Ventilation Strategies for Mitigation of Infection Disease Transmission in an Indoor Environment: A Case Study in Office
Abstract
:1. Introduction
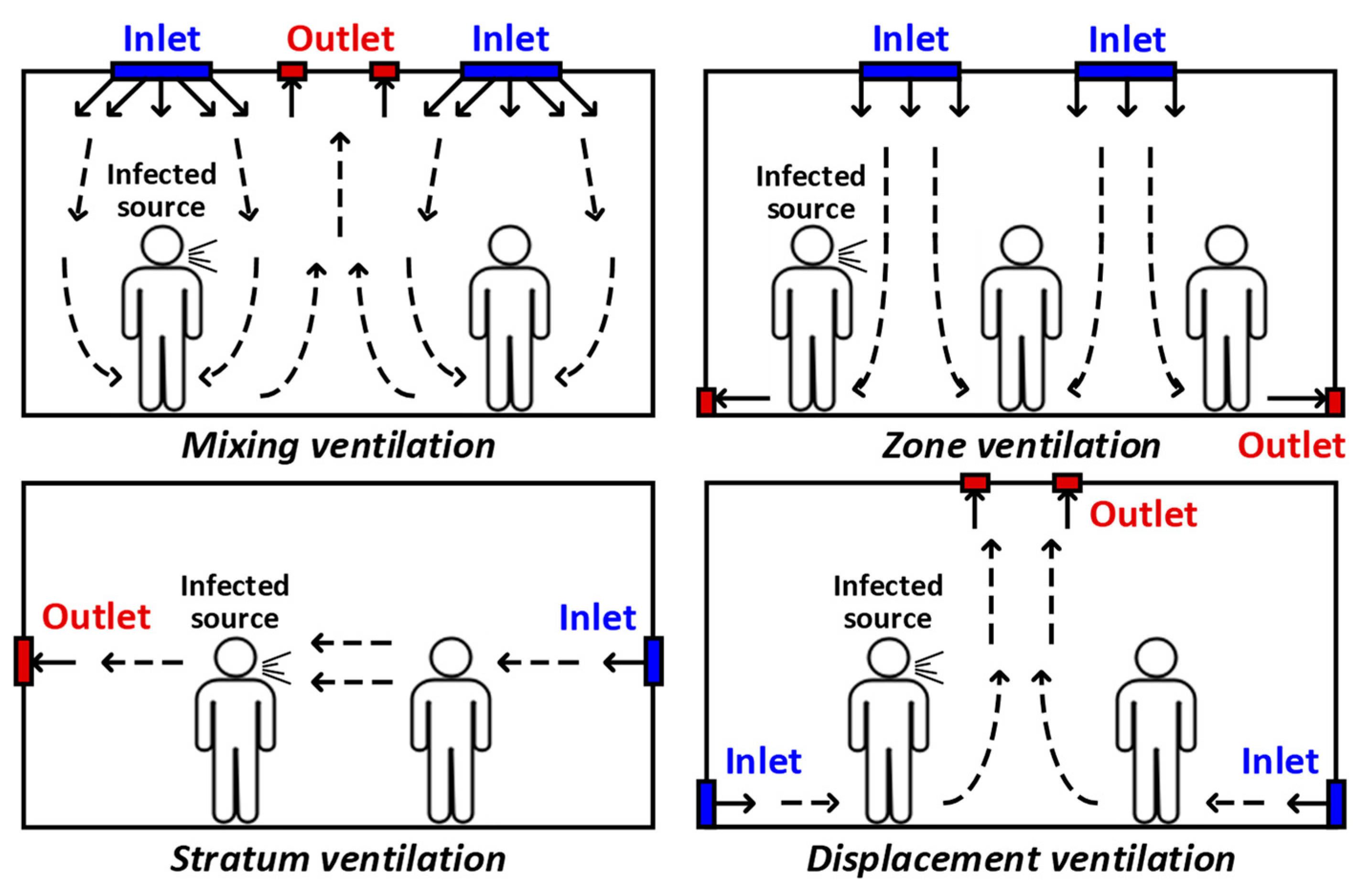
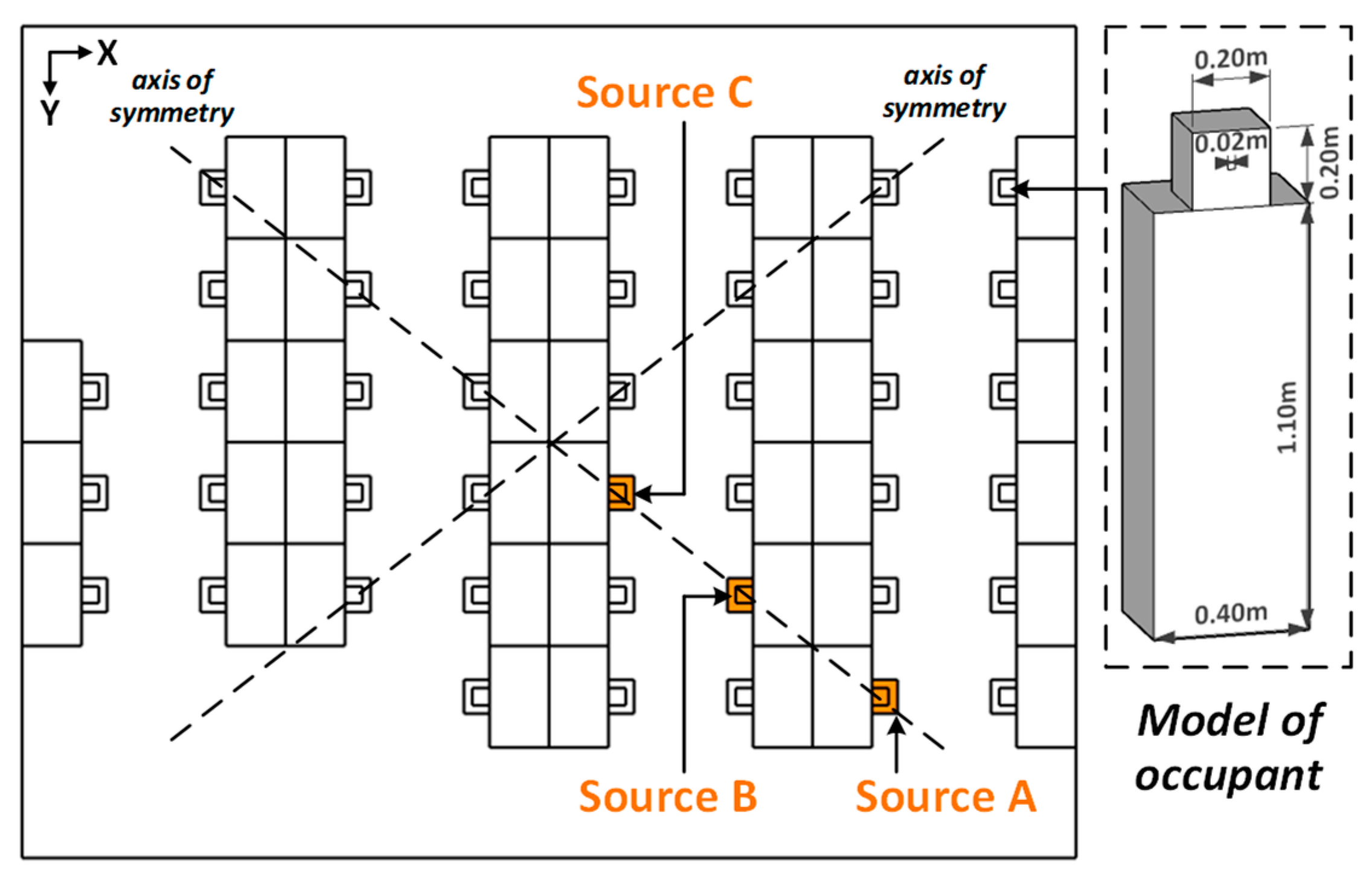
2. Materials and Methods
2.1. Model Information
2.2. Numerical Simulation
2.3. Evaluation Models
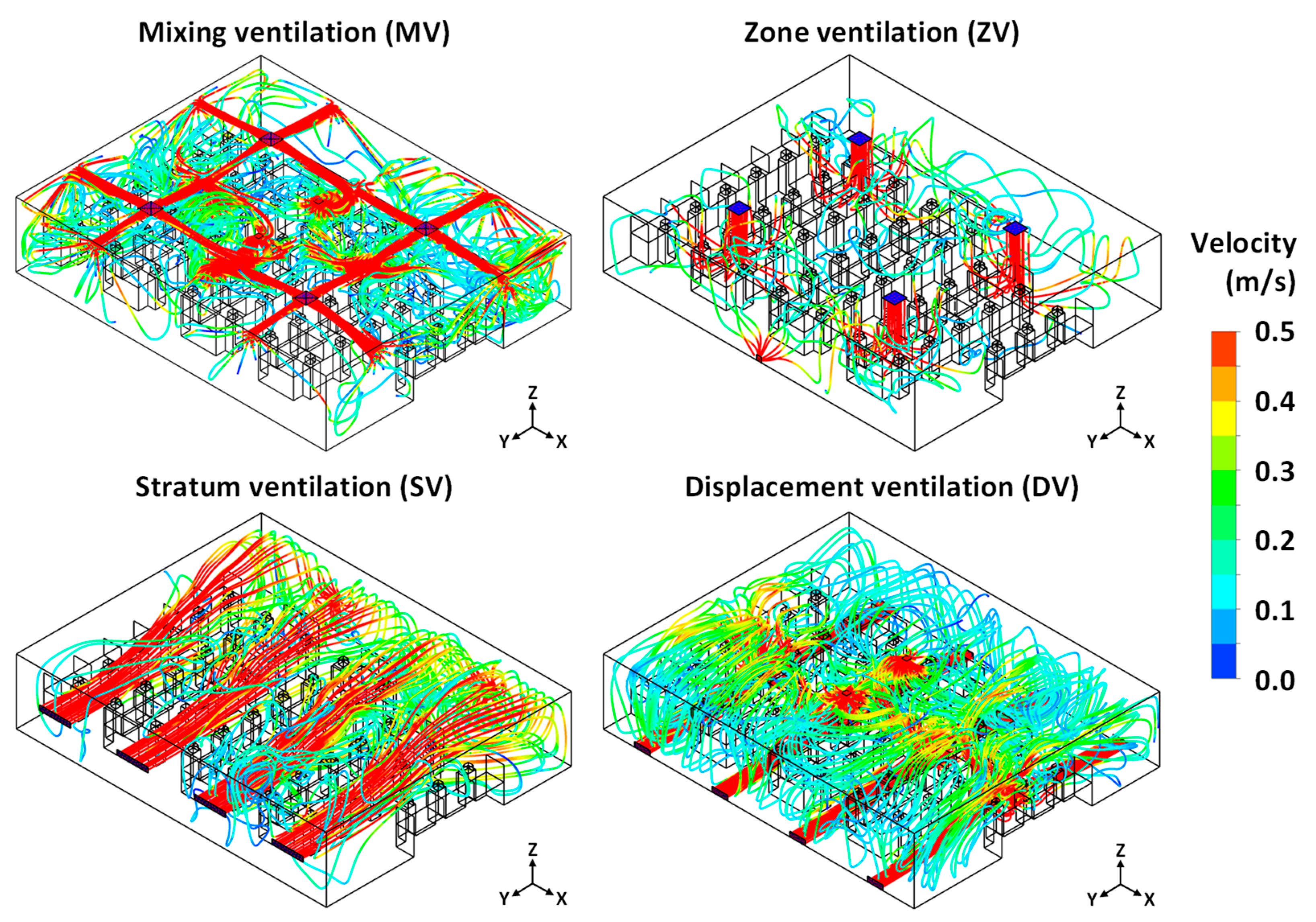
3. Results
3.1. Influence of Ventilation Modes on Ventilation Performance
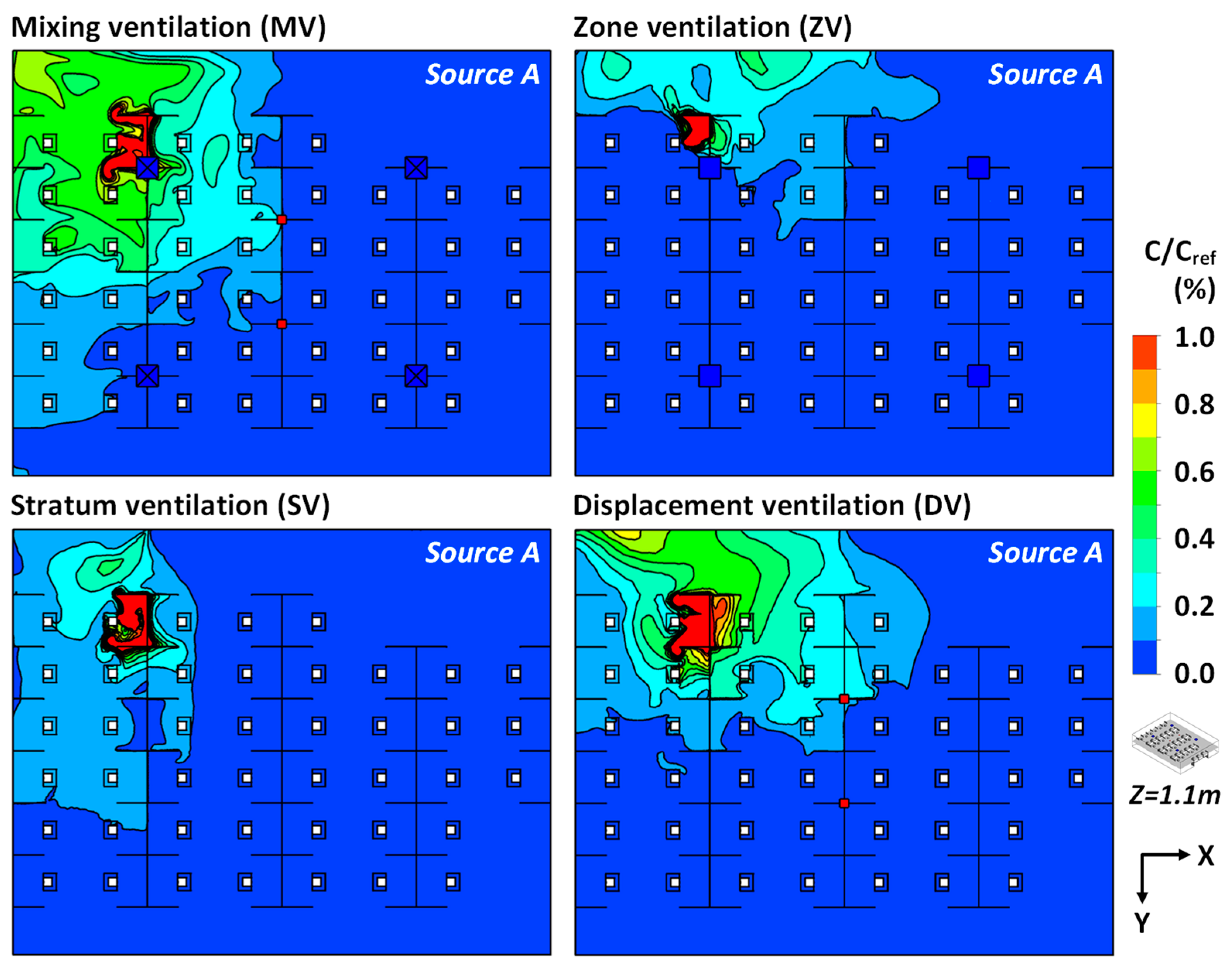
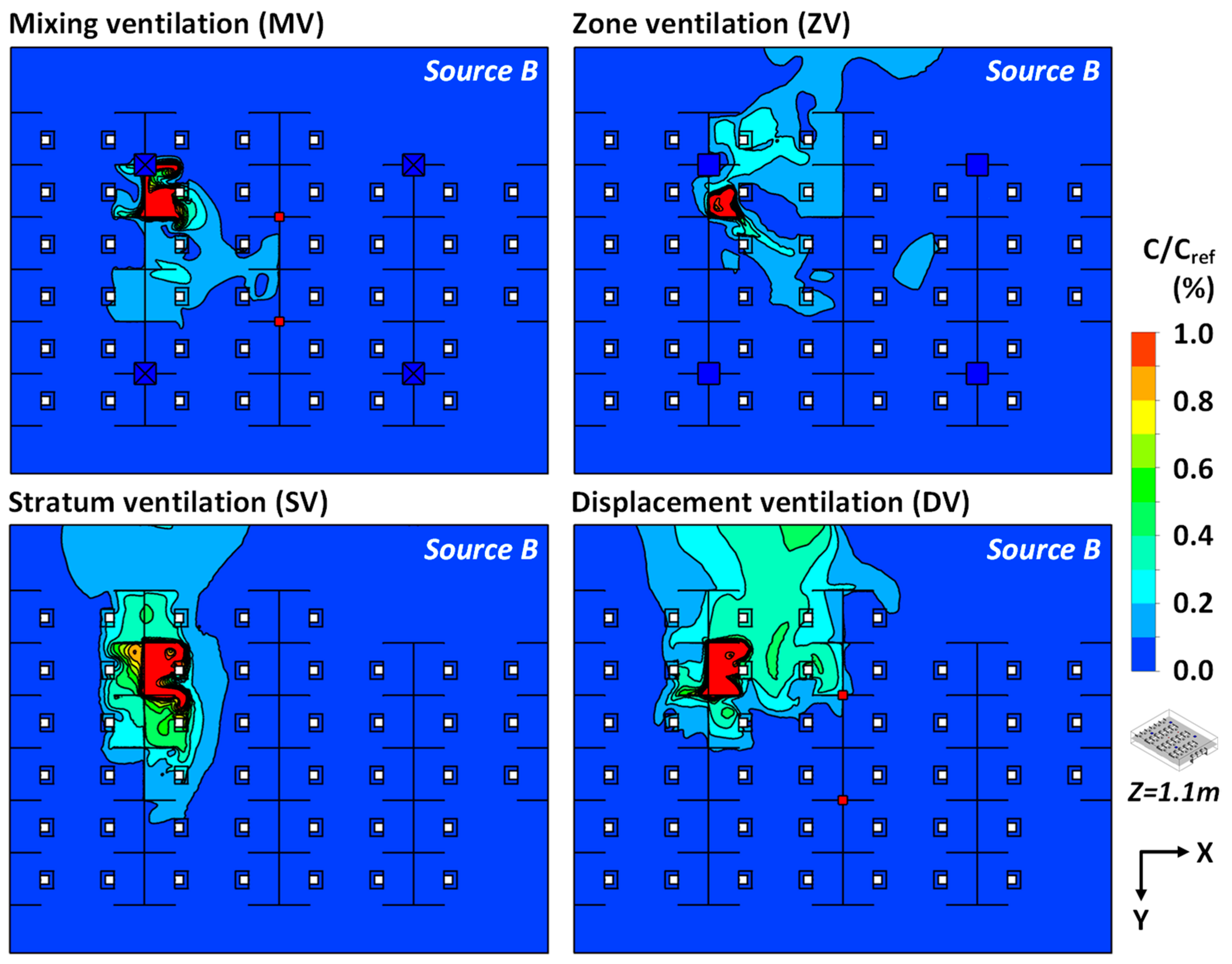
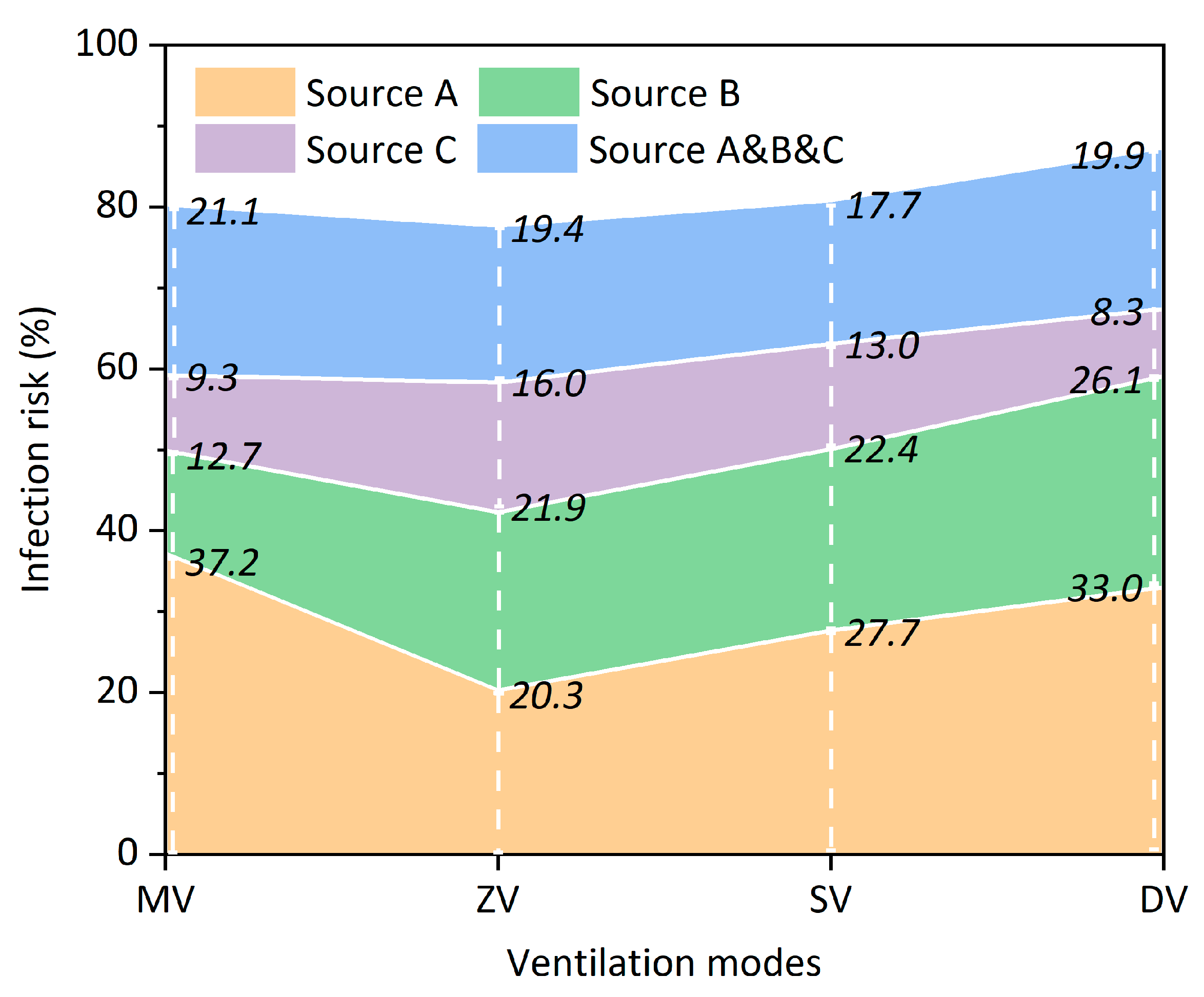
3.2. Influence of Ventilation Modes on Pollutant Diffusion and Infection Risk
4. Discussion
5. Conclusions
- Compared to MV, the ZV, SV and DV increased indoor average velocity by 12.5%, 43.8% and 31.3%, respectively. The SV and ZV could deliver the air from inlets directly to the breathing zone, which is more favorable for improving air distribution performance in an office. The ADPI values for MV, ZV, SV and DV reached above 80%. The SV could provide the ADPI value of 90.5%, which was largely increased by 6.3% as compared to that of MV.
- The ZV, SV and DV could improve the removal efficiency of airborne contaminant at different levels compared to MV, with the average pollutant concentration in the breathing region largely diminished by around 59.3%, 56.1% and 10.3%. The ZV and SV showed a stable and efficient mitigation performance of airborne pollutant transmission in the office.
- Regarding the average infection probability under different scenarios of a single infected source, a minimum infection risk of about 19.4% could be calculated for ZV and SV. The DV would result in a maximum infection risk of about 22.5%, increased by 2.8% compared to MV. Under the scenarios of multiple infected sources, the SV provided the lowest infection risk of 17.7%.
- From the perspective of ventilation performance and infection risk, the SV showed an excellent performance in mitigating the transmission of airborne infectious disease in a real office room. The infection probability in an indoor environment using MV and DV was greatly dependent on the relative distance between the infected occupant and the outlet.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Nomenclature
| COVID-2019 | Coronavirus disease 2019 |
| CDC | Centers for Disease Control and Prevention |
| ASHRAE | American Society of Heating, Refrigerating and Air conditioning Engineer |
| MV | Mixing ventilation |
| ZV | Zone ventilation |
| SV | Stratum ventilation |
| DV | Displacement ventilation |
| CFD | Computational fluid dynamics |
| RANS | Reynolds-averaged Navier–Stokes |
| Solved variables (i.e., velocity and temperature) | |
| Convection term | |
| Air density | |
| Average airflow velocity | |
| Diffusion term | |
| UDS | User-defined scalar |
| The reference value of pollutant concentration | |
| FVM | Finite volume method |
| EDT | Effective draught temperature |
| Value of EDT | |
| Local air temperature | |
| Average air temperature | |
| Local airflow velocity | |
| ADPI | Air Diffusion Performance Index |
| Infection possibility | |
| Inhalation rate of the exposed occupant | |
| T | Total exposure time |
| Pollutant concentration (#/m3) over time t |
References
- Salamone, F.; Barozzi, B.; Bellazzi, A.; Belussi, L.; Danza, L.; Devitofrancesco, A.; Ghellere, M.; Meroni, I.; Scamoni, F.; Scrosati, C. Working from home in italy during covid-19 lockdown: A survey to assess the indoor environmental quality and productivity. Buildings 2021, 11, 660. [Google Scholar] [CrossRef]
- WHO. Coronavirus Disease (COVID-19): How Is It Transmitted? Available online: www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-how-is-it-transmitted (accessed on 23 December 2021).
- Morawska, L.; Tang, J.L.W.; Bahnfleth, W.; Bluyssen, P.M.; Boerstra, A.; Buonanno, G.; Cao, J.J.; Dancer, S.; Floto, A.; Franchimon, F.; et al. How can airborne transmission of COVID-19 indoors be minimised? Environ. Int. 2020, 142, 105832. [Google Scholar] [CrossRef] [PubMed]
- Bak, A.; Mugglestone, M.A.; Ratnaraja, N.V.; Wilson, J.A.; Rivett, L.; Stoneham, S.M.; Bostock, J.; Moses, S.E.; Price, J.R.; Weinbren, M.; et al. SARS-CoV-2 routes of transmission and recommendations for preventing acquisition: Joint british infection association (bia), healthcare infection society (his), infection prevention society (ips) and royal college of pathologists (rcpath) guidance. J. Hosp. Infect. 2021, 114, 79–103. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.N.; Liu, W.B.; Luo, X.L.; Huang, X.Y.; Nielsen, P.V. Prediction and control of aerosol transmission of SARS-CoV-2 in ventilated context: From source to receptor. Sustain. Cities Soc. 2022, 76, 103416. [Google Scholar] [CrossRef]
- Wan, J.Y.; Wei, J.J.; Lin, Y.T.; Zhang, T.F. Numerical investigation of bioaerosol transport in a compact lavatory. Buildings 2021, 11, 526. [Google Scholar] [CrossRef]
- Law, R.C.K.; Lai, J.H.K.; Edwards, D.J.; Hou, H.Y. COVID-19: Research directions for non-clinical aerosol-generating facilities in the built environment. Buildings 2021, 11, 282. [Google Scholar] [CrossRef]
- Ren, C.; Xi, C.; Wang, J.Q.; Feng, Z.B.; Nasiri, F.; Cao, S.J.; Haghighat, F. Mitigating COVID-19 infection disease transmission in indoor environment using physical barriers. Sustain. Cities Soc. 2021, 74, 103175. [Google Scholar] [CrossRef]
- Feng, Z.B.; Cao, S.J.; Haghighat, F. Removal of SARS-CoV-2 using uv+filter in built environment. Sustain. Cities Soc. 2021, 74, 103226. [Google Scholar] [CrossRef]
- Feng, Z.B.; Cao, S.J. A newly developed electrostatic enhanced pleated air filters towards the improvement of energy and filtration efficiency. Sustain. Cities Soc. 2019, 49, 101569. [Google Scholar] [CrossRef]
- Ding, J.W.; Yu, C.W.; Cao, S.J. Hvac systems for environmental control to minimize the COVID-19 infection. Indoor Built Environ. 2020, 29, 1195–1201. [Google Scholar] [CrossRef]
- Xu, C.W.; Luo, X.L.; Yu, C.; Cao, S.J. The 2019-ncov epidemic control strategies and future challenges of building healthy smart cities. Indoor Built Environ. 2020, 29, 639–644. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Leung, G.M.; Tang, J.W.; Yang, X.; Chao, C.Y.H.; Lin, J.Z.; Lu, J.W.; Nielsen, P.V.; Niu, J.; Qian, H.; et al. Role of ventilation in airborne transmission of infectious agents in the built environment—A multidisciplinary systematic review. Indoor Air 2007, 17, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, K.; Chowell, G. Transmission potential of the novel coronavirus (COVID-19) onboard the diamond princess cruises ship, 2020. Infect. Dis. Model. 2020, 5, 264–270. [Google Scholar] [CrossRef]
- CDC. Ventilation in Buildings. Available online: www.cdc.gov/coronavirus/2019-ncov/community/ventilation.html (accessed on 4 May 2021).
- ASHRAE. Ashrae Position Document on Infectious Aerosols. Available online: www.ashrae.org/file%20library/about/position%20documents/pd_infectiousaerosols_2020.pdf (accessed on 14 April 2020).
- REHVA. Rehva COVID-19 Guidance. Available online: http://www.rehva.eu/fileadmin/user_upload/REHVA_COVID-19_guidance_document_ver2_20200403_1.pdf (accessed on 3 April 2020).
- Cao, S.J.; Ren, C. Ventilation control strategy using low-dimensional linear ventilation models and artificial neural network. Build. Environ. 2018, 144, 316–333. [Google Scholar] [CrossRef]
- Dai, H.; Zhao, B. Association of the infection probability of COVID-19 with ventilation rates in confined spaces. Build. Simul-China 2020, 13, 1321–1327. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.J.; Zhai, Z.Q. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain. Cities Soc. 2020, 62, 102390. [Google Scholar] [CrossRef]
- Cao, S.J.; Yu, C.W.; Luo, X.L. New and emerging building ventilation technologies. Indoor Built Environ. 2020, 29, 483–484. [Google Scholar] [CrossRef] [Green Version]
- Motamedi, H.; Shirzadi, M.; Tominaga, Y.; Mirzaei, P.A. Cfd modeling of airborne pathogen transmission of COVID-19 in confined spaces under different ventilation strategies. Sustain. Cities Soc. 2022, 76, 103397. [Google Scholar] [CrossRef]
- Ren, C.; Cao, S.J.; Haghighat, F. A practical approach for preventing dispersion of infection disease in naturally ventilated room. J. Build. Eng. 2022, 48, 103921. [Google Scholar] [CrossRef]
- Dincer, D.; Gocer, O. Quarantine hotels: The adaptation of hotels for quarantine use in australia. Buildings 2021, 11, 617. [Google Scholar] [CrossRef]
- Wang, J.Q.; Huang, J.J.; Feng, Z.B.; Cao, S.J.; Haghighat, F. Occupant-density-detection based energy efficient ventilation system: Prevention of infection transmission. Energy Build. 2021, 240, 110883. [Google Scholar] [CrossRef]
- Jia, L.R.; Han, J.; Chen, X.; Li, Q.Y.; Lee, C.C.; Fung, Y.H. Interaction between thermal comfort, indoor air quality and ventilation energy consumption of educational buildings: A comprehensive review. Buildings 2021, 11, 591. [Google Scholar] [CrossRef]
- Hawendi, S.; Gao, S. Impact of windward inlet-opening positions on fluctuation characteristics of wind-driven natural cross ventilation in an isolated house using les. Int. J. Vent. 2018, 17, 93–119. [Google Scholar] [CrossRef]
- Park, S.; Choi, Y.; Song, D.; Kim, E.K. Natural ventilation strategy and related issues to prevent coronavirus disease 2019 (covid-19) airborne transmission in a school building. Sci. Total Environ. 2021, 789, 147764. [Google Scholar] [CrossRef]
- Qi, J.; Wei, C.Y. Performance evaluation of climate-adaptive natural ventilation design: A case study of semi-open public cultural building. Indoor Built Environ. 2021, 30, 1714–1724. [Google Scholar] [CrossRef]
- Li, C.Y.; Tang, H.D. Study on ventilation rates and assessment of infection risks of covid-19 in an outpatient building. J. Build. Eng. 2021, 42, 103090. [Google Scholar] [CrossRef]
- Cao, S.J.; Feng, Z.B.; Wang, J.Q.; Ren, C.; Zhu, H.C.; Chen, G.; Mei, J.T. Ergonomics-oriented operation, maintenance and control of indoor air environment for public buildings. Chin. Sci. Bull. 2020, 67, 1–13. [Google Scholar] [CrossRef]
- Li, Y.G.; Qian, H.; Hang, J.; Chen, X.G.; Cheng, P.; Ling, H.; Wang, S.Q.; Liang, P.; Li, J.S.; Xiao, S.L.; et al. Probable airborne transmission of SARS-CoV-2 in a poorly ventilated restaurant. Build. Environ. 2021, 196, 107788. [Google Scholar] [CrossRef]
- Cao, G.Y.; Awbi, H.; Yao, R.M.; Fan, Y.Q.; Siren, K.; Kosonen, R.; Zhang, J.S. A review of the performance of different ventilation and airflow distribution systems in buildings. Build. Environ. 2014, 73, 171–186. [Google Scholar] [CrossRef]
- Tomasi, R.; Krajcik, M.; Simone, A.; Olesen, B.W. Experimental evaluation of air distribution in mechanically ventilated residential rooms: Thermal comfort and ventilation effectiveness. Energy Build. 2013, 60, 28–37. [Google Scholar] [CrossRef]
- Kang, Z.Q.; Zhang, Y.X.; Fan, H.B.; Feng, G.H. Numerical simulation of coughed droplets in the air-conditioning room. Procedia Eng. 2015, 121, 114–121. [Google Scholar] [CrossRef] [Green Version]
- Tian, X.; Lin, Z. Dynamic modelling of air temperature in breathing zone with stratum ventilation using a pulsating air supply. Build. Environ. 2021, 210, 108697. [Google Scholar] [CrossRef]
- Tian, X.; Li, B.Z.; Ma, Y.X.; Liu, D.; Li, Y.C.; Cheng, Y. Experimental study of local thermal comfort and ventilation performance for mixing, displacement and stratum ventilation in an office. Sustain. Cities Soc. 2019, 50, 101630. [Google Scholar] [CrossRef]
- Li, H.; Xi, C.; Kong, X.F.; Lin, Z.; Wang, L. A comparative experimental investigation on radiant floor heating system and stratum ventilation. Sustain. Cities Soc. 2020, 52, 101823. [Google Scholar] [CrossRef]
- Lu, Y.L.; Oladokun, M.; Lin, Z. Reducing the exposure risk in hospital wards by applying stratum ventilation system. Build. Environ. 2020, 183, 107204. [Google Scholar] [CrossRef]
- Cao, G.; Nielsen, P.V.; Jensen, R.L.; Heiselberg, P.; Liu, L.; Heikkinen, J. Protected zone ventilation and reduced personal exposure to airborne cross-infection. Indoor Air 2015, 25, 307–319. [Google Scholar] [CrossRef]
- Cao, G.Y.; Siren, K.; Kilpelainen, S. Modelling and experimental study of performance of the protected occupied zone ventilation. Energ Build. 2014, 68, 515–531. [Google Scholar] [CrossRef]
- Cheng, Y.; Lin, Z. Experimental investigation into the interaction between the human body and room airflow and its effect on thermal comfort under stratum ventilation. Indoor Air 2016, 26, 274–285. [Google Scholar] [CrossRef]
- Li, H.Y.; Leong, F.Y.; Xu, G.; Kang, C.W.; Lim, K.H.; Tan, B.H.; Loo, C.M. Airborne dispersion of droplets during coughing: A physical model of viral transmission. Sci. Rep. 2021, 11, 4617. [Google Scholar] [CrossRef]
- Liu, S.C.; Novoselac, A. Air diffusion performance index (adpi) of diffusers for heating mode. Build. Environ. 2015, 87, 215–223. [Google Scholar] [CrossRef]
- Buonanno, G.; Stabile, L.; Morawska, L. Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ. Int. 2020, 141, 105794. [Google Scholar] [CrossRef]
- Ren, C.; Cao, S.J. Development and application of linear ventilation and temperature models for indoor environmental prediction and hvac systems control. Sustain. Cities Soc. 2019, 51, 101673. [Google Scholar] [CrossRef]
- Sha, H.H.; Qi, D.H. A review of high-rise ventilation for energy efficiency and safety. Sustain. Cities Soc. 2020, 54, 101971. [Google Scholar] [CrossRef]
- Georgescu, M.R.; Meslem, A.; Nastase, I.; Bode, F. Personalized ventilation solutions for reducing co2 levels in the crew quarters of the international space station. Build. Environ. 2021, 204, 108150. [Google Scholar] [CrossRef]
- Afroz, Z.; Higgins, G.; Shafiullah, G.M.; Urmee, T. Evaluation of real-life demand-controlled ventilation from the perception of indoor air quality with probable implications. Energy Build. 2020, 219, 110018. [Google Scholar] [CrossRef]
- Ren, C.; Cao, S.J. Implementation and visualization of artificial intelligent ventilation control system using fast prediction models and limited monitoring data. Sustain. Cities Soc. 2020, 52, 101860. [Google Scholar] [CrossRef]
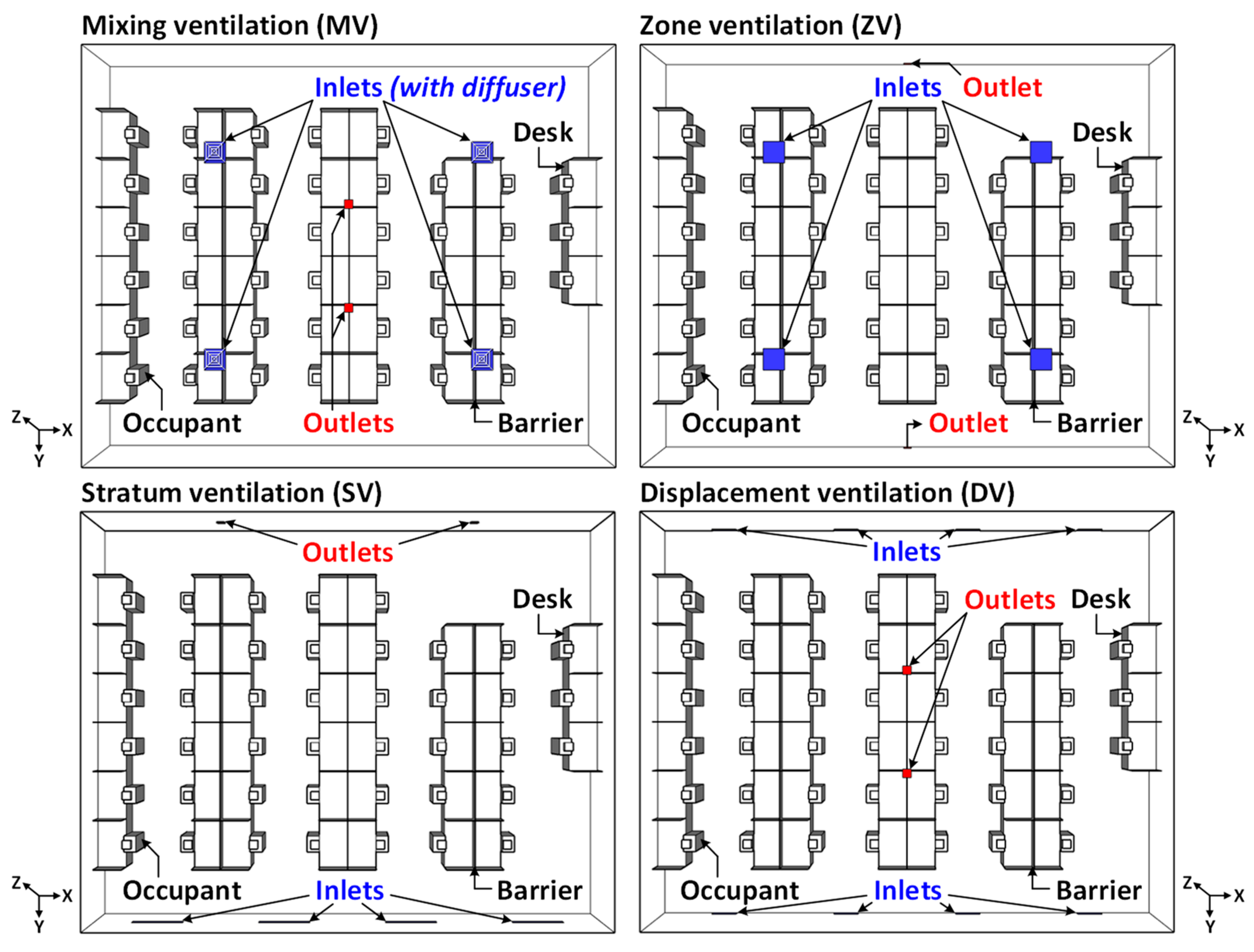


| Ventilation Modes | Mixing Ventilation (MV) | Zone Ventilation (ZV) | Stratum Ventilation (SV) | Displacement Ventilation (DV) |
|---|---|---|---|---|
| inlet size (m) | 0.5 × 0.5 (with diffuser) | 0.5 × 0.5 | 1.25 × 0.2 | 0.625 × 0.2 |
| number of inlets | 4 | 4 | 4 | 8 |
| supply air velocity (m/s) | 1.73 | 1.73 | 1.73 | 1.73 |
| outlet size (m) | 0.2 × 0.2 | 0.2 × 0.2 | 0.2 × 0.2 | 0.2 × 0.2 |
| number of outlets | 2 | 2 | 2 | 2 |
| Boundary | Type | Conditions |
|---|---|---|
| Inlet | Velocity-inlet | Supply air velocity: 1.73 m/s Supply air temperature: 25 °C |
| Outlet | Outflow | |
| Wall | Non-slip wall | Wall temperature: 15 °C |
| Occupant | Non-slip wall | Body temperature: 24 °C Head temperature: 34 °C Mouth temperature: 36 °C Average airflow velocity of coughing: 13 m/s downwards at 27.5° Average breathing rate: 0.7 m/s Airflow temperature for coughing and breathing: 36 °C |
| Physical barrier and desk | Non-slip wall |
| Case No. | Ventilation Mode | Infected Source | Note |
|---|---|---|---|
| 1 | MV | None | Evaluation of ventilation performance |
| 2 | ZV | None | |
| 3 | SV | None | |
| 4 | DV | None | |
| 5–7 | MV | A, B and C | Evaluation of infection risk |
| 8–10 | ZV | A, B and C | |
| 11–13 | SV | A, B and C | |
| 14–16 | DV | A, B and C |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ren, C.; Zhu, H.-C.; Cao, S.-J. Ventilation Strategies for Mitigation of Infection Disease Transmission in an Indoor Environment: A Case Study in Office. Buildings 2022, 12, 180. https://doi.org/10.3390/buildings12020180
Ren C, Zhu H-C, Cao S-J. Ventilation Strategies for Mitigation of Infection Disease Transmission in an Indoor Environment: A Case Study in Office. Buildings. 2022; 12(2):180. https://doi.org/10.3390/buildings12020180
Chicago/Turabian StyleRen, Chen, Hao-Cheng Zhu, and Shi-Jie Cao. 2022. "Ventilation Strategies for Mitigation of Infection Disease Transmission in an Indoor Environment: A Case Study in Office" Buildings 12, no. 2: 180. https://doi.org/10.3390/buildings12020180
APA StyleRen, C., Zhu, H.-C., & Cao, S.-J. (2022). Ventilation Strategies for Mitigation of Infection Disease Transmission in an Indoor Environment: A Case Study in Office. Buildings, 12(2), 180. https://doi.org/10.3390/buildings12020180







