Abstract
Background: The UK Department for Digital, Culture, Media, and Sport (DCMS) grassroots concussion guidance, May 2023, advised that all community-based sport-related concussions (SRCs) be diagnosed by a healthcare practitioner. This may require that general practitioners (GPs) diagnose and manage SRCs. Diagnosing SRCs in primary care settings in the United Kingdom (UK) presents significant challenges, primarily due to the lack of validated tools specifically designed for general practitioners (GPs). This scoping review aims to identify diagnostic and management tools for SRCs in grassroots sports and primary care settings. Aims: To identify tools that can be used by GPs to diagnose and manage concussions in primary care, both adult and paediatric populations. Design and Methods: A scoping review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScRs). Five databases (MEDLINE, EMBASE, CINAHL, Cochrane Library, Google Scholar) were searched from 1946 to April 2025. Search terms included “concussion”, “primary care”, and “diagnosis”. Studies that discussed SRCs in community or primary care settings were included. Those that exclusively discussed secondary care and elite sports were excluded, as well as non-English studies. Two reviewers independently screened titles, abstracts, and full texts, with a third resolving any disagreements. Data were extracted into Microsoft Excel. Studies were assessed for quality using the Joanna Briggs critical appraisal tools and AGREE II checklist. Results: Of 727 studies, 12 met the inclusion criteria. Identified tools included Sport Concussion Assessment Tool 6 (SCAT6, 10–15 min, adolescent/adults), Sport Concussion Office Assessment Tool 6 (SCOAT6, 45–60 min, multidisciplinary), the Buffalo Concussion Physical Examination (BCPE, 5–6 min, adolescent-focused), and the Brain Injury Screening Tool (BIST, 6 min, ages 8+). As part of BCPE, a separate Telehealth version was developed for remote consultations. SCAT6 and SCOAT6 are designed for healthcare professionals, including GPs, but require additional training and time beyond typical UK consultation lengths (9.2 min). BIST and BCPE show promise but require UK validation. Conclusions: SCAT6, SCOAT6, BIST, and BCPE could enhance SRC care, but their feasibility in UK primary care requires adaptation (e.g., integration with GP IT systems and alignment with NICE guidelines). Further research is required to validate these tools and assess additional training needs.
1. Introduction
SRC, defined as a “traumatic brain injury caused by a direct blow to the head, neck or body resulting in an impulsive force being transmitted to the brain” [1], is a growing concern in grassroots sports. Characterised by non-specific symptoms that evolve over days, SRC lacks a definitive diagnostic test, posing challenges for timely and accurate assessment [1]. In the UK, the 2023 DCMS grassroots concussion guidance mandates that all community SRC cases be diagnosed by healthcare practitioners [2], increasingly directing patients to GPs via self-referral, 111 triage, or emergency departments. This policy is a response to a 2021 DCMS inquiry highlighting the absence of community-specific guidelines, variable clinician knowledge, and inadequate data collection, contributing to mismanagement, such as inappropriate return-to-play decisions [3].
GPs, often the initial point of contact for health issues [4], encounter significant barriers in delivering effective care. Rising workloads, a 19% increase from 2015 to 2023 [5], and brief consultation times (averaging 9.2 min in the UK) [6] limit patient-to-doctor time and primary care consultations. A survey of Irish GPs revealed that while most encounter SRC cases (1–5 annually), only 10% have had formal training in concussion diagnosis and management. In concussion diagnosis and management, indeed, three-quarters of these GPs provided return-to-play (RTP) guidance despite only 10% reporting adequate knowledge of RTP protocols [4]. Worryingly, one-fifth advised immediate return to play when patients were asymptomatic, without using any RTP protocol [4]. This indicates the need for accessible tools and education, particularly for paediatric and adult presentations with differing symptom profiles [7]. Tools like Sport Concussion Assessment Tool 6 (SCAT6, adolescents/adults, 10–15 min) and Sport Concussion Office Assessment Tool 6 (SCOAT6, subacute, 45–60 min), designed for healthcare professionals, including GPs, are time intensive and training dependent, reducing practicality in routine practice [8,9].
This scoping review seeks to identify diagnostic and management tools for SRCs suitable for use by GPs in primary care, for both adult and paediatric populations. By addressing the gap in UK-validated tools, it aims to support standardised care, enhance data collection, and improve patient outcomes in a resource-constrained environment.
2. Methods
This scoping review adhered to the Arksey and O’Malley framework [10,11] and PRISMA-ScR guidelines [12] (see Supplementary S1), although no formal protocol was registered.
Research Question:
What tools are used internationally for the diagnosis and management of SRCs in grassroots sports, primary care, and the community for adult and paediatric populations?
Search Strategy:
Five databases (MEDLINE, EMBASE, CINAHL, Cochrane Library, Google Scholar) were searched from 1946 to April 2025, with assistance from a medical librarian specialising in medical research to ensure a comprehensive search was conducted.
Key terms included (concussion OR head injury OR mild traumatic head injury) AND (grassroot OR community OR primary care OR non elite OR clinic OR accident and emergency OR emergency department) AND (assessment OR diagnosis OR monitoring)
Google Scholar searches used broader terms (e.g., concussion community assessment tool).
Inclusion: Studies discussing SRC diagnosis/management, conducted in primary care/grassroots settings, including adult/paediatric populations, published in English
Exclusion: Studies exclusively in secondary care/elite sports, non-original research (e.g., reviews, editorials), not published in English, or inaccessible full texts.
Data Extraction and Quality Assessment:
Data were extracted into Microsoft Excel, including author, year, time, study design, population, tools and target population, and management recommendations (see Table 1). Study quality was assessed using the Joanna Briggs critical appraisal tools and AGREE II checklists [13,14]. Bias was minimised through independent review and predefined criteria.

Table 1.
Summary of studies included.
3. Results: Evaluation of Guidelines and Tools
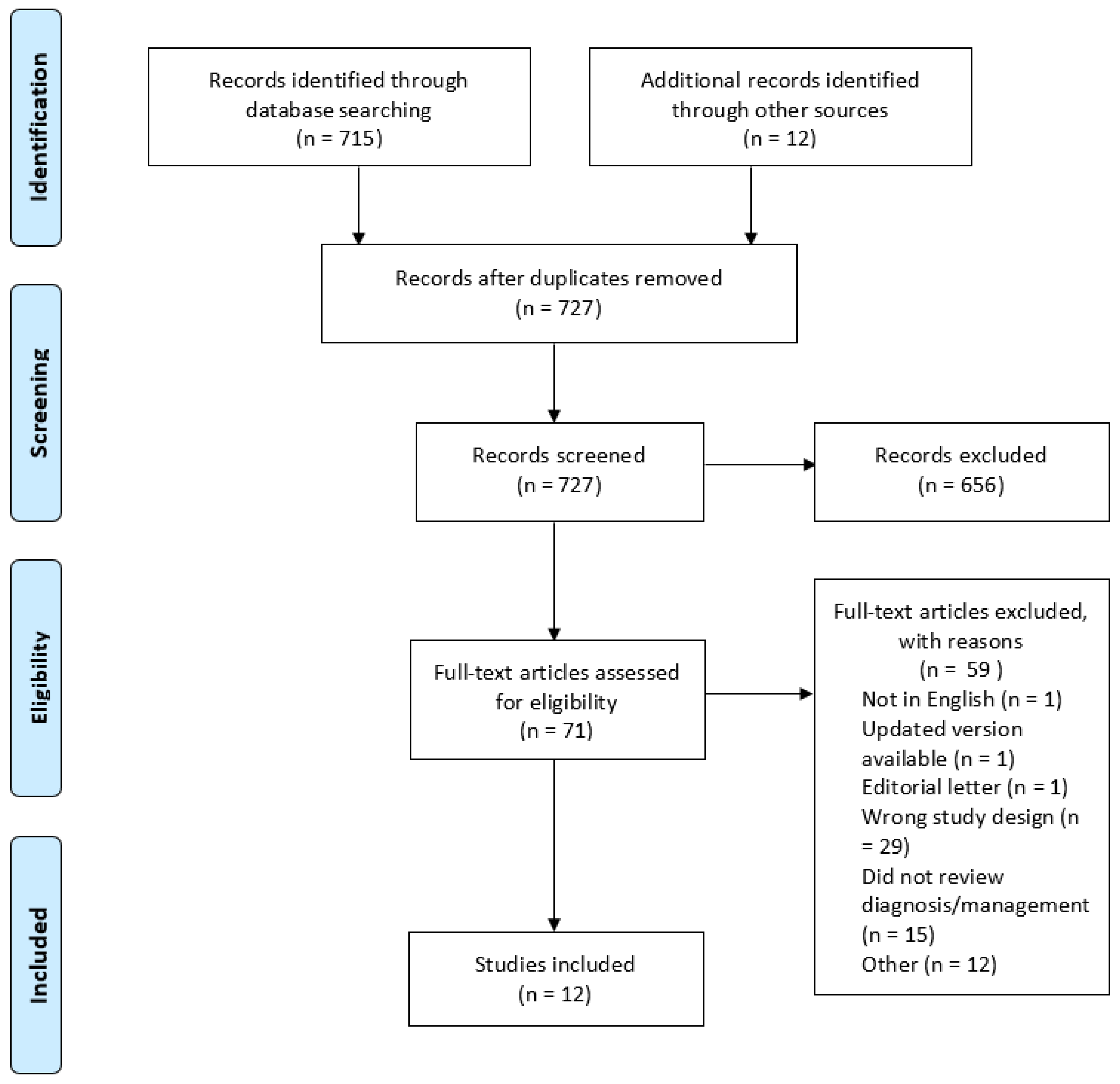
From 727 identified studies, two authors (SB and SM) independently screened titles and abstracts. Disagreements were resolved through discussion or by a third reviewer (NH). A full-text review was conducted on 71 articles. Reasons for exclusion included secondary care focus (1 article), inaccessible full texts (12 articles), not published in English (1 article), updated version published (1 article), editorial letter (1 article), or protocol (1 article). Additional exclusion reasons included a review or discussion paper (27 articles) or no review of diagnosis or management (15 articles). A total of 12 articles were included in this scoping review. A PRISMA flowchart (see Figure 1) summarises the process [28].
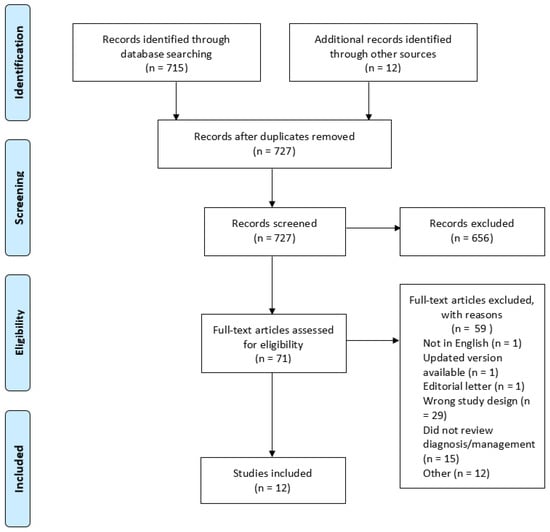
Figure 1.
Prisma flowchart for diagnosis and management of sports-related concussion for general practitioners—a scoping review.
The scoping review identified four additional tools and one guideline relevant to the diagnosis and management of SRCs in primary care. An evaluation of these tools was conducted to gain insight into their available psychometric properties, validation status, alignment with the NICE head injury guidelines [29], and feasibility within UK general practice. Notably, none of the tools were specifically validated for use in UK primary care, thus highlighting a critical gap.
Living Concussion Guidelines: A Canadian resource regularly maintained by the Ontario Ministry of Health offers evidence-based recommendations for managing all concussion subtypes, including SRCs [15]. There are two separate guidelines available: one for the paediatric population (5–18 years) and a second for the adult population [15,16]. The guidelines assist healthcare professionals, including primary care clinicians, in diagnosing all causes of concussion [15,16]. Embedded within the Living Concussion guidelines for adults (aged 18 years and older) is the Acute Concussion Evaluation (ACE) form (see Supplementary S2) [30]. This ACE form explores symptoms via a checklist as well as risk factors for prolonged recovery to help with diagnosis (Supplementary S2), with any score more than 0 indicating a positive symptom history [30]. Although a user-friendly, practical resource, there are limited psychometric data giving insight into the specific sensitivity and specificity. There are no studies validating the applicability of the guidelines in UK primary care. The ACE tool incorporates many of the NICE head injury red flag symptoms [29,30]; however, this section would require slight adaptation to ensure incorporation of all NICE red flag criteria.
BCPE: A physical examination, supplemented with the Buffalo Concussion Treadmill Test (BCTT) if additional testing is required, is utilised for adolescents (aged 13–19 years) to assess concussion [19]. Studies have demonstrated, by assessing oculomotor and vestibular signs, components included in the BCPE, the ability to distinguish between suspected concussion and healthy controls within the first week following injury [19,21,31]. Donner et al. propose that a VVE should be included as part of the SRC assessment due to its reliability and sensitivity in the paediatric population [18]. Furthermore, it was found that the BCPE had 85% predictive accuracy in identifying children at low, medium, or high risk for delayed recovery [32]. The full brief physical examination is described by Haider et al., and the brief Buffalo Concussion Physical Exam Assessment (BCPE) form is freely available (Supplementary S3) [19]. After measuring orthostatic vital signs, the physical examination should take no more than 5 min to perform [19]. It is important to caveat that these studies were not conducted in primary care, and there are no supporting adult data. From a feasibility standpoint, the tool suits the time constraints of UK primary care consultations; however, it is yet to be seen whether it could be utilised across heterogenous cohorts, how much education clinicians would require on its use, supplemental equipment costs, and whether it could be integrated within primary care IT systems. Lack of an incorporated symptom tool to screen for red flags could pose a challenge.
Tele-BCPE: A Telehealth version of the BCPE (Supplementary S4) was developed during the COVID-19 pandemic when virtual consultations were implemented to reduce the risk of COVID virus transmission [22]. The examination took 15 min to administer [22]. The reliability and validity of this examination are not known.
BIST: A 6 min symptom-based screening tool, created by the Auckland University of Technology (AUT) Brain Injury Network for assessing anyone over the age of 8 years old to triage high-risk cases, diagnoses and monitors the recovery of those who have sustained a suspected concussion [33]. It is not specific to SRCs. The recommendation is to use this tool with additional questions or examinations, including balance or visual tests [33]. The BIST comprises 12 clinical indicator questions and a symptom checklist that spans physical, emotional, cognitive, and vestibular domains. These domains have been validated for concurrent validity with tools such as the Rivermead Post-Concussion Symptoms Questionnaire [27]. No studies have reported specific sensitivity or specificity data. Compared to the risk factors that prompt community healthcare workers to refer to emergency departments as recommended by NICE guidelines for head injury assessment, the BIST does not include amnesia for events before and after injury, a persistent headache since the injury, current drug or alcohol intoxication, or previous brain surgery [29,33]. These areas would need to be added to BIST-2 for it to be used routinely within the UK. From a feasibility standpoint, the examination is brief but effectively triages patients, it is user-friendly and would require minimal training, and it would likely be straightforward to implement into UK primary care IT systems.
Digital Tools: HeadCheck, a smartphone-based application developed in Australia, consists of two components: Recognition and Recovery [17]. It is used for children aged 5–18 and aimed at parents/community sport organisers. Validated tools such as SCAT5 and childSCAT5 are incorporated [17]. The app is not freely available in the UK. As a result, no further data or information could be obtained. Similarly, the New Zealand Rugby Concussion Assessment (NZRCA) is an application designed to record normative cognitive data to help clinicians delineate a deviation from baseline and place the individual on a standardised concussion management pathway [23]. This has yet to be validated. Both these tools are in the early stages of development, at the grassroots level, and require further research.
4. Discussion: Guiding Clinical Practice
The 2023 DCMS guidance has significantly raised awareness of SRCs at the grassroots and community levels [2]. Given that GPs are already grappling with substantial workloads, it is imperative to adopt a proactive approach to pre-emptively prepare for the anticipated surge in SRC presentations. It is evident that there is a pressing need for a comprehensive tool that can seamlessly integrate within the primary care network and be consistently completed within the timeframe (approximately 10 min) of an average primary care consultation. This tool should effectively aid in diagnosing, triaging, and managing SRC cases. This scoping review has identified a number of tools and evaluated them based on specific criteria. It is important to consider the variables faced in primary care. Patients may present at different times following a concussion, recover at different rates, and different tools might be better suited to acute or delayed presentations.
4.1. 0–72 h Post-Injury: Optimising Acute Diagnosis
The initial 72 h period following a suspected SRC is a critical window for identifying post-concussive symptoms and NICE red flags [29]. SCAT6 is sensitive for detecting symptoms and balance deficits but cannot be performed correctly in less than 10 to 15 min [8], exceeding typical primary care consultation times of 10 min [6]. Prioritisation of key components, for example, symptom checklist and red-flag assessments, is required. However, this complicates matters, leaving assessment down to the clinician’s discretion, risking inconsistent practices. The BIST is a quick and effective way to triage high-risk cases but omits NICE red flags such as focal neurological symptoms, thus limiting its standalone use [29,33]. Slightly adapting BIST to include NICE-specific red flag criteria and pairing it with condensed elements of the SCAT6 could offer a standardised approach for clinicians to identify high-risk cases and streamline acute assessments in time-constrained settings. Additionally, embedding flowcharts in primary care IT systems could further aid decision-making and reduce diagnostic variability. Further research is required to confirm this.
4.2. 72 h to 2 Weeks: Monitoring Recovery
From 72 h to 2 weeks, an effective tool must provide quantitative data to track symptom progression and guide clinicians to optimise recovery, while integrating with primary care workflows. SCOAT6 offers a comprehensive approach in serial monitoring [1], although it takes 45–60 min, making it impractical for a single practitioner [9]. Delegating components to other members of the team could enhance feasibility, akin to diagnostic workflows. However, UK primary care faces a shortage of appropriately trained healthcare professionals, particularly GPs, and this is therefore not practical currently. BCPE offers a quick approach, although only validated on paediatric populations, leveraging routine observations to detect autonomic dysfunction [19]. It promises brevity, but that comes at the cost of potential training requirements in tandem with gait and eye-tracking examinations for the untrained GP. The Living Concussion Guidelines offer simple and concise evidence-backed management advice, which can supplement tools and knowledge gaps [15]. Digitising SCOAT6 checklists or BCPE orthostatic observations into patient-facing apps could enable pre-consultation tracking, reducing workload and improving information availability, but is reliant on patient engagement with recovery.
4.3. 2–4 Weeks: Guiding Return-to-Play (RTP)
Weeks 2 to 4 represent a key transition point in care. Tools must aid clinicians in assessing symptom resolution to ensure safe return-to-play (RTP) and, indeed, safe return to life, education and work. SCAT6 and SCOAT6 provide structured protocols assessing symptoms, cognition, and balance [1,8,9], but time constraints persist. The Living Concussion Guidelines offer evidence-based RTP strategies for adults and children [15,16]. Only 43% of clinicians use standardised tools currently to guide management, citing complexity and training gaps. This is a barrier that must be overcome for effective implementation [20]. Educational interventions can promote clinician confidence in using SCAT6 or SCOAT6, but systemic solutions remain fundamental [26]. Embedding RTP algorithms into primary care IT systems, such as EMIS templates, makes information easily accessible and removes resistance for clinicians to check clearance criteria. Not only would this promote compliance with NICE guidance, but it would also ensure medico-legal standards are adhered to and avoid unnecessary premature RTP risks.
4.4. Managing Prolonged Symptoms
For those suffering from prolonged symptoms, tools must predict recovery trajectories and guide appropriate referrals in accordance with the guidance provided by the DCMS, that individuals exhibiting symptoms that persist beyond a 21-day period should be referred to a specialist healthcare professional. As part of the BCPE, a Risk for Delayed Recovery (RDR) score can be calculated around 2 weeks post-injury to identify children at risk of persistent post-concussive symptoms (PPCS), facilitating early specialist referral [19,32]. No equivalent adult-specific tools exist at present, leaving GPs reliant on clinical judgement for recognising PPCS. Although BIST monitors symptoms, it lacks validated sensitivity for detecting PPCS, thereby limiting its utility [27]. The Living Concussion Guidelines provide management strategies for dealing with such symptoms, but are limited in their predictive capabilities [15]. Future innovation and development of an adult-focused RDR equivalent is vital. Adapting the BCPE’s framework could offer a potential route. As improvements are made, linking predictive tools with referral pathways could mitigate delays. Until such tools emerge, a targeted PPCS screening question could be combined with current tools to identify referral needs. It would be necessary for GPs to receive training and be equipped with follow-up specialist clinics to address these referrals effectively.
5. Barriers to Tool Adoption
Three of the studies from the literature search utilised cross-sectional surveys to ascertain the current knowledge base of SRCs amongst clinicians and how this translated into clinical practice. Across the studies, utilisation of the SCATs remained limited, largely due to perceived complexity and training gaps [20,24,25]. Stoller et al. reported that 50% of family physicians avoided SCATs, even when aware of them [24]. Training alone is insufficient if tools feel misaligned with workflows. Adapting the aforementioned tools into user-friendly algorithms within primary care workflows, utilising IT systems, such as EMIS, could act as the cornerstone in identifying red flags, standardising concussion practice, ensuring proper documentation, and aiding continuity of care. Patient-facing apps such as HeadCheck could enable symptom tracking pre-consultation, potentially reducing workloads. Recently, a 2-year government-backed trial has seen the development of a similar app in the UK called SportSmart [34], showing the promise that suitable infrastructure could be available in the near future. These solutions could leverage and build on existing infrastructure via a build-test-scale approach to be implemented across the primary care network within the UK.
6. Strengths, Limitations, and Future Directions
This study comprehensively charts international practices of SRC diagnosis and management for primary care, supported by input from clinicians in primary care, secondary care, and sports medicine. However, its reliance on 12 studies reflects a global paucity of primary care-focused SRCs research. A total of 12 studies were inaccessible, possibly due to the age of the research, despite using an academic librarian backed by a research institution to conduct the search. In addition, one paper was not available in English. It is plausible that the inability to review these studies may have omitted crucial insights. Future research should prioritise validating SCAT6, SCOAT6, BCPE, and BIST within primary care consultations, particularly within the time constraints faced by primary care practitioners. Studies should assess the sensitivity of these tools in detecting SRCs and general usability. Pilot studies integrating adapted tools with primary care IT systems could confirm feasibility while addressing training and workflow barriers. Cost–benefit analysis should also be conducted to ascertain whether tool adoption and application creation would be economically feasible.
7. Conclusions
It is anticipated that SRC presentations to primary care will increase following the release of the 2023 DCMS grassroots concussion guidance in the UK. It is vital that GPs are adequately equipped with effective and efficient tools that align with their workflows. SCOAT6 and SCAT6 are effective, but cannot be carried out within the typical 10 min consultation time of UK general practice. BIST and BCPE offer quicker alternatives but lack UK validation and alignment with NICE head injury advice. The Living Concussion Guidelines provide practical management for recovery and persistent symptoms. A UK-adapted tool, incorporating the BIST’s symptom triage, BCPE physical exam, and NICE red flag criteria, should be developed as a template on primary care IT systems for seamless integration. Educational and training initiatives are pivotal to address knowledge gaps and improve clinician confidence in implementing tools effectively. Further research should prioritise pilot studies to assess tool accuracy, feasibility, and patient outcomes in UK primary care. This will help establish standardised care practices and facilitate robust data collection on concussion diagnosis and management, which can then be used to create feedback loops and guide future iterations in practice for long-term concussion management.
Key Findings:
- No UK-validated SRCs tools exist specifically for primary care, despite DCMS guidance on concussion management within the community.
- SCAT6 and SCOAT6 are suitable for GPs but time-intensive; BIST and BCPE are quicker but not validated in the UK setting.
- Development of standardised concussion assessment tools for use in UK primary care could improve concussion diagnosis and management, with improved patient outcomes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/sports13070201/s1, Supplementary S1: Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist; Supplementary S2: Acute Concussion Evaluation (ACE) Form; Supplementary S3: Buffalo Concussion Physical Exam Assessment; Supplementary S4: Components of In-person BCPE and Tele-BCPE.
Author Contributions
S.Y.G.M. and S.B. independently reviewed the article titles and abstracts to decide which articles required full-text review. Relevant articles were selected. Both authors wrote the manuscript. N.H. acted as arbitrator for article selection and reviewer/editor of the manuscript. J.R. acted as reviewer/editor of the manuscript. All authors contributed to and reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no competing interests.
References
- Patricios, J.S.; Schneider, K.J.; Dvorak, J.; Ahmed, O.H.; Blauwet, C.; Cantu, R.C.; Davis, G.A.; Echemendia, R.J.; Makdissi, M.; McNamee, M.; et al. Consensus statement on concussion in sport: The 6th International Conference on Concussion in Sport-Amsterdam, October 2022. Br. J. Sports Med. 2023, 57, 695–711. [Google Scholar] [CrossRef] [PubMed]
- UK Government. UK Concussion Guidelines for Non-Elite (Grassroots) Sport Contents; UK Government: London, UK, 2023; Available online: http://sramedia.s3.amazonaws.com/media/documents/9ced1e1a-5d3b-4871-9209-bff4b2575b46.pdf (accessed on 31 October 2023).
- House of Commons Digital, Culture, Media and Sport Committee. Concussion in Sport; House of Commons: London, UK, 2021; Available online: https://publications.parliament.uk/pa/cm5802/cmselect/cmcumeds/46/4604.htm#_idTextAnchor001 (accessed on 31 October 2023).
- Scully, P.; Falvey, E.C. Concussion management in general practice: A survey of general practitioners in primary care in the Republic of Ireland. Ir. J. Med. Sci. 2021, 190, 197–203. [Google Scholar] [CrossRef]
- British Medical Association. Pressures in General Practice Data Analysis; British Medical Association: London, UK, 2023; Available online: https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressures-in-general-practice-data-analysis (accessed on 31 October 2023).
- Salisbury, H. Helen Salisbury: The 10 minute appointment. BMJ 2019, 365, l2389. [Google Scholar] [CrossRef] [PubMed]
- Van Ierssel, J.; Osmond, M.; Hamid, J.; Sampson, M.; Zemek, R. What is the risk of recurrent concussion in children and adolescents aged 5–18 years? A systematic review and meta-analysis. Br. J. Sports Med. 2021, 55, 663–669. [Google Scholar] [CrossRef]
- Echemendia, R.J.; Brett, B.L.; Broglio, S.; Davis, G.A.; Giza, C.C.; Guskiewicz, K.M.; Harmon, K.G.; Herring, S.; Howell, D.R.; Master, C.L.; et al. Introducing the Sport Concussion Assessment Tool 6 (SCAT6). Br. J. Sports Med. 2023, 57, 619–621. [Google Scholar] [CrossRef] [PubMed]
- Patricios, J.S.; Schneider, G.M.; Van Ierssel, J.; Purcell, L.K.; Davis, G.A.; Echemendia, R.J.; Fremont, P.; Fuller, G.W.; Herring, S.A.; Harmon, K.G.; et al. Beyond acute concussion assessment to office management: A systematic review informing the development of a Sport Concussion Office Assessment Tool (SCOAT6) for adults and children. Br. J. Sports Med. 2023, 57, 737–748. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Joanna Briggs Institute. JBI Critical Appraisal Tools; Joanna Briggs Institute: Adelaide, Australia, 2023; Available online: https://jbi.global/critical-appraisal-tools (accessed on 31 October 2023).
- Brouwers, M.C.; Kho, M.E.; Browman, G.P.; Burgers, J.S.; Cluzeau, F.; Feder, G.; Fervers, B.; Graham, I.D.; Grimshaw, J.; Hanna, S.E.; et al. AGREE II: Advancing guideline development, reporting and evaluation in health care. Can. Med. Assoc. J. 2010, 182, E839–E842. [Google Scholar] [CrossRef]
- Marshall, S.; Lithopoulos, A.; Curran, D.; Fischer, L.; Velikonja, D.; Bayley, M. Living Concussion Guidelines: Guideline for Concussion & Prolonged Symptoms for Adults 18 Years of Age or Older; Concussions Ontario: Toronto, ON, Canada, 2023; Available online: https://concussionsontario.org/ (accessed on 31 October 2023).
- Reed, N.; Zemek, R.; Dawson, J.; Ledoux, A.A.; Provvidenza, C.; Paniccia, M.; Tataryn, Z.; Sampson, M.; Eady, K.; Bourke, T.; et al. Living Guideline for Pediatric Concussion Care; Pediatric Concussion Community of Practice: Toronto, ON, Canada, 2021; Available online: https://osf.io/3vwn9/ (accessed on 19 December 2023).
- Clarke, C.; Anderson, V.; Babl, F.E.; Rausa, V.C.; Davis, G.A.; Barnett, P.; Crichton, A.; Takagi, M.; Hearps, S.J.C.; Davies, K.; et al. Child concussion recognition and recovery: A community delivered, evidenced-based solution. Ann. Transl. Med. 2020, 8, 595. [Google Scholar] [CrossRef] [PubMed]
- Donner, J.R.; Corwin, D.J.; Master, C.L.; Zonfrillo, M.R. Documented visio-vestibular examination and anticipatory guidance for pediatric concussion patients. Pediatr. Emerg. Care 2023, 39, 179–183. [Google Scholar] [CrossRef]
- Haider, M.N.; Leddy, J.J.; Du, W.; Macfarlane, A.J.; Viera, K.B.; Willer, B.S. Practical management: Brief physical examination for sport-related concussion in the outpatient setting. Clin. J. Sport Med. 2020, 30, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Lebrun, C.M.; Mrazik, M.; Prasad, A.S.; Tjarks, B.J.; Dorman, J.C.; Bergeron, M.F.; Munce, T.A.; Valentine, V.D. Sport concussion knowledge base, clinical practices and needs for continuing medical education: A survey of family physicians and cross-border comparison. Br. J. Sports Med. 2013, 47, 54–59. [Google Scholar] [CrossRef]
- Leddy, J.; Lesh, K.; Haider, M.N.; Czuczman, N.; Baker, J.G.; Miecznikowski, J.; Willer, B. Derivation of a focused, brief concussion physical examination for adolescents with sport-related concussion. Clin. J. Sport Med. 2021, 31, 7–14. [Google Scholar] [CrossRef]
- McPherson, J.I.; Saleem, G.T.; Haider, M.N.; Leddy, J.J.; Torres, D.M.; Willer, B. Practical management: Telehealth examination for sport-related concussion in the outpatient setting. Clin. J. Sport Med. 2022, 32, 72–75. [Google Scholar] [CrossRef]
- Salmon, D.M.; Chua, J.; Sullivan, S.J.; Whatman, C.; Brown, J.; Register-Mihalik, J.; Murphy, I.; Walters, S.; Clacy, A.; Sole, G.; et al. Sport concussion assessment in New Zealand high school rugby players: A collaborative approach to the challenges faced in primary care. Brain Inj. 2022, 36, 258–270. [Google Scholar] [CrossRef]
- Stoller, J.; Carson, J.D.; Garel, A.; Libfeld, P.; Snow, C.L.; Law, M.; Frémont, P. Do family physicians, emergency department physicians, and pediatricians give consistent sport-related concussion management advice? Can. Fam. Physician 2014, 60, 548–552. [Google Scholar]
- Stuart, C.; Reid, D.; Theadom, A.; Fulcher, M.; Hardaker, N. Knowledge and management of sport-related concussion in primary care in New Zealand. N. Z. Med. J. 2022, 135, 31–41. [Google Scholar]
- Taylor, A.M.; Nigrovic, L.E.; Saillant, M.L.; Trudell, E.K.; Modest, J.R.; Kuhn, M.; Vernacchio, L. Educational initiative to standardize concussion management in pediatric primary care. Clin. Pediatr. 2018, 57, 806–814. [Google Scholar] [CrossRef]
- Theadom, A.; Hardaker, N.; Bray, C.; Siegert, R.; Henshall, K.; Forch, K.; Fernando, K.; King, D.; Fulcher, M.; Jewell, S.; et al. The Brain Injury Screening Tool (BIST): Tool development, factor structure and validity. PLoS ONE 2021, 16, e0246512. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Head Injury: Assessment and Early Management; NICE Guideline [NG232]; NICE: London, UK, 2023; Available online: https://www.nice.org.uk/guidance/ng232 (accessed on 31 October 2023).
- Gioia, G.; Collins, M. Acute Concussion Evaluation (ACE): Physician/Clinician Office Version. 2006. Available online: https://concussionsontario.org/sites/default/files/2024-07/ACE%20Questionnaire.pdf (accessed on 31 October 2023).
- Mucha, A.; Collins, M.W.; Elbin, R.J.; Furman, J.M.; Troutman-Enseki, C.; DeWolf, R.M.; Marchetti, G.; Kontos, A.P. A brief vestibular/ocular motor screening (VOMS) assessment to evaluate concussions: Preliminary findings. Am. J. Sports Med. 2014, 42, 2479–2486. [Google Scholar] [CrossRef] [PubMed]
- Haider, M.N.; Cunningham, A.; Darling, S.; Suffoletto, H.N.; Freitas, M.S.; Jain, R.K.; Willer, B.; Leddy, J.J. Derivation of the Buffalo Concussion Physical Examination risk of delayed recovery (RDR) score to identify children at risk for persistent postconcussive symptoms. Br. J. Sports Med. 2021, 55, 1427–1433. [Google Scholar] [CrossRef]
- Traumatic Brain Injury Network. Brain Injury Screening Tool: A Guide to TBI Assessment; Auckland University of Technology: Auckland, New Zealand, 2023; Available online: https://tbin.aut.ac.nz/support-and-resources/brain-injury-screening-tool-bist (accessed on 31 October 2023).
- Podium Analytics. SportSmart Programme; Podium Analytics: London, UK, 2023; Available online: https://podiumanalytics.org/sportsmart/ (accessed on 20 December 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).