Long Term Outcomes of Blended CBT Compared to Face-to-Face CBT and Treatment as Usual for Adolescents with Depressive Disorders: Analyses at 12 Months Post-Treatment
Abstract
:1. Introduction
2. Method
2.1. Ethics
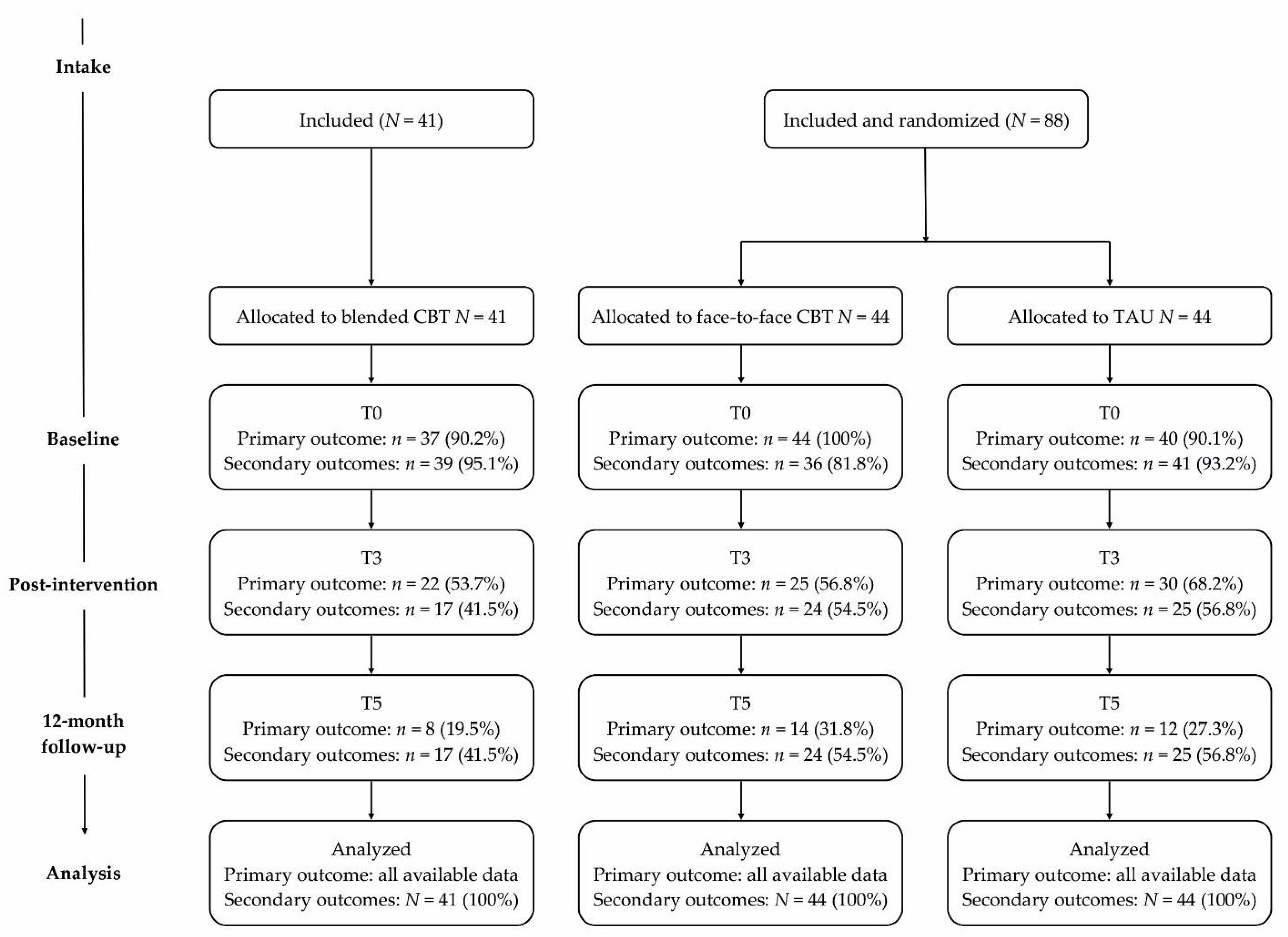
2.2. Design and Procedure
2.3. Sample Size
2.4. Participants
2.5. Interventions
2.6. Measures
2.6.1. Primary Outcome
2.6.2. Secondary Outcomes
2.7. Missing Data
2.8. Statistical Analyses
3. Results
3.1. Sample Characteristics
3.2. Primary Outcome
3.3. Secondary Outcomes
3.4. Reliable Change in Depressive Symptoms
3.5. Other Outcomes
3.6. Sensitivity Analyses
4. Discussion
4.1. Strengths and Limitations
4.2. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Achenbach, Thomas M. 1991. Manual for the Child Behavior Checklist/4-18, YSR, and TRF Profiles. Burlington: Department of Psychiatry, University of Vermont. [Google Scholar]
- Achenbach, Thomas M. 1999. The Child Behavior Checklist and related instruments. In The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. Edited by Mark E. Maruish. Mahwah: Lawrence Erlbaum Associates Publishers, pp. 429–66. [Google Scholar]
- Achenbach, Thomas M., and Leslie A. Rescorla. 2004. The Achenbach system of empirically based assessment (ASEBA) for ages 1.5 to 18 years. In The Use of Psychological Testing for Treatment Planning Outcomes Assessment. Edited by M. E. Maruish. Mahwah: Lawrence Erlbaum Associated Publishers, pp. 179–213. [Google Scholar]
- Andrews, Gavin, Pim Cuijpers, Michelle G. Craske, Peter McEvoy, and Nickolai Titov. 2010. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: A meta-analysis. PLoS ONE 5: e13196. [Google Scholar] [CrossRef] [PubMed]
- Bates, Douglas M., Martin Maechler, Ben Bolker, and Steve Walker. 2015. Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software 67: 1–48. [Google Scholar] [CrossRef]
- Birmaher, Boris, David A. Brent, David Kolko, Marianne Baugher, Jeffrey Bridge, Diane Holder, Satish Iyengar, and Rosa E. Ulloa. 2000. Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Archives of General Psychiatry 57: 29–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bodden, Denise H. M., Yvonne Stikkelbroek, and Caroline Braet. 2016. The Child Depression Inventory 2 (CDI-2). Utrecht: Utrecht University. [Google Scholar]
- Chan, An-Wen, Jennifer M. Tetzlaff, Douglas G. Altman, Andreas Laupacis, Peter C. Gøtzsche, Karmela Krleža-Jerić, Asbjørn Hróbjartsson, Howard Mann, Kay Dickersin, and Jesse A. Berlin. 2013. SPIRIT 2013 statement: Defining standard protocol items for clinical trials. Annals of Internal Medicine 158: 200–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clarke, Gregory N., Peter M. Lewinsohn, and Hyman Hops. 1990. Adolescent Coping with Depression Course. Eugene: Castalia Publishing. [Google Scholar]
- Clarke, Gregory N., Peter Rohde, Peter M. Lewinsohn, Hyman Hops, and J. R. Seeley. 1999. Cognitive-behavioral treatment of adolescent depression: Efficacy of acute group treatment and booster sessions. Journal of the American Academy of Child Adolescent Psychiatry 38: 272–79. [Google Scholar] [CrossRef]
- Clarke, Gregory N., Mark Hornbrook, Frances Lynch, Michael Polen, John Gale, Elizabeth O’Conner, John R. Seeley, and Lynn Debar. 2002. Group cognitive-behavioral treatment for depressed adolescent offspring of depressed parents in a health maintenance organization. Journal of the American Academy of Child Adolescent Psychiatry 41: 305–13. [Google Scholar] [CrossRef]
- Cuijpers, Pim, Eirini Karyotaki, Dikla Eckshtain, Mei Yi Ng, Katherine A. Corteselli, Hisashi Noma, Soledad Quero, and John R. Weisz. 2020. Psychotherapy for depression across different age groups: A systematic review and meta-analysis. JAMA Psychiatry 77: 694–702. [Google Scholar] [CrossRef]
- De Haan, Anna M., Albert E. Boon, Joop T. V. M. De Jong, Machteld Hoeve, and Robert R.J.M. Vermeiren. 2013. A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clinical Psychology Review 33: 698–711. [Google Scholar] [CrossRef]
- Ellis, Rachel E. R., Marc L. Seal, Julian G. Simmons, Sarah Whittle, Orli S. Schwartz, Michelle L. Byrne, and Nicholas B. Allen. 2017. Longitudinal trajectories of depression symptoms in adolescence: Psychosocial risk factors and outcomes. Child Psychiatry Human Development 48: 554–71. [Google Scholar] [CrossRef]
- Erbe, Doris, Hans-Christoph Eichert, Heleen Riper, and David Daniel Ebert. 2017. Blending face-to-face and internet-based interventions for the treatment of mental disorders in adults: Systematic review. Journal of Medical Internet Research 19: e306. [Google Scholar] [CrossRef] [Green Version]
- Gould, Madelyn S., Ted Greenberg, Drew M. Velting, and David Shaffer. 2003. Youth suicide risk and preventive interventions: A review of the past 10 years. Journal of the American Academy of Child Adolescent Psychiatry 42: 386–405. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, Neil S., and Paula Truax. 1991. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology 59: 12–19. [Google Scholar] [CrossRef] [PubMed]
- Jaycox, Lisa H., Bradley D. Stein, Susan Paddock, Jeremy N. V. Miles, Anita Chandra, Lisa S. Meredith, Terri Tanielian, Scot Hickey, and M. Audrey Burnam. 2009. Impact of teen depression on academic, social, and physical functioning. Pediatrics 124: e596–e605. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, Joan, Boris Birmaher, David A. Brent, Uma Rao, Cynthia Flynn, Paula Moreci, Douglas Williamson, and Neal Ryan. 1997. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry 36: 980–88. [Google Scholar] [CrossRef]
- Kessler, Ronald C., Shelli Avenevoli, E. Jane Costello, Katholiki Georgiades, Jennifer G. Green, Machael J. Gruber, Jian Ping He, Doreen Koretz, Katie A. McLaughlin, and Maria Petukhova. 2012. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry 69: 372–80. [Google Scholar] [CrossRef] [PubMed]
- Kim-Cohen, Julia, Avshalom Caspi, Terrie E. Moffitt, HonaLee Harrington, Barry J. Milne, and Rachie Poulton. 2003. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry 60: 709–17. [Google Scholar] [CrossRef]
- Klein, Jesse B., Rachel H. Jacobs, and Mark A. Reinecke. 2007. Cognitive-behavioral therapy for adolescent depression: A meta-analytic investigation of changes in effect-size estimates. Journal of the American Academy of Child and Adolescent Psychiatry 46: 1403–13. [Google Scholar] [CrossRef] [Green Version]
- Kovacs, Maria. 2011. The Children’s Depression Inventory 2: Manual. North Tonawanda: Multi-Health Systems. [Google Scholar]
- Lewinsohn, Peter M., Gregory N. Clarke, Hyman Hops, and Judy Andrews. 1990. Cognitive-behavioral treatment for depressed adolescents. Behavior Therapy 21: 385–401. [Google Scholar] [CrossRef]
- Moher, David, Sally Hopewell, Kenneth F. Schulz, Victor Montori, Peter C. Gøtzsche, P. J. Devereaux, Diana Elbourne, Matthias Egger, and Douglas G. Altman. 2012. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. International Journal of Surgery 10: 28–55. [Google Scholar] [CrossRef] [Green Version]
- Portzky, Gwendolyn, and Cornelis Van Heeringen. 2009. Suïcide bij jongeren. Psychologie en Gezondheid 37: 75–89. [Google Scholar] [CrossRef]
- Posner, Kelly, Gregory K. Brown, Barbara Stanley, David A. Brent, Kseniya V. Yershova, Maria A. Oquendo, Glenn W. Currier, Glenn A. Melvin, Laurence Greenhill, Sa Shen, and et al. 2011. The Columbia–Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. American Journal of Psychiatry 168: 1266–77. [Google Scholar] [CrossRef] [Green Version]
- R Core Team. 2020. R: A Language and Environment for Statistical Computing. Available online: https://www.R-project.org (accessed on 16 April 2021).
- Rasing, Sanne PA. 2021. Blended Treatment for Depressive Disorders in Youth: A Narrative Review. International Journal of Cognitive Therapy 14: 47–85. [Google Scholar] [CrossRef]
- Rasing, Sanne, Yvonne A. J. Stikkelbroek, and Denise H. M. Bodden. 2019a. Is Digital Treatment the Holy Grail? Literature Review on Computerized and Blended Treatment for Depressive Disorders in Youth. International Journal of Environmental Research and Public Health 17: 153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasing, Sanne P. A., Yvonne A. J. Stikkelbroek, Heleen Riper, Maja Dekovic, Maaike H. Nauta, Carmen D. Dirksen, Daan H. M. Creemers, and Denise H. M. Bodden. 2019b. Effectiveness and Cost-Effectiveness of Blended Cognitive Behavioral Therapy in Clinically Depressed Adolescents: Protocol for a Pragmatic Quasi-Experimental Controlled Trial. JMIR Research Protocols 8: e13434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasing, Sanne P. A., Yvonne A. J. Stikkelbroek, Wouter Den Hollander, Heleen Riper, Maja Deković, Maaike H. Nauta, Daan H. M. Creemers, Marianne C. P. Immink, Mariken Spuij, and Denise H. M. Bodden. 2021. Pragmatic quasi-experimental controlled trial evaluating the outcomes of blended CBT compared to face-to-face CBT and treatment as usual for adolescents with depressive disorders. International Journal of Environmental Research and Public Health 18: 3102. [Google Scholar] [CrossRef] [PubMed]
- Reichart, Catrien. G., Marjolein Wals, and Manon Hillegers. 2000. Vertaling K-Sads. Utrecht: HC Rümke Groep. [Google Scholar]
- Reynolds, William M. 1988. SIQ, Suicidal Ideation Questionnaire: Professional Manual. Odessa: Psychological Assessment Resources. [Google Scholar]
- Rubin, Donald B. 1987. Multiple Imputation for Nonresponse in Surveys. New York: Wiley. [Google Scholar]
- Schulz, Kenneth F., Douglas G. Altman, and David Moher. 2010. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. Trials 11: 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seeley, John R., Eric Stice, and Paul Rohde. 2009. Screening for depression prevention: Identifying adolescent girls at high risk for future depression. Journal of Abnormal Psychology 118: 161–70. [Google Scholar] [CrossRef] [Green Version]
- Stikkelbroek, Yvonne A. J., and Johan Van Dijk. 2013. D(o)epressie Blended. Utrecht: Jouw Omgeving. [Google Scholar]
- Stikkelbroek, Yvonne A. J., Henk Bouman, and Pim Cuijpers. 2005. De Doepressiecursus. Dordrecht: Doepressie. [Google Scholar]
- Stikkelbroek, Yvonne A. J., Denise H. M. Bodden, Maja Deković, and Anneloes L. van Baar. 2013. Effectiveness and cost effectiveness of cognitive behavioral therapy (CBT) in clinically depressed adolescents: Individual CBT versus treatment as usual (TAU). BMC Psychiatry 13: 314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stikkelbroek, Yvonne, Gerko Vink, Maaike H. Nauta, Marko A. Bottelier, Leonieke J. J. Vet, Cathelijne M. Lont, Anneloes L. Van Baar, and Denise H. M. Bodden. 2020. Effectiveness and moderators of individual cognitive behavioral therapy versus treatment as usual in clinically depressed adolescents: A randomized controlled trial. Scientific Reports 10: 1–13. [Google Scholar] [CrossRef]
- Topooco, Naira, Sandra Byléhn, Ellen Dahlström Nysäter, Jenny Holmlund, Johanna Lindegaard, Sanna Johansson, Linnea Åberg, Lise Bergman Nordgren, Maria Zetterqvist, and Gerhard Andersson. 2019. Evaluating the Efficacy of Internet-Delivered Cognitive Behavioral Therapy Blended With Synchronous Chat Sessions to Treat Adolescent Depression: Randomized Controlled Trial. Journal of Medical Internet Research 21: e13393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Treatment for Adolescents with Depression Study (TADS) Team. 2009. The Treatment for Adolescents With Depression Study (TADS): Outcomes over 1 year of naturalistic follow-up. American Journal of Psychiatry 166: 1141–49. [Google Scholar] [CrossRef]
- Twisk, Jos, Lisa Bosman, Trynke Hoekstra, Judith Rijnhart, Marieke Welten, and Martijn Heymans. 2018. Different ways to estimate treatment effects in randomised controlled trials. Contemporary Clinical Trials Communications 10: 80–85. [Google Scholar] [CrossRef]
- Van Buuren, Stef. 2018. Flexible Imputation of Missing Data. Boca Raton: Chapman and Hall. [Google Scholar]
- Van Buuren, Stef, and Karin Groothuis-Oudshoorn. 2011. Mice: Multivariate imputation by chained equations in R. Journal of Statistical Software 45: 1–68. [Google Scholar] [CrossRef] [Green Version]
- Van der Vaart, Rosalie, Marjon Witting, Heleen Riper, Lisa Kooistra, Ernst T. Bohlmeijer, and Lisette J. van Gemert-Pijnen. 2014. Blending online therapy into regular face-to-face therapy for depression: Content, ratio and preconditions according to patients and therapists using a Delphi study. BMC Psychiatry 14: 355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verboom, Charlotte E., Jelle. J. Sijtsema, Frank. C. Verhulst, Brenda. W. J. H. Penninx, and Hans Ormel. 2014. Longitudinal associations between depressive problems, academic performance, and social functioning in adolescent boys and girls. Developmental Psychology 50: 247. [Google Scholar] [CrossRef]
- Verhulst, Frank, Jan van der Ende, and Hans M. Koot. 1996. Handleiding voor de CBCL/4-18. Rotterdam: Erasmus University Rotterdam. [Google Scholar]
- Vernmark, Kristofer, Hugo Hesser, Naira Topooco, Thomas Berger, Heleen Riper, Liisa Luuk, Lisa Backlund, Per Carlbring, and Gerhard Andersson. 2019. Working alliance as a predictor of change in depression during blended cognitive behaviour therapy. Cognitive Behaviour. Therapy 48: 285–99. [Google Scholar] [CrossRef] [PubMed]
- Weisz, John R., Carolyn A. McCarty, and Sylvia M. Valeri. 2006. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin 132: 132. [Google Scholar] [CrossRef] [Green Version]
- Weisz, John R., Sofie Kuppens, Dikla Eckshtain, Ana M. Ugueto, Kristin M. Hawley, and Amanda Jensen-Doss. 2013. Performance of evidence-based youth psychotherapies compared with usual clinical care: A multilevel meta-analysis. JAMA Psychiatry 70: 750–61. [Google Scholar] [CrossRef] [Green Version]
- Weisz, John R., Lauren S. Krumholz, Lauren Santucci, Kristel Thomassin, and Mei Yi Ng. 2015. Shrinking the gap between research and practice: Tailoring and testing youth psychotherapies in clinical care contexts. Annual Review of Clinical Psychology 11: 139–63. [Google Scholar] [CrossRef] [Green Version]
- Wickrama, Kandauda. A. S., Rand D. Conger, Frederic O. Lorenz, and Tony Jung. 2008. Family antecedents and consequences of trajectories of depressive symptoms from adolescence to young adulthood: A life course investigation. Journal of Health and Social Behavior 49: 468–83. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. 2017. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization. [Google Scholar]
| Blended CBT | Face-to-Face CBT | Treatment as Usual | |
|---|---|---|---|
| M (SD) | M (SD) | M (SD) | |
| Depressive symptoms T0 | 25.93 (6.29) | 25.94 (9.59) | 24.43 (7.40) |
| Depressive symptoms T3 | 18.12 (15.61) | 15.95 (13.02) | 18.19 (10.52) |
| Depressive symptoms T5 | 11.55 (13.07) | 8.88 (12.20) | 10.42 (11.42) |
| Suicide risk T0 | 3.51 (3.09) | 4.42 (4.02) | 3.58 (3.41) |
| Suicide risk T3 | 2.58 (4.75) | 2.27 (3.55) | 2.43 (3.59) |
| Suicide risk T5 | 1.15 (3.12) | 0.65 (2.10) | 0.70 (2.19) |
| Internalizing symptoms T0 | 27.94 (9.11) | 28.92 (9.44) | 28.52 (9.33) |
| Internalizing symptoms T3 | 20.96 (14.85) | 19.96 (15.74) | 20.70 (13.31) |
| Internalizing symptoms T5 | 13.06 (12.43) | 10.43 (8.51) | 11.62 (12.15) |
| Externalizing symptoms T0 | 11.05 (7.41) | 13.51 (9.45) | 12.64 (8.27) |
| Externalizing symptoms T3 | 9.32 (10.31) | 11.03 (8.76) | 10.14 (7.99) |
| Externalizing symptoms T5 | 6.26 (7.94) | 6.43 (7.59) | 6.55 (8.31) |
| Blended CBT vs. Face-to-Face CBT | Blended CBT vs. Treatment as Usual | |||||
|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | |
| Depressive symptoms T0–T5 | 2.41 | 2.07 | 0.24 | 1.01 | 2.08 | 0.63 |
| Depressive symptoms T3–T5 | 2.21 | 1.88 | 0.24 | 1.13 | 1.87 | 0.55 |
| Suicide risk T0–T5 | 0.56 | 0.61 | 0.36 | 0.41 | 0.60 | 0.50 |
| Suicide risk T3–T5 | 0.42 | 0.55 | 0.45 | 0.43 | 0.54 | 0.43 |
| Internalizing symptoms T0–T5 | 2.41 | 2.33 | 0.30 | 1.62 | 2.28 | 0.48 |
| Internalizing symptoms T3–T5 | 2.43 | 2.08 | 0.23 | 1.48 | 2.04 | 0.47 |
| Externalizing symptoms T0–T5 | 0.66 | 1.47 | 0.66 | 0.23 | 1.48 | 0.88 |
| Externalizing symptoms T3–T5 | 0.27 | 1.34 | 0.84 | -0.18 | 1.35 | 0.90 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rasing, S.P.A.; Stikkelbroek, Y.A.J.; den Hollander, W.; Okorn, A.; Bodden, D.H.M. Long Term Outcomes of Blended CBT Compared to Face-to-Face CBT and Treatment as Usual for Adolescents with Depressive Disorders: Analyses at 12 Months Post-Treatment. Soc. Sci. 2021, 10, 373. https://doi.org/10.3390/socsci10100373
Rasing SPA, Stikkelbroek YAJ, den Hollander W, Okorn A, Bodden DHM. Long Term Outcomes of Blended CBT Compared to Face-to-Face CBT and Treatment as Usual for Adolescents with Depressive Disorders: Analyses at 12 Months Post-Treatment. Social Sciences. 2021; 10(10):373. https://doi.org/10.3390/socsci10100373
Chicago/Turabian StyleRasing, Sanne P. A., Yvonne A. J. Stikkelbroek, Wouter den Hollander, Ana Okorn, and Denise H. M. Bodden. 2021. "Long Term Outcomes of Blended CBT Compared to Face-to-Face CBT and Treatment as Usual for Adolescents with Depressive Disorders: Analyses at 12 Months Post-Treatment" Social Sciences 10, no. 10: 373. https://doi.org/10.3390/socsci10100373
APA StyleRasing, S. P. A., Stikkelbroek, Y. A. J., den Hollander, W., Okorn, A., & Bodden, D. H. M. (2021). Long Term Outcomes of Blended CBT Compared to Face-to-Face CBT and Treatment as Usual for Adolescents with Depressive Disorders: Analyses at 12 Months Post-Treatment. Social Sciences, 10(10), 373. https://doi.org/10.3390/socsci10100373






