 8 April, a total of 77 days). Some studies suggested that self-compassion is an important means to help those who struggle with shame and self-criticism that can result from a large-scale epidemic (Gilbert 2009). Positive psychology may also help. However, collective community memories will not go away easily for Wuhan.
7.3. Milan
Psychological Impacts
- (a)
- Cerami et al. (2020) started a psychosocial survey as soon as the COVID-19 outbreak hit Italy in March 2020. A total of 1163 Italian residents above 18 years of age all over Italy responded to this anonymous online survey between 14 and 21 March 2020. Among them, 99 respondents (8.5%) were aged over 65. The Italian version of the Depression and Anxiety Scale and the Italian Version of the Loneliness Scale were used. To quote the authors:
They concluded that the Italian general population may have moderate-to-severe psychological distress during the early phases of the COVID-19 emergency“In line with this evidence, baseline findings of the PsyCOVID study suggest that COVID-19 will represent a psychosocial catastrophe. On the one side, healthcare workers face the emergency not only at the physical level, as they are continuously exposed to the contagion and engaged in patient assistance and care, but they have to cope with a huge psychosocial burden. This requires healthcare professionals to put into play enormous resources to adapt themselves to the new dystopic situation, managing the increasing distress while trying to bring out the most effective coping strategy. On the other side, quarantine and other social distancing measures imposed by Italian authorities to the majority of the population can exacerbate feelings of loneliness and lack of connectedness in socially fragile individuals, as well as enhance the risk of negative mental health outcomes”.(p. 5) - (b)
- Social distancing is in large contrast to Italian culture, which has a custom in which the young often live with the old, hence exposing them to the virus (Auriemma and Iannaccone 2020). This may increase psychological resistance among older people to social distancing policy and leads to anxiety.
- (c)
- Italy is characterized by its familistic orientation in which the family plays a central role in assisting its senior members. This orientation, legitimizing the traditional definition of roles in the family, was fostered by the Catholic Church in Italian society. Although the social structure of the family in Italy was gradually transformed by the modernization of society (Blangiardo and Rimoldi 2014), the care of seniors had limited support from external caregivers and even less from public institutions (Gagliardi et al. 2022). During COVID-19 when home quarantine was imposed, it stirred up family conflicts.
- (d)
- Guida and Carpentieri (2021) researched the accessibility of public and private primary healthcare facilities in Milan, which showed that the usage of public transportation dropped significantly (See Figure 17). Using GIS to measure pedestrian flow, the research confirmed that older people who needed health services regularly were significantly affected when the city regulated its transportation and designated some primary healthcare facilities as hubs for COVID-19 cases.
- (e)
- Cesvi, an international NGO, launched an assistance program for older people over 65 in Bergamo and Milan. The project in Milan sponsored by the Cesvi was called “Veniamo Noi da Te” (We Come to You). It had a team of 15 social workers who assisted more than 200 elderly aged over 65, providing deliveries of necessities and carrying out errands, as well as psychological support through helplines for the elderly. “We meet people who tend to be alone, who don’t see anyone and are afraid”, explained Marina Malgeri, a worker on the project. “I meet about 4–5 elderly people every day and often at first they don’t agree to meet me because fear takes over them. But most of the time I find the front door open and that they want to have a chat and share their fears and hopes to ease the burden of loneliness”.
- (f)
- Nicoletta Rossi, who worked on the project for Bergamo explained, “Often, those who call us are upset and confused. Behind every person is a story and I feel that it is my responsibility and duty to listen to and understand it to find the correct solution” (Cesvi 2020). With the help of 450 volunteers in Bergamo, more than 1000 requests for support and around 922 elderly people were assisted on requests for home deliveries of groceries, urgent medication, balanced meals, and personal protective equipment, as well as providing transport for essential medical visits.
- (g)
- Gallè et al. (2021) carried out a web-based survey from June to August 2021. Of 1041 elderly respondents, (mean age 76.6, SD = 6.5), 60% of participants reported decreased physical activity, worsening sleep, and weight gain due to improper dietary habits
7.4. Help Seeking, Coping, and Resilience of Older People
- (a)
- In the same survey by Gallè et al. (2021), it was found that respondents had a satisfactory level of knowledge about COVID-19. It showed that older people were also coping with the COVID-19 challenge by having active access to health information.
- (b)
- Rossi et al. (2021) were interested in identifying the protective factors against mental distress caused by COVID-19. Their findings highlight that older adults reported lower levels of depressive symptoms, anxiety, and stress compared to the younger population. People aged 60 and over were more willing to follow more stringent measures than the others. They confirmed that age was negatively related to self-perceived stress (r = −0.16, p < 0.001) in the survey of 21,334 respondents. Unfortunately, only 3.5% of the respondents (748 respondents) were over 60 years of age. In other words, older people perform better in overcoming stressful life events such as the COVID-19 pandemic.
- (c)
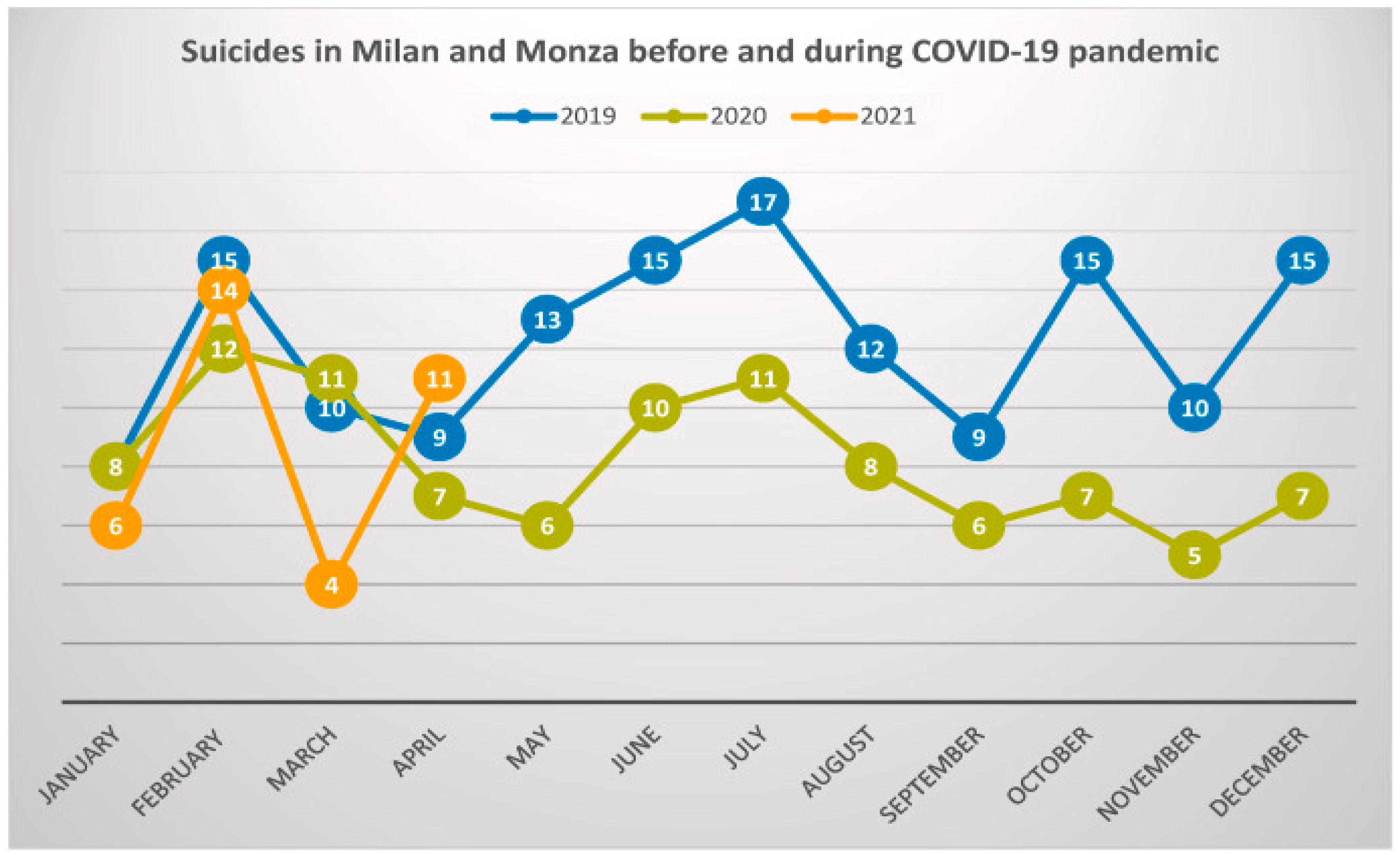
- A study of suicides in Milan showed that the number of suicides in 2020 was lower than that in 2019 (Calati et al. 2021). However, suicides in early 2021 rebounded to higher than 2019 levels (see Figure 18). This can be explained by the delayed effect of post-traumatic psychological disorder following disasters. To everybody’s surprise, the total number of deaths recorded in Italy reached 174,300 by 18 August 2022 (Worldometers 2022a).
7.5. London
Psychological Impacts
- (a)
- Nazroo et al. (2020), in their report commissioned by the Greater London Authority, quoted the data of the London Community Response Survey (Greater London Authority 2020) that older people living in London were more likely to be shielded than younger age groups, with 10% of those aged 50 or older shielding in May 2020, compared with 6% of 30–49-year-olds and 7% of 16–29-year-olds. The same survey showed that between April and May, there was a noticeable increase in the prevalence of loneliness for those aged 50 or older who were living in London (3% reported feeling recently lonely in April, rising to 8% in May). One factor that might be particularly relevant to this is that older people are less likely to be digitally connected, and this is particularly the case for poorer older people and older women (Age UK 2020).
- (b)
- Robb et al. (2020) from the Imperial College of London surveyed older adults in London to explore the associations between social isolation, anxiety, and depression. Questionnaires were sent by email and 7127 voluntary participants (mean age = 70.7 (SD = 7.4)) were recruited from May to July 2020. The Hospital Anxiety Depression Scale (HADS) was used to measure changes during COVID-19. Poor sleep, feelings of loneliness, and living alone were also related to worsening anxiety and depression. “During the period of reduced social contact, have you experienced poor sleep (restless and unable to sleep)?” was the question designed to examine sleep problems. The sleep and loneliness questions were obtained from the Imperial College Sleep Quality questionnaire adapted from the Pittsburgh Sleep Quality Index and Centre for Epidemiologic Studies of Depression Scale.
- (c)
- A total of 12.8% of participants reported feeling worse on the depression components of HADS (7.8% men and 17.3% women), and 12.3% reported feeling worse on the anxiety components (7.8% men and 16.5% women). Fewer participants reported feeling improved (1.5% for depression and 4.9% for anxiety). Social statuses of being female, single, widowed, and divorced were more likely to indicate feeling worse in both depression and anxiety.
- (d)
- Furthermore, 40% of participants reported sleep disturbances. Circumstances surrounding the COVID-19 pandemic increased levels of stress. Worry and ruminating thoughts provoked cognitive arousal and disturbed cortisol homeostasis, resulting in poorer sleep. Furthermore, loneliness and poor sleep have a bi-directional relationship. In this study, 24.6% of those who smoke reported that they had smoked more since the lockdown, and 14.7% of alcohol consumers reported that they had drank more.
7.6. Help Seeking, Coping, and Resilience of Older People
- (a)
- The Physiological Society and Centre for Ageing Better of the UK called for a National COVID-19 Resilience Program to support older people. It was believed that the program would mitigate the negative effects of lockdown and allow older people to take greater control of their health and well-being. This COVID-19 Resilience Program was tailored to the older age groups and included the following goals:
- Encourage appropriate exercise;
- Support optimized nutrition;
- Enhance mental health and wellbeing;
- Influence behavior change.
- (b)
- McKinlay et al. (2021) conducted a qualitative study by interviewing 20 elderly people aged over 70 in London. They found that participants were able to engage in activities and behaviors that helped to protect their mental health, including adopting a slower pace of life, maintaining a routine, and socializing. They drew on their resilience, life experience, and past coping skills to self-manage fear and uncertainty associated with the pandemic. The findings of their survey are similar to those conducted in the United States mentioned earlier.
7.7. Hong Kong
Psychological Impacts
- (a)
- Zhao et al. (2020) reported that during the COVID-19 outbreak, from 1501 respondents, stress levels increased by 28.3%, the prevalence of anxiety increased by 42.3%, and depression symptoms and unhappiness doubled (p < 0.001) as compared to the Hong Kong Family and Health Information Trend Survey (FHInTS) in 2016 and 2017. Furthermore, their results showed that increases in stress levels among older and less educated respondents were significantly larger.
- (b)
- Wong et al. (2020) confirmed in their study that there were significant increases in loneliness, anxiety, and insomnia after the onset of the COVID-19 outbreak. Their data were collected from 583 older (≥60 years) adults. Missed medical appointments over 3 months increased from 16.5% 1 year before the outbreak to 22.0% after the onset of the outbreak. In adjusted analysis, being female, living alone, and having >4 chronic conditions were each independently associated with increased loneliness. Females were also more likely to have increased anxiety and insomnia.
- (c)
- Wand et al. (2020) speculated in a commentary that the suicide rates in Hong Kong would rise under COVID-19. There was no research evidence, but the authors noticed that Hong Kong suffered from economic downturns and social unrest in the year 2019. A valid observation the authors made was that many people who were already in need of mental health services were not able to receive proper care because the city closed down for COVID-19 control. Nevertheless, the prediction of this commentary has yet to be verified.
- (d)
- The first two studies above were conducted in early 2020 and have not taken into account the actual impact of the fifth wave of COVID-19 that happened in the spring of 2022. Furthermore, the third study has no empirical evidence.
7.8. Help Seeking, Coping, and Resilience of Older People
- (a)
- In a follow-up study by Wong et al. (2020); Sit et al. (2022) found that in qualitative interviews of 20 older people, aged between 63 and 86, the use of digital tools and telecommunications contributed to maintaining social connection. At the same time, loneliness was aggravated by depleted family and community support. However, overexposure to digital media had led to a vicious cycle of anxiety and distress because of information overload.
- (b)
- Lau et al. (2021), in their research, focused more on the resilience of Hong Kong people during COVID-19. In a descriptive list of eleven benefits of COVID-19, the two statements “I became more aware of the health of myself and my family/friends”, and “the pandemic enabled me to care more about my family and friends”, were most endorsed, by 761 respondents. The average scale score of perceived benefits was 4.64 (SD = 0.99).
7.9. Summary
8. Discussion
8.1. Vulnerability Strategy in Public Health Disaster
Over the next two weeks, I continued to see patients who were critically ill, requiring noninvasive ventilatory support or intubation, but who was declined admission to the intensive care unit due to frailty or advanced diseases. Many of them were over 80. Some of them were from old age homes. In my brief experience in these isolation wards, I could truly grasp the meaning of “isolation”. In these purpose-built rooms, human contact is a rare entity. Separated by glass panes and hooked up to monitors, patients with communication barriers, be it technological or verbal, received an efficient yet dehumanizing medical processing. When the world is focusing on the safety of the masses, the frail, the silent, and the old have no voice. When the next epidemic comes, I do hope that we could have some elderly-friendly isolation wards.(p. 57)
8.2. Older People Were Social Adherents
8.3. How to Offer Protection to Older People?
8.4. Fail to Shield
8.5. Effects of the Weakened Healthcare System
8.6. Poor Public Health Emergency Responses
8.7. The Pandemic Is Over?
8.8. Limitations of This Study
9. Conclusions
9.1. Preventable Deaths Should and Could Have Been Prevented
9.2. Coping with Social Isolation Needs Supports
9.3. The Danger of an Ambivalent Public Policy
9.4. Whole Government and Whole Community Approach
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Age UK. 2020. COVID-19: Human Rights Implications for Older People. Joint Committee On Human Rights. Available online: https://www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/equality-and-human-rights/age-uk-submission-to-jchr---covid-19-and-human-rights.pdf (accessed on 18 October 2022).
- Amnesty International UK. 2020a. Care Home Report. October 4. Available online: https://www.amnesty.org.uk/care-homes-report (accessed on 18 October 2022).
- Amnesty International UK. 2020b. Older People in Care Homes Abandoned to Die. October 4. Available online: https://www.amnesty.org/en/latest/press-release/2020/10/uk-older-people-in-care-homes-abandoned-to-die-amid-government-failures-during-covid-19-pandemic/ (accessed on 18 October 2022).
- Arup. 2018. Shaping Ageing Neighbourhoods, Gallaratese, Milan. Available online: Shapingageingneighbourhoodsmilan.pdf (accessed on 18 October 2022).
- Auriemma, Vincenzo, and Chiara Iannaccone. 2020. COVID-19 Pandemic: Socio-Economic Consequences of Social Distancing Measures in Italy. Frontier Sociology 5: 575791. [Google Scholar] [CrossRef] [PubMed]
- Auyeung, Tung Wai, Felix H. W. Chan, T. Y. Chan, Carolyn P. L. Kng, Jenny S. W. Lee, James K. H. Luk, Winnie Y. W. Mok, C. K. Shum, and C. W. Wong. 2020. COVID-19 and older adults: Experience in Hong Kong. Asian Journal of Gerontology and Geriatrics 15: 54–59. [Google Scholar] [CrossRef]
- Azarian, Resa. 2011. Potentials and Limitations of Comparative Method in Social Science. International Journal of Humanities and Social Science 1: 113–25. [Google Scholar]
- Bell, David, Adelina Comas-Herrera, David Henderson, Sion Jones, Elizabeth Lemmon, Mirco Moro, Siobhan Murphy, Dermot O’Reilly, and Pietro Patrignani. 2020. COVID-19 Mortality and Long-Term Care: A UK Comparison. International Long Term Care Policy Network, CPEC-LSE, August. Available online: https://ltccovid.org/2020/08/28/covid-19-mortality-and-long-term-care-a-uk-comparison/#_ftnref1 (accessed on 18 October 2022).
- Belli, Brita. 2020. Yale researchers Pursuing COVID-19 Vaccine Based on Powerful Yale Platform. YaleNews. April 29. Available online: https://news.yale.edu/2020/04/29/yale-researchers-pursuing-covid-19-vaccine-based-powerful-yale-platform (accessed on 18 October 2022).
- Blangiardo, Gian Carlo, and Stefania Rimoldi. 2014. Portraits of the Italian Family: Past, Present and Future. Journal of Comparative Family Studies 45: 201–19. [Google Scholar] [CrossRef]
- Brehm, Sharon S., and Jack W. Brehm. 1981. Psychological Reactance: A Theory of Freedom and Control. San Diego: Academic Press. [Google Scholar]
- British Geriatric Society. 2022. Managing the COVID-19 Pandemic in Care Homes for Older People. September 4. Available online: https://www.bgs.org.uk/resources/covid-19-managing-the-covid-19-pandemic-in-care-homes (accessed on 18 October 2022).
- Calati, Rafaella, Guendalina Gentile, Michelle Fornaro, Stefeno Tambuzzi, and Richardo Zoja. 2021. Preliminary suicide trends during the COVID-19 pandemic in Milan, Italy. Journal of Psychiatric Research 143: 21–22. [Google Scholar] [CrossRef] [PubMed]
- CDC. 2021. Suicide in the U.S. Declined during the Pandemic. November 5. Available online: https://www.cdc.gov/nchs/pressroom/podcasts/2021/20211105/20211105.htm (accessed on 18 October 2022).
- Cerami, Chiara, Gaia C. Santi, Caterina Galandra, Allesandra Dodich, Stefeno F. Cappa, Tomaso Vecchi, and Chiara Crespi. 2020. COVID-19 Outbreak In Italy: Are We Ready for the Psychosocial and the Economic Crisis? Baseline Findings From the PsyCovid Study. Front Psychiatry 11: 556. [Google Scholar] [CrossRef]
- Cereda, Danilo, Mattia Manica, Marcello Tirani, Francesca Rovida, Vittorio Demicheli, Marco Ajelli, Piero Poletti, Filippo Trentini, Giorgio Guzzetta, Valentina Marziano, and et al. 2021. The early phase of COVID-19 Outbreak in Lombardy, Italy. Epidemics 37: 100528. Available online: https://www.sciencedirect.com/science/article/pii/S1755436521000724 (accessed on 18 October 2022). [CrossRef] [PubMed]
- Cesvi. 2020. United against Coronavirus to Protect the Elderly People. March 19. Available online: https://www.cesvi.eu/news/united-against-coronavirus-to-protect-the-elderly-people/ (accessed on 18 October 2022).
- Chow, Lina. 2021. Care homes and COVID-19 in Hong Kong: How the lessons from SARS were used to good effect. Age Ageing 50: 21–24. [Google Scholar] [CrossRef] [PubMed]
- Ciceri, Fabio, Antonella Castagna, Patrizia Rovere-Querini, Francesco De Cobelli, Annalisa Ruggeri, Laura Galli, Caterina Conte, Rebecca De Lorenzo, Andrea Poli, and Alberto Ambrosio. 2020. Early predictors of clinical outcomes of COVID-19 outbreak in Milan, Italy. Clinical Immunology 217: 108509. [Google Scholar] [CrossRef] [PubMed]
- City of Milan Statistics Unit. 2020. City Profile–Milan, Italy. Mayors Dialouge on Growth and Prosperity. Available online: https://cdn.odi.org/media/documents/hmi_mayors_dialogue_milan.pdf (accessed on 18 October 2022).
- Di Gessa, Giorgio, and Debora Price. 2022. The impact of shielding during the COVID-19 pandemic on mental health: Evidence from the English Longitudinal Study of Ageing. The British Journal of Psychiatry 221: 1–7. [Google Scholar] [CrossRef]
- Ebbinghaus, Bernhard. 2005. When Less is More: Selection Problems in Large-N and Small-N Cross-National Comparison. International Sociology 20: 133–52. [Google Scholar] [CrossRef]
- Fonseca, Xavier, Stephan Lukosch, and Frances Brazier. 2019. Social cohesion revisited: A new definition and how to characterize it, Innovation. The European Journal of Social Science Research 32: 231–53. [Google Scholar] [CrossRef]
- Füzéki, Eszter, Jan Schröder, Nicholo Carraro, Laura Merlo, Rudiger Reer, David R. Groneberg, and Winfried Banzer. 2021. Physical Activity during the First COVID-19-Related Lockdown in Italy. International Journal of Environmental Research and Public Health 18: 2511. [Google Scholar] [CrossRef]
- Gagliardi, Cristina, Flavia Piccinin, Giovanni Lamura, Georgia Casanova, Paolo Fabbietti, and Marco Socci. 2022. The Burden of Caring for Dependent Older People and the Resultant Risk of Depression in Family Primary Caregivers in Italy. Sustainability 14: 3375. [Google Scholar] [CrossRef]
- Gallè, Francesca, Elita Anna Sabella, Paolo Roma, Stefano Ferracuti, Giovanna Da Molin, Giusy Diella, Maria Teresa Montagna, Giovanni Battista Orsi, Giorgio Liguori, and Christian Napoli. 2021. Knowledge and Lifestyle Behaviors Related to COVID-19 Pandemic in People over 65 Years Old from Southern Italy. International Journal of Environmental Research and Public Health 18: 10872. [Google Scholar] [CrossRef]
- Gilbert, Paul. 2009. Introducing compassion-focused therapy. Advances in Psychiatric Treatment 15: 199–208. [Google Scholar] [CrossRef] [Green Version]
- Golant, Stephen. 2021. COVID-19 Assaulted the Health and Well-Being of Older People, But Their Resilience Helped Them to Cope. Orlando: Booming Encore, September 9. [Google Scholar]
- Gonzalez, Silvia R. 2020. L.A.’s COVID-19 Economic Crisis: Renter Vulnerability Index. UCLA. Center for Neighborhood Knowledge, May 6. Available online: https://knowledge.luskin.ucla.edu/2020/05/06/la-covid-19-economic-crisis-renter-vulnerability-index/ (accessed on 18 October 2022).
- Greater London Authority. 2020. The London Community Response Survey. July 9. Available online: https://www.london.gov.uk/city-hall-blog/london-community-response-survey (accessed on 18 October 2022).
- Greater London Authority. 2022. Coronavirus (COVID-19) Deaths. September 2. Available online: https://data.london.gov.uk/dataset/coronavirus--covid-19--deaths (accessed on 18 October 2022).
- Guida, Carmen, and Gerardo Carpentieri. 2021. Quality of life in the urban environment and primary health services for the elderly during the COVID-19 pandemic: An application to the city of Milan (Italy). Cities 110: 101038. [Google Scholar] [CrossRef] [PubMed]
- Guterres, Antonio. 2020. Our Response to COVID-19 Must Respect the Rights and Dignity of Older People. May 1. Available online: https://www.un.org/en/coronavirus/our-response-covid-19-must-respect-rights-and-dignity-older-people (accessed on 18 October 2022).
- He, Guanhao, Fangfang Zeng, Jianpeng Xiao, Jianguo Zhao, Tao Liu, Jianxiong Hu, Sicong Zhang, Ziqiang Lin, Huaiping Zhu, Dan Liu, and et al. 2022. Association between COVID-19 Vaccination Coverage and Case Fatality Ratio: A Comparative Study-Hong Kong SAR, China and Singapore, December 2021-March 2022. China CDC Weekly 4: 649–54. [Google Scholar] [CrossRef] [PubMed]
- Hills, Stephen, and Yolanda Eraso. 2021. Factors associated with non-adherence to social distancing rules during the COVID-19 pandemic: A logistic regression analysis. BMC Public Health 21: 352. [Google Scholar] [CrossRef] [PubMed]
- HK Census and Statistics Department. 2022. The Profile of Persons Residing in Private Elderly Homes 2021. Available online: https://www.censtatd.gov.hk/en/EIndexbySubject.html?scode=160&pcode=FA100097 (accessed on 18 October 2022).
- HKSAR. 2022. Archive of Statistics on Provisional Analysis on Reported Death Cases. Available online: https://www.coronavirus.gov.hk/pdf/death_analysis/death_analysis_20220831.pdf (accessed on 18 October 2022).
- Huang, Feng Feng, Peng Fai Guo, and Yulan Wang. 2022. Modeling Patients’ Illness Perception and Equilibrium Analysis of Their Doctor Shopping Behavior. Production and Operations Management 31: 1216–34. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/poms.13606 (accessed on 18 October 2022). [CrossRef]
- Hubei Psychological Association. 2020. New Problems Continued to Be Reported after Intervention to 14 Suicide Attempts. Available online: https://www.163.com/dy/article/FAA68JRE0512BEVO.html (accessed on 18 October 2022).
- ifeng.com. 2020. Much More Efforts Are Required to Treat PTSD for the Wuhan Survivors, Than in the Case of Wenchuan Earthquake. Available online: https://news.ifeng.com/c/7uX5GJ1ADzc (accessed on 18 October 2022).
- istat. 2021a. Annual Report 2021—The State of the Nation. Available online: https://www.istat.it/it/files//2021/09/Annual-Report-2021_Summary_EN.pdf (accessed on 18 October 2022).
- istat. 2021b. Impact of COVID-19 Epidemic on Total Mortality of Resident Population. March 5. Available online: https://www.istat.it/en/archivio/254537 (accessed on 18 October 2022).
- istat. 2022. Total Deaths during the Period 1 January–31 May 2022, 2021 and 2020 and Average Years 2015–2019. Available online: https://www.istat.it/en/archivio/268504 (accessed on 18 October 2022).
- Jiang, Nan, Alfred M. Wu, and Edmund W. Cheng. 2022. Social trust and stress symptoms among older adults during the COVID-19 pandemic: Evidence from Asia. BMC Geriatrics 22: 330. Available online: https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-022-02847-5 (accessed on 18 October 2022). [CrossRef] [PubMed]
- JHU (John Hopkins University). 2020. COVID-19 and the Long Road to Herd Immunity. April 30. Available online: https://hub.jhu.edu/2020/04/30/herd-immunity-covid-19-coronavirus/ (accessed on 18 October 2022).
- Kontokosta, Constantine E., Boyeong Hong, and Bartosz J. Bonczak. 2022. Measuring sensitivity to social distancing behavior during the COVID-19 pandemic. Scientific Reports 12: 16350. [Google Scholar] [CrossRef]
- Kwok, Kin On, Kin Kit Li, Henry H. Chan, Yuan Yuan Yi, Arthur Tang, Wan In Wei, and Samuel Y. S. Wong. 2020. Community Responses during Early Phase of COVID-19 Epidemic, Hong Kong. Emerging Infectious Disease 26: 1575–79. [Google Scholar] [CrossRef] [PubMed]
- Lam, Wendy Wing Tak, Jingyi Xiao, Michael Yuxuan Ni, Benjamin John Cowling, Qiuyan Liao, and Jiehu Yuan. 2022. Why do Chinese older adults in Hong Kong delay or refuse COVID-19 vaccination? A qualitative study based on Grounded Theory, Preprint (Version 1) April 18. Available online: https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/ppcovidwho-334380 (accessed on 18 October 2022).
- Lau, H. P. Bobo, Cecilia L. W. Chan, and Siu-Man Ng. 2021. Resilience of Hong Kong people in the COVID-19 pandemic: Lessons learned from a survey at the peak of the pandemic in Spring, 2020. Asia Pacific Journal of Social Work and Development 31: 105–14. [Google Scholar] [CrossRef]
- Light, Ben. 2013. Digitally Mediated Social Networking Practices: A Focus on Connectedness and Disconnectedness. Paper presented at the ITI 2013 35th International Conference on Information Technology Interfaces, Cavtat, Croatia, June 24–27; pp. 3–8. [Google Scholar]
- Lorenzo-Redondo, Ramen, Egon A. Ozer, and Judd F. Hultquist. 2022. COVID-19: Is omicron less lethal than delta? British Medical Journal 378: o1806. [Google Scholar] [CrossRef] [PubMed]
- Macmahon, Alle. 2020. Coronavirus: UK Government’s ‘Herd Immunity’ Plan Sparks Fear and Fury, New Zealand Herald. March 17. Available online: https://www.nzherald.co.nz/world/coronavirus-uk-governments-herd-immunity-plan-sparks-fear-and-fury/ARQ3BOD4IGBLSM3WEQXAYBMGYI/ (accessed on 18 October 2022).
- Manchia, Mirko, Anouk W. Gathier, Hale Yapici-Eser, Mathias V. Schmidt, Dominique de Quervain, Therese van Amelsvoort, Jonathan I. Bisson, John F. Cryan, Oliver D. Howes, Luisa Pinto, and et al. 2022. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: A critical review across waves. European Neuropsychopharmacology 55: 22–83. [Google Scholar] [CrossRef]
- Marples, Megan. 2020. Pandemic Denial: Why Some People Can’T Accept COVID-19’s Realities. CNN. August 16. Available online: https://www.cnn.com/2020/08/16/health/pandemic-covid-19-denial-mental-health-wellness/index.html (accessed on 18 October 2022).
- Marvel, Skylar W., John S. House, Matthew Wheeler, Kucheng Song, Yi-hui Zhou, Fred A. Wright, Weihsueh A. Chiu, Ivan Rusyn, Alison Motsinger-Reif, and David M. Reif. 2020. The COVID-19 Pandemic Vulnerability Index (PVI) Dashboard: Monitoring county-level vulnerability using visualization, statistical modeling, and machine learning. medRxiv [Preprint] 13. reprinted in Environ Health Perspect 129: 17701. [Google Scholar] [CrossRef]
- Mazzola, Paolo, Stefania Maria Lorenza Rimoldi, Paolo Rossi, Marianna Noale, Federico Rea, Carla Facchini, Stefania Maggi, Giovanni Corrao, and Giorgio Annoni. 2015. Aging in Italy: The Need for New Welfare Strategies in an Old Country. Gerontologist 56: 383–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKinlay, Alison Ruth, Daisy Fancourt, and Alexandra Burton. 2021. A qualitative study about the mental health and wellbeing of older adults in the UK during the COVID-19 pandemic. BMC Geriatrics 21: 439. [Google Scholar] [CrossRef] [PubMed]
- McPhee, Sarah. 2020. Swab from Milan Boy, 4, Tests Positive to Coronavirus Weeks before Wuhan Outbreak. News.com.au. December 3. Available online: https://www.news.com.au/world/coronavirus/global/swab-from-milan-boy-4-tests-positive-to-covid-weeks-before-wuhan-outbreak/news-story/93445d56f87996fa33fbae233ad7712e (accessed on 18 October 2022).
- Megna, Rosario. 2020. First month of the epidemic caused by COVID-19 in Italy: Current status and real-time outbreak development forecast. Global Health Research and Policy 5: 43. [Google Scholar] [CrossRef]
- Mills, Melinda, Gerhard G. Van de Bunt, and Jeanne De Bruijn. 2006. Comparative research: Persistent problems and promising solutions. International Sociology 21: 619–31. [Google Scholar] [CrossRef]
- Morgan, Craig, Tom Burns, Ray Fitzpatrick, Vanessa Pinfold, and Stefan Priebe. 2007. Social exclusion and mental health conceptual and methodological review. The British Journal of Psychiatry 191: 477–83. [Google Scholar] [CrossRef] [PubMed]
- Nazroo, James, Karl Murray, Harry Taylor, Laia Bécares, Yvonne Field, Dharmi Kapadia, and Yansie Rolston. 2020. Rapid Evidence Review: Inequalities in Relation to COVID-19 and Their Effects on London, Greater London Authority. Available online: https://www.london.gov.uk/decisions/add2449-rapid-evidence-review-inequalities-relation-covid-19 (accessed on 18 October 2022).
- NHS. 2022. COVID-19 Total Deaths Supplementary File Archive. October 5. Available online: https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-deaths/supplementary-total-archive/ (accessed on 18 October 2022).
- NTI. 2022. GHSI-Assessing Global Health Conditions. October 16. Available online: https://www.nti.org/about/programs-projects/project/global-health-security-index/ (accessed on 18 October 2022).
- Ortenzi, Flaminia, Emiliano Albanese, and Marta Fadda. 2020. A Transdisciplinary Analysis of COVID-19 in Italy: The Most Affected Country in Europe. International Journal of Environmental Research and Public Health 17: 9488. [Google Scholar] [CrossRef]
- Osborne, Geraint. 2020. We Can’t Stress the Importance of Social Connection Enough. Folio: University of Alberta, May, Available online: https://www.ualberta.ca/folio/2020/05/commentary--we-cant-stress-the-importance-of-social-connection-enough.html (accessed on 18 October 2022).
- Pan, An, Li Liu, Chaolong Wang, Huan Guo, Xingjie Hao, Qi Wang, Jiao Huang, Na He, Hongjie Yu, and Xihong Lin. 2020. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA 323: 1915–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pathirathna, Malshani L., Hapugahapitiye Mohottalage Renu Kalhari Geethani Nandasena, Atapattu Mudiyanselage Muditha Piumali Atapattu, and Ishanka Weerasekara. 2022. Impact of the COVID-19 pandemic on suicidal attempts and death rates: A systematic review. BMC Psychiatry 22: 506. [Google Scholar] [CrossRef]
- Prante, Franz J., Alessandro Bramucci, and Achim Truger. 2020. Decades of Tight Fiscal Policy Have Left the Health Care System in Italy Ill-Prepared to Fight the COVID-19 Outbreak. Intereconomics 55: 147–52. [Google Scholar] [CrossRef] [PubMed]
- qq.com. 2020. Older Person Refused to Return Home after Discharged a Case of Wuhan Trauma, Explained the Shanghai Psychological Response Team. Available online: https://new.qq.com/rain/a/20200302A0OOCG00 (accessed on 18 October 2022).
- Reuters. 2020a. G20 Health Ministers Acknowledge Health Systems’ Vulnerability to Pandemics: Statement. April 12. Available online: https://www.reuters.com/article/us-health-coronavirus-g20-idUSKBN2210PP (accessed on 18 October 2022).
- Reuters. 2020b. Why Has Italy Suffered So Badly during the Pandemic? December 7. Available online: https://www.weforum.org/agenda/2020/12/italy-death-toll-pandemic-covid-coronavirus-health-population-europe/ (accessed on 18 October 2022).
- Robb, Catherine E., Celeste A. de Jager, Sara Ahmadi-Abhari, Parthenia Giannakopoulou, Chinedu Udeh-Momoh, James McKeand, Geraint Price, Josip Car, Azeem Majeed, Helen Ward, and et al. 2020. Associations of Social Isolation with Anxiety and Depression During the Early COVID-19 Pandemic: A Survey of Older Adults in London, UK. Frontier Psychiatry 11: 591120. [Google Scholar] [CrossRef]
- Rossi, Rodolfo, Tommaso B. Jannini, Valentina Socci, Francesca Pacitti, and Giorgio Di Lorenzo. 2021. Stressful Life Events and Resilience during the COVID-19 Lockdown Measures in Italy: Association With Mental Health Outcomes and Age. Front Psychiatry 12: 635832. [Google Scholar] [CrossRef]
- Ruthman, Tobias, Fahima Farkhari, Flavio Azevedo, and Carolin T. Ziemer. 2022. Psychological underpinnings of pandemic denial-patterns of disagreement with scientific experts in the German public during the COVID-19 pandemic. Public Understanding of Science 31: 437–57. [Google Scholar] [CrossRef]
- Santini, Ziggi Ivan, Paul E. Jose, Erin York Cornwell, Ai Koyanagi, Line Nielsen, Carsten Hinrichsen, Charlotte Meilstrup, Katrine Rich Madsen, and Vibeke Koushede. 2020. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 5: e62–e70. [Google Scholar] [CrossRef] [Green Version]
- Santini, Ziggi Ivan, Veronica S. C. Pisinger, Line Nielsen, Katrine Rich Madsen, and Charlotte Meilstrup. 2021. Social disconnectedness, loneliness, and mental health among adolescents in Danish high schools: A nationwide cross-sectional study. Frontiers in Behavioral Neuroscience 15: 632906. [Google Scholar] [CrossRef] [PubMed]
- Saraceno, Chiara, David Benassi, and Enrica Morlicchio. 2021. Poverty in Italy A Regime Approach. Cambridge: Cambridge University Press, March 4, Available online: https://www.cambridge.org/core/books/abs/poverty-in-italy/regime-approach/54462F06DC24C6CECA3C3C90C102D198 (accessed on 18 October 2022).
- Schmidt-Sane, Megan, Leslie Jones, and Oilivia Tulloch. 2020. Key Considerations: Emerging Evidence on Shielding Vulnerable Groups during COVID-19. Social Science in Humanitarian Action Platform. Available online: https://www.preventionweb.net/publication/key-considerations-emerging-evidence-shielding-vulnerable-groups-during-covid-19 (accessed on 18 October 2022).
- Schultze, Anna, Emily Nightingale, David Evans, William Hulme, Alicia Rosello, Chris Bates, Brian MacKenna, Helen J. Curtis, Caroline E. Morton, Richard Croker, and et al. 2022. Mortality among Care Home Residents in England during the first and second waves of the COVID-19 pandemic: An observational study of 4.3 million adults over the age of 65. The Lancet Regional Health—Europe 14: 100295. [Google Scholar] [CrossRef] [PubMed]
- Sher, Leo. 2020. The impact of the COVID-19 pandemic on suicide rates. QJM 113: 707–12. [Google Scholar] [CrossRef] [PubMed]
- Sit, Regina W.-S., Harmony Hoi Ki Lai, Dong Dong, Bo Wang, Martin Chi-sang Wong, Roger Yat Nork Chung, and Samuel Y.-S. Wong. 2022. Explaining the Psychosocial Effects of COVID-19 Among Older Hong Kong Chinese People-A Qualitative Analysis. Journal of Geriatric Psychiatry Neurology 35: 206–14. [Google Scholar] [CrossRef]
- Social Welfare Department HKSAR. 2022. Social Security Allowance (SSA) Scheme. September 5. Available online: https://www.swd.gov.hk/en/index/site_pubsvc/page_socsecu/sub_ssallowance/index.html (accessed on 18 October 2022).
- Sputnik. 2020. Swedish Model: Ruined Economy Will Cause More Deaths than Coronavirus. May 7. Available online: https://www.sott.net/article/434004-Swedish-Model-Ruined-economy-will-cause-more-deaths-than-coronavirus-Prof (accessed on 18 October 2022).
- Statista. 2022a. COVID-19 Coronavirus Facts and Figures. September 2. Available online: https://www.statista.com/page/covid-19-coronavirus (accessed on 18 October 2022).
- Statista. 2022b. Average Living Space of Public Rental Housing Tenants in Hong Kong from 2007 to 2021. Available online: https://www.statista.com/statistics/630746/hong-kong-public-rental-housing-average-living-space-per-person/ (accessed on 18 October 2022).
- Tognotti, Eugenia. 2013. Lessons from the history of quarantine, from plague to influenza A. Emergency Infectious Diseases 19: 254–59. [Google Scholar] [CrossRef]
- Torres, Juliana Lustosa, Luciana de Souza Braga, Bruno de Souza Moreira, Camila Menezes Sabino Castro, Camila Teixeira Vaz, Amanda Cristina de Souza Andrade, Fabíola Bof Andrade, Maria Fernanda Lima-Costa, and Waleska Teixeira Caiaffa. 2021. Loneliness and social disconnectedness in the time of pandemic period among brazilians: Evidence from the elsi COVID-19 initiative. Aging & Mental Health. Advance Online Publication. [Google Scholar] [CrossRef]
- UK Parliament. 2022. The Government’s Response to COVID-19: Human Rights Implications. October 16. Available online: https://committees.parliament.uk/work/218/the-government-s-response-to-covid-19--human-rights-implications/ (accessed on 18 October 2022).
- United Nations. 2020. United Nations Comprehensive Response to COVID-19: Saving Lives, Protecting Societies, Recovering Better. Available online: https://www.un.org/sites/un2.un.org/files/2020/07/un_comprehensive_response_to_covid-19_june_2020.pdf (accessed on 18 October 2022).
- United Nations Habitat. 2020. UN-Habitat COVID-19 Response Plan. April. Available online: https://unhabitat.org/sites/default/files/2020/04/final_un-habitat_covid-19_response_plan.pdf (accessed on 18 October 2022).
- UNSDG (United Nations Sustainable Development Group). 2020. Policy Brief: The Impact of COVID-19 on Older Persons. Available online: https://unsdg.un.org/sites/default/files/2020-05/Policy-Brief-The-Impact-of-COVID-19-on-Older-Persons.pdf (accessed on 18 October 2022).
- University of Oxford. 2020. COVID-19 Government Response Tracker. Available online: https://www.bsg.ox.ac.uk/research/research-projects/covid-19-government-response-tracker (accessed on 18 October 2022).
- Vetter, David. 2019. How Hong Kong’s Public Housing System Works: Costs, Waiting Times and Sales. South China Morning Post. January 19. Available online: https://www.scmp.com/news/hong-kong/society/article/2182106/why-public-housing-shortfall-will-remain-thorn-hong-kongs (accessed on 18 October 2022).
- Wand, Anne Pamela Frances, Bao-Liang Zhong, Helen Fung Kum Chiu, Brian Draper, and Diego De Leo. 2020. COVID-19: The Implications for Suicide in Older Adults. International Psychogeriatrics 32: 1225–30. [Google Scholar] [CrossRef]
- WHO. 2019. Health Emergency and Disaster Risk Framework. Available online: https://www.who.int/publications/i/item/health-emergency-and-disaster-risk-management-framework (accessed on 18 October 2022).
- WHO. 2022a. COVID-19 Dashboard. Overview. Available online: https://covid19.who.int/?mapFilter=deaths (accessed on 18 October 2022).
- WHO. 2022b. COVID-19 Explorer. Available online: https://worldhealthorg.shinyapps.io/covid/ (accessed on 18 October 2022).
- WHO. 2022c. Essential Health Services Face Continued Disruption during COVID-19 Pandemic. February 7. Available online: https://www.who.int/news/item/07-02-2022-essential-health-services-face-continued-disruption-during-covid-19-pandemic (accessed on 18 October 2022).
- WHO. 2022d. COVID-19 Cases and Deaths with Age and Gender Reported. Available online: https://app.powerbi.com/view?r=eyJrIjoiYWRiZWVkNWUtNmM0Ni00MDAwLTljYWMtN2EwNTM3YjQzYmRmIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9 (accessed on 18 October 2022).
- Wilkinson, Annie, and James Fairhead. 2016. Comparison of social resistance to Ebola response in Sierra Leone and Guinea suggests explanations lie in political configurations not culture. Critical Global Health 27: 14–27. [Google Scholar] [CrossRef] [Green Version]
- Wong, Samuel Yeung Shan, Dexing Zhang, Regina Wing Shan Sit, Benjamin Hon Kei Yip, Roger Yat-Nork Chung, Carmen Ka Man Wong, Dicken Cheong Chun Chan, Wen Sun, Kin On Kwok, and Stewart W. Mercer. 2020. Impact of COVID-19 on loneliness, mental health, and health service utilisation: A prospective cohort study of older adults with multimorbidity in primary care. British Journal of General Practice 70: e817–e824. [Google Scholar] [CrossRef]
- World-in-Data. 2022. Hong Kong Coronavirus Pandemic Profile. September 4. Available online: https://ourworldindata.org/coronavirus/country/hong-kong (accessed on 18 October 2022).
- Worldometers. 2020. COVID-19, Coronavirus Pandemic. March 27. Available online: https://www.worldometers.info/coronavirus/#countries (accessed on 18 October 2022).
- Worldometers. 2022a. Coronavirus. September 2. Available online: https://www.worldometers.info/coronavirus/country/italy/ (accessed on 18 October 2022).
- Worldometers. 2022b. Daily New Deaths in China, Hong Kong SAR. October 14. Available online: https://www.worldometers.info/coronavirus/country/china-hong-kong-sar/#graph-deaths-daily (accessed on 18 October 2022).
- Wright, Nicola, and Theo Stickley. 2013. Concepts of social inclusion, exclusion and mental health: A review of the international literature. Journal of Psychiatric Mental Health Nursing 20: 71–81. [Google Scholar] [CrossRef]
- Yan, Bo, Xiaoming Zhang, Long Wu, Heng Zhu, and Bin Chen. 2020. Why Do Countries Respond Differently to COVID-19? A Comparative Study of Sweden, China, France, and Japan. The American Review of Public Administration. 50. Available online: https://journals.sagepub.com/doi/full/10.1177/0275074020942445 (accessed on 18 October 2022).
- Yang, Juan, Xinhua Chen, Xiaowei Deng, Zhiyuan Chen, Hui Gong, Han Yan, Qianhui Wu, Huilin Shi, Shengjie Lai, Marco Ajelli, and et al. 2020. Disease burden and clinical severity of the first pandemic wave of COVID-19 in Wuhan, China. Nature Communications 11: 5411. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Sheng Zhi, Janet Yuen Ha Wong, Tzu Tsun Luk, Abraham Ka Chung Wai, Tai Hing Lam, and Man Ping Wang. 2020. Mental health crisis under COVID-19 pandemic in Hong Kong, China. International Journal of Infectious Diseases 100: 431–33. [Google Scholar] [CrossRef] [PubMed]















| Age | Female | Male | Sub-Total | Percentage |
|---|---|---|---|---|
| 80+ | 433,122 | 421,803 | 854,925 | 36.98 |
| 75–79 | 119,816 | 170,698 | 290,514 | 12.57 |
| 70–74 | 113,943 | 171,581 | 285,524 | 12.35 |
| 65–69 | 763,92 | 149,851 | 226,243 | 9.79 |
| above 65 | 743,273 | 913,933 | 1,657,206 | 71.68 |
| City | Population | Aging Rate | Older Population |
|---|---|---|---|
| Wuhan | 8.4 M | 11.61% | 0.975 M |
| Hong Kong | 7.8 M | 19% | 1.482 M |
| Milan | 10.8 M | 22.4% | 2.419 M |
| London | 9.0 M | 11.9% | 1.071 M |
| City | Time Frame |
|---|---|
| Wuhan | Jan to May 2020 |
| Milan | Feb to May 2020 |
| London | March 2020 to March 2021 |
| Hong Kong | Jan to June 2022 |
| City | Aged Population | COVID Deaths | Deaths per 100,000 |
|---|---|---|---|
| Wuhan | 0.975 M | 2114 | 216.8 |
| Hong Kong | 1.482 M | 5118 | 345.34 |
| Milan | 2.419 M | 19,921 | 823.52 |
| London | 1.071 M | 19,102 | 1783.57 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, J.H.C.; Ho, G.W. Shielding without a Shield—Older People under COVID-19: A Comparison of Four Cities. Soc. Sci. 2022, 11, 498. https://doi.org/10.3390/socsci11110498
Wong JHC, Ho GW. Shielding without a Shield—Older People under COVID-19: A Comparison of Four Cities. Social Sciences. 2022; 11(11):498. https://doi.org/10.3390/socsci11110498
Chicago/Turabian StyleWong, Johnston H. C., and Ghee W. Ho. 2022. "Shielding without a Shield—Older People under COVID-19: A Comparison of Four Cities" Social Sciences 11, no. 11: 498. https://doi.org/10.3390/socsci11110498
APA StyleWong, J. H. C., & Ho, G. W. (2022). Shielding without a Shield—Older People under COVID-19: A Comparison of Four Cities. Social Sciences, 11(11), 498. https://doi.org/10.3390/socsci11110498







