Empirical Research on the Life Satisfaction and Influencing Factors of Users of Community-Embedded Elderly Care Facilities
Abstract
1. Introduction
- It clarifies the LS of users of community-embedded elderly care service facilities, as well as the characteristics of users, staff, and living spaces.
- It confirms a significant correlation between user LS and the characteristics of users, staff, and living spaces.
- It constructs a model of structural equations of user satisfaction with life and its influencing factors.
- Based on these findings, optimization strategies are proposed to improve facility space and service design, improving user LS.
2. Related Works
2.1. Research on LS Impact
2.2. Research on Community-Embedded Elderly Care
3. Materials and Methods
3.1. Research Area
- Identify user characteristics, staff characteristics, and living space characteristics affecting LS.
- Analyze the relationships among these characteristics and LS.
- Validate the correlates of LS and the structural relationships among them using exploratory factor analysis and structural equation modeling (SEM).
3.2. Procedures and Data Collection
3.3. Data Analysis
4. Results
4.1. Descriptive Statistical Analysis of Data Sets
4.2. Correlation Analysis
- User characteristics: income status (0.59) and usage time (0.84) showed a strong positive correlation with LS, while level of care (−0.63) was strongly negatively correlated. Age (0.36), child status (0.31), willingness to stay (0.36), and LS showed a moderate positive correlation. Marital status (−0.29) showed a slight correlation. Interestingly, no correlation was found at all between gender and LS.
- Staff characteristics: The retention rate of qualification certificates (0.56) shows a strong positive correlation with LS, and the percentage of household registration in Tianjin (−0.56) shows a strong negative correlation. The average age of staff (−0.19) shows a slight negative correlation with LS, and the proportion of male staff (0.19), percentage of participation in training (0.16), and the average working years (0.21) show a slight positive correlation.
- Living space characteristics:The bedroom window status (−0.51) and outdoor space status (−0.65) showed a strong negative correlation with LS, indicating that a lack of windows in a bedroom and a lack of outdoor space in the facility would greatly reduce the LS of the users. The positional relationship between the bedroom and LD (−0.38), bedroom toilet status (−0.37), the number of available shared-space rooms (0.42), and LS showed moderate correlations. A slight correlation was presented between the per capita shared-space area (0.26), the per capita bedroom area (0.26), the number of people in the bedroom (−0.14), and LS.The correlation between the distance between the bedroom door and LD (−0.01), the space layout form (−0.05), LD window status (0.03), and LS were very low.
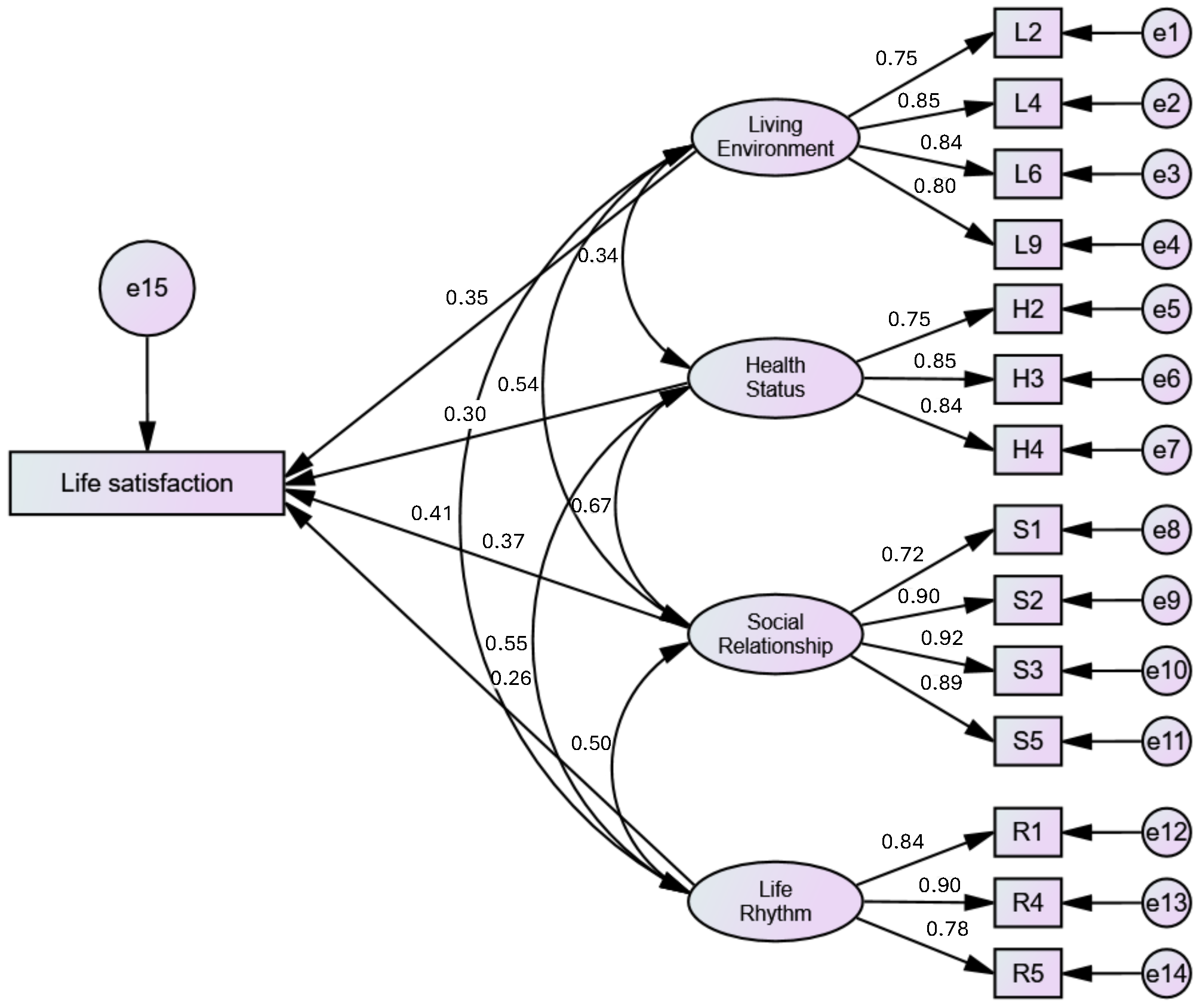
4.3. Structural Model
- Factor 1 consisted of four factors (L2, L4, L6, L9) related to living environment satisfaction;
- Factor 2 consisted of three factors (H2, H3, H4) related to health status satisfaction;
- Factor 3 consisted of four factors (S1, S2, S3, S5) related to social relationship satisfaction;
- Factor 4 consisted of three factors (R1, R4, R5) related to life-rhythm satisfaction.
- Living environment satisfaction was affected by ease of access from the bedroom to the LD (L4: 0.85), satisfaction with lighting and ventilation (L6: 0.84), ease of use and spaciousness of toilets and bathrooms (L9: 0.80), and comfort and spaciousness of the bedroom (L2: 0.75).
- Health status satisfaction was affected by frequency of stress (H3: 0.85), sleep quality (H4: 0.84), and frequency of body pain (H2: 0.72).
- Social relationship satisfaction was mainly influenced by relationship status with staff (S3: 0.92), relationship status with other users (S2: 0.90), participation in social activities (S5: 0.89), and family relationship status (S1: 0.72).
- Life-rhythm satisfaction was affected by satisfaction with the implementation of care-type activities (R4: 0.90), timeliness of needs being met (R1: 0.84), and satisfaction with the implementation of health-type activities (R5: 0.78).
5. Discussion
5.1. Correlations Between User, Staff, Living Space Characteristics, and User LS
5.2. Factors Influencing Life Satisfaction
5.2.1. Impact of Social Relationship Satisfaction on LS
5.2.2. Impact of Living Environment Satisfaction on LS
5.2.3. Impact of Health Status Satisfaction on LS
5.2.4. Impact of Life-Rhythm Satisfaction on LS
5.3. Potential Applications of Life Satisfaction Research in the Actual Operation of CEECFs
5.4. Limitations and Future Research Directions
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. World Social Report 2023: Leaving No One Behind in an Ageing World. Available online: https://desapublications.un.org/publications/world-social-report-2023-leaving-no-one-behind-ageing-world (accessed on 13 November 2024).
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) approach to healthy ageing. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, K. Healthy ageing begins with a healthy lifestyle. EBioMedicine 2023, 89, 104528. [Google Scholar]
- WHO. UN Decade of Healthy Ageing: Plan of Action. Available online: https://cdn.who.int/media/docs/default-source/decade-of-healthy-ageing/decade-proposal-final-apr2020-en.pdf?sfvrsn=b4b75ebc_28 (accessed on 13 November 2024).
- Jin, M.; Deng, Q.; Wang, S.; Wei, L. Equity evaluation of elderly-care institutions based on Ga2SFCA: The case study of Jinan, China. Sustainability 2023, 15, 16943. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, X.; Dong, Z.; Li, L.; Li, W.; Li, S. More Urban Elderly Care Facilities Should Be Placed in Densely Populated Areas for an Aging Wuhan of China. Land 2023, 12, 220. [Google Scholar] [CrossRef]
- Cao, M.; Guo, X.; Yu, H.; Chen, L.; McDonald, T.A. Chinese community-dwelling elders’ needs: Promoting ageing in place. Int. Nurs. Rev. 2014, 61, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Wu, M.; Guo, T.; Li, E. Research on the Construction of Tianjin Embedded Nursing Care Model. Chin. Nurs. Mag. 2018, 52, 84–89. [Google Scholar]
- Office of the State Council of the People’s Republic of China. Implementation Plan for the Construction of Urban Community Embedded Service Facilities. Available online: https://www.gov.cn/zhengce/zhengceku/202311/content_6917191.html (accessed on 15 November 2024).
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The satisfaction with life scale. J. Personal. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Zhang, H.; Wang, Y.; Wu, D.; Chen, J. Evolutionary path of factors influencing life satisfaction among Chinese elderly: A perspective of data visualization. Data 2018, 3, 35. [Google Scholar] [CrossRef]
- Hao, Y.; Wang, J. Life satisfaction and influencing factors of elderly people in Guangzhou endowment institutions. Chin. J. Gerontol. 2018, 38, 6101–6103. [Google Scholar]
- Zeng, Y.; Wang, L.; Zhang, L.; Weng, C.; Fang, Y. Influencing Factors on Life Satisfaction of the Elderly in Nursing Home: Based on Principal Component Logistic Regression. China Health Stat. 2018, 35, 699–702+706. [Google Scholar]
- Sun, Z.; Ge, Y.; Zhang, B. Research on the Impact of Providing Services to the Elderly at Home on Elderly Satisfaction–Analysis Based on Survey Data from Eight Provinces and Cities. Acad. J. Cent. Party Sch. Communist Party China (State Adm. Inst.) 2021, 25, 111–118. [Google Scholar]
- Li, W. Effects of child support on life satisfaction of elderly people living alone. Chin. J. Gerontol. 2017, 37, 5417–5419. [Google Scholar]
- Chen L, W.L. Effect of accessibility of community care services on life satisfaction of urban elderly. Chin. Oral Sci. 2023, 56–69. [Google Scholar]
- Wang, X.; Jia, W. Investigation on Real Status of Community Retirement & Primary Exploration on Satisfaction Evaluation Index for It. Archit. Sci. J. 2014, S2, 157–159. [Google Scholar]
- Wen, H.; Wang, Y. Satisfaction and Influencing Factors Analysis of Older People Lived in “Embedded” Nursing Home: Take Shanghai as an Example. J. Beijing Univ. Aeronaut. Astronaut. Sci. Ed. 2020, 33, 72–79. [Google Scholar] [CrossRef]
- Chang, X.; Zhang, Y.; Lei, X.; Luo, J.; Zhao, G. The demands and influencing factors of community “embedded” pension service among older adult. J. Nurs. 2022, 37, 91–93. [Google Scholar]
- Ying, Z. Study on the Demand for Embedded Elderly Care Services in Taiyuan City Based on the Kano Model. Master’s Thesis, Shanxi University of Finance and Economics, Taiyuan, China, 2024. [Google Scholar]
- Dian, L. A Study on Quality Evaluation of Community Embedded Elderly Services Based on SERVQUAL Modeling. Master’s Thesis, Sichuan University, Chengdu, China, 2023. [Google Scholar]
- Sa, Y.H.; Cho, S.J. Effect of the Facility Satisfaction, Anxiety, Self-esteem, Stress, and Depression of the Elderly in Care Facilities on Their Life Satisfaction. J. Korea Acad.-Ind. Coop. Soc. 2014, 15, 6998–7004. [Google Scholar]
- Hanif, N.R.; Abd Aziz, W.N.A.W.; Aini, A.M.; Wenjia, X.; Hua, A.K. Residents’ Level of Satisfaction about Retirement Home Facilities Based on the Happiness Index Measures. J. Des. Built Environ. 2018, 18, 1–15. [Google Scholar] [CrossRef][Green Version]
- Xu, S.; Zhang, T.; Fukuda, H.; He, J.; Bao, X. Comprehensive study of residential environment preferences and characteristics among older adults: Empirical evidence from China. Buildings 2024, 14, 2175. [Google Scholar] [CrossRef]
- Bengtsson, A.; Carlsson, G. Outdoor environments at three nursing homes-qualitative interviews with residents and next of kin. Urban For. Urban Green. 2013, 12, 393–400. [Google Scholar] [CrossRef]
- Junko, S.; Keiko, I.; Satoru, S.; Takahiro, T. The Relationship Between Residents’ Recognition of Nature and Satisfaction with Local Areas: For the purpose of town and city planning utilizing nature in local area in Kanagawa prefecture. Jpn. J. Environ. Eng. 2023, 88, 204–213. [Google Scholar]
- Fu, G.; Gai, Y.; Xiang, L.; Lin, L. Quantifying Older Adults’ Spatial Perceptions of Outdoor Activity Areas for Embedded Retirement Facilities. Buildings 2025, 15, 271. [Google Scholar] [CrossRef]
- Ng, S.T.; Tey, N.P.; Asadullah, M.N. What matters for life satisfaction among the oldest-old? Evidence from China. PLoS ONE 2017, 12, e0171799. [Google Scholar] [CrossRef] [PubMed]
- Ziolkowski, A.; Blachnio, A.; Pachalska, M. An evaluation of life satisfaction and health–Quality of life of senior citizens. Ann. Agric. Environ. Med. 2015, 22, 147–151. [Google Scholar] [CrossRef]
- Steptoe, A. Happiness and health. Annu. Rev. Public Health 2019, 40, 339–359. [Google Scholar] [CrossRef]
- Park, S.; Sok, S.R. Relation modeling of factors influencing life satisfaction and adaptation of Korean older adults in long-term care facilities. Int. J. Environ. Res. Public Health 2020, 17, 317. [Google Scholar] [CrossRef]
- Zhu, C.; Zhou, L.; Zhang, X.; Walsh, C.A. Reciprocal effects between sleep quality and life satisfaction in older adults: The mediating role of health status. Healthcare 2023, 11, 1912. [Google Scholar] [CrossRef]
- Pan, Y.; Chan, S.H.; Xu, Y.; Yeung, K.C. Determinants of life satisfaction and self-perception of ageing among elderly people in China: An exploratory study in comparison between physical and social functioning. Arch. Gerontol. Geriatr. 2019, 84, 103910. [Google Scholar] [CrossRef]
- Kim, M.S.; Ko, J.W. Study on the determinants of life satisfaction among the elderly: An integrative approach. J. Korea Contents Assoc. 2013, 13, 246–259. [Google Scholar] [CrossRef]
- Chen, X.; Silverstein, M. Intergenerational social support and the psychological well-being of older parents in China. Res. Aging 2000, 22, 43–65. [Google Scholar] [CrossRef]
- Yanık, A.; Sağlam, Y. Evaluating the perception of life satisfaction and social support of the elderly ındividuals. J. Health Sci. Prof. 2019, 6, 501–512. [Google Scholar] [CrossRef]
- Zhang, Z.; Yan, Z.; Mao, Y. Effect of the establishment of age-friendly communities on the life satisfaction levels of the elderly in Beijing. J. Tsinghua Univ. (Sci. Technol.) 2025, 65, 12–21. [Google Scholar]
- Ng, S.T.; Tey, N.P.; Yew, S.Y.; Sia, B.K.; Long, B.S. Effects of quality of service and activities on life satisfaction of residents in nursing homes. Wulfenia J. 2012, 19, 153–160. [Google Scholar]
- Jinrong, H.; Keke, Z. Demand Level and Precise Supply Order of Embedded EldercareService in Communities: Take Xi’an as an Example. Sci. Res. Aging 2024, 12, 48–61. [Google Scholar]
- Kewen, Z.; Ran, Y.; Jieyu, L.; Yuqi, J.; Jiayi, Z.; Yuhan, Z.; Lijuan, X. A Demand Analysis on Community Embedded Elderly Care ServicesBased on KANO Model. J. Lishui Univ. 2022, 44, 102–109. [Google Scholar]
- Yue, K. The Progress of the Community-based Integrated Care System for the Elderly in Japan and its Experiences. J. Beijing Union Univ. Soc. Sci. 2017, 15, 110–117. [Google Scholar] [CrossRef]
- Luo, P.; Yu, S.; Lei, F.; Yang, Y. Experience and inspiration of elderly care services and planning in Japanese aging citiesfrom the perspective of community embedding. J. Hum. Settlements West China 2024, 39, 8–14. [Google Scholar] [CrossRef]
- Huan, Z.; Guohong, J. Community Embedded Pension Model SWOT Analysis. Chin. J. Gerontol. 2021, 41, 439–443. [Google Scholar]
- Wang, S.; Yang, R.; Mu, L.; Zhang, M.; Li, P.; Liu, X. SWOT Analysis of Community Embedded Elderly Care Services from the Perspectives of Elderly Care Managers and the Elderly. J. Nurs. Sci. 2023, 38, 88–92. [Google Scholar]
- Hu, H.; Wang, Y.; Wang, X.; Zhang, L. Situation Evaluation and Improving Pathof Embedded Retirement Pattern. Soc. Secur. Stud. 2015, 10–17. [Google Scholar]
- Du, P.; Ma, Q. Community-embedded Elderly Care in China: Brief Analysis of Current Situations and Issues. Popul. Dev. 2024, 30, 113–124. [Google Scholar]
- Yuan, Y.; Chen, Y.; Liu, Y.; Ding, K. The neighborhood effect of residential greenery on residents’self-rated health: A case study of Guangzhou, China. Acta Geogr. Sin. 2021, 76, 1965–1975. [Google Scholar]
- Qi, L. Research on Optimization of Community-embedded Elderly CareService Model in Yangquan City. Master’s Thesis, Xi’an University of Architecture and Technology, Xi’an, China, 2024. [Google Scholar]
- Li, J.; Chen, N.; Yuan, Y.; Chen, Y. Research on the planning of elderly care facilities in large cities under the background of positive aging—Taking the planning of embedded elderly care service institutions in Guangzhou as an example. Shanghai Urban Plan. Rev. 2024, 55–61. [Google Scholar]
- National Bureau of Statistics of China. 2020 7th National Population Census. Available online: https://www.gov.cn/guoqing/2021-05/13/content_5606149.htm (accessed on 15 May 2024).
- Tianjin Municipal Bureau of Statistics. Tianjin Statistical Yearbook. Available online: https://stats.tj.gov.cn/nianjian/2022nj/zk/indexch.htm (accessed on 15 May 2024).
- Tianjin Civil Affairs Bureau Publicly Available List of Senior Social care Service Centers operated by Tianjin Municipal Society for the Elderly (as of the End of 2020). Available online: https://mz.tj.gov.cn/tjsmzjylc/gspd/sqylfwss/202107/t20210714_5509166.html (accessed on 15 May 2024).
- Tianjin Civil Affairs Bureau Guidelines on Promoting the Development of Community-Embedded Elderly Service Organizations. Available online: https://mz.tj.gov.cn/ZWGK5878/ZCFG9602/zcwj/202112/t20211230_5766473.html (accessed on 15 May 2024).
- Xiao, S.; Li, L.; Ma, J.; Liu, D.; Li, J. A study of residents’ intentions to participate in the renovation of older communities under the perspective of urban renewal: Evidence from Zhangjiakou, China. J. Asian Archit. Build. Eng. 2023, 22, 1094–1109. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, Q.W.; Tao, Y.Y.; Xie, W.W. Empirical study of consumption behavior of college students under the influence of internet-based financing services. Procedia Comput. Sci. 2021, 187, 152–157. [Google Scholar] [CrossRef]
- Zhang, J.; Gao, R.; Hu, J.; Zheng, Y. Application comparison of grey correlation degree and Pearson correlation coefficient. J. Chifeng Univ 2014, 21, 1–2. [Google Scholar]
- Kim, S.; Jeon, S. The Impact of Housing Vulnerability on the Relationship Between Social Capital, Residential Satisfaction, and Attitudes Toward Disadvantaged Groups in South Korea. Buildings 2024, 15, 36. [Google Scholar] [CrossRef]
- Jiao, J.; Shi, L.; Yang, M.; Yang, J.; Liu, M.; Sun, G. The impact of containment policy and mobility on COVID-19 cases through structural equation model in Chile, Singapore, South Korea and Israel. PeerJ 2023, 11, e15769. [Google Scholar] [CrossRef]
- Li, Y.; Wu, Y.; Luo, Y.; Fu, Z.; Zhang, S. The Influence of Smart Green Spaces on Environmental Awareness, Social Cohesion, and Life Satisfaction in High-Rise Residential Communities. Buildings 2024, 14, 2917. [Google Scholar] [CrossRef]
- Bagozzi, R.P.; Yi, Y. On the evaluation of structural equation models. J. Acad. Mark. Sci. 1988, 16, 74–94. [Google Scholar] [CrossRef]
- Borg, C.; Hallberg, I.R.; Blomqvist, K. Life satisfaction among older people (65+) with reduced self-care capacity: The relationship to social, health and financial aspects. J. Clin. Nurs. 2006, 15, 607–618. [Google Scholar] [CrossRef] [PubMed]
- Baird, B.M.; Lucas, R.E.; Donnellan, M.B. Life satisfaction across the lifespan: Findings from two nationally representative panel studies. Soc. Indic. Res. 2010, 99, 183–203. [Google Scholar] [CrossRef]
- Chen, C. Aging and life satisfaction. Soc. Indic. Res. 2001, 54, 57–79. [Google Scholar] [CrossRef]
- Angelini, V.; Cavapozzi, D.; Corazzini, L.; Paccagnella, O. Age, health and life satisfaction among older Europeans. Soc. Indic. Res. 2012, 105, 293–308. [Google Scholar] [CrossRef]
- Cho, D.; Cheon, W. Older adults’ advance aging and life satisfaction levels: Effects of lifestyles and health capabilities. Behav. Sci. 2023, 13, 293. [Google Scholar] [CrossRef]
- Goodrow, B.; Bohnenblust, S.; Staynings, A. Health and life satisfaction among nursing home residents in Europe and the United States. J.-Am. Health Care Assoc. 1979, 5, 49–52. [Google Scholar]
- Celik, S.S.; Celik, Y.; Hikmet, N.; Khan, M.M. Factors affecting life satisfaction of older adults in Turkey. Int. J. Aging Hum. Dev. 2018, 87, 392–414. [Google Scholar] [CrossRef] [PubMed]
- Sulandari, S.; Johnson, J.; Coats, R.O. Life satisfaction and its associated factors among young and older adults in the United Kingdom (UK). Aging Ment. Health 2024, 1–9. [Google Scholar] [CrossRef]
- Kahneman, D.; Deaton, A. High income improves evaluation of life but not emotional well-being. Proc. Natl. Acad. Sci. USA 2010, 107, 16489–16493. [Google Scholar] [CrossRef]
- Blanchflower, D.G.; Oswald, A.J. Is well-being U-shaped over the life cycle? Soc. Sci. Med. 2008, 66, 1733–1749. [Google Scholar] [CrossRef]
- Diener, E.; Ng, W.; Harter, J.; Arora, R. Wealth and happiness across the world: Material prosperity predicts life evaluation, whereas psychosocial prosperity predicts positive feeling. J. Personal. Soc. Psychol. 2010, 99, 52. [Google Scholar] [CrossRef] [PubMed]
- Brownie, S.; Horstmanshof, L.; Garbutt, R. Factors that impact residents’ transition and psychological adjustment to long-term aged care: A systematic literature review. Int. J. Nurs. Stud. 2014, 51, 1654–1666. [Google Scholar] [CrossRef] [PubMed]
- Infurna, F.J. and Gerstorf, D.; Ram, N.; Schupp, J.; Wagner, G.G. Long-term antecedents and outcomes of perceived control. Psychol. Aging 2011, 26, 559. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.-H.; Kao, C.-C.; Ying, J.C. Functional capacity and life satisfaction in older adult residents living in long-term care facilities: The mediator of autonomy. J. Nurs. Res. 2020, 28, e102. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.A.; Levin, C.A.; Lowe, T.J.; Robertson, B.; Akincigil, A.; Sambamoorthi, U.; Bilder, S.; Paek, E.K.; Crystal, S. The relationship between organizational factors and resident satisfaction with nursing home care and life. J. Aging Soc. Policy 2007, 19, 125–151. [Google Scholar] [CrossRef]
- Han, J.; Wang, M.; Li, J.; Ma, H. A Review of Comparative Research on the EvaluationSystems of Age-Friendly Communities Abroad. Archit. J. 2024, 56–62. [Google Scholar] [CrossRef]
- Cramm, J.M.; Van Dijk, H.M.; Nieboer, A.P. The importance of neighborhood social cohesion and social capital for the well being of older adults in the community. Gerontologist 2013, 53, 142–152. [Google Scholar] [CrossRef]
- Cramm, J.M.; Nieboer, A.P. Social cohesion and belonging predict the well-being of community-dwelling older people. BMC Geriatr. 2015, 15, 30. [Google Scholar] [CrossRef]
- Gao, J.; Weaver, S.R.; Fu, H.; Jia, Y.; Li, J. Relationships between neighborhood attributes and subjective well-being among the Chinese elderly: Data from Shanghai. Biosci. Trends 2017, 11, 516–523. [Google Scholar] [CrossRef]
- Kruzich, J.M.; Clinton, J.F.; Kelber, S.T. Personal and environmental influences on nursing home satisfaction. Gerontologist 1992, 32, 342–350. [Google Scholar] [CrossRef]
- Bangerter, L.R.; Heid, A.R.; Abbott, K.; Van Haitsma, K. Honoring the everyday preferences of nursing home residents: Perceived choice and satisfaction with care. Gerontologist 2017, 57, 479–486. [Google Scholar] [CrossRef]
- Haugan, G. The relationship between nurse–patient interaction and meaning-in-life in cognitively intact nursing home patients. J. Adv. Nurs. 2014, 70, 107–120. [Google Scholar] [CrossRef]
- Gutiérrez, M.; Tomás, J.; Galiana, L.; Sancho, P.; Cebrià, M. Predicting life satisfaction of the Angolan elderly: A structural model. Aging Ment. Health 2013, 17, 94–101. [Google Scholar] [CrossRef]
- Li, L.M.W.; Hamamura, T. Cultural fit and life satisfaction: Endorsement of cultural values predicts life satisfaction only in collectivistic societies. J. Psychol. Chin. Soc. 2010, 11, 109. [Google Scholar]
- Fernández-Portero, C.; Alarcón, D.; Padura, Á.B. Dwelling conditions and life satisfaction of older people through residential satisfaction. J. Environ. Psychol. 2017, 49, 1–7. [Google Scholar] [CrossRef]
- Moen, P.; Erickson, M.A. Decision-making and satisfaction with a continuing care retirement community. In Housing Choices and Well-Being of Older Adults; Routledge: Abingdon, UK, 2013; pp. 53–69. [Google Scholar]
- Prawitz, A.D.; Wozniak, P. Selection of a Continuing Care Retirement Community: Does Extent of Search Help Predict Resident Satisfaction? J. Hous. Elder. 2005, 19, 27–48. [Google Scholar] [CrossRef]
- Zhu, W.; Wang, Y.; Tang, J.; Wang, F. Sleep quality as a mediator between family function and life satisfaction among Chinese older adults in nursing home. BMC Geriatr. 2024, 24, 379. [Google Scholar] [CrossRef] [PubMed]
- Pilcher, J.J.; Callan, C.; Posey, J.L. Sleep deprivation affects reactivity to positive but not negative stimuli. J. Psychosom. Res. 2015, 79, 657–662. [Google Scholar] [CrossRef] [PubMed]
- Gueldner, S.H.; Loeb, S.; Morris, D.; Penrod, J.; Bramlett, M.; Johnston, L.; Schlotzhauer, P. A comparison of life satisfaction and mood in nursing home residents and community-dwelling elders. Arch. Psychiatr. Nurs. 2001, 15, 232–240. [Google Scholar] [CrossRef]





| Living Environment Satisfaction | Health Status Satisfaction | Social Relationship Satisfaction | Life-Rhythm Satisfaction | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Daily Life Space | Accessi Bility | Lighting and Ventilation | Outdoor Activities | Toilet and Bathroom | Medical Rehabilitation Equipment | Self-Evaluated Health Status | Physical Health Status | Mental Health Status | Sleep | With Family | With Other Users | With Staff | Social Activities | Quality of Service | Activity Status | |
| Sa, Young-Haw et al. [22] | ◯ | ◯ | △ | |||||||||||||
| Noor Rosly Hanif et al. [23] | ◯ | ◯ | ◯ | ◯ | ||||||||||||
| Anna Bengtsson et al. [24] | ◯ | |||||||||||||||
| Junko SATO et al. [25] | ◯ | |||||||||||||||
| Sor Tho Ng et al. [26] | △ | △ | △ | |||||||||||||
| Artur Ziółkowski et al. [27] | △ | △ | △ | |||||||||||||
| Andrew Steptoe [28] | △ | △ | ||||||||||||||
| Soonyoung Park et al. [29] | △ | △ | △ | □ | ||||||||||||
| Zhu, Change et al. [30] | △ | |||||||||||||||
| Pan, Y. et al. [31] | □ | □ | ||||||||||||||
| Kim, Myeong-Su et al. [32] | □ | ▲ | ||||||||||||||
| Xuan Chen et al. [33] | □ | |||||||||||||||
| Aygül YANIK et al. [34] | □ | □ | ▲ | |||||||||||||
| Tey, N.P et al. [35] | ▲ | ▲ | ||||||||||||||
| Region | Population (Persons) | Percentage of Population Aged 60 (%) | Average Aging Rate (%) | |
|---|---|---|---|---|
| Tianjin | 13,866,009 | 21.66 | 21.66 (±0) | |
| Six central urban districts | Heping | 355,000 | 22.11 | 28.12 (+6.46) |
| Hedong | 858,787 | 28.84 | ||
| Hexi | 822,174 | 28.00 | ||
| Nankai | 890,422 | 28.07 | ||
| Hebei | 647,702 | 30.98 | ||
| Hongqiao | 483,130 | 30.73 | ||
| Surrounding 4 districts | Dongli | 857,027 | 18.31 | 19.42 (−2.24) |
| Xiqing | 1,195,124 | 16.47 | ||
| Jinnan | 928,066 | 15.90 | ||
| Beichen | 909,643 | 20.53 | ||
| Suburban 5 districts | Wuqing | 1,151,313 | 19.86 | 21.53 (−0.13) |
| Baodi | 722,367 | 21.96 | ||
| Ninghe | 395,314 | 22.58 | ||
| Jingha | 787,106 | 18.66 | ||
| Jingha | 795,516 | 22.78 | ||
| Binhai New District | 2,067,318 | 17.15 | 17.15 (−4.51) | |
| Survey Items | |
|---|---|
| Living Environment Satisfaction | L1. Comfort and spaciousness of the shared activity space |
| L2. Comfort and spaciousness of the bedroom | |
| L3. The quietness of the bedroom | |
| L4. Ease of access from the bedroom to the LD (living/dining room) | |
| L5. Diversity of room choices for shared activity space | |
| L6. Satisfaction with lighting and ventilation | |
| L7. Ease of use and spaciousness of outdoor activities | |
| L8. Cleanliness of the living environment | |
| L9. Ease of use and spaciousness of toilets and bathrooms | |
| L10.Ease of use of barrier-free facilities | |
| L11.Ease of use of medical rehabilitation equipment | |
| Health Status Satisfaction | H1. Changes in health status after moving |
| H2. Frequency of body pain | |
| H3. Frequency of stress | |
| H4. Sleep status | |
| Social Relationship Satisfaction | S1. Family Relationship Status |
| S2. Relationship status with other users | |
| S3. Relationship status with staff | |
| S4. Frequency of use of shared activity spaces | |
| S5. Participation in social activities | |
| Life-rhythm Satisfaction | R1. Timeliness of needs being met |
| R2. Expertise in receiving services | |
| R3. Satisfaction with the response to the sudden situation | |
| R4. Satisfaction with the implementation of care type activities | |
| R5. Satisfaction with the implementation of health type activities | |
| R6. Satisfaction with the implementation of leisure type activities | |
| R7. Satisfaction with the implementation status of free activity type activities |
| Facility Number | Number of Beds | Number of Resident Users | Participants (%) | Number of Staff | Participants (%) |
|---|---|---|---|---|---|
| 1 | 22 | 20 | 18 | 9 | 9 |
| 2 | 12 + 2 | 10 | 7 | 6 | 6 |
| 3 | 12 + 2 | 12 | 10 | 7 | 7 |
| 4 | 13 | 11 | 11 | 6 | 8 |
| 5 | 12 | 11 | 7 | 5 | 5 |
| 6 | 24 | 21 | 18 | 8 | 8 |
| 7 | 27 + 2 | 23 | 18 | 9 | 9 |
| 8 | 23 + 2 | 16 | 14 | 8 | 8 |
| 9 | 17 | 14 | 12 | 5 | 5 |
| 10 | 10 + 2 | 8 | 6 | 4 | 4 |
| 11 | 30 | 24 | 19 | 6 | 6 |
| 12 | 15 | 13 | 10 | 5 | 5 |
| 13 | 14 | 13 | 8 | 6 | 6 |
| Total | 231 + 10 | 196 | 158 (80.6%) | 84 | 84 (100%) |
| Survey of Residents | |
|---|---|
| Content (Questions) | User characteristics survey: age, gender, level of care, marital status, child status, income status, usage time, willingness to stay. |
| LS survey: Table 1 presents 27 questions related to four dimensions—life satisfaction, health satisfaction, social relationship satisfaction, and life rhythm satisfaction—as well as overall life satisfaction. | |
| Method | Surveys, interviews |
| Survey of Staff | |
| Content (Questions) | Staff characteristics survey: age, gender, household registration, qualification certificate, training participation status, working years |
| Method | Surveys |
| Survey of Facilities | |
| Content (Questions) | Data on the built environment of the 13 facilities: per capita shared-space area, per capita bedroom area, number of people in the bedroom, the positional relationship between the bedroom and LD, the distance between the bedroom door and LD, the space layout form, bedroom window status, LD window status, the number of available shared-space rooms, outdoor space status, bedroom toilet status |
| Method | Field measurements |
| Cronbach’s | N of Items |
|---|---|
| 0.949 | 27 |
| KMO | 0.919 | |
|---|---|---|
| Bartlett’s Test of Sphericity | Approx. Chi-Square | 3739.333 |
| df | 351 | |
| sig. | 0.000 |
| Frequency | Percentage% | ||
|---|---|---|---|
| Gender | Male | 67 | 43.2 |
| Female | 88 | 56.8 | |
| Age | 60–69 | 5 | 3.2 |
| 70–79 | 38 | 24.5 | |
| 80–89 | 99 | 62.7 | |
| 90– | 16 | 10.3 | |
| Degree of nursing care | Support 2 | 2 | 1.3 |
| Nursing care 1 | 39 | 24.7 | |
| Nursing care 2 | 74 | 46.8 | |
| Nursing care 3 | 30 | 27.2 | |
| Marriage status | Married (couple) | 30 | 19.0 |
| Married (now living alone) | 121 | 76.6 | |
| Unmarried | 7 | 4.4 | |
| Child status | None | 8 | 5.1 |
| 1 | 8 | 5.1 | |
| 2 | 73 | 46.2 | |
| 3 | 51 | 32.3 | |
| More than 4 | 18 | 11.4 | |
| Income status | –3000 | 2 | 1.3 |
| 3001–5000 | 94 | 59.5 | |
| 5001–8000 | 49 | 31.0 | |
| More than 8001 | 13 | 8.2 | |
| Usage time | Less than 1 year | 28 | 17.7 |
| 1–2 years | 47 | 29.7 | |
| 2–3 years | 51 | 32.3 | |
| 3–4 years | 25 | 15.8 | |
| More than 4 years | 7 | 4.4 | |
| Willingness to stay | Self-determination | 12 | 7.6 |
| Decision with family | 98 | 62.0 | |
| Decision by family | 48 | 30.4 |
| Frequency | Percentage% | ||
|---|---|---|---|
| Gender | Male | 20 | 23.8 |
| Female | 62 | 76.2 | |
| Age | 20– | 5 | 6.0 |
| 30– | 8 | 9.5 | |
| 40– | 33 | 39.3 | |
| 50– | 34 | 40.5 | |
| 60– | 4 | 4.8 | |
| Education | Elementary school | 11 | 13.1 |
| Junior High School | 38 | 45.2 | |
| High school (vocational school) | 22 | 26.2 | |
| University | 13 | 15.5 | |
| Household registration | Local residents | 30 | 35.7 |
| Non-local residents | 54 | 64.3 | |
| Qualification certificate | Have | 52 | 61.9 |
| Do not have | 32 | 38.1 | |
| Training status | Participation | 46 | 54.8 |
| Non-participation | 38 | 45.2 | |
| Average length of service | Less than 1 year | 5 | 6.0 |
| 1–3 years | 18 | 21.4 | |
| 3–5 years | 18 | 21.4 | |
| More than 5 years | 43 | 51.2 |
| No | Floor Area | Architectural Form | Shared-Space Area/Person | Bedroom Area/Person | The Number of Rooms for Shared Space | LD Windows | Outdoor Space |
|---|---|---|---|---|---|---|---|
| 1 | 585 m2 | second-floor independent | 9.0 m2 | 7.2 m2 | 12 | ◯× | ◯ |
| 2 | 298 m2 | first-floor composite | 6.6 m2 | 7.5 m2 | 6 | × | × |
| 3 | 597 m2 | second-floor composite | 11.8 m2 | 13.2 m2 | 9 | ◯ | × |
| 4 | 630 m2 | second-floor composite | 7.1 m2 | 12.1 m2 | 3 | × | × |
| 5 | 220 m2 | first-floor independent | 2.1 m2 | 9.7 m2 | 3 | ◯ | × |
| 6 | 699 m2 | second-floor composite | 10.5 m2 | 9.4 m2 | 5 | ◯ | × |
| 7 | 618 m2 | second-floor composite | 9.5 m2 | 8.6 m2 | 9 | ◯ | ◯ |
| 8 | 547 m2 | first-floor composite | 9.1 m2 | 8.0 m2 | 6 | ◯ | × |
| 9 | 309 m2 | first-floor independent | 7.1 m2 | 7.0 m2 | 4 | ◯ | ◯ |
| 10 | 296 m2 | first-floor composite | 9.7 m2 | 9.4 m2 | 4 | ◯ | × |
| 11 | 430 m2 | first-floor composite | 5.2 m2 | 6.1 m2 | 6 | ◯ | × |
| 12 | 276 m2 | first-floor composite | 5.1 m2 | 6.3 m2 | 3 | × | × |
| 13 | 228 m2 | second-floor composite | 9.1 m2 | 7.1 m2 | 8 | ◯ | × |
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Cronbach’s Alpha Coefficient | |
|---|---|---|---|---|---|
| L9 | 0.865 | 0.890 | |||
| L2 | 0.859 | ||||
| L6 | 0.859 | ||||
| L4 | 0.743 | ||||
| H2 | 0.853 | 0.852 | |||
| H4 | 0.801 | ||||
| H3 | 0.780 | ||||
| S2 | 0.853 | 0.911 | |||
| S3 | 0.812 | ||||
| S1 | 0.810 | ||||
| S5 | 0.760 | ||||
| R4 | 0.877 | 0.871 | |||
| R1 | 0.844 | ||||
| R5 | 0.810 |
| Mean Variance Extracted AVE Value | Composite Reliability CR | |
|---|---|---|
| Factor 1 | 0.677 | 0.893 |
| Factor 2 | 0.664 | 0.855 |
| Factor 3 | 0.742 | 0.919 |
| Factor 4 | 0.706 | 0.877 |
| Index Name | Meaning | Value | Standard | Result |
|---|---|---|---|---|
| CMIN/df | Chi-square degree of freedom ratio | 2.174 | <3.0 | Acceptable |
| CFI | Comparative fit index | 0.955 | >0.9 | Acceptable |
| RMR | Root mean square residual | 0.029 | <0.1 | Acceptable |
| GFI | Goodness of fit index | 0.865 | >0.8 | Acceptable |
| NFI | Normative fit index | 0.921 | >0.9 | Acceptable |
| TLI | Tucker–Lewis index | 0.942 | >0.9 | Acceptable |
| Variable Relationship | Value | p Value | Test Result |
|---|---|---|---|
| LS<—LE | 0.283 | *** | Acceptable |
| LS<—SR | 0.325 | *** | Acceptable |
| LS<—LR | 0.244 | *** | Acceptable |
| LS<—HS | 0.272 | *** | Acceptable |
| LE<–>HS | 0.134 | *** | Acceptable |
| LE<–>SR | 0.221 | *** | Acceptable |
| LE<–>LR | 0.158 | *** | Acceptable |
| HS<–>SR | 0.245 | *** | Acceptable |
| HS<–>LR | 0.189 | *** | Acceptable |
| SR<–>LR | 0.179 | *** | Acceptable |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, X.; Nakayama, T. Empirical Research on the Life Satisfaction and Influencing Factors of Users of Community-Embedded Elderly Care Facilities. Buildings 2025, 15, 894. https://doi.org/10.3390/buildings15060894
Hu X, Nakayama T. Empirical Research on the Life Satisfaction and Influencing Factors of Users of Community-Embedded Elderly Care Facilities. Buildings. 2025; 15(6):894. https://doi.org/10.3390/buildings15060894
Chicago/Turabian StyleHu, Xiaoni, and Toru Nakayama. 2025. "Empirical Research on the Life Satisfaction and Influencing Factors of Users of Community-Embedded Elderly Care Facilities" Buildings 15, no. 6: 894. https://doi.org/10.3390/buildings15060894
APA StyleHu, X., & Nakayama, T. (2025). Empirical Research on the Life Satisfaction and Influencing Factors of Users of Community-Embedded Elderly Care Facilities. Buildings, 15(6), 894. https://doi.org/10.3390/buildings15060894





