Incidence of Ulnar Collateral Ligament Surgery and Revision in Baseball Players: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources
Search Methods for Identification of Studies
2.3. Selection Process
2.4. Data Collection Process
2.5. Data Extraction and Data Items
2.6. Risk of Bias in Individual Studies
| Study | Clearly Stated Aim | Consecutive Patients | Prospective Collection Data | Endpoints | Assessment Endpoint | Follow-Up Period | Loss Less than 5% | Study Size | Adequate Control Group | Contemporary Group | Baseline Control | Statistical Analyses | MINORS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Marcus A. Rothermich et al., 2018 [12] | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 12 | ||||
| Marcus A. Rothermich et al., 2021 [11] | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 12 | ||||
| Mason F. Beaudry et al., 2023 [15] | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 1 | 2 | 2 | 2 | 2 | 17 |
| Brandon J. Erickson et al., 2017 [16] | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 1 | 9 | ||||
| Kevin E. Wilk et al., 2014 [17] | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 21 |
| Peter N. Chalmers et al., 2020 [13] | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 1 | 11 |
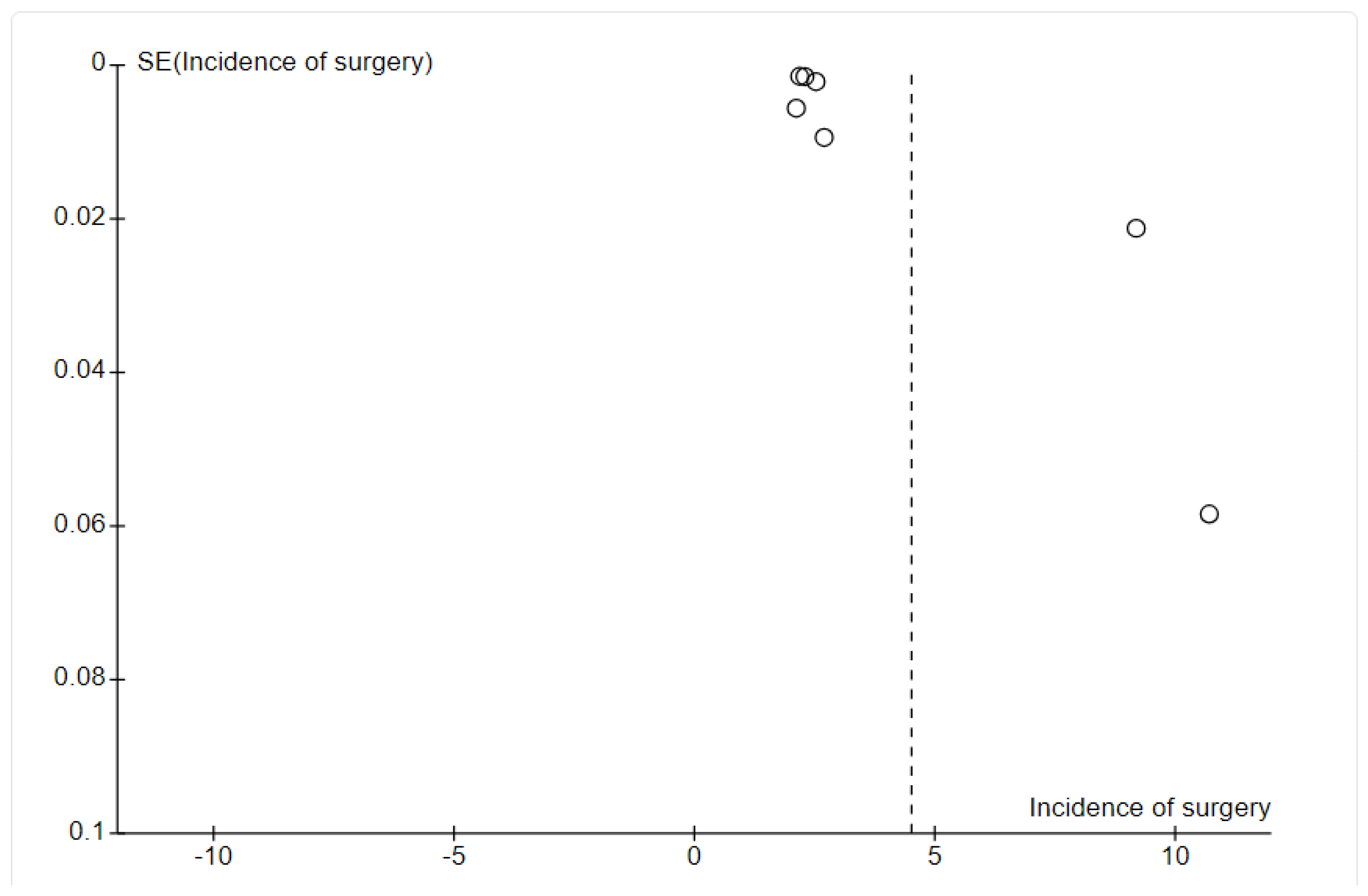
2.7. Publication Bias Assessment
2.8. Summary Measures
- Incidence of UCL surgery: Proportion of baseball players undergoing UCL surgery.
- Incidence of revision UCL surgery: proportion of baseball players undergoing revision UCL surgery.
2.9. Synthesis of Results
3. Results
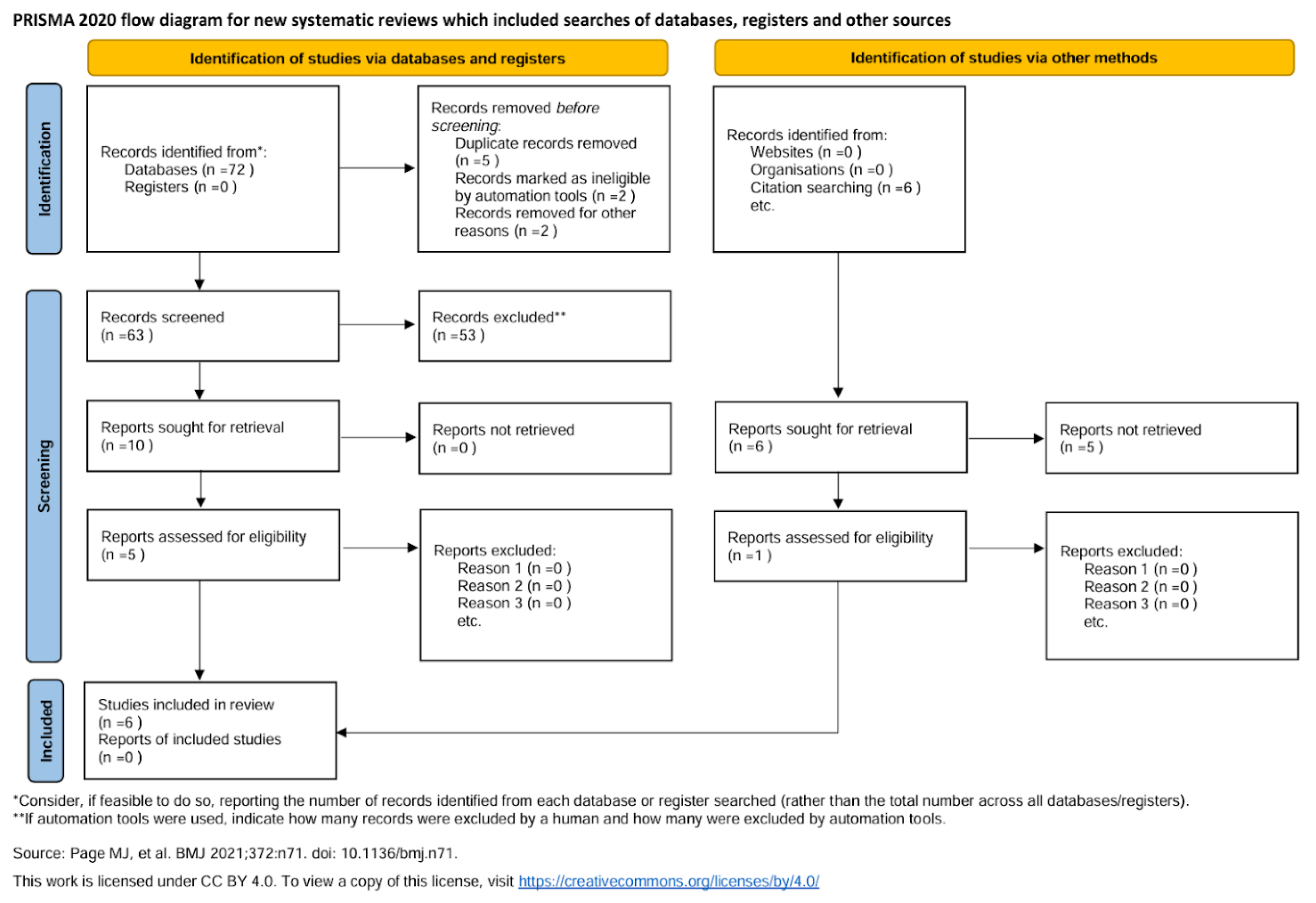
3.1. Study Selection
3.2. Study Characteristics
3.3. Additional Analyses
4. Results
4.1. Study Selection
4.2. Study Characteristics
4.3. Outcomes
4.4. Publication Bias
5. Synthesis of Results
5.1. Assessment of Results
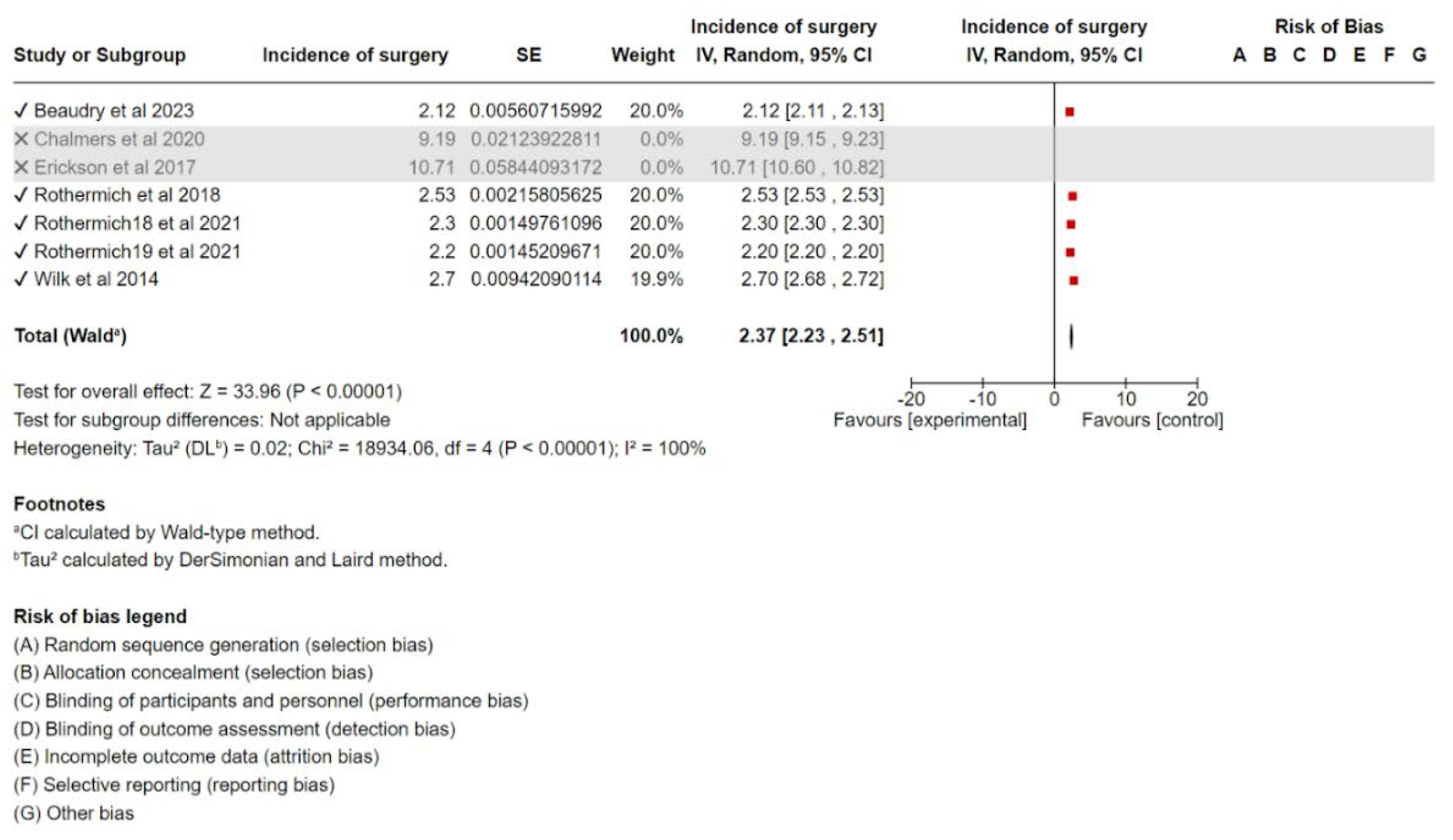
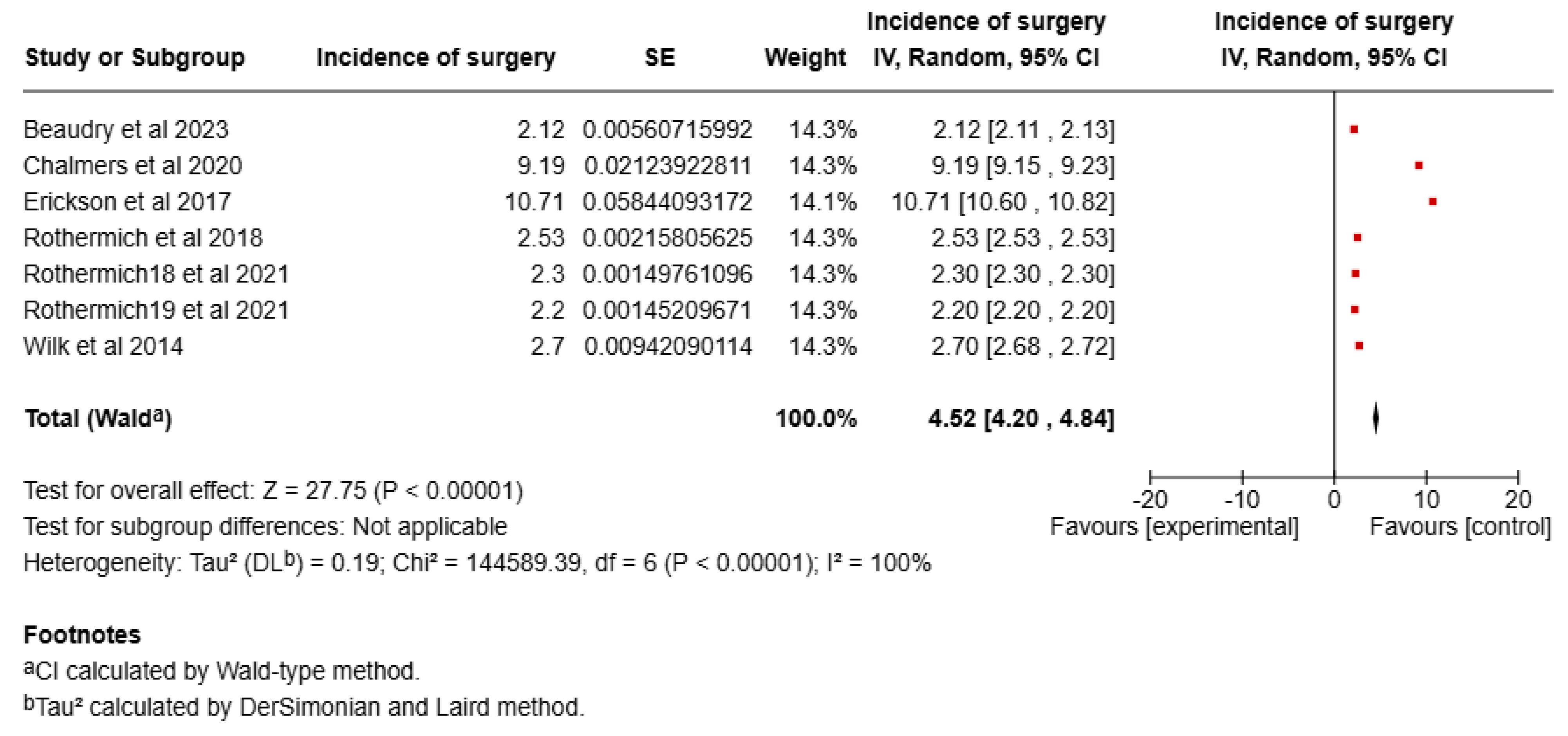
5.1.1. Incidence of UCL Surgery
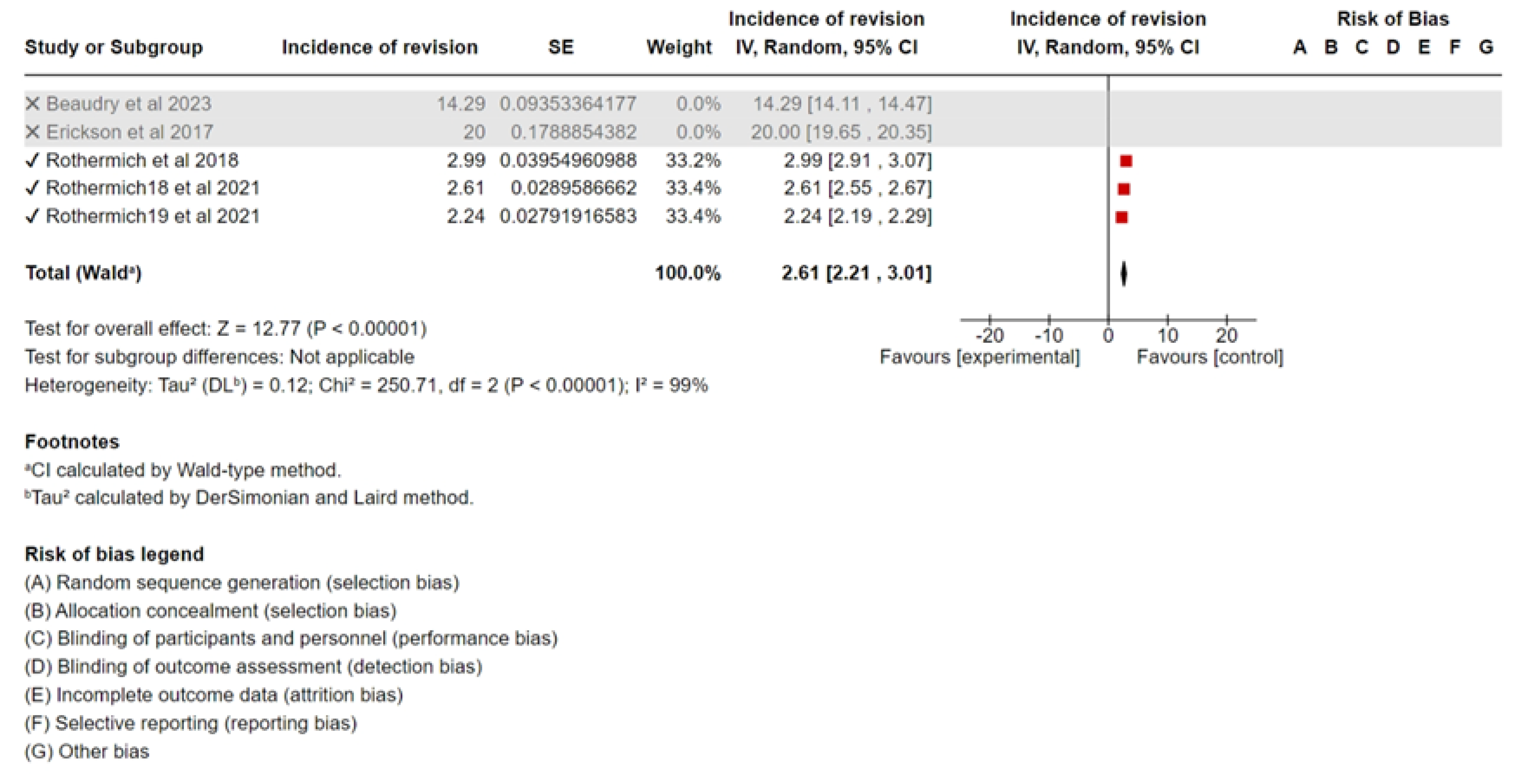
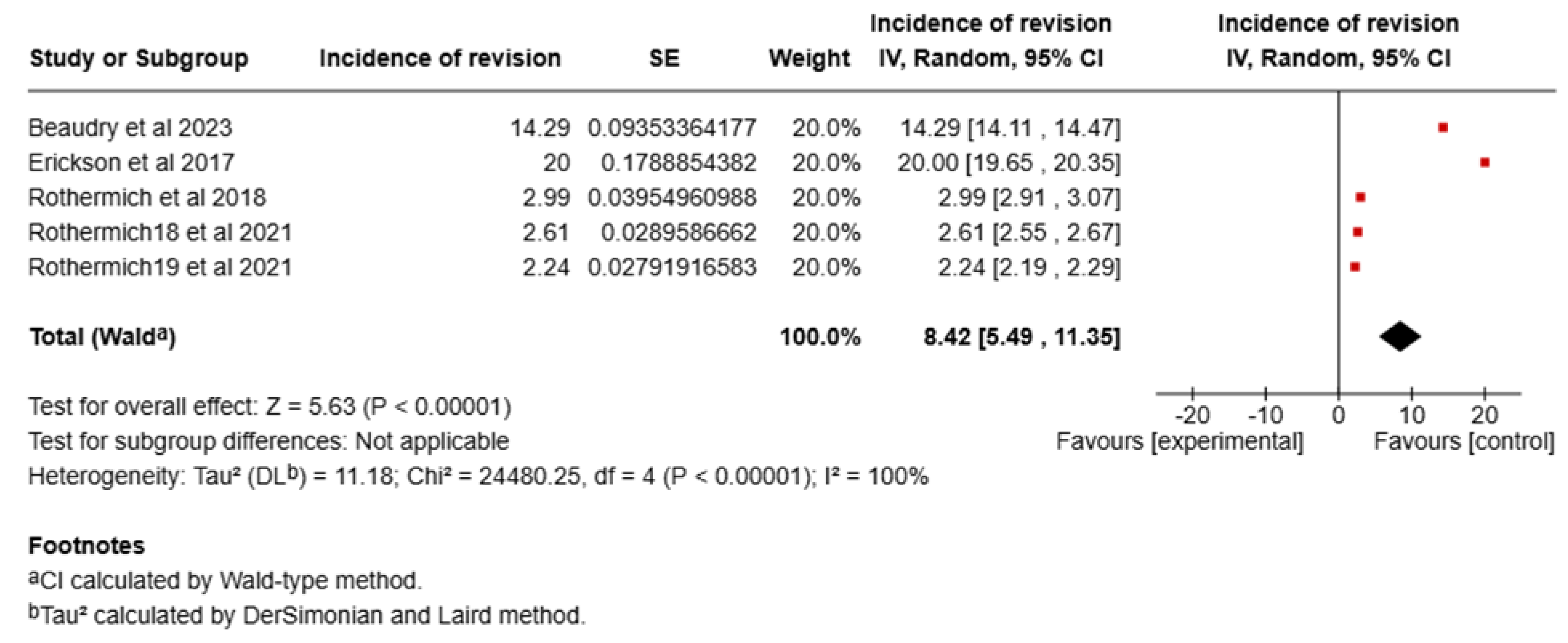
5.1.2. Revision Surgery
5.1.3. Sensitivity Analysis
6. Discussion
7. Limitations
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wilson, A.T.; Pidgeon, T.S.; Morrell, N.T.; DaSilva, M.F. Trends in revision elbow ulnar collateral ligament reconstruction in professional baseball pitchers. J. Hand Surg. 2015, 40, 2249–2254. [Google Scholar] [CrossRef]
- Hodgins, J.L.; Vitale, M.; Arons, R.R.; Ahmad, C.S. Epidemiology of medial ulnar collateral ligament reconstruction: A 10-year study in New York State. Am. J. Sports Med. 2016, 44, 729–734. [Google Scholar] [CrossRef]
- Erickson, B.J.; Nwachukwu, B.U.; Rosas, S.; Schairer, W.W.; McCormick, F.M.; Bach, B.R., Jr.; Romeo, A.A. Trends in medial ulnar collateral ligament reconstruction in the United States: A retrospective review of a large private-payer database from 2007 to 2011. Am. J. Sports Med. 2015, 43, 1770–1774. [Google Scholar] [CrossRef]
- Meldau, J.E.; Srivastava, K.; Okoroha, K.R.; Ahmad, C.S.; Moutzouros, V.; Makhni, E.C. Cost analysis of Tommy John surgery for Major League Baseball teams. J. Shoulder Elb. Surg. 2020, 29, 121–125. [Google Scholar] [CrossRef]
- Carr, J.B., II; Wilson, L.; Sullivan, S.W.; Poeran, J.; Liu, J.; Memtsoudis, S.G.; Nwachukwu, B.U. Revision ulnar collateral ligament reconstruction in professional baseball: Current trends, surgical techniques, and outcomes. Orthop. J. Sports Med. 2020, 7, 2325967119864104. [Google Scholar] [CrossRef]
- Camp, C.L.; Conte, S.; D’Angelo, J.; Fealy, S.A. Epidemiology of ulnar collateral ligament reconstruction in Major and Minor League Baseball pitchers: Comprehensive report of 1429 cases. J. Shoulder Elb. Surg. 2018, 27, 871–878. [Google Scholar] [CrossRef]
- Conte, S.A.; Fleisig, G.S.; Dines, J.S.; Wilk, K.E.; Aune, K.T.; Patterson-Flynn, N.; ElAttrache, N. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am. J. Sports Med. 2015, 43, 1764–1769. [Google Scholar] [CrossRef]
- Leland, D.P.; Conte, S.; Flynn, N.; Conte, N.; Crenshaw, K.; Wilk, K.E.; Camp, C.L. Prevalence of medial ulnar collateral ligament surgery in 6135 current professional baseball players: A 2018 update. Orthop. J. Sports Med. 2019, 7, 2325967119871442. [Google Scholar] [CrossRef]
- Erickson, B.J.; Gupta, A.K.; Harris, J.D.; Bush-Joseph, C.; Bach, B.R.; Abrams, G.D.; San Juan, A.M.; Cole, B.J.; Romeo, A.A. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am. J. Sports Med. 2014, 42, 536–543. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: Updated guidelines for reporting systematic reviews and meta-analyses. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Rothermich, M.A.; Fleisig, G.S.; Conte, S.A.; Hart, K.M.; Cain, E.L., Jr.; Dugas, J.R. Short-term trends in elbow ulnar collateral ligament surgery in collegiate baseball players: An analysis of 25,587 player-years. Orthop. J. Sports Med. 2021, 9, 23259671211016846. [Google Scholar] [CrossRef]
- Rothermich, M.A.; Conte, S.A.; Aune, K.T.; Fleisig, G.S.; Cain, E.L., Jr.; Dugas, J.R. Incidence of elbow ulnar collateral ligament surgery in collegiate baseball players. Orthop. J. Sports Med. 2018, 6, 2325967118764657. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, S.N.; English, J.; Cushman, D.; Yoon, S.H.; Schulz, B.M.; Li, B. The ulnar collateral ligament responds to stress in professional pitchers. Orthop. J. Sports Med. 2020, 8, 2325967120S0013. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Beaudry, M.F.; Beaudry, A.G.; Bradley, J.P.; Haynes, D.E.; Holland, G.; Edwards, A.; Chetlin, R.D. Comparison of the “tall and fall” versus “drop and drive” pitching styles: Analysis of Major League Baseball pitchers during a single season. Orthop. J. Sports Med. 2023, 11, 23259671231173691. [Google Scholar] [CrossRef] [PubMed]
- Erickson, B.J.; Chalmers, P.N.; Axe, M.J.; Romeo, A.A. Exceeding pitch count recommendations in little league baseball increases the chance of requiring Tommy John surgery as a professional baseball pitcher. Orthop. J. Sports Med. 2017, 5, 2325967117695085. [Google Scholar] [CrossRef]
- Wilk, K.E.; Macrina, L.C.; Fleisig, G.S.; Aune, K.T.; Porterfield, R.A.; Harker, P.; Andrews, J.R. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: A prospective study. Am. J. Sports Med. 2014, 42, 2075–2081. [Google Scholar] [CrossRef]
- Cain, E.L., Jr.; Andrews, J.R.; Dugas, J.R.; Wilk, K.E.; McMichael, C.S.; Walter, J.C., II; Arthur, S.T. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: Results in 743 athletes with minimum 2-year follow-up. Am. J. Sports Med. 2010, 38, 2426–2434. [Google Scholar] [CrossRef]
- Fleisig, G.S.; Andrews, J.R.; Dillman, C.J.; Escamilla, R.F. Kinetics of baseball pitching with implications about injury mechanisms. Am. J. Sports Med. 1995, 23, 233–239. [Google Scholar] [CrossRef]
- Ahmad, C.S.; Lee, T.Q.; ElAttrache, N.S. Biomechanical evaluation of a new ulnar collateral ligament reconstruction technique with interference screw fixation. Am. J. Sports Med. 2003, 31, 332–337. [Google Scholar] [CrossRef]
- Azar, F.M.; Andrews, J.R.; Wilk, K.E.; Groh, D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am. J. Sports Med. 2000, 28, 16–23. [Google Scholar] [CrossRef]
- Conway, J.E.; Jobe, F.W.; Glousman, R.E.; Pink, M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J. Bone Jt. Surg. Am. 1992, 74, 67–83. [Google Scholar] [CrossRef]
- Fleisig, G.S.; Kingsley, D.S.; Loftice, J.W.; Dinnen, K.P.; Ranganathan, R.; Dun, S.; Andrews, J.R. Kinetic comparison among the fastball, curveball, change-up, and slider in collegiate baseball pitchers. Am. J. Sports Med. 2006, 34, 423–430. [Google Scholar] [CrossRef]
- Hechtman, K.S.; Tjin-A-Tsoi, E.W.; Zvijac, J.E.; Uribe, J.W.; Latta, L.L. Biomechanics of a less invasive procedure for reconstruction of the ulnar collateral ligament of the elbow. Am. J. Sports Med. 1998, 26, 620–624. [Google Scholar] [CrossRef]
- Lyman, S.; Fleisig, G.S.; Andrews, J.R.; Osinski, E.D. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am. J. Sports Med. 2002, 30, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Petty, D.H.; Andrews, J.R.; Fleisig, G.S.; Cain, E.L. Ulnar collateral ligament reconstruction in high school baseball players: Clinical results and injury risk factors. Am. J. Sports Med. 2004, 32, 1158–1164. [Google Scholar] [CrossRef] [PubMed]
- Conte, S.; Camp, C.L.; Dines, J.S. Injury trends in Major League Baseball over 18 seasons: 1998–2015. Am. J. Orthop. 2016, 45, 116–123. [Google Scholar] [PubMed]
- Puga, T.; Scigliano, N.M.; Box, M.W.; Riehl, J.T. The major league baseball pitch clock: One year position player injury analysis. Physician Sportsmed. 2024, 53, 147–151. [Google Scholar] [CrossRef]
- Pescatore, S.M.; DeShazo, S.J.; Weiss, W.M. Frequency of Tommy John surgery in NCAA Division I college pitchers versus weather conditions. Orthop. J. Sports Med. 2025, 13, 23259671241311601. [Google Scholar] [CrossRef]
- Zaremski, J.L.; Horodyski, M.; Donlan, R.M.; Brisbane, S.T.; Farmer, K.W. Does geographic location matter on the prevalence of ulnar collateral ligament reconstruction in collegiate baseball pitchers? Orthop. J. Sports Med. 2015, 3, 2325967115616582. [Google Scholar] [CrossRef]
- Zaremski, J.L.; McClelland, J.; Vincent, H.K.; Horodyski, M. Trends in sports-related elbow ulnar collateral ligament injuries. Orthop. J. Sports Med. 2017, 5, 2325967117731296. [Google Scholar] [CrossRef]
- Carr, J.B., II; Wilson, L.; Sullivan, S.W.; Poeran, J.; Liu, J.; Memtsoudis, S.G.; Nwachukwu, B.U. Seasonal and monthly trends in elbow ulnar collateral ligament injuries and surgeries: A national epidemiological study. JSES Rev. Rep. Tech. 2022, 2, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Zaremski, J.; Bowers, R.L.; Pazik, M. The Tommy John Epidemic: A 50 year analysis of UCL surgeries using publicly available data in professional baseball. Clin. J. Sport Med. 2024, 34, 177–245. [Google Scholar]
- Prodromo, J.; Patel, N.; Kumar, N.; Denehy, K.; Tabb, L.P.; Tom, J. Pitch characteristics before ulnar collateral ligament reconstruction in major league pitchers compared with age-matched controls. Orthop. J. Sports Med. 2016, 4, 2325967116653946. [Google Scholar] [CrossRef] [PubMed]
- Zaremski, J.L.; Pazik, M.; Hunt, H.; Dodd, W.S.; Nguyen, B.K.; Farmer, K.W.; Horodyski, M. UCL throwing injuries in nonprofessional baseball players: A 14-year retrospective study. Sports Health 2024, 17, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Almonroeder, T.; Jones, M.T.; Fields, J.B.; Erickson, J.L.; Taylor, W.A.; Bittner, M.H.; Jagim, A.R. Examining changes in ulnar collateral ligament reconstruction surgery patterns among professional baseball players. Clin. J. Sport Med. 2024, 35, 465–470. [Google Scholar] [CrossRef]

| Region | Type of Study | Years Studied | Age | USAplayer% | Type Surgery | Season (Moment) | Position | Revision | Incidence of Surgery | Hand | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Marcus A. Rothermich et al., 2018 [12] | USA | Descriptive epidemiology study | 2016–2017 season | 19.7 years. (Age at which surgery was performed) | 132/133 (one of them unknown) | Reconstruction: 83.8% (83/99) Repair: 16.2% (16/99) (35/134 total type of surgery unknown) | In-season: 65/134; 48.5% Postseason, offseason, and preseason: 69/134; 51.0% | PP: 19/134; 14.18% Pitchers:(115/134; 85.8%) | 4/134 | 134/5295 (2.54%) | Dominant extremity: (133/134; 99.2%) |
| Marcus A. Rothermich et al., 2021 [11] | USA | Descriptive epidemiology study | 2016–2019 | 19.9 years (19.7 years in 2017, 20.0 years in 2018, and 19.8 years in 2019). | 583/587 USA | UCLR (572/587) players (112/570) UCL repair | In-season 49%-16 to 17 41%-17 to 18 38%-18 to 19; postseason, offseason, and preseason 51%-16 to 17 59%-17 to 18 62%-18 to 19 | PP: 19/2757 in 2017, 36/5172 in 2018, and 37/5233 in 2019 Pitchers: 4.4% in 2017 (115/2607), 4.0% in 2018 (194/4847), and 3.7% in 2019 (186/4971). | revision rate in 2017 (4/134), 2.6% in 2018 (6/230), and 2.24% in 2019 (5/223). | (587/25,587)-2.3% 17, 18, 19 2.5% in 2017 (134/5364), 2.3% in 2018 (230/10,019), 2.2% in 2019 (223/10,204) | Dominant extremity (586/587; 99.8%). season 2016 to 2017: 133/134 |
| Mason F. Beaudry et al., 2023 [15] | USA | Cross-sectional study | 2019 season | age, 27.39 ± 3.51 years * | USANR | Surgery 11 + 3-Reconstruction 10 + 2 -Other surgeries 1 + 1 other 2/660 | NR (not reported) | Pitchers (MLB) | 2/660 reinjury (2019) | 14/660 (total UCL surgery) -UCLR: 12/660 -Other surgeries: 2/660 | Right-handed 311 -TF 177-DD Left-handed 101-TF 71-DD ** |
| Brandon J. Erickson et al., 2017 [16] | USA | Cohort study | 2001–2009 | 11–13 years * | USA 306/638 4.0% [1/25] UCLR Other nationality 332/638 5.4% [2/37] UCLR | NR | NR | Baseball players (Pitcher and PP) | Revision 1/2 pitcher MiLB 0/3MLB | 1/3 MBL pitcher 2/25 MiBL pitcher (LLWS that played in MLB) 33%(1/3) required UCLR 8% (2/25) (LLWS that played in MiLB) | NR |
| Kevin E. Wilk et al., 2014 [17] | USA | Cohort study | 2005–2012 | Overall 24.7 ± 4.1 Elbow Injury 25.0 ± 4.2 No Elbow Injury 24.7 ± 4.1 | NR | NR | NR | NR | NR | 8/296 surgery 3/296 UCLR (2 loose-body removals, 2 ulnar nerve transposition, 1 open reduction internal fixation) | NR |
| Peter N. Chalmers et al., 2020 [13] | USA | Prospective study | pre-2018–post-2018–pre-2019 season | 23 years old (pitchers) | NR | NR | NR | Pitchers | NR | 17/185 UCLR (pre-2018 to pre-2019). Pre-2018 to post-2018: 10/185 UCLR. Post-2018 to pre-2019: 7/185 UCLR | 36/185 left 148/185 right ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sáez, A.; Mariscal, G.; Barrios, C. Incidence of Ulnar Collateral Ligament Surgery and Revision in Baseball Players: A Systematic Review and Meta-Analysis. Sports 2025, 13, 299. https://doi.org/10.3390/sports13090299
Sáez A, Mariscal G, Barrios C. Incidence of Ulnar Collateral Ligament Surgery and Revision in Baseball Players: A Systematic Review and Meta-Analysis. Sports. 2025; 13(9):299. https://doi.org/10.3390/sports13090299
Chicago/Turabian StyleSáez, Alberto, Gonzalo Mariscal, and Carlos Barrios. 2025. "Incidence of Ulnar Collateral Ligament Surgery and Revision in Baseball Players: A Systematic Review and Meta-Analysis" Sports 13, no. 9: 299. https://doi.org/10.3390/sports13090299
APA StyleSáez, A., Mariscal, G., & Barrios, C. (2025). Incidence of Ulnar Collateral Ligament Surgery and Revision in Baseball Players: A Systematic Review and Meta-Analysis. Sports, 13(9), 299. https://doi.org/10.3390/sports13090299