Randomized Clinical Trial of Primary Care Based Online Depression Prevention Intervention: Impact on Adolescent Modifiable Factors and Behaviors
Abstract
1. Introduction
2. Materials and Methods
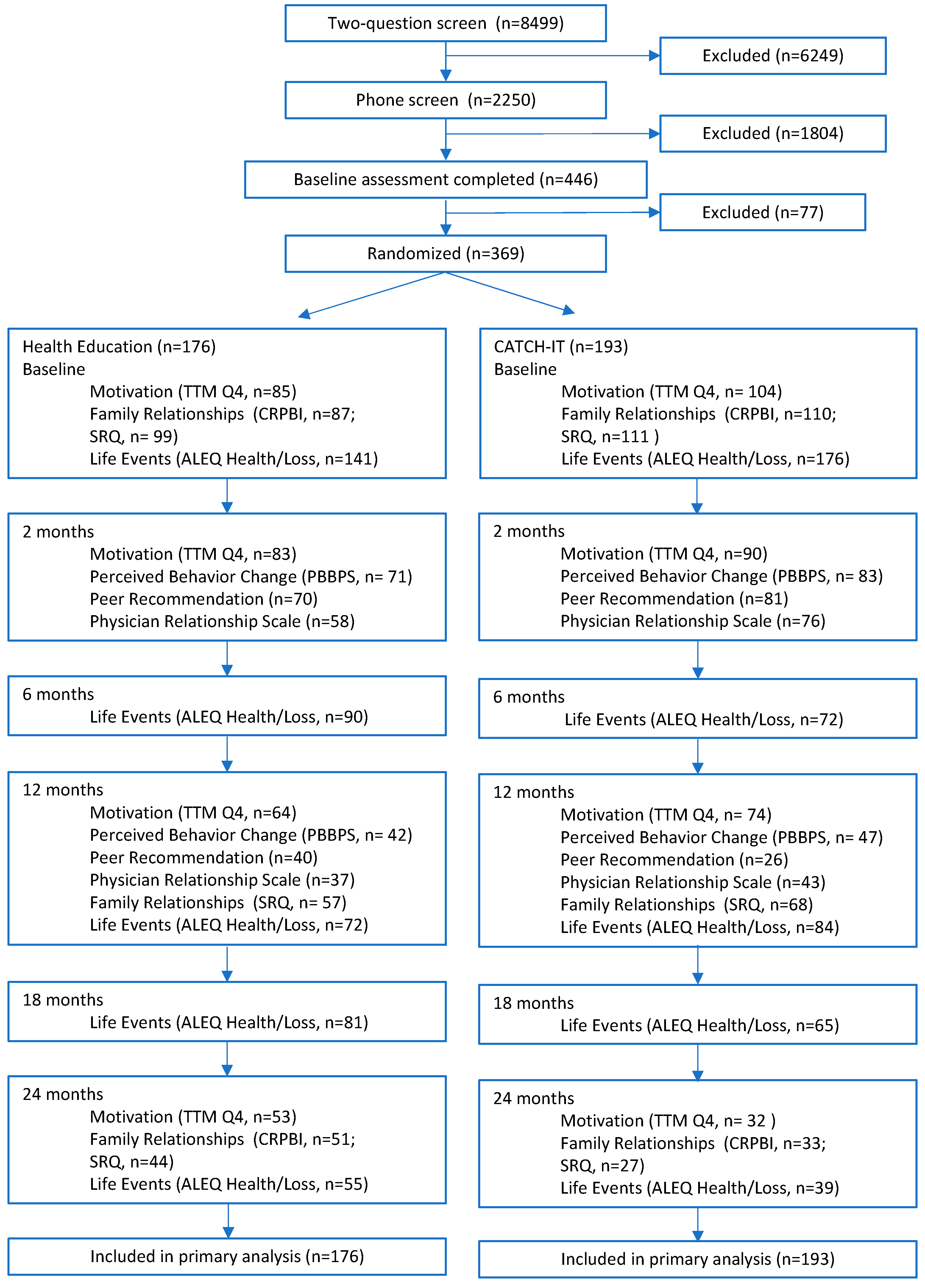
2.1. Study Design and Setting
2.2. CATCH-IT Intervention
2.3. Health Education Intervention
2.4. Intervention Shared Elements
2.5. Measures
2.6. Outcomes
3. Analysis
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Armitage, Christopher J., and Mark Conner. 2001. Efficacy of the theory of planned behaviour: A meta-analytic review. British Journal of Social Psychology 40: 471–99. [Google Scholar] [CrossRef]
- Bardach, Naomi S., Tumaini R. Coker, Bonnie T. Zima, J. Michael Murphy, Penelope Knapp, Laura P. Richardson, Glenace Edwall, and Rita Mangione-Smith. 2014. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics 133: 602–9. [Google Scholar] [CrossRef]
- Beck, Aaron T., Arlene Weissman, David Lester, and Larry Trexler. 1974. The measurement of pessimism: The hopelessness scale. Journal of Consulting and Clinical Psychology 42: 861. [Google Scholar] [CrossRef]
- Birmaher, Boris, David Brent, and ACAP Work Group on Quality Issues. 2007. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. Journal of the American Academy of Child & Adolescent Psychiatry 46: 1503–26. [Google Scholar]
- Birmaher, Boris, Neal D. Ryan, Douglas E. Williamson, David A. Brent, and Joan Kaufman. 1996a. Childhood and adolescent depression: A review of the past 10 years. Part II. Journal of the American Academy of Child & Adolescent Psychiatry 35: 1575–83. [Google Scholar]
- Birmaher, Boris, Neal D. Ryan, Douglas E. Williamson, David A. Brent, Joan Kaufman, Ronald E. Dahl, James Perel, and Beverly Nelson. 1996b. Childhood and adolescent depression: A review of the past 10 years. Part I. Journal of the American Academy of Child & Adolescent Psychiatry 35: 1427–39. [Google Scholar]
- Booth, Karin Vander Ploeg, David Paunesku, Michael Msall, Joshua Fogel, and Benjamin W. Van Voorhees. 2008. Using population attributable risk to help target preventive interventions for adolescent depression. International Journal of Adolescent Medicine and Health 20: 307–20. [Google Scholar] [CrossRef] [PubMed]
- Buhrmester, Duane, and Wyndol Furman. 1990. Perceptions of sibling relationships during middle childhood and adolescence. Child Development 61: 1387–98. [Google Scholar] [CrossRef]
- Daniels, Denise, and Robert Plomin. 1985. Differential experience of siblings in the same family. Developmental Psychology 21: 747–60. [Google Scholar] [CrossRef]
- Durlak, Joseph A., and Emily P. DuPre. 2008. Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. American Journal of Community Psychology 41: 327. [Google Scholar] [CrossRef]
- Eisma, Marteen C., Margaret S. Stroebe, Hank A. Schut, Wolfgang Stroebe, Paul A. Boelen, and Jan van den Bout. 2013. Avoidance processes mediate the relationship between rumination and symptoms of complicated grief and depression following loss. Journal of Abnormal Psychology 122: 961. [Google Scholar] [CrossRef] [PubMed]
- Embry, Dennis D. 2002. The Good Behavior Game: A best practice candidate as a universal behavioral vaccine. Clinical Child and Family Psychology Review 5: 273–97. [Google Scholar] [CrossRef] [PubMed]
- Georgiades, Katholiki, Peter M. Lewinsohn, Scott M. Monroe, and John R. Seeley. 2006. Major depressive disorder in adolescence: The role of subthreshold symptoms. Journal of the American Academy of Child & Adolescent Psychiatry 25: 936–44. [Google Scholar]
- Gladstone, Tracy, Katherine R. Buchholz, Marian Fitzgibbon, Linda Schiffer, Miae Lee, and Benjamin W. Van Voorhees. 2020. Randomized clinical trial of an internet-based adolescent depression prevention intervention in primary care: Internalizing symptom outcomes. International Journal of Environmental Research and Public Health 17: 7736. [Google Scholar] [CrossRef] [PubMed]
- Gladstone, Tracy G., Monika Marko-Holguin, Phyllis Rothberg, Jennifer Nidetz, Anne Diehl, Daniela T. DeFrino, Mary Harris, Eumene Ching, Milton Eder, Jason Canel, and et al. 2015. An internet-based adolescent depression preventive intervention: Study protocol for a randomized control trial. Trials 16: 1–17. [Google Scholar] [CrossRef]
- Gladstone, Tracy R., and Nadine J. Kaslow. 1995. Depression and attributions in children and adolescents: A meta-analytic review. Journal of Abnormal Child Psychology 23: 597–606. [Google Scholar] [CrossRef]
- Gottlieb, Lev, Zoran Martinovich, Kathryn M. Meyers, and Mark A. Reinecke. 2016. Treatment for Depression Enhances Protection: Findings From the Treatment for Adolescents With Depression Study (TADS). International Journal of Cognitive Therapy 9: 38–56. [Google Scholar] [CrossRef]
- Griffiths, Kathleen M., Dimitry Crisp, Helen Christensen, Andrew J. Mackinnon, and Kylie Bennett. 2010. The ANU WellBeing study: A protocol for a quasi-factorial randomised controlled trial of the effectiveness of an Internet support group and an automated Internet intervention for depression. BMC Psychiatry 10: 20. [Google Scholar] [CrossRef]
- Group, Whoqol. 1998. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine 28: 551–58. [Google Scholar] [CrossRef]
- Hankin, Benjamin L. 2006. Adolescent depression: Description, causes, and interventions. Epilepsy & Behavior 8: 102–14. [Google Scholar]
- Hankin, Benjamin L., and Lyn Y. Abramson. 2002. Measuring cognitive vulnerability to depression in adolescence: Reliability, validity, and gender differences. Journal of Clinical Child and Adolescent Psychology 31: 491–504. [Google Scholar] [CrossRef] [PubMed]
- Hollon, Steven D., Mark D. Evans, and Robert J. DeRubeis. 1990. Cognitive Mediation of Relapse Prevention Following Treatment for Depression: Implications of Differential Risk. Boston: Springer. [Google Scholar]
- Iloabachie, Corrie Wells, Brady Goodwin, Melinda Baldwin, Karen Vanderplough-Booth, Tracy Gladstone, Michael Murray, Joshua Fogel, and Benjamin W. Van Voorhees. 2011. Adolescent and parent experiences with a primary care/Internet-based depression prevention intervention (CATCH-IT). General Hospital Psychiatry 33: 543–55. [Google Scholar] [CrossRef] [PubMed]
- Klein, Daniel N., Peter M. Lewinsohn, Paul Rohde, John R. Seeley, and Thomas M. Olino. 2005. Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychological Medicine 35: 353–65. [Google Scholar] [CrossRef] [PubMed]
- Knight, John R., Lon Sherritt, Lydia A. Shrier, Sion Kim Harris, and Grace Chang. 2002. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Archives of Pediatrics & Adolescent Medicine 156: 607–14. [Google Scholar]
- Knight, John R., Lydia A. Shrier, Terrill D. Bravender, Michelle Farrell, Vander Joni Bilt, and Howard J. Shaffer. 1999. A new brief screen for adolescent substance abuse. Archives of Pediatrics & Adolescent Medicine 153: 591–96. [Google Scholar]
- Lewinsohn, Peter M., Hyman Hops, Robert E. Roberts, John R. Seeley, and Judy A. Andrews. 1993. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III—R disorders in high school students. Journal of Abnormal Psychology 102: 133. [Google Scholar] [CrossRef]
- Lewinsohn, Peter M., Ian H. Gotlib, and John R. Seeley. 1995. Adolescent psychopathology: IV. Specificity of psychosocial risk factors for depression and substance abuse in older adolescents. Journal of the American Academy of Child & Adolescent Psychiatry 34: 1221–29. [Google Scholar]
- Lewinsohn, Peter M., Ian H. Gotlib, and John R. Seeley. 1997. Depression-related psychosocial variables: Are they specific to depression in adolescents? Journal of Abnormal Psychology 106: 365. [Google Scholar] [CrossRef]
- Lewinsohn, Peter M., Paul Rohde, Daniel N. Klein, and John R. Seeley. 1999. Natural course of adolescent major depressive disorder: I. Continuity into young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry 38: 56–63. [Google Scholar]
- Lewinsohn, Peter M., Paul Rohde, and John R. Seeley. 1998. Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clinical Psychology Review 18: 765–94. [Google Scholar] [CrossRef]
- Lewinsohn, Peter M., Robert E. Roberts, John R. Seeley, Paul Rohde, Ian H. Gotlib, and Hyman Hops. 1994. Adolescent psychopathology: II. Psychosocial risk factors for depression. Journal of Abnormal Psychology 103: 302. [Google Scholar] [CrossRef]
- Liu, Yih-Lan. 2002. The role of perceived social support and dysfunctional attitudes in predicting Taiwanese adolescents’ depressive tendency. Adolescence 148: 823–35. [Google Scholar]
- Lynch, John, and George D. Smith. 2005. A life course approach to chronic disease epidemiology. Annual Review Public Health, 1–35. [Google Scholar] [CrossRef]
- Madras, Bertha K., Wilson M. Compton, Deepa Avula, Tom Stegbauer, Jack B. Stein, and H. Westley Clark. 2009. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug and Alcohol Dependence 99: 280–95. [Google Scholar] [CrossRef] [PubMed]
- Marko, Monika, Joshua Fogel, Elton Mykerezi, and Benjamin W. Van Voorhees. 2010. Adolescent internet depression prevention: Preferences for intervention and predictors of intentions and adherence. Journal of Cyber Therapy and Rehabilitation 3: 9. [Google Scholar] [PubMed]
- Miller, William R., and Stephen Rollnick. 1991. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York: Guilford Press. [Google Scholar]
- Mohr, David, Pim Cuijpers, and Kenneth Lehman. 2011. Supportive accountability: A model for providing human support to enhance adherence to eHealth interventions. Journal of Medical Internet Research 13: e30. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Peral, Patricia, Sonia Conejo-Cerón, Ana Fernández, Anna Berenguera, María Martínez-Andrés, Mariona Pons-Vigués, Emma Motrico, Beatriz Rodríguez-Martín, Juan A. Bellón, and Maria Rubio-Valera. 2015. Primary care patients’ perspectives of barriers and enablers of primary prevention and health promotion—A meta-ethnographic synthesis. PLoS ONE 10: e0125004. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, Susan. 2001. Ruminative coping and adjustment to bereavement. In Handbook of Bereavement Research: Consequences, Coping, and Care. Edited by Margaret S. Stroebe, Robert O. Hansson, Wolfgang Stroebe and Henk Schut. Washington, DC: American Psychological Association. [Google Scholar]
- Nolen-Hoeksema, Susan, Blair E. Wisco, and Sonja Lyubomirsky. 2008. Rethinking rumination. Perspectives on Psychological Science 3: 400–24. [Google Scholar] [CrossRef]
- O’Connell, Mary Ellen, Thomas Boat, and Kenneth E. Warner. 2009. Preventing Mental, Emotional, and Behavioral Disorders among Young People: Progress and Possibilities. Washington, DC: National Academies Press. [Google Scholar]
- Paunesku, David, Justin Ellis, Joshua Fogel, Sachiko A. Kuwabara, Jackie Gollan, Tracy Gladstone, Mark Reinecke, and Benjamin W. Van Voorheesa. 2008. Clusters of behaviors and beliefs predicting adolescent depression: Implications for prevention. Journal of Cognitive and Behavioral Psychotherapies 8: 147–68. [Google Scholar]
- Pelham, William E., Jr., Elizabeth M. Gnagy, Karen E. Greenslade, and Richard Milich. 1992. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry 31: 210–18. [Google Scholar]
- Pine, Daniel S., Patricia Cohen, Diana Gurley, Judith Brook, and Yuju Ma. 1998. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry 55: 56–64. [Google Scholar] [CrossRef]
- Prinz, Ronald J., Sharon Foster, Ronald N. Kent, and K. Daniel O’Leary. 1979. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of Applied Behavior Analysis 12: 691–700. [Google Scholar] [CrossRef]
- Radloff, Lenore Sawyer. 1991. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of Youth and Adolescence 20: 149–66. [Google Scholar] [CrossRef] [PubMed]
- Ritterband, Lee M., Frances P. Thorndike, Daniel J. Cox, Boris P. Kovatchev, and Linda A. Gonder-Frederick. 2009. A behavior change model for internet interventions. Annals of Behavioral Medicine 38: 18–27. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Valera, Maria, Mariona Pons-Vigués, Maria Martínez-Andrés, Patricia Moreno-Peral, Anna Berenguera, and Ana Fernández. 2014. Barriers and facilitators for the implementation of primary prevention and health promotion activities in primary care: A synthesis through meta-ethnography. PLoS ONE 9: e89554. [Google Scholar] [CrossRef]
- Rushton, Jerry L., Michelle Forcier, and Robin M. Schectman. 2002. Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. Journal of the American Academy of Child & Adolescent Psychiatry 41: 199–205. [Google Scholar]
- Schaefer, Earl S. 1965. A configurational analysis of children’s reports of parent behavior. Journal of Consulting Psychology 29: 552. [Google Scholar] [CrossRef] [PubMed]
- Sterling, Stacy, Andrea H. Kline-Simon, Ashley Jones, Lauren Hartman, Katrina Saba, Constance Weisner, and Sujaya Parthasarathy. 2019. Health care use over 3 years after adolescent SBIRT. Pediatrics 143: e20182803. [Google Scholar] [CrossRef]
- Van Voorhees, Benjamin, Tracy R. G. Gladstone, Kunmi Sobowale, C. Hendricks Brown, David A. Aaby, Daniela A. Terrizzi, Jason Canel, Eumene Ching, Anita D. Berry, James Cantorna, and et al. 2020. 24-Month Outcomes of Primary Care Web-Based Depression Prevention Intervention in Adolescents: Randomized Clinical Trial. Journal of Medical Internet Research 22: e16802. [Google Scholar] [CrossRef]
- Van Voorhees, Benajmin W., David Paunesku, Jackie Gollan, Sachiko Kuwabara, Mark Reinecke, and Anirban Basu. 2008a. Predicting future risk of depressive episode in adolescents: The Chicago Adolescent Depression Risk Assessment (CADRA). The Annals of Family Medicine 6: 503–11. [Google Scholar] [CrossRef]
- Van Voorhees, Benjamin W., David Paunesku, Sachiko A. Kuwabara, Anirban Basu, Jackie Gollan, Benjamin L. Hankin, Stephanie Melkonian, and Mark Reinecke. 2008b. Protective and vulnerability factors predicting new-onset depressive episode in a representative of US adolescents. Journal of Adolescent Health 42: 605–16. [Google Scholar] [CrossRef]
- Van Voorhees, Benjamin W., Joshua Fogel, Benjamin E. Pomper, Monika Marko, Nicholas Reid, Natalie Watson, John Larson, Nathan Bradford, Blake Fagan, Steve Zuckerman, and et al. 2009a. Adolescent dose and ratings of an Internet-based depression prevention program: A randomized trial of primary care physician brief advice versus a motivational interview. Journal of Cognitive and Behavioral Psychotherapies 9: 1–19. [Google Scholar]
- Van Voorhees, Benjamin W., Joshua Fogel, Mark A. Reinecke, Tracy Gladstone, Scott Stuart, Jackie Gollan, Nathan Bradford, Rocco Domanico, Blake Fagan, Ruth Ross, and et al. 2009b. Randomized clinical trial of an Internet-based depression prevention program for adolescents (Project CATCH-IT) in primary care: Twelve-week outcomes. Journal of Developmental and Behavioral Pediatrics 30: 23–37. [Google Scholar] [CrossRef] [PubMed]
- Van Voorhees, Benjamin W., Karen Vanderplough-Booth, Joshua Fogel, Tracy Gladstone, Carl Bell, Scott Stuart, Jackie Gollan, Nathan Bradford, Rocco Domanico, Blake Fagan, and et al. 2008c. Integrative internet-based depression prevention for adolescents: A randomized clinical trial in primary care for vulnerability and protective factors. Journal of the Canadian Academy of Child and Adolescent Psychiatry 17: 184. [Google Scholar]
- Van Voorhees, Benjamin W., Nicholas Mahoney, Rina Mazo, Alinne Z. Barrera, Christopher P. Siemer, Tracy Gladstone, and Ricardo F. Muñoz. 2011. Internet-based depression prevention over the life course: A call for behavioral vaccines. The Psychiatric Clinics of North America 34: 167–83. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Van Voorhees, Benjamin W., Tracy Gladstone, Stephanie Cordel, Monika Marko-Holguin, William Beardslee, Sachiko Kuwabara, Mark Allan Kaplan, Joshua Fogel, Anne Diehle, Chris Hansen, and et al. 2015. Development of a technology-based behavioral vaccine to prevent adolescent depression: A health system integration model. Internet Interventions 2: 303–13. [Google Scholar] [CrossRef] [PubMed][Green Version]
- van Zoonen, Kim, Claudia Buntrock, David Daniel Ebert, Filip Smit, Charles F. Reynolds, III, Aartjan T. F. Beekman, and Pim Cuijpers. 2014. Preventing the onset of major depressive disorder: A meta-analytic review of psychological interventions. International Journal of Epidemiology 43: 318–29. [Google Scholar] [CrossRef] [PubMed]
- Weissman, Myrna M., Brigitte A. Prusoff, W. Douglas Thompson, Pamela S. Harding, and Jerome K. Myers. 1978. Social adjustment by self-report in a community sample and in psychiatric outpatients. Journal of Nervous and Mental Disease 166: 317–26. [Google Scholar] [CrossRef]
- Weissman, Myrna M., Susan Wolk, Risë B. Goldstein, Donna Moreau, Philip Adams, Steven Greenwald, Claudia M. Klier, Neal D. Ryan, Ronald E. Dahl, and Priya Wickramaratne. 1999. Depressed adolescents grown up. JAMA 281: 1707–13. [Google Scholar] [CrossRef] [PubMed]
- Weisz, John R., Irwin N. Sandler, Joseph A. Durlak, and Barry S. Anton. 2005. Promoting and protecting youth mental health through evidence-based prevention and treatment. American Psychologist 60: 628. [Google Scholar] [CrossRef]
- Zabinski, Marion F., Denise E. Wilfley, Meredith A. Pung, Andrew J. Winzelberg, Kathleen Eldredge, and C. Barr Taylor. 2001. An interactive internet-based intervention for women at risk of eating disorders: A pilot study. International Journal of Eating Disorders 30: 129–37. [Google Scholar] [CrossRef]
- Zuckerbrot, Rachel A., Amy Cheung, Peter S. Jensen, Ruth E. Stein, Danielle Laraque, and GLAD-PC Steering Group. 2018. Guidelines for adolescent depression in primary care (GLAD-PC): Part I. Practice preparation, identification, assessment, and initial management. Pediatrics 141: e20174081. [Google Scholar] [CrossRef] [PubMed]
| Domain | Measure | Description | Sample Item |
|---|---|---|---|
| 1. Modifiable Factors Related to Program Completion | Trans-Theoretical Model | A 3-item (plus a fourth separate item) self-report of motivation that measures self-efficacy and intention to change risk-factor behaviors before, during, and after the intervention. The standard motivation measure approach described by Miller and Rollnick (Miller and Rollnick 1991) was adapted for our study. A higher score indicates a higher ranking on three items assessing importance, ability, or readiness to reduce depression risk on a 10-point Likert scale ranging from 1 = not important to 10 = very important, which are reported together as the scale. The fourth item assessing stage of change asked adolescents about their current position on reducing depression risk (ranging from precontemplation to decision, with plan) and is analyzed separately. Measures were taken at baseline and 2, 12, and 24 months. | Rate the importance of preventing/stopping an episode of clinical depression over the next two weeks. Question 4: Please click the bubble next to the one statement that best fits your current position with regard to changing the way you think about and solve everyday problems to reduce /lower your risk of developing clinical depression (severe enough to need a treatment). |
| Theory of Planned Behavior | A 19-item self-report on motivation utilizing a 5-point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree, with higher scores indicating stronger agreement with positive attitudes toward subthreshold depression intervention participation. Measures were taken at baseline and 12 and 24 months (Armitage and Conner 2001). | I believe going through an online program like this one would help me be healthy. | |
| Physician Relationship Scale | A 9 question self-report, which rates the adolescent’s relationship with their primary care provider in the following areas: understanding, engagement, helpfulness, comfort, and trust, reported on a 5 point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree (Van Voorhees et al. 2009b). | I am more likely to change behaviors or thought patterns because of the interview with the primary care provider. | |
| Satisfaction, Usefulness, and Peer Recommendation | Adolescents responded to six items about satisfaction, usefulness, and recommendation for peers who may become depressed regarding the intervention on a 10 point Likert scale ranging from 1 = very unsatisfied to 10 = very satisfied, with higher scores being more positive. | I would recommend this program to a friend who could develop depression. | |
| 2. Modifiable Factors Related to Adolescent Development | Social Adjustment Scale | A 36-item self-report with higher scores indicating worse social functioning on a Likert scale ranging from 1 = never or none to 5 = always or all or vice versa depending on the question. Measures were taken at baseline and at 12 and 24 months (Weissman et al. 1978). | How many days of classes did you miss in the last 2 weeks? |
| Quality of Life | A self-report of 26 total items regarding overall health (2 items, scored 0–100, on a Likert scale of 1 = very poor or dissatisfied to 5 = very good or satisfied) and four domains scored 0–100 generally on a Likert scale ranging from 1 = not at all or very dissatisfied or very poor or never to 5 = completely or very satisfied or very good or always: physical health (7 items), psychological (6 items scored), social relationships (3 items), and environment (8 items). Measures were taken at baseline and 6, 12, and 24 months (Group 1998). | How satisfied are you with your health? | |
| Adolescent Life Events Questionnaire | A six-month retrospective self-report scored in a range of 0–51 and includes seven subscales of specific groups of life events scored on a range from 0–9 using yes/no questions, with higher scores indicating more life events. Measures were taken at baseline and 2, 6, 12, 18, and 24 months (Hankin and Abramson 2002). | You were seriously ill or injured, hospitalized, or had surgery. | |
| 3. Modifiable Factors Related to Coping | Perceived Benefits of Behavioral Principles | Adolescents were asked to respond to 10 items about perceived behavior-related cognitive skill acquisition or perceived behavior modification due to a lesson relating to the core content of CATCH-IT based on either cognitive behavioral therapy (CBT), behavioral activation (BA), or interpersonal therapy (IPT). Higher scores on the 10 point Likert scale (1 = very unhelpful to 10 = extremely helpful) represented a stronger perceived benefit of a given type of therapy. The scale was created by Zubinski et al. assessing an eating disorder technology intervention (Zabinski et al. 2001) and the items were rephrased by Van Voorhees et al. to apply to CATCH-IT (referred to as sociocultural relevance scale in protocol paper) (Gladstone et al. 2015; Van Voorhees et al. 2015). Measures were taken at 2 and 12 months (Gladstone et al. 2015; Van Voorhees et al. 2015). | The program has helped me challenge negative thought patterns about everyday situation and problems. |
| Beck Hopelessness Scale | A self-report on a scale of 0–20 utilizing 20 true or false items, with higher scores indicating increased hopelessness. Administered at baseline and at 2, 6, 18, and 24 months (Beck et al. 1974). | I look forward to the future with hope and enthusiasm. | |
| 4. Modifiable Factors Related to Family Relations | Conflict Behavior Questionnaire | A self-report of conflict with mother or father, with a higher score indicating increased conflict on a scale of 0–20. Adolescents responded to 40 true or false questions. Measures were taken at baseline and 6 and 18 months (Prinz et al. 1979). | At least three times a week, my father and I get angry at each other. |
| Children’s Report of Parent Behavior Inventory | A self-report by adolescents and parents where higher scores indicate increased acceptance, psychological control, and monitoring by the mother or father. Participants responded to 15 items on a 3 point Likert scale with options being 1 = not like him/her, 2 = somewhat like him/her, or 3 = a lot like him/her at baseline and 24 months (Schaefer 1965). | Makes me feel better after talking over my worries with him. | |
| Sibling Relationships Questionnaire | A self-report of relationship with sibling in four domains, with higher scores indicating increased warmth/closeness (scored 1–5), relative status/power (scored −4 to 4), conflict (scored 1–5), and rivalry (scored 0–2) (Buhrmester and Furman 1990). Measures were taken at baseline, 12 and 24 months. | Who usually gets treated better by your mother, you or this sibling? | |
| The Sibling Differential Experience | A self-report of relative relationship with parent in comparison to sibling in affection and control by mother or father, with higher scores indicating a greater difference between participant and sibling. Participants responded to 18 items on a Likert scale of 1 = In general, this parent has been much more this way toward my sibling than me to 5 = in general, this parent has been much more this way toward me than my sibling. Measures were taken at baseline and at 24 months (Daniels and Plomin 1985). | Mother has been strict with us. | |
| Center for Epidemiological Studies-Depression Scale (CES-D10). | The CES-D10 is a seven-day self-report (or administered over the phone) of depressive symptoms with 20 items on a 4-point Likert scale ranging from 0 = rarely or none of the time to 3 = most or all of the time. Higher scores indicate increased symptoms on a score range of 0–30 (Radloff 1991). Measures from adolescents and parents were taken at baseline and at 2, 6, 12, 18, and 24 months. | During the past week I was bothered by things that usually don’t bother me. | |
| 5. Modifiable Factors Related to General Health Behaviors | Teen Behavior Questionnaire | A self-report questionnaire, with questions about diet, exercise, religion, and internet use. The questionnaire uses a variety of formats, some open ended, some no/yes, and some Likert scales (Gladstone et al. 2015; Van Voorhees et al. 2015). We identified the items used in the questionnaire by conducting a series of analyses using the National Longitudinal Study of Adolescent Health data set to examine the relationship between various reported behaviors at baseline and likelihood of experiencing a depressive episode at one-year follow-up (Booth et al. 2008; Van Voorhees et al. 2008b). These items have been previously reported by our group in relationship to depression risk (Booth et al. 2008; Van Voorhees et al. 2008b). Measures were taken at baseline and 2 and 12 months. Physical activity was assessed by asking adolescents how frequently they engaged in certain exercises (team sport, weightlifting, yoga, or others) over the previous week, in terms of both number of sessions and total minutes spent exercising. Adolescents selected activities and provided text answers. Religious activity was assessed via an open-ended question, while frequency of prayer or attendance at religious services was assessed via a Likert scale (5-point scale for prayer, from 1 = never to 5 = at least once a day, and a 4 point scale for religious service attendance and attendance at special activities at place of worship, from 1 = never to 4 = at least once a week. Diet was assessed by asking adolescents to responded to 9 items of dietary preferences: on a 6 point Likert scale ranging from 1 = less than once a month to 6 = more than 2 times a week for eating fish and yes/no items on willing to eat applesauce, pudding, yogurt, milk, apple juice, mango juice, orange juice, takes omega-3 fatty acids fish oil supplements. Internet use and media use was assessed via a self-report of number of internet activities adolescents engaged in the past week (six options provided, scored on a scale 0–6) and mental health website use was assessed via a self-report of number of websites adolescents visited (six options provided, scored on a scale 0–6). | Did you engage in any of the following activities during the past week? If yes please check the box and indicate the number of times and how many total minutes spent on each activity. |
| Body Mass Index | BMI was calculated from self-reported height and weight at baseline, 2, 6, 12, and at 24 months. | Self-reported height and weight. | |
| 6. Modifiable factors related to externalizing disorders | Disruptive Behaviors Disorder Scale | A self-report by the adolescent and parent regarding the adolescent measuring the level of adolescent’s behavioral problems. Adolescents answered 41 questions on a Likert scale ranging from 1 = not at all to 5 = very much. Measures were taken at baseline and at 6, 12, and 24 months (Pelham et al. 1992). | Often loses temper. |
| The CRAFT | The CRAFT measures drug use using 6 yes or no items regarding context and family/friend concern to detect substance use disorders in adolescents. Measures were taken at baseline and at 2, 6, 12, and 24 months (Knight et al. 1999, 2002). | Have you used alcohol or drugs to relax, feel better about yourself, or to fit in? |
| CATCH-IT (N = 193) | HE (N = 176) | ||||||
| Total N | N | % | Total N | N | % | p-Value a | |
| Trans-Theoretical Model Question 4 | |||||||
| Baseline | 104 | 85 | 0.19 | ||||
| Precontemplation | 25 | (24.0%) | 17 | (20.0%) | |||
| Contemplation | 33 | (31.7%) | 23 | (27.1%) | |||
| Preparation | 27 | (26.0%) | 21 | (24.7%) | |||
| Decision, no plan | 13 | (12.5%) | 19 | (22.4%) | |||
| Decision with plan | 6 | (5.8%) | 5 | (5.9%) | |||
| 2 months | 90 | 83 | 0.47 | ||||
| Precontemplation | 7 | (7.8%) | 12 | (14.5%) | |||
| Contemplation | 24 | (26.7%) | 25 | (30.1%) | |||
| Preparation | 23 | (25.6%) | 16 | (19.3%) | |||
| Decision, no plan | 26 | (28.9%) | 15 | (18.1%) | |||
| Decision with plan | 10 | (11.1%) | 15 | (18.1%) | |||
| 12 months | 74 | 64 | 0.02 | ||||
| Precontemplation | 8 | (10.8%) | 18 | (28.1%) | |||
| Contemplation | 20 | (27.0%) | 17 | (26.6%) | |||
| Preparation | 14 | (18.9%) | 10 | (15.6%) | |||
| Decision, no plan | 16 | (21.6%) | 11 | (17.2%) | |||
| Decision with plan | 16 | (21.6%) | 8 | (12.5%) | |||
| 24 months | 32 | 53 | 0.61 | ||||
| Precontemplation | 7 | (21.9%) | 12 | (22.6%) | |||
| Contemplation | 8 | (25.0%) | 17 | (32.1%) | |||
| Preparation | 9 | (28.1%) | 10 | (18.9%) | |||
| Decision, no plan | 4 | (12.5%) | 11 | (20.8%) | |||
| Decision with plan | 4 | (12.5%) | 3 | (5.7%) | |||
| N | Mean | SD | N | Mean | SD | p-Value b | |
| Physician Relationship Scale (1–5) c | |||||||
| 2 months | 76 | 4.0 | (0.7) | 58 | 3.9 | (0.9) | 0.28 |
| 12 months | 43 | 4.2 | (0.6) | 37 | 3.8 | (0.7) | 0.02 |
| Would recommend to friend who could develop depression (1–10) d | |||||||
| 2 months | 81 | 7.8 | (2.4) | 70 | 7.7 | (2.4) | 0.85 |
| 12 months | 26 | 8.3 | (2.3) | 40 | 7.0 | (2.1) | 0.02 |
| Unadjusted Means | Within-Group Slopes a | Between-Group Slope Difference p-Value a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CATCH-IT (N = 193) | Health Ed (N = 176) | CATCH-IT | Health Ed | ||||||||
| N | Mean | SD | N | Mean | SD | b | p-Value a | b | p-Value a | p-Value a | |
| Adolescents Life Events Questionnaire (ALEQ) b | |||||||||||
| LEQ total score (0–51) | −0.122 | <0.001 | −0.158 | <0.001 | 0.25 | ||||||
| Baseline | 168 | 8.1 | (5.8) | 134 | 8.2 | (5.7) | |||||
| 6 months | 69 | 4.5 | (3.8) | 90 | 5.5 | (6.1) | |||||
| 12 months | 82 | 4.7 | (4.5) | 70 | 3.7 | (4.6) | |||||
| 18 months | 65 | 4.9 | (4.6) | 81 | 4.6 | (4.7) | |||||
| 24 months | 39 | 4.9 | (5.4) | 54 | 3.9 | (4.6) | |||||
| Health and loss (0–9) | −0.038 | <0.001 | −0.067 | <0.001 | 0.03 | ||||||
| Baseline | 176 | 2.6 | (2.1) | 141 | 2.9 | (2.1) | |||||
| 6 months | 72 | 1.8 | (1.9) | 90 | 1.9 | (2.1) | |||||
| 12 months | 84 | 1.7 | (1.9) | 72 | 1.3 | (1.5) | |||||
| 18 months | 65 | 1.7 | (1.8) | 81 | 1.4 | (1.7) | |||||
| 24 months | 39 | 1.7 | (2.2) | 55 | 1.1 | (1.7) | |||||
| Arguments or conflicts (0–9) | −0.041 | <0.001 | −0.033 | <0.001 | 0.51 | ||||||
| Baseline | 174 | 2.3 | (1.8) | 140 | 2.3 | (1.9) | |||||
| 6 months | 70 | 1.3 | (1.5) | 88 | 1.5 | (1.9) | |||||
| 12 months | 83 | 1.3 | (1.8) | 72 | 0.8 | (1.3) | |||||
| 18 months | 65 | 1.4 | (1.7) | 81 | 1.5 | (1.8) | |||||
| 24 months | 39 | 1.2 | (1.7) | 55 | 1.2 | (1.6) | |||||
| Moves and changes (0–6) | −0.010 | 0.06 | −0.020 | <0.001 | 0.16 | ||||||
| Baseline | 173 | 0.6 | (1.0) | 140 | 0.7 | (1.1) | |||||
| 6 months | 70 | 0.3 | (0.6) | 89 | 0.4 | (0.9) | |||||
| 12 months | 83 | 0.4 | (0.7) | 70 | 0.3 | (0.7) | |||||
| 18 months | 65 | 0.3 | (0.7) | 81 | 0.3 | (0.6) | |||||
| 24 months | 39 | 0.4 | (0.8) | 54 | 0.2 | (0.6) | |||||
| School and job (0–9) | −0.013 | 0.02 | −0.017 | 0.002 | 0.62 | ||||||
| Baseline | 169 | 0.9 | (1.1) | 136 | 1.0 | (1.1) | |||||
| 6 months | 69 | 0.5 | (0.9) | 89 | 0.6 | (0.9) | |||||
| 12 months | 82 | 0.5 | (0.8) | 70 | 0.6 | (1.0) | |||||
| 18 months | 65 | 0.6 | (1.0) | 80 | 0.6 | (1.0) | |||||
| 24 months | 39 | 0.6 | (0.9) | 54 | 0.6 | (0.9) | |||||
| Finances/money (0–4) | −0.010 | 0.02 | −0.009 | 0.03 | 0.89 | ||||||
| Baseline | 168 | 0.8 | (1.1) | 134 | 0.7 | (1.0) | |||||
| 6 months | 69 | 0.3 | (0.7) | 90 | 0.4 | (0.8) | |||||
| 12 months | 82 | 0.5 | (0.9) | 70 | 0.3 | (0.8) | |||||
| 18 months | 65 | 0.4 | (0.8) | 81 | 0.4 | (0.9) | |||||
| 24 months | 39 | 0.5 | (0.9) | 54 | 0.3 | (0.8) | |||||
| Crime and legal issues (0–8) | −0.015 | <0.001 | −0.018 | <0.001 | 0.69 | ||||||
| Baseline | 168 | 0.7 | (1.3) | 133 | 0.6 | (1.2) | |||||
| 6 months | 70 | 0.2 | (0.6) | 90 | 0.5 | (1.1) | |||||
| 12 months | 82 | 0.2 | (0.6) | 72 | 0.2 | (0.5) | |||||
| 18 months | 65 | 0.3 | (0.7) | 81 | 0.2 | (0.7) | |||||
| 24 months | 39 | 0.4 | (0.7) | 54 | 0.2 | (0.7) | |||||
| Other (0–6) | 0.001 | 0.68 | −0.001 | 0.56 | 0.48 | ||||||
| Baseline | 169 | 0.2 | (0.5) | 135 | 0.2 | (0.4) | |||||
| 6 months | 71 | 0.1 | (0.3) | 90 | 0.2 | (0.5) | |||||
| 12 months | 81 | 0.1 | (0.4) | 72 | 0.2 | (0.5) | |||||
| 18 months | 64 | 0.2 | (0.4) | 81 | 0.2 | (0.5) | |||||
| 24 months | 39 | 0.2 | (0.4) | 54 | 0.1 | (0.4) | |||||
| CATCH-IT (N = 193) | Health Ed (N = 176) | ||||||||||
| N | Mean | SD | N | Mean | SD | p-Value a | |||||
| Perceived Benefits of Behavioral Principles Scale (1–10) b | |||||||||||
| 2 months | 83 | 6.5 | (2.1) | 71 | 5.5 | (2.2) | 0.008 | ||||
| 12 months | 47 | 6.9 | (2.1) | 42 | 5.5 | (2.1) | 0.003 | ||||
| Subscales (1–10) b | |||||||||||
| Behavioral Activation (BA) | |||||||||||
| 2 months | 80 | 6.8 | (2.1) | 71 | 5.8 | (2.4) | 0.005 | ||||
| 12 months | 47 | 7.0 | (2.2) | 42 | 5.8 | (2.2) | 0.01 | ||||
| Cognitive Behavioral Therapy (CBT) | |||||||||||
| 2 months | 80 | 6.5 | (2.1) | 70 | 5.6 | (2.4) | 0.01 | ||||
| 12 months | 45 | 6.8 | (2.3) | 42 | 5.6 | (2.2) | 0.02 | ||||
| Interpersonal Psychotherapy (IPT) | |||||||||||
| 2 months | 80 | 5.9 | (2.4) | 70 | 5.3 | (2.4) | 0.14 | ||||
| 12 months | 46 | 6.8 | (2.2) | 41 | 5.0 | (2.2) | <0.001 | ||||
| Unadjusted Means | Within-Group Slopes c | Between-Group Slope Differences p-Value c | |||||||||
| CATCH-IT | HE | CATCH-IT | HE | ||||||||
| N | Mean | SD | N | Mean | SD | b | p-Value a | b | p-Value a | p-Value a | |
| Children’s Report of Parent Behavior Inventory (CRPBI) d | |||||||||||
| CRPBI, Mother | |||||||||||
| Acceptance (10–30) | 0.024 | 0.45 | 0.003 | 0.92 | 0.60 | ||||||
| Baseline | 109 | 25.0 | (4.8) | 87 | 24.7 | (4.6) | |||||
| 24 months | 33 | 26.3 | (4.6) | 52 | 24.8 | (5.1) | |||||
| Psychological control (8–24) | −0.052 | 0.03 | 0.013 | 0.50 | 0.04 | ||||||
| Baseline | 110 | 12.3 | (3.5) | 87 | 11.6 | (3.3) | |||||
| 24 months | 33 | 10.9 | (3.0) | 51 | 12.0 | (3.7) | |||||
| Monitoring (5–15) | −0.009 | 0.55 | −0.014 | 0.29 | 0.84 | ||||||
| Baseline | 103 | 13.5 | (2.0) | 84 | 12.8 | (2.4) | |||||
| 24 months | 32 | 13.5 | (1.9) | 49 | 12.7 | (2.7) | |||||
| CRPBI, Father | |||||||||||
| Acceptance (10–30) | 0.035 | 0.36 | −0.012 | 0.72 | 0.36 | ||||||
| Baseline | 102 | 22.6 | (5.4) | 74 | 21.9 | (5.6) | |||||
| 24 months | 33 | 23.4 | (6.3) | 46 | 21.5 | (6.3) | |||||
| Psychological control (8–24) | −0.031 | 0.16 | 0.027 | 0.17 | 0.053 | ||||||
| Baseline | 102 | 11.8 | (3.6) | 74 | 11.8 | (3.6) | |||||
| 24 months | 33 | 11.2 | (3.2) | 46 | 12.6 | (4.4) | |||||
| Monitoring (5–15) | 0.023 | 0.24 | −0.005 | 0.77 | 0.28 | ||||||
| Baseline | 97 | 11.1 | (2.9) | 73 | 11.0 | (3.3) | |||||
| 24 months | 32 | 11.4 | (3.2) | 44 | 11.0 | (3.2) | |||||
| Sibling Relationships Questionnaire (SRQ) | |||||||||||
| Warmth/closeness (1–5) e | 0.012 | 0.01 | 0.009 | 0.04 | 0.62 | ||||||
| Baseline | 107 | 3.1 | (0.8) | 89 | 3.2 | (0.8) | |||||
| 12 months | 69 | 3.1 | (0.8) | 56 | 3.2 | (0.8) | |||||
| 24 months | 27 | 3.3 | (0.9) | 44 | 3.3 | (0.8) | |||||
| Relative status/power (−4 to 4) f | 0.003 | 0.57 | −0.011 | 0.01 | 0.03 | ||||||
| Baseline | 111 | 0.1 | (0.9) | 99 | 0.2 | (1.0) | |||||
| 12 months | 68 | 0.2 | (0.8) | 57 | 0.3 | (0.9) | |||||
| 24 months | 27 | 0.1 | (0.8) | 44 | 0.1 | (0.8) | |||||
| Conflict (1–5) g | −0.017 | 0.002 | −0.008 | 0.11 | 0.19 | ||||||
| Baseline | 107 | 2.7 | (0.9) | 92 | 2.6 | (0.8) | |||||
| 12 months | 69 | 2.5 | (0.8) | 57 | 2.4 | (0.8) | |||||
| 24 months | 27 | 2.4 | (0.8) | 44 | 2.5 | (0.9) | |||||
| Rivalry (0–2) h | −0.007 | 0.03 | −0.005 | 0.11 | 0.57 | ||||||
| Baseline | 105 | 0.5 | (0.5) | 90 | 0.5 | (0.5) | |||||
| 12 months | 64 | 0.5 | (0.5) | 53 | 0.4 | (0.5) | |||||
| 24 months | 26 | 0.2 | (0.4) | 42 | 0.4 | (0.5) | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gupta, K.B.; Rusiewski, C.; Koczara, C.; Fitzgibbon, M.; Reinecke, M.; Fogel, J.; Schiffer, L.; Lee, M.; Sykes, E.; Griffiths, K.; et al. Randomized Clinical Trial of Primary Care Based Online Depression Prevention Intervention: Impact on Adolescent Modifiable Factors and Behaviors. Soc. Sci. 2021, 10, 385. https://doi.org/10.3390/socsci10100385
Gupta KB, Rusiewski C, Koczara C, Fitzgibbon M, Reinecke M, Fogel J, Schiffer L, Lee M, Sykes E, Griffiths K, et al. Randomized Clinical Trial of Primary Care Based Online Depression Prevention Intervention: Impact on Adolescent Modifiable Factors and Behaviors. Social Sciences. 2021; 10(10):385. https://doi.org/10.3390/socsci10100385
Chicago/Turabian StyleGupta, Kushagra B., Calvin Rusiewski, Camilla Koczara, Marian Fitzgibbon, Mark Reinecke, Joshua Fogel, Linda Schiffer, Miae Lee, Emily Sykes, Kathy Griffiths, and et al. 2021. "Randomized Clinical Trial of Primary Care Based Online Depression Prevention Intervention: Impact on Adolescent Modifiable Factors and Behaviors" Social Sciences 10, no. 10: 385. https://doi.org/10.3390/socsci10100385
APA StyleGupta, K. B., Rusiewski, C., Koczara, C., Fitzgibbon, M., Reinecke, M., Fogel, J., Schiffer, L., Lee, M., Sykes, E., Griffiths, K., Gladstone, T. R. G., & Van Voorhees, B. W. (2021). Randomized Clinical Trial of Primary Care Based Online Depression Prevention Intervention: Impact on Adolescent Modifiable Factors and Behaviors. Social Sciences, 10(10), 385. https://doi.org/10.3390/socsci10100385





