Association between Subjective Indicators of Recovery Status and Heart Rate Variability among Divison-1 Sprint-Swimmers
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.2.1. Observation Period
2.2.2. Heart Rate Parameters
2.2.3. Athlete Self-Report Measures
2.3. Statistical Analysis
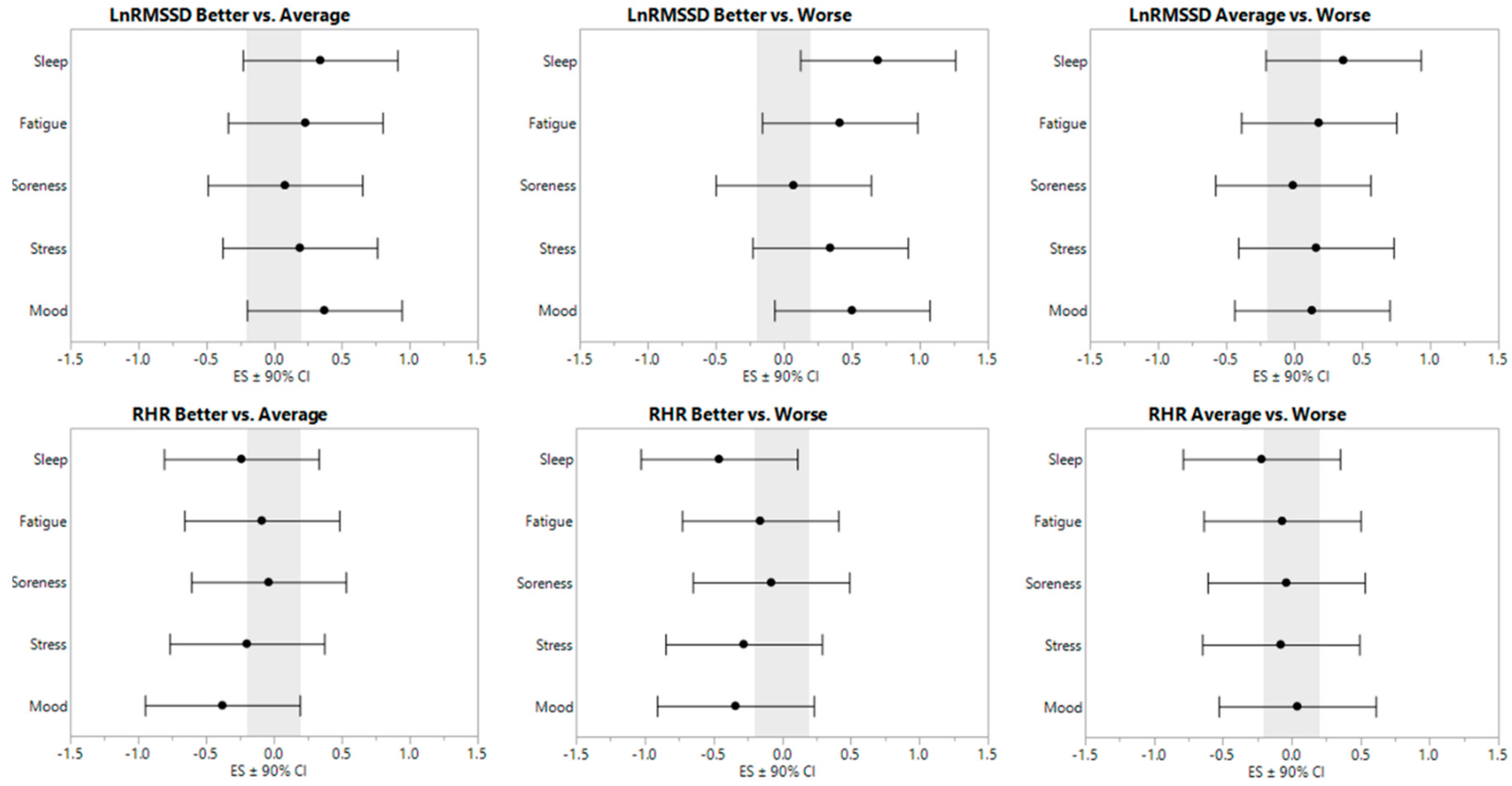
3. Results
3.1. HR-Parameters
3.1.1. RHR
3.1.2. LnRMSSD
3.1.3. Within-Subject Correlations
3.1.4. Multicollinearity
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fatisson, J.; Oswald, V.; Lalonde, F. Influence diagram of physiological and environmental factors affecting heart rate variability: An extended literature overview. Heart Int. 2016, 11, e32. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.A.; Howells, D. Effects of varying training load on heart rate variability and running performance among an olympic rugby sevens team. J. Sci. Med. Sport 2018. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.A.; Esco, M.R.; Allen, J.R.; Robinson, J.B.; Bragg, A.; Keith, C.M.; Fedewa, M.V.; Earley, R.L. Cardiac-autonomic responses to in-season training among division-1 college football players. J. Strength Cond. Res. 2018. [Google Scholar] [CrossRef] [PubMed]
- Atlaoui, D.; Pichot, V.; Lacoste, L.; Barale, F.; Lacour, J.; Chatard, J. Heart rate variability, training variation and performance in elite swimmers. Int. J. Sports Med. 2007, 28, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, L.; Regnard, J.; Parmentier, A.; Mauny, F.; Mourot, L.; Coulmy, N.; Millet, G. Typology of “fatigue” by heart rate variability analysis in elite nordic-skiers. Int. J. Sports Med. 2015, 36, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Le Meur, Y.; Pichon, A.; Schaal, K.; Schmitt, L.; Louis, J.; Gueneron, J.; Vidal, P.; Hausswirth, C. Evidence of parasympathetic hyperactivity in functionally overreached athletes. Med. Sci. Sports Exerc. 2013, 45, 2061–2071. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.; Hornikel, B.; Esco, M. Heart rate variability and psychometric responses to overload and tapering in collegiate sprint-swimmers. J. Sci. Med. Sport 2017, 20, 606–610. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, M. Monitoring training status with HR measures: Do all roads lead to Rome? Front. Physiol. 2014, 5, 73. [Google Scholar] [CrossRef] [PubMed]
- Stanley, J.; Peake, J.M.; Buchheit, M. Cardiac parasympathetic reactivation following exercise: Implications for training prescription. Sports Med. 2013, 43, 1259–1277. [Google Scholar] [CrossRef] [PubMed]
- Plews, D.J.; Laursen, P.B.; Stanley, J.; Kilding, A.E.; Buchheit, M. Training adaptation and heart rate variability in elite endurance athletes: Opening the door to effective monitoring. Sports Med. 2013, 43, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.A.; Esco, M.R.; Allen, J.R.; Robinson, J.B.; Earley, R.L.; Fedewa, M.V.; Bragg, A.; Keith, C.M.; Wingo, J.E. Heart rate variability and training load among national collegiate athletic association division 1 college football players throughout spring camp. J. Strength Cond. Res. 2018. [Google Scholar] [CrossRef] [PubMed]
- Bellenger, C.R.; Karavirta, L.; Thomson, R.L.; Robertson, E.Y.; Davison, K.; Buckley, J.D. Contextualizing parasympathetic hyperactivity in functionally overreached athletes with perceptions of training tolerance. Int. J. Sports Physiol. Perform. 2016, 11, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Saw, A.E.; Main, L.C.; Gastin, P.B. Monitoring the athlete training response: Subjective self-reported measures trump commonly used objective measures: A systematic review. Br. J. Sports Med. 2015. [Google Scholar] [CrossRef] [PubMed]
- Hooper, S.L.; Mackinnon, L.T.; Howard, A.; Gordon, R.D.; Bachmann, A.W. Markers for monitoring overtraining and recovery. Med. Sci. Sports Exerc. 1995, 27, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Hooper, S.L.; Mackinnon, L.T.; Howard, A. Physiological and psychometric variables for monitoring recovery during tapering for major competition. Med. Sci. Sports Exerc. 1999, 31, 1205–1210. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; He, Z.; Zhao, J.; Tao, D.; Xu, K.; Earnest, C.; Mc Naughton, L. Heart rate variability threshold values for early-warning nonfunctional overreaching in elite female wrestlers. J. Strength Cond. Res. 2013, 27, 1511–1519. [Google Scholar] [CrossRef] [PubMed]
- Werner, G.G.; Ford, B.Q.; Mauss, I.B.; Schabus, M.; Blechert, J.; Wilhelm, F.H. High cardiac vagal control is related to better subjective and objective sleep quality. Biol. Psychol. 2015, 106, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-G.; Cheon, E.-J.; Bai, D.-S.; Lee, Y.H.; Koo, B.-H. Stress and heart rate variability: A meta-analysis and review of the literature. Psychiatry Investig. 2018, 15, 235–245. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.; Stoney, C. Depressed mood is related to high-frequency heart rate variability during stressors. Psychosom. Med. 2000, 62, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Esco, M.; Flatt, A.; Nakamura, F. Agreement between a smartphone pulse sensor application and electrocardiography for determining lnrmssd. J. Strength Cond. Res. 2017, 31, 380–385. [Google Scholar] [PubMed]
- Flatt, A.; Esco, M. Heart rate variability stabilization in athletes: Towards more convenient data acquisition. Clin. Physiol. Funct. Imaging 2016, 36, 331–336. [Google Scholar] [CrossRef] [PubMed]
- McLean, B.D.; Coutts, A.J.; Kelly, V.; McGuigan, M.R.; Cormack, S.J. Neuromuscular, endocrine, and perceptual fatigue responses during different length between-match microcycles in professional rugby league players. Int. J. Sports Physiol. Perform. 2010, 5, 367–383. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, R.T.; Strudwick, A.J.; Buchheit, M.; Atkinson, G.; Drust, B.; Gregson, W. The influence of changes in acute training load on daily sensitivity of morning-measured fatigue variables in elite soccer players. Int. J. Sports Physiol. Perform. 2017, 12, S2107–S2113. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Hopkins, W.; Marshall, S.; Batterham, A.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Batterham, A.M.; Hopkins, W.G. Making meaningful inferences about magnitudes. Int. J. Sports Physiol. Perform. 2006, 1, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Gupta, L.; Morgan, K.; Gilchrist, S. Does elite sport degrade sleep quality? A systematic review. Sports Med. 2017, 47, 1317–1333. [Google Scholar] [CrossRef] [PubMed]
- Haddad, H.A.; Parouty, J.; Buchheit, M. Effect of daily cold water immersion on heart rate variability and subjective ratings of well-being in highly trained swimmers. Int. J. Sports Physiol. Perform. 2012, 7, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Ma, R.C.; Kong, A.P.; So, W.Y.; Li, A.M.; Lam, S.P.; Li, S.X.; Yu, M.W.; Ho, C.S.; Chan, M.H. Relationship of sleep quantity and quality with 24-hour urinary catecholamines and salivary awakening cortisol in healthy middle-aged adults. Sleep 2011, 34, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Vgontzas, A.N.; Zoumakis, E.; Bixler, E.O.; Lin, H.-M.; Follett, H.; Kales, A.; Chrousos, G.P. Adverse effects of modest sleep restriction on sleepiness, performance, and inflammatory cytokines. J. Clin. Endocrinol. Metab. 2004, 89, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Beaumont, A.; Burton, A.R.; Lemon, J.; Bennett, B.K.; Lloyd, A.; Vollmer-Conna, U. Reduced cardiac vagal modulation impacts on cognitive performance in chronic fatigue syndrome. PLoS ONE 2012, 7, e49518. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.; Esco, M.; Nakamura, F.; Plews, D. Interpreting daily heart rate variability changes in collegiate female soccer players. J. Sports Med. Phys. Fit. 2017, 57, 907–915. [Google Scholar]
- Baumert, M.; Brechtel, L.; Lock, J.; Hermsdorf, M.; Wolff, R.; Baier, V.; Voss, A. Heart rate variability, blood pressure variability, and baroreflex sensitivity in overtrained athletes. Clin. J. Sport Med. 2006, 16, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, M.; Foster, C.; Dickhuth, H.-H.; Gastmann, U. Autonomic imbalance hypothesis and overtraining syndrome. Med. Sci. Sports Exerc. 1998, 30, 1140–1145. [Google Scholar] [CrossRef] [PubMed]
- Ulrich-Lai, Y.M.; Herman, J.P. Neural regulation of endocrine and autonomic stress responses. Nat. Rev. Neurosci. 2009, 10, 397–409. [Google Scholar] [CrossRef] [PubMed]
- Kumar, Y.; Agarwal, V.; Gautam, S. Heart rate variability during examination stress in medical students. Int. J. Physiol. 2013, 1, 83–86. [Google Scholar]
- Buchheit, M.; Voss, S.; Nybo, L.; Mohr, M.; Racinais, S. Physiological and performance adaptations to an in-season soccer camp in the heat: Associations with heart rate and heart rate variability. Scand. J. Med. Sci. Sports 2011, 21, e477–e485. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.-L.; Yeh, D.-P.; Lee, J.-P.; Chen, C.-Y.; Huang, C.-Y.; Lee, S.-D.; Chen, C.-C.; Kuo, T.B.; Kao, C.-L.; Kuo, C.-H. Parasympathetic nervous activity mirrors recovery status in weightlifting performance after training. J. Strength Cond. Res. 2011, 25, 1546–1552. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.A.; Esco, M.R. Evaluating individual training adaptation with smartphone-derived heart rate variability in a collegiate female soccer team. J. Strength Cond. Res. 2016, 30, 378–385. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Better | Average | Worse |
|---|---|---|---|
| RHR (b·min−1) | |||
| Sleep | 62.0 ± 7.7 * | 63.9 ± 7.7 | 65.6 ± 7.8 |
| Fatigue | 63.0 ± 7.7 | 63.6 ± 7.8 | 64.2 ± 7.8 |
| Soreness | 63.2 ± 7.8 | 63.5 ± 7.7 | 63.8 ± 7.7 |
| Stress | 62.3 ± 7.7 * | 63.9 ± 7.8 | 64.5 ± 7.7 |
| Mood | 61.8 ± 7.7 *¥ | 64.7 ± 7.8 | 64.3 ± 7.6 |
| LnRMSSD | |||
| Sleep | 86.6 ± 7.5 *¥ | 84.1 ± 7.5 * | 81.3 ± 7.6 |
| Fatigue | 85.9 ± 7.9 * | 84.1 ± 7.9 | 82.7 ± 7.9 |
| Soreness | 84.8 ± 7.8 | 84.2 ± 7.7 | 84.2 ± 7.8 |
| Stress | 85.7 ± 7.8 * | 84.3 ± 7.9 | 83.0 ± 7.8 |
| Mood | 86.6 ± 7.7 *¥ | 83.7 ± 7.8 | 82.7 ± 7.7 |
| Parameter | Subject | Sleep | Fatigue | Soreness | Stress | Mood |
|---|---|---|---|---|---|---|
| RHR (b·min−1) | A | −0.56 ** | −0.44 * | −0.51 ** | −0.60 ** | −0.46 * |
| B | −0.22 | −0.20 | 0.11 | −0.33 | −0.05 | |
| C | −0.63 ** | −0.09 | 0.21 | 0.19 | −0.20 | |
| D | −0.67 ** | −0.06 | −0.01 | −0.05 | −0.35 | |
| E | −0.27 | −0.09 | 0.45 * | −0.35 | −0.31 | |
| F | −0.20 | −0.14 | −0.06 | −0.30 | 0.19 | |
| G | 0.18 | −0.12 | −0.30 | 0.17 | 0.03 | |
| H | −0.58 ** | 0.11 | −0.17 | −0.38 * | −0.35 | |
| I | −0.14 | −0.27 | −0.10 | 0.04 | −0.26 | |
| J | 0.05 | 0.06 | 0.15 | −0.02 | 0.06 | |
| K | −0.02 | −0.13 | −0.12 | −0.44 * | −0.27 | |
| L | 0.03 | −0.05 | 0.09 | −0.01 | −0.22 | |
| M | −0.24 | 0.20 | 0.21 | −0.07 | −0.10 | |
| N | 0.23 | 0.12 | −0.14 | 0.29 | 0.14 | |
| O | −0.36 | −0.19 | −0.14 | −0.22 | −0.35 | |
| P | −0.41 * | −0.36 | −0.30 | −0.22 | −0.41 * | |
| Q | −0.07 | −0.49 ** | −0.27 | −0.16 | −0.07 | |
| LnRMSSD | A | 0.49 ** | 0.46 * | 0.27 | 0.55 ** | 0.37 * |
| B | 0.06 | 0.49 ** | 0.01 | 0.43 * | 0.25 | |
| C | 0.61 ** | 0.08 | −0.26 | −0.11 | 0.36 | |
| D | 0.69 ** | 0.24 | 0.02 | 0.12 | 0.25 | |
| E | 0.43 * | 0.27 | 0.01 | 0.45 * | 0.53 ** | |
| F | 0.04 | 0.25 | −0.13 | 0.01 | 0.15 | |
| G | 0.21 | 0.14 | 0.23 | 0.39 * | 0.28 | |
| H | 0.58 ** | −0.08 | 0.03 | 0.45 * | 0.53 ** | |
| I | 0.35 | 0.53 ** | 0.09 | 0.13 | 0.18 | |
| J | −0.06 | −0.16 | −0.16 | −0.23 | −0.22 | |
| K | 0.10 | 0.23 | 0.15 | 0.39 * | 0.25 | |
| L | 0.65 ** | 0.74 ** | −0.05 | 0.10 | 0.41 * | |
| M | 0.47 * | −0.15 | −0.22 | 0.36 | 0.19 | |
| N | 0.07 | 0.24 | 0.40 * | −0.08 | 0.02 | |
| O | 0.32 | 0.34 | 0.15 | 0.23 | 0.50 ** | |
| P | 0.48 ** | 0.30 | 0.47 * | 0.09 | 0.25 | |
| Q | 0.13 | 0.46 * | 0.21 | 0.33 | 0.18 |
| Sleep | Fatigue | Soreness | Stress | Mood | |
|---|---|---|---|---|---|
| Sleep | - | 0.41 | 0.18 | 0.26 | 0.33 |
| Fatigue | 0.41 | - | 0.45 | 0.21 | 0.26 |
| Soreness | 0.18 | 0.45 | - | 0.11 | 0.11 |
| Stress | 0.26 | 0.21 | 0.11 | - | 0.52 |
| Mood | 0.33 | 0.26 | 0.11 | 0.52 | - |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flatt, A.A.; Esco, M.R.; Nakamura, F.Y. Association between Subjective Indicators of Recovery Status and Heart Rate Variability among Divison-1 Sprint-Swimmers. Sports 2018, 6, 93. https://doi.org/10.3390/sports6030093
Flatt AA, Esco MR, Nakamura FY. Association between Subjective Indicators of Recovery Status and Heart Rate Variability among Divison-1 Sprint-Swimmers. Sports. 2018; 6(3):93. https://doi.org/10.3390/sports6030093
Chicago/Turabian StyleFlatt, Andrew A., Michael R. Esco, and Fabio Y. Nakamura. 2018. "Association between Subjective Indicators of Recovery Status and Heart Rate Variability among Divison-1 Sprint-Swimmers" Sports 6, no. 3: 93. https://doi.org/10.3390/sports6030093
APA StyleFlatt, A. A., Esco, M. R., & Nakamura, F. Y. (2018). Association between Subjective Indicators of Recovery Status and Heart Rate Variability among Divison-1 Sprint-Swimmers. Sports, 6(3), 93. https://doi.org/10.3390/sports6030093







