Survival Rate and Deformation of External Hexagon Implants with One-Piece Zirconia Crowns
Abstract
:1. Introduction
2. Materials and Methods
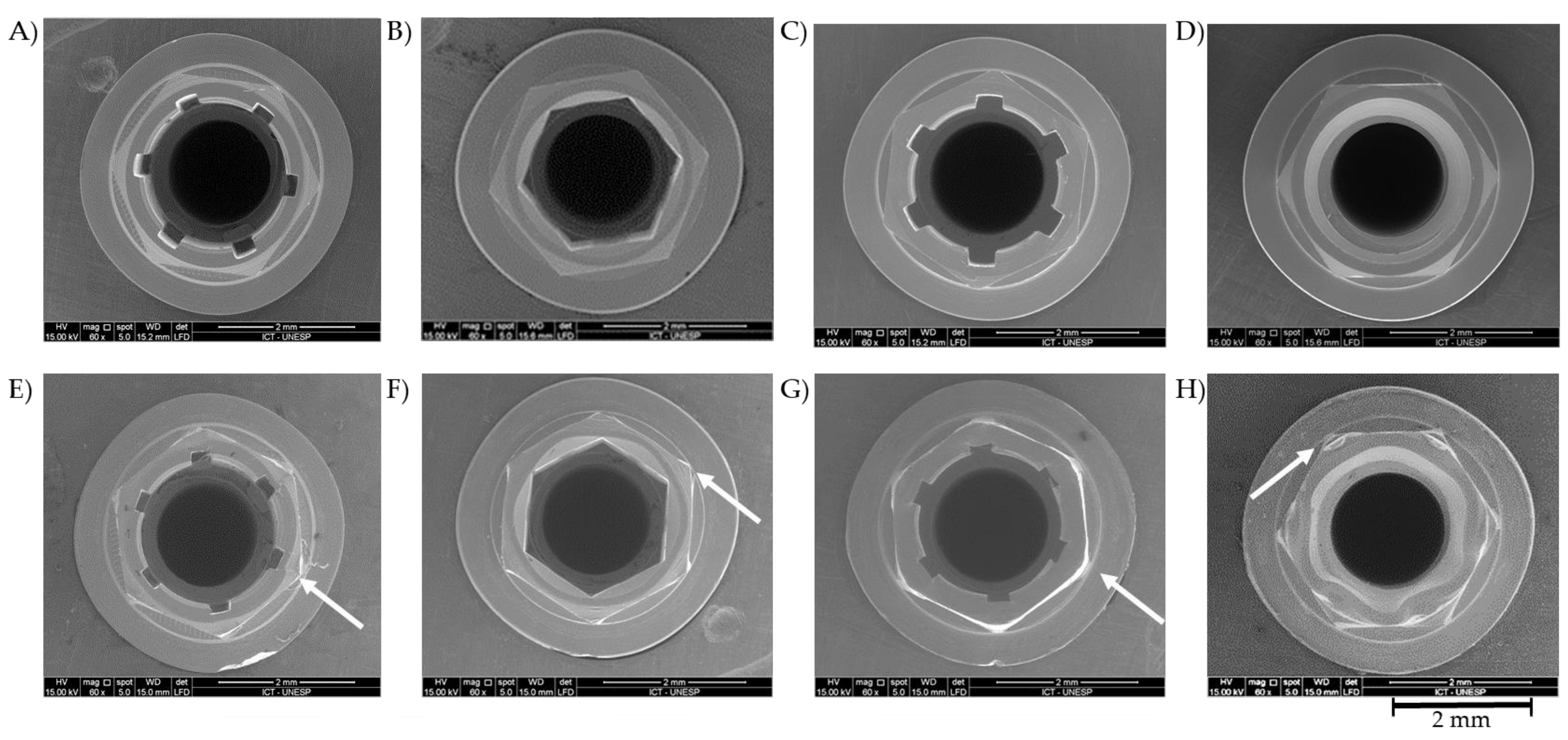
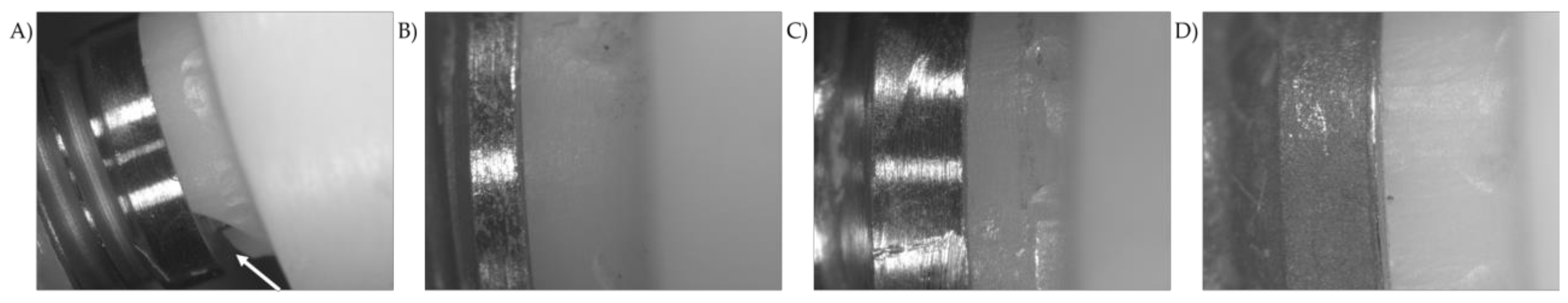
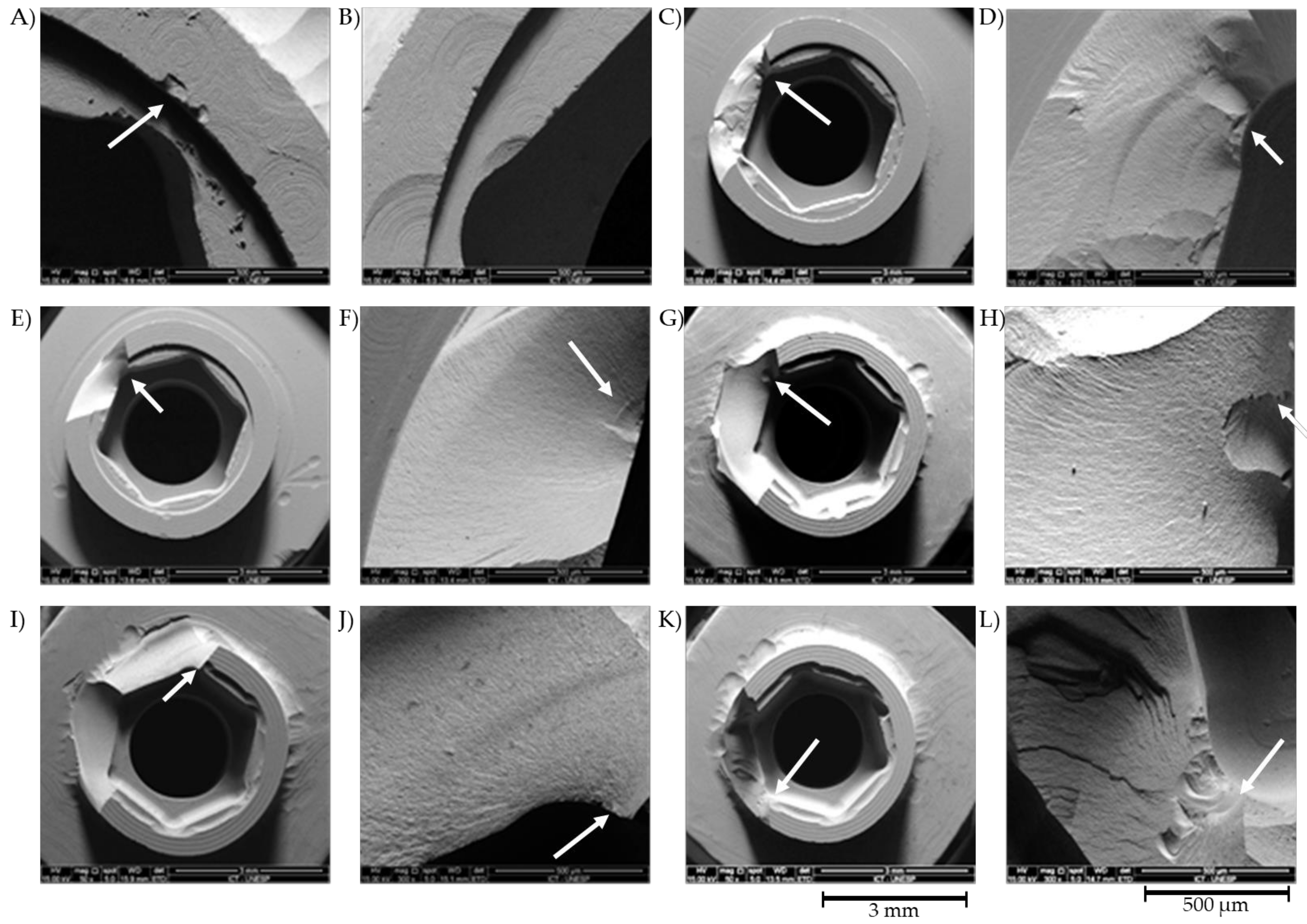
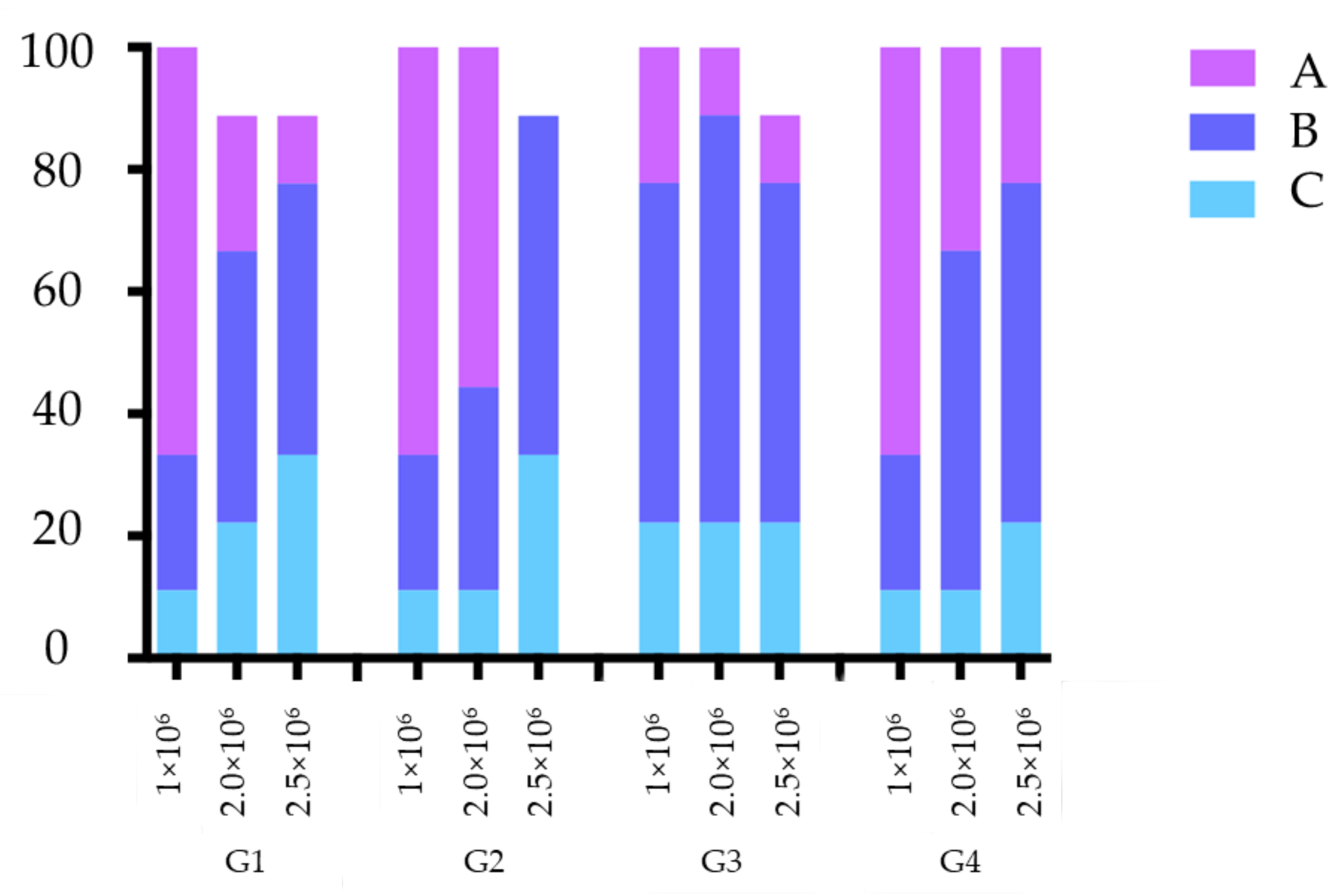
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abuhussein, H.; Pagni, G.; Rebaudi, A.; Wang, H.-L. The effect of thread pattern upon implant osseointegration. Clin. Oral Implants Res. 2010, 21, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Jalalian, E.; Yousofi, Z. Comparing torque loss in standard implants and short implants with increased vertical cantilever abutments: An in vitro study. Braz. Dent. Sci. 2020, 24, 1–8. [Google Scholar]
- Pjetursson, B.E.; Sailer, I.; Zwahlen, M.; Hämmerle, C.H.F. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: Single crowns. Clin. Oral Implants Res. 2007, 18 (Suppl. 3), 73–85. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, M.; Molinero-Mourelle, P.; Forrer, F.A.; Schnider, N.; Paul Hicklin, S.; Schimmel, M.; Brägger, U. Clinical performance of implant crowns with customized zirconia abutments. A prospective cohort study with a 4.5- to 8.8-year follow-up. Clin. Oral Implants Res 2021. [Google Scholar] [CrossRef]
- Mühlemann, S.; Truninger, T.C.; Stawarczyk, B.; Hämmerle, C.H.F.; Sailer, I. Bending moments of zirconia and titanium implant abutments supporting all-ceramic crowns after aging. Clin. Oral Implants Res. 2014, 25, 74–81. [Google Scholar] [CrossRef] [Green Version]
- Bottino, M.A.; Rocha, R.F.V.; Anami, L.C.; Özcan, M.; Marques de Melo, R. Fracture of Zirconia abutment with metallic insertion on anterior single titanium implant with internal hexagon: Retrieval analysis of a failure. Eur. J. Prosthodont. Restor. Dent. 2016, 24, 164–168. [Google Scholar] [PubMed]
- Datte, C.E.; Tribst, J.P.M.; Dal Piva, A.M.O.; Nishioka, R.S.; Bottino, M.A.; Evangelhista, A.D.M.; Monteiro, F.M.M.; Borges, A.L.S. Influence of different restorative materials on the stress distribution in dental implants. J. Clin. Exp. Dent. 2018, 10, 439–444. [Google Scholar] [CrossRef]
- Sailer, I.; Philipp, A.; Zembic, A.; Pjetursson, B.E.; Hämmerle, C.H.F.; Zwahlen, M. A systematic review of the performance of ceramic and metal implant abutments supporting fixed implant reconstructions. Clin. Oral Implants Res. 2009, 20 (Suppl. 4), 4–31. [Google Scholar] [CrossRef] [Green Version]
- Rauscher, O. Impression-free implant restorations with Cerec InLab. Int. J. Comput. Dent. 2011, 14, 139–146. [Google Scholar]
- Adolfi, D.; Mendes Tribst, J.P.; Souto Borges, A.L.; Bottino, M.A. Torque maintenance capacity, vertical misfit, load to failure, and stress concentration of Zirconia restorations cemented or notched to titanium bases. Int. J. Oral Maxillofac. Implants 2020, 35, 357–365. [Google Scholar] [CrossRef]
- Sailer, I.; Sailer, T.; Stawarczyk, B.; Jung, R.E.; Hämmerle, C.H.F. In vitro study of the influence of the type of connection on the fracture load of zirconia abutments with internal and external implant-abutment connections. Int. J. Oral Maxillofac. Implants 2009, 24, 850–858. [Google Scholar] [PubMed]
- Gehrke, S.A.; Poncio da Silva, P.M.; Calvo Guirado, J.L.; Delgado-Ruiz, R.A.; Dedavid, B.A.; Aline Nagasawa, M.; Shibli, J.A. Mechanical behavior of zirconia and titanium abutments before and after cyclic load application. J. Prosthet. Dent. 2016, 116, 529–535. [Google Scholar] [CrossRef]
- Hoyer, S.A.; Stanford, C.M.; Buranadham, S.; Fridrich, T.; Wagner, J.; Gratton, D. Dynamic fatigue properties of the dental implant-abutment interface: Joint opening in wide-diameter versus standard-diameter hex-type implants. J. Prosthet. Dent. 2001, 85, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.d.O.; da Silva-Concílio, L.R.; Ausiello, P.; Kalman, L. Influence of Implant-Abutment Contact Surfaces and Prosthetic Screw Tightening on the Stress Concentration, Fatigue Life and Microgap Formation: A Finite Element Analysis. Oral 2021, 1, 9. [Google Scholar] [CrossRef]
- Karl, M.; Graef, F.; Wichmann, M.G.; Heckmann, S.M. The effect of load cycling on metal ceramic screw-retained implant restorations with unrestored and restored screw access holes. J. Prosthet. Dent. 2008, 99, 19–24. [Google Scholar] [CrossRef]
- Thomé, G.; Torres Gomes, A.F.; de Moura, M.B.; Felippi, C.; Trojan, L.C. Evaluation of the mechanical reliability of different implant-abutment connections for single crowns according to the ISO 14801 fatigue test protocol. Int. J. Oral Maxillofac. Implants 2021, 36, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Truninger, T.C.; Stawarczyk, B.; Leutert, C.R.; Sailer, T.R.; Hämmerle, C.H.F.; Sailer, I. Bending moments of zirconia and titanium abutments with internal and external implant-abutment connections after aging and chewing simulation: Bending moments of zirconia and titanium abutments. Clin. Oral Implants Res. 2012, 23, 12–18. [Google Scholar] [CrossRef]
- Sailer, I.; Asgeirsson, A.G.; Thoma, D.S.; Fehmer, V.; Aspelund, T.; Özcan, M.; Pjetursson, B.E. Fracture strength of zirconia implant abutments on narrow diameter implants with internal and external implant abutment connections: A study on the titanium resin base concept. Clin. Oral Implants Res. 2018, 29, 411–423. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.d.O.; Borges, A.L.S.; Rodrigues, V.A.; Bottino, M.A.; Kleverlaan, C.J. Does the prosthesis weight matter? 3D finite element analysis of a fixed implant-supported prosthesis at different weights and implant numbers. J. Adv. Prosthodont. 2020, 12, 67–74. [Google Scholar] [CrossRef] [Green Version]
- Tribst, J.P.M.; Dal Piva, A.M.d.O.; Gonçalves, N.I.Ê.; Borges, A.L.S.; Bottino, M.A.; Kleverlaan, C.J. Polymerization shrinkage and push-out bond strength of different composite resins for sealing the screw-access hole on implant-supported crowns. J. Adhes. Dent. 2020, 22, 523–530. [Google Scholar] [PubMed]
- Guazzato, M.; Albakry, M.; Ringer, S.P.; Swain, M.V. Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part II. Zirconia-based dental ceramics. Dent. Mater. 2004, 20, 449–456. [Google Scholar] [CrossRef]
- Amaral, M.; Valandro, L.F.; Bottino, M.A.; Souza, R.O.A. Low-temperature degradation of a Y-TZP ceramic after surface treatments: Zirconia Ltd After Surface Treatments. J. Biomed. Mater. Res. B Appl. Biomater. 2013, 101, 1387–1392. [Google Scholar] [CrossRef] [PubMed]
- Moilanen, P.; Hjerppe, J.; Lassila, L.V.J.; Närhi, T.O. Fracture strength and precision of fit of implant-retained monolithic Zirconia crowns. J. Oral Implantol. 2018, 44, 330–334. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.Q.; Tan, K.B.; Nicholls, J.I. Load fatigue performance of implant-ceramic abutment combinations. Int. J. Oral Maxillofac. Implants 2009, 24, 636–646. [Google Scholar] [PubMed]
- Manicone, P.F.; Rossi Iommetti, P.; Raffaelli, L. An overview of zirconia ceramics: Basic properties and clinical applications. J. Dent. 2007, 35, 819–826. [Google Scholar] [CrossRef]
- De Boever, A.L.; Keersmaekers, K.; Vanmaele, G.; Kerschbaum, T.; Theuniers, G.; De Boever, J.A. Prosthetic complications in fixed endosseous implant-borne reconstructions after an observations period of at least 40 months: Prosthetic Complications In Implant-Borne Fixed Reconstructions. J. Oral Rehabil. 2006, 33, 833–839. [Google Scholar] [CrossRef]
- Silveira, M.P.M.; Campaner, L.M.; Bottino, M.A.; Nishioka, R.S.; Borges, A.L.S.; Tribst, J.P.M. Influence of the dental implant number and load direction on stress distribution in a 3-unit implant-supported fixed dental prosthesis. Dent. Med. Probl. 2021, 58, 69–74. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.O.; Özcan, M.; Borges, A.L.S.; Bottino, M.A. Influence of ceramic materials on biomechanical behavior of implant supported fixed prosthesis with hybrid abutment. Eur. J. Prosthodont. Restor. Dent. 2019, 27, 76–82. [Google Scholar] [PubMed]
- Matos, J.D.; Arcila, L.V.; Ortiz, L.P.; Lopes, G.R.; Anami, L.C.; Ramos, N.C.; Saavedra, G.S.; Tribst, J.P.; Bottino, M.A. Hybrid abutment during prosthetic planning and oral rehabilitation. Minerva Dent. Oral Sci. 2021. [Google Scholar] [CrossRef]

| Material | Commercial Name | Manufacturer |
|---|---|---|
| Polyurethane resin | F160 | Axson Brasil HighTech (Socorro, SP, Brazil) |
| Grade 4 Titanium | Bonelike | Biotechnology 3i (Rio Claro, SP, Brazil) |
| Grade 4 Titanium | Master | Conexão Sistemas de Prótese (Arujá, SP, Brazil) |
| Grade 4 Titanium | Titamax Smart | Neodent (Curitiba, PR, Brazil) |
| Grade 4 Titanium | Branemark System MK III RP | Nobel Biocare (Gotenborg, Sweden) |
| 3-YTZP | Prettau Zirkon | Zirkonzahn GmbH (Gais, Italy) |
| Material | Average | Standard Deviation |
|---|---|---|
| Zirconia Crown | 1645.53 | 71.77 |
| G1 | 325.12 a | 20.60 |
| G2 | 390.80 a | 41.25 |
| G3 | 373.75 a | 25.65 |
| G4 | 368.41 a | 24.44 |
| Log-Rank Test | |||
|---|---|---|---|
| Implant | n | Sum | Mean |
| G1 | 9 | 1.5294 | 0.1699 |
| G2 | 9 | 0.4706 | 0.0523 |
| G3 | 9 | −1.4706 | −0.1634 |
| G4 | 9 | −0.5294 | −0.0588 |
| Chi-Square | 3.45 | 3.49 | 3.29 |
| DF | 3 | 3 | 3 |
| p | 0.3275 | 0.3219 | 0.3487 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bottino, M.A.; de Oliveira, F.R.; Sabino, C.F.; Dinato, J.C.; Silva-Concílio, L.R.; Tribst, J.P.M. Survival Rate and Deformation of External Hexagon Implants with One-Piece Zirconia Crowns. Metals 2021, 11, 1068. https://doi.org/10.3390/met11071068
Bottino MA, de Oliveira FR, Sabino CF, Dinato JC, Silva-Concílio LR, Tribst JPM. Survival Rate and Deformation of External Hexagon Implants with One-Piece Zirconia Crowns. Metals. 2021; 11(7):1068. https://doi.org/10.3390/met11071068
Chicago/Turabian StyleBottino, Marco Antonio, Flávio Rosa de Oliveira, Clarice Ferreira Sabino, José Cícero Dinato, Laís Regiane Silva-Concílio, and João Paulo Mendes Tribst. 2021. "Survival Rate and Deformation of External Hexagon Implants with One-Piece Zirconia Crowns" Metals 11, no. 7: 1068. https://doi.org/10.3390/met11071068
APA StyleBottino, M. A., de Oliveira, F. R., Sabino, C. F., Dinato, J. C., Silva-Concílio, L. R., & Tribst, J. P. M. (2021). Survival Rate and Deformation of External Hexagon Implants with One-Piece Zirconia Crowns. Metals, 11(7), 1068. https://doi.org/10.3390/met11071068







