Intersections of Immigration and Sexual/Reproductive Health: An Umbrella Literature Review with a Focus on Health Equity
Abstract
1. Introduction
- -
- Public health considerations relates to the effect of migration on population health. Poor management of migration can lead to lower utilization of healthcare. The reasons for this are mostly associated with the unresolved legal status of the migrant, poor working conditions, and/or insufficient information, etc. Ultimately, this is reflected on public health, e.g., untreated communicable diseases carry the risk of spread, while undiagnosed and untreated chronic conditions may result in ill health and higher costs. One of the most prominent examples is the natural experiment that resulted from a set of policy changes in Germany in the period 1994–2013. The results indicated that it is less costly to allow refugees and asylum-seekers access to healthcare then to exclude them (Bozorgmehr and Razum 2015).
- -
- Economic contributions: 17% of doctors and 6% of nurses in the Organisation for Economic Co-operation and Development (OECD) countries have been trained abroad. During the COVID-19 pandemic, migrant workers provided an immense contribution by being on the frontline of the crises, with one in four medical doctors, one in six nurses, and more than 30% of key workforce being migrants (OECD 2020; Vearey et al. 2020). An inclusive health system is critical to sustain the health of workers and supporting their participation in the labor market.
- -
- Social integration and cohesion provides an inclusive healthcare system recognized as one of the policies for social integration of migrants (Ledoux et al. 2018).
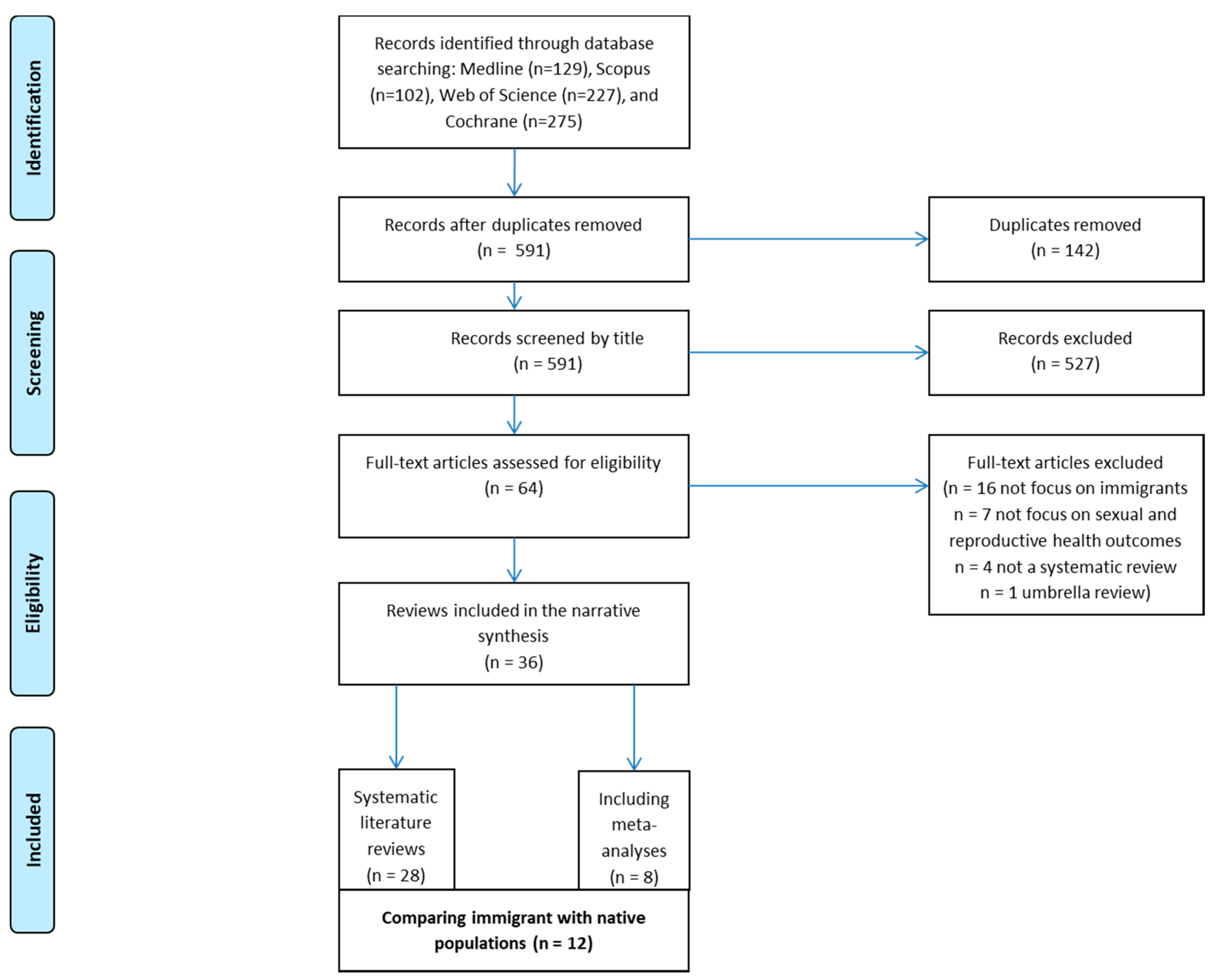
2. Methods
2.1. Design
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Study Selection and Data Extraction
2.5. Quality Appraisal and Data Synthesis
3. Results
3.1. Who Is Being Studied?
3.2. How Is It Being Studied?
3.3. What Is Being Studied?
3.4. Social-Structural Domain
3.5. Sexual Health Domain
3.6. Reproductive Health Domain
3.7. Interventions for Promoting SRH and Gender Equality
4. Discussion
4.1. Strengths and Limitation of the Research
4.2. Recommendations for Research and Action
- -
- To improve identification of migrants at increased risk for poor SRH outcomes.
- -
- To implement multi- and inter-sectorial interventions, to fulfil the specific needs of increasingly heterogeneous populations, namely poverty, discrimination, and exclusion.
- -
- To provide culturally sensitive healthcare that adjusts its provisions to cultural differences.
- -
- To ensure that the healthcare system is easily accessible to migrants by promoting accessibility on the same terms as the general population.
- -
- To improve patient-care provider communication that provides interpreting and translation assistance.
- -
- Provide equitable SRH treatment of migrants by designing programs that offer partnerships between the doctor and the patients, as well as between the healthcare and minority community.
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Alhasanat, Dalia, and Carmen Giurgescu. 2017. Depressive Symptoms among Hispanic Women in the United States: Systematic Review’Depressive Symptoms among Hispanic Women in the United States: Systematic Review. MCN The American Journal of Maternal/Child Nursing. [Google Scholar] [CrossRef] [PubMed]
- Almeida, Lígia Moreira, José Caldas, Diogo Ayres-de-Campos, Dora Salcedo-Barrientos, and Sónia Dias. 2013. Maternal healthcare in migrants: A systematic review. Maternal and Child Health Journal 17: 1346–54. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Del Arco, Debora, Susana Monge, Amaya Azcoaga, Isabel Rio, Victoria Hernando, Cristina Gonzalez, Belen Alejos, Ana Maria Caro, Santiago Perez-Cachafeiro, Oriana Ramirez-Rubio, and et al. 2013. HIV testing and counselling for migrant populations living in high-income countries: A systematic review. European Journal of Public Health. [Google Scholar] [CrossRef] [PubMed]
- Anderson, Fraser M., Stephani L. Hatch, Carla Comacchio, and Louise M. Howard. 2017. Prevalence and risk of mental disorders in the perinatal period among migrant women: A systematic review and meta-analysis. Archives of Women’s Mental Health 20: 449–62. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, Katrina, Karima L. Ravenell, Suzanne McMurphy, and Mary Putt. 2007. Racial/ethnic differences in physician distrust in the United States. American Journal of Public Health 97: 1283–89. [Google Scholar] [CrossRef]
- Balaam, Marie-Clare, Kristin Akerjordet, Anne Lyberg, Barbara Kaiser, Eva Schoening, Anne-Mari Fredriksen, Angelica Ensel, Olga Gouni, and Elisabeth Severinsson. 2013. A qualitative review of migrant women’s perceptions of their needs and experiences related to pregnancy and childbirth. Journal of Advanced Nursing. [Google Scholar] [CrossRef] [PubMed]
- Barnes, Erin Frances, Alejandra Saraí Dominguez, and Isabel Jazmín González. 2013. Sexual health interventions targeting Mexican migrants: A review. International Journal of Migration, Health and Social Care. [Google Scholar] [CrossRef]
- Blondell, Sarah J., Bryony Kitter, Mark P. Griffin, and Jo Durham. 2015. Barriers and Facilitators to HIV Testing in Migrants in High-Income Countries: A Systematic Review. AIDS and Behavior. [Google Scholar] [CrossRef]
- Bollini, Paola, Sandro Pampallona, Philippe Wanner, and Bruce Kupelnick. 2009. Pregnancy outcome of migrant women and integration policy: A systematic review of the international literature. Social Science and Medicine. [Google Scholar] [CrossRef]
- Bozorgmehr, Kayvan, and Oliver Razum. 2015. Effect of restricting access to health care on health expenditures among asylum-seekers and refugees: A quasi-experimental study in Germany, 1994–2013. PLoS ONE 10: e0131483. [Google Scholar] [CrossRef]
- Carling, Jørgen. 2020. Explaining the Meaning of Migrants and Refugees. Available online: https://meaningofmigrants.org/ (accessed on 14 December 2020).
- Cooke, Alison, Debbie Smith, and Andrew Booth. 2012. Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qualitative Health Research 22: 1435–43. [Google Scholar] [CrossRef] [PubMed]
- De Jong, Lea, Milena Pavlova, Marjolein Winters, and Bernd Rechel. 2017. A systematic literature review on the use and outcomes of maternal and child healthcare services by undocumented migrants in Europe. European Journal of Public Health. [Google Scholar] [CrossRef] [PubMed]
- Denize, Kathryn M., Nina Acharya, Stephanie A. Prince, Danilo Fernandes da Silva, Alysha LJ Harvey, Zachary M. Ferraro, and Kristi B. Adamo. 2018. Addressing cultural, racial and ethnic discrepancies in guideline discordant gestational weight gain: A systematic review and meta-analysis. PeerJ. [Google Scholar] [CrossRef] [PubMed]
- Du, Hongfei, and Xiaoming Li. 2015. Acculturation and HIV-related sexual behaviours among international migrants: A systematic review and meta-analysis. Health Psychology Review. [Google Scholar] [CrossRef]
- Dune, Tinashe, Janette Perz, Zelalem Mengesha, and David Ayika. 2017. Culture Clash? Investigating constructions of sexual and reproductive health from the perspective of 1.5 generation migrants in Australia using Q methodology. Reproductive Health 14: 50. [Google Scholar] [CrossRef] [PubMed]
- Dzomba, Armstrong, Andrew Tomita, Kaymarlin Govender, and Frank Tanser. 2019. Effects of Migration on Risky Sexual Behavior and HIV Acquisition in South Africa: A Systematic Review and Meta-analysis, 2000–2017. AIDS and Behavior. [Google Scholar] [CrossRef]
- ECDC. 2020. Guidance on Infection Prevention and Control of COVID-19 in Migrant and Refugee Reception and Detention Centres in the EU/EEA and the UK. Available online: https://www.ecdc.europa.eu/en/publications-data/covid-19-guidance-prevention-control-migrant-refugee-centres (accessed on 2 February 2021).
- Evans, Tim, and Hilary Brown. 2003. Road traffic crashes: Operationalizing equity in the context of health sector reform. Inj Control Saf Promot 10: 11–2. [Google Scholar] [CrossRef] [PubMed]
- Fakoya, Ibidun, Débora Álvarez-del Arco, Melvina Woode-Owusu, Susana Monge, Yaiza Rivero-Montesdeoca, Valerie Delpech, Brian Rice, Teymur Noori, Anastasia Pharris, Andrew J. Amato-Gauci, and et al. 2015. A systematic review of post-migration acquisition of HIV among migrants from countries with generalised HIV epidemics living in Europe: Implications for effectively managing HIV prevention programmes and. BMC Public Health. [Google Scholar] [CrossRef]
- Gagnon, Anita J., Meg Zimbeck, Jennifer Zeitlin, and Roam Collaboration. 2009. Migration to western industrialised countries and perinatal health: A systematic review. Social Science and Medicine. [Google Scholar] [CrossRef]
- Gagnon, Anita J., Meg Zimbeck, and Jennifer Zeitlin. 2010. Migration and perinatal health surveillance: An international Delphi survey. European Journal of Obstetrics and Gynecology and Reproductive Biology 149: 37–43. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, Sajana, Jonathan Hallett, Corie Gray, Roanna Lobo, and Gemma Crawford. 2019. What works? Prevention and control of sexually transmitted infections and blood-borne viruses in migrants from sub-saharan Africa, Northeast Asia and Southeast Asia living in high-income countries: A systematic review. International Journal of Environmental Research and Public Health. [Google Scholar] [CrossRef]
- Gissler, Mika, Sophie Alexander, Alison MacFarlane, Rhonda Small, Babill Stray-Pedersen, Jennifer Zeitlin, Megan Zimbeck, Anita Gagnon, and Roam Collaboration (Reproductive Outcomes and Migration: An International Research Collaboration). 2009. Stillbirths and infant deaths among migrants in industrialized countries. Acta Obstetricia et Gynecologica Scandinavica. [Google Scholar] [CrossRef] [PubMed]
- Greenaway, Christina, Sally Hargreaves, Sapha Barkati, Christina M. Coyle, Federico Gobbi, Apostolos Veizis, and Paul Douglas. 2020. COVID-19: Exposing and addressing health disparities among ethnic minorities and migrants. Journal of Travel Medicine, 1–3. [Google Scholar] [CrossRef]
- Heaman, Maureen, Hamideh Bayrampour, Dawn Kingston, Béatrice Blondel, Mika Gissler, Carolyn Roth, S. Alexander, and A. Gagnon. 2013. Migrant women’s utilization of prenatal care: A systematic review. Maternal and Child Health Journal. [Google Scholar] [CrossRef] [PubMed]
- Higginbottom, Gina M. A., Myfanwy Morgan, Mirande Alexandre, Yvonne Chiu, Joan Forgeron, Deb Kocay, and Rubina Barolia. 2015. Immigrant women’s experiences of maternity-care services in Canada: A systematic review using a narrative synthesis. Systematic Reviews. [Google Scholar] [CrossRef] [PubMed]
- Hu, Yang. 2020. Intersecting ethnic and native–migrant inequalities in the economic impact of the COVID-19 pandemic in the UK. Research in Social Stratification and Mobility 68: 100528. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, John P. A. 2009. Integration of evidence from multiple meta-analyses: A primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ 181: 488–93. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, John. 2017. Next-generation systematic reviews: Prospective meta-analysis, individual-level data, networks and umbrella reviews. British Journal of Sports Medicine, 1456–58. [Google Scholar] [CrossRef]
- IOM. 2019. Glossary on Migration N° 34. Available online: www.iom.int (accessed on 14 December 2020).
- Ivanova, Olena, Masna Rai, and Elizabeth Kemigisha. 2018. A systematic review of sexual and reproductive health knowledge, experiences and access to services among refugee, migrant and displaced girls and young women in Africa. International Journal of Environmental Research and Public Health. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh, Josephine, Oliver Sandy, and Theo Lorenc. 2008. Reflections on developing and using PROGRESS-Plus. Equity Update 2: 1–3. [Google Scholar]
- Kyung Kim, Sun, Seyeon Park, and Sukhee Ahn. 2017. Effectiveness of Psychosocial and Educational Prenatal and Postnatal Care Interventions for Married Immigrant Women in Korea: Systematic Review and Meta-analysis. Asia-Pacific Journal of Public Health 29: 351–66. [Google Scholar] [CrossRef] [PubMed]
- Ledoux, Céline, Eva Pilot, Esperanza Diaz, and Thomas Krafft. 2018. Migrants’ access to healthcare services within the European Union: A content analysis of policy documents in Ireland, Portugal and Spain. Globalization and Health 14: 57. [Google Scholar] [CrossRef] [PubMed]
- Llácer, Alicia, María Victoria Zunzunegui, Julia Del Amo, Lucía Mazarrasa, and Francisco Bolůmar. 2007. The contribution of a gender perspective to the understanding of migrants’ health. Journal of Epidemiology and Community Health 61: ii4–ii10. [Google Scholar] [CrossRef] [PubMed]
- Loganathan, Tharani, Zhie X. Chan, Allard W. de Smalen, and Nicola S. Pocock. 2020. Migrant women’s access to sexual and reproductive health services in Malaysia: A qualitative study. International Journal of Environmental Research and Public Health 17: 1–18. [Google Scholar] [CrossRef] [PubMed]
- Maria da Conceição, F. Santiago, and Maria Henriqueta Figueiredo. 2015. Immigrant women’s perspective on prenatal and postpartum care: Systematic review. Journal of Immigrant and Minority Health Center for Minority Public Health. [Google Scholar] [CrossRef]
- Michael Marmot, Jessica Allen, Peter Goldblatt, Eleanor Herd, and Joana Morrison. 2020. Build Back Fairer: The COVID-19 Marmot Review. The Pandemic, Socioeconomic and Health Inequalities in England. London: Institute of Health Equity. [Google Scholar]
- Mengesha, Zelalem Birhanu, Tinashe Dune, and Janette Perz. 2016. Culturally and linguistically diverse women’s views and experiences of accessing sexual and reproductive health care in Australia: A systematic review. Sexual Health 13: 299–310. [Google Scholar] [CrossRef] [PubMed]
- Merry, Lisa, Rhonda Small, Béatrice Blondel, and Anita J. Gagnon. 2013. International migration and caesarean birth: A systematic review and meta-analysis. BMC Pregnancy and Childbirth. [Google Scholar] [CrossRef] [PubMed]
- Metusela, Christine, Jane Ussher, Janette Perz, Alexandra Hawkey, Marina Morrow, Renu Narchal, Jane Estoesta, and Melissa Monteiro. 2017. “In My Culture, We Don’t Know Anything About That”: Sexual and Reproductive Health of Migrant and Refugee Women. International Journal of Behavioral Medicine 24: 836–45. [Google Scholar] [CrossRef] [PubMed]
- Michalopoulos, Lynn Murphy, Angela Aifah, and Nabila El-Bassel. 2016a. A Systematic Review of HIV Risk Behaviors and Trauma among Forced and Unforced Migrant Populations from Low and Middle-Income Countries: State of the Literature and Future Directions. AIDS and Behavior. [Google Scholar] [CrossRef] [PubMed]
- Michalopoulos, Lynn Murphy, Angela Aifah, and Nabila El-Bassel. 2016b. Racial/Ethnic Disparities in Antenatal Depression in the United States: A Systematic Review. Maternal and Child Health Journal. [Google Scholar] [CrossRef]
- Mukherjee, Soumyadeep, Mary Jo Trepka, Dudith Pierre-Victor, Raed Bahelah, and Tenesha Avent. 2016. Racial/Ethnic Disparities in Antenatal Depression in the United States: A Systematic Review. Maternal and Child Health Journal 20: 1780–97. [Google Scholar] [CrossRef]
- Nilaweera, Irosha, Frances Doran, and Jane Fisher. 2014. Prevalence, nature and determinants of postpartum mental health problems among women who have migrated from South Asian to high-income countries: A systematic review of the evidence. Journal of Affective Disorders. [Google Scholar] [CrossRef]
- OECD. 2020. COVID-19 Crisis Puts Migration and Progress on Integration at Risk. Available online: https://www.oecd.org/migration/covid-19-crisis-puts-migration-and-progress-on-integration-at-risk.htm (accessed on 13 December 2020).
- O’Neill, Jennifer, Hilary Tabish, Vivian Welch, Mark Petticrew, Kevin Pottie, Mike Clarke, Tim Evans, Jordi Pardo Pardo, Elizabeth Waters, Howard White, and et al. 2014. Applying an equity lens to interventions: Using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. Journal of Clinical Epidemiology 67: 56–64. [Google Scholar] [CrossRef] [PubMed]
- Platt, Lucy, Pippa Grenfell, Adam Fletcher, Annik Sorhaindo, Emma Jolley, Tim Rhodes, and Chris Bonell. 2013. Systematic review examining differences in HIV, sexually transmitted infections and health-related harms between migrant and non-migrant female sex workers. Sexually Transmitted Infections. [Google Scholar] [CrossRef]
- Rade, Donna Angelina, Gemma Crawford, Roanna Lobo, Corie Gray, and Graham Brown. 2018. Sexual Health Help-Seeking Behavior among Migrants from Sub-Saharan Africa and South East Asia living in High Income Countries: A Systematic Review. International Journal of Environmental Research and Public Health 15: 1311. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, Scott D., Kenneth C. Hergenrather, Aimee Wilkin, Jose Alegría-Ortega, and Jaime Montaño. 2006. Preventing HIV infection among young immigrant Latino men: Results from focus groups using community-based participatory research. Journal of the National Medical Association 98: 564–73. [Google Scholar] [PubMed]
- Scamell, Mandie, and Aliyha Ghumman. 2019. The experience of maternity care for migrant women living with female genital mutilation: A qualitative synthesis. Birth. [Google Scholar] [CrossRef]
- Shea, Beverley J., Barnaby C. Reeves, George Wells, Micere Thuku, Candyce Hamel, Julian Moran, David Moher, Peter Tugwell, Vivian Welch, Elizabeth Kristjansson, and et al. 2017. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomized or non-randomised studies of healthcare interventions, or both. BMJ 358: j4008. [Google Scholar] [CrossRef]
- Small, Rhonda, Carolyn Roth, Manjri Raval, Touran Shafiei, Dineke Korfker, Maureen Heaman, Christine McCourt, and Anita Gagnon. 2014. Immigrant and non-immigrant women’s experiences of maternity care: A systematic and comparative review of studies in five countries. BMC Pregnancy and Childbirth 14: 152. [Google Scholar] [CrossRef] [PubMed]
- Tai, Don Bambino Geno, Aditya Shah, Chyke A. Doubeni, Irene G. Sia, and Mark L. Wieland. 2020. The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. Clinical Infectious Diseases. [Google Scholar] [CrossRef]
- Thomas, Samantha L., and Stuart D. M. Thomas. 2004. Displacement and health. British Medical Bulletin 69: 115–27. [Google Scholar] [CrossRef]
- Tulloch, Olivia, Fortunate Machingura, and Claire Melamed. 2016. Health, Migration and the 2030 Agenda for Sustainable Development. London: Overseas Development Institute (ODI). Available online: https://www.odi.org/sites/odi.org.uk/files/resource-documents/10761.pdf (accessed on 2 February 2021).
- Turkmani, Sabera, Caroline S. E. Homer, and Angela Dawson. 2019. Maternity care experiences and health needs of migrant women from female genital mutilation–practicing countries in high-income contexts: A systematic review and meta-synthesis. Birth 46: 3–14. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. 2014. The Gap Report. Available online: https://www.unaids.org/en/resources/documents/2014/20140716_UNAIDS_gap_report (accessed on 14 December 2020).
- UNFPA. 2011. Socio-Cultural Influences on the Reproductive Health of Migrant Women. New York: UNFPA. [Google Scholar]
- UNSDSN. 2020. Indicators and a Monitoring Framework. Available online: https://indicators.report/targets/3-7/ (accessed on 14 December 2020).
- Urquia, Marcelo Luis, Richard Henry Glazier, Beatrice Blondel, Jennifer Zeitlin, Mika Gissler, Alison Macfarlane, Edward Ng, Maureen Heaman, Babill Stray-Pedersen, and Anita J. Gagnon. 2010. International migration and adverse birth outcomes: Role of ethnicity, region of origin and destination. Journal of Epidemiology and Community Health. [Google Scholar] [CrossRef] [PubMed]
- Vearey, J. O., C. Hui, and K. Wickramage. 2020. World Migration Report 2020. Chapter 7—Migration and Health: Current Issues, Governance and Knowledge Gaps. Geneva: International Organization for Migration. Available online: https://publications.iom.int/system/files/pdf/wmr_2020_en_ch_7.pdf (accessed on 2 February 2021).
- Villalonga-Olives, E., I. Kawachi, and N. von Steinbüchel. 2017. Pregnancy and Birth Outcomes among Immigrant Women in the US and Europe: A Systematic Review. Journal of Immigrant and Minority Health. [Google Scholar] [CrossRef]
- Weine, Stevan M., and Adrianna B. Kashuba. 2012. Labor migration and HIV risk: A systematic review of the literature. AIDS and Behavior. [Google Scholar] [CrossRef] [PubMed]
- Welch, Vivian, Mark Petticrew, Peter Tugwell, David Moher, Jennifer O’Neill, Elizabeth Waters, Howard White, and PRISMA-Equity Bellagio Group. 2012. PRISMA-Equity 2012 Extension: Reporting Guidelines for Systematic Reviews with a Focus on Health Equity. PLoS Medicine 9: e1001333. [Google Scholar] [CrossRef] [PubMed]
- WHO. 2006. Defining Sexual Health: Report of a Technical Consultation on Sexual Health, 28–31 January 2002. Geneva: WHO. [Google Scholar]
- WHO. 2016. Action Plan for Sexual and Reproductive Health: Towards Achieving the 2030 Agenda for Sustainable Development in Europe—Leaving No One Behind. Copenhagen: WHO. [Google Scholar]
- Williamson, Elizabeth J., Alex J. Walker, Krishnan Bhaskaran, Seb Bacon, Chris Bates, Caroline E. Morton, Helen J. Curtis, Amir Mehrkar, David Evans, Peter Inglesby, and et al. 2020. Factors associated with COVID-19-related death using OpenSAFELY. Nature 584: 430–36. [Google Scholar] [CrossRef] [PubMed]
- Winn, Anika, Erin Hetherington, and Suzanne Tough. 2017. Systematic Review of Immigrant Women’s Experiences with Perinatal Care in North America. JOGNN Journal of Obstetric, Gynecologic, and Neonatal Nursing. [Google Scholar] [CrossRef] [PubMed]
- Yu, Juping. 2010. Young people of Chinese origin in western countries: A systematic review of their sexual attitudes and behaviour. Health and Social Care in the Community. [Google Scholar] [CrossRef]
| Sample | Men and women in reproductive age (both migrants and natives) |
| Phenomenon of interest | Social, cultural, and structural factors influencing sexual and reproductive health |
| Design | Systematic literature reviews and meta-analyses of any research type. No publication date restrictions. No restrictions on country and location. No language exclusions |
| Evaluation | Any sexual and reproductive health or health inequity outcomes |
| Research type | Systematic literature reviews or meta-analyses |
| Author, Date | Number of Individual Papers Included in the Review | Year of Publication (Range) | Continents of Destination | Continents of Origin | Methods | Population Included | Search Strategy Conducted in the Paper (Databases and Supplementary Searches) |
|---|---|---|---|---|---|---|---|
| Anderson et al. 2017 | 53 | 1986–2015 | North America (United States, Canada), and Australia | NR | Quantitative with meta-analysis | Migrant women (including refugees and asylum-seekers versus non-migrant women | PsycINFO, CINAHL, EMBASE, MEDLINE, Maternal and Infant Care and Cochrane Register of Controlled Trials (CENTRAL). Supplementary searches: Backward and forward citation tracking of papers included |
| Bollini et al. 2009 | 65 | 1966–2004 | Europe (mostly United Kingdom and France) | NR | Quantitative | Migrant women in European countries versus native women | Medline. Supplementary searches: reference list |
| Denize et al. 2018 | 86 | 1963–2018 | North America (mostly United States), Europe, Asia, and Africa | NR | Quantitative with meta-analysis | Pregnant women with different ethnicity/nationality/race/language/immigration status | Ovid MEDLINE; EMBASE; Clinicaltrials.gov; Cochrane Central Register of Controlled Trials; CINAHL; PsycINFO; Sociological Abstracts; Literature Latino-Americana e do Caribe em Ciencias da Saude (LILACS), IBECS; and Cuba Medicina (CUMED). Supplementary searches: Canadian Agency for Drugs and Technologies in Health (CADTH’s) Grey matters and citations of relevant systematic reviews and trials |
| Dzomba et al. 2019 | 29 | 2000–2017 | South Africa | NR | Quantitative with meta-analysis | Male and female migrants in South Africa compared to their non-migrant counterparts | PubMed Central, Sage Publications, Google Scholar, Web of Science, and J-STOR. Supplementary searches: contents of specific journals and citing articles |
| Gagnon et al. 2009 | 133 | 1995–2008 | North America, Europe and Australia | NR | Quantitative with meta-analysis | International migrant women versus native-born women of the receiving countries | Medline, Health Star, Embase, and PsychInfo. Additional searches: reference list |
| Gissler et al. 2009 | 34 | 1983–2002 | North America (United States) and Europe (Italy, Norway, The Netherlands, Serbia, Croatia, Sweden, Belgium, Spain) | Japan, North Africa, Pacific Islands, Mexico, Surinam/Antilles, Republic of Serb Krajina and Serb Republic, Morocco, Turkey, Suriname, Antilles | Quantitative | International migrant or refugee women versus native-born women of the receiving countries | Medline, Health Star, Embase, and PsychInfo. Supplementary searches: reference list |
| Heaman et al. 2013 | 29 | 1996–2010 | North America (mostly United States) and Europe | NR | Quantitative | Women who migrated to Western industrialized countries versus non-migrant women | Medline, Embase, and PsychInfo. Supplementary searches: an existing database of the Reproductive Outcomes and Migration international research collaboration, known experts, and reference list |
| Merry et al. 2013 | 76 | 1956–2010 | Europe (68%), Australia (11%), the US (11%), Canada (6%), and Israel (4%) | Latin America and Caribbean (39%) ‘origin unspecified’ (11%), and South Asia (7%) | Quantitative with meta-analysis | International migrant women versus native-born women of the receiving countries | Embase, PsycInfo, CINAHL, Medline, Health Star, Sociological Abstracts, Web of Science, Proquest Research Library, Proquest Dissertations and Theses, POPLINE, Global Health, and PAIS. Supplementary searches: reference list, website searches and contact with authors |
| Platt et al. 2013 | 26 | 1985–2009 | Europe, Australia, Southeast Asia, Sub-Saharan Africa, Central, and South America | Europe, South America, and Asia | Narrative synthesis | Migrant versus non-migrant female sex workers | Social Science Citation Index, Medline, Embase, Popline, CINAHL, Global Health, African Healthline, Index Medicus for the Eastern European Region, Latin American and Caribbean Centre on Health Sciences Information, Index Medicus of the South-East Asian Region, and Western Pacific Region of the Index Medicus. |
| Small et al. 2014 | 34 | 1990–2012 | Australia, North America, and Europe | Asia, America | Mixed methods | Migrant (or refugee) and non-immigrant women | Medline, CINAHL, Health Star, Embase and PsychInfo. Supplementary searches: undefined sources |
| Urquia et al. 2010 | 24 | 1996–2006 | North America (United States) and Europe | NR | Quantitative with meta-analysis | International migrant women versus native-born women of the receiving countries | Medline, Health Star, Embase, and PsychInfo. Supplementary searches: reference list and relevant articles referred to the authors |
| Villalonga-Olives et al. 2017 | 68 | 1964–2011 | North America (United States) and Europe | NR | Qualitative | Migrant women | Pubmed and Embase. |
| Author, Date (Type of Review) | Review Aim | SRH Outcomes | Determinants/PROGRESS-PLUS | Overall Results of the Review | Overall Limitations of the Study | Overall Recommendations of the Study |
|---|---|---|---|---|---|---|
| Anderson et al. 2017 (MA) | To evaluate the prevalence and risk of mental disorders in the perinatal period among migrant women | Perinatal mental health |
| No evidence for an overall increased risk of antenatal or postnatal depression among migrant women compared to non-migrant women was found. Migrant women in Canada were at increased risk of antenatal and postnatal depression compared to native-born, whereas migrant women in America and Australia were not. | There were no studies conducted in low- and middle-income countries, which reduces generalizability. Only English language papers were included. Lack of high-quality studies, as most studies had risk of selection and measurement bias. |
|
| Bollini et al. 2009 (SLR) | To make a synthesis of available evidence on the association between pregnancy outcomes and integration policies | Pregnancy/birth outcomes |
| Migrant women are clearly disadvantaged as compared to native women, their pregnancies ending up significantly more frequently with unfavorable outcomes. In countries where a definite effort to establish strong integration policies has been made, there is a sizeable significant reduction in the gap between native and migrant women. Overall, living in a country with a strong integration policy represented a powerful protective factor for adverse pregnancy outcomes. | Collapsing all migrant groups into a single category of migrants may obscure the differences existing among ethnic groups. |
|
| Denize et al. 2018 (MA) | To systematically review the literature and describe the discrepancies in achieving the 2009 Institute of Medicine (IOM) gestational weight gain (GWG) guidelines across cultures. | (1) Inadequate or excessive GWG, as defined by the IOM; (2) maternal-fetal health outcomes (such as large-for-gestational-age, macrosomia, gestational diabetes mellitus, and all pregnancy-induced hypertension disorders). |
| Most women experienced discordant GWG; this was culturally dependent, wherein minority groups such as black, Hispanic and Asian women are more likely to gain below current recommendations, and Caucasian women to exceed them. Studies among Black women indicated they were at risk of both inadequate and excessive GWG. Less acculturated women (mainly to the US), were at a greater risk of inadequate GWG. | 87% of the included articles were carried out in North America (especially the US), most of which compared a small number of racial/ethnic groups (Black, White, Hispanic and Asian).The limited literature present on cultural differences in secondary outcomes did not provide clear trends of which groups are more at risk of pregnancy-related complications than others. |
|
| Dzomba et al. 2019 (MA) | To understand the role of migration in HIV risk acquisition and sexual behavior | Risk of HIV acquisition; unprotected sexual intercourse; sex work |
| Mobility is highly associated with increased prevalence of HIV risk behaviors and confers up to 69% increase in the risk of HIV acquisition. Studies included in this review documented increased multiple sexual partnering, unprotected sexual intercourse, visiting sex workers and engaging in sex work in migrants compared to non-migrants. Escalation of this sexual behaviour and risk of HIV acquisition among migrants in comparison to non-migrants calls for increased reliance on the targeted and best-combination HIV prevention strategies. | Several the existing studies examining multiple partnering did not collect data on the characteristics of the sexual partnerships, such as the length of overlaps between and the type of sexual partners. This information is particularly important in determining transmission during concurrent partnerships |
|
| Gagnon et al. 2009 (MA) | To understand why migrant women have poorer perinatal health outcomes than receiving country women | Perinatal health outcomes (preterm birth, low birthweight and health-promoting behavior) | (1) Place of origin | Being a migrant was not a consistent marker of risk of poorer perinatal health outcomes; migrants did as well as or better than host-county women for all outcomes in a large proportion of studies. However, Asian, North-, and other-African migrants were at greater perinatal health risk than their receiving-country counterparts in the small number of studies that could be included in meta-analyses for each subgroup. | Insufficient data to do a meta-analysis by receiving country. Despite the large number of studies of migration and perinatal health, only limited data were available to shed light on why certain groups of migrants were at higher risk. There is an absence of data on other key notions correlated with migration, such as language ability, length of time in receiving country or immigration status. |
|
| Gissler et al. 2009 (SLR) | To determine (1) if migrants in western industrialized countries have higher risks of stillbirth, neonatal mortality, or infant mortality, (2) if there are migrant sub-groups at potentially higher risk, and (3) explanations for risk differences found. | Feto-infant mortality including stillbirths, early neonatal deaths (a death occurring 0–6 days after birth), perinatal deaths (stillbirths and early neonatal deaths), neonatal deaths (a death occurring 0–27 days) and infant deaths (a death occurring 0–364 days) |
| Mortality risk among migrant babies born is not consistently higher, but appears to be greatest among refugees, non-European migrants to Europe, and foreign-born blacks in the US. | Limitations in the available data on potentially important risk factors. |
|
| Heaman et al. 2013 (SLR) | To determine whether migrant women in Western industrialized countries have higher odds of inadequate prenatal care (PNC) compared to receiving-country women | Prenatal care access; health disparities between migrants and non-migrants |
| Migrant women were more likely to receive inadequate PNC than receiving-country women. The odds of inadequate PNC were greater among migrant women younger than 20 years, multiparous, single, with poor or fair language proficiency, less than 5 years of education, unplanned pregnancy, and no health insurance. | Most included studies (70%) were from the US. A consistent definition of inadequate PNC was missing. Another limitation was the comparison groups used in the included studies: most US studies used white receiving-country-born women as the comparison group, while the European studies usually used all country-born women. In addition, studies did not control consistently for potential confounders. |
|
| Merry et al. 2013 (MA) | To determine if migrants in Western industrialized countries have different rates of caesarean than host-country-born women and to identify associated factors | Caesarean rates disparities between migrants and non-migrants; birth outcomes |
| Meta-analyses revealed consistently higher overall caesarean rates for Sub-Saharan African, Somali, and South Asian women; higher emergency rates for North African/West Asian and Latin American women; and lower overall rates for Eastern European and Vietnamese women. Evidence to explain the consistently different rates was limited. Frequently postulated risk factors for caesarean included: language/communication barriers, low SES, poor maternal health, gestational diabetes /high BMI, feto-pelvic disproportion, and inadequate prenatal care. | The web searches, although extensive, did not include all the government and professional agency websites from all OECD countries. Most included studies were rated as ‘fair’ quality for not controlling for confounding or due to some ambiguity in their definitions of the study groups. There was heterogeneity for the meta-analysis due to variation in the migrant populations studied or how source countries were grouped to represent regions. |
|
| Platt et al. 2013 (SLR) | To assess the evidence of differences in the risk of HIV, sexually transmitted infections (STI), and health-related behaviors between migrant and non-migrant female sex workers (FSWs). | HIV, STIs, and risk behavior (practicing of anal sex with clients and accepting of extra money for unprotected sex, vaginal douching with an over the counter medication, undergoing a cervical smear test, termination, and use of contraceptives, use of alcohol or illegal drugs). |
| The lack of consistent differences in risk between migrants and non-migrants highlights the importance of the local context in mediating risk among migrant female sexual workers. The higher prevalence of HIV among some FSWs originating from African countries is likely to be due to infection at home where HIV prevalence is high. | Search was limited to literature written in English. Lack of a standardized definition of sex work. Similarly, inconsistency in the behavioral outcomes and the wide range of STI outcomes reported prevented any meta-analysis. |
|
| Small et al. 2014 (SLR) | To compare what it is known about migrant and non-migrant women’s experiences of maternity care | Migrant women’s experiences of maternity care (overall expectations regarding maternity care: pregnancy care, intrapartum care, postpartum care) | Migrant women vs. non-migrant women | Migrant and non-migrant women desire similar things from maternity care: safe, high quality, attentive and individualized care, with adequate information and support. Migrant women are less positive about their care than non-migrant women. Lack of familiarity with care systems and communication problems impacted negatively on migrant women’s experiences, as did perceptions of discrimination and disrespectful care. In sum, women want: Q = Quality care that promotes wellbeing for mothers and babies with a focus on individual needs. U = Unrushed caregivers with enough time to give information, explanations and support. I = Involvement in decision-making about care and procedures. C = Continuity of care with caregivers who get to know and understand women’s individual needs and who communicate effectively. K = Kindness and respect. | Globally, relatively few countries have undertaken population-based studies of women’s experiences of their maternity care. Of these, only the Canadian study has used a multi-language strategy in an attempt to address the under-representativeness of migrant women in population studies, and the Australian research involved a companion study of three migrant groups in tandem with one of the three population surveys undertaken there. Recent waves of migration in the European Union and of refugee and asylum-seeking arrivals are not yet well represented. |
|
| Urquia et al. 2010 (SLR) | To clarify the relation between migration and these birth outcomes by determining the differences in low birth weight (LBW) and preterm birth (PTB) between migrants and non-migrants by migrant subgroups | Birth outcomes disparities between migrants and non-migrants; international disparities of prenatal healthcare |
| The association between foreign-born status and birth outcomes varies according to the migrant subgroup, either defined by a combination of maternal race/ethnicity and migrant status or by the world region of origin and actual destination. Sub-Saharan African and Latin-American and Caribbean migrants were at higher odds of LBW in Europe but not in the USA, and south-central Asians were at higher odds in both continents. | As the social and historical complexity involved in each migrant population was not explored in a meta-analysis, findings should be regarded as global tendencies which may not apply to migrant subgroups settling countries, regions, or cities. Another potential source of bias results from self-reported race/ethnicity and country of birth and nationality in birth certificates. |
|
| Villalonga-Olives et al. 2017 (SLR) | To review the literature regarding health and migration in US and Europe to observe which features can influence reproductive health outcomes among migrants | Pregnancy outcomes; migrant health disparities between US and Europe |
| The differences in migrant health between the US and Europe could be due to US migrants being typically labor migrants, although this is a changing aspect, while migrants in Europe are more heterogeneous. The social environment of the receiving country is an important factor for health outcomes, but also the migration regime, meaning certain people arriving in migration waves (like refugees) could have poorer health outcomes. | US articles study health related outcomes of Latinos and do not consider the reasons for migration, which makes the comparisons between countries more difficult. | There is a need to understand migration trends and reasons as they heavily contribute to health outcomes. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alarcão, V.; Stefanovska-Petkovska, M.; Virgolino, A.; Santos, O.; Costa, A. Intersections of Immigration and Sexual/Reproductive Health: An Umbrella Literature Review with a Focus on Health Equity. Soc. Sci. 2021, 10, 63. https://doi.org/10.3390/socsci10020063
Alarcão V, Stefanovska-Petkovska M, Virgolino A, Santos O, Costa A. Intersections of Immigration and Sexual/Reproductive Health: An Umbrella Literature Review with a Focus on Health Equity. Social Sciences. 2021; 10(2):63. https://doi.org/10.3390/socsci10020063
Chicago/Turabian StyleAlarcão, Violeta, Miodraga Stefanovska-Petkovska, Ana Virgolino, Osvaldo Santos, and Andreia Costa. 2021. "Intersections of Immigration and Sexual/Reproductive Health: An Umbrella Literature Review with a Focus on Health Equity" Social Sciences 10, no. 2: 63. https://doi.org/10.3390/socsci10020063
APA StyleAlarcão, V., Stefanovska-Petkovska, M., Virgolino, A., Santos, O., & Costa, A. (2021). Intersections of Immigration and Sexual/Reproductive Health: An Umbrella Literature Review with a Focus on Health Equity. Social Sciences, 10(2), 63. https://doi.org/10.3390/socsci10020063








