Assessing Indoor Air Quality and Ventilation to Limit Aerosol Dispersion—Literature Review
Abstract
1. Introduction
- How has IAQ been assessed so far to reduce the dispersion of aerosols?
- Which indicators and approaches have been used and for what purpose?
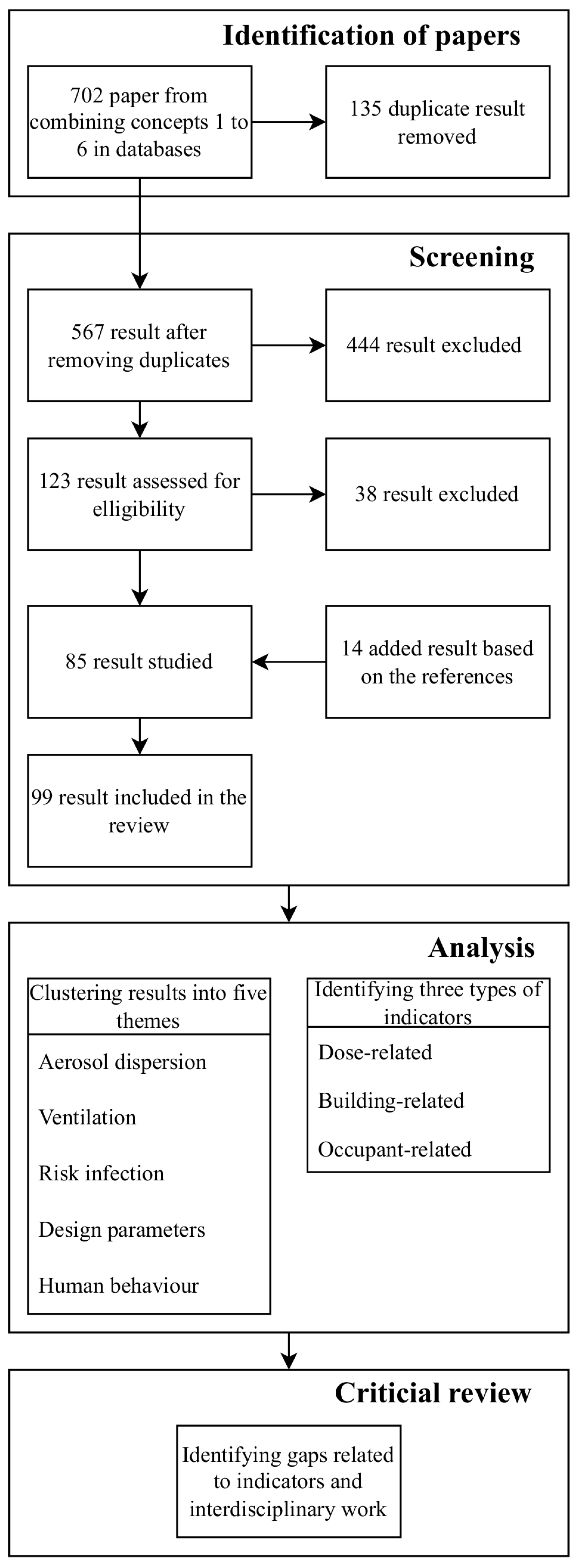
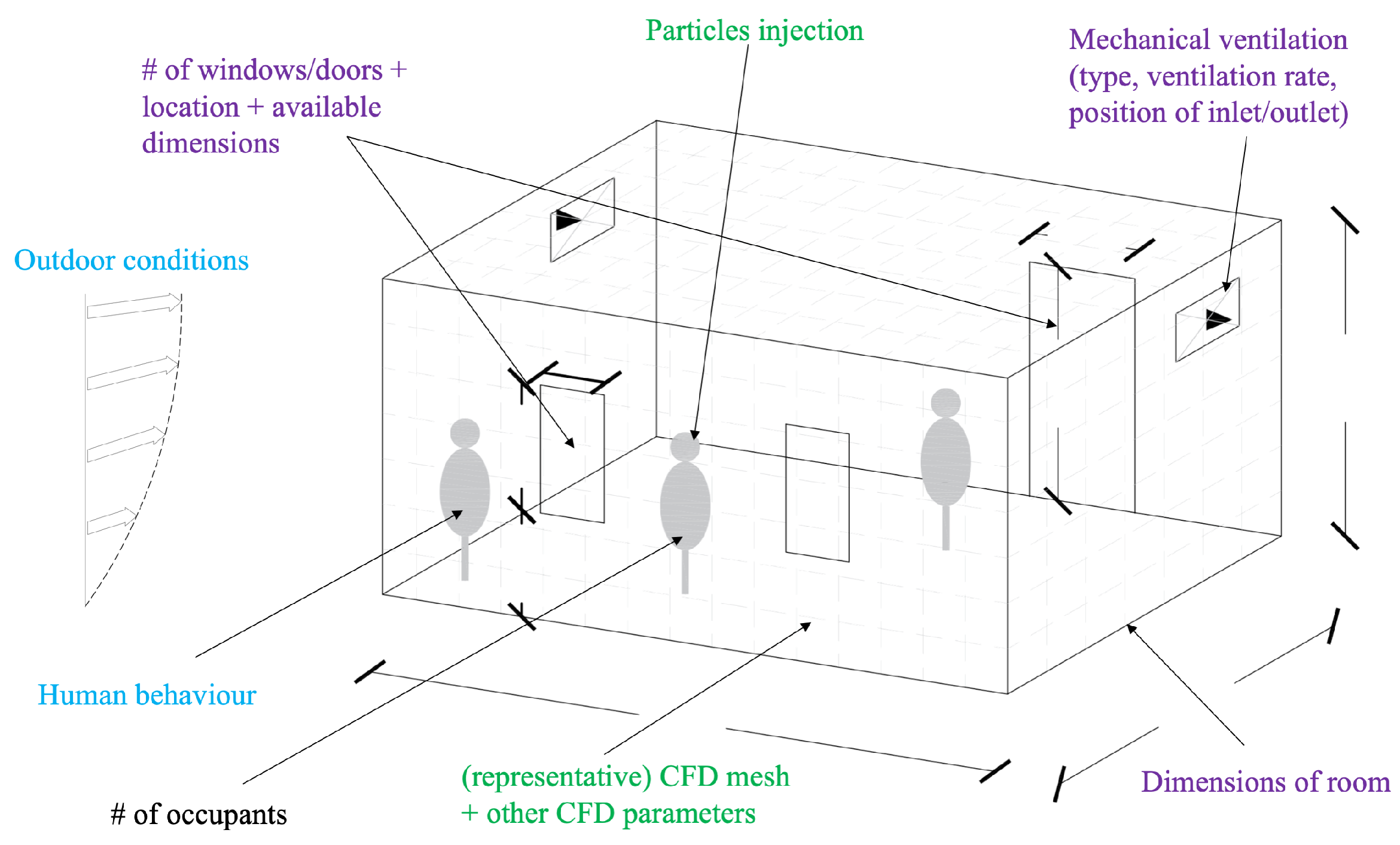
2. Materials and Methods
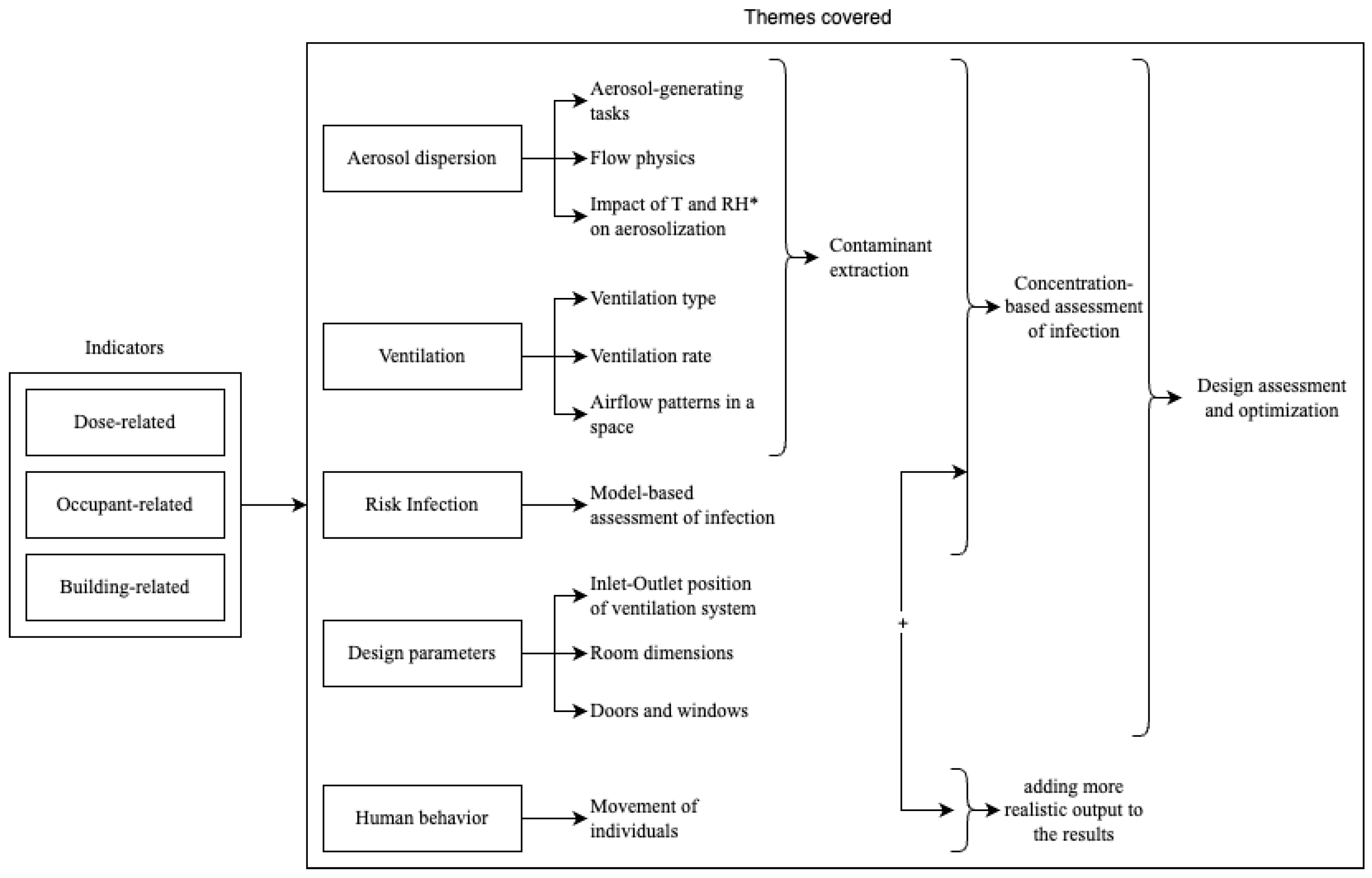
3. Results—Assessment of IAQ
3.1. General Overview of IAQ Assessment Methods
- Aerosol dispersion;
- Ventilation;
- Infection risk;
- Design parameters;
- Human behavior.
3.2. Aerosol Dispersion
- near-field dispersions, which impact a few meters from the source of the aerosol.
- far-field dispersions, which impact the entire ventilated space of a room.
3.3. Ventilation
Aerosol Dispersion and Ventilation
3.4. Infection Risk
3.4.1. Infection Risk and Ventilation
3.4.2. Aerosol Dispersion, Ventilation, and Infection Risk
3.5. Design Parameters of a Room
3.5.1. Ventilation and Design Parameters
3.5.2. Infection Risk and Design Parameters
3.5.3. Aerosol Dispersion, Infection Risk, and Design Parameters
- The geometry of the space: the room dimensions, size, and position of the doors and windows;
- The room conditions: the temperature and relative humidity;
- Occupant-related parameters: the number and location of the people and their orientation, gender, height, weight, and clothing type;
- The types of aerosol-generating tasks: breathing, speaking, coughing, sneezing;
- Particle size;
- Type of mask.
3.5.4. Aerosol Dispersion, Ventilation, and Design Parameters
3.6. Human Behavior
3.6.1. Aerosol Dispersion and Human Behavior
3.6.2. Aerosol Dispersion, Ventilation, and Human Behavior
3.6.3. Infection Risk and Human Behavior
4. Discussion
4.1. Indicators
4.2. Numerical Simulations and Tools
4.3. Need for a Holistic Approach
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| BPNN | Back-Propagation Neural Network |
| CFD | Computational Fluid Dynamics |
| CO2 | Carbon dioxide |
| CRW | Continuous Random Walk |
| DRW | Discontinuous Random Walk |
| HEPA | High-Efficiency Particulate Air |
| IAQ | Indoor Air Quality |
| MERS | Middle East Respiratory Syndrome |
| PIV | Particle Image Velocimetry |
| PSO | Particle Swarm Optimiser |
| PTV | Particle-Tracking Velocimetry |
| REHVA | Federation of European Heating, Ventilation, and Air-Conditioning Associations |
| RH | Relative Humidity |
| RNG | Re-Normalization Group |
| SARS-CoV-1 | Severe Acute Respiratory Syndrome Coronavirus 1 |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Coronavirus 2 |
| SDE | Stochastic Differential Equation |
References
- Worldometer. Coronavirus Cases. 2022. Available online: https://www.worldometers.info/coronavirus/ (accessed on 21 February 2022).
- Gameiro da Silva, M. How to Operate and Use Building Services during the COVID-19 Crisis [Build Up Webinar]. 2020. Available online: https://www.rehva.eu/fileadmin/user_upload/2020.04.28_COVID-19_BuildUp_webinar_by_REHVA.pdf (accessed on 21 February 2022).
- Morawska, L.; Milton, D.K. It is time to address airborne transmission of coronavirus disease 2019 (COVID-19). Clin. Infect. Dis. 2020, 71, 2311–2313. [Google Scholar] [CrossRef] [PubMed]
- Morawska, L.; Tang, J.W.; Bahnfleth, W.; Bluyssen, P.M.; Boerstra, A.; Buonanno, G.; Cao, J.; Dancer, S.; Floto, A.; Franchimon, F.; et al. How can airborne transmission of COVID-19 indoors be minimised? Environ. Int. 2020, 142, 105832. [Google Scholar] [CrossRef]
- Qian, H.; Zheng, X. Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. J. Thorac. Dis. 2018, 10, S2295. [Google Scholar] [CrossRef] [PubMed]
- Fu, S.; Biwole, P.H.; Mathis, C. Particle tracking velocimetry for indoor airflow field: A review. Build. Environ. 2015, 87, 34–44. [Google Scholar] [CrossRef]
- Cao, X.; Liu, J.; Jiang, N.; Chen, Q. Particle image velocimetry measurement of indoor airflow field: A review of the technologies and applications. Energy Build. 2014, 69, 367–380. [Google Scholar] [CrossRef]
- Sun, Y.; Zhang, Y. An overview of room air motion measurement: Technology and application. HVAC&R Res. 2007, 13, 929–950. [Google Scholar] [CrossRef]
- Ai, Z.T.; Melikov, A.K. Airborne spread of expiratory droplet nuclei between the occupants of indoor environments: A review. Indoor Air 2018, 28, 500–524. [Google Scholar] [CrossRef]
- Vuorinen, V.; Aarnio, M.; Alava, M.; Alopaeus, V.; Atanasova, N.; Auvinen, M.; Balasubramanian, N.; Bordbar, H.; Erästö, P.; Grande, R.; et al. Modelling aerosol transport and virus exposure with numerical simulations in relation to SARS-CoV-2 transmission by inhalation indoors. Saf. Sci. 2020, 130, 104866. [Google Scholar] [CrossRef]
- Lipinski, T.; Ahmad, D.; Serey, N.; Jouhara, H. Review of ventilation strategies to reduce the risk of disease transmission in high occupancy buildings. Int. J. Thermofluids 2020, 7, 100045. [Google Scholar] [CrossRef]
- Sheikhnejad, Y.; Aghamolaei, R.; Fallahpour, M.; Motamedi, H.; Moshfeghi, M.; Mirzaei, P.A.; Bordbar, H. Airborne and aerosol pathogen transmission modeling of respiratory events in buildings: An overview of computational fluid dynamics. Sustain. Cities Soc. 2022, 79, 103704. [Google Scholar] [CrossRef]
- de Crane D’Heysselaer, S.; Parisi, G.; Lisson, M.; Bruyère, O.; Donneau, A.F.; Fontaine, S.; Gillet, L.; Bureau, F.; Darcis, G.; Thiry, E.; et al. Systematic Review of the Key Factors Influencing the Indoor Airborne Spread of SARS-CoV-2. Pathogens 2023, 12, 382. [Google Scholar] [CrossRef]
- Morawska, L.; Allen, J.; Bahnfleth, W.; Bluyssen, P.M.; Boerstra, A.; Buonanno, G.; Cao, J.; Dancer, S.J.; Floto, A.; Franchimon, F.; et al. A paradigm shift to combat indoor respiratory infection. Science 2021, 372, 689–691. [Google Scholar] [CrossRef]
- Bluyssen, P.M. What do we need to be able to (re) design healthy and comfortable indoor environments? Intell. Build. Int. 2014, 6, 69–92. [Google Scholar] [CrossRef]
- Bluyssen, P.M. Towards new methods and ways to create healthy and comfortable buildings. Build. Environ. 2010, 45, 808–818. [Google Scholar] [CrossRef]
- Xu, C.; Liu, W.; Luo, X.; Huang, X.; Nielsen, P. Prediction and control of aerosol transmission of SARS-CoV-2 in ventilated context: From source to receptor. Sustain. Cities Soc. 2022, 76, 103416. [Google Scholar] [CrossRef] [PubMed]
- Bluyssen, P.M. Towards an integrated analysis of the indoor environmental factors and its effects on occupants. Intell. Build. Int. 2020, 12, 199–207. [Google Scholar] [CrossRef]
- Eijkelenboom, A.; Bluyssen, P.M. Comfort and health of patients and staff, related to the physical environment of different departments in hospitals: A literature review. Intell. Build. Int. 2022, 14, 95–113. [Google Scholar] [CrossRef]
- Bluyssen, P.M. The Healthy Indoor Environment: How to Assess Occupants’ Wellbeing in Buildings; Taylor & Francis: London, UK, 2014. [Google Scholar] [CrossRef]
- Ascione, F.; De Masi, R.F.; Mastellone, M.; Vanoli, G.P. The design of safe classrooms of educational buildings for facing contagions and transmission of diseases: A novel approach combining audits, calibrated energy models, building performance (BPS) and computational fluid dynamic (CFD) simulations. Energy Build. 2021, 230, 110533. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Weng, W. COVID-19 virus released from larynx might cause a higher exposure dose in indoor environment. Environ. Res. 2021, 199, 111361. [Google Scholar] [CrossRef]
- Villafruela, J.; Olmedo, I.; San José, J. Influence of human breathing modes on airborne cross infection risk. Build. Environ. 2016, 106, 340–351. [Google Scholar] [CrossRef]
- Spalart, P.; Allmaras, S. A one-equation turbulence model for aerodynamic flows. In Proceedings of the 30th Aerospace Sciences Meeting and Exhibit, Reno, NV, USA, 6–9 January 1992; p. 439. [Google Scholar] [CrossRef]
- Launder, B.E.; Spalding, D.B. The numerical computation of turbulent flows. In Numerical Prediction of Flow, Heat Transfer, Turbulence and Combustion; Elsevier: Amsterdam, The Netherlands, 1983; pp. 96–116. [Google Scholar] [CrossRef]
- Wilcox, D.C. Reassessment of the scale-determining equation for advanced turbulence models. AIAA J. 1988, 26, 1299–1310. [Google Scholar] [CrossRef]
- Valen-Sendstad, K.; Mortensen, M.; Langtangen, H.P.; Reif, B.A.P.; Mardal, K.A. Implementing a k-ϵ Turbulence Model in the FEniCS Finite Element Programming Environment. In Proceedings of the Fifth National Conference on Computational Mechanics (MekIT’09), Trondheim, Norway, 26–27 May 2013; p. 13. [Google Scholar]
- Weaver, D.S.; Mišković, S. A Study of RANS Turbulence Models in Fully Turbulent Jets: A Perspective for CFD-DEM Simulations. Fluids 2021, 6, 271. [Google Scholar] [CrossRef]
- Dai, Y.; Xu, D.; Wang, H.; Zhang, F. CFD Simulations of Ventilation and Interunit Dispersion in Dormitory Complex: A Case Study of Epidemic Outbreak in Shanghai. Int. J. Environ. Res. Public Health 2023, 20, 4603. [Google Scholar] [CrossRef] [PubMed]
- Ovando-Chacon, G.E.; Ovando-Chacon, S.L.; Rodríguez-León, A.; Díaz-González, M. Numerical Study of Indoor Air Quality in a University Professor’s Office. Sustainability 2023, 15, 4221. [Google Scholar] [CrossRef]
- Faleiros, D.E.; van den Bos, W.; Botto, L.; Scarano, F. TU Delft COVID-app: A tool to democratize CFD simulations for SARS-CoV-2 infection risk analysis. Sci. Total Environ. 2022, 826, 154143. [Google Scholar] [CrossRef]
- Li, L.; Zhang, Y.; Fung, J.C.; Qu, H.; Lau, A.K. A coupled computational fluid dynamics and back-propagation neural network-based particle swarm optimizer algorithm for predicting and optimizing indoor air quality. Build. Environ. 2022, 207, 108533. [Google Scholar] [CrossRef]
- De Simone, Z.; Kastner, P.; Dogan, T. Towards Safer Work Environments During the COVID-19 Crisis: A Study Of Different Floor Plan Layouts and Ventilation Strategies Coupling Open FOAM and Airborne Pathogen Data for Actionable, Simulation-based Feedback in Design. In Proceedings of the Building Simulation 2021: 17th Conference of IBPSA, Bruges, Belgium, 1–3 September 2021. [Google Scholar]
- Foster, A.; Kinzel, M. Estimating COVID-19 exposure in a classroom setting: A comparison between mathematical and numerical models. Phys. Fluids 2021, 33, 021904. [Google Scholar] [CrossRef] [PubMed]
- Muthusamy, J.; Haq, S.; Akhtar, S.; Alzoubi, M.A.; Shamim, T.; Alvarado, J. Implication of coughing dynamics on safe social distancing in an indoor environment—A numerical perspective. Build. Environ. 2021, 206, 108280. [Google Scholar] [CrossRef]
- Blocken, B.; Malizia, F.; Van Druenen, T.; Marchal, T. Towards Aerodynamically Equivalent COVID-19 1.5 m Social Distancing for Walking and Running. 2020. preprint. Available online: https://www.euroga.org/system/1/user_files/files/000/045/111/45111/150d3060c/original/Social_Distancing_v20_White_Paper.pdf (accessed on 20 June 2022).
- Dbouk, T.; Drikakis, D. On coughing and airborne droplet transmission to humans. Phys. Fluids 2020, 32, 053310. [Google Scholar] [CrossRef]
- Dbouk, T.; Drikakis, D. Weather impact on airborne coronavirus survival. Phys. Fluids 2020, 32, 093312. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Zheng, X.; Shen, S. A numerical study of the effect of breathing mode and exposure conditions on the particle inhalation and deposition. Inhal. Toxicol. 2020, 32, 456–467. [Google Scholar] [CrossRef]
- Jiao, Z.; Yuan, S.; Ji, C.; Mannan, M.S.; Wang, Q. Optimization of dilution ventilation layout design in confined environments using Computational Fluid Dynamics (CFD). J. Loss Prev. Process Ind. 2019, 60, 195–202. [Google Scholar] [CrossRef]
- Murakami, Y.; Ikegaya, N.; Hagishima, A.; Tanimoto, J. Coupled simulations of indoor-outdoor flow fields for cross-ventilation of a building in a simplified urban array. Atmosphere 2018, 9, 217. [Google Scholar] [CrossRef]
- Keshavarz, S.; Salmanzadeh, M.; Ahmadi, G. Computational modeling of time resolved exposure level analysis of a heated breathing manikin with rotation in a room. J. Aerosol Sci. 2017, 103, 117–131. [Google Scholar] [CrossRef]
- Gilani, S.; Montazeri, H.; Blocken, B. CFD simulation of stratified indoor environment in displacement ventilation: Validation and sensitivity analysis. Build. Environ. 2016, 95, 299–313. [Google Scholar] [CrossRef]
- Romano, F.; Marocco, L.; Gustén, J.; Joppolo, C.M. Numerical and experimental analysis of airborne particles control in an operating theater. Build. Environ. 2015, 89, 369–379. [Google Scholar] [CrossRef]
- van Hooff, T.; Blocken, B. CFD evaluation of natural ventilation of indoor environments by the concentration decay method: CO2 gas dispersion from a semi-enclosed stadium. Build. Environ. 2013, 61, 1–17. [Google Scholar] [CrossRef]
- Aliabadi, A.A.; Rogak, S.N.; Green, S.I.; Bartlett, K.H. CFD simulation of human coughs and sneezes: A study in droplet dispersion, heat, and mass transfer. In Proceedings of the ASME International Mechanical Engineering Congress and Exposition, Vancouver, BC, Canada, 12–18 November 2010; Volume 44441, pp. 1051–1060. [Google Scholar] [CrossRef]
- Mao, S.; Celik, I.B. Modeling of indoor airflow and dispersion of aerosols using immersed boundary and random flow generation methods. Comput. Fluids 2010, 39, 1275–1283. [Google Scholar] [CrossRef]
- Lai, A.C.; Chen, F. Comparison of a new Eulerian model with a modified Lagrangian approach for particle distribution and deposition indoors. Atmos. Environ. 2007, 41, 5249–5256. [Google Scholar] [CrossRef]
- Rohdin, P.; Moshfegh, B. Numerical predictions of indoor climate in large industrial premises. A comparison between different k–ε models supported by field measurements. Build. Environ. 2007, 42, 3872–3882. [Google Scholar] [CrossRef]
- Zhang, T.; Chen, Q.Y.; Lin, C.H. Optimal sensor placement for airborne contaminant detection in an aircraft cabin. HVAC&R Res. 2007, 13, 683–696. [Google Scholar] [CrossRef]
- Brohus, H.; Balling, K.; Jeppesen, D. Influence of movements on contaminant transport in an operating room. Indoor Air 2006, 16, 356–372. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.W.; Chen, G.Q. A numerical study of turbulent line puffs via the renormalization group (RNG) k–ϵ model. Int. J. Numer. Methods Fluids 1998, 26, 217–247. [Google Scholar] [CrossRef]
- de Man, P.; Ortiz, M.A.; Bluyssen, P.M.; de Man, S.J.; Rentmeester, M.J.; van der Vliet, M.; Wils, E.J.; Ong, D.S. Airborne SARS-CoV-2 in home and hospital environments investigated with a high-powered air sampler. J. Hosp. Infect. 2022, 119, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Han, M.; Ooka, R.; Kikumoto, H.; Oh, W.; Bu, Y.; Hu, S. Experimental measurements of airflow features and velocity distribution exhaled from sneeze and speech using particle image velocimetry. Build. Environ. 2021, 205, 108293. [Google Scholar] [CrossRef]
- Hebbink, R.H.J.; Elshof, J.; Wanrooij, S.; Lette, W.; Lokate, M.; Venner, C.H.; Duiverman, M.; Hagmeijer, R. Passive Tracer Visualization to Simulate Aerodynamic Virus Transport in Noninvasive Respiratory Support Methods. Respiration 2021, 100, 1196–1207. [Google Scholar] [CrossRef]
- Ho, K.M.A.; Davies, H.; Epstein, R.; Bassett, P.; Hogan, Á.; Kabir, Y.; Rubin, J.; Shin, G.Y.; Reid, J.P.; Torii, R.; et al. Spatiotemporal droplet dispersion measurements demonstrate face masks reduce risks from singing. Sci. Rep. 2021, 11, 24183. [Google Scholar] [CrossRef]
- Li, X.; Mak, C.M.; Ma, K.W.; Wong, H.M. Evaluating flow-field and expelled droplets in the mockup dental clinic during the COVID-19 pandemic. Phys. Fluids 2021, 33, 047111. [Google Scholar] [CrossRef]
- Ortiz, M.A.; Ghasemieshkaftaki, M.; Bluyssen, P.M. Testing of outward leakage of different types of masks with a breathing manikin head, ultraviolet light and coloured water mist. Intell. Build. Int. 2022, 14, 623–641. [Google Scholar] [CrossRef]
- Tan, Z.P.; Silwal, L.; Bhatt, S.P.; Raghav, V. Experimental characterization of speech aerosol dispersion dynamics. Sci. Rep. 2021, 11, 3953. [Google Scholar] [CrossRef]
- Akhtar, J.; Luna Garcia, A.; Saenz, L.; Kuravi, S.; Shu, F.; Kota, K. Can face masks offer protection from airborne sneeze and cough droplets in close-up, face-to-face human interactions?—A quantitative study. Phys. Fluids 2020, 32, 127112. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.T.; Jeong, H.; Kang, Y.J.; Chamorro, L.P.; Rogers, J.A. Dynamics of droplets on COVID-19 transmission via a soft wireless device and Particle Tracking Velocimetry. In Proceedings of the APS Division of Fluid Dynamics Meeting Abstracts, Virtual Event, 20–24 November 2020; pp. Y01–002. [Google Scholar]
- Bourouiba, L.; Dehandschoewercker, E.; Bush, J.W. Violent expiratory events: On coughing and sneezing. J. Fluid Mech. 2014, 745, 537–563. [Google Scholar] [CrossRef]
- Hui, D.S.; Chow, B.K.; Chu, L.; Ng, S.S.; Lee, N.; Gin, T.; Chan, M.T. Exhaled air dispersion during coughing with and without wearing a surgical or N95 mask. PLoS ONE 2012, 7, e50845. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.W.; Liebner, T.J.; Craven, B.A.; Settles, G.S. A schlieren optical study of the human cough with and without wearing masks for aerosol infection control. J. R. Soc. Interface 2009, 6, S727–S736. [Google Scholar] [CrossRef]
- Chen, W.; Zhang, N.; Wei, J.; Yen, H.L.; Li, Y. Short-range airborne route dominates exposure of respiratory infection during close contact. Build. Environ. 2020, 176, 106859. [Google Scholar] [CrossRef]
- Wei, J.; Li, Y. Enhanced spread of expiratory droplets by turbulence in a cough jet. Build. Environ. 2015, 93, 86–96. [Google Scholar] [CrossRef]
- Xie, X.; Li, Y.; Chwang, A.; Ho, P.; Seto, W. How far droplets can move in indoor environments–revisiting the Wells evaporation-falling curve. Indoor Air 2007, 17, 211–225. [Google Scholar] [CrossRef]
- Mumtaz, R.; Zaidi, S.M.H.; Shakir, M.Z.; Shafi, U.; Malik, M.M.; Haque, A.; Mumtaz, S.; Zaidi, S.A.R. Internet of Things (IoT) based indoor air quality sensing and predictive analytic—A COVID-19 perspective. Electronics 2021, 10, 184. [Google Scholar] [CrossRef]
- Chen, Q. Ventilation performance prediction for buildings: A method overview and recent applications. Build. Environ. 2009, 44, 848–858. [Google Scholar] [CrossRef]
- Zhou, L.; Haghighat, F. Optimization of ventilation system design and operation in office environment, Part I: Methodology. Build. Environ. 2009, 44, 651–656. [Google Scholar] [CrossRef]
- Miller, S.L.; Nazaroff, W.W.; Jimenez, J.L.; Boerstra, A.; Buonanno, G.; Dancer, S.J.; Kurnitski, J.; Marr, L.C.; Morawska, L.; Noakes, C. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. Indoor Air 2021, 31, 314–323. [Google Scholar] [CrossRef]
- Dai, H.; Zhao, B. Association of the infection probability of COVID-19 with ventilation rates in confined spaces. In Proceedings of the Building Simulation; Springer: Berlin/Heidelberg, Germany, 2020; Volume 13, pp. 1321–1327. [Google Scholar] [CrossRef]
- Sun, C.; Zhai, Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain. Cities Soc. 2020, 62, 102390. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Jimenez, J. Exhaled CO2 as COVID-19 infection risk proxy for different indoor environments and activities. Environ. Sci. Technol. Lett. 2020. [Google Scholar] [CrossRef]
- Sze To, G.N.; Chao, C.Y.H. Review and comparison between the Wells–Riley and dose-response approaches to risk assessment of infectious respiratory diseases. Indoor Air 2010, 20, 2–16. [Google Scholar] [CrossRef] [PubMed]
- Rudnick, S.; Milton, D. Risk of indoor airborne infection transmission estimated from carbon dioxide concentration. Indoor Air 2003, 13, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Riley, E.; Murphy, G.; Riley, R. Airborne spread of measles in a suburban elementary school. Am. J. Epidemiol. 1978, 107, 421–432. [Google Scholar] [CrossRef]
- Zhang, D.; Bluyssen, P.M. Exploring the possibility of using CO2 as a proxy for exhaled particles to predict the risk of indoor exposure to pathogens. Indoor Built Environ. 2022. accepted. [Google Scholar] [CrossRef]
- Zhang, D.; Ding, E.; Bluyssen, P.M. Guidance to assess ventilation performance of a classroom based on CO2 monitoring. Indoor Built Environ. 2022, 1420326X211058743. [Google Scholar] [CrossRef]
- Bluyssen, P.M.; Ortiz, M.; Zhang, D. The effect of a mobile HEPA filter system on ‘infectious’ aerosols, sound and air velocity in the SenseLab. Build. Environ. 2021, 188, 107475. [Google Scholar] [CrossRef]
- Bolashikov, Z.D.; Barova, M.; Melikov, A.K. Wearable personal exhaust ventilation: Improved indoor air quality and reduced exposure to air exhaled from a sick doctor. Sci. Technol. Built Environ. 2015, 21, 1117–1125. [Google Scholar] [CrossRef]
- Nielsen, P.V.; Olmedo, I.; de Adana, M.R.; Grzelecki, P.; Jensen, R.L. Airborne cross-infection risk between two people standing in surroundings with a vertical temperature gradient. HVAC&R Res. 2012, 18, 552–561. [Google Scholar] [CrossRef]
- Nielsen, P.V. Control of airborne infectious diseases in ventilated spaces. J. R. Soc. Interface 2009, 6, S747–S755. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, P.; Buus, M.; Winther, F.; Thilageswaran, M. Contaminant flow in the microenvironment between people under different ventilation conditions. Ashrae Trans. 2008, 114, 632. [Google Scholar]
- Melikov, A.K.; Cermak, R.; Majer, M. Personalized ventilation: Evaluation of different air terminal devices. Energy Build. 2002, 34, 829–836. [Google Scholar] [CrossRef]
- Cao, G.; Nielsen, P.; Jensen, R.; Heiselberg, P.; Liu, L.; Heikkinen, J. Protected zone ventilation and reduced personal exposure to airborne cross-infection. Indoor Air 2015, 25, 307–319. [Google Scholar] [CrossRef]
- Hou, D.; Katal, A.; Wang, L.L. Bayesian calibration of using CO2 sensors to assess ventilation conditions and associated COVID-19 airborne aerosol transmission risk in schools. medRxiv 2021. [Google Scholar] [CrossRef]
- Liu, W.; Liu, L.; Xu, C.; Fu, L.; Wang, Y.; Nielsen, P.V.; Zhang, C. Exploring the potentials of personalized ventilation in mitigating airborne infection risk for two closely ranged occupants with different risk assessment models. Energy Build. 2021, 253, 111531. [Google Scholar] [CrossRef]
- Wu, Y.; Tung, T.C.; Niu, J.l. On-site measurement of tracer gas transmission between horizontal adjacent flats in residential building and cross-infection risk assessment. Build. Environ. 2016, 99, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Shao, S.; Zhou, D.; He, R.; Li, J.; Zou, S.; Mallery, K.; Kumar, S.; Yang, S.; Hong, J. Risk assessment of airborne transmission of COVID-19 by asymptomatic individuals under different practical settings. J. Aerosol Sci. 2021, 151, 105661. [Google Scholar] [CrossRef]
- Guo, Y.; Qian, H.; Sun, Z.; Cao, J.; Liu, F.; Luo, X.; Ling, R.; Weschler, L.B.; Mo, J.; Zhang, Y. Assessing and controlling infection risk with Wells-Riley model and spatial flow impact factor (SFIF). Sustain. Cities Soc. 2021, 67, 102719. [Google Scholar] [CrossRef]
- Zivelonghi, A.; Lai, M. Mitigating aerosol infection risk in school buildings: The role of natural ventilation, volume, occupancy and CO2 monitoring. Build. Environ. 2021, 204, 108139. [Google Scholar] [CrossRef]
- Park, S.; Choi, Y.; Song, D.; Kim, E.K. Natural ventilation strategy and related issues to prevent coronavirus disease 2019 (COVID-19) airborne transmission in a school building. Sci. Total Environ. 2021, 789, 147764. [Google Scholar] [CrossRef] [PubMed]
- Kembel, S.W.; Meadow, J.F.; O’Connor, T.K.; Mhuireach, G.; Northcutt, D.; Kline, J.; Moriyama, M.; Brown, G.; Bohannan, B.J.; Green, J.L. Architectural design drives the biogeography of indoor bacterial communities. PLoS ONE 2014, 9, e87093. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.F.; King, S.; Behnia, M.; Prasad, D. Coupled outdoor and indoor airflow prediction for buildings using Computational Fluid Dynamics (CFD). Buildings 2013, 3, 399–421. [Google Scholar] [CrossRef]
- Kapoor, N.R.; Kumar, A.; Kumar, A.; Kumar, A.; Kumar, K. Transmission Probability of SARS-CoV-2 in Office Environment Using Artificial Neural Network. IEEE Access 2022, 10, 121204–121229. [Google Scholar] [CrossRef]
- Peng, Z.; Rojas, A.P.; Kropff, E.; Bahnfleth, W.; Buonanno, G.; Dancer, S.; Kurnitski, J.; Li, Y.; Loomans, M.G.; Marr, L.C.; et al. Practical indicators for risk of airborne transmission in shared indoor environments and their application to COVID-19 outbreaks. Environ. Sci. Technol. 2022. [Google Scholar] [CrossRef]
- Afshari, A.; Hultmark, G.; Nielsen, P.V.; Maccarini, A. Ventilation system design and the coronavirus (COVID-19). Front. Built Environ. Front. Built Environ. 2021, 7, 662489. [Google Scholar] [CrossRef]
- Wang, H.; Li, Z.; Liu, Y.; Zhu, L.; Zhou, Z. Experimental study of the dispersion of cough-generated droplets from a person going up or down stairs. AIP Adv. 2022, 12, 015002. [Google Scholar] [CrossRef]
- Blocken, B.; van Druenen, T.; Ricci, A.; Kang, L.; van Hooff, T.; Qin, P.; Xia, L.; Ruiz, C.A.; Arts, J.; Diepens, J.; et al. Ventilation and air cleaning to limit aerosol particle concentrations in a gym during the COVID-19 pandemic. Build. Environ. 2021, 193, 107659. [Google Scholar] [CrossRef]
- Halvoňová, B.; Melikov, A.K. Performance of “ductless” personalized ventilation in conjunction with displacement ventilation: Impact of disturbances due to walking person(s). Build. Environ. 2010, 45, 427–436. [Google Scholar] [CrossRef]
- Duives, D.; Chang, Y.; Sparnaaij, M.; Wouda, B.; Boschma, D.; Liu, Y.; Yuan, Y.; Daamen, W.; de Jong, M.; Teberg, C.; et al. The multi-dimensional challenges of controlling SARS-CoV-2 transmission in indoor spaces: Insights from the linkage of a microscopic pedestrian simulation and virus transmission models. medRxiv 2021. [Google Scholar] [CrossRef]
- Xiao, Y.; Yang, M.; Zhu, Z.; Yang, H.; Zhang, L.; Ghader, S. Modeling indoor-level non-pharmaceutical interventions during the COVID-19 pandemic: A pedestrian dynamics-based microscopic simulation approach. Transp. Policy 2021, 109, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Chraibi, M. On the effectiveness of the measures in supermarkets for reducing contact among customers during COVID-19 period. Sustainability 2020, 12, 9385. [Google Scholar] [CrossRef]
- Mazumdar, S.; Yin, Y.; Guity, A.; Marmion, P.; Gulick, B.; Chen, Q. Impact of moving objects oncontaminant concentration distributions in an inpatient ward with displacement ventilation. Hvac&R Res. 2010, 16, 545–563. [Google Scholar] [CrossRef]
- Yang, W.; Marr, L.C. Mechanisms by which ambient humidity may affect viruses in aerosols. Appl. Environ. Microbiol. 2012, 78, 6781–6788. [Google Scholar] [CrossRef] [PubMed]
- Bluyssen, P.M.; van Zeist, F.; Kurvers, S.; Tenpierik, M.; Pont, S.; Wolters, B.; van Hulst, L.; Meertins, D. The creation of SenseLab: A laboratory for testing and experiencing single and combinations of indoor environmental conditions. Intell. Build. Int. 2018, 10, 5–18. [Google Scholar] [CrossRef]
- Eykelbosh, A. Indoor CO2 Sensors for COVID-19 Risk Mitigation: Current Guidance and Limitations; National Collaborating Centre for Environmental Health: Vancouver, BC, Canada, 2021. [Google Scholar]
- SAGE-EMG. Role of Ventilation in Controlling SARS-CoV-2 Transmission; Tech. Report; SAGE: London, UK, 2020. [Google Scholar]
- Ijaz, M.; Brunner, A.; Sattar, S.; Nair, R.C.; Johnson-Lussenburg, C. Survival characteristics of airborne human coronavirus 229E. J. Gen. Virol. 1985, 66, 2743–2748. [Google Scholar] [CrossRef] [PubMed]
- Morris, D.H.; Yinda, K.C.; Gamble, A.; Rossine, F.W.; Huang, Q.; Bushmaker, T.; Fischer, R.J.; Matson, M.J.; Van Doremalen, N.; Vikesland, P.J.; et al. Mechanistic theory predicts the effects of temperature and humidity on inactivation of SARS-CoV-2 and other enveloped viruses. Elife 2021, 10, e65902. [Google Scholar] [CrossRef]
- Yuan, S.; Jiang, S.C.; Li, Z.L. Do humidity and temperature impact the spread of the novel coronavirus? Front. Public Health 2020, 240. [Google Scholar] [CrossRef]
- ISO/DIS 12913-1; Acoustics—Soundscape—Part 1: Definition and Conceptual Framework. ISO: Geneva, Switzerland, 2014.
- Bluyssen, P. TU Delft—Ventilation against the Coronavirus—Philomena Bluyssen. 2022. Available online: https://www.youtube.com/watch?v=bTiE6bF_PZo (accessed on 4 February 2022).
- Megahed, N.A.; Ghoneim, E.M. Indoor Air Quality: Rethinking rules of building design strategies in post-pandemic architecture. Environ. Res. 2021, 193, 110471. [Google Scholar] [CrossRef]
- Mendell, M.J.; Fisk, W.J.; Kreiss, K.; Levin, H.; Alexander, D.; Cain, W.S.; Girman, J.R.; Hines, C.J.; Jensen, P.A.; Milton, D.K.; et al. Improving the health of workers in indoor environments: Priority research needs for a national occupational research agenda. Am. J. Public Health 2002, 92, 1430–1440. [Google Scholar] [CrossRef]
- Shen, J.; Kong, M.; Dong, B.; Birnkrant, M.J.; Zhang, J. Airborne transmission of SARS-CoV-2 in indoor environments: A comprehensive review. Sci. Technol. Built Environ. 2021, 27, 1331–1367. [Google Scholar] [CrossRef]
- Sha, H.; Zhang, X.; Qi, D. Optimal control of high-rise building mechanical ventilation system for achieving low risk of COVID-19 transmission and ventilative cooling. Sustain. Cities Soc. 2021, 74, 103256. [Google Scholar] [CrossRef] [PubMed]
- Heo, S.; Nam, K.; Loy-Benitez, J.; Li, Q.; Lee, S.; Yoo, C. A deep reinforcement learning-based autonomous ventilation control system for smart indoor air quality management in a subway station. Energy Build. 2019, 202, 109440. [Google Scholar] [CrossRef]


| Concept 1 | Concept 2 | Concept 3 | Concept 4 | Concept 5 | Concept 6 |
|---|---|---|---|---|---|
| airborne diseases | ventilation (system) | air quality | classrooms | indicators | assessment |
| airborne transmission | ventilating (system) | indoor air quality | schools | parameter | measurements |
| airborne infection | air diffuser | offices | criteria | simulations | |
| aerosol dispersion | exhaust | room | models | ||
| droplet dynamics |
| Paper | Solver | Type of Solver | (un)Steady | Model |
|---|---|---|---|---|
| Dai et al. [29] | SIMPLEC | Eulerian | Steady state | RNG k- |
| Ovando-Chacon et al. [30] | - | Eulerian | Steady state | - |
| Faleiros et al. [31] | DPM | Eulerian–Lagrangian | Unsteady state | SST k- |
| Li et al. [32] | SIMPLE | Eulerian | Steady state | RNG k- |
| De Simone et al. [33] | buoyant-SimpleFoam | Eulerian | Steady state | - |
| Foster and Kinzel [34] | StarCCM + QDE (Quanta Dispersion Equation) | Eulerian–Lagrangian | Unsteady state | Spalart–Allmaras |
| Muthusamy et al. [35] | StarCCM | Eulerian–Lagrangian | Unsteady state | (realizable) k- |
| Wu and Weng [22] | DPM (+ SIMPLE to decouple p and U) | Eulerian–Lagrangian | Steady state | SST k- |
| Blocken et al. [36] | SIMPLE | Eulerian–Lagrangian | Steady state | realizable k- |
| Dbouk and Drikakis [37] | - | Eulerian–Lagrangian | Unsteady state | SST k- |
| Dbouk and Drikakis [38] | - | Eulerian–Lagrangian | Unsteady state | - |
| Vuorinen et al. [10] | buoyant-PimpleFoam | Eulerian (in OpenFOAM) | Unsteady state | implicit LES |
| Xu et al. [39] | DPM | Eulerian–Lagrangian | Unsteady state | RNG k- + SST k- |
| Jiao et al. [40] | SIMPLE | Eulerian | Steady state | realizable k- |
| Murakami et al. [41] | SIMPLE | Eulerian | Steady state | standard k- |
| Keshavarz et al. [42] | DPM | Eulerian–Lagrangian | Unsteady state | enhanced k- |
| Gilani et al. [43] | SIMPLE | Eulerian | Steady state | SST k-, standard k-, 3 k- models |
| Villafruela et al. [23] | PISO | Eulerian | Unsteady state | RNG k- |
| Romano et al. [44] | DPM | Eulerian–Lagrangian | Steady state | realizable k- |
| van Hooff and Blocken [45] | SIMPLEC | Eulerian | Unsteady state | realizable k- |
| Aliabadi et al. [46] | - | Eulerian–Lagrangian | Unsteady state | RNG k- + DRW |
| Mao and Celik [47] | - | LS | URANS + RFG | - |
| Lai and Chen [48] | - | Eulerian + Eulerian–Lagrangian | Unsteady state | RNG k- |
| Rohdin and Moshfegh [49] | SIMPLE | Eulerian | Steady state | standard k-, realizable k-, RNG k- |
| Zhang et al. [50] | SIMPLE | Eulerian | Steady state | RNG k- |
| Brohus et al. [51] | - | Eulerian | Steady state | standard k- |
| Lee and Chen [52] | SIMPLEC | Eulerian | Steady state | RNG k- |
| Methods | Articles | Aerosol Dispersion | Ventilation | Infection Risk | Design Parameters | Human Behavior |
|---|---|---|---|---|---|---|
| E | de Man et al. [53], Han et al. [54], Hebbink et al. [55], Ho et al. [56], Li et al. [57], Ortiz et al. [58], Tan et al. [59], Akhtar et al. [60], Kim et al. [61], Bourouiba et al. [62], Hui et al. [63], Tang et al. [64] |  | ||||
| N | Wu and Weng [22], Dbouk and Drikakis [37], Dbouk and Drikakis [38], Xu et al. [39], Aliabadi et al. [46], Mao and Celik [47], Lai and Chen [48], Lee and Chen [52], Chen et al. [65], Wei and Li [66], Xie et al. [67] | |||||
| E | Fu et al. [6], Cao et al. [7], Sun and Zhang [8] |  | ||||
| both | Gilani et al. [43], van Hooff and Blocken [45], Rohdin and Moshfegh [49], Mumtaz et al. [68], Chen [69] | |||||
| N | Lipinski et al. [11], Li et al. [32], Zhang et al. [50], Zhou and Haghighat [70] | |||||
| N | Miller et al. [71], Dai and Zhao [72], Sun and Zhai [73], Peng and Jimenez [74], Sze To and Chao [75], Rudnick and Milton [76], Riley et al. [77] |  |  | |||
| E | Zhang and Bluyssen [78], Zhang et al. [79], Bluyssen et al. [80], Bolashikov et al. [81], Nielsen et al. [82], Nielsen [83], Nielsen et al. [84], Melikov et al. [85] |  |  | |||
| both | Villafruela et al. [23], Romano et al. [44] | |||||
| N | Ovando-Chacon et al. [30], Muthusamy et al. [35], Keshavarz et al. [42], Cao et al. [86] | |||||
| E | Hou et al. [87], Liu et al. [88], Wu et al. [89] |  |  |  | ||
| both | Dai et al. [29], Shao et al. [90] | |||||
| N | Xu et al. [17], Foster and Kinzel [34], Guo et al. [91], Zivelonghi and Lai [92] | |||||
| both | Faleiros et al. [31] |  |  |  | ||
| E | Bluyssen [15], Park et al. [93], Kembel et al. [94] |  |  | |||
| N | Murakami et al. [41], Mohamed et al. [95] | |||||
| N | Kapoor et al. [96], Peng et al. [97] |  |  | |||
| both | Ascione et al. [21] |  |  |  | ||
| N | De Simone et al. [33], Jiao et al. [40], Afshari et al. [98] | |||||
| E | Wang et al. [99] |  |  | |||
| both | Blocken et al. [36] | |||||
| E | Blocken et al. [100], Halvoňová and Melikov [101] |  |  |  | ||
| N | Vuorinen et al. [10], Brohus et al. [51], Duives et al. [102], Xiao et al. [103], Xu and Chraibi [104], Mazumdar et al. [105] |
| Input Parameters |
|---|
| Initial boundary conditions for exhaled breath (velocity, pressure, relative humidity, temperature, turbulence parameters) |
| Initial boundary conditions for ventilation system (velocity, pressure, turbulence parameters) |
| Turbulence model and solver |
| Mesh resolution |
| Ventilation type |
| Room volume (x, y, z) |
| “Human” parameters (dimension of mouth and nostrils, body surface temperature) |
| For mechanical ventilation, position, direction, and airflow of inlets and outlets and ventilation rate |
| Ambient conditions (temperature, pressure, relative humidity) |
| For natural ventilation, number, size, and location of windows and doors, regional climate |
| Number of occupants |
| Number of infected people (usually one) |
| Position of occupants with respect to each other |
| Position of the source generating aerosols (i.e., occupant’s location) |
| Presence of personal ventilation |
| With or without masks |
| Particle injection (kinematic or particle cloud parameters) (in some cases, it was a tracer gas) |
| Articles’ References | [48,55,56] | [6,7,8,11,53,54,58,63,64] | [32,35,37,39,42,44,47,51,52,57,59,60,62,78,79,80,81,84,99] | [61] | [66,106] | [43,49,50,70] | [22,30] | [67] | [38,68] | [45,46,100] | [65] | [17,83,90] | [10,36,86,88] | [71] | [23,85] | [82,101] | [75,77] | [41,69,95] | [72,74] | [29,34,73,76,91,97] | [87,92] | [89] | [96] | [31] | [40] | [21] | [33] | [98] | [93] | [94] | [102] | [103,104] | [105] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dose-related indicators | Physics of particles | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Airflow patterns | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||||
| Temperature | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||||||||||||||||
| Relative Humidity | x | x | x | x | x | x | x | x | ||||||||||||||||||||||||||
| Occupant-related indicators | Infection (exposure) risk | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||||||||||||
| Relative position | x | x | x | x | x | x | ||||||||||||||||||||||||||||
| Duration of stay | x | x | x | x | x | x | x | |||||||||||||||||||||||||||
| Building-related indicators | Windows/doors | x | x | x | x | x | x | x | x | |||||||||||||||||||||||||
| Inlet–outlet mechanical | x | x | x | x | ||||||||||||||||||||||||||||||
| Space layout/volume | x | x | x | x | x | x | x | x | ||||||||||||||||||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hobeika, N.; García-Sánchez, C.; Bluyssen, P.M. Assessing Indoor Air Quality and Ventilation to Limit Aerosol Dispersion—Literature Review. Buildings 2023, 13, 742. https://doi.org/10.3390/buildings13030742
Hobeika N, García-Sánchez C, Bluyssen PM. Assessing Indoor Air Quality and Ventilation to Limit Aerosol Dispersion—Literature Review. Buildings. 2023; 13(3):742. https://doi.org/10.3390/buildings13030742
Chicago/Turabian StyleHobeika, Nadine, Clara García-Sánchez, and Philomena M. Bluyssen. 2023. "Assessing Indoor Air Quality and Ventilation to Limit Aerosol Dispersion—Literature Review" Buildings 13, no. 3: 742. https://doi.org/10.3390/buildings13030742
APA StyleHobeika, N., García-Sánchez, C., & Bluyssen, P. M. (2023). Assessing Indoor Air Quality and Ventilation to Limit Aerosol Dispersion—Literature Review. Buildings, 13(3), 742. https://doi.org/10.3390/buildings13030742









