Exploring the Use of the AEDET Hospital Evaluation Toolkit to Create a Better Healing Environment for Cancer Patients beyond the Global North
Abstract
1. Introduction
1.1. The Importance and the Study Challenge
- Shortening hospital stays;
- The great effect of exposure to nature on pain;
- Increased motivation and productivity in patients and staff.
1.2. Purpose and Objective of the Study
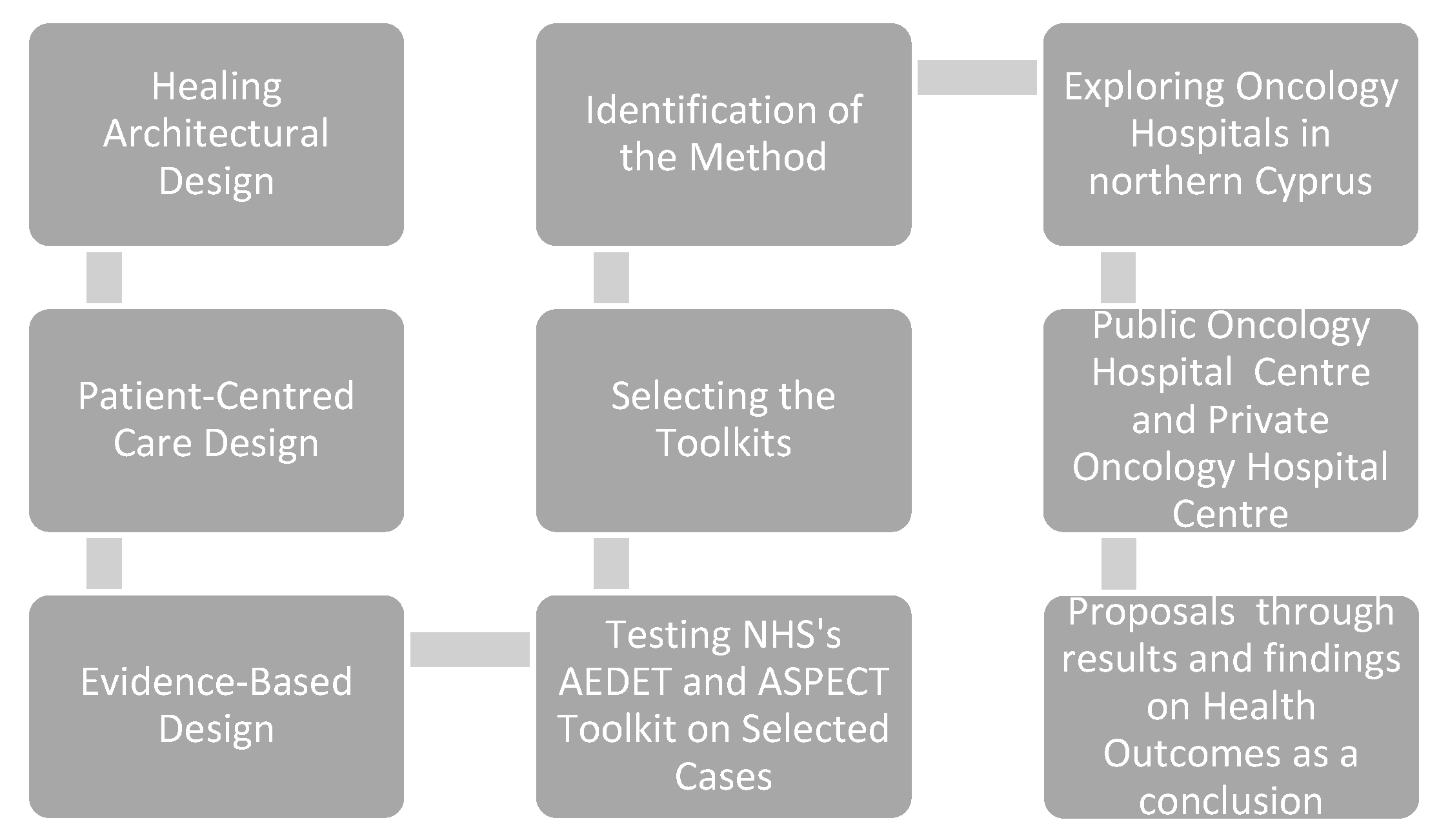
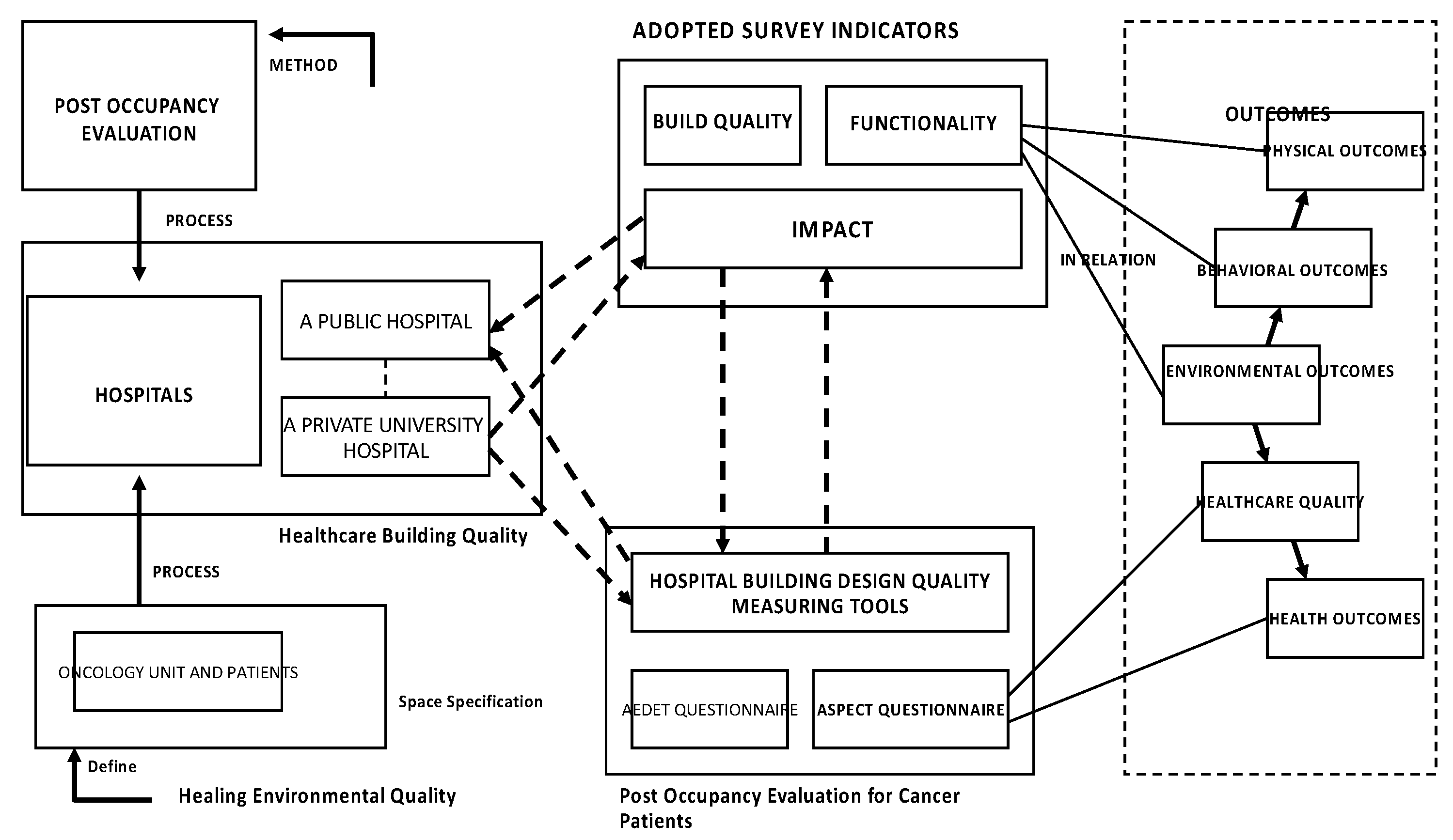
1.3. Study Framework
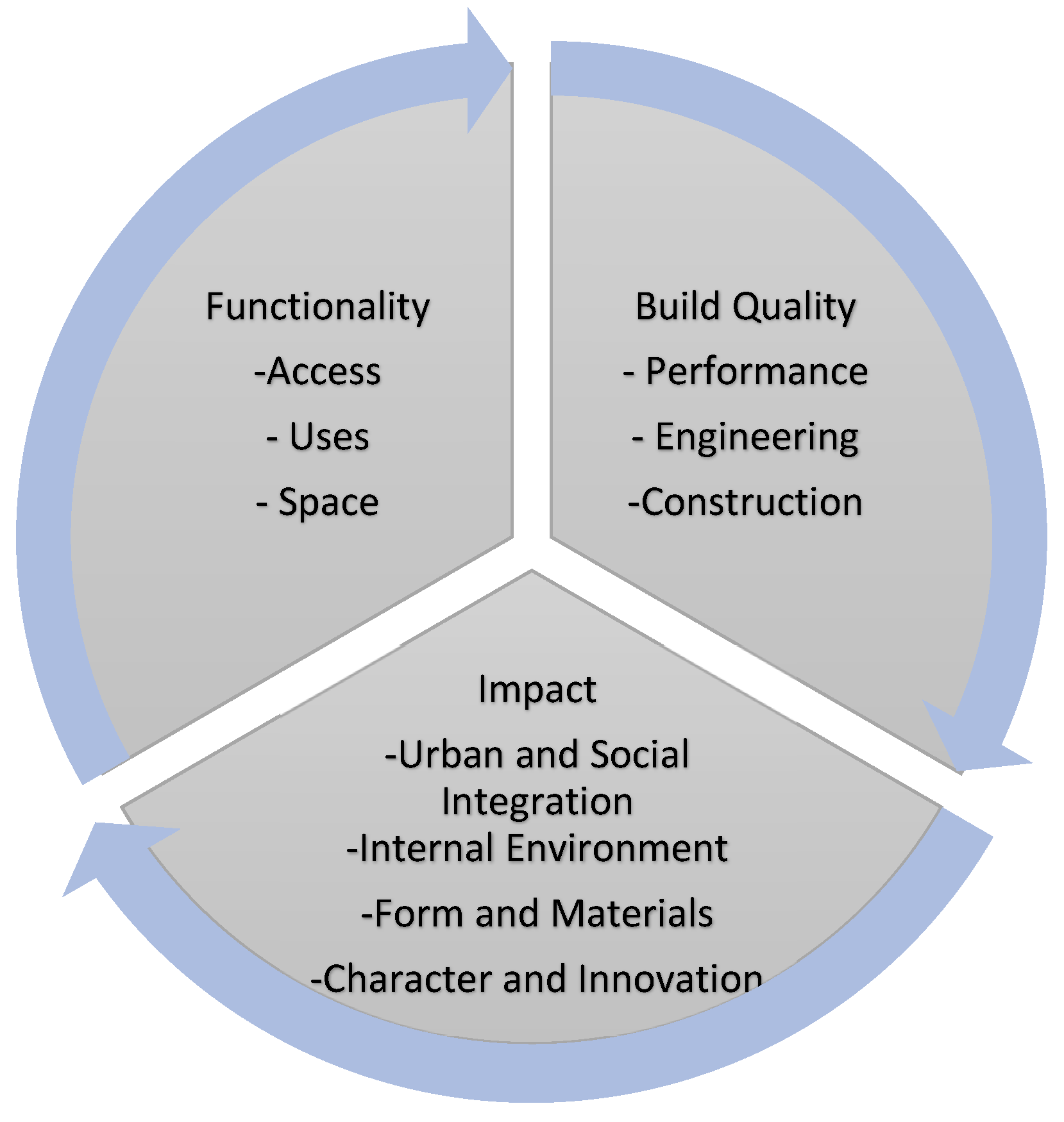
- The AEDET (achieving excellence design evaluation toolkit) Evolution questionnaire is part of a benchmarking tool that assists in measuring and managing the design quality in healthcare facilities. In terms of reliability, it includes references to the evidence-based design literature, and this is related to the criteria used in the evaluation. In terms of validity, its use is mandatory in major hospital design development in N. Cyprus. It evaluates a design through a series of statements that encompass three areas. The impact area deals with the degree to which the building creates a sense of place and contributes positively to the lives of the users and its neighbors. It involves four sections—character and innovation, form and materials, staff and patient environment, and urban and social integration. The build quality area deals with the physical components of the building rather than the spaces and involves three sections—performance, construction, and engineering. The functionality area deals with issues on the primary purpose of the building and involves three sections—use, access, and space—as follows [26]. Table 1. below, shows the criteria for the AEDET evolution in detail which is reproduced from the AEDET checklist under the open government licence and transformed to a table.
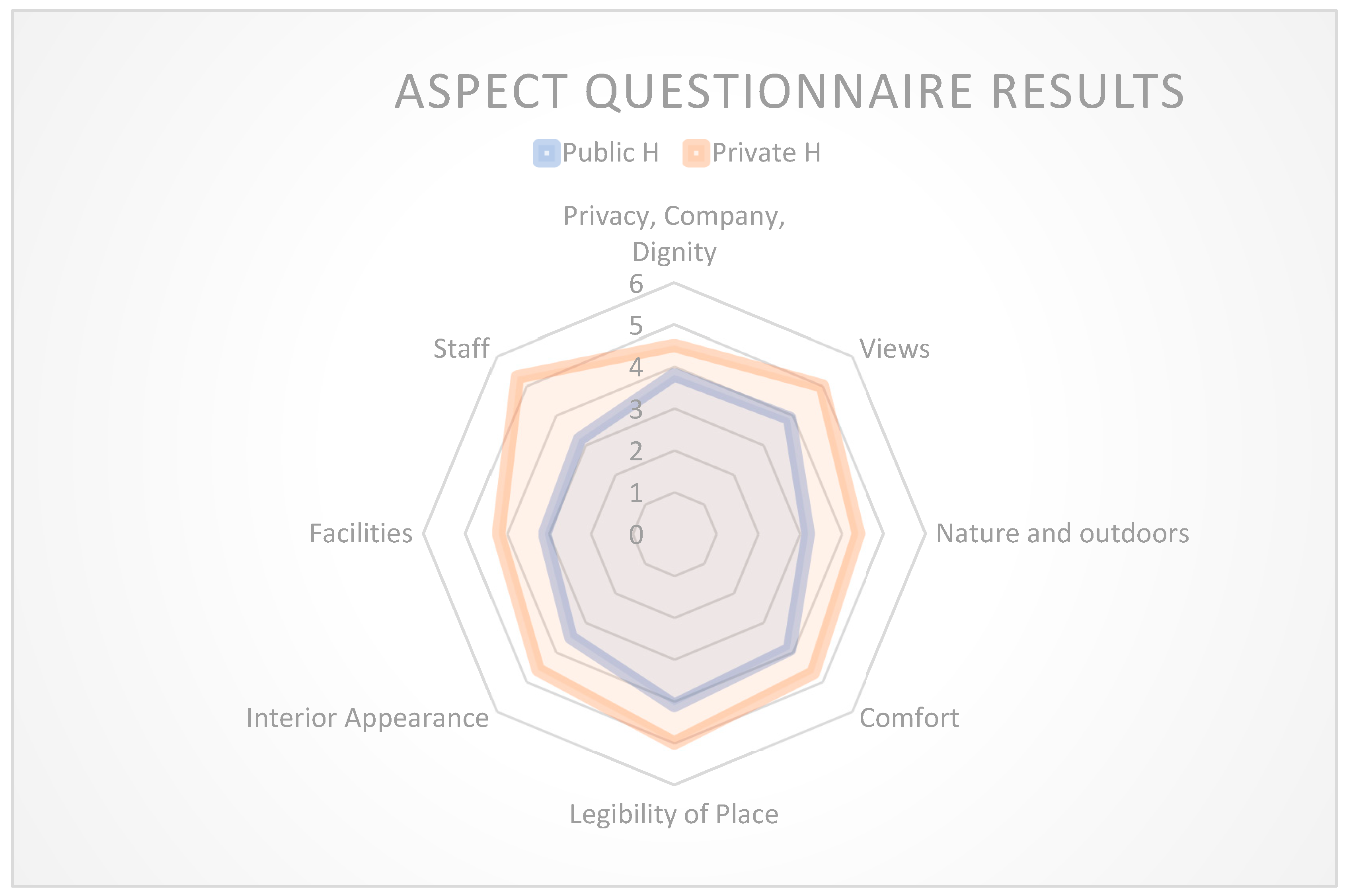
- The ASPECT (a staff and patient environment calibration toolkit) toolkit measures the manner in which the healthcare environment can impact both the satisfaction levels of patients and the provision of facilities to staff. It evaluates eight sections—privacy, company, and dignity, views; nature and outdoors; comfort and control; legibility of place; interior appearance; facilities; and staff. In terms of reliability and validity, the ASPECT toolkit is based on a database of over 600 pieces of research. The ASPECT evaluation toolkit, in the form of questionnaires, assesses users’ satisfaction with both nurses and patients. In this study, an overall total of 50 staff, 20 professionals, including architects, engineers, and stakeholders, and 150 cancer patients responded to the questionnaires as follows [35]. Table 2 shows the criteria for the AEDET evolution in detail which is reproduced from the ASPECT checklist under the open government licence and transformed to a table.
1.4. Case Study Setting
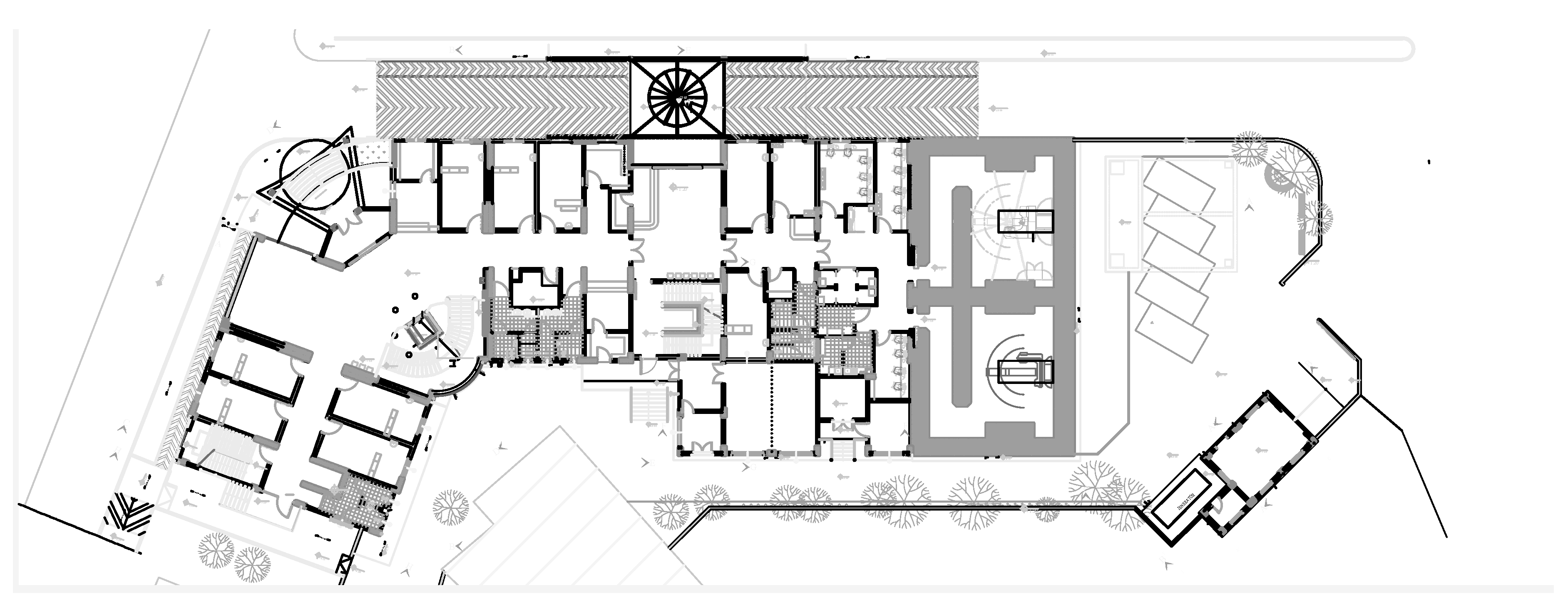
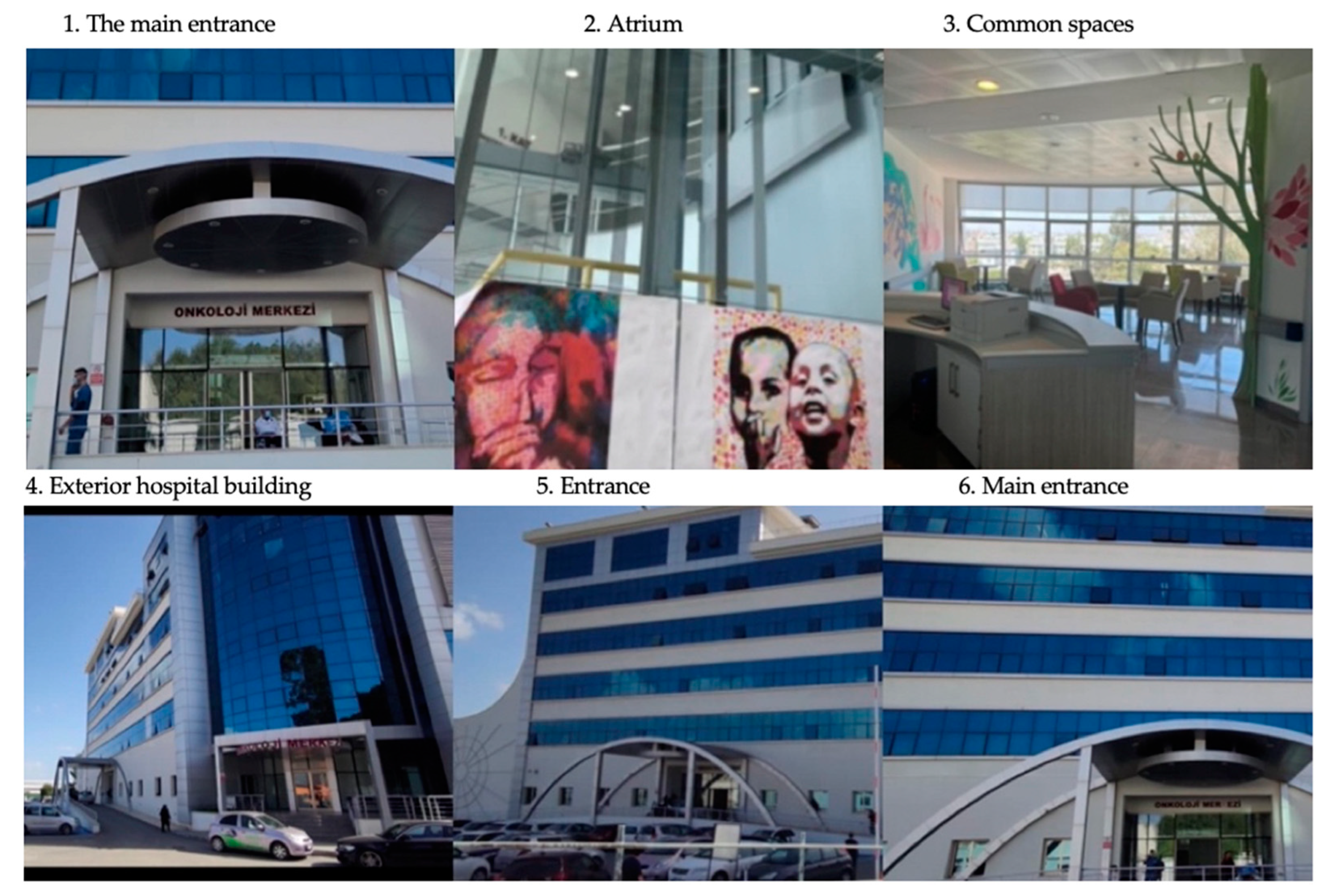
1.4.1. Hospital A: A Public Central Hospital’s Oncology Centre
1.4.2. Hospital B: Private Hospital Oncology Unit
2. Materials and Methods
2.1. Data Collection and Research Design
Data Analysis
- -
- A literature review;
- -
- A comparative analysis between the two hospitals;
- -
- Testing the AEDET and ASPECT toolkits as questionnaires in these hospitals amongst patients, relatives, and staff;
- -
- Semi-structured interviews with architects;
- -
- Personal building observations;
- -
- A photo content analysis;
- -
- Results being shown as tables in numeric form and as charts for comparison.
- -
- One hundred and fifty cancer patients and relatives above 18 years old (75 per hospital);
- -
- Fifty doctors and staff (25 per hospital);
- -
- Twenty professionals such as architects, engineers, and stakeholders.
3. Results
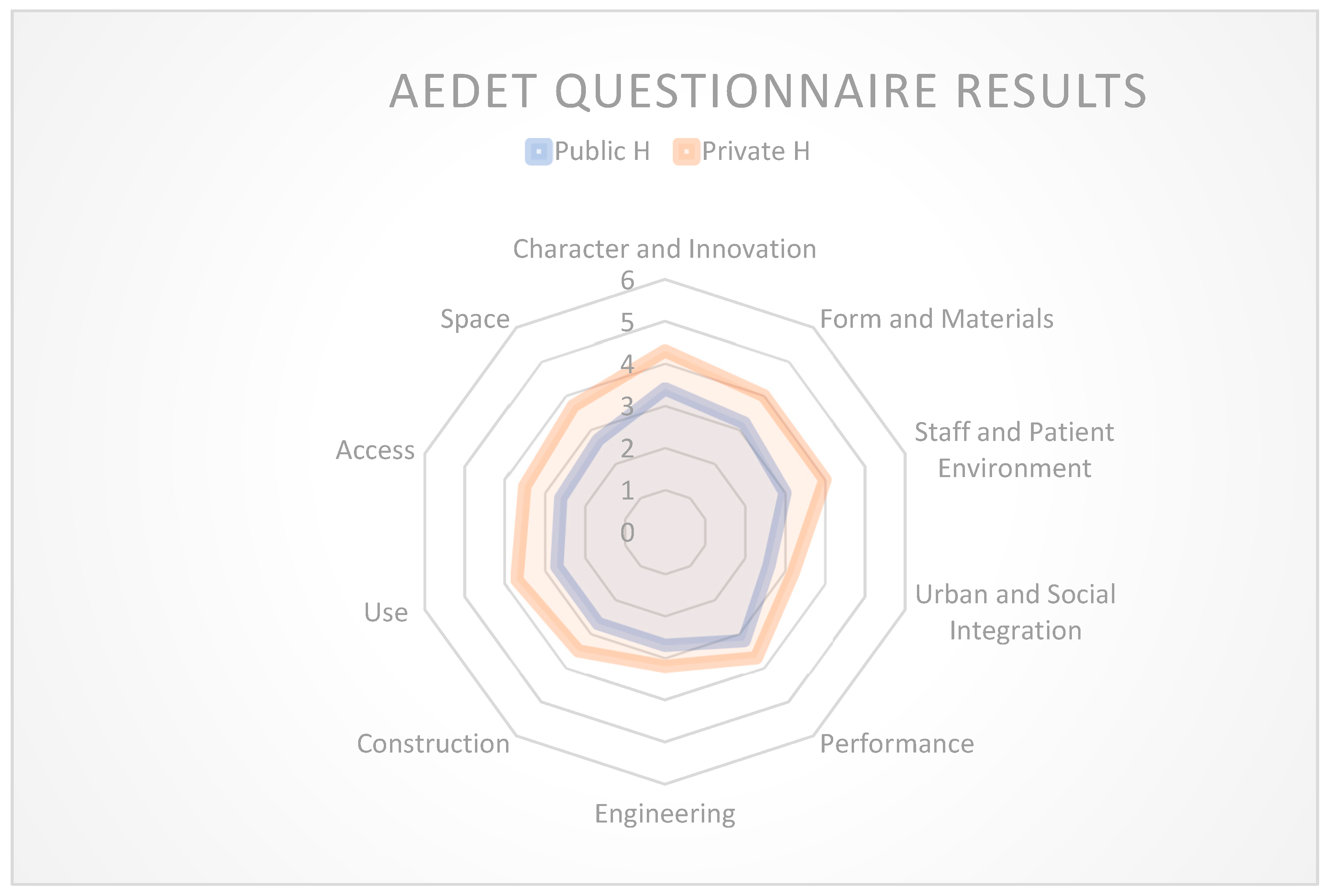
3.1. AEDET Toolkit Findings
3.2. Comparative Case Study Findings between Hospitals
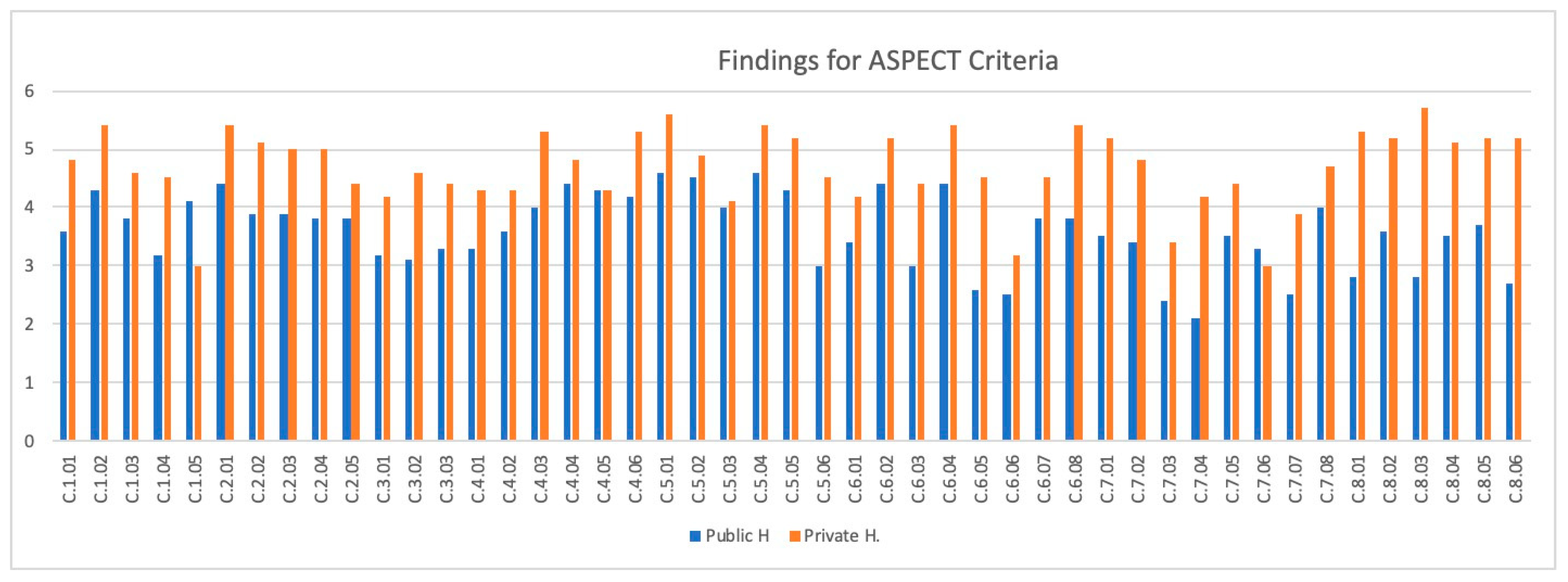
3.3. Findings of the Data Analysis Method for the ASPECT Toolkit
3.4. Comparative Case Study Findings between Hospitals
4. Discussion
4.1. According to Data Analysis Results for AEDET Toolkit
- The goal in healthcare environments is to create nurturing, home-like spaces for patients that prioritize patient-centered care. This can be achieved by optimizing the design to provide access to nature, maximize natural light through large windows, reduce noise with single-bed patient rooms and outdoor healing gardens, and use calming natural colors. Technology integration is also important for sustainability. Proximity to nature is a key element in designing healing spaces, with factors like daylight, ventilation, tranquility, and natural colors being consistent considerations in hospital design [41].
- Environmental factors significantly impact building designs, including healthcare facilities. However, there is often a lack of consideration for these factors in healthcare facility planning. To enhance patient health and wellness, it is essential to integrate natural settings, establish visual connections with nature, and create therapeutic healing gardens. The use of natural light and color can elevate environmental quality standards, leading to faster patient recovery [42].
- Patient rooms must be designed to create a homely, attractive environment that contributes to patient well-being and faster recovery. Therefore, in stationary rooms and waiting areas, attention should be paid to the use of natural light, natural materials, and textures, as well as artistic objects [43].
- The location of the building and the selection of the place with the city center;
- Contextual design principles;
- The functional relationship of efficient and appropriate interior spaces;
- Easy signs for in-hospital navigation;
- Suitably designed and accessible structures for all people [44].
4.2. According to Data Analysis Results for ASPECT Toolkit
4.3. Recommended Design Criteria Checklist
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huisman, E.R.C.M.; Morales, E.; van Hoof, J.; Kort, H.S.M. Healing Environment: A Review of the Impact of Physical Environmental Factors on Users. Build. Environ. 2012, 58, 70–80. [Google Scholar] [CrossRef]
- Nightingale, F. Introductory Notes on Lying-In Institutions; Longmans, Green: London, UK, 1871; Volume 3. [Google Scholar]
- Tekin, B.H.; Corcoran, R.; Gutiérrez, R.U. A Systematic Review and Conceptual Framework of Biophilic Design Parameters in Clinical Environments. Health Environ. Res. Des. J. 2023, 16, 233–250. [Google Scholar] [CrossRef]
- Sternberg, E.M. Healing Spaces: The Science of Place and Well-Being; Harvard University Press: Cambridge, MA, USA, 2010; pp. 50–70. [Google Scholar]
- Smith, R.; Watkins, N. Therapeutic Environments | WBDG—Whole Building Design Guide. Wbdg.org. Available online: https://www.wbdg.org/resources/therapeutic-environments (accessed on 20 July 2023).
- Alfonsi, E.; Capolongo, S.; Buffoli, M. Evidence-Based Design and healthcare: An unconventional approach to hospital design. Ann. Ig. 2014, 26, 137–143. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Simons, R.F.; Losito, B.D.; Fiorito, E.; Miles, M.A.; Zelson, M. Stress Recovery during Exposure to Natural and Urban Environments. J. Environ. Psychol. 1991, 11, 201–230. [Google Scholar] [CrossRef]
- Hamilton, D.K.; Watkins, D.H. Evidence-Based Design for Multiple Building Types; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2009. [Google Scholar]
- Cama, R. Evidence-Based Healthcare Design; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Berry, L.L.; Crane, J.; Deming, K.A.; Barach, P. Using Evidence to Design Cancer Care Facilities. Am. J. Med. Qual. 2020, 35, 397–404. [Google Scholar] [CrossRef]
- Browning, W.; Ryan, C.O.; Clancy, J.O. 14 Patterns of Biophilic Design; Terrapin Bright Green: New York, NY, USA, 2014. [Google Scholar]
- Kellert, S.R.; Heerwagen, J.; Mador, M. Biophilic Design: The Theory, Science and Practice of Bringing Buildings to Life; Wiley: Hoboken, NJ, USA, 2013. [Google Scholar]
- The World Health Organisation. Public Health 1946, 60, 74–75. [CrossRef]
- Høybye, M.T. Healing environments in cancer treatment and care. Relations of space and practice in hematological cancer treatment. Acta Oncol. 2013, 52, 440–446. [Google Scholar] [CrossRef]
- Jencks, C. The Architecture of Hope; Frances Lincoln Ltd.: London, UK, 2015. [Google Scholar]
- Gokcora, N.; Ince, F.; Hocaoglu, M.; Akcay, N.; Eker, O. Kidem Cyprus Cancer Statistics; Ministry of Health Report; Ministry of Health: North Cyprus, Türkiye, 2018; pp. 2–37. [Google Scholar]
- Gashoot, M.M. Holistic Healing Framework: Impact of the Physical Surrounding Design on Patient Healing and Wellbeing. Art Des. Rev. 2022, 10, 18–28. [Google Scholar] [CrossRef]
- Phiri, M. Design Tools for Evidence-Based Healthcare Design; Routledge: London, UK, 2015. [Google Scholar]
- Design Quality Indicator as a Tool for Thinking. Available online: https://www.tandfonline.com/doi/abs/10.1080/0961321032000107564 (accessed on 20 July 2023).
- Ulrich, R. Nature, and Mental Health: Biophilia and Biophobia. Environ. Ment. Health 1993, 3, 179–196. [Google Scholar]
- Sussman, A.; Hollander, J.B. Cognitive Architecture: Designing for How We Respond to the Built Environment; Routledge: New York, NY, USA, 2015. [Google Scholar]
- Lavdas, A.A.; Tasser, E.; Schirpke, U. Assessing Landscape Aesthetic Values: Do Clouds in Photographs Influence People’s Preferences? PLoS ONE 2023, 18, e0288424. [Google Scholar] [CrossRef]
- KKTC Sağlık Bakanlığı > İSTATİSTİKİ BİLGİLER > KANSER İSTATİSTİKLERİ. Gov.ct.tr. Available online: http://arsiv.salik.gov.ct.tr/ (accessed on 20 June 2023).
- Ruggles, D.H. Beauty, Neuroscience, and Architecture: Timeless Patterns and Their Impact on Our Well-Being; Fibonacci: Denver, CO, USA, 2018. [Google Scholar]
- Taylor, E.; Hignett, S. DEEP SCOPE: A Framework for Safe Healthcare Design. Int. J. Environ. Res. Public Health 2021, 18, 7780. [Google Scholar] [CrossRef] [PubMed]
- Achieving Excellence Design Evaluation Toolkit. Available online: https://www.pcpd.scot.nhs.uk/Capital/SCIM_Pilot/2017/AEDET%20Refresh%20Guidance.docx (accessed on 10 May 2023).
- Ghazali, R.; Abbas, M.Y. Natural Environment in Paediatric Wards: Status and Implications. Procedia-Soc. Behav. Sci. 2012, 68, 173–182. [Google Scholar] [CrossRef][Green Version]
- Alalouch, C.; Aspinall, P.A.; Smith, H. Design Criteria for Privacy-Sensitive Healthcare Buildings. Int. J. Eng. Technol. 2016, 8, 32–39. [Google Scholar] [CrossRef]
- Fouad, J.; Mahmood, F. Post-occupancy evaluation Correlated with Medical Staffs’ Satisfaction: A Case Study of Indoor Environments of General Hospitals in Sulaimani City. J. Eng. 2021, 27, 28–48. [Google Scholar] [CrossRef]
- Kobus, R.L. Building Type Basics for Healthcare Facilities; Wiley: Hoboken, NJ, USA, 2008. [Google Scholar]
- CHD. Center for Health Design. Available online: https://www.healthdesign.org/certification-outreach/edac/about-ebd (accessed on 31 August 2022).
- Preiser, W.F.E.; Rabinowitz, H.Z.; White, E.T. Post-Occupancy Evaluation; Van Nostrand Reinhold: New York, NY, USA, 1988. [Google Scholar]
- Miller, R.L.; Swensson, E.S. New Directions In Hospital and Healthcare Facility Design; McGraw-Hill: New York, NY, USA, 1995. [Google Scholar]
- van der Voordt, D.J.M.; van Wegen, H.B.R. Architecture in Use: An Introduction to the Programming, Design, and Evaluation of Buildings; Elsevier: Amsterdam, The Netherlands, 2005. [Google Scholar]
- The National Archives ASPECT. Available online: http://webarchive.nationalarchives.gov.uk/20130124042001/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_082081.pdf (accessed on 21 August 2022).
- Kvåle, K.; Bondevik, M. What Is Important for Patient Centred Care? A Qualitative Study about the Perceptions of Patients with Cancer. Scand. J. Caring Sci. 2008, 22, 582–589. [Google Scholar] [CrossRef]
- Ulrich, R.S. Viewing through a window may influence recovery from surgery. Science 1984, 224, 420–421. [Google Scholar] [CrossRef] [PubMed]
- North Cyprus Ministry of Health. North Cyprus. Available online: http://bndh.gov.ct.tr/tr/servisler/dahili-birimler/onkoloji (accessed on 8 February 2022).
- Near East University Hospital. North Cyprus. Available online: https://neareasthospital.com/departments/medical-oncology/?lang=en (accessed on 8 February 2022).
- Zeisel, J. Inquiry by Design: Environment/Behavior/Neuroscience in Architecture, Interiors, Landscape, and Planning; W.W. Norton & Co.: New York, NY, USA, 2006. [Google Scholar]
- Ulrich, R.S. How design impacts wellness. Healthc. Forum J. 1992, 35, 20–25. [Google Scholar]
- Berg, A.E.V.D. Health Impacts of Healing Environments: A Review of the Evidence for Benefits of Nature, Daylight, Fresh Air, and Quiet in Healthcare Settings; University Hospital: Groningen, The Netherlands, 2005. [Google Scholar]
- Greenberg, J.; Jonas, E. Psychological Motives and Political Orientation—The Left, the Right, and the Rigid: Comment on Jost et al. (2003). Psychol. Bull. 2003, 129, 376–382. [Google Scholar] [CrossRef]
- Sunand, P. Changing Hospital Architecture, 1st ed.; RIBA: London, UK, 2008. [Google Scholar]
- Ismaeil, E.M.H.; Sobaih, A.E.E. Enhancing Healing Environment and Sustainable Finishing Materials in Healthcare Buildings. Buildings 2022, 12, 1676. [Google Scholar] [CrossRef]
- Akinluyi Muyiwa, L.; Fadamiro Joseph, A.; Ayoola Hezekiah, A.; Alade Morakinyo, J. Theoretical Issues and Conceptual Framework for Physical Facilities Design in Hospital Buildings. J. Archit. Environ. Struct. Eng. Res. 2021, 4, 28–35. [Google Scholar]
- Pantavou, K.; Giallouros, G.; Philippopoulos, K.; Piovani, D.; Cartalis, C.; Bonovas, S.; Nikolopoulos, G.K. Thermal Conditions and Hospital Admissions: Analysis of Longitudinal Data from Cyprus (2009–2018). Int. J. Environ. Res. Public Health 2021, 18, 13361. [Google Scholar] [CrossRef] [PubMed]


| Aedet Evolution | Criteria | Layers |
|---|---|---|
| Impact | A: Character and Innovation | A.01: There are clear ideas behind the design of the building and grounds. A.02: The building and grounds are interesting to look at and move around in. A.03: The building, grounds, and art design contribute to the local setting. A.04: The design appropriately expresses the appropriate values. A.05: The project is likely to influence future healthcare designs. |
| B: Form and Materials | B.01: The design has a human scale and feels welcoming. B.02: The design contributes to the local microclimate, maximizing sunlight and shelter from prevailing winds. B.03: Entrances are obvious and logical, about likely points of arrival on site. B.04: The external materials and detailing appear to be of high quality. B.05: The external colours and textures seem appropriate and attractive. B.06: The design maximizes the site opportunities and enhances a sense of place. | |
| C: Staff and Patient Environment | C.01: The design respects the dignity of patients and allows for appropriate levels of privacy and company. C.02: The design maximzses opportunities for daylight/views of greenery or natural landscape. C.03: The design maximizes opportunities for access to usable outdoor space. C.04: There are high levels both of comfort and control of comfort. C.05: The design is understandable, and wayfinding is intuitive. C.06: The interior of the facility is attractive. C.07: There are good baths/toilets and other facilities for patients. C.08: There are good facilities for staff, including convenient places to work and relax without being on demand. | |
| D: Urban Social Integration | D.01: The height, volume, and skyline of the design relate well to its setting. D.02: The facility contributes positively to its locality. D.03: The hard and soft landscapes contribute positively to the locality. D.04: The design is sensitive to neighbors and passers-by. | |
| Build Quality | E: Performance | E.01: The facility is easy to operate. E.02: The facility is easy to clean and maintain. E.03: The facility has appropriately durable finishes and components. E.04: The facility will weather and age well. E.05: Access to daylight, views of nature, and outdoor space are robust. E.06: The design maximizes the opportunities for sustainability. |
| F: Engineering | F.01: The engineering systems are well designed, flexible, and effective. F.02: The engineering systems exploit any benefits from standardization and prefabrication where relevant. F.03: The engineering systems are energy-efficient. F.04: There are emergency backup systems that are designed to minimize disruption. F.05: During construction, disruption to essential healthcare services is minimized. | |
| G: Construction | G.01: If phased construction is necessary, the various stages are well organized. G.02: Temporary construction work is minimized. G.03: The impact of the building process on continuing healthcare provision is minimized. G.04: The building and grounds can be readily maintained. G.05: The construction is robust. G.06: The construction allows easy access to engineering systems for maintenance. G.07: The construction exploits any benefits from standardization and prefabrication where relevant. | |
| Functionality | H: Use | H.01: The prime functional requirements of the brief are satisfied. H.02: The design facilitates the care model. H.03: Overall the design is capable of handling the projected throughput. H.04: Workflows and logistics are arranged optimally. H.05: The design is sufficiently flexible to respond to enable expansion. H.06: Where possible, spaces are standardized and flexible in use patterns. H.07: The design facilitates both security and supervision. |
| I: Access | I.01: There is good access from available public transport including any on-site roads. I.02: There is adequate parking for visitors and staff cars with appropriate provisions for disabled people. I.03: The approach and access for ambulances are appropriately provided. I.04: Service vehicle circulation is good and does not inappropriately impact the experience for service users and staff. I.05: Pedestrian access routes are obvious, pleasant, and suitable for wheelchair users and people with other disabilities/impaired sight. I.06: Outdoor spaces, wherever appropriate, are useable, with safe lighting indicating paths, ramps, steps, and fire egress. I.07: Active travel is encouraged, and connections to local green routes and spaces are enhanced. | |
| J: Space | J.01: The design achieves appropriate space standards J.02: The ratio of usable space to the total area is good J.03: The circulation distances travelled by staff, patients and visitors are minimized by the layout J.04: Any necessary isolation and segregation of spaces is achieved. J.05: The design maximises opportunities for space to encourage informal social interaction and wellbeing. J.06: There is adequate storage space |
| Aspect | Aspect criteria | Layers |
|---|---|---|
| C: Staff and Patient Environment | C1: Privacy, company, and dignity | 1.01: Patients can choose to have visual privacy. 1.02: Patients can have private conservations. 1.03: Patients can be alone. 1.04: Patients have places where they can be with others. 1.05: Toilets/bathrooms are located logically, conveniently, and discretely. |
| C2: Views | 2.01: Spaces where staff and patients spend time have windows. 2.02: Patients and staff can easily see the sky. 2.03: Patients and staff can easily see the ground. 2.04: The view outside is calming. 2.05: The view outside is interesting. | |
| C3: Nature and Outdoors | 3.01: Patients can go outside. 3.02: Patients and staff have access to usable landscaped areas. 3.03: Patients and staff can easily see plants, vegetation, and nature. | |
| C4: Comfort | 4.01: There is a variety of artificial lighting patterns appropriate for day and night and for summer and winter. 4.02: Patients and staff can easily control the artificial lighting. 4.03: Patients and staff can easily exclude sunlight and daylight. 4.04: Patients and staff can easily control the temperature. 4.05: Patients and staff can easily open windows/doors. 4.06: The design layout minimizes unwanted noise in staff and patient areas. | |
| C5: Legibility of Place | 5.01: When you arrive at the building, the entrance is obvious. 5.02: It is easy to understand the way the building is laid out. 5.03: There is a logical hierarchy of places in the building. 5.04: When you leave the building, the way out is obvious. 5.05: It is obvious where to go find a member or staff. 5.06: Different parts of the building have different characters. | |
| C6: Interior Appearance | 6.01: Patients’ spaces feel homely. 6.02: The interior feels light and airy. 6.03: The interior has a variety of colors, textures, and views. 6.04: The interior looks clean, tidy, and cared for. 6.05: The interior has provisions for art, plants, and flowers. 6.06: The ceilings are designed to look interesting. 6.07: Patients can have and display personal items in their own space. 6.08: Floors are covered with suitable material. | |
| C7: Facilities | 7.01: The bathroom has seats, handrails, non-slip flooring, a shelf for toiletries, and somewhere to hang clothes within easy reach. 7.02: Patients can have a choice of bath/shower and assisted/unassisted bathrooms. 7.03: There is a space where religious observances can take place. 7.04: There is a place where live performances can take place. 7.05: There is a place where live performances can take place. 7.06: Patients have facilities to make drinks. 7.07: There are accessible vending machines for snacks. 7.08: There are facilities for patients’ relatives/friends to stay overnight. | |
| C8: Staff | 8.01: Staff have a convenient place to change and securely store belongings and clothes. 8.02: Staff have convenient places to concentrate on work without being in demand. 8.03: There are convenient places where staff can speedily get snacks and meals. 8.04: Staff can rest and relax in places segregated from patient and visitor areas 8.05: All staff have easy and convenient access to IT. 8.06: Staff have convenient access to basic banking facilities and can shop for essentials. 8.07: The design facilitates both security and supervision. |
| AEDET Design Criteria | Public Oncology Hospital-A | Private Oncology Hospital-B | AEDET Design Criteria | Public Oncology Hospital-A | Private Oncology Hospital-B | AEDET Design Criteria | Public Oncology Hospital-A | Private Oncology Hospital-B | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Impact | A. Character and Innovation | A.01 | 3.4 | 4.4 | Build Quality | E. Performance | E.01 | 3.5 | 3.8 | Functionality | H. Use | H.01 | 2.7 | 3.5 |
| A.02 | 3.2 | 4.1 | E.02 | 3.5 | 3.8 | H.02 | 2.7 | 3.2 | ||||||
| A.03 | 3.6 | 4.4 | E.03 | 3 | 3.5 | H.03 | 2.9 | 4 | ||||||
| A.04 | 3.5 | 4.2 | E.04 | 3.3 | 3.8 | H.04 | 2.7 | 4.1 | ||||||
| A.05 | 3.2 | 4.3 | E.05 | 3 | 3.8 | H.05 | 2.5 | 4.1 | ||||||
| B. Form and Materials | B.01 | 3.6 | 4.5 | E.06 | 3.3 | 3.5 | H.06 | 2.8 | 3.4 | |||||
| B.02 | 3.2 | 3.7 | F. Engineering | F.01 | 3.4 | 3.6 | H.07 | 2.7 | 4.1 | |||||
| B.03 | 3.6 | 4 | F.02 | 2.8 | 3.2 | I. Access | I.01 | 2.4 | 2.9 | |||||
| B.04 | 3.2 | 4.1 | F.03 | 2.5 | 2.9 | I.02 | 2.5 | 3.9 | ||||||
| B.05 | 3 | 3.6 | F.04 | 2.5 | 3.2 | I.03 | 3.4 | 4 | ||||||
| B.06 | 3 | 3.6 | F.05 | 2.5 | 3.1 | I.04 | 2.6 | 3.6 | ||||||
| C. Staff and Patient Environment | C.01 | 3.3 | 4 | G. Construction | G.01 | 2.4 | 3.3 | I.05 | 2.4 | 3.6 | ||||
| C.02 | 3 | 4.1 | G.02 | 2.5 | 2.8 | I.06 | 2.4 | 3.3 | ||||||
| C.03 | 3.3 | 3.6 | G.03 | 2.3 | 3.2 | I.07 | 2.8 | 3.3 | ||||||
| C.04 | 2.8 | 4 | G.04 | 2.9 | 3.7 | J. Space | J.01 | 2.9 | 3.8 | |||||
| C.05 | 3.1 | 3.8 | G.05 | 3.3 | 4 | J.02 | 2.3 | 3.6 | ||||||
| C.06 | 2.9 | 4.3 | G.06 | 3.1 | 3.6 | J.03 | 3.1 | 3.7 | ||||||
| C.07 | 3.1 | 4.1 | G.07 | 2.8 | 3.7 | J.04 | 2.8 | 3.6 | ||||||
| C.08 | 3.1 | 3.7 | J.05 | 2.5 | 4 | |||||||||
| D. Urban and Social Integration | D.01 | 3 | 3.2 | J.06 | 2.6 | 3.9 | ||||||||
| D.02 | 3.3 | 4 | ||||||||||||
| D.03 | 2 | 2.9 | ||||||||||||
| D.04 | 2.4 | 2.8 | ||||||||||||
| ASPECT Design Criteria | Public Oncology Hospital-A | Private Oncology Hospital-B | ASPECT Design Criteria | Public Oncology Hospital-A | Private Oncology Hospital-B | ASPECT Design Criteria | Public Oncology Hospital-A | Private Oncology Hospital-B | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C.Staff and Patient Environment | C1. Privacy, company and dignity | C1.01 | 3.6 | 4.8 | C5. Legibility Of Place | C5.01 | 4.6 | 5.6 | C7. Facilities | C7.01 | 3.5 | 5.2 |
| C1.02 | 4.3 | 5.4 | C5.02 | 4.5 | 4.9 | C7.02 | 3.4 | 4.8 | ||||
| C1.03 | 3.8 | 4.6 | C5.03 | 4 | 4.1 | C7.03 | 2.4 | 3.4 | ||||
| C1.04 | 3.2 | 4.5 | C5.04 | 4.6 | 5.4 | C7.04 | 2.1 | 4.2 | ||||
| C1.05 | 4.1 | 3 | C5.05 | 4.3 | 5.2 | C7.05 | 3.5 | 4.4 | ||||
| C2. Views | C2.01 | 4.4 | 5.4 | C5.06 | 3 | 4.5 | C7.06 | 3.3 | 3 | |||
| C2.02 | 3.9 | 5.1 | C6. Interior Appearance | C6.01 | 3.4 | 4.2 | C7.07 | 2.5 | 3.9 | |||
| C2.03 | 3.9 | 5 | C6.02 | 4.4 | 5.2 | C7.08 | 4 | 4.7 | ||||
| C2.04 | 3.8 | 5 | C6.03 | 3 | 4.4 | C8. Staff | C8.01 | 2.8 | 5.3 | |||
| C2.05 | 3.8 | 4.4 | C6.04 | 4.4 | 5.4 | C8.02 | 3.6 | 5.2 | ||||
| C3. Nature and outdoors | C3.01 | 3.2 | 4.2 | C6.05 | 2.6 | 4.5 | C8.03 | 2.8 | 5.7 | |||
| C3.02 | 3.1 | 4.6 | C6.06 | 2.5 | 3.2 | C8.04 | 3.5 | 5.1 | ||||
| C3.03 | 3.3 | 4.4 | C6.07 | 3.8 | 4.5 | C8.05 | 3.7 | 5.2 | ||||
| C4. Comfort | C4.01 | 3.3 | 4.3 | C6.08 | 3.8 | 5.4 | C8.06 | 2.7 | 5.2 | |||
| C4.02 | 3.6 | 4.3 | ||||||||||
| C4.03 | 4 | 5.3 | ||||||||||
| C4.04 | 4.4 | 4.8 | ||||||||||
| C4.05 | 4.3 | 4.3 | ||||||||||
| C4.06 | 4.2 | 5.3 | ||||||||||
| AEDET Aspectsin Detail | Results for Physical Appearence |
|---|---|
| A. ‘Character and Innovation’ | There was a slight difference in the impact session, which formed the character and innovation in both hospitals; the public oncology center was accepted as moderate for this section. The private hospital’s oncology unit could be accepted as ‘good’. |
| B. ‘Form and Materials’ | This section consisted of eight aspects, where both hospital’s results were obtained with nearly similar or very small differences between them. In terms of forms and materials, colors, and textures, the main concern was the use of external colours. |
| C. ‘Staff and Patient Environment’ | In the interior environment section, which is extremely important in terms of the general appearance, c7 was found to be almost the same for both hospitals. C6 needs to be improved for the public oncology center as well as for staff. |
| D. ‘Urban and Social Integration’ | In general, in four aspects of urban and social integration, including the height of the settings, positive attributes, landscape, and parking spaces, the private hospital was more successful; however, landscaping and neighborhood were very poor in both hospitals and need to be improved. |
| E. ‘Performance’ | The building performance and facilities were average and very similar for both hospitals. |
| F. ‘Engineering’ | During construction, disruption to essential healthcare services was minimized. The public hospital was below the average and could be constructed with a better engineering level. |
| G. ‘Construction’ | There were emergency backup systems that were designed to minimize disruption. The average values were very clearly different from each other for both hospitals, where the private hospital could be accepted as above average and the public hospital was still below average. |
| H. ‘Use’ | The use of materials, colours, and engineering systems were energy-efficient for the private hospital; however, again, for the public hospital, this needs to be improved in the weakest areas. |
| I. ‘Access’ | The engineering systems exploited any benefits from standardization and prefabrication, and where relevant, they need to be improved for both hospitals. Access to the hospitals could be better; if improved well, this can be easily achieved. |
| J. ‘Space’ | This is also a strong aspect that needs to be improved for the public hospital. |
| ASPECT CRITERIA | Discussion through Results |
|---|---|
| C1. ‘Privacy, company and dignity’ | Patient privacy decisions, private conversations, being alone, and having places to be with others were higher in value in the private hospital when compared with the public oncology center. However, only the choice of the location of toilets/bathrooms was conducted more logically in the public oncology center. Overall, the private hospital had better privacy, company, and dignity recognition compared to the public oncology center. |
| C2. ‘Views’ | The aspects of having a natural view, time spent with windows, seeing the sky, seeing the ground, an outside calming view, and an outside interesting view nearly reached the highest standards in the private hospital oncology unit. On the other hand, an obvious difference was observed in the decrease in these values in the public hospital’s oncology center, where the location and the view still scored average values but were not more than those of the private hospital. |
| C3. ‘Nature’ | Connection with nature and the outdoors needs to be studied further by providing more access to the existing landscape or creating a landscape for the users to feel more engaged with nature itself. In this sense, the public hospital’s oncology center was very poor in terms of providing a natural environment, and the private hospital’s oncology unit could also be developed to be better. |
| C4. ‘Comfort’ | In terms of comfort, the findings were almost close to each other, with the private hospital’s oncology unit being slightly more successful. Patients and staff could easily control the temperature, patients and staff could easily open windows, and doors were quite equal for both hospitals, which need to be taken into consideration again. |
| C5. ‘Legibility of Place’ | The legibility of space, especially in different parts of the buildings, had different characteristics and was not at the standard level in the public oncology center. However, the aspects of entrance definition, exit definition, and finding related staff were in near-complete agreement for the private oncology unit. The hierarchy of places was almost the same and could be better; for example, if a patient needs to go to the upper levels to find treatment rooms, the access could be located closer to the entrance area. |
| C6. ‘Interior Appearance’ | The interior appearance was more successful in the private oncology unit, where the usage of suitable floor materials was successful and hygienic, and the use of art, plants, and flowers was not applied for the oncology units, but their use in general in the hospital was adequate. In both hospitals, the ceiling design was not successful and was below acceptable limits. Unfortunately, the public hospital’s appearance needs to be revised according to the standards and could be more flexible, sustainable, and easy to clean by providing more character to the interior design. |
| C7. ‘Facilities’ | The facilities were the poorest aspects of all the factors. Providing spaces for religious activities, live performances, and snacks again failed to pass the average in the public oncology center. The scores in the private hospital were successful; however, it could be better in terms of providing facilities to make drinks, and even if there was a religious room, the users did not know about it in order to carry out religious activities. |
| C8. Staff | Staff was the section where the most difference occurred between both the hospitals. The private hospital’s oncology unit was nearly in complete agreement and demonstrated the highest standards for the staff; however, on the other hand, the poorest results were obtained for the public oncology center for the staff due to having only nurse stations in the middle of the hospital but without any resting rooms provided for them. |
| Recommended Design Criteria Checklist for Oncology Hospitals Based on the AEDET and ASPECT Toolkit Aspects and Findings in Northern Cyprus |
|---|
| 1 According to functionality |
|
| 2 According to build quality |
|
| 3 According to impact |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tekbiyik Tekin, B.; Dincyurek, O. Exploring the Use of the AEDET Hospital Evaluation Toolkit to Create a Better Healing Environment for Cancer Patients beyond the Global North. Buildings 2023, 13, 2588. https://doi.org/10.3390/buildings13102588
Tekbiyik Tekin B, Dincyurek O. Exploring the Use of the AEDET Hospital Evaluation Toolkit to Create a Better Healing Environment for Cancer Patients beyond the Global North. Buildings. 2023; 13(10):2588. https://doi.org/10.3390/buildings13102588
Chicago/Turabian StyleTekbiyik Tekin, Bedia, and Ozgur Dincyurek. 2023. "Exploring the Use of the AEDET Hospital Evaluation Toolkit to Create a Better Healing Environment for Cancer Patients beyond the Global North" Buildings 13, no. 10: 2588. https://doi.org/10.3390/buildings13102588
APA StyleTekbiyik Tekin, B., & Dincyurek, O. (2023). Exploring the Use of the AEDET Hospital Evaluation Toolkit to Create a Better Healing Environment for Cancer Patients beyond the Global North. Buildings, 13(10), 2588. https://doi.org/10.3390/buildings13102588









