1. Introduction
Acute patellar dislocation represents 2%–3% of all knee injuries in adults and children [
1,
2,
3,
4,
5]. Traditionally, management of patients following primary patellar dislocation has been non-operative, characterized by a short period of immobilization followed by physiotherapy and gradual return to activities [
6,
7]. Recurrent patellar instability has previously been reported in up to 60% of patients following non-operative management, and has prompted some authors to advocate early surgical intervention aimed at reducing the morbidity associated with recurrent instability, including the time lost from activity and the development of early-onset patellofemoral arthritis [
4,
8,
9,
10,
11,
12,
13].
Radiographic assessment of anatomic risk factors for patellar dislocation has traditionally included the use of plain radiographs and computed tomography (CT) [
6,
7]. More recently, magnetic resonance imaging (MRI) has become an important diagnostic tool in the evaluation of patients with patellofemoral instability. Although surgical management of recurrent patellar instability continues to evolve, current techniques aim to correct the anatomic risk factors that appear to predispose patients to patellar instability [
14,
15]. Previous studies have identified morphologic differences between skeletally mature patients with and without patellar instability. Radiographic thresholds that can aid in operative planning have been established based on anatomic differences [
9,
14,
16,
17]. It is largely unknown if these thresholds are applicable to skeletally immature patients, as there are only a limited number of studies reporting radiographic norms in pediatric patients with patellar instability [
15,
18] The purpose of the current study is to report morphological differences between skeletally immature patients with and without acute, lateral patellar instability.
2. Methods
Following the institutional review board (IRB) approval, a retrospective review (August 2009–June 2014) of patients diagnosed with an acute patellar dislocation was performed. Inclusion criteria consisted of skeletally immature patients that had a diagnosis of acute patellar dislocation and had an MRI of the symptomatic knee. The diagnosis of acute patellar dislocation was made clinically with a history and/or physical examination consistent with patellar dislocation. Exclusion criteria included skeletal maturity (defined as closed distal femur physis on plain radiograph and/or MRI), patients with obligatory or habitual patellar instability, and patients who had undergone a previous knee surgery altering their native anatomy (e.g., tibial tubercle transfer, trochleoplasty). A total of 108 patients (108 knees), all between the ages of 9 and 16 years old, were identified. All patients enrolled were skeletally immature with open physes on imaging.
To obtain the control group, a retrospective review of skeletally immature patients presenting between 2002 and 2014, who had undergone MRI imaging to evaluate for knee pathology other than patellar dislocation, was performed. Only MRIs interpreted by a pediatric-trained radiologist as normal or without pathologic features interfering with normal morphology (e.g., popliteal cysts, discoid menisci, and small effusions) were included for analysis. Ten patients were randomly selected at every age within the age range of our acute patellar dislocation study group (9–16 years old) for comparison. This identified a total of 70 patients (70 knees) for analysis (control group).
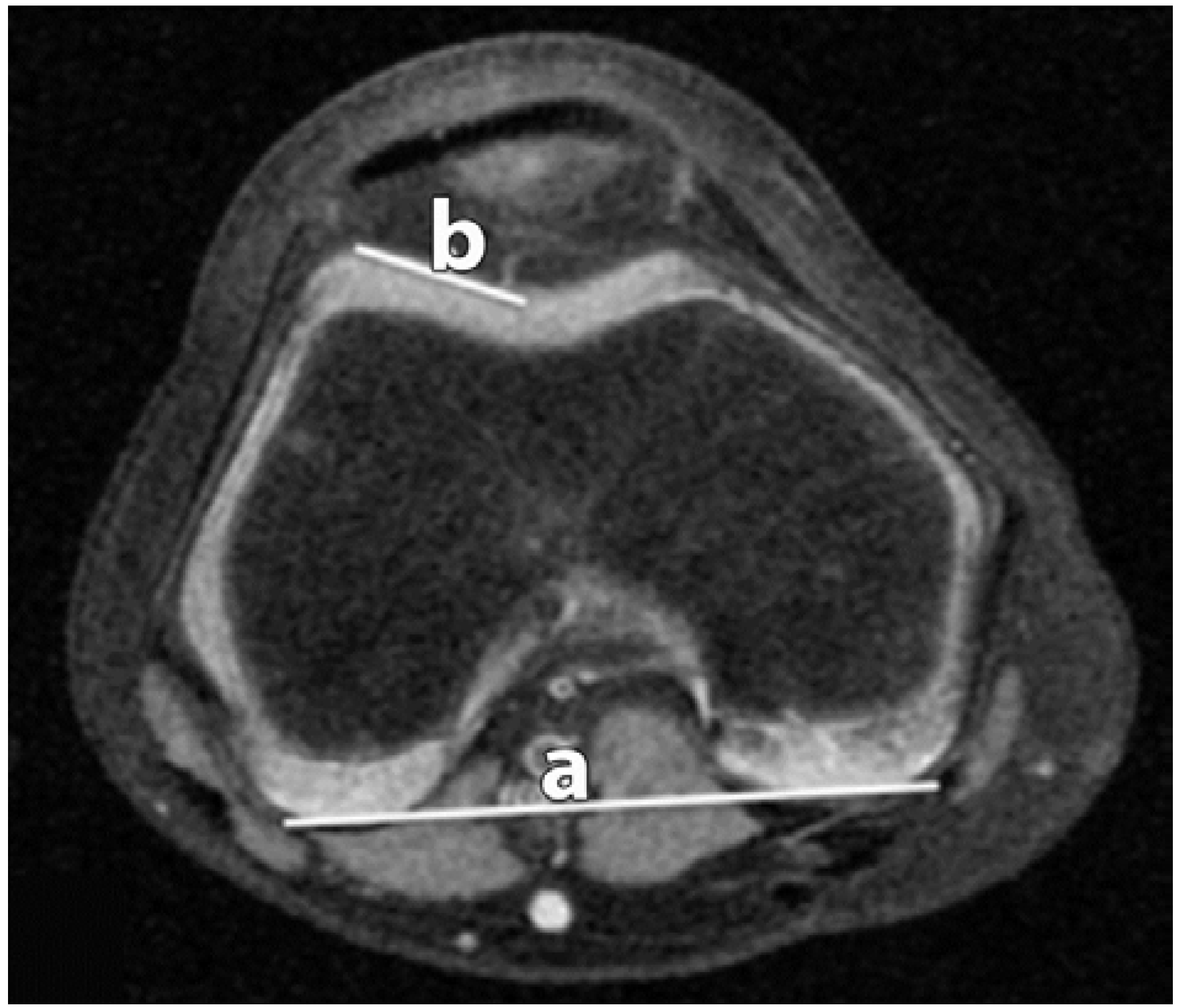
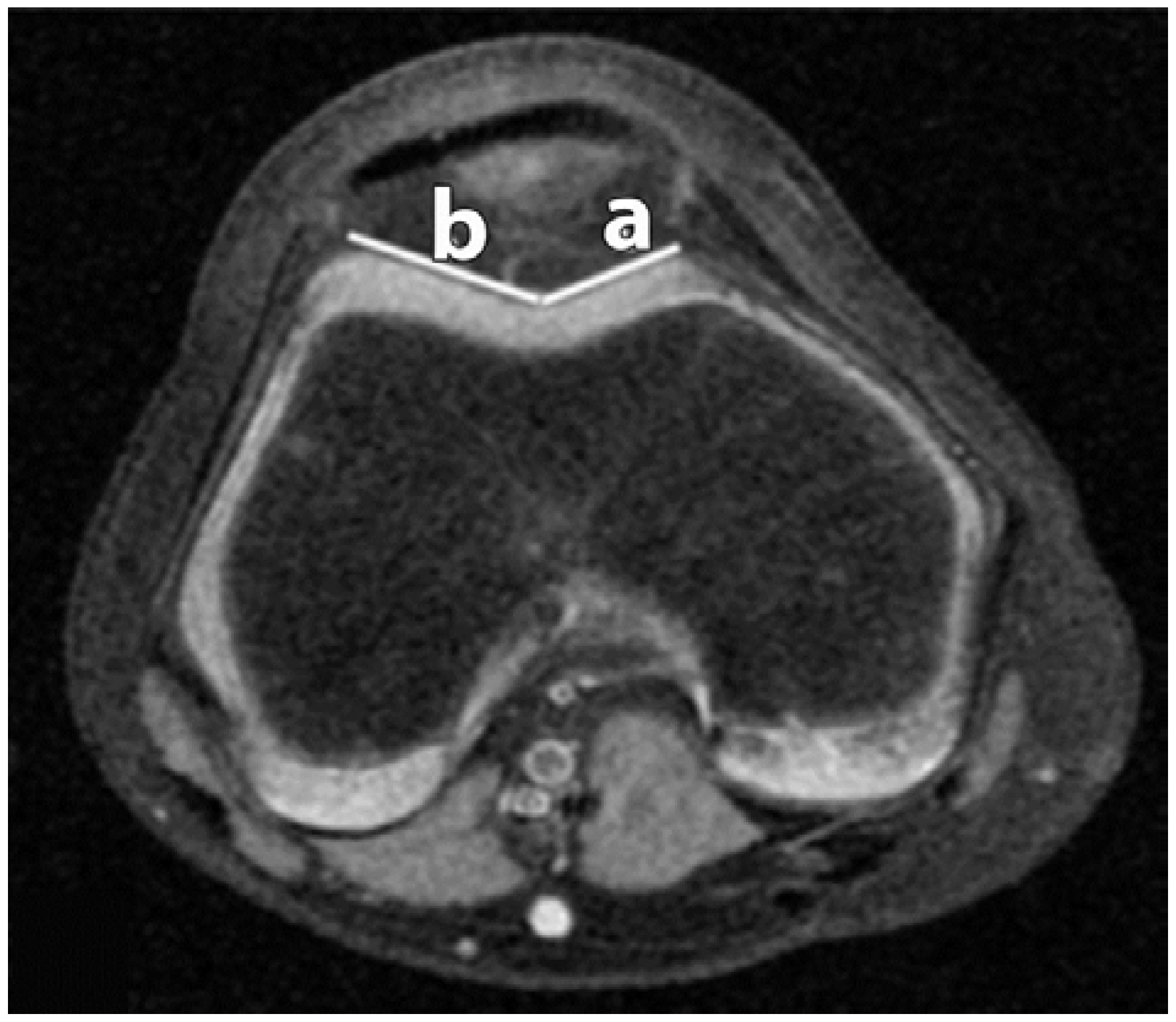
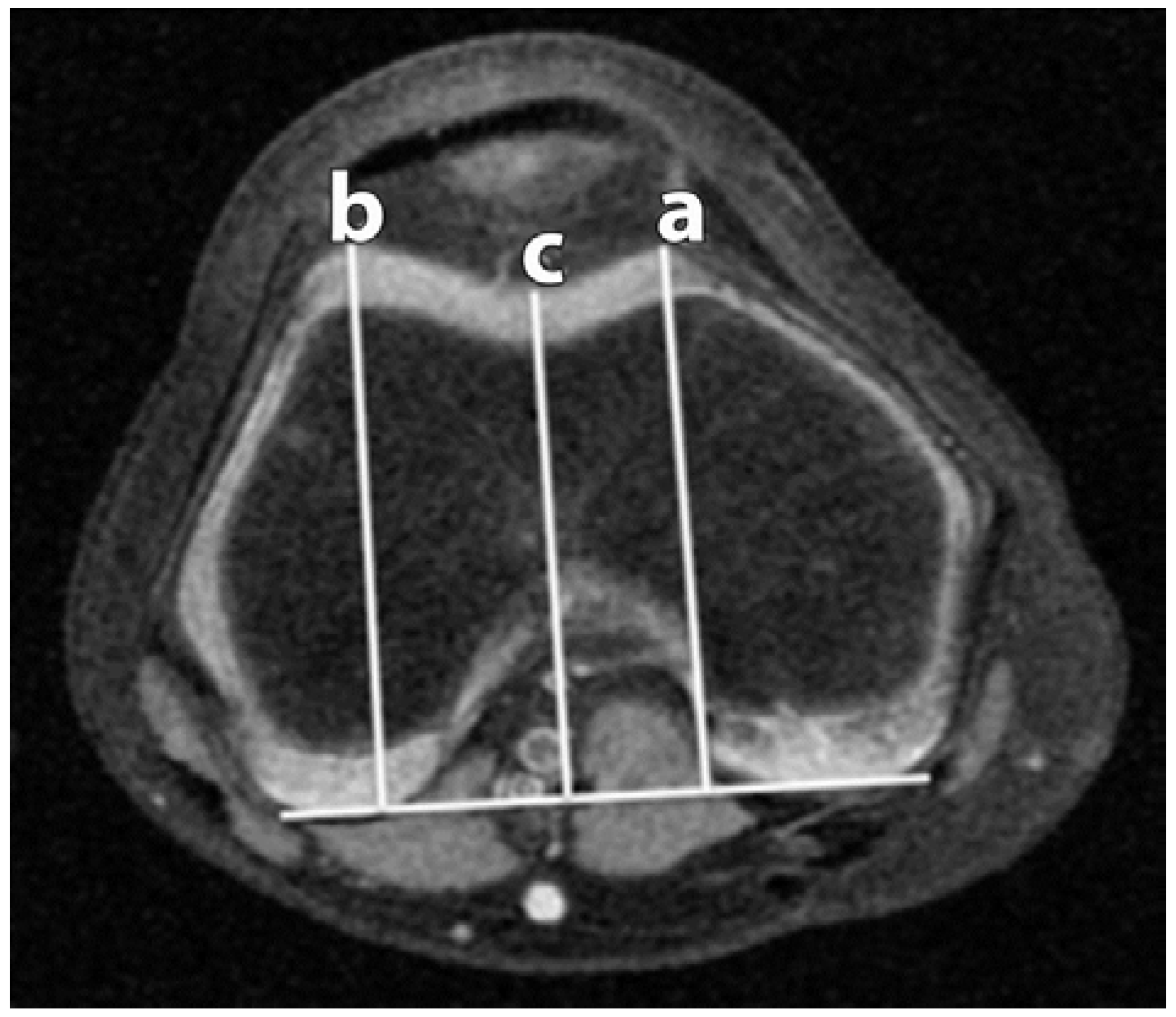
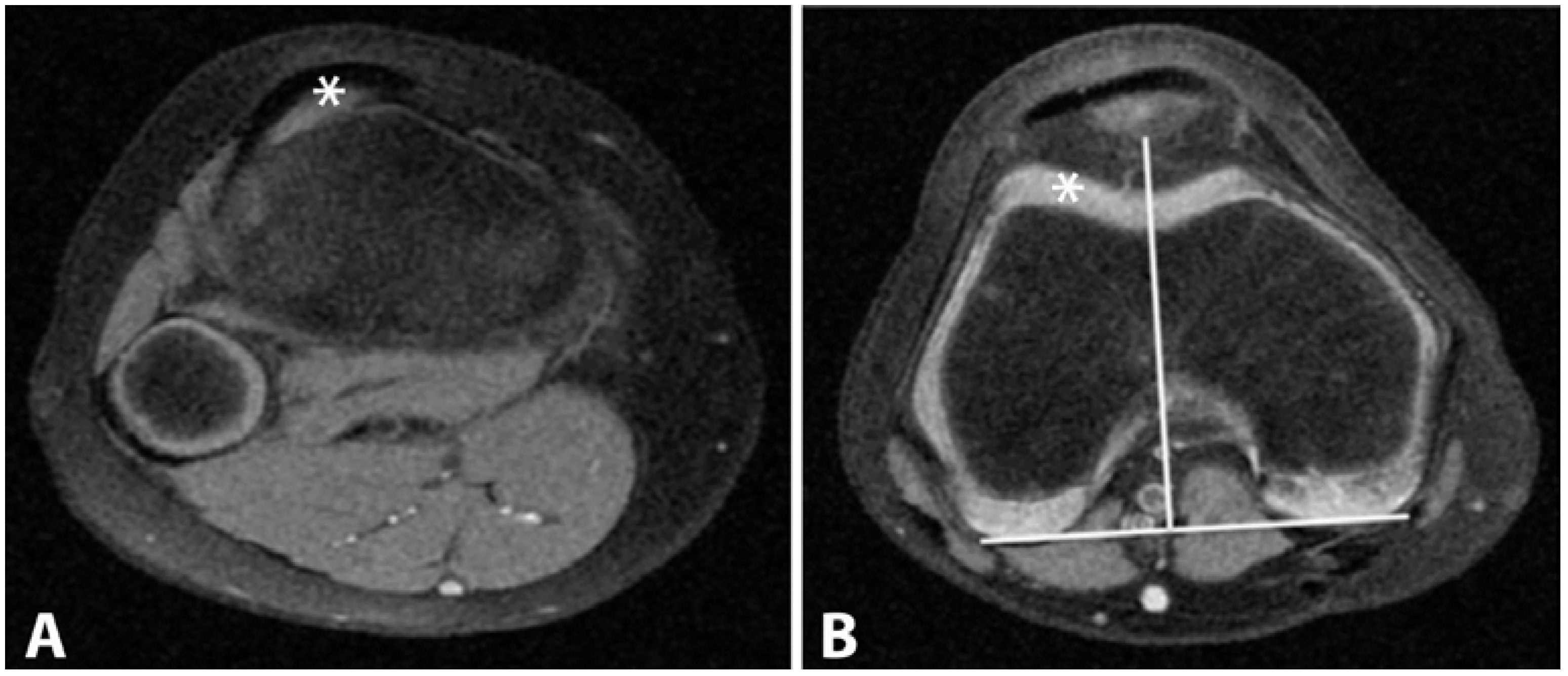
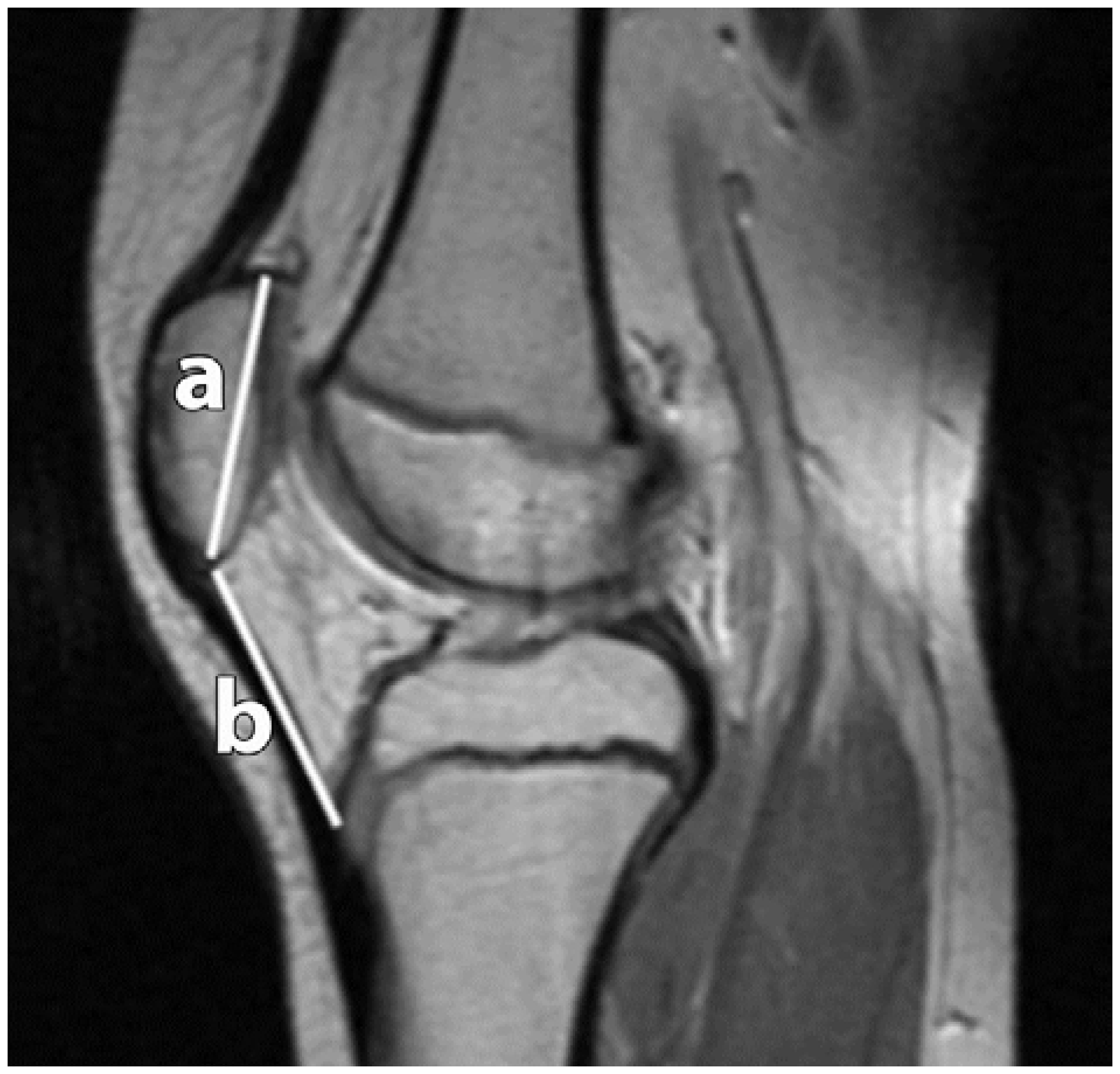
MRI images were obtained at our institution utilizing MRI scanners possessing a magnetic field strength ranging from 1.5 to 3.0 T. A total of six measurements were recorded utilizing either T2 or proton density (PD) sequences: lateral trochlear inclination (LTI), trochlear facet asymmetry (TFA), trochlear depth (TD), tibial tuberosity–trochlear groove (TT–TG), sulcus angle (SA) and patellar height ratio according to Insall-Salvati [
17] (
Figure 1,
Figure 2,
Figure 3,
Figure 4,
Figure 5 and
Figure 6).
These measurements were selected based on their use in previous literature assessing patellofemoral morphology [
5,
17].
Statistical analysis was performed utilizing the StatPlus LE software (AnalystSoft, Walnut, CA, USA) [
19]. All continuous data satisfied the assumption of normality and thus only parametric analysis was performed. Continuous outcome data between study and control groups were analyzed utilizing a two-sample T test. Categorical data between groups were analyzed utilizing a Pearson Chi-square test. Statistical significance was set at
p < 0.05.
3. Results
A total of 178 patients were included for analysis (study:
n = 108, control:
n = 70). The mean age for patients in the study and control groups was 13.7 and 12.1 years, respectively (
p < 0.001). There was no difference in the distribution of males and females (
p = 0.29) or laterality (
p = 0.55) between groups (
Table 1).
All radiographic measurements of interest were obtained in patients comprising the study and control groups. Summarized data is presented in
Figure 7.
Measurements characterizing the morphology of the trochlea (LTI, TFA, TD, and SA) were statistically different between patients in the study and control groups (
Table 2).
Patients in the study group were characterized as having a decreased lateral trochlear inclination (15.6° vs. 20.7°, p < 0.001), increased sulcus angle (150.2° vs. 141.6°, p < 0.001) and an increased trochlear facet asymmetry (2.3 vs. 1.5, p < 0.001). The study group also demonstrated a shallower trochlear groove compared to patients in the control group (3.4 mm vs. 5.6 mm, p ≤ 0.001). The mean TT–TG distance for patients in the study and control groups were 17.0 mm and 8.9 mm, respectively (p < 0.001). A difference in patellar height was also noted between groups with patients in the study group (1.3 ± 0.2 mm) possessing increased patellar height compared to controls (1.1 ± 0.2 mm) (p < 0.001).
4. Conclusions
The purpose of the current study was to examine morphological differences between skeletally immature patients with and without acute, lateral patellar instability. Our findings suggest that anatomic differences in trochlear and patellar morphology may result in an increased risk of acute patellofemoral instability in skeletally immature patients. Previous studies examining patellofemoral instability in adults have suggested that surgical correction of aberrant anatomy may decrease the risk of recurrent instability. Although pathologic thresholds for considering surgical treatment in adults have been proposed [
7,
12,
20], it is unclear if these same thresholds are appropriate for the skeletally immature patient, as normal radiographic parameters used to quantify patellofemoral morphology have yet to be established in this population [
15]. Mundy
et al.[
18] have shown high inter and intraobserver reliability in the utilization of such measurements in the immature knee. In addition, such measurements develop with maturation, gradually reaching adult norms by age 10 [
15,
18].
In a retrospective analysis of patients with and without patellar instability, Charles
et al. [
14] reported significant variations in trochlear morphology using MRI. Although the mean age and the status of the distal femoral/proximal tibial physis of patients examined in this study were not disclosed, patients experiencing recurrent patellar instability were shown to have significant differences in trochlear morphology as assessed by the lateral trochlear inclination, trochlear facet asymmetry, trochlear depth, and sulcus angle. The current study reports similar findings in a subset of skeletally immature patients.
Despite the identified differences in trochlear morphology between skeletally mature and immature patients, the clinical implications as it relates to operative management are currently undefined. Previous literature has reported satisfactory outcomes following trochleoplasty in skeletally mature patients experiencing recurrent instability in the setting of trochlear dysplasia [
21]. There is likely a limited role for this procedure in the pediatric population due to implications associated with physeal arrest. Furthermore, little is known about the post-operative changes in patellofemoral kinematics and its influence on cartilaginous and bony development following a trochleoplasty procedure. Similarly, tibial tubercle transfers cannot be performed until proximal tibial physeal closure has occurred. Stabilization procedures in the skeletally immature knee thus rely on soft tissue procedures which do not disturb growth.
Limitations of the current study are primarily related to its retrospective design. In order to identify patients for the control group, we retrospectively analyzed all patients who underwent MRI imaging of the knee without a history of patellofemoral instability. In doing so, there is inherent selection bias for patients who presented for evaluation of knee pathology. Differences may exist between this group and those asymptomatic patients who would not have undergone MRI evaluation. Additional limitations include the wide age range of patients in both the study and control groups. For the purposes of the current study, patients were categorized as skeletally immature based on the presence of an open distal femoral physis. There is currently a paucity of literature pertaining to age related changes of the patellofemoral joint. It is possible that different stages of development may alter the anatomy in such a way that what would be considered pathologic at one stage of development, but falls into the spectrum of normal during another. Therefore, considering skeletally immature patients as a group makes the assumption that irregular anatomy contributes to the development of patellofemoral instability equally throughout development. Larger studies are needed to further evaluate the possibility of age related changes to the patellofemoral joint and the implications of these changes as it pertains to management of patients with patellar instability.
Despite these limitations, the current study is the first to compare radiographic differences in patellofemoral morphology between skeletally immature patients with and without acute, lateral patellofemoral instability. Results suggest morphologic abnormalities may predispose skeletally immature patients to an increased risk of such injury. Further research is needed to determine the clinical implications of these differences in order to optimize both surgical and non-surgical management of recurrent instability in skeletally immature patients.
Author Contributions
Thai Trinh and Kevin Klingele conceived and designed the experiments; Thai Trinh performed the experiments; Kevin Klingele and Matthew Beran analyzed the data; Kevin Klingele and Matthew Beran contributed patient data and radiographic images; Andrew Mundy wrote the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Apostolovic, M.; Vukomanovic, B.; Slavkovic, N.; Vuckovic, V.; Vukcevic, M.; Djuricic, G.; Kocev, N. Acute patellar dislocation in adolescents: Operative versus nonoperative treatment. Int. Orthop. 2011, 35, 1483–1487. [Google Scholar] [CrossRef] [PubMed]
- Balcarek, P.; Jung, K.; Ammon, J.; Walde, T.A.; Frosch, S.; Schüttrumpf, J.P.; Stürmer, K.M.; Frosch, K.H. Anatomy of lateral patellar instability: Trochlear dysplasia and tibial tubercle-trochlear groove distance is more pronounced in women who dislocate the patella. Am. J. Sports Med. 2010, 38, 2320–2327. [Google Scholar] [CrossRef] [PubMed]
- Fithian, D.C.; Paxton, E.W.; Stone, M.L.; Silva, P.; Davis, D.K.; Elias, D.A.; White, L.M. Epidemiology and natural history of acute patellar dislocation. Am. J. Sports Med. 2004, 32, 1114–1121. [Google Scholar] [CrossRef] [PubMed]
- Lewallen, L.W.; McIntosh, A.L.; Dahm, D.L. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am. J. Sports Med. 2013, 41, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Stefancin, J.J.; Parker, R.D. First-time traumatic patellar dislocation: A systematic review. Clin. Orthop. Relat. Res. 2007, 455, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Dejour, H.; Walch, G.; Neyret, P.; Adeleine, P. Dysplasia of the femoral trochlea. Rev. Chir. Orthop. Reparatr. Appar. Mot. 1990, 76, 45–54. [Google Scholar]
- Dejour, H.; Walch, G.; Nove-Josserand, L.; Guier, C. Factors of patellar instability: An anatomic radiographic study. Knee Surg. Sports Traumatol. Arthrosc. 1994, 2, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Camanho, G.L.; Viegas Ade, C.; Bitar, A.C.; Demange, M.K.; Hernandez, A.J. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy 2009, 25, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Cofield, R.H.; Bryan, R.S. Acute dislocation of the patella: Results of conservative treatment. J. Trauma 1977, 17, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Hansen, E.B.; Frost, B.; Jensen, E.M. The arthrographic picture following anterior dislocation of the shoulder. A consecutive study of 71 patients. Ugeskr. Laeger. 1985, 147, 4193–4195. [Google Scholar] [PubMed]
- Jacobsen, K.; Metz, P. Occult traumatic dislocation of the patella. J. Trauma 1976, 16, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Koeter, S.; Diks, M.J.; Anderson, P.G.; Wymenga, A.B. A modified tibial tubercle osteotomy for patellar maltracking: Results at two years. J. Bone Jt. Surg. Br. 2007, 89, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.O.; Song, F.; Donell, S.T.; Hing, C.B. Operative versus non-operative management of patellar dislocation. A meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 988–998. [Google Scholar] [CrossRef] [PubMed]
- Charles, M.D.; Haloman, S.; Chen, L.; Ward, S.R.; Fithian, D.; Afra, R. Magnetic resonance imaging-based topographical differences between control and recurrent patellofemoral instability patients. Am. J. Sports Med. 2013, 41, 374–384. [Google Scholar] [CrossRef] [PubMed]
- Dickens, A.J.; Morrell, N.T.; Doering, A.; Tandberg, D.; Treme, G. Tibial tubercle-trochlear groove distance: Defining normal in a pediatric population. J. Bone Jt. Surg. Am. 2014, 96, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Dejour, D.; Byn, P.; Ntagiopoulos, P.G. The Lyon’s sulcus-deepening trochleoplasty in previous unsuccessful patellofemoral surgery. Int. Orthop. 2013, 37, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Insall, J.; Goldberg, V.; Salvati, E. Recurrent dislocation and the high-riding patella. Clin. Orthop. Relat. Res. 1972, 88, 67–69. [Google Scholar] [CrossRef] [PubMed]
- Mundy, A.; Ravindra, A.; Yang, J.; Adler, B.H.; Klingele, K.E. Standardization of patellofemoral morphology in the pediatric knee. Pediatr. Radiol. 2015, 46, 255–262. [Google Scholar] [CrossRef] [PubMed]
- AnalystSoft. Available online: http://www.analystsoft.com/en/ (accessed on 14 April 2016).
- Balcarek, P.; Jung, K.; Frosch, K.H.; Sturmer, K.M. Value of the tibial tuberosity–trochlear groove distance in patellar instability in the young athlete. Am. J. Sports Med. 2011, 39, 1756–1761. [Google Scholar] [CrossRef] [PubMed]
- Von Knoch, F.; Bohm, T.; Burgi, M.L.; von Knoch, M.; Bereiter, H. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J. Bone Jt. Surg. Br. 2006, 88, 1331–1335. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).