Thermal Comfort Differences Between the Elderly and Young People Under Different Infrared Radiation Conditions: A Quantitative Study Based on Subjective Evaluation and EEG Characteristics
Abstract
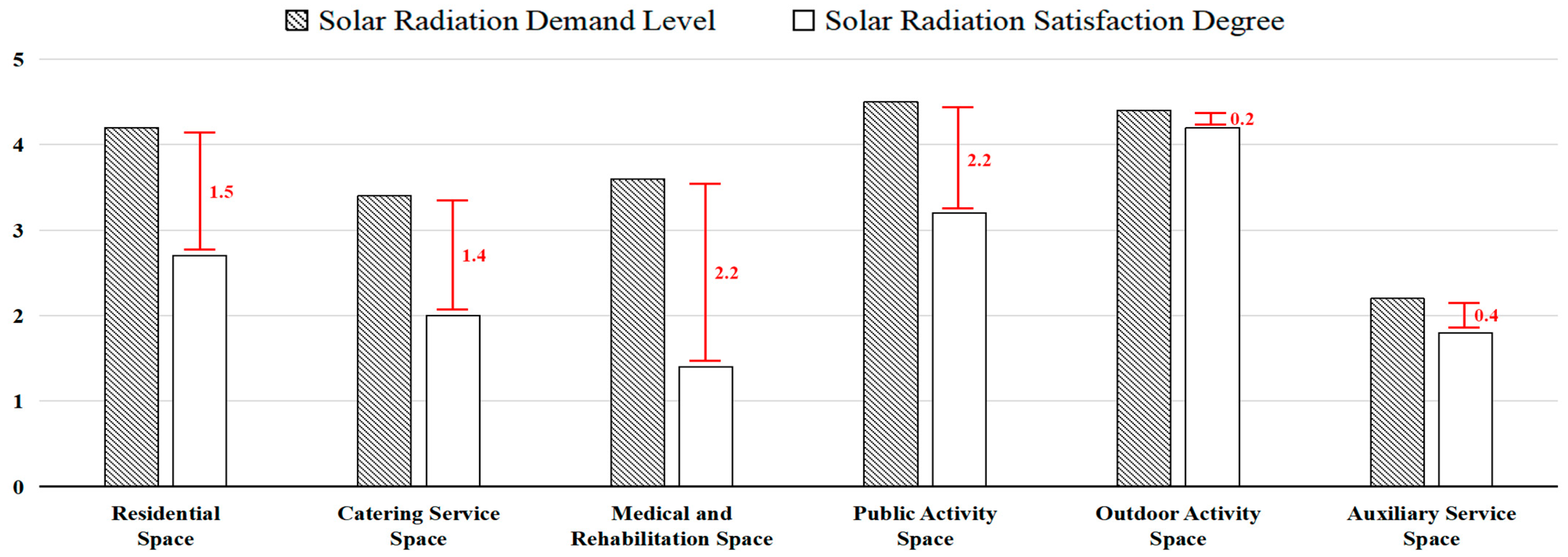
1. Introduction
- (1)
- What effects do different infrared radiation conditions have on the subjective thermal comfort of the elderly and young people?
- (2)
- What are the differences in EEG power changes between the elderly and young people under infrared radiation?
- (3)
- Which EEG channel or frequency band best reflects thermal comfort in the elderly and young people?
2. Methods
2.1. Experimental Protocol
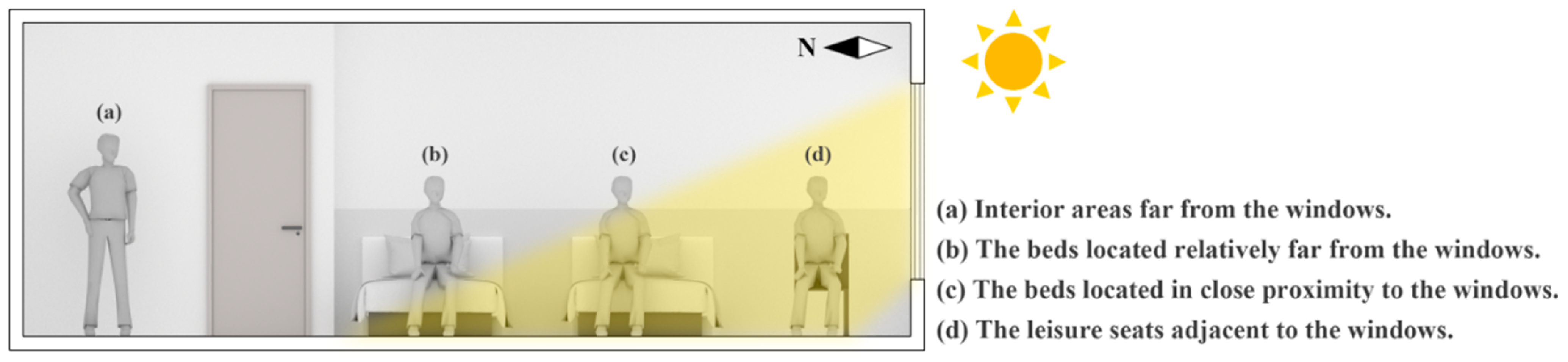
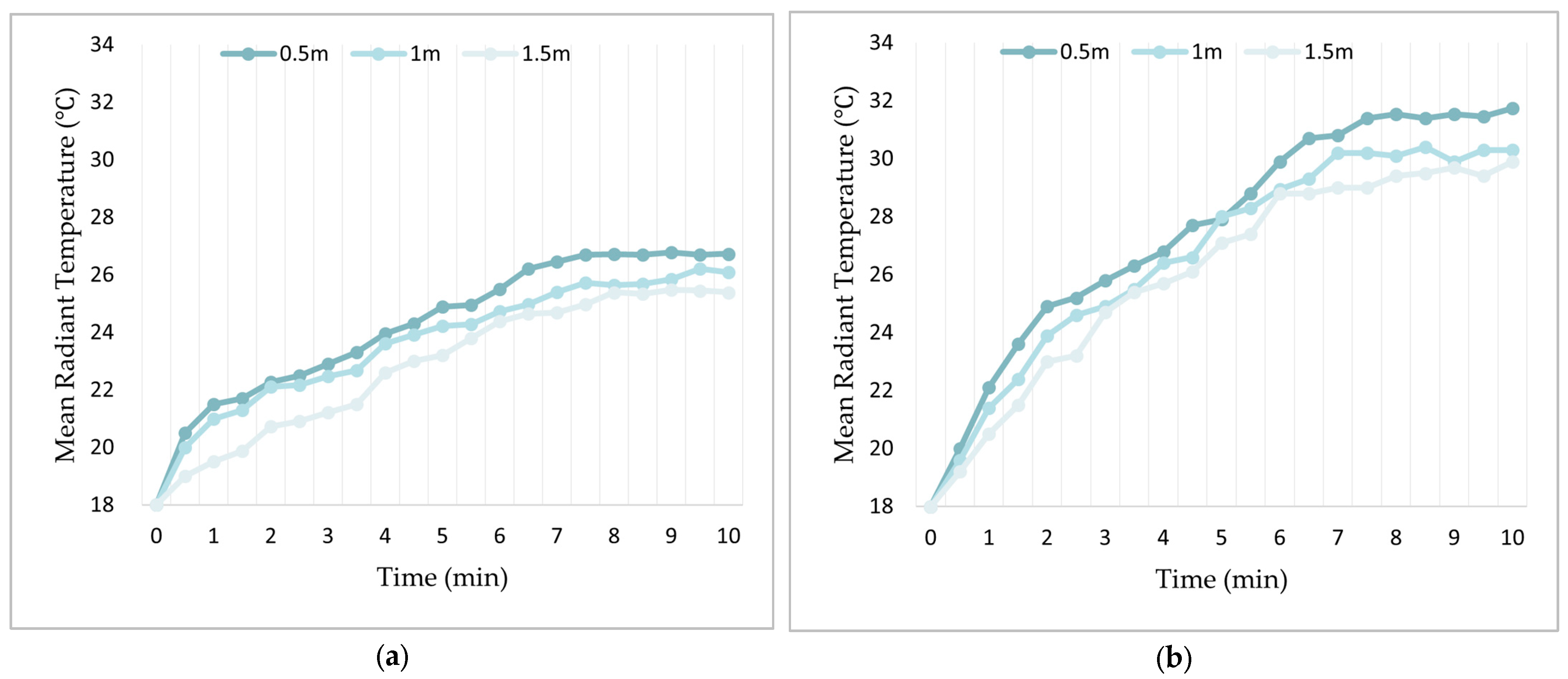
2.1.1. Determination of Experimental Conditions
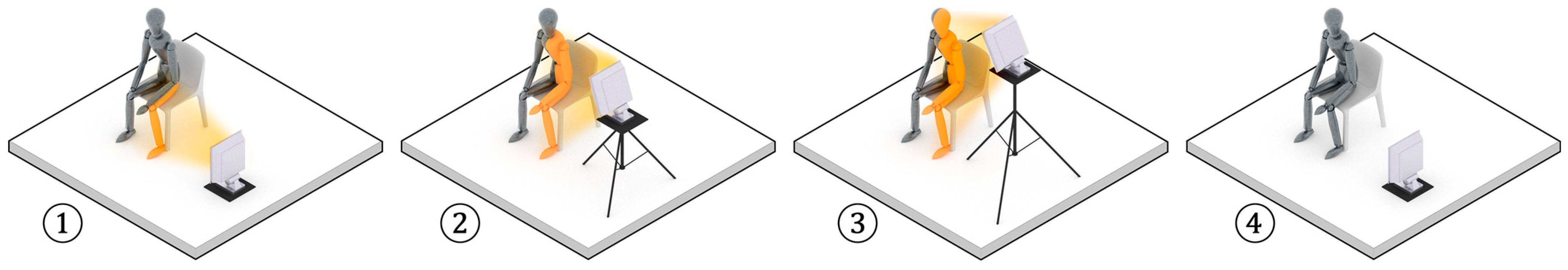
2.1.2. Selection and Arrangement of Infrared Radiators
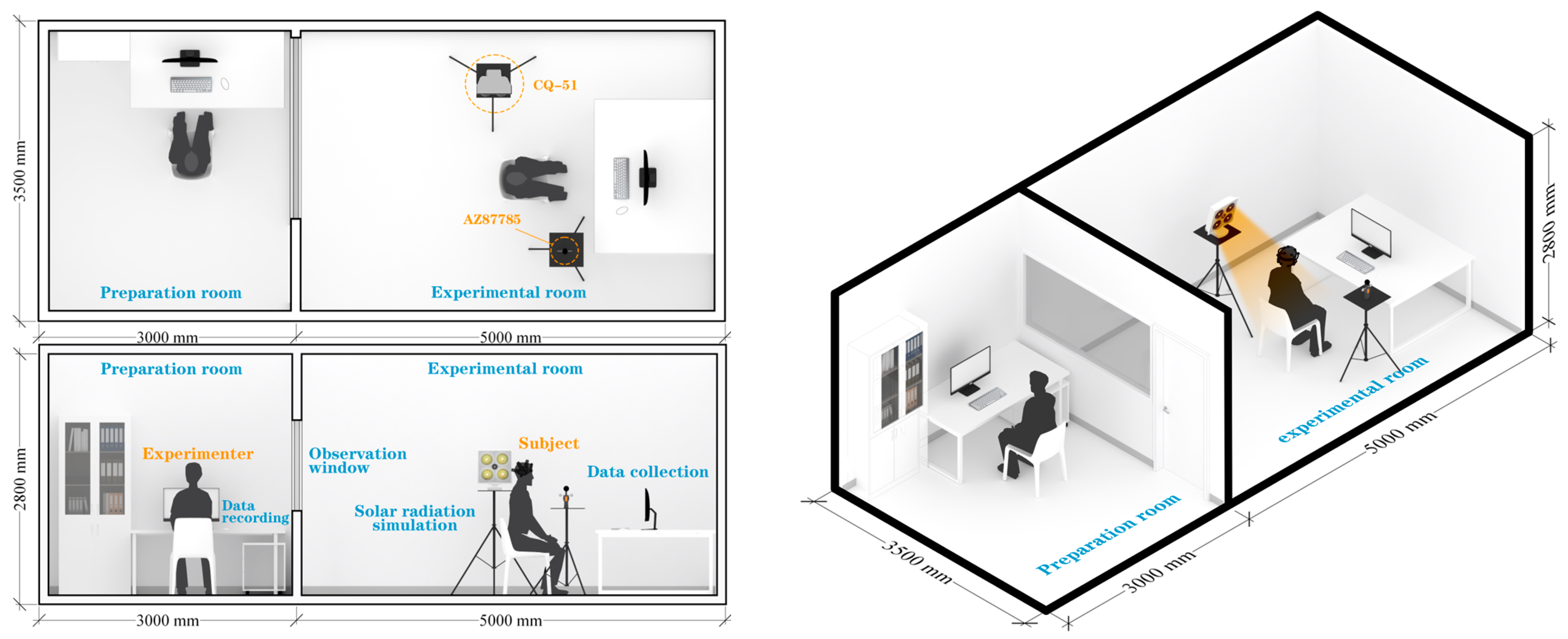
2.1.3. Laboratory Layout
2.2. Participants
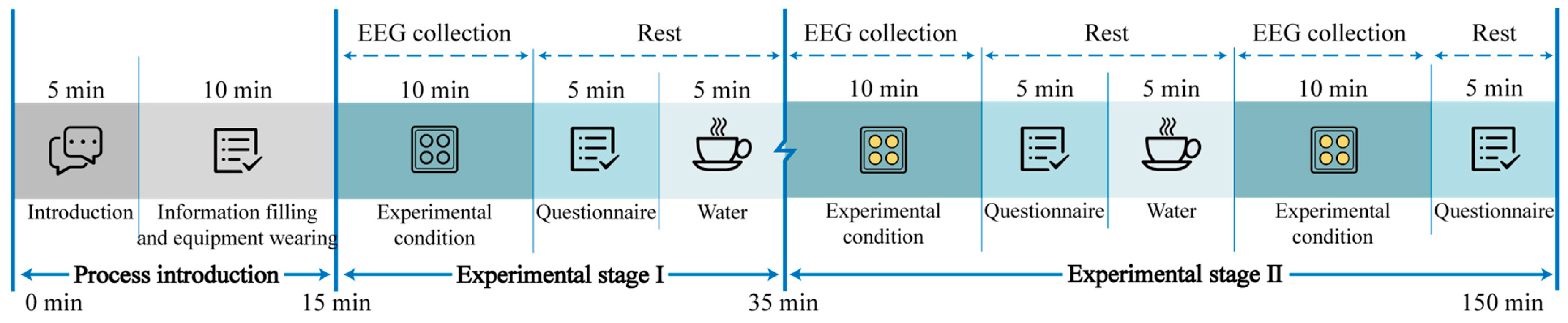
2.3. Procedure of Experiments
2.4. Data Collection and Processing
2.4.1. Subjective Questionnaires
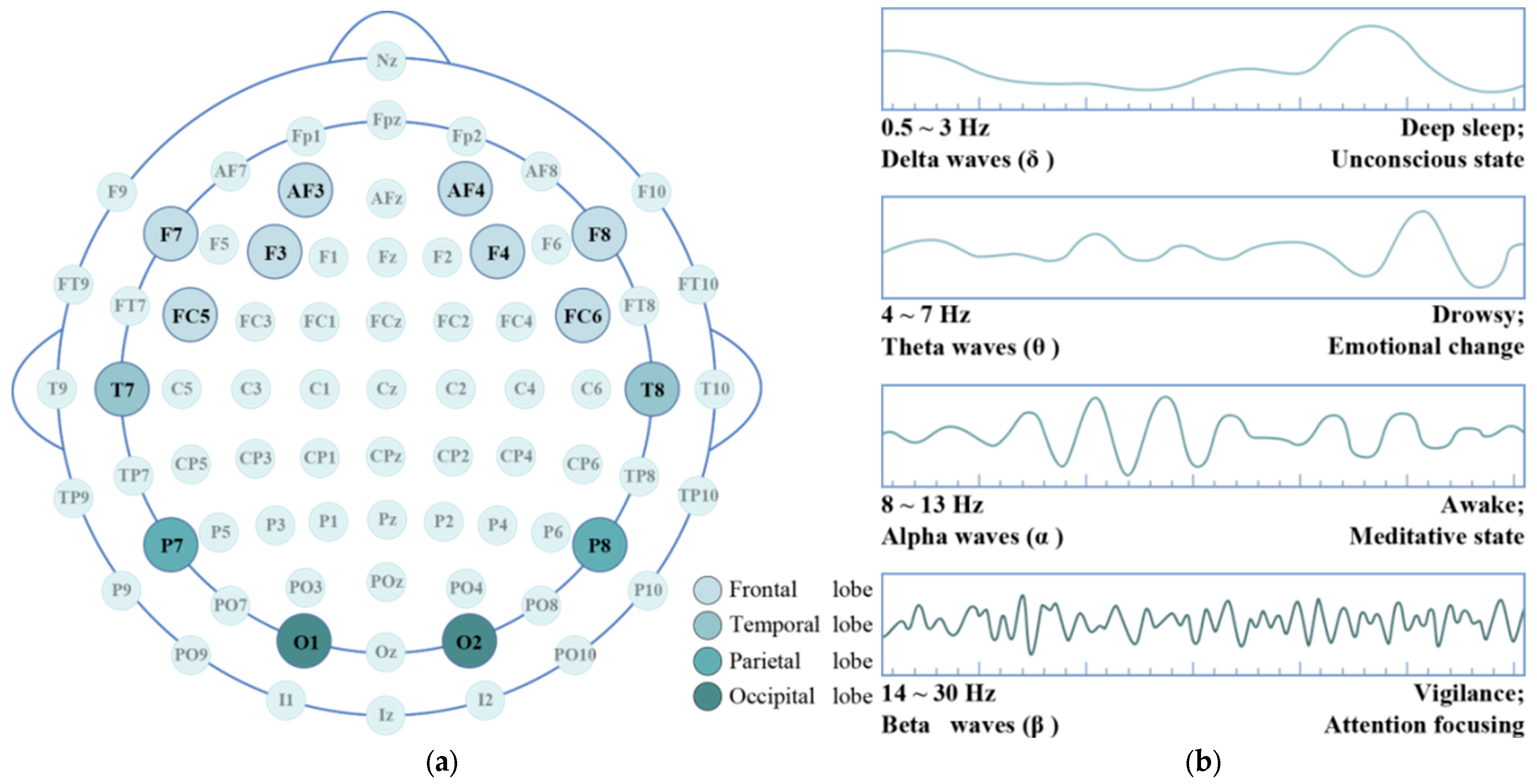
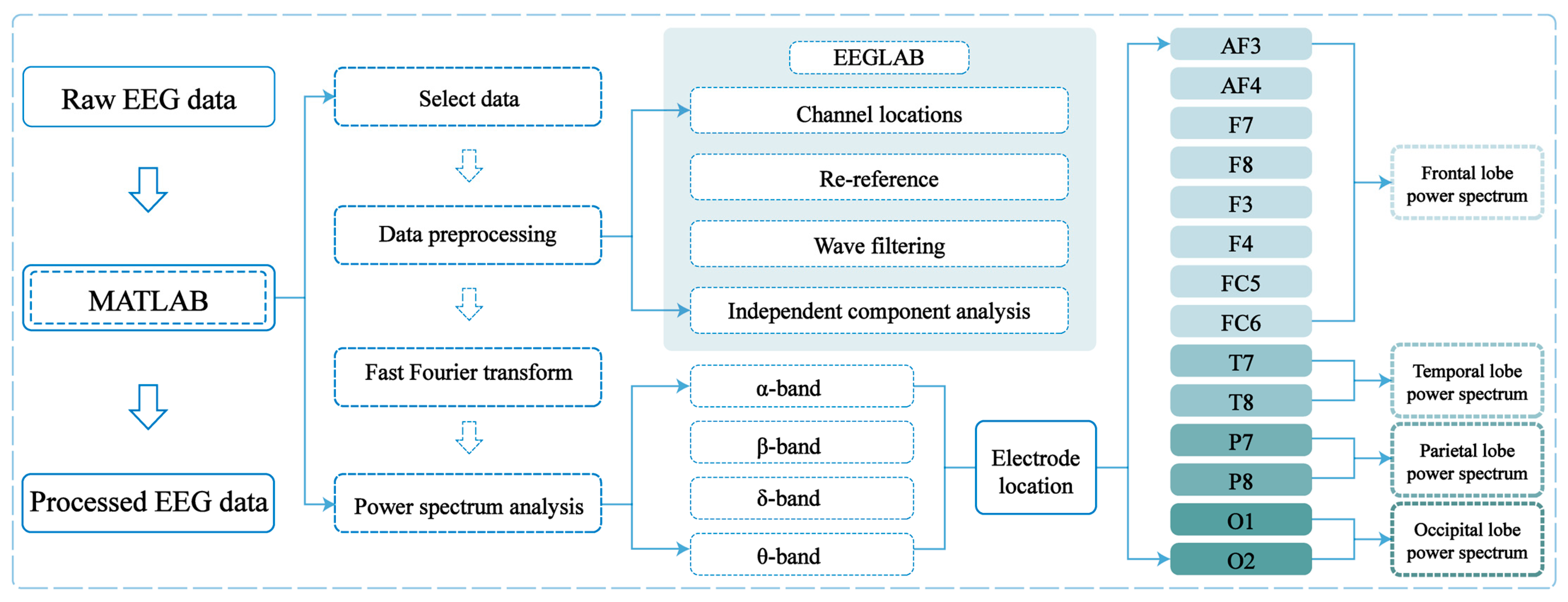
2.4.2. EEG Signals
3. Results
3.1. Results of Subjective Evaluation
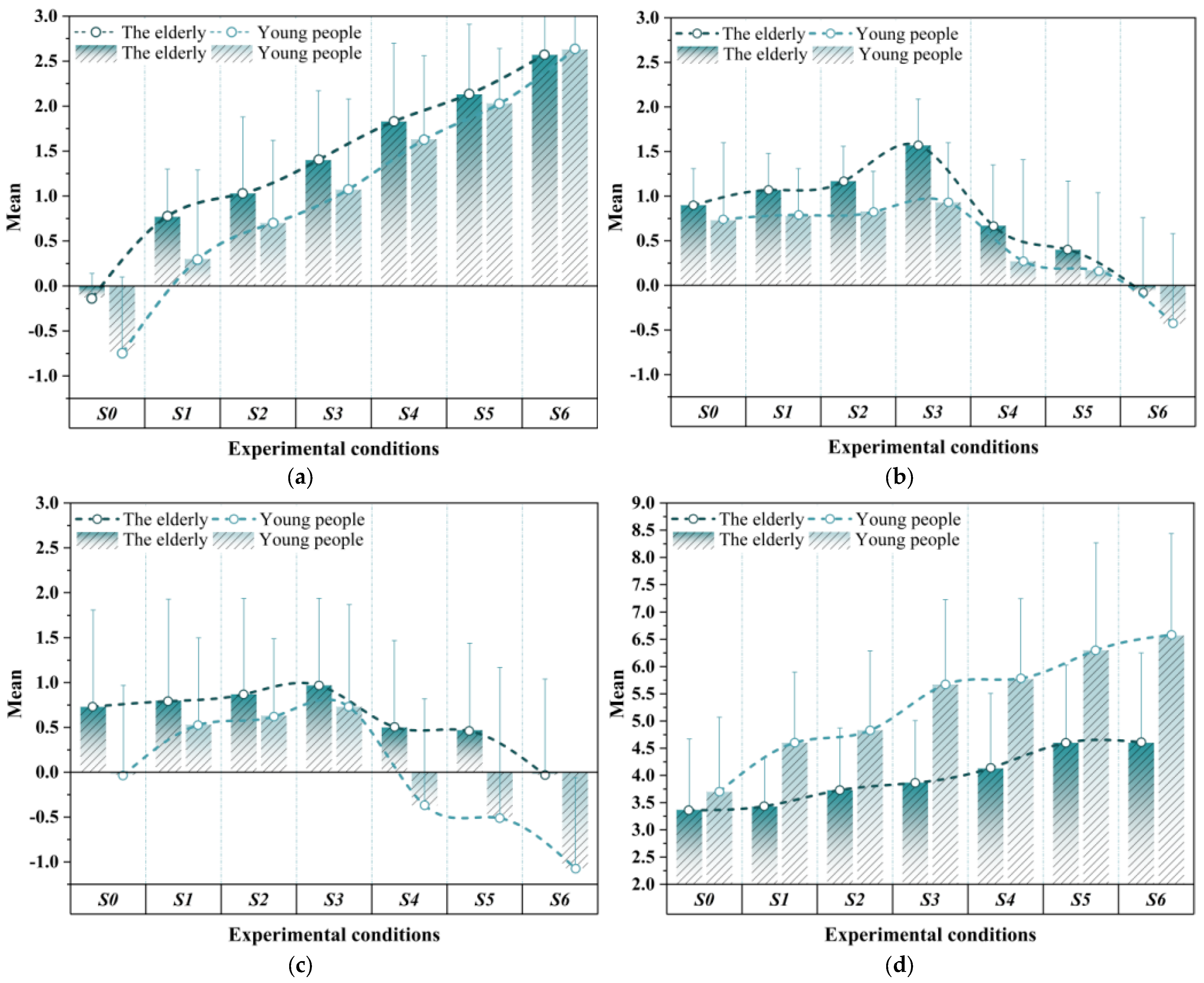
3.1.1. TSV
3.1.2. TCV
3.1.3. RSV
3.1.4. ALV
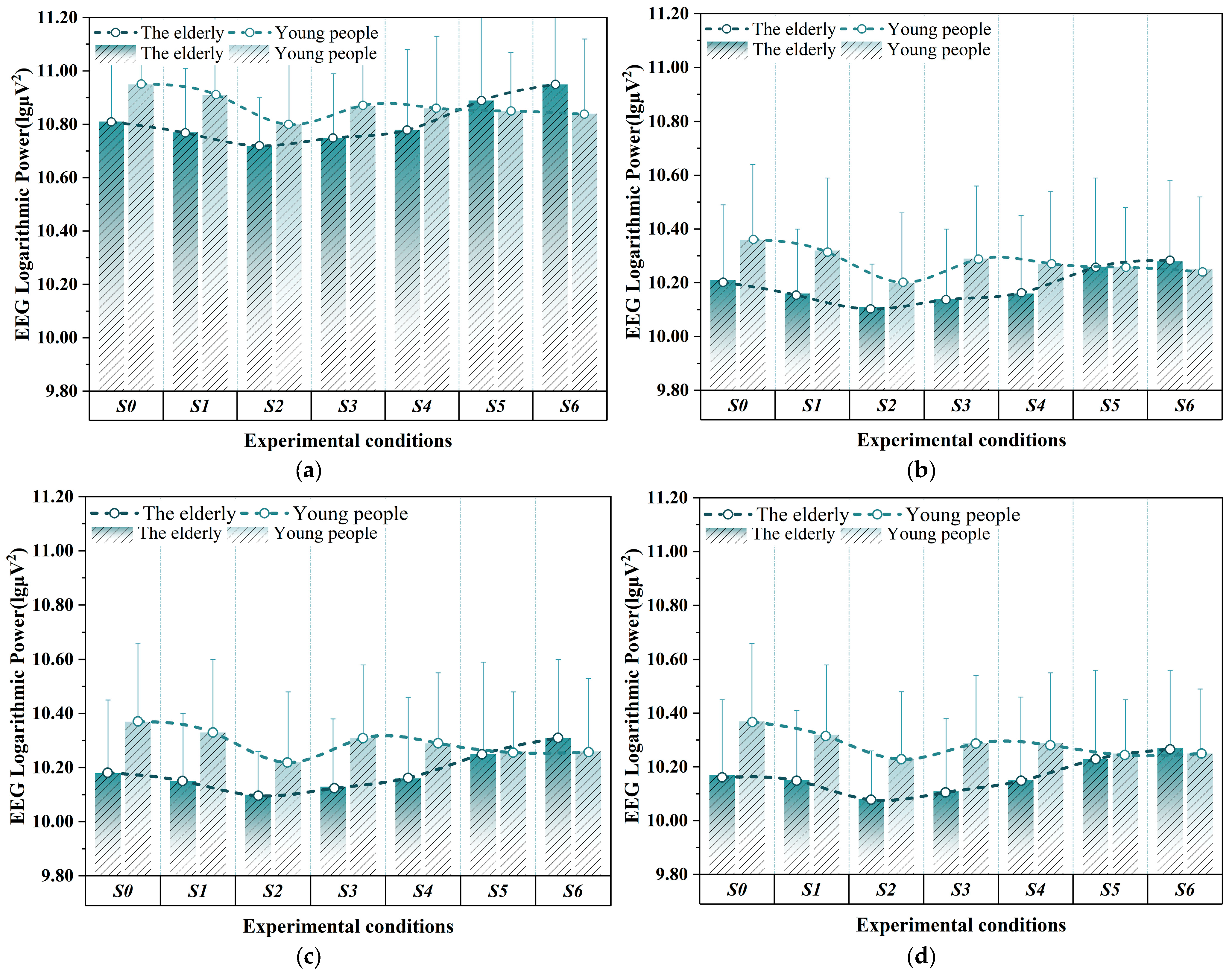
3.2. Results of EEG Features
3.2.1. Brain Region Power
3.2.2. Band Power
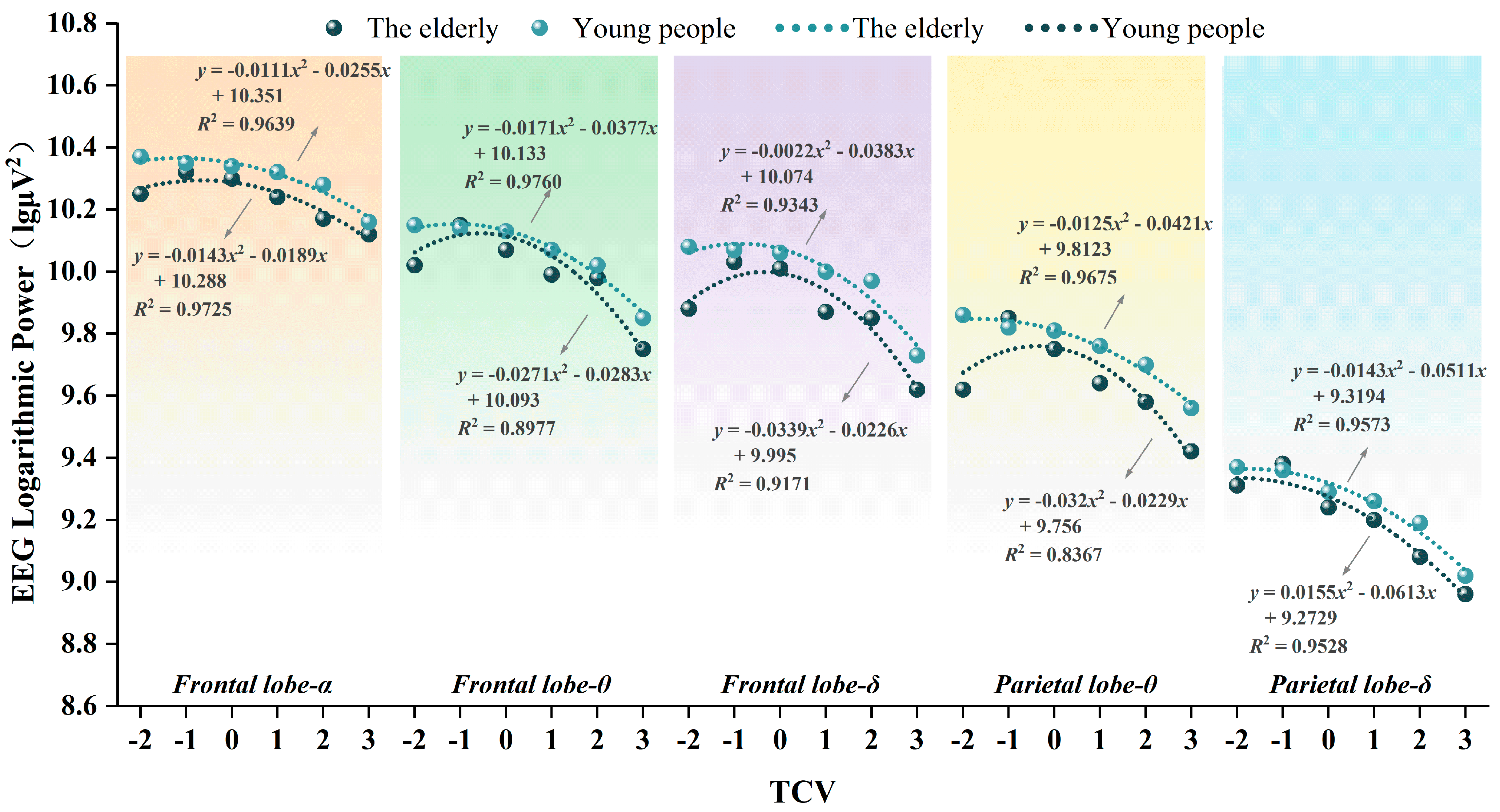
3.3. Comprehensive Evaluation Between EEG and TCV
4. Discussion
4.1. Subjective Evaluations
4.1.1. Evaluation of Thermal Environment
4.1.2. Evaluation of Mental State
4.2. EEG Features
4.3. Correlation Between Subjective Evaluation and EEG Features
4.4. Application and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kinsella, K.; Phillips, D. Global Aging: The Challenge of Success. Popul. Bull. 2005, 60, 5–42. [Google Scholar]
- Feng, Z. Global Convergence: Aging and Long-Term Care Policy Challenges in the Developing World. J. Aging Soc. Policy 2019, 31, 291–297. [Google Scholar] [CrossRef]
- Bloom, D.E.; Canning, D.; Lubet, A. Global Population Aging: Facts, Challenges, Solutions & Perspectives. Daedalus 2015, 144, 80–92. [Google Scholar] [CrossRef]
- Khan, H.T.A. Population Ageing in a Globalized World: Risks and Dilemmas? J. Eval. Clin. Pract. 2019, 25, 754–760. [Google Scholar] [CrossRef] [PubMed]
- Khajehzadeh, I.; Vale, B. How New Zealanders Distribute Their Daily Time between Home Indoors, Home Outdoors and out of Home. Kōtuitui N. Z. J. Soc. Sci. Online 2017, 12, 17–31. [Google Scholar] [CrossRef]
- Lewis, T.; Holcombe-James, I.; Glover, A. More than Just ‘Working from Home’: Domestic Space, Economies and Living Infrastructures during and beyond Pandemic Times. Cult. Stud. 2024, 38, 299–321. [Google Scholar] [CrossRef]
- Fletcher, M.J.; Johnston, D.K.; Glew, D.W.; Parker, J.M. An Empirical Evaluation of Temporal Overheating in an Assisted Living Passivhaus Dwelling in the UK. Build. Environ. 2017, 121, 106–118. [Google Scholar] [CrossRef]
- Almeida-Silva, M.; Wolterbeek, H.T.; Almeida, S.M. Elderly Exposure to Indoor Air Pollutants. Atmos. Environ. 2014, 85, 54–63. [Google Scholar] [CrossRef]
- Baniassadi, A.; Lipsitz, L.; Pascual-Leone, A.; Manor, B.; Yu, W. A Platform to Study the Effects of Home Environment on Health and Wellbeing of Older Adults. Innov. Aging 2021, 5, 965. [Google Scholar] [CrossRef]
- Engineer, A.; Sternberg, E.M.; Najafi, B. Designing Interiors to Mitigate Physical and Cognitive Deficits Related to Aging and to Promote Longevity in Older Adults: A Review. Gerontology 2018, 64, 612–622. [Google Scholar] [CrossRef]
- Tsoulou, I.; Taylor, J.; Symonds, P.; Mohajeri, N.; Davies, M. Improving Indoor Thermal Comfort, Air Quality and the Health of Older Adults through Environmental Policies in London. J. Phys. Conf. Ser. 2021, 2069, 012240. [Google Scholar] [CrossRef]
- Rajapaksha, I.; Sandamini, R.G.P. Appraising Indoor Thermal Perception of Elderly in Hot Climates: An Experimental Investigation of Free-Running Residential Aged Care Homes in Colombo. In Proceedings of the Faculty of Architecture Research Unit (FARU), Moratuwa, Katubedda, 3–5 December 2021. [Google Scholar] [CrossRef]
- Traynor, V.; Fernandez, R.; Caldwell, K. What Are the Effects of Spending Time Outdoors in Daylight on the Physical Health of Older People and Family Carers: A Systematic Review Protocol. JBI Evid. Synth. 2013, 11, 76. [Google Scholar] [CrossRef]
- Hodder, S.; Parsons, K. The Effects of Solar Radiation and Black Body Re-Radiation on Thermal Comfort. Ergonomics 2008, 51, 476–491. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Gao, Y.; Wang, Y.; Meng, X. Effects of Solar Radiation on Thermal Sensation and Physical Fatigue of the Human Body under Heavy-Load Exercise. Indoor Built Environ. 2022, 31, 7–16. [Google Scholar] [CrossRef]
- Otani, H.; Goto, T.; Goto, H.; Hosokawa, Y.; Shirato, M. Solar Radiation Exposure Has Diurnal Effects on Thermoregulatory Responses During High-Intensity Exercise in the Heat Outdoors. J. Strength Cond. Res. 2019, 33, 2608. [Google Scholar] [CrossRef]
- Hendler, E.; Hardy, J.D. Infrared and Microwave Effects on Skin Heating and Temperature Sensation. IRE Trans. Med. Electron. 1960, ME-7, 143–152. [Google Scholar] [CrossRef]
- Meffert, H.; Piazena, H. Wirkungen Künstlich Erzeugter Infra-rotstrahlung Auf Den Menschen. Aktuelle Dermatol. 2002, 28, 187–192. [Google Scholar] [CrossRef]
- Van Hoof, J. Forty Years of Fanger’s Model of Thermal Comfort: Comfort for All? Abstract. Indoor Air 2008, 18, 182–201. [Google Scholar] [CrossRef]
- Taylor, N.A.; Allsopp, N.K.; Parkes, D.G. Preferred Room Temperature of Young vs Aged Males: The Influence of Thermal Sensation, Thermal Comfort, and Affect. J. Gerontol. A Biol. Sci. Med. Sci. 1995, 50, M216–M221. [Google Scholar] [CrossRef]
- Kalmár, F. An Indoor Environment Evaluation by Gender and Age Using an Advanced Personalized Ventilation System. Build. Serv. Eng. Res. Technol. 2017, 38, 505–521. [Google Scholar] [CrossRef]
- Soebarto, V.; Zhang, H.; Schiavon, S. A Thermal Comfort Environmental Chamber Study of Older and Younger People. Build. Environ. 2019, 155, 1–14. [Google Scholar] [CrossRef]
- Schellen, L.; Van Marken Lichtenbelt, W.D.; Loomans, M.G.L.C.; Toftum, J.; De Wit, M.H. Differences between Young Adults and Elderly in Thermal Comfort, Productivity, and Thermal Physiology in Response to a Moderate Temperature Drift and a Steady-State Condition. Indoor Air 2010, 20, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Yokoe, A.; Mitsuda, M.; Tanamura, T.; Yamaha, M.; Nepal, B. Observed Thermal and Odor Environment in Elderly Welfare Facilities: Results of Summer Survey on Two Facilities in Kasugai City. J. Environ. Eng. (Trans. AIJ) 2020, 85, 29–35. [Google Scholar] [CrossRef]
- Yi, C.y.; Childs, C.; Peng, C.; Robinson, D. Thermal Comfort Modelling of Older People Living in Care Homes: An Evaluation of Heat Balance, Adaptive Comfort, and Thermographic Methods. Build. Environ. 2022, 207, 108550. [Google Scholar] [CrossRef]
- Itani, M.; Ghaddar, N.; Ghali, K.; Laouadi, A. Development of Heat Stress Charts for Older People under Indoor Environmental Conditions. Energy Build. 2020, 224, 110274. [Google Scholar] [CrossRef]
- Zhang, Z.; Wu, Y.; Liu, H.; Li, B.; Kosonen, R. Experimental Study on the Thermal Comfort and Physiological Responses of the Elderly in Unstable Environments. In Proceedings of the 16th ROOMVENT Conference (ROOMVENT 2022), Xi’an, China, 16–19 September 2022; Volume 356, p. 03011. [Google Scholar] [CrossRef]
- Mansi, S.A.; Barone, G.; Forzano, C.; Pigliautile, I.; Ferrara, M.; Pisello, A.L.; Arnesano, M. Measuring Human Physiological Indices for Thermal Comfort Assessment through Wearable Devices: A Review. Measurement 2021, 183, 109872. [Google Scholar] [CrossRef]
- Wu, M.; Li, H.; Qi, H. Using Electroencephalogram to Continuously Discriminate Feelings of Personal Thermal Comfort between Uncomfortably Hot and Comfortable Environments. Indoor Air 2020, 30, 534–543. [Google Scholar] [CrossRef]
- Tuţă, L.; Roşu, G.; Popovici, C.; Nicolaescu, I. Real- Time EEG Data Processing Using Independent Component Analysis (ICA). In Proceedings of the 2022 14th International Conference on Communications (COMM), Bucharest, Romania, 16–18 June 2022; pp. 1–4. [Google Scholar]
- Kirschstein, T.; Köhling, R. What Is the Source of the EEG? Clin. EEG Neurosci. 2009, 40, 146–149. [Google Scholar] [CrossRef]
- Hu, S.; Lu, M.; He, M.; Wang, G.; Liang, P.; Tong, L.; Liu, G. Research on the Light Comfort Characterization Method Based on Visual Evoked Potential Energy. Build. Environ. 2021, 197, 107831. [Google Scholar] [CrossRef]
- Loughran, S.P.; Verrender, A.; Dalecki, A.; Burdon, C.A.; Tagami, K.; Park, J.; Taylor, N.A.S.; Croft, R.J. Radiofrequency Electromagnetic Field Exposure and the Resting EEG: Exploring the Thermal Mechanism Hypothesis. Int. J. Environ. Res. Public Health 2019, 16, 1505. [Google Scholar] [CrossRef]
- Yao, Y.; Lian, Z.; Liu, W.; Jiang, C.; Liu, Y.; Lu, H. Heart Rate Variation and Electroencephalograph--the Potential Physiological Factors for Thermal Comfort Study. Indoor Air 2009, 19, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Lian, Z.; Liu, W.; Shen, Q. Experimental Study on Physiological Responses and Thermal Comfort under Various Ambient Temperatures. Physiol. Behav. 2008, 93, 310–321. [Google Scholar] [CrossRef] [PubMed]
- Lv, B.; Su, C.; Yang, L.; Wu, T. Effects of Stimulus Mode and Ambient Temperature on Cerebral Responses to Local Thermal Stimulation: An EEG Study. Int. J. Psychophysiol. 2017, 113, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Al-Dabbas, M.A. Heating by Catalytic Gas Infrared Rays. Energy Eng. 2011, 108, 26–45. [Google Scholar] [CrossRef]
- Petras, D.; Kalús, D. Effect of Thermal Comfort/Discomfort Due to Infrared Heaters Installed at Workplaces in Industrial Buildings. Indoor Built Environ. 2000, 9, 148–156. [Google Scholar] [CrossRef]
- Hirn, T.; Kirmas, A.; Backes, D.; Eckstein, L. Impact of Different Radiation Types on Thermal Comfort Modelling. In Proceedings of the Comfort Congress 2021 Proceedings, Nottingham, UK, 2–3 September 2021. [Google Scholar]
- ISO 7726: 2023; Ergonomics of the Thermal Environment—Instruments for Measuring and Monitoring Physical Quantities. ISO: Geneva, Switzerland, 2023.
- Yao, F.; Fang, H.; Han, J.; Zhang, Y. Study on the Outdoor Thermal Comfort Evaluation of the Elderly in the Tibetan Plateau. Sustain. Cities Soc. 2022, 77, 103582. [Google Scholar] [CrossRef]
- Hu, J.; Lyu, C.; Hou, Y.; Zhu, N.; Liu, K. Research on Summer Indoor Air Conditioning Design Parameters in Haikou City: A Field Study of Indoor Thermal Perception and Comfort. Sustainability 2024, 16, 3864. [Google Scholar] [CrossRef]
- GB/T 50785-2012; Evaluation Standard for Indoor Thermal and Humid Environment of Civil Buildings. Standardization Administration of the People’s Republic of China & Ministry of Housing and Urban-Rural Development of the People’s Republic of China: Beijing, China, 2012.
- Wu, Z.; Li, N.; Schiavon, S. Experimental Evaluation of Thermal Comfort, SBS Symptoms and Physiological Responses in a Radiant Ceiling Cooling Environment under Temperature Step-Changes. Build. Environ. 2022, 224, 109512. [Google Scholar] [CrossRef]
- Smallcombe, J.W.; Foster, J.; Hodder, S.G.; Jay, O.; Flouris, A.D.; Havenith, G. Quantifying the Impact of Heat on Human Physical Work Capacity; Part IV: Interactions between Work Duration and Heat Stress Severity. Int. J. Biometeorol. 2022, 66, 2463–2476. [Google Scholar] [CrossRef]
- Sun, R.; Xu, S.; Han, Y.; Zhuang, D.; Yan, B.; Sun, C. Exploring Impacts of Thermal and Lighting Conditions on Office Workers’ Subjective Evaluations, Cognitive Performance and EEG Features in Multi-Person Offices. J. Build. Eng. 2024, 95, 110170. [Google Scholar] [CrossRef]
- Shahid, A.; Wilkinson, K.; Marcu, S.; Shapiro, C. STOP, THAT and One Hundred Other Sleep Scales; Springer: Berlin/Heidelberg, Germany, 2012; ISBN 978-1-4419-9892-7. [Google Scholar]
- Gwak, J.; Shino, M.; Ueda, K.; Kamata, M. An Investigation of the Effects of Changes in the Indoor Ambient Temperature on Arousal Level, Thermal Comfort, and Physiological Indices. Appl. Sci. 2019, 9, 899. [Google Scholar] [CrossRef]
- Yadav, H.; Maini, S. Electroencephalogram Based Brain-Computer Interface: Applications, Challenges, and Opportunities. Multimed. Tools Appl. 2023, 82, 47003–47047. [Google Scholar] [CrossRef]
- López-Hernández, J.L.; González-Carrasco, I.; López-Cuadrado, J.L.; Ruiz-Mezcua, B. Framework for the Classification of Emotions in People With Visual Disabilities Through Brain Signals. Front. Neuroinform. 2021, 15, 642766. [Google Scholar] [CrossRef]
- Chu, H.; Cao, Y.; Jiang, J.; Yang, J.; Huang, M.; Li, Q.; Jiang, C.; Jiao, X. Optimized Electroencephalogram and Functional Near-Infrared Spectroscopy-Based Mental Workload Detection Method for Practical Applications. Biomed. Eng. OnLine 2022, 21, 9. [Google Scholar] [CrossRef]
- Wang, Z.; Hu, C.; Liu, W.; Zhou, X.; Zhao, X. EEG-Based High-Performance Depression State Recognition. Front. Neurosci. 2024, 17, 1301214. [Google Scholar] [CrossRef] [PubMed]
- Naydenov, C.; Yordanova, A.; Mancheva, V. Methodology for EEG and Reference Values of the Software Analysis. Open Access Maced. J. Med. Sci. 2022, 10, 2351–2354. [Google Scholar] [CrossRef]
- Frank, S.M.; Raja, S.N.; Bulcao, C.; Goldstein, D.S. Age-Related Thermoregulatory Differences during Core Cooling in Humans. Am. J. Physiol -Regul. Integr. Comp. Physiol. 2000, 279, R349–R354. [Google Scholar] [CrossRef] [PubMed]
- Tsuzuki, K.; Ohfuku, T. Thermal Sensation and Thermoregulation in Elderly Compared to Young People in Japanese Winter Season. In Proceedings of the Indoor Air 2002, Monterey, CA, USA, 30 June–5 July 2002. [Google Scholar]
- Umemiya, N.; Terao, K.; Chen, Y. Difference of Cooling Use during Sleep between Elderly and Young People. J. Phys. Conf. Ser. 2021, 2069, 012239. [Google Scholar] [CrossRef]
- McKenna, Z.J.; Foster, J.; Atkins, W.C.; Belval, L.N.; Watso, J.C.; Jarrard, C.P.; Orth, B.D.; Crandall, C.G. Age Alters the Thermoregulatory Responses to Extreme Heat Exposure with Accompanying Activities of Daily Living. J. Appl. Physiol. 2023, 135, 445–455. [Google Scholar] [CrossRef]
- Navas-Martín, M.Á.; López-Bueno, J.A.; Ascaso-Sánchez, M.S.; Follos, F.; Vellón, J.M.; Mirón, I.J.; Luna, M.Y.; Sánchez-Martínez, G.; Linares, C.; Díaz, J. Heat Adaptation among the Elderly in Spain (1983–2018). IJERPH 2023, 20, 1314. [Google Scholar] [CrossRef]
- Mukhopadhyay, B.; Weitz, C.A. Heat Exposure, Heat-Related Symptoms and Coping Strategies among Elderly Residents of Urban Slums and Rural Vilages in West Bengal, India. IJERPH 2022, 19, 12446. [Google Scholar] [CrossRef]
- Sun, N.; Ding, X.; Bi, J.; Cui, Y. Field Study on Winter Thermal Comfort of Occupants of Nursing Homes in Shandong Province, China. Buildings 2024, 14, 2881. [Google Scholar] [CrossRef]
- Robison, M.K.; Diede, N.T.; Nicosia, J.; Ball, H.; Bugg, J. A Multimodal Analysis of Sustained Attention in Younger and Older Adults. Psychol. Aging 2021, 37, 307–325. [Google Scholar] [CrossRef]
- Murty, D.V.P.S.; Manikandan, K.; Kumar, W.S.; Ramesh, R.G.; Purokayastha, S.; Javali, M.; Rao, N.P.; Ray, S. Gamma Oscillations Weaken with Age in Healthy Elderly in Human EEG. Neuroimage 2020, 215, 116826. [Google Scholar] [CrossRef]
- Laouadi, A. A New General Formulation for the PMV Thermal Comfort Index. Buildings 2022, 12, 1572. [Google Scholar] [CrossRef]
- Zhang, H.; Hu, S.; Wang, Z.; Li, X.; Wang, S.; Chen, G. A Temporospatial Study of Sympathetic Skin Response and Electroencephalogram in Oral Mucosa Thermal Perception. Front. Neurosci. 2022, 16, 907658. [Google Scholar] [CrossRef]
- Wang, X.; Li, D.; Menassa, C.C.; Kamat, V.R. Investigating the Neurophysiological Effect of Thermal Environment on Individuals’ Performance Using Electroencephalogram. Computing in Civil Engineering 2019, Atlanta, GA, USA, 17–19 June 2019; pp. 598–605. [Google Scholar] [CrossRef]
- Manes, F.; Torralba, T. Funciones Ejecutivas y Trastornos Del Lóbulo Frontal; Instituto de Neurología Cognitiva (INECO): Buenos Aires, Argentina, 2005. [Google Scholar]
- Lorenz, J.; Minoshima, S.; Casey, K.L. Keeping Pain out of Mind: The Role of the Dorsolateral Prefrontal Cortex in Pain Modulation. Brain 2003, 126, 1079–1091. [Google Scholar] [CrossRef] [PubMed]
- Davidson, R.J.; Ekman, P.; Saron, C.D.; Senulis, J.A.; Friesen, W.V. Approach-Withdrawal and Cerebral Asymmetry: Emotional Expression and Brain Physiology: I. J. Personal. Soc. Psychol. 1990, 58, 330–341. [Google Scholar] [CrossRef]
- Worfolk, J.B. Heat Waves: Their Impact on the Health of Elders. Geriatr. Nurs. 2000, 21, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Yu, H.; Jiao, Y.; Chu, X.; Luo, M. Chinese Older People’s Subjective and Physiological Responses to Moderate Cold and Warm Temperature Steps. Build. Environ. 2019, 149, 526–536. [Google Scholar] [CrossRef]
- Lin, C.; Feng, Q.; Huang, J.; Zhong, R. Investigation on the Perception of Microclimatic Factors by the Elderly in Humid and Hot Areas: The Case of Guangzhou, China. Atmosphere 2023, 14, 1570. [Google Scholar] [CrossRef]
- Spitzer, S.; Weber, D. Reporting Biases in Self-Assessed Physical and Cognitive Health Status of Older Europeans. PLoS ONE 2019, 14, e0223526. [Google Scholar] [CrossRef]
- Lim, J.; Baek, G.; Jeon, E. Analysis of the Correlation between Thermal Sensations and Brain Waves via EEG Measurements. Int. J. Appl. Eng. Res. 2018, 13, 6069–6075. [Google Scholar]
- Lang, X.; Wargocki, P.; Liu, W. Investigating the Relation between Electroencephalogram, Thermal Comfort, and Cognitive Performance in Neutral to Hot Indoor Environment. Indoor Air 2022, 32, e12941. [Google Scholar] [CrossRef]

| Experimental Conditions | Radiator Power | Irradiation Area |
|---|---|---|
| S0 | 0 W | No irradiation (control group) |
| S1 | 500 W | Lower body |
| S2 | 500 W | Lower body + Upper body |
| S3 | 500 W | Lower body + Upper body + Head |
| S4 | 1000 W | Lower body |
| S5 | 1000 W | Lower body + Upper body |
| S6 | 1000 W | Lower body + Upper body + Head |
| Equipment | Specific Parameters | Equipment | Specific Parameters | ||||
|---|---|---|---|---|---|---|---|
 | Model | Xianhe CQ-51 |  | Model | AZ87785 | Temperature Accuracy | ±0.6 °C |
| Power | 500 W/ 1000 W | Diameter | 75 mm | Temperature Measurement Resolution | 0.1 °C | ||
| Spectrum | 2–25 μm | Operating Temperature | 0~50 °C | Black Globe Temperature Range | 0~80 °C | ||
| Frequency | 50 Hz | Temperature Range | 0~50 °C | Black Globe Temperature Accuracy | ±1.5 °C (at 15–40 °C) | ||
| Parameter | Unit | Range |
|---|---|---|
| Air temperature | °C | 18 ± 0.5 |
| Relative humidity | % | 55 ± 5 |
| Wind speed | m/s | <0.1 |
| Sound pressure | dB | <40 |
| Subjects | Sample Size | Age | Maximum Age | Minimum Age | Body Weight (kg) | Stature (cm) | Body Mass Index (kg/m2) |
|---|---|---|---|---|---|---|---|
| Elderly Males | 15 | 66.20 ± 2.51 | 72 | 62 | 61.00 ± 4.41 | 166.67 ± 3.66 | 21.99 ± 1.80 |
| Elderly Females | 15 | 68.73 ± 3.47 | 75 | 64 | 54.87 ± 6.52 | 159.20 ± 4.18 | 21.59 ± 1.73 |
| Young Males | 15 | 24.53 ± 0.74 | 26 | 24 | 64.53 ± 5.99 | 173.00 ± 5.58 | 21.56 ± 1.72 |
| Young Females | 15 | 25.13 ± 1.73 | 30 | 24 | 54.00 ± 4.21 | 159.00 ± 3.21 | 21.37 ± 1.66 |
| Total | 60 | 46.15 ± 21.64 | 75 | 24 | 58.60 ± 6.84 | 164.47 ± 7.18 | 21.62 ± 1.70 |
| Score (Implication) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| TSV | −3 | −2 | −1 | 0 | 1 | 2 | 3 | ||
| Cold | Cool | Mildly cool | Neutral | Mildly warm | Warm | Hot | |||
| TCV | −3 | −2 | −1 | 0 | 1 | 2 | 3 | ||
| Intensely unpleasant | Discomforting | Mildly uncomfortable | Balanced | Mildly comfortable | Cozy | Highly pleasant | |||
| RSV | −3 | −2 | −1 | 0 | 1 | 2 | 3 | ||
| Extremely unrelaxed | Unrelaxed | Slightly unrelaxed | Neutral | Slightly relaxed | Relaxed | Extremely relaxed | |||
| ALV | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
| Extremely alert | Very alert | Alert | Slightly alert | Neutral | Slightly sleepy | Sleepy | Very sleepy | Extremely sleepy | |
| Subjects | Subjective Evaluations | Sample Size | Mean | Standard Deviation | Skewness | Kurtosis | Kolmogorov–Smirnov | |
|---|---|---|---|---|---|---|---|---|
| D | p | |||||||
| The elderly | TSV | 210 | 1.371 | 1.122 | −0.075 | −1.008 | 0.184 | 0.000 ** |
| TCV | 210 | 0.69 | 0.855 | −0.609 | 0.468 | 0.317 | 0.000 ** | |
| RSV | 210 | 0.505 | 1.175 | −0.226 | −1.109 | 0.197 | 0.000 ** | |
| ALV | 210 | 4.019 | 1.359 | 0.37 | −0.446 | 0.24 | 0.000 ** | |
| Young people | TSV | 210 | 1.09 | 1.347 | −0.356 | −0.754 | 0.198 | 0.000 ** |
| TCV | 210 | 0.471 | 0.924 | −0.412 | 0.416 | 0.259 | 0.000 ** | |
| RSV | 210 | 0.224 | 1.242 | −0.101 | −1.142 | 0.201 | 0.000 ** | |
| ALV | 210 | 5.348 | 1.83 | −0.061 | −0.814 | 0.111 | 0.000 ** | |
| Subjects | Subjective Evaluations | S0 (n = 30) | S1 (n = 30) | S2 (n = 30) | S3 (n = 30) | S4 (n = 30) | S5 (n = 30) | S6 (n = 30) | F | p |
|---|---|---|---|---|---|---|---|---|---|---|
| The elderly | TSV | 0.51 | 0.73 | 0.85 | 0.77 | 0.87 | 0.78 | 0.68 | 1.867 | 0.088 |
| TCV | 0.71 | 0.64 | 0.59 | 0.92 | 0.88 | 0.77 | 0.83 | 2.223 | 0.042 * | |
| RSV | 1.08 | 1.13 | 1.07 | 0.98 | 1.01 | 0.96 | 1.16 | 0.953 | 0.458 | |
| ALV | 1.30 | 0.90 | 1.14 | 1.14 | 1.38 | 1.43 | 1.65 | 3.231 | 0.005 ** | |
| Young people | TSV | 0.83 | 0.99 | 0.92 | 1.01 | 0.93 | 0.61 | 0.61 | 4.157 | 0.001 ** |
| TCV | 0.87 | 0.53 | 0.45 | 0.87 | 1.14 | 0.87 | 1.01 | 3.691 | 0.002 ** | |
| RSV | 1.00 | 0.97 | 0.86 | 1.14 | 1.19 | 1.67 | 1.51 | 11.559 | 0.000 ** | |
| ALV | 1.37 | 1.30 | 1.46 | 1.56 | 1.48 | 1.97 | 1.87 | 0.96 | 0.454 |
| Regression Coefficient | Regression Coefficient | Standard Error | z | p | 95% CI | OR Value | OR 95% CI | |
|---|---|---|---|---|---|---|---|---|
| TSV | Intercept | −4.784 | 0.751 | −6.369 | 0.001 ** | −6.256~−3.312 | 0.008 | 0.002~0.036 |
| Age | 1.167 | 0.445 | 2.621 | 0.013 * | 0.294~2.039 | 3.211 | 1.342~7.682 | |
| Radiation intensity | 1.549 | 0.375 | 4.13 | 0.001 ** | 0.814~2.285 | 4.709 | 2.257~9.823 | |
| Radiation area | 3.168 | 0.355 | 8.922 | 0.000 ** | 2.472~3.864 | 23.77 | 11.851~47.676 | |
| Age × Radiation intensity | −0.233 | 0.227 | −1.028 | 0.304 | −0.678~0.212 | 0.792 | 0.507~1.236 | |
| Age × Radiation area | −0.533 | 0.232 | −2.295 | 0.022 * | −0.989~−0.078 | 0.587 | 0.372~0.925 | |
| Radiation intensity × Radiation area | −0.996 | 0.157 | −6.347 | 0.003 ** | −1.304~−0.689 | 0.369 | 0.271~0.502 | |
| Age × Radiation intensity × Radiation area | 0.167 | 0.1 | 1.659 | 0.097 | −0.030~0.364 | 1.181 | 0.970~1.438 | |
| TCV | Intercept | 2.321 | 0.821 | 2.828 | 0.005 ** | 0.713~3.930 | 10.186 | 2.039~50.884 |
| Age | 0.219 | 0.104 | 2.099 | 0.036 * | 0.014~0.424 | 1.245 | 1.015~1.527 | |
| Radiation intensity | −1.008 | 0.403 | −2.500 | 0.012 * | −1.798~−0.218 | 0.365 | 0.166~0.804 | |
| Radiation area | −1.36 | 0.428 | −3.18 | 0.001 ** | −2.198~−0.522 | 0.257 | 0.111~0.594 | |
| Age × Radiation intensity | 0.507 | 0.244 | 2.079 | 0.038 * | 0.029~0.986 | 1.661 | 1.029~2.679 | |
| Age × Radiation area | 0.278 | 0.265 | 1.048 | 0.295 | −0.242~0.798 | 1.321 | 0.785~2.222 | |
| Radiation intensity × Radiation area | 0.597 | 0.172 | 3.468 | 0.001 ** | 0.260~0.935 | 1.817 | 1.297~2.547 | |
| Age × Radiation intensity × Radiation area | −0.194 | 0.105 | −1.84 | 0.066 | −0.400~0.013 | 0.824 | 0.670~1.013 | |
| RSV | Intercept | −2.213 | 0.986 | −2.244 | 0.025 * | −4.146~−0.280 | 0.109 | 0.016~0.756 |
| Age | 2.415 | 0.609 | 3.967 | 0.000 ** | 1.222~3.609 | 11.195 | 3.394~36.929 | |
| Radiation intensity | 0.774 | 0.353 | 2.193 | 0.028 * | 0.082~1.466 | 2.169 | 1.086~4.332 | |
| Radiation area | 0.777 | 0.62 | 1.253 | 0.210 | −0.439~1.993 | 2.175 | 0.645~7.339 | |
| Age × Radiation intensity | −0.719 | 0.219 | −3.279 | 0.001 ** | −1.149~−0.289 | 0.487 | 0.317~0.749 | |
| Age × Radiation area | −1.143 | 0.364 | −3.136 | 0.002 ** | −1.857~−0.429 | 0.319 | 0.156~0.651 | |
| Radiation intensity × Radiation area | −0.262 | 0.207 | −1.267 | 0.205 | −0.668~0.143 | 0.769 | 0.513~1.154 | |
| Age × Radiation intensity × Radiation area | 0.397 | 0.119 | 3.335 | 0.001 ** | 0.164~0.631 | 1.488 | 1.178~1.879 | |
| ALV | Intercept | 0.685 | 1.403 | 0.489 | 0.625 | −2.064~3.434 | 1.985 | 0.127~31.012 |
| Age | −1.095 | 0.518 | −2.112 | 0.035 * | −2.111~−0.079 | 0.335 | 0.121~0.924 | |
| Radiation intensity | 1.454 | 0.538 | 2.7 | 0.007 ** | 0.399~2.510 | 4.281 | 1.490~12.299 | |
| Radiation area | 3.221 | 0.886 | 3.634 | 0.000 ** | 1.484~4.958 | 25.054 | 4.410~142.355 | |
| Age × Radiation intensity | −0.541 | 0.311 | −1.741 | 0.082 | −1.149~0.068 | 0.582 | 0.317~1.071 | |
| Age × Radiation area | −1.095 | 0.518 | −2.112 | 0.035 * | −2.111~−0.079 | 0.335 | 0.121~0.924 | |
| Radiation intensity × Radiation area | 0.838 | 0.828 | 1.011 | 0.312 | −0.786~2.462 | 2.312 | 0.456~11.726 | |
| Age × Radiation intensity × Radiation area | 0.311 | 0.181 | 1.714 | 0.087 | −0.045~0.666 | 1.364 | 0.956~1.946 |
| Prefrontal Cortex | Lateral Cortex | Upper Brain Region | Visual Cortex | |
|---|---|---|---|---|
| Age | 0.125 * | 0.164 ** | 0.206 ** | 0.218 ** |
| S0 (n = 30) | S1 (n = 30) | S2 (n = 30) | S3 (n = 30) | S4 (n = 30) | S5 (n = 30) | S6 (n = 30) | p | |
|---|---|---|---|---|---|---|---|---|
| Frontal lobe-δ | ||||||||
| The elderly | 9.93 ± 0.38 | 9.91 ± 0.30 | 9.84 ± 0.28 | 9.88 ± 0.39 | 9.93 ± 0.44 | 10.04 ± 0.42 | 10.10 ± 0.42 | 0.030 * |
| Young people | 10.07 ± 0.43 | 10.07 ± 0.45 | 9.91 ± 0.34 | 10.05 ± 0.32 | 10.00 ± 0.35 | 10.01 ± 0.31 | 9.95 ± 0.39 | 0. 533 |
| Temporal lobe-δ | ||||||||
| The elderly | 9.26 ± 0.45 | 9.26 ± 0.33 | 9.19 ± 0.29 | 9.22 ± 0.40 | 9.28 ± 0.44 | 9.43 ± 0.45 | 9.53 ± 0.41 | 0.008 ** |
| Young people | 9.39 ± 0.45 | 9.39 ± 0.50 | 9.18 ± 0.42 | 9.39 ± 0.38 | 9.31 ± 0.40 | 9.33 ± 0.33 | 9.39 ± 0.45 | 0.362 |
| Parietal lobe-δ | ||||||||
| The elderly | 9.19 ± 0.45 | 9.19 ± 0.35 | 9.12 ± 0.27 | 9.17 ± 0.38 | 9.22 ± 0.47 | 9.39 ± 0.47 | 9.50 ± 0.43 | 0.002 ** |
| Young people | 9.35 ± 0.46 | 9.31 ± 0.51 | 9.11 ± 0.46 | 9.32 ± 0.41 | 9.26 ± 0.42 | 9.29 ± 0.34 | 9.19 ± 0.52 | 0.403 |
| Occipital lobe-δ | ||||||||
| The elderly | 9.17 ± 0.46 | 9.16 ± 0.36 | 9.08 ± 0.29 | 9.12 ± 0.42 | 9.15 ± 0.51 | 9.35 ± 0.50 | 9.50 ± 0.46 | 0.001 ** |
| Young people | 9.30 ± 0.46 | 9.27 ± 0.51 | 9.06 ± 0.46 | 9.27 ± 0.41 | 9.21 ± 0.44 | 9.23 ± 0.33 | 9.15 ± 0.51 | 0.432 |
| S0 (n = 30) | S1 (n = 30) | S2 (n = 30) | S3 (n = 30) | S4 (n = 30) | S5 (n = 30) | S6 (n = 30) | p | |
|---|---|---|---|---|---|---|---|---|
| AF4-θ | 9.19 ± 0.44 | 9.20 ± 0.33 | 9.12 ± 0.31 | 9.21 ± 0.34 | 9.23 ± 0.45 | 9.40 ± 0.48 | 9.44 ± 0.44 | 0.016 * |
| F4-δ | 8.76 ± 0.50 | 8.67 ± 0.36 | 8.60 ± 0.43 | 8.63 ± 0.49 | 8.58 ± 0.64 | 8.82 ± 0.55 | 8.98 ± 0.44 | 0.025 * |
| F4-θ | 9.23 ± 0.38 | 9.22 ± 0.28 | 9.17 ± 0.28 | 9.24 ± 0.33 | 9.28 ± 0.41 | 9.40 ± 0.46 | 9.45 ± 0.40 | 0.037 * |
| F8-θ | 9.21 ± 0.39 | 9.21 ± 0.30 | 9.17 ± 0.30 | 9.24 ± 0.34 | 9.28 ± 0.42 | 9.40 ± 0.47 | 9.44 ± 0.43 | 0.049 * |
| FC6-δ | 8.78 ± 0.53 | 8.72 ± 0.37 | 8.66 ± 0.39 | 8.69 ± 0.47 | 8.65 ± 0.63 | 8.88 ± 0.53 | 9.04 ± 0.43 | 0.021 * |
| Frontal Lobe-α | Frontal Lobe-β | Frontal Lobe-δ | Frontal Lobe-θ | Parietal Lobe-α | Parietal Lobe-β | Parietal Lobe-δ | Parietal Lobe-θ | |
|---|---|---|---|---|---|---|---|---|
| TCV | −0.126 ** | −0.085 | −0.195 ** | −0.182 ** | −0.085 | −0.07 | −0.186 ** | −0.157 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gao, P.; Li, Y.; Hou, K.; Lu, M.; Liu, C.; Guan, H.; Yan, W.; Li, J. Thermal Comfort Differences Between the Elderly and Young People Under Different Infrared Radiation Conditions: A Quantitative Study Based on Subjective Evaluation and EEG Characteristics. Buildings 2025, 15, 3798. https://doi.org/10.3390/buildings15203798
Gao P, Li Y, Hou K, Lu M, Liu C, Guan H, Yan W, Li J. Thermal Comfort Differences Between the Elderly and Young People Under Different Infrared Radiation Conditions: A Quantitative Study Based on Subjective Evaluation and EEG Characteristics. Buildings. 2025; 15(20):3798. https://doi.org/10.3390/buildings15203798
Chicago/Turabian StyleGao, Peiping, Yunhao Li, Keming Hou, Mingli Lu, Chao Liu, Hongyu Guan, Wenjing Yan, and Juanmei Li. 2025. "Thermal Comfort Differences Between the Elderly and Young People Under Different Infrared Radiation Conditions: A Quantitative Study Based on Subjective Evaluation and EEG Characteristics" Buildings 15, no. 20: 3798. https://doi.org/10.3390/buildings15203798
APA StyleGao, P., Li, Y., Hou, K., Lu, M., Liu, C., Guan, H., Yan, W., & Li, J. (2025). Thermal Comfort Differences Between the Elderly and Young People Under Different Infrared Radiation Conditions: A Quantitative Study Based on Subjective Evaluation and EEG Characteristics. Buildings, 15(20), 3798. https://doi.org/10.3390/buildings15203798





