Implant Treatment in Atrophic Maxilla by Titanium Hybrid-Plates: A Finite Element Study to Evaluate the Biomechanical Behavior of Plates
Abstract
:1. Introduction
2. Materials and Methods
2.1. Description of the Protocol
- Reduced bone volume in the upper and lower jaws such as stage D or E according to the Lekholm and Zarb classification of bone quality.
- Severely reduced vertical bone height over the trajectory of the mandibular canal in the lower jaw where there is insufficient vertical bone height to place conventional implants.
- Where short implants are not deemed justified, or in cases where bone reconstruction is not feasible.
- In very sharp dentoalveolar ridges.
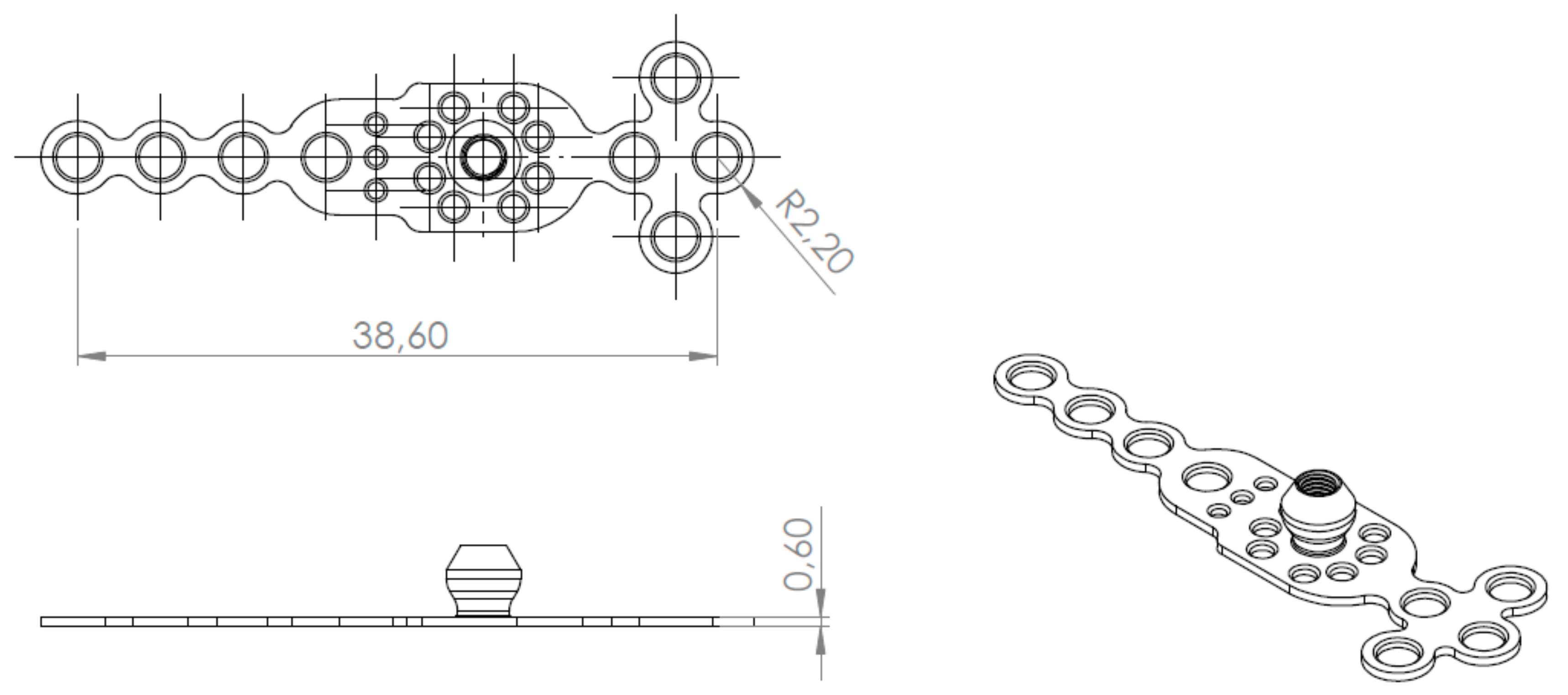
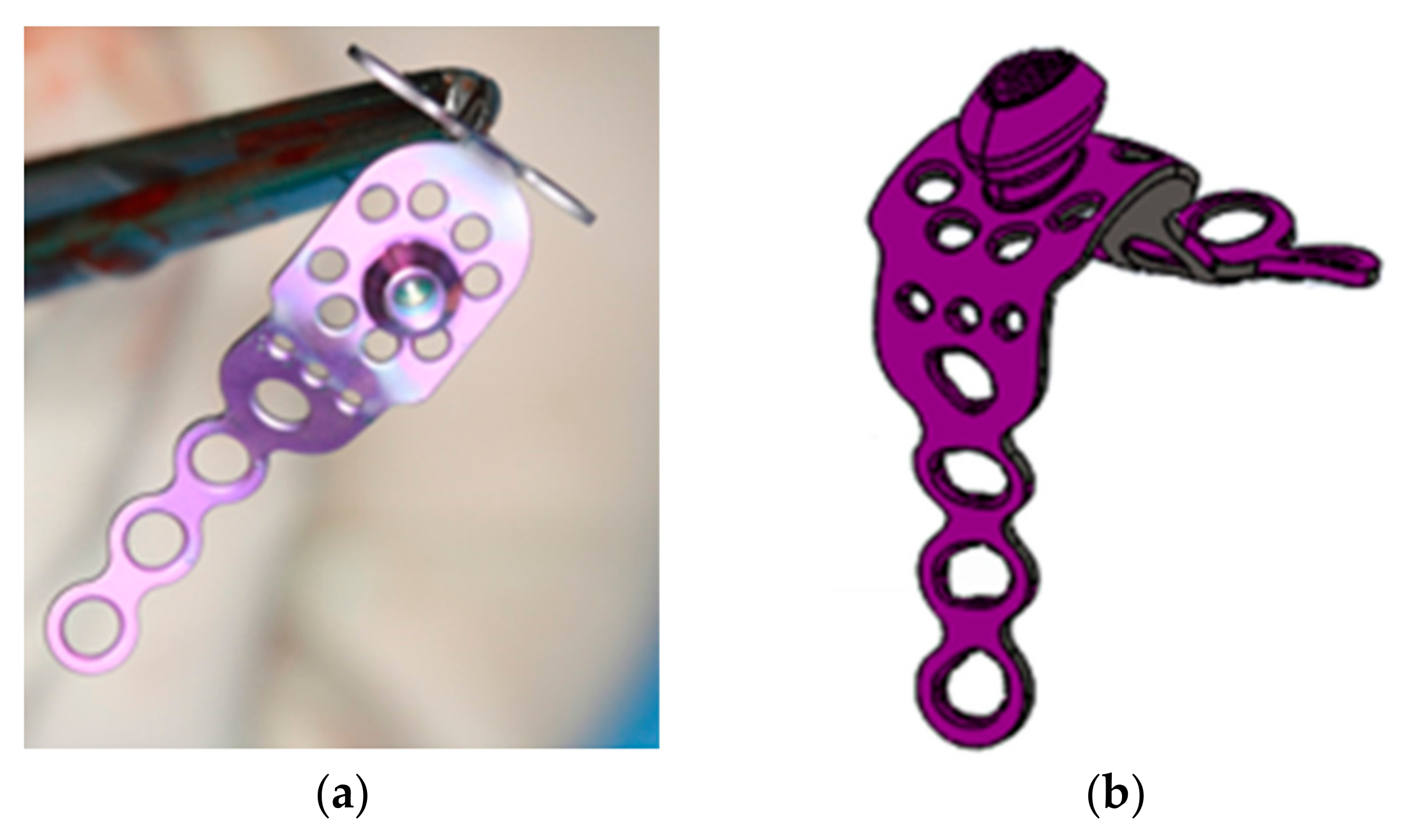
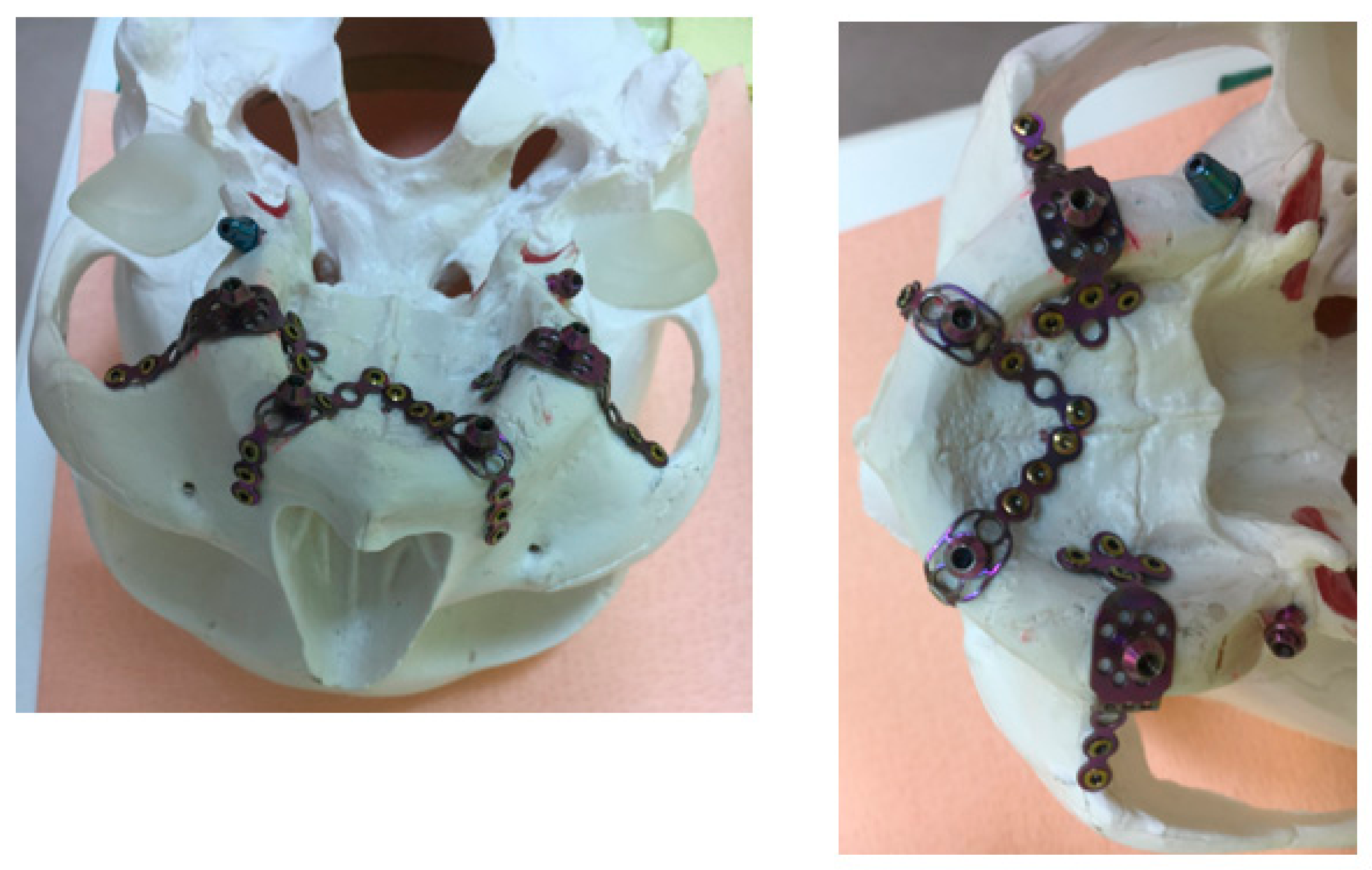
2.2. Plates
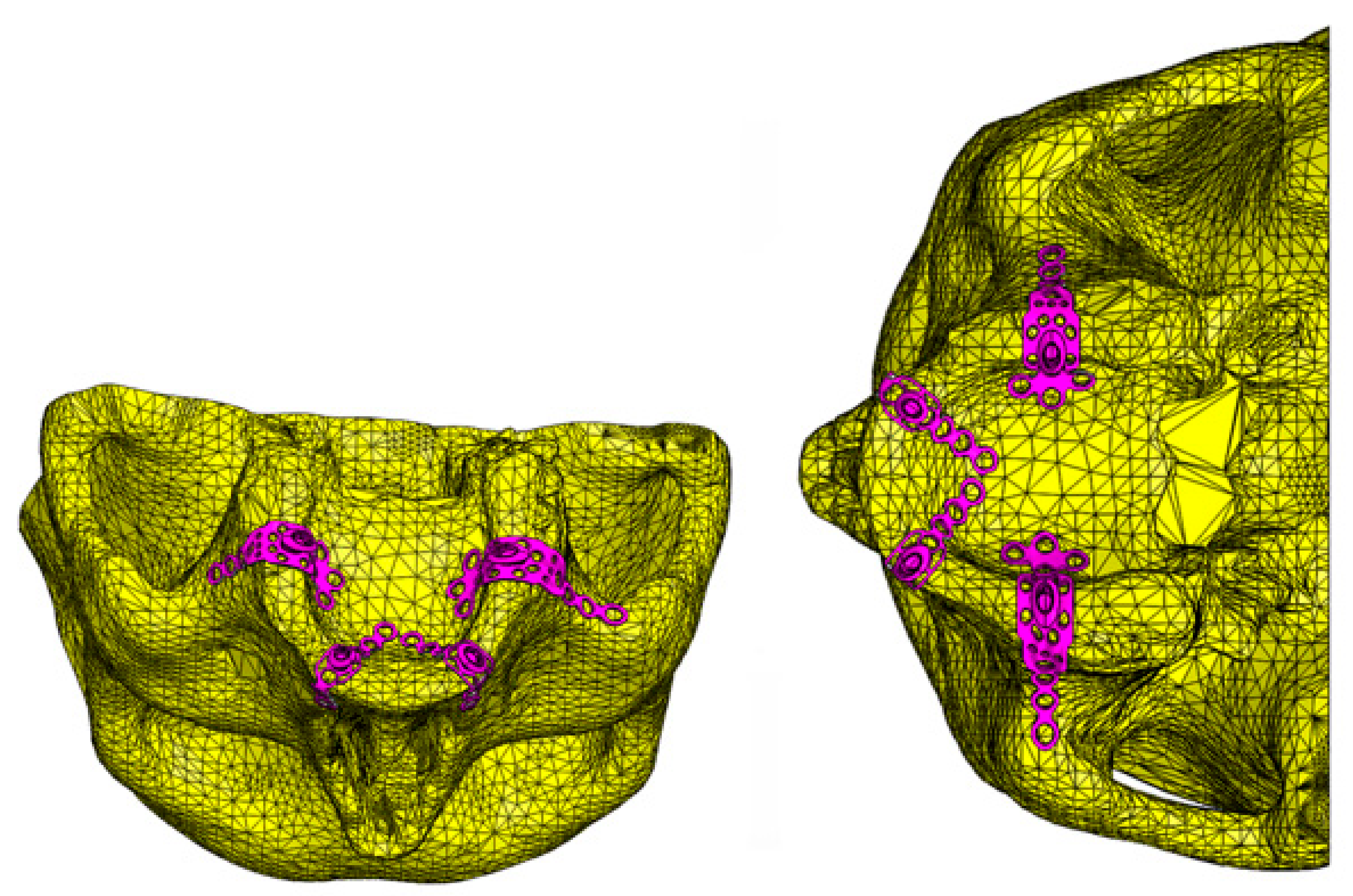
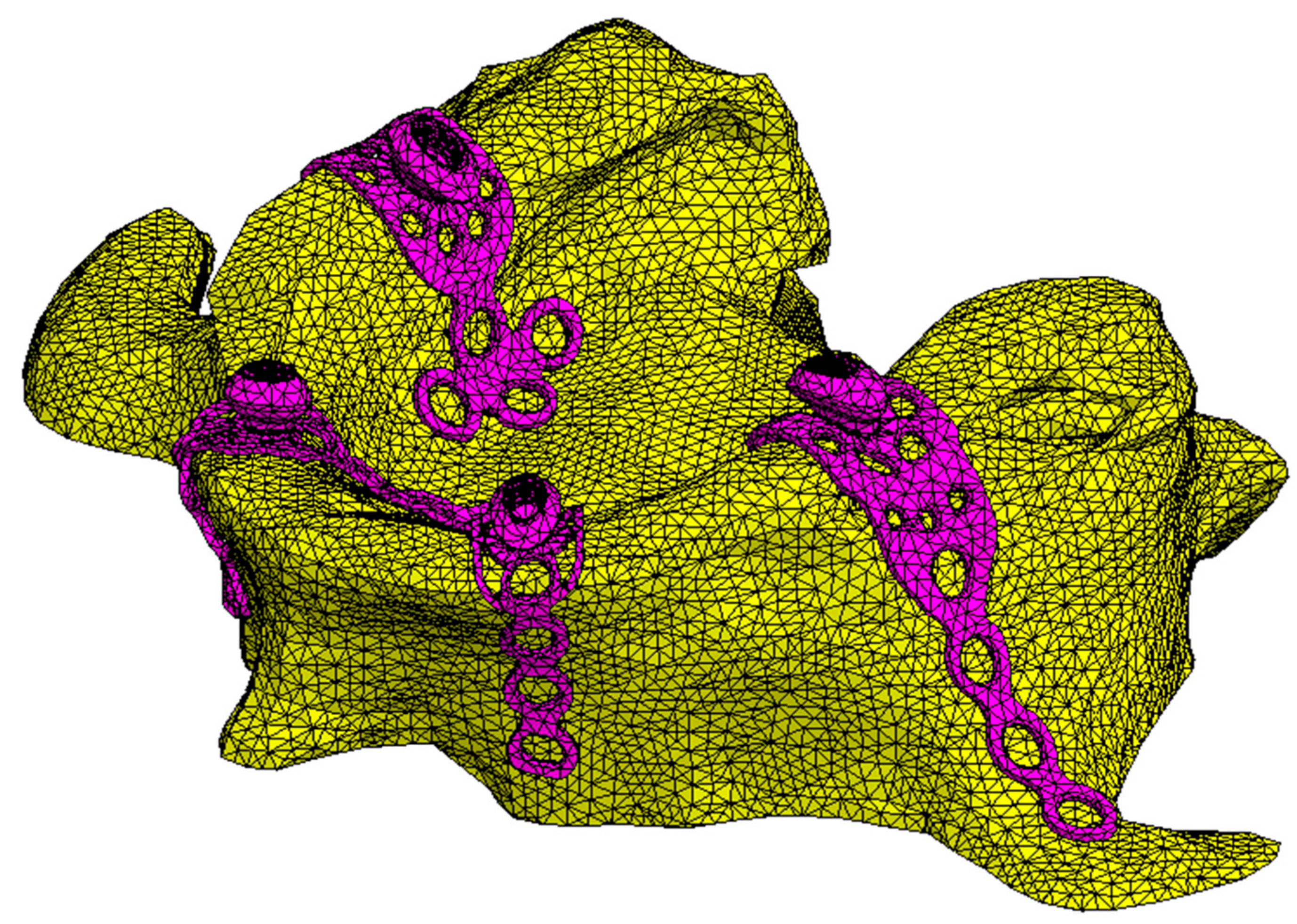
2.3. Finite Element Reconstruction
2.4. Material Properties
2.5. Meshing
2.6. Boundary Conditions and Loading Configuration
2.7. Probabilistic Fatigue Model
- (1)
- Damage cycles (DC) are repetitive and of constant severity.
- (2)
- The levels of damage a component will go through until final failure are discrete (1, 2, …, j, …, b), and failure occurs at the last level of damage (b). This hypothesis merely discretizes the total life of the component in b levels.
- (3)
- The accumulation of damage that occurs in each DC depends only on the DC itself and the level of damage of the component at the start of said DC.
- (4)
- The level of damage in each DC can only be increased from the occupied level at the beginning of said DC to the next immediate level.
3. Results
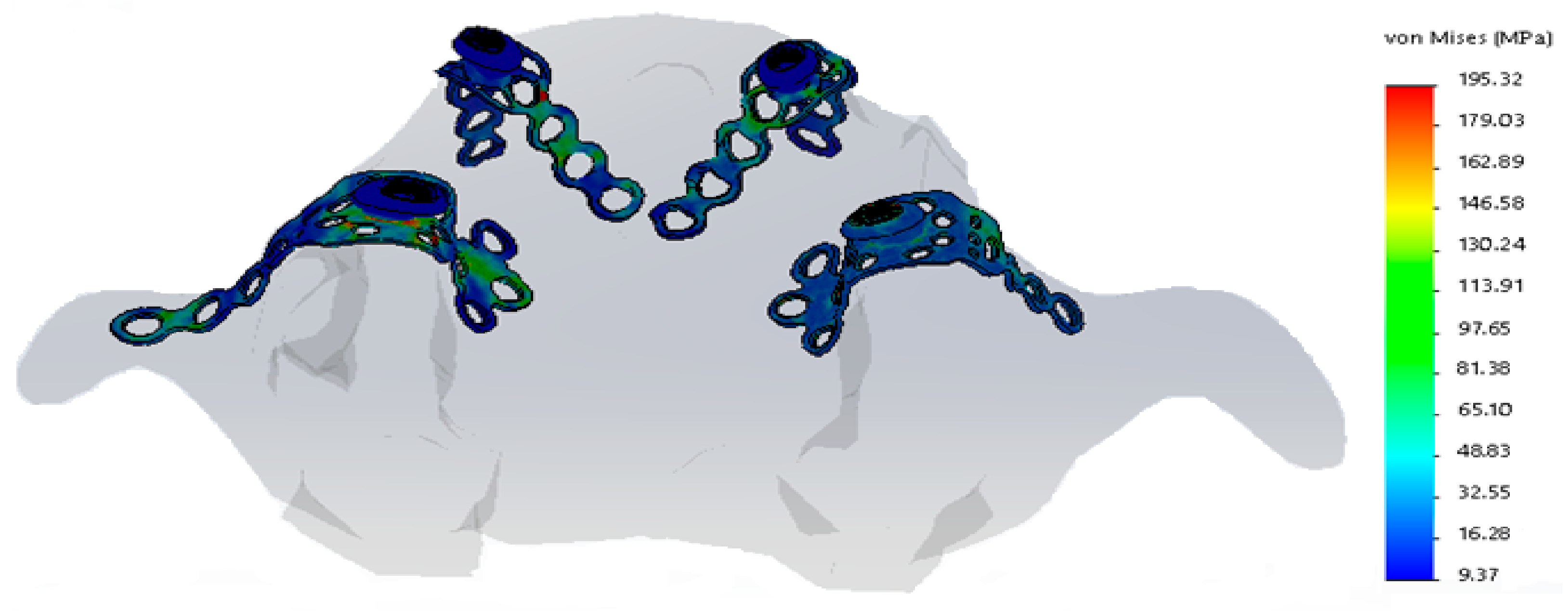
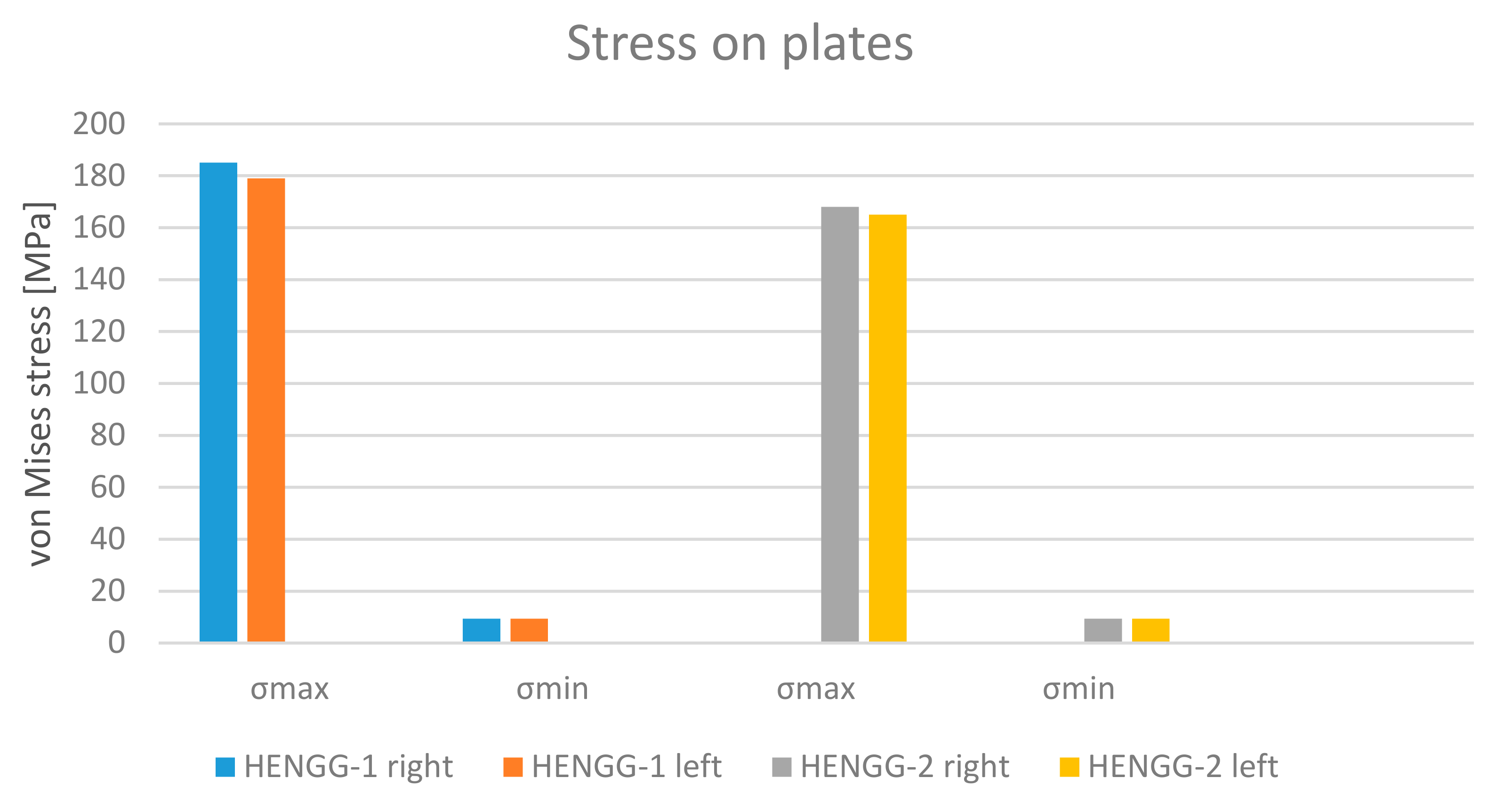
3.1. Plates
3.2. Maxilla
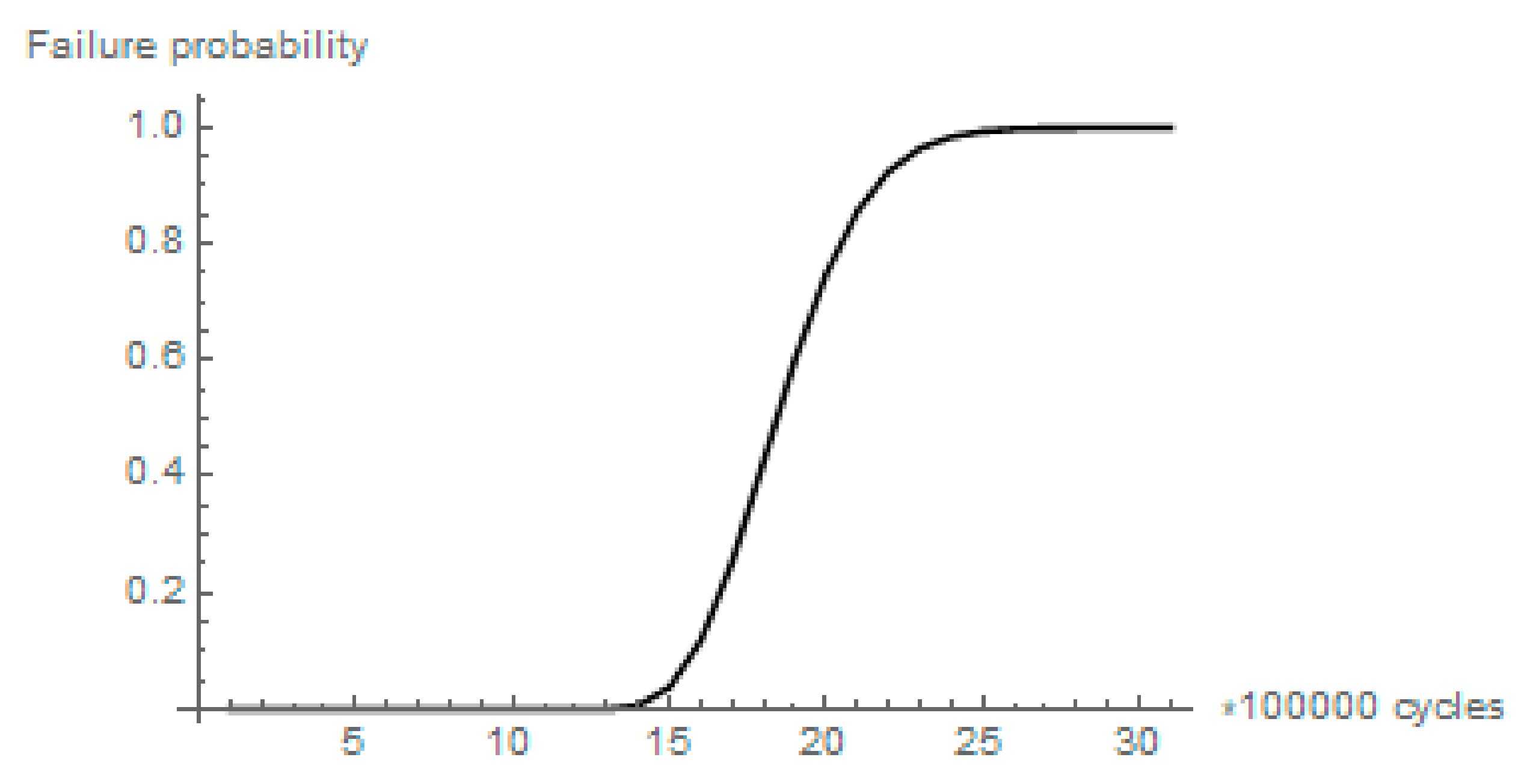
3.3. Long-Term Behavior
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Van der Mark, E.L.; Bierenbroodspot, F.; Baas, E.M.; de Lange, J. Reconstruction of an atrophic maxilla: Comparison of two methods. Br. J. Oral Maxillofac. Surg. 2011, 49, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Karthigeyan, S.; Deivanai, M.; Kumar, A. Implant Rehabilitation For Atrophic Maxilla: A Review. J. Indian Prosthodont. Soc. 2014, 13, 196–207. [Google Scholar] [CrossRef] [PubMed]
- Spencer, K. Implant based rehabilitation options for the atrophic edentulous jaw. Aust. Dent. J. 2018, 63, S100–S107. [Google Scholar] [CrossRef] [PubMed]
- Cawood, J.I.; Howell, R.A. A classification of the edentulous jaws. Int. J. Oral Maxillofac. Surg. 1988, 17, 232–236. [Google Scholar] [CrossRef]
- Chiapasco, M.; Zaniboni, M. Methods to Treat the Edentulous Posterior Maxilla: Implants With Sinus Grafting. J. Oral Maxillofac. Surg. 2009, 67, 867–871. [Google Scholar] [CrossRef] [PubMed]
- Cucchi, A.; Vignudelli, E.; Franco, S.; Corinaldesi, G. Minimally Invasive Approach Based on Pterygoid and Short Implants for Rehabilitation of an Extremely Atrophic Maxilla. Implant Dent. 2017, 26, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Aparicio, C.; Manresa, C.; Francisco, K.; Claros, P.; Alández, J.; González-Martín, O.; Albrektsson, T. Zygomatic implants: Indications, techniques and outcomes, and the Zygomatic Success Code. Periodontol. 2000 2014, 66, 41–58. [Google Scholar] [CrossRef] [PubMed]
- Gultekin, B.A.; Cansiz, E.; Borahan, M.O. Clinical and 3-Dimensional Radiographic Evaluation of Autogenous Iliac Block Bone Grafting and Guided Bone Regeneration in Patients With Atrophic Maxilla. J. Oral Maxillofac. Surg. 2017, 75, 709–722. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, T.; Nakamura, S.; Hino, S.; Norio, H.; Shimoyama, T. Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: A case report. Int. J. Implant Dent. 2016, 2, 16. [Google Scholar] [CrossRef] [PubMed]
- Alqutaibi, A.Y.; Altaib, F. Short dental implant is considered as a reliable treatment option for patients with atrophic posterior maxilla. J. Evid. Based Dent. Pract. 2016, 16, 173–175. [Google Scholar] [CrossRef] [PubMed]
- Candel, E.; Peñarrocha, D.; Peñarrocha, M. Rehabilitation of the Atrophic Posterior Maxilla With Pterygoid Implants: A Review. J. Oral Implantol. 2012, 38, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Orive, G.; Aguirre, J.J.; Andía, I. Five-Year Clinical Evaluation of Short Dental Implants Placed in Posterior Areas: A Retrospective Study. J. Periodontol. 2008, 79, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Piñas, L.; Begoña, L.; Orive, G. Long-term retrospective evaluation of short implants in the posterior areas: Clinical results after 10–12 years. J. Clin. Periodontol. 2014, 41, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Scortecci, G.; Misch, C.; Benner, K. Implants and Restorative Dentistry; Martin Dunitz: London, UK, 2001. [Google Scholar]
- Wu, C.; Lin, Y.; Liu, Y.; Lin, C. Biomechanical evaluation of a novel hybrid reconstruction plate for mandible segmental defects: A finite element analysis and fatigue testing. J. Cranio-Maxillofac. Surg. 2017. [Google Scholar] [CrossRef] [PubMed]
- Sidambe, A. Biocompatibility of Advanced Manufactured Titanium Implants—A Review. Materials 2014, 7, 8168–8188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torres, Y.; Lascano, S.; Bris, J.; Pavón, J.; Rodriguez, J.A. Development of porous titanium for biomedical applications: A comparison between loose sintering and space-holder techniques. Mater. Sci. Eng. C 2014, 37, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.; Takano, T.; Takemoto, S.; Ueda, T.; Yoshiari, M.; Sakurai, K. Influence of grade and surface topography of commercially pure titanium on fatigue properties. Dent. Mater. J. 2018, 37, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Elias, C.N.; Lima, J.H.C.; Valiev, R.; Meyers, M.A. Biomedical applications of titanium and its alloys. JOM 2008, 60, 46–49. [Google Scholar] [CrossRef]
- Natali, A.N. Dental Biomechanics, 1st ed.; Taylor & Francis Group: London, UK, 2003; ISBN 0-415-30666-3. [Google Scholar]
- Scortecci, G.; Bourbon, B. Dentures on the Diskimplant. Rev. Fr. Prothes. Dent. 1990, 13, 31–48. [Google Scholar]
- Prados-Privado, M.; Bea, J.A.; Rojo, R.; Gehrke, S.A.; Calvo-Guirado, J.L.; Prados-Frutos, J.C. A New Model to Study Fatigue in Dental Implants Based on Probabilistic Finite Elements and Cumulative Damage Model. Appl. Bionics Biomech. 2017, 2017, 3726361. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.B.; Barão, V.A.; Faverani, L.P.; Hipólito, A.C.; Assunção, W.G. The role of superstructure material on the stress distribution in mandibular full-arch implant-supported fixed dentures. A CT-based 3D-FEA. Mater. Sci. Eng. C 2014, 35, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Agbaje, J.O.; Vrielinck, L.; Diederich, H. Rehabilitation of Edentulous Jaw Using Cortically Fixed at Once (Cf@O) Protocol: Proof of Principle. Biomed. J. Sci. Tech. Res. 2018, 5, 1–5. [Google Scholar] [CrossRef]
- Diederich, H.; Junqueira, M.A.; Guimarães, S.L. Immediate Loading of an Atrophied Maxilla Using the Principles of Cortically Fixed Titanium Hybrid Plates. Adv. Dent. Oral Health 2017, 3, 1–3. [Google Scholar] [CrossRef]
- Bhering, C.L.B.; Mesquita, M.F.; Kemmoku, D.T.; Noritomi, P.Y.; Consani, R.L.X.; Barão, V.A.R. Comparison between all-on-four and all-on-six treatment concepts and framework material on stress distribution in atrophic maxilla: A prototyping guided 3D-FEA study. Mater. Sci. Eng. C 2016, 69, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Boyer, R.; Welsch, G.; Collings, E.W. Materials Properties Handbook: Titanium Alloys; ASM International: Materials Park, OH, USA, 1994. [Google Scholar]
- Peixoto, H.E.; Camati, P.R.; Faot, F.; Sotto-Maior, B.; Martinez, E.F.; Peruzzo, D.C. Rehabilitation of the atrophic mandible with short implants in different positions: A finite elements study. Mater. Sci. Eng. C 2017, 80, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Shimura, Y.; Sato, Y.; Kitagawa, N.; Omori, M. Biomechanical effects of offset placement of dental implants in the edentulous posterior mandible. Int. J. Implant Dent. 2016, 2, 17. [Google Scholar] [CrossRef] [PubMed]
- Arat Bilhan, S.; Baykasoglu, C.; Bilhan, H.; Kutay, O.; Mugan, A. Effect of attachment types and number of implants supporting mandibular overdentures on stress distribution: A computed tomography-based 3D finite element analysis. J. Biomech. 2015, 48, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Prados-Privado, M.; Prados-Frutos, J.C.; Calvo-Guirado, J.L.; Bea, J.A. A random fatigue of mechanize titanium abutment studied with Markoff chain and stochastic finite element formulation. Comput. Methods Biomech. Biomed. Eng. 2016, 19, 1583–1591. [Google Scholar] [CrossRef] [PubMed]
- Riahi, H.; Bressolette, P.; Chateauneuf, A. Random fatigue crack growth in mixed mode by stochastic collocation method. Eng. Fract. Mech. 2010, 77, 3292–3309. [Google Scholar] [CrossRef]
- Bogdanoff, J.; Kozin, F. Probabilistic Models of Cumulative Damage; Wiley: New York, NY, USA, 1985. [Google Scholar]
- Neuber, H. Theory of Stress Concentration for Shear-Strained Prismatical Bodies With Arbitrary Nonlinear Stress-Strain Law. J. Appl. Mech. 1961, 28, 544–550. [Google Scholar] [CrossRef]
- Wentaschek, S.; Hartmann, S.; Walter, C.; Wagner, W. Six-implant-supported immediate fixed rehabilitation of atrophic edentulous maxillae with tilted distal implants. Int. J. Implant Dent. 2017, 3, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Odin, G.; Misch, C.E.; Binderman, I.; Scortecci, G. Fixed Rehabilitation of Severely Atrophic Jaws Using Immediately Loaded Basal Disk Implants After In Situ Bone Activation. J. Oral Implantol. 2012, 38, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Del Fabbro, M.; Rosano, G.; Taschieri, S. Implant survival rates after maxillary sinus augmentation. Eur. J. Oral Sci. 2008, 116, 497–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Staden, R.C.; Guan, H.; Loo, Y.C. Application of the finite element method in dental implant research. Comput. Methods Biomech. Biomed. Eng. 2006, 9, 257–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almeida, E.O.; Rocha, E.P.; Júnior, A.C.F.; Anchieta, R.B.; Poveda, R.; Gupta, N.; Coelho, P.G. Tilted and Short Implants Supporting Fixed Prosthesis in an Atrophic Maxilla: A 3D-FEA Biomechanical Evaluation. Clin. Implant Dent. Relat. Res. 2015, 17, e332–e342. [Google Scholar] [CrossRef] [PubMed]
- Küçükkurt, S.; Alpaslan, G.; Kurt, A. Biomechanical comparison of sinus floor elevation and alternative treatment methods for dental implant placement. Comput. Methods Biomech. Biomed. Eng. 2017, 20, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Ihde, S.; Goldmann, T.; Himmlova, L.; Aleksic, Z.; Kuzelka, J. Implementation of contact definitions calculated by FEA to describe the healing process of basal implants. Biomed. Pap. Med. Fac. Univ. Palacky Univ. Olomouc 2008, 152, 169–73. [Google Scholar] [CrossRef]
- Ihde, S.; Goldmann, T.; Himmlova, L.; Aleksic, Z. The use of finite element analysis to model bone-implant contact with basal implants. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2008, 106, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Kopp, S.; Kuzelka, J.; Goldmann, T.; Himmlova, L.; Ihde, S. Modeling of load transmission and distribution of deformation energy before and after healing of basal dental implants in the human mandible. Biomed. Tech. Eng. 2011, 56, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Pérez, M.A.; Prados-Frutos, J.C.; Bea, J.A.; Doblaré, M. Stress transfer properties of different commercial dental implants: A finite element study. Comput. Methods Biomech. Biomed. Eng. 2012, 15, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Marsico, V.; Lehmann, R.B.; de Assis Claro, C.A.; Amaral, M.; Vitti, R.P.; Neves, A.C.C.; da Silva Concilio, L.R. Three-dimensional finite element analysis of occlusal splint and implant connection on stress distribution in implant–supported fixed dental prosthesis and peri-implantal bone. Mater. Sci. Eng. C 2017, 80, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Gümrükçü, Z.; Korkmaz, Y.T.; Korkmaz, F.M. Biomechanical evaluation of implant-supported prosthesis with various tilting implant angles and bone types in atrophic maxilla: A finite element study. Comput. Biol. Med. 2017, 86, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Sevimay, M.; Turhan, F.; Kiliçarslan, M.A.; Eskitascioglu, G. Three-dimensional finite element analysis of the effect of different bone quality on stress distribution in an implant-supported crown. J. Prosthet. Dent. 2005, 93, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Haug, R.; Fattahi, T.; Goltz, M. A biomechanical evaluation of mandibular angle fracture plating techniques. J. Oral Maxillofac. Surg. 2001, 59, 1199–1210. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; Nobre Mde, A.; Lopes, A.; Ferro, A.; Moss, S. Five-year outcome of a retrospective cohort study on the rehabilitation of completely edentulous atrophic maxillae with immediately loaded zygomatic implants placed extra-maxillary. Eur. J. Oral Implantol. 2014, 7, 267–281. [Google Scholar] [PubMed]
- Migliorança, R.; Coppedê, A.; Dias Rezende, R.; de Mayo, T. Restoration of the edentulous maxilla using extrasinus zygomatic implants combined with anterior conventional implants: A retrospective study. Int. J. Oral Maxillofac. Implants 2011, 26, 665–672. [Google Scholar] [PubMed]



| Title | Young’s Modulus | Poisson’s Ratio |
|---|---|---|
| Plates (titanium grade II) [27] | 105 GPa | 0.37 |
| Maxilla: cortical bone [26] | 13.7 GPa | 0.3 |
| Maxilla: trabecular bone [26] | 1.37 GPa | 0.3 |
| Parameter | Value | Parameter | Value |
|---|---|---|---|
| 0.352 × 10−2 | 0.0140 × 106 | ||
| b | −0.1203 | 0.1701 | |
| c | −0.349 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prados-Privado, M.; Diederich, H.; Prados-Frutos, J.C. Implant Treatment in Atrophic Maxilla by Titanium Hybrid-Plates: A Finite Element Study to Evaluate the Biomechanical Behavior of Plates. Metals 2018, 8, 573. https://doi.org/10.3390/met8080573
Prados-Privado M, Diederich H, Prados-Frutos JC. Implant Treatment in Atrophic Maxilla by Titanium Hybrid-Plates: A Finite Element Study to Evaluate the Biomechanical Behavior of Plates. Metals. 2018; 8(8):573. https://doi.org/10.3390/met8080573
Chicago/Turabian StylePrados-Privado, María, Henri Diederich, and Juan Carlos Prados-Frutos. 2018. "Implant Treatment in Atrophic Maxilla by Titanium Hybrid-Plates: A Finite Element Study to Evaluate the Biomechanical Behavior of Plates" Metals 8, no. 8: 573. https://doi.org/10.3390/met8080573
APA StylePrados-Privado, M., Diederich, H., & Prados-Frutos, J. C. (2018). Implant Treatment in Atrophic Maxilla by Titanium Hybrid-Plates: A Finite Element Study to Evaluate the Biomechanical Behavior of Plates. Metals, 8(8), 573. https://doi.org/10.3390/met8080573






