Influences of COVID-19 Work-Related Fears and Anhedonia on Resilience of Workers in the Health Sector during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Materials
2.3. Participants
2.4. Statistical Analyses
3. Results
3.1. Descriptive Statistics of Resilience, Anhedonia and COVID-19 Work-Related Fears in WHS at t1 and t2
3.2. Correlation between Resilience Anhedonia and COVID-19 Work-Related Fears at t1 and t2
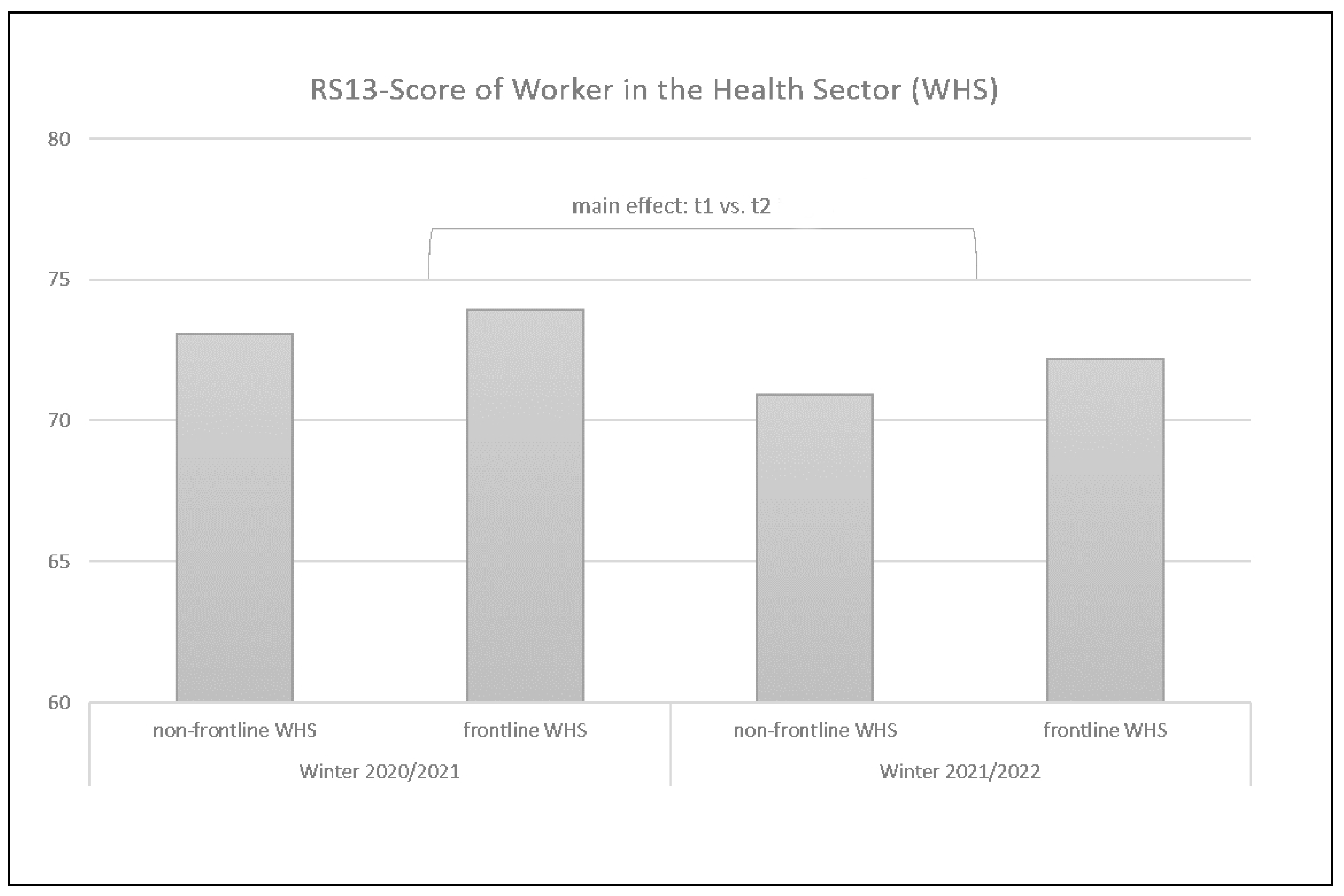
3.3. Frontline WHS vs. Non-Frontline WHS at t1 and t2
3.4. Repeated Measure Analyses for a Subsample at t1 Compared to t2 (n = 186)
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Awano, Nobuyasu, Nene Oyama, Keiko Akiyama, Minoru Inomata, Naoyuki Kuse, Mari Tone, Kohei Takada, Yutaka Muto, Kazushi Fujimoto, Yu Akagi, and et al. 2020. Anxiety, depression, and resilience of healthcare workers in Japan during the coronavirus disease 2019 outbreak. Internal Medicine 59: 2693–99. [Google Scholar] [CrossRef] [PubMed]
- Baskin, Rachel G., and Robin Bartlett. 2021. Healthcare worker resilience during the COVID-19 pandemic: An integrative review. Journal of Nursing Management 29: 2329–42. [Google Scholar] [CrossRef] [PubMed]
- Braquehais, Maria Dolores, Sebastián Vargas-Cáceres, Esperanza Gómez-Durán, Gemma Nieva, Sergi Valero, Miquel Casas, and Eugeni Bruguera. 2020. The Impact of the COVID-19 pandemic on the mental health of healthcare professionals. Social Psychiatry and Psychiatric Epidemiology 57: 633–45. [Google Scholar] [CrossRef] [PubMed]
- Buscetta, Ashley J., Khadijah E. Abdallah, K. Jameson Floyd, Faeben S. Wossenseged, Corinne A. Conn, Hasmin C. Ramirez, and Vence L. Bonham. 2022. Examining resilience of individuals living with sickle cell disease in the COVID-19 pandemic. BMC Psychology 10: 1–10. [Google Scholar] [CrossRef]
- Çam, Olcay, and Ayşe Büyükbayram. 2017. Nurses’ Resilience and Effective Factors. Journal of Psychiatric Nursing/Psikiyatri Hemsireleri Dernegi 8: 118–26. [Google Scholar] [CrossRef]
- Christensen, Trine, Christina F. Bisgaard, and Ove Wiborg. 2011. Biomarkers of anhedonic-like behavior, antidepressant drug refraction, and stress resilience in a rat model of depression. Neuroscience 196: 66–79. [Google Scholar] [CrossRef]
- D’Addario, Sebastian Luca, Matteo Di Segni, Ada Ledonne, Rosamaria Piscitelli, Lucy Babicola, Alessandro Martini, Elena Spoleti, Camilla Mancini, Donald Ielpo, Francesca R. D’Amato, and et al. 2021. Resilience to anhedonia-passive coping induced by early life experience is linked to a long-lasting reduction of Ih current in VTA dopaminergic neurons. Neurobiology of Stress 14: 100324. [Google Scholar]
- Dalkner, Nina, Jolana Wagner-Skacel, Michaela Ratzenhofer, Frederike Fellendorf, Melanie Lenger, Alexander Maget, Adelina Tmava-Berisha, René Pilz, Robert Queissner, Carlo Hamm, and et al. 2021. Psychological symptoms during and after Austrian first lockdown in individuals with bipolar disorder? A follow-up control-group investigation. International Journal of Bipolar Disorders 9: 1–15. [Google Scholar] [CrossRef]
- Dias, Caroline, Jian Feng, Haosheng Sun, Michelle S. Mazei-Robison, Diane Damez-Werno, Kimberly Scobie, Rosemary Bagot, Benoit LaBonté, Efrain Ribeiro, XiaoChuan Liu, and et al. 2014. β-catenin mediates stress resilience through Dicer1/microRNA regulation. Nature 516: 51–55. [Google Scholar] [CrossRef]
- El Sayed, Samir, Doaa Shokry, and Sarah Mohamed Gomaa. 2021. Post-COVID-19 fatigue and anhedonia: A cross-sectional study and their correlation to post-recovery period. Neuropsychopharmacology Reports 41: 50–55. [Google Scholar] [CrossRef]
- Elliott, Evan, Gili Ezra-Nevo, Limor Regev, Adi Neufeld-Cohen, and Alon Chen. 2010. Resilience to social stress coincides with functional DNA methylation of the Crf gene in adult mice. Nature Neuroscience 13: 1351–53. [Google Scholar] [CrossRef] [PubMed]
- Fellendorf, Frederike T., Eva Z. Reininghaus, Michaela Ratzenhofer, Melanie Lenger, Alexander Maget, Martina Platzer, Susanne A. Bengesser, Armin Birner, Robert Queissner, Carlo Hamm, and et al. 2021. COVID-19-related fears and information frequency predict sleep behavior in bipolar disorder. Brain and Behavior 11: e02182. [Google Scholar] [CrossRef] [PubMed]
- Fleischmann, Eva, Frederike T. Fellendorf, Jennifer Ortner, Susanne A. Bengesser, Michaela Ratzenhofer, René Pilz, Melanie Lenger, Armin Birner, Robert Queissner, Martina Platzer, and et al. 2022. Anxious Temperament Predicts Poor Acceptance of Self and Life in Bipolar Disorder during the COVID-19 Pandemic. Psychiatry International 3: 236–47. [Google Scholar] [CrossRef]
- Fletcher, David, and Mustafa Sarkar. 2013. Psychological resilience: A review and critique of definitions, concepts, and theory. European Psychologist 18: 12. [Google Scholar] [CrossRef]
- Franz, M., T. Meyer, F. Ehlers, P. Runzheirmer, and B. Gallhofer. 1998. German version of the Snaith-Hamilton-Pleasure Scale (SHAPS-D): Assessing anhedonia in schizophrenic patients. European Psychiatry 13: 174s. [Google Scholar] [CrossRef]
- Nationale Referenzzentrale für Influenza-Epidemiologie. 2020. Österreichische Agentur für Gesundheit und Ernährungssicherheit AGES Dashboard COVID19. Available online: https://covid19-dashboard.ages.at (accessed on 13 October 2022).
- Gaspar, Rita, Carina Soares-Cunha, Ana Verónica Domingues, Bárbara Coimbra, Filipa I. Baptista, Luísa Pinto, António F. Ambrósio, Ana João Rodrigues, and Catarina A. Gomes. 2021. Resilience to stress and sex-specific remodeling of microglia and neuronal morphology in a rat model of anxiety and anhedonia. Neurobiology of Stress 14: 100302. [Google Scholar] [CrossRef]
- Gawlytta, Romina, and Jenny Rosendahl. 2015. Was ist Resilienz und wie kann sie gemessen werden? Public Health Forum. Berlin: De Gruyter, vol. 23, pp. 212–14. [Google Scholar]
- Heshmati, Mitra, and Scott J. Russo. 2015. Anhedonia and the brain reward circuitry in depression. Current Behavioral Neuroscience Reports 2: 146–53. [Google Scholar] [CrossRef]
- Hjemdal, Odin, Oddgeir Friborg, and Tore C. Stiles. 2012. Resilience is a good predictor of hopelessness even after accounting for stressful life events, mood and personality (NEO-PI-R). Scandinavian Journal of Psychology 53: 174–80. [Google Scholar] [CrossRef]
- Hjemdal, Odin, Patrick A. Vogel, Stian Solem, Kristen Hagen, and Tore C. Stiles. 2011. The relationship between resilience and levels of anxiety, depression, and obsessive–compulsive symptoms in adolescents. Clinical Psychology & Psychotherapy 18: 314–21. [Google Scholar]
- Kim, Geun Myun, Ji Young Lim, Eun Joo Kim, and Seung-Min Park. 2019. Resilience of patients with chronic diseases: A systematic review. Health & Social Care in the Community 27: 797–807. [Google Scholar]
- Kimhi, Shaul, Yohanan Eshel, Hadas Marciano, and Bruria Adini. 2020. A renewed outbreak of the COVID-19 pandemic: A longitudinal study of distress, resilience, and subjective well-being. International Journal of Environmental Research and Public Health 17: 7743. [Google Scholar] [CrossRef] [PubMed]
- King, Danielle D., Alexander Newman, and Fred Luthans. 2016. Not if, but when we need resilience in the workplace. Journal of Organizational Behavior 37: 782–86. [Google Scholar] [CrossRef]
- Landaeta-Díaz, Leslie, Gabriel González-Medina, and Samuel Durán Agüero. 2021. Anxiety, anhedonia and food consumption during the COVID-19 quarantine in Chile. Appetite 164: 105259. [Google Scholar] [CrossRef]
- Leppert, Karena, Benjamin Koch, Elmar Brähler, and Bernhard Strauß. 2008. Die Resilienzskala (RS)–Überprüfung der Langform RS-25 und einer Kurzform RS-13. Klinische Diagnostik und Evaluation 1: 226–43. [Google Scholar]
- Li, Zhizhuan, Jianxiang Zha, Pengcheng Zhang, Chenyu Shangguan, Xia Wang, Jiamei Lu, and Min Zhang. 2020. Negative life events and mood states: Emotional resilience as mediator and moderator. Social Behavior and Personality: An International Journal 48: 1–12. [Google Scholar] [CrossRef]
- Liu, Jenny JW, Maureen Reed, and Todd A. Girard. 2017. Advancing resilience: An integrative, multi-system model of resilience. Personality and Individual Differences 111: 111–18. [Google Scholar] [CrossRef]
- Masten, Ann S., and Marie-Gabrielle J. Reed. 2002. Resilience in development. Handbook of Positive Psychology 74: 88. [Google Scholar]
- McCann, Clare M., Elizabeth Beddoe, Katie McCormick, Peter Huggard, Sally Kedge, Carole Adamson, and Jayne Huggard. 2013. Resilience in the health professions: A review of recent literature. International Journal of Wellbeing 3: 60–81. [Google Scholar] [CrossRef]
- Meichenbaum, Donald. 2017. Stress Inoculation Training: A Preventative and Treatment Approach. The Evolution of Cognitive Behavior Therapy. London: Routledge, pp. 101–24. [Google Scholar]
- Min, Jung-Ah, Jeong Jin Yu, Chang-Uk Lee, and Jeong-Ho Chae. 2013. Cognitive emotion regulation strategies contributing to resilience in patients with depression and/or anxiety disorders. Comprehensive Psychiatry 54: 1190–97. [Google Scholar] [CrossRef]
- Morgan, Charles A., III, Ann M. Rasmusson, Sheila Wang, Gary Hoyt, Richard L. Hauger, and Gary Hazlett. 2002. Neuropeptide-Y, cortisol, and subjective distress in humans exposed to acute stress: Replication and extension of previous report. Biological Psychiatry 52: 136–42. [Google Scholar] [CrossRef]
- Nierenberg, Andrew A., Jonathan E. Alpert, Joel Pava, Jerrold F. Rosenbaum, and Maurizio Fava. 1998. Course and treatment of atypical depression. The Journal of Clinical Psychiatry 59: 5–9. [Google Scholar] [PubMed]
- Pearman, Ann, MacKenzie L. Hughes, Emily L. Smith, and Shevaun D. Neupert. 2020. Mental health challenges of United States healthcare professionals during COVID-19. Frontiers in Psychology 11: 2065. [Google Scholar] [CrossRef] [PubMed]
- Prakash, Nandkishore, Christiana J. Stark, Maria N. Keisler, Lily Luo, Andre Der-Avakian, and Davide Dulcis. 2020. Serotonergic Plasticity in the Dorsal Raphe Nucleus Characterizes Susceptibility and Resilience to Anhedonia. Journal of Neuroscience 40: 569–84. [Google Scholar] [CrossRef]
- Rasmusson, Ann M., Meena Vythilingam, and Charles A. Morgan. 2003. The neuroendocrinology of posttraumatic stress disorder: New directions. CNS Spectrums 8: 651–67. [Google Scholar] [CrossRef]
- Rayani, Saba, Mohammad Rayani, and Fatemeh Najafi-Sharjabad. 2022. Correlation between anxiety and resilience of healthcare workers during COVID-19 pandemic in the southwest of Iran. Environmental Science and Pollution Research 29: 21528–36. [Google Scholar] [CrossRef]
- Rees, Clare S., Lauren J. Breen, Lynette Cusack, and Desley Hegney. 2015. Understanding individual resilience in the workplace: The international collaboration of workforce resilience model. Frontiers in Psychology 6: 73. [Google Scholar] [CrossRef] [PubMed]
- Robertson, Ivan T., Cary L. Cooper, Mustafa Sarkar, and Thomas Curran. 2015. Resilience training in the workplace from 2003 to 2014: A systematic review. Journal of Occupational and Organizational Psychology 88: 533–62. [Google Scholar] [CrossRef]
- Russo, Scott J., James W. Murrough, and Ming-Hu Han. 2012. Neurobiology of resilience. Nature Neuroscience 15: 1475–84. [Google Scholar] [CrossRef] [PubMed]
- Rutter, Michael. 1987. Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry 57: 316–31. [Google Scholar] [CrossRef] [PubMed]
- Santos, Manuel C., Luísa Barros, and Elisabete Carolino. 2010. Occupational stress and coping resources in physiotherapists: A survey of physiotherapists in three general hospitals. Physiotherapy 96: 303–10. [Google Scholar] [CrossRef]
- Sbragia, Elvira, Eleonora Colombo, Chiara Pollio, Maria Cellerino, Caterina Lapucci, Matilde Inglese, Gianluigi Mancardi, and Giacomo Boffa. 2022. Embracing resilience in multiple sclerosis: A new perspective from COVID-19 pandemic. Psychology Health Medicine 27: 352–60. [Google Scholar] [CrossRef] [PubMed]
- Schneider, Frank, Martin Härter, and Susanne Schorr. 2017. S3-Leitlinie/Nationale VersorgungsLeitlinie Unipolare Depression. Berlin/Heidelberg: Springer. [Google Scholar]
- Schönthaler, Elena M. D., Nina Dalkner, Michaela Ratzenhofer, Eva Fleischmann, Frederike T. Fellendorf, Susanne A. Bengesser, Armin Birner, Alexander Maget, Melanie Lenger, Martina Platzer, and et al. 2022. Greater Emotional Distress Due to Social Distancing and Greater Symptom Severity during the COVID-19 Pandemic in Individuals with Bipolar Disorder: A Multicenter Study in Austria, Germany, and Denmark. International Journal of Environmental Research and Public Health 19: 7626. [Google Scholar] [CrossRef] [PubMed]
- Seiler, Annina, and Josef Jenewein. 2019. Resilience in cancer patients. Frontiers in Psychiatry 10: 208. [Google Scholar] [CrossRef] [PubMed]
- Setiawati, Yunias, Joni Wahyuhadi, Florentina Joestandari, Margarita M. Maramis, and Atika Atika. 2021. Anxiety and Resilience of Healthcare Workers During COVID-19 Pandemic in Indonesia. Journal of Multidisciplinary Healthcare 14: 1–8. [Google Scholar] [CrossRef] [PubMed]
- Shi, Meng, Li Liu, Ziyue Wang, and Lie Wang. 2015. The mediating role of resilience in the relationship between big five personality and anxiety among Chinese medical students: A cross-sectional study. PLoS ONE 10: e0119916. [Google Scholar] [CrossRef]
- Shin, Young-Chul, Sun Mi Kim, Hyeri Kim, Kyoung Joon Min, Seo-Koo Yoo, Eun-Jin Kim, and Sang Won Jeon. 2019. Resilience as a Protective Factor for Depressive Mood and Anxiety among Korean Employees. Journal of Korean Medical Science 34: e188. [Google Scholar] [CrossRef]
- Shrivastava, Amresh, and Avinash Desousa. 2016. Resilience: A psychobiological construct for psychiatric disorders. Indian Journal of Psychiatry 58: 38–43. [Google Scholar] [CrossRef]
- Smith, P. 2009. Resilience: Resistance factor for depressive symptom. Journal of Psychiatric and Mental Health Nursing 16: 829–37. [Google Scholar] [CrossRef]
- Snaith, R. Philip, Max Hamilton, S. Morley, A. Humayan, D. Hargreaves, and P. Trigwell. 1995. A scale for the assessment of hedonic tone the Snaith–Hamilton Pleasure Scale. The British Journal of Psychiatry 167: 99–103. [Google Scholar] [CrossRef]
- Sood, Amit, Kavita Prasad, Darrell Schroeder, and Prathibha Varkey. 2011. Stress management and resilience training among Department of Medicine faculty: A pilot randomized clinical trial. Journal of General Internal Medicine 26: 858–61. [Google Scholar] [CrossRef]
- Struyf, Thomas, Jonathan J. Deeks, Jacqueline Dinnes, Yemisi Takwoingi, Clare Davenport, Mariska M. G. Leeflang, René Spijker, Lotty Hooft, Devy Emperador, Julie Domen, and et al. 2020. Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVID-19 disease. Cochrane Database of Systematic Reviews 5. [Google Scholar] [CrossRef]
- Stuijfzand, Suzannah, Camille Deforges, Vania Sandoz, Consuela-Thais Sajin, Cecile Jaques, Jolanda Elmers, and Antje Horsch. 2020. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: A rapid review. BMC Public Health 20: 1–18. [Google Scholar] [CrossRef] [PubMed]
- Tso, Winnie W. Y., Rosa S. Wong, Keith T. S. Tung, Nirmala Rao, King Wa Fu, Jason Yam, Gilbert T. Chua, Eric Y. H. Chen, Tatia M. C. Lee, Sherry K. W. Chan, and et al. 2020. Vulnerability and resilience in children during the COVID-19 pandemic. European Child & Adolescent Psychiatry 31: 161–76. [Google Scholar]
- Ungar, Michael. 2008. Resilience across cultures. The British Journal of Social Work 38: 218–35. [Google Scholar] [CrossRef]
- Wagnild, Gail M., and Heather M. Young. 1993. Development and psychometric evaluation of the Resilience Scale. Journal of Nursing Measurement 2: 165–78. [Google Scholar]
- Zanardo, Vincenzo, Valeria Manghina, Lara Giliberti, Michela Vettore, Lorenzo Severino, and Gianluca Straface. 2020. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. International Journal of Gynecology & Obstetrics 150: 184–88. [Google Scholar]
| Are the actual developments around the SARS-CoV-2 pandemic scaring you in any way? | Yes, I am fearing a potential economic crisis. |
| Yes, I am worrying about my health. | |
| Yes, I am worried about the health of my relatives. | |
| Yes, I am fearing for my job. | |
| Yes, for other reasons. | |
| No |
| t1 1 (df = 103) | ||||
| Total Resilience 2 | Competence | Acceptance | ||
| COVID-related fears | r sig. | 0.271 0.005 ** | 0.263 0.007 ** | 0.222 0.023 ** |
| t2 1 (df = 1169) | ||||
| Total Resilience 2 | Competence | Acceptance | ||
| r sig. | −0.137 0.000 ** | −0.120 0.000 ** | −0.145 0.000 ** | |
| t1 1 (df = 103) | ||||
| Total Resilience 2 | Competence | Acceptance | ||
| SHAPS | r sig. | 0.536 0.000 ** | 0.517 0.000 ** | 0.443 0.000 ** |
| t2 1 (df = 1169) | ||||
| Total Resilience 2 | Competence | Acceptance | ||
| r sig. | 0.374 0.000 ** | 0.371 0.000 ** | 0.315 0.000 ** | |
| SHAPS t1 | SHAPS t2 | RS13-Score t1 | RS13-Score t2 | ||
|---|---|---|---|---|---|
| SHAPS t1 | r sig. N | 1 - 1362 | 0.529 1 0.000 187 | 0.365 1 0.000 1362 | 0.187 2 0.011 186 |
| SHAPS t2 | r sig. N | - | 1 - 1138 | 0.216 1 0.003 187 | 0.363 1 0.000 1137 |
| Total Resilience t1 | r sig. N | - | - | 1 - 1362 | 0.616 1 0.000 186 |
| Total Resilience t2 | r sig. N | - | - | - | 1 - 1137 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maget, A.; Lenger, M.; Bengesser, S.A.; Birner, A.; Fellendorf, F.T.; Fleischmann, E.; Lang, J.N.; Platzer, M.; Queissner, R.; Ratzenhofer, M.; et al. Influences of COVID-19 Work-Related Fears and Anhedonia on Resilience of Workers in the Health Sector during the COVID-19 Pandemic. Soc. Sci. 2022, 11, 578. https://doi.org/10.3390/socsci11120578
Maget A, Lenger M, Bengesser SA, Birner A, Fellendorf FT, Fleischmann E, Lang JN, Platzer M, Queissner R, Ratzenhofer M, et al. Influences of COVID-19 Work-Related Fears and Anhedonia on Resilience of Workers in the Health Sector during the COVID-19 Pandemic. Social Sciences. 2022; 11(12):578. https://doi.org/10.3390/socsci11120578
Chicago/Turabian StyleMaget, Alexander, Melanie Lenger, Susanne A. Bengesser, Armin Birner, Frederike T. Fellendorf, Eva Fleischmann, Jorgos N. Lang, Martina Platzer, Robert Queissner, Michaela Ratzenhofer, and et al. 2022. "Influences of COVID-19 Work-Related Fears and Anhedonia on Resilience of Workers in the Health Sector during the COVID-19 Pandemic" Social Sciences 11, no. 12: 578. https://doi.org/10.3390/socsci11120578
APA StyleMaget, A., Lenger, M., Bengesser, S. A., Birner, A., Fellendorf, F. T., Fleischmann, E., Lang, J. N., Platzer, M., Queissner, R., Ratzenhofer, M., Schönthaler, E., Tmava-Berisha, A., Trojak, R. M., Dalkner, N., & Reininghaus, E. Z. (2022). Influences of COVID-19 Work-Related Fears and Anhedonia on Resilience of Workers in the Health Sector during the COVID-19 Pandemic. Social Sciences, 11(12), 578. https://doi.org/10.3390/socsci11120578






