Effects of a Traditional versus an Alternative Strengthening Exercise Program on Shoulder Pain, Function and Physical Performance in Individuals with Subacromial Shoulder Pain: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
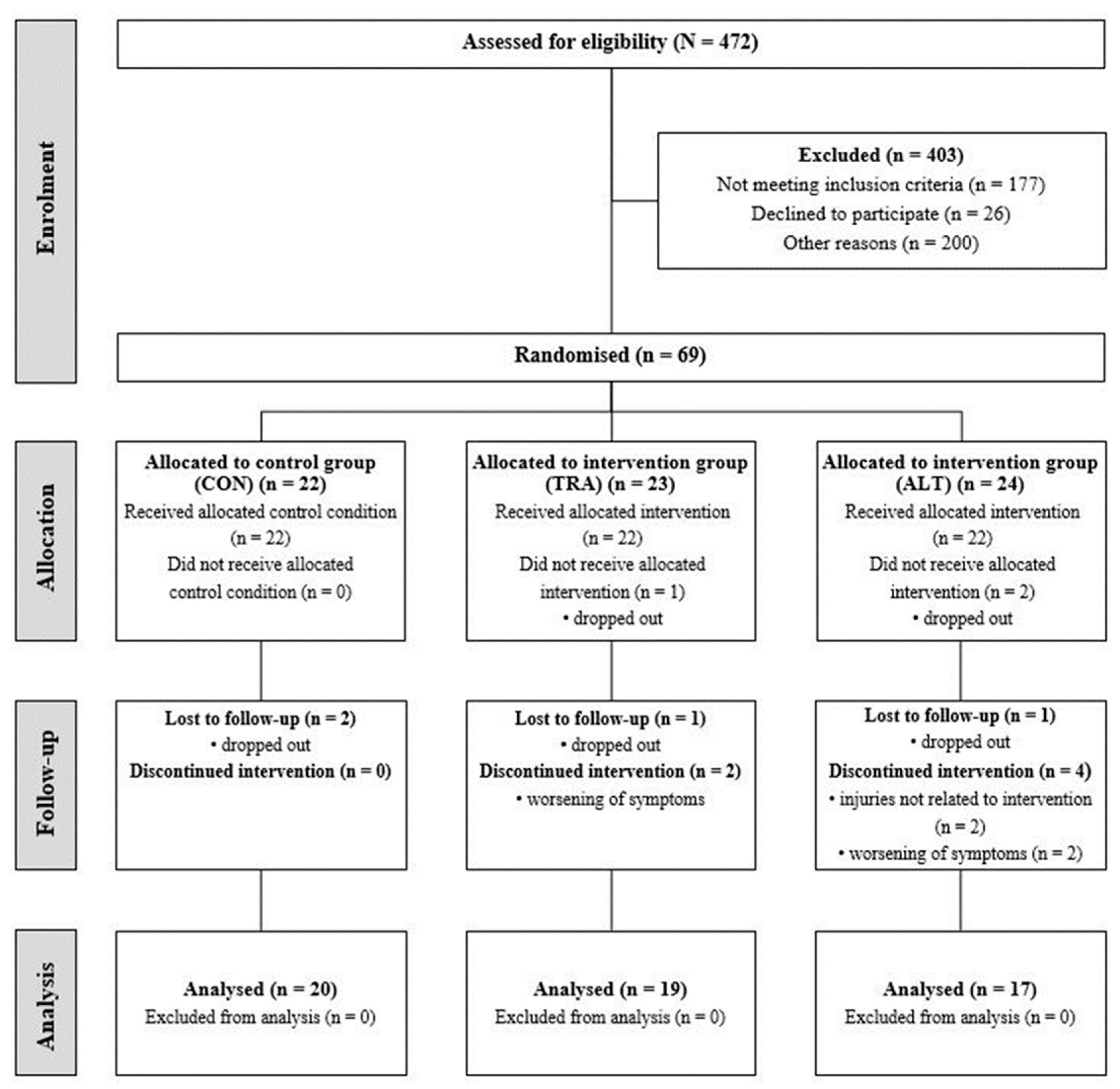
2.1. Participants
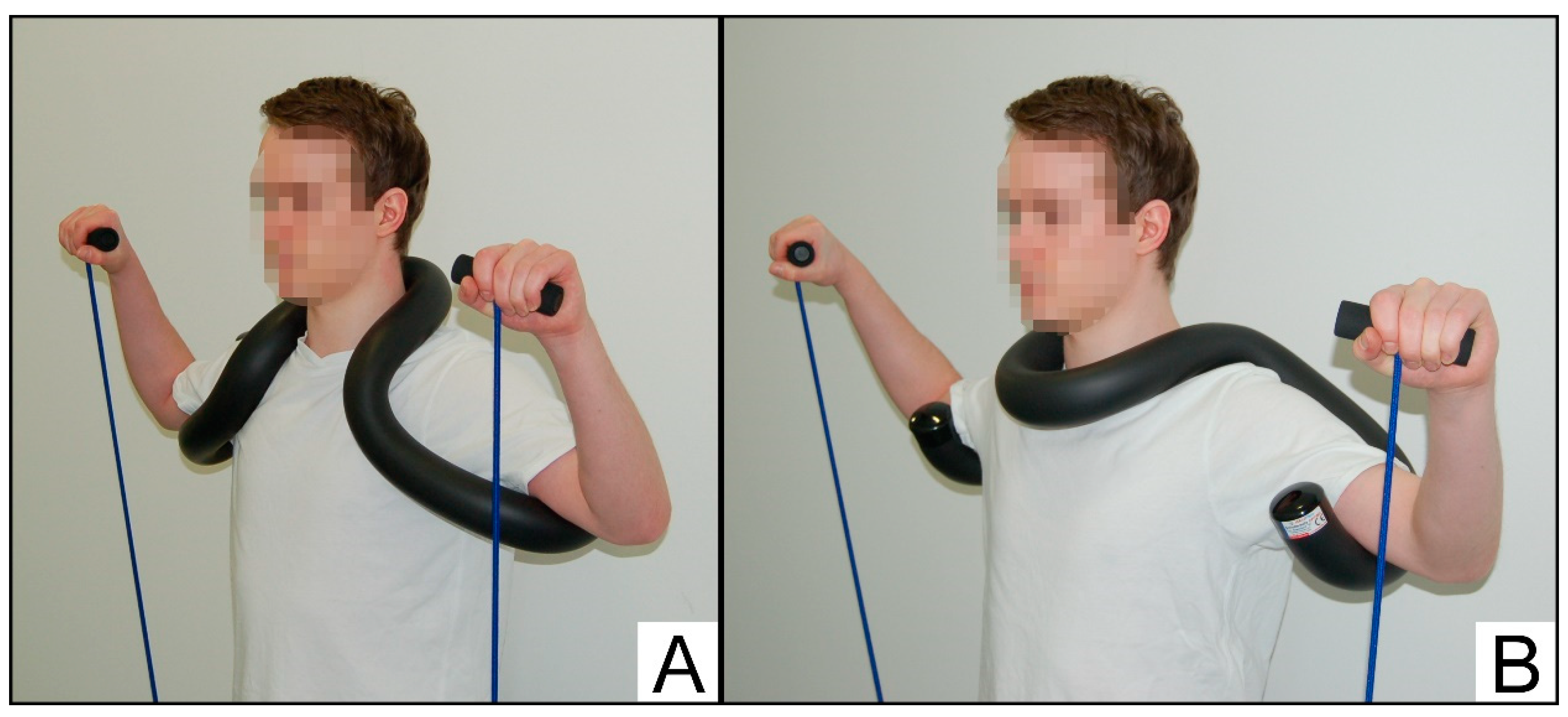
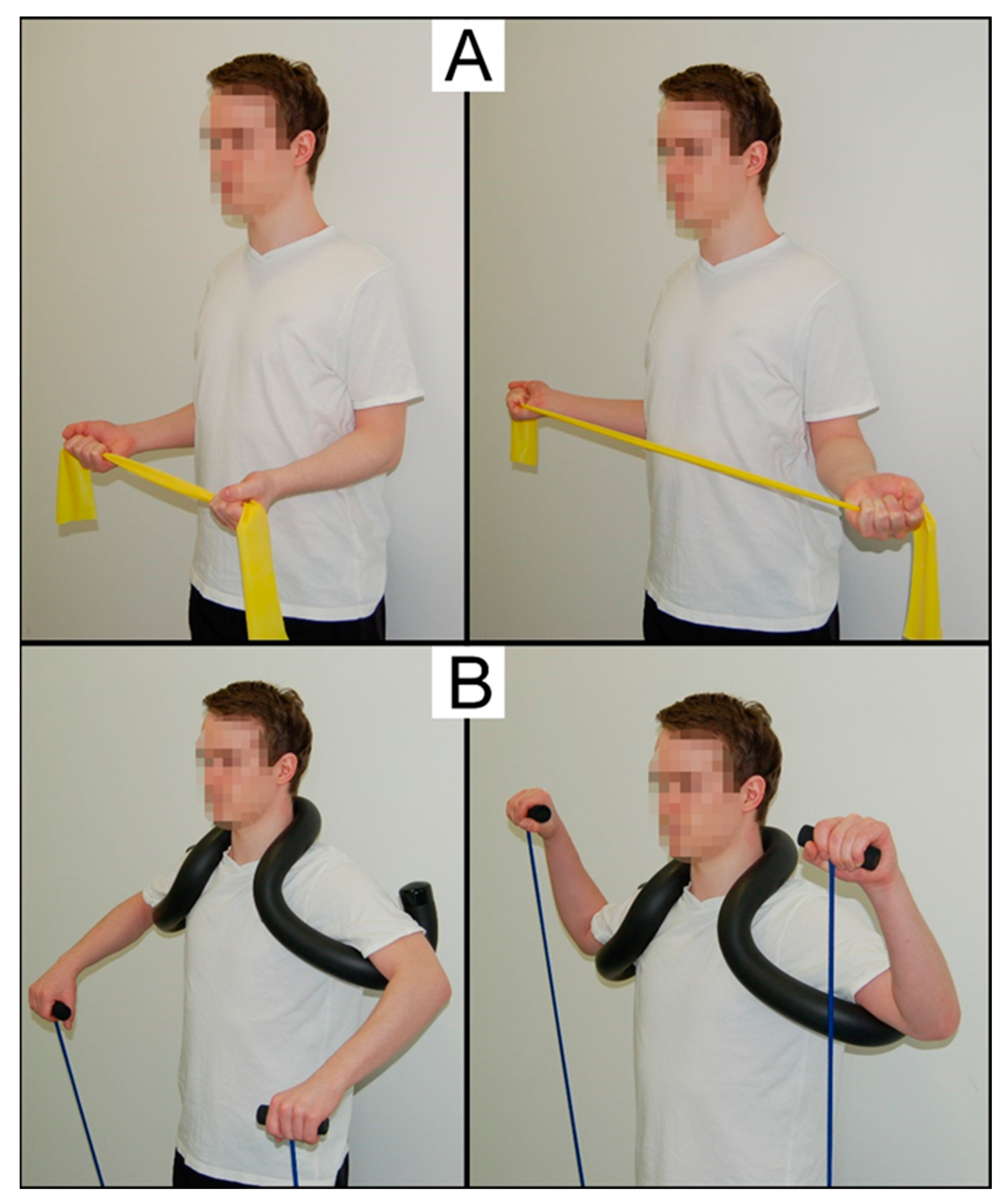
2.2. Shoulder Training Programs
2.3. Testing Procedures
2.3.1. Assessment of Anthropometric Variables
2.3.2. Assessment of Shoulder Pain and Function
2.3.3. Assessment of Shoulder Flexibility
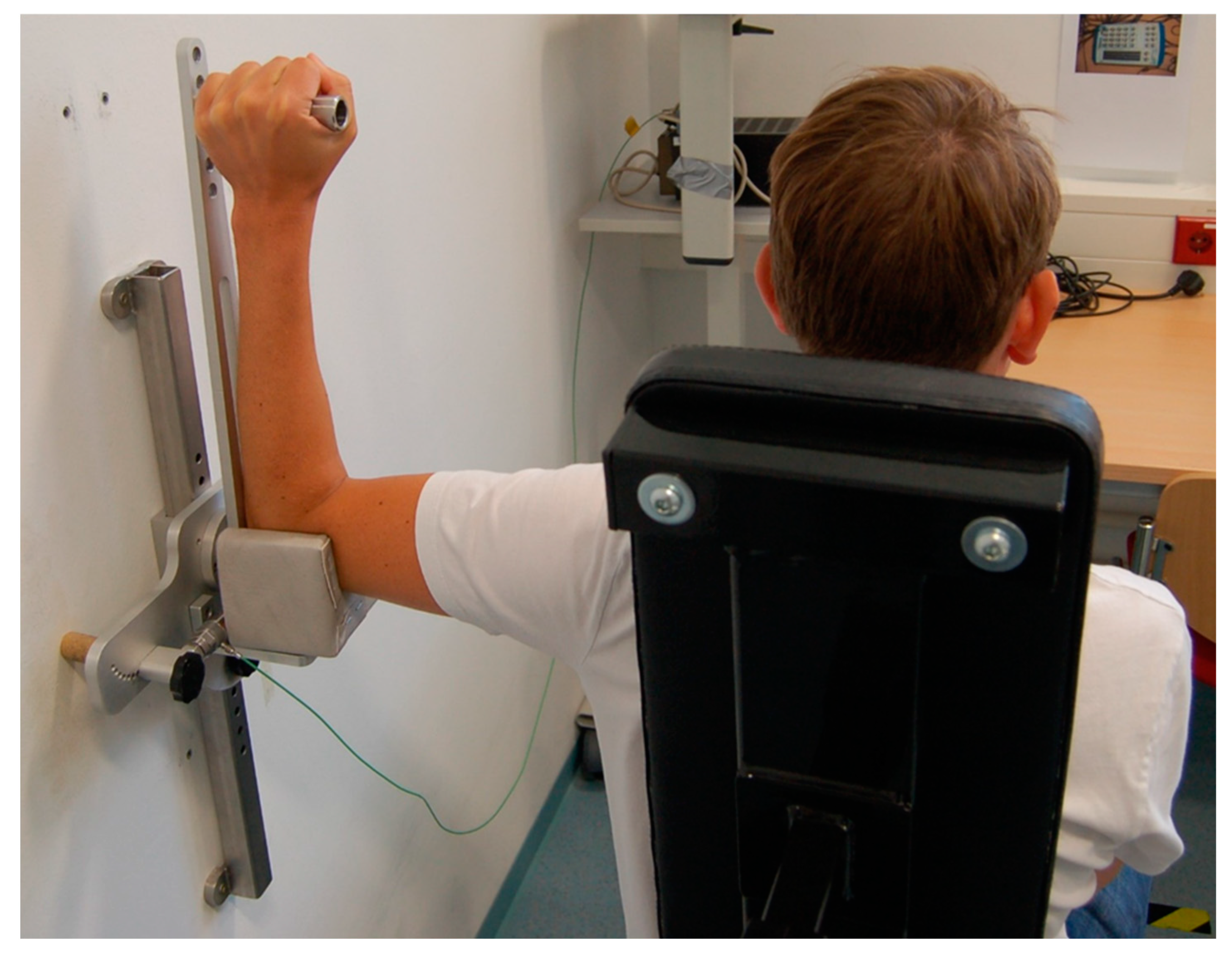
2.3.4. Assessment of Maximal Isometric Strength
2.3.5. Assessment of Strength Endurance
2.4. Statistical Analyses
3. Results
3.1. Shoulder Pain and Function
3.2. Shoulder Flexibility
3.3. Maximal Isometric Strength
3.4. Strength Endurance
4. Discussion
4.1. Training Effects on Measures of Shoulder Pain and Function
4.2. Training Effects on Measures of Physical Performance
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ostor, A.J.; Richards, C.A.; Prevost, A.T.; Speed, C.A.; Hazleman, B.L. Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology 2005, 44, 800–805. [Google Scholar] [CrossRef] [PubMed]
- Van der Windt, D.A.; Koes, B.W.; de Jong, B.A.; Bouter, L.M. Shoulder disorders in general practice: Incidence, patient characteristics, and management. Ann. Rheum. Dis. 1995, 54, 959–964. [Google Scholar] [CrossRef] [PubMed]
- Urwin, M.; Symmons, D.; Allison, T.; Brammah, T.; Busby, H.; Roxby, M.; Simmons, A.; Williams, G. Estimating the burden of musculoskeletal disorders in the community: The comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann. Rheum. Dis. 1998, 57, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Michener, L.A.; McClure, P.W.; Karduna, A.R. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin. Biomech. 2003, 18, 369–379. [Google Scholar] [CrossRef]
- Harrison, A.K.; Flatow, E.L. Subacromial impingement syndrome. J. Am. Acad. Orthop. Surg. 2011, 19, 701–708. [Google Scholar] [CrossRef]
- MacDermid, J.C.; Ramos, J.; Drosdowech, D.; Faber, K.; Patterson, S. The impact of rotator cuff pathology on isometric and isokinetic strength, function, and quality of life. J. Shoulder Elbow Surg. 2004, 13, 593–598. [Google Scholar] [CrossRef]
- Tekeoglu, I.; Ediz, L.; Hiz, O.; Toprak, M.; Yazmalar, L.; Karaaslan, G. The relationship between shoulder impingement syndrome and sleep quality. Eur. Rev. Med. Pharmacol. Sci. 2013, 17, 370–374. [Google Scholar]
- Van der Heijden, G.J. Shoulder disorders: A state-of-the-art review. Baillieres Clin. Rheumatol. 1999, 13, 287–309. [Google Scholar] [CrossRef]
- Khan, M.; Alolabi, B.; Horner, N.; Bedi, A.; Ayeni, O.R.; Bhandari, M. Surgery for shoulder impingement: A systematic review and meta-analysis of controlled clinical trials. CMAJ Open 2019, 7, E149–E158. [Google Scholar] [CrossRef]
- Steuri, R.; Sattelmayer, M.; Elsig, S.; Kolly, C.; Tal, A.; Taeymans, J.; Hilfiker, R. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: A systematic review and meta-analysis of RCTs. Br. J. Sports Med. 2017, 51, 1340–1347. [Google Scholar] [CrossRef]
- Littlewood, C.; Bateman, M.; Brown, K.; Bury, J.; Mawson, S.; May, S.; Walters, S.J. A self-managed single exercise programme versus usual physiotherapy treatment for rotator cuff tendinopathy: A randomised controlled trial (the SELF study). Clin. Rehabil. 2016, 30, 686–696. [Google Scholar] [CrossRef] [PubMed]
- Ellenbecker, T.S.; Cools, A. Rehabilitation of shoulder impingement syndrome and rotator cuff injuries: An evidence-based review. Br. J. Sports Med. 2010, 44, 319–327. [Google Scholar] [CrossRef]
- Linsell, L.; Dawson, J.; Zondervan, K.; Rose, P.; Randall, T.; Fitzpatrick, R.; Carr, A. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology 2006, 45, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Grigereit, A.; Ziesing, A.; Vogt, L.; Banzer, W. EMG analysis of shoulder muscles during preventive and therapeutic exercise in the overhead athlete. Sportverletz. Sportschaden 2003, 17, 21–25. [Google Scholar] [CrossRef] [PubMed]
- General Assembly of the World Medical, A. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. J. Am. Coll. Dent. 2014, 81, 14–18. [Google Scholar]
- McKenna, L.; Straker, L.; Smith, A. The inter-tester reliability of anthropometric measurement with portable tools. Eur. J. Physiother. 2013, 15, 34–41. [Google Scholar] [CrossRef]
- Angst, F.; Goldhahn, J.; Pap, G.; Mannion, A.F.; Roach, K.E.; Siebertz, D.; Drerup, S.; Schwyzer, H.K.; Simmen, B.R. Cross-cultural adaptation, reliability and validity of the German Shoulder Pain and Disability Index (SPADI). Rheumatology 2007, 46, 87–92. [Google Scholar] [CrossRef]
- Ryf, C.; Weymann, A. The neutral zero method-A principle of measuring joint function. Injury 1995, 26, 1–11. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Schmitt, J.S.; Di Fabio, R.P. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J. Clin. Epidemiol. 2004, 57, 1008–1018. [Google Scholar] [CrossRef]
- Clausen, M.B.; Merrild, M.B.; Witten, A.; Christensen, K.B.; Zebis, M.K.; Holmich, P.; Thorborg, K. Conservative treatment for patients with subacromial impingement: Changes in clinical core outcomes and their relation to specific rehabilitation parameters. PeerJ 2018, 6, e4400. [Google Scholar] [CrossRef] [PubMed]
- Kromer, T.O.; de Bie, R.A.; Bastiaenen, C.H. Physiotherapy in patients with clinical signs of shoulder impingement syndrome: A randomized controlled trial. J. Rehabil. Med. 2013, 45, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Bae, Y.H.; Lee, G.C.; Shin, W.S.; Kim, T.H.; Lee, S.M. Effect of Motor Control and Strengthening Exercises on Pain, Function, Strength and the Range of Motion of Patients with Shoulder Impingement Syndrome. J. Phys. Ther. Sci. 2011, 23, 687–692. [Google Scholar] [CrossRef]
- Bang, M.D.; Deyle, G.D. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J. Orthop. Sports Phys. Ther. 2000, 30, 126–137. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, I., Jr.; Magri, A.G.; Fleury, A.M.; Da Silva, A.C.; Natour, J. Progressive resistance training in patients with shoulder impingement syndrome: A randomized controlled trial. Arthritis Rheum. 2008, 59, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Tyler, T.F.; Nahow, R.C.; Nicholas, S.J.; McHugh, M.P. Quantifying shoulder rotation weakness in patients with shoulder impingement. J. Shoulder Elbow. Surg. 2005, 14, 570–574. [Google Scholar] [CrossRef]
- Tucci, H.T.; Martins, J.; Sposito Gde, C.; Camarini, P.M.; de Oliveira, A.S. Closed Kinetic Chain upper Extremity Stability test (CKCUES test): A reliability study in persons with and without shoulder impingement syndrome. BMC Musculoskelet. Disord. 2014, 15. [Google Scholar] [CrossRef]
- Haik, M.N.; Alburquerque-Sendin, F.; Moreira, R.F.; Pires, E.D.; Camargo, P.R. Effectiveness of physical therapy treatment of clearly defined subacromial pain: A systematic review of randomised controlled trials. Br. J. Sports Med. 2016, 50, 1124–1134. [Google Scholar] [CrossRef]

| Characteristic | CON (n = 20) | TRA (n = 19) | ALT (n = 17) | p-Value |
|---|---|---|---|---|
| Sex (f/m) | 11/9 | 10/9 | 8/9 | - |
| Age (years) | 53.0 ± 6.6 | 54.3 ± 8.4 | 52.7 ± 7.0 | 0.771 |
| Body height (cm) | 170.4 ± 9.8 | 174.7 ± 9.7 | 171.1 ± 8.5 | 0.319 |
| Body mass (kg) | 82.0 ± 18.0 | 83.0 ± 17.9 | 79.6 ± 26.6 | 0.886 |
| BMI (kg/m2) | 28.0 ± 4.2 | 27.2 ± 5.4 | 26.9 ± 7.1 | 0.823 |
| Outcome | CON (n = 20) | TRA (n = 19) | ALT (n = 17) | p-/d-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | ∆% * | Pre | Post | ∆% * | Pre | Post | ∆% * | T | T × G | |
| Shoulder pain/function | |||||||||||
| SPADI total scale (pt) | 41.0 ± 19.8 | 40.7 ± 21.9 | +4 (43) | 44.1 ± 19.2 | 31.4 ± 20.5 | +28 (36) | 40.0 ± 21.7 | 20.0 ± 16.3 | +51 (34) | <0.001 (1.68) | <0.001 # (1.25) |
| SPADI subscale “disability” (pt) | 36.5 ± 21.9 | 35.2 ± 22.2 | +5 (87) | 37.3 ± 20.3 | 26.3 ± 20.7 | +24 (55) | 35.4 ± 22.4 | 15.8 ± 13.0 | +58 (33) | <0.001 (1.56) | 0.001 # (1.09) |
| SPADI subscale “pain” (pt) | 48.1 ± 18.8 | 49.5 ± 23.1 | −1 (34) | 55.1 ± 19.3 | 39.6 ± 21.6 | +27 (32) | 47.5 ± 21.9 | 26.8 ± 23.3 | +44 (39) | <0.001 (1.48] | <0.001 # (1.22) |
| Shoulder flexibility | |||||||||||
| ROM, external rotation, left arm (°) | 67.9 ± 22.0 | 66.8 ± 21.5 | −1 (18) | 72.5 ± 14.5 | 83.7 ± 15.3 | +18 (24) | 73.1 ± 15.7 | 91.8 ± 17.1 | +28 (23) | <0.001 (1.57) | <0.001 # (1.34) |
| ROM external rotation, right arm (°) | 83.0 ± 15.0 | 80.8 ± 14.8 | −2 (14) | 82.0 ± 12.8 | 85.9 ± 15.3 | +6 (19) | 82.5 ± 13.1 | 94.9 ± 13.7 | +17 (20 | 0.011 (0.73) | 0.006 # (0.92) |
| ROM, internal rotation, left arm (°) | 50.3 ± 17.5 | 51.4 ± 15.7 | +21 (77) | 47.9 ± 20.1 | 58.4 ± 23.5 | +39 (69) | 51.2 ± 21.6 | 66.6 ± 22.7 | +55 (80) | <0.001 (1.02) | 0.057 # (0.67) |
| ROM, internal rotation, right arm (°) | 48.3 ± 16.7 | 46.4 ± 17.4 | −1 (30) | 45.4 ± 21.5 | 56.4 ± 19.9 | +41 (36) | 48.0 ± 12.5 | 66.2 ± 20.3 | +57 (100) | <0.001 (1.20) | 0.001 # (1.10) |
| Maximal strength | |||||||||||
| MIS external rotators, left arm (Nm) | 9.3 ± 4.7 | 11.3 ± 5.8 | +31 (48) | 13.3 ± 6.5 | 16.7 ± 8.2 | +37 (50) | 11.4 ± 5.3 | 14.4 ± 5.4 | +39 (37) | <0.001 (1.49) | 0.510 (0.33) |
| MIS external rotators, right arm (Nm) | 12.3 ± 7.3 | 13.6 ± 6.1 | +36 (67) | 13.1 ± 7.2 | 17.3 ± 8.9 | +42 (49) | 11.3 ± 5.1 | 16.1 ± 5.6 | +54 (53) | <0.001 (1.90) | 0.010 # (0.87) |
| MIS internal rotators, left arm (Nm) | 20.7 ± 15.1 | 20.9 ± 14.5 | +12 (36) | 23.2 ± 16.4 | 26.8 ± 17.7 | +26 (38) | 19.7 ± 12.3 | 23.1 ± 11.9 | +35 (59) | 0.012 (0.75) | 0.225 (0.35) |
| MIS internal rotators, right arm (Nm) | 22.0 ± 16.6 | 22.1 ± 15.1 | +27 (72) | 24.0 ± 18.6 | 29.3 ± 19.4 | +41 (64) | 17.8 ± 8.6 | 23.5 ± 10.8 | +35 (39) | 0.001 (1.00) | 0.217 (0.35) |
| Strength endurance | |||||||||||
| Metronome-paced strength endurance test (n) | 52.3 ± 66.5 | 56.1 ± 95.3 | +1 (39) | 37.0 ± 20.6 | 38.5 ± 13.7 | +23 (66) | 42.8 ± 18.0 | 66.4 ± 29.3 | +89 (141) | 0.015 (0.70) | 0.051 # (0.70) |
| CKCUEST (n) | 17.2 ± 5.2 | 18.6 ± 5.4 | +10 (16) | 16.5 ± 3.0 | 19.5 ± 2.9 | +19 (13) | 18.3 ± 3.0 | 20.9 ± 3.7 | +14 (8) | <0.001 (2.77) | 0.017 # (0.83) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schedler, S.; Brueckner, D.; Hagen, M.; Muehlbauer, T. Effects of a Traditional versus an Alternative Strengthening Exercise Program on Shoulder Pain, Function and Physical Performance in Individuals with Subacromial Shoulder Pain: A Randomized Controlled Trial. Sports 2020, 8, 48. https://doi.org/10.3390/sports8040048
Schedler S, Brueckner D, Hagen M, Muehlbauer T. Effects of a Traditional versus an Alternative Strengthening Exercise Program on Shoulder Pain, Function and Physical Performance in Individuals with Subacromial Shoulder Pain: A Randomized Controlled Trial. Sports. 2020; 8(4):48. https://doi.org/10.3390/sports8040048
Chicago/Turabian StyleSchedler, Simon, Dennis Brueckner, Marco Hagen, and Thomas Muehlbauer. 2020. "Effects of a Traditional versus an Alternative Strengthening Exercise Program on Shoulder Pain, Function and Physical Performance in Individuals with Subacromial Shoulder Pain: A Randomized Controlled Trial" Sports 8, no. 4: 48. https://doi.org/10.3390/sports8040048
APA StyleSchedler, S., Brueckner, D., Hagen, M., & Muehlbauer, T. (2020). Effects of a Traditional versus an Alternative Strengthening Exercise Program on Shoulder Pain, Function and Physical Performance in Individuals with Subacromial Shoulder Pain: A Randomized Controlled Trial. Sports, 8(4), 48. https://doi.org/10.3390/sports8040048





