The Effect of Carbohydrate Ingestion on Performance and Indices of Fatigue in Adolescent Soccer Players During a Simulated Game
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
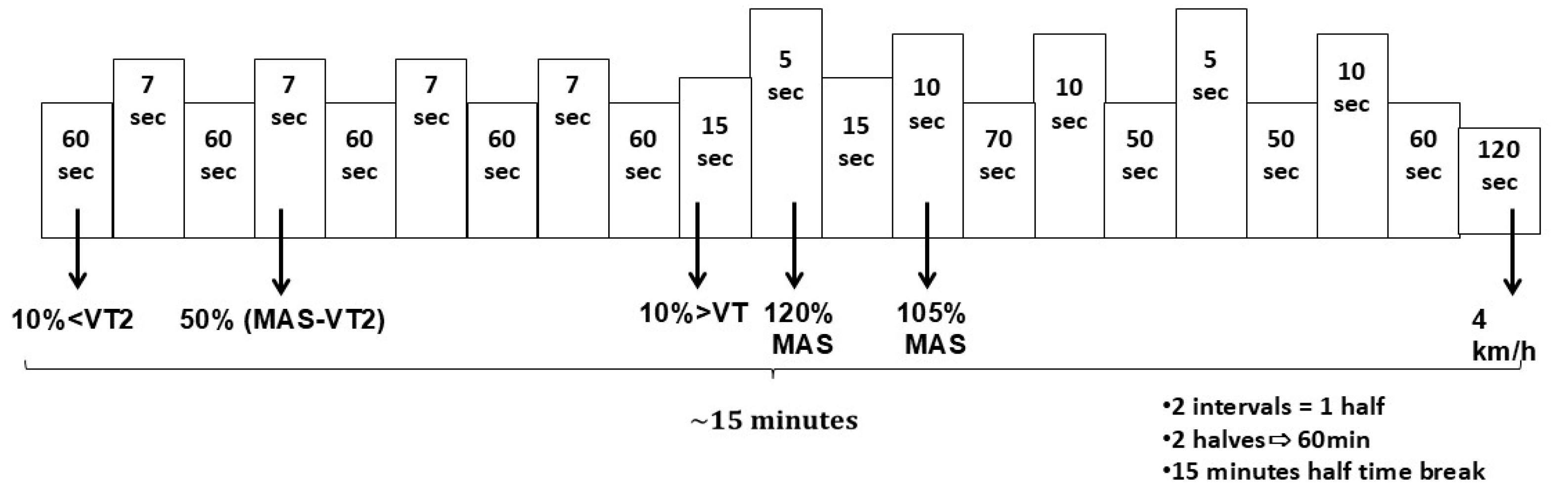
2.2. Reliability of Soccer Simulation Exercise Protocol
2.3. Study Design
2.4. Treatment Administration
2.5. Baseline Exercise Testing
2.6. Experimental Procedure
2.7. Fatigue Measurements
2.8. Statistical Analysis
2.8.1. Reliability of Soccer Simulation Exercise Protocol
2.8.2. Carbohydrate Ingestion
3. Results
3.1. Reliability of Soccer Simulation Exercise Protocol
3.2. Carbohydrate Ingestion
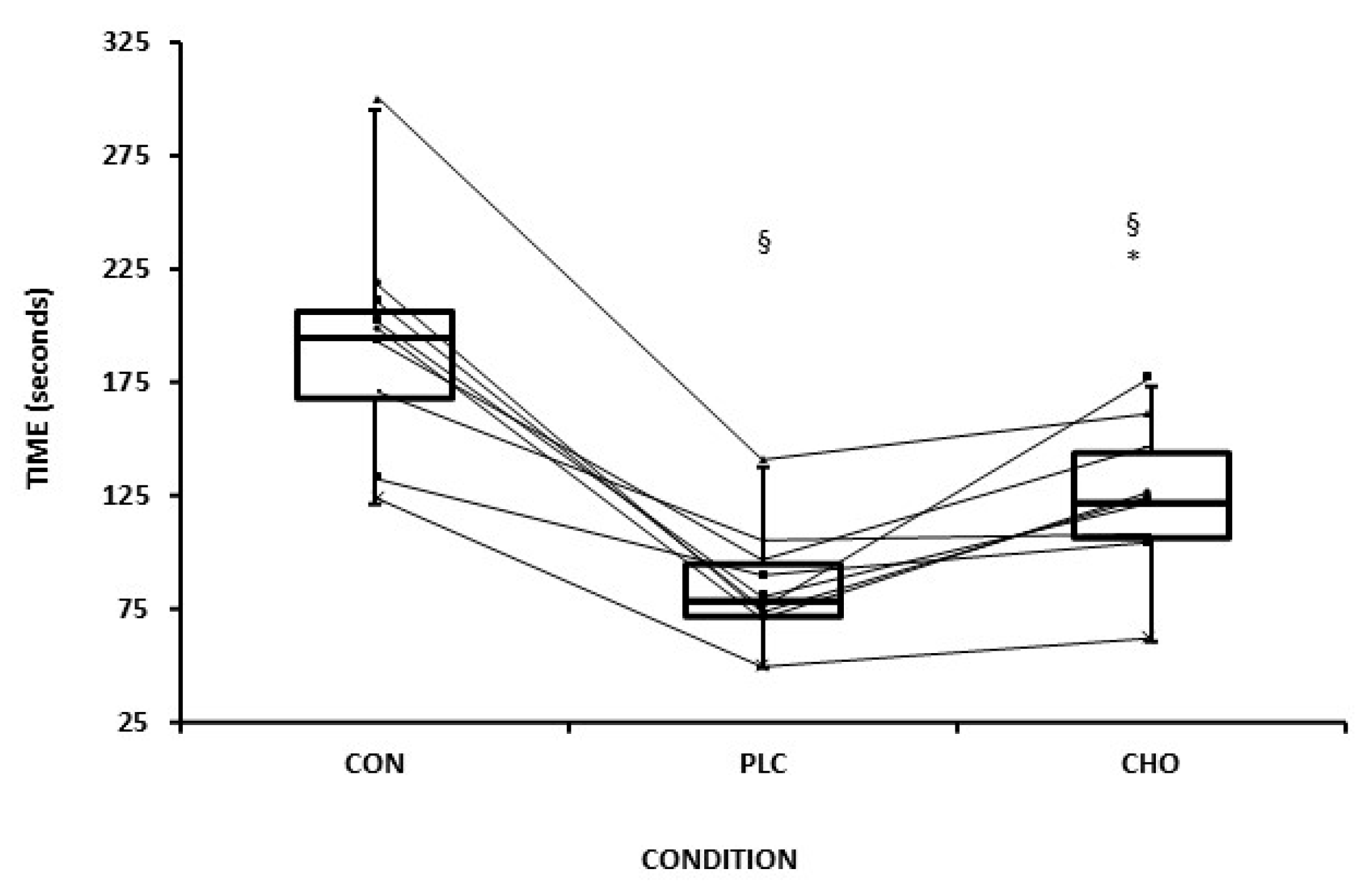
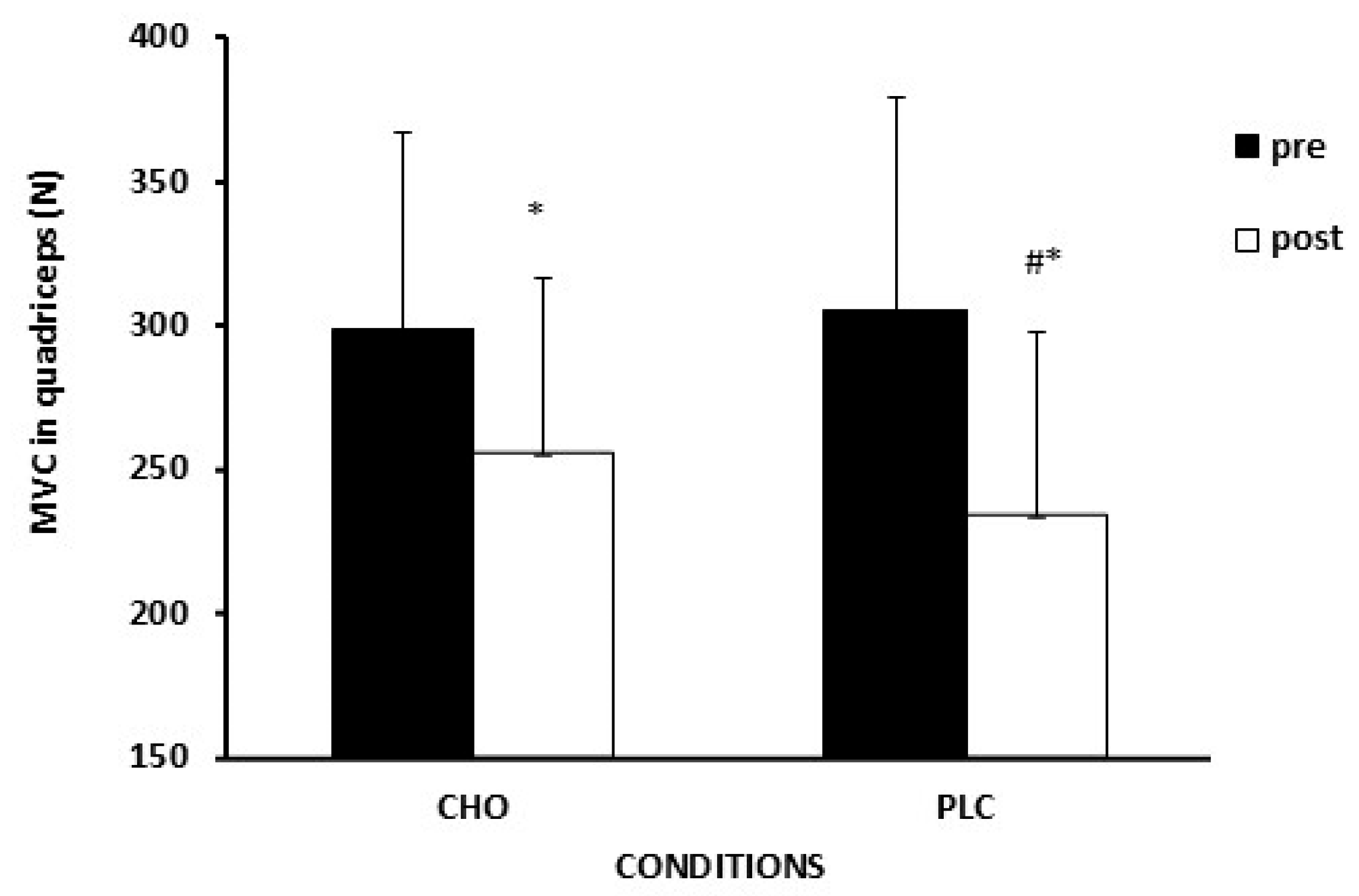
3.3. Exercise Performance and Fatigue Indices
3.4. Rating of Perceived Exertion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CHO | Carbohydrate ingestion condition |
| PLC | Placebo condition (no carbohydrates) |
| MVC | Maximal Voluntary Contraction |
| TTE | Time To Exhaustion endurance performance test |
| PHV | Peak Height Velocity |
| CV | Coefficient of Variation |
| ICC | Intraclass Correlation Coefficient |
References
- Palucci Vieira, L.H.; Carling, C.; Barbieri, F.A.; Aquino, R.; Santiago, P.R.P. Match Running Performance in Young Soccer Players: A Systematic Review. Sports Med. 2019, 49, 289–318. [Google Scholar] [CrossRef] [PubMed]
- Osgnach, C.; Poser, S.; Bernardini, R.; Rinaldo, R.; di Prampero, P.E. Energy cost and metabolic power in elite soccer: A new match analysis approach. Med. Sci. Sports Exerc. 2010, 42, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Stroyer, J.; Hansen, L.; Klausen, K. Physiological profile and activity pattern of young soccer players during match play. Med. Sci. Sports Exerc. 2004, 36, 168–174. [Google Scholar] [CrossRef]
- Lovell, R.; Fransen, J.; Ryan, R.; Massard, T.; Cross, R.; Eggers, T.; Duffield, R. Biological maturation and match running performance: A national football (soccer) federation perspective. J. Sci. Med. Sport 2019, 22, 1139–1145. [Google Scholar] [CrossRef]
- Bangsbo, J.; Mohr, M.; Krustrup, P. Physical and metabolic demands of training and match-play in the elite football player. J. Sports Sci. 2006, 24, 665–674. [Google Scholar] [CrossRef]
- Krustrup, P.; Mohr, M.; Steensberg, A.; Bencke, J.; Kjaer, M.; Bangsbo, J. Muscle and blood metabolites during a soccer game: Implications for sprint performance. Med. Sci. Sports Exerc. 2006, 38, 1165–1174. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.C.; Ferreira, D.; Caetano, C.; Granja, D.; Pinto, R.; Mendes, B.; Sousa, M. Nutrition and Supplementation in Soccer. Sports 2017, 5, 28. [Google Scholar] [CrossRef]
- Phillips, S.M.; Sproule, J.; Turner, A.P. Carbohydrate ingestion during team games exercise: Current knowledge and areas for future investigation. Sports Med. 2011, 41, 559–585. [Google Scholar] [CrossRef]
- Nedelec, M.; McCall, A.; Carling, C.; Legall, F.; Berthoin, S.; Dupont, G. Recovery in soccer: Part I—Post-match fatigue and time course of recovery. Sports Med. 2012, 42, 997–1015. [Google Scholar] [CrossRef]
- Mohr, M.; Ermidis, G.; Jamurtas, A.Z.; Vigh-Larsen, J.F.; Poulios, A.; Draganidis, D.; Papanikolaou, K.; Tsimeas, P.; Batsilas, D.; Loules, G.; et al. Extended Match Time Exacerbates Fatigue and Impacts Physiological Responses in Male Soccer Players. Med. Sci. Sports Exerc. 2023, 55, 80–92. [Google Scholar] [CrossRef]
- Silva, J.R.; Rumpf, M.C.; Hertzog, M.; Castagna, C.; Farooq, A.; Girard, O.; Hader, K. Acute and Residual Soccer Match-Related Fatigue: A Systematic Review and Meta-analysis. Sports Med. 2018, 48, 539–583. [Google Scholar] [CrossRef] [PubMed]
- Cermak, N.M.; van Loon, L.J. The use of carbohydrates during exercise as an ergogenic aid. Sports Med. 2013, 43, 1139–1155. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.; Rollo, I. Carbohydrate Nutrition and Team Sport Performance. Sports Med. 2015, 45 (Suppl. S1), S13–S22. [Google Scholar] [CrossRef]
- Phillips, S.M.; Turner, A.P.; Gray, S.; Sanderson, M.F.; Sproule, J. Ingesting a 6% carbohydrate-electrolyte solution improves endurance capacity, but not sprint performance, during intermittent, high-intensity shuttle running in adolescent team games players aged 12–14 years. Eur. J. Appl. Physiol. 2010, 109, 811–821. [Google Scholar] [CrossRef] [PubMed]
- Stephens, B.R.; Cole, A.S.; Mahon, A.D. The influence of biological maturation on fat and carbohydrate metabolism during exercise in males. Int. J. Sport. Nutr. Exerc. Metab. 2006, 16, 166–179. [Google Scholar] [CrossRef]
- Phillips, S.M. Carbohydrate supplementation and prolonged intermittent high-intensity exercise in adolescents: Research findings, ethical issues and suggestions for the future. Sports Med. 2012, 42, 817–828. [Google Scholar] [CrossRef]
- Timmons, B.W.; Bar-Or, O.; Riddell, M.C. Influence of age and pubertal status on substrate utilization during exercise with and without carbohydrate intake in healthy boys. Appl. Physiol. Nutr. Metab. 2007, 32, 416–425. [Google Scholar] [CrossRef]
- Welsh, R.S.; Davis, J.M.; Burke, J.R.; Williams, H.G. Carbohydrates and physical/mental performance during intermittent exercise to fatigue. Med. Sci. Sports Exerc. 2002, 34, 723–731. [Google Scholar] [CrossRef]
- Winnick, J.J.; Davis, J.M.; Welsh, R.S.; Carmichael, M.D.; Murphy, E.A.; Blackmon, J.A. Carbohydrate feedings during team sport exercise preserve physical and CNS function. Med. Sci. Sports Exerc. 2005, 37, 306–315. [Google Scholar] [CrossRef]
- Backhouse, S.H.; Ali, A.; Biddle, S.J.; Williams, C. Carbohydrate ingestion during prolonged high-intensity intermittent exercise: Impact on affect and perceived exertion. Scand. J. Med. Sci. Sports 2007, 17, 605–610. [Google Scholar] [CrossRef]
- Zafeiridis, A.; Dalamitros, A.; Dipla, K.; Manou, V.; Galanis, N.; Kellis, S. Recovery during high-intensity intermittent anaerobic exercise in boys, teens, and men. Med. Sci. Sports Exerc. 2005, 37, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Ratel, S.; Bedu, M.; Hennegrave, A.; Dore, E.; Duche, P. Effects of age and recovery duration on peak power output during repeated cycling sprints. Int. J. Sports Med. 2002, 23, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Patikas, D.A.; Williams, C.A.; Ratel, S. Exercise-induced fatigue in young people: Advances and future perspectives. Eur. J. Appl. Physiol. 2018, 118, 899–910. [Google Scholar] [CrossRef]
- Martin-Garetxana, I.; Hughes, J.; De Ste Croix, M.; Larruskain, J.; Lekue, J.A.; Ayala, F. Acute pre- and post-competitive soccer match-play changes in neuromuscular factors, physical performance, and muscle response in youth male players. Sci. Med. Footb. 2024, 8, 427–437. [Google Scholar] [CrossRef]
- Pérez, P.; Toro-Román, V.; Siquier-Coll, J.; Bartolomé, I.; Pérez, F.J. Effect of Combined Intra-Session Glucose and Fructose Intake on the Performance of Young Super-Sprint Triathletes: A Randomised, Crossover, Blind, Placebo-Controlled Study. Appl. Sci. 2024, 14, 3005. [Google Scholar] [CrossRef]
- Phillips, S.M.; Turner, A.P.; Sanderson, M.F.; Sproule, J. Beverage carbohydrate concentration influences the intermittent endurance capacity of adolescent team games players during prolonged intermittent running. Eur. J. Appl. Physiol. 2012, 112, 1107–1116. [Google Scholar] [CrossRef]
- Moore, S.A.; McKay, H.A.; Macdonald, H.; Nettlefold, L.; Baxter-Jones, A.D.; Cameron, N.; Brasher, P.M. Enhancing a Somatic Maturity Prediction Model. Med. Sci. Sports Exerc. 2015, 47, 1755–1764. [Google Scholar] [CrossRef]
- Armstrong, N.; Welsman, J.; Winsley, R. Is peak VO2 a maximal index of children’s aerobic fitness? Int. J. Sports Med. 1996, 17, 356–359. [Google Scholar] [CrossRef]
- Mays, R.J.; Goss, F.L.; Nagle, E.F.; Gallagher, M., Jr.; Haile, L.; Schafer, M.A.; Kim, K.H.; Robertson, R.J. Cross-validation of Peak Oxygen Consumption Prediction Models from OMNI Perceived Exertion. Int. J. Sports Med. 2016, 37, 831–837. [Google Scholar] [CrossRef]
- Wasserman, K.; McIlroy, M.B. Detecting the Threshold of Anaerobic Metabolism in Cardiac Patients during Exercise. Am. J. Cardiol. 1964, 14, 844–852. [Google Scholar] [CrossRef]
- Binder, R.K.; Wonisch, M.; Corra, U.; Cohen-Solal, A.; Vanhees, L.; Saner, H.; Schmid, J.P. Methodological approach to the first and second lactate threshold in incremental cardiopulmonary exercise testing. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Bar-Or, O. The Wingate anaerobic test. An update on methodology, reliability and validity. Sports Med. 1987, 4, 381–394. [Google Scholar] [CrossRef] [PubMed]
- Cherouveim, E.D.; Miliotis, P.G.; Koskolou, M.D.; Dipla, K.; Vrabas, I.S.; Geladas, N.D. The Effect of Skeletal Muscle Oxygenation on Hemodynamics, Cerebral Oxygenation and Activation, and Exercise Performance during Incremental Exercise to Exhaustion in Male Cyclists. Biology 2023, 12, 981. [Google Scholar] [CrossRef]
- Roemmich, J.N.; Barkley, J.E.; Epstein, L.H.; Lobarinas, C.L.; White, T.M.; Foster, J.H. Validity of PCERT and OMNI walk/run ratings of perceived exertion. Med. Sci. Sports Exerc. 2006, 38, 1014–1019. [Google Scholar] [CrossRef]
- Kounalakis, S.N.; Geladas, N.D. Cardiovascular drift and cerebral and muscle tissue oxygenation during prolonged cycling at different pedalling cadences. Appl. Physiol. Nutr. Metab. 2012, 37, 407–417. [Google Scholar] [CrossRef]
- Nybo, L.; Nielsen, B. Hyperthermia and central fatigue during prolonged exercise in humans. J. Appl. Physiol. 2001, 91, 1055–1060. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Giavarina, D. Understanding Bland Altman analysis. Biochem. Med. 2015, 25, 141–151. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar] [CrossRef]
- Mohr, M.; Vigh-Larsen, J.F.; Krustrup, P. Muscle Glycogen in Elite Soccer—A Perspective on the Implication for Performance, Fatigue, and Recovery. Front. Sports Act. Living 2022, 4, 876534. [Google Scholar] [CrossRef]
- Saltin, B. Metabolic fundamentals in exercise. Med. Sci. Sports 1973, 5, 137–146. [Google Scholar] [CrossRef]
- Stolen, T.; Chamari, K.; Castagna, C.; Wisloff, U. Physiology of soccer: An update. Sports Med. 2005, 35, 501–536. [Google Scholar] [CrossRef] [PubMed]
- Harley, J.A.; Barnes, C.A.; Portas, M.; Lovell, R.; Barrett, S.; Paul, D.; Weston, M. Motion analysis of match-play in elite U12 to U16 age-group soccer players. J. Sports Sci. 2010, 28, 1391–1397. [Google Scholar] [CrossRef] [PubMed]
- Mendez-Villanueva, A.; Buchheit, M.; Simpson, B.; Bourdon, P.C. Match play intensity distribution in youth soccer. Int. J. Sports Med. 2013, 34, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Saward, C.; Morris, J.G.; Nevill, M.E.; Nevill, A.M.; Sunderland, C. Longitudinal development of match-running performance in elite male youth soccer players. Scand. J. Med. Sci. Sports 2016, 26, 933–942. [Google Scholar] [CrossRef]
- Timmons, B.W.; Bar-Or, O.; Riddell, M.C. Energy substrate utilization during prolonged exercise with and without carbohydrate intake in preadolescent and adolescent girls. J. Appl. Physiol. 2007, 103, 995–1000. [Google Scholar] [CrossRef]
- Phillips, S.M.; Turner, A.P.; Sanderson, M.F.; Sproule, J. Carbohydrate gel ingestion significantly improves the intermittent endurance capacity, but not sprint performance, of adolescent team games players during a simulated team games protocol. Eur. J. Appl. Physiol. 2012, 112, 1133–1141. [Google Scholar] [CrossRef]
- Thorlund, J.B.; Aagaard, P.; Madsen, K. Rapid muscle force capacity changes after soccer match play. Int. J. Sports Med. 2009, 30, 273–278. [Google Scholar] [CrossRef]
- Krustrup, P.; Ortenblad, N.; Nielsen, J.; Nybo, L.; Gunnarsson, T.P.; Iaia, F.M.; Madsen, K.; Stephens, F.; Greenhaff, P.; Bangsbo, J. Maximal voluntary contraction force, SR function and glycogen resynthesis during the first 72 h after a high-level competitive soccer game. Eur. J. Appl. Physiol. 2011, 111, 2987–2995. [Google Scholar] [CrossRef]
- Rampinini, E.; Bosio, A.; Ferraresi, I.; Petruolo, A.; Morelli, A.; Sassi, A. Match-related fatigue in soccer players. Med. Sci. Sports Exerc. 2011, 43, 2161–2170. [Google Scholar] [CrossRef]
- Ratel, S.; Duche, P.; Williams, C.A. Muscle fatigue during high-intensity exercise in children. Sports Med. 2006, 36, 1031–1065. [Google Scholar] [CrossRef]
- Edwards, R.H. Human muscle function and fatigue. Ciba Found. Symp. 1981, 82, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Thomas, K.; Dent, J.; Howatson, G.; Goodall, S. Etiology and Recovery of Neuromuscular Fatigue after Simulated Soccer Match Play. Med. Sci. Sports Exerc. 2017, 49, 955–964. [Google Scholar] [CrossRef] [PubMed]
- Massamba, A.; Kouzkouz, N.; Geny, B.; Favret, F.; Hureau, T.J. Neuromuscular Fatigue in Hamstring and Quadriceps Muscles Following Simulated Soccer Match-Play and Typical Training Sessions. Med. Sci. Sports Exerc. 2024, 57, 984–995. [Google Scholar] [CrossRef] [PubMed]


| Carbohydrate Ingestion (n = 9) | Simulation Protocol (n = 7) | |
|---|---|---|
| Age (yrs) | 13.4 ± 0.4 (12.8–14) | 13.7 ± 0.2 (13.3–13.9) |
| Height (cm) | 159.6 ± 6 (146–168) | 153 ± 4 (148–156) |
| Weight (kg) | 51.8 ± 4 (44.1–55.9) | 45 ± 6 (42.1–53.8) |
| V̇O2peak (L/min) | 2.9 ± 0.4 (2.36–3.43) | |
| V̇O2peak (mL/kg/min) | 55 ± 5.7 (49.3–65.8) | 53.5 ± 4 (50.2–59.7) |
| vVT2 (km/h) | 11.3 ± 1.5 (10–14) | 12.2 ± 2 (9.5–15) |
| MAS (km/h) | 14.3 ± 0.9 (14–16) | 15.9 ± 0.5 (14.1–17.5) |
| Pmax (w/kg) | 9.8 ± 0.4 (9.35–10.52) | |
| Body fat (%) | 10.4 ± 2 (8.8–13.1) | 10.6 ± 4 (7.3–13.9) |
| PHV (yrs) | −1.4 ± 0.3 (−1.09 to −2.01) | −1.01 ± 0.3 (−0.8 to −1.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miliotis, P.G.; Ntalapera, S.D.; Stergiopoulos, D.C.; Zavvos, A.C.; Klentrou, P.; Giannopoulou, I.; Geladas, N.D. The Effect of Carbohydrate Ingestion on Performance and Indices of Fatigue in Adolescent Soccer Players During a Simulated Game. Sports 2025, 13, 192. https://doi.org/10.3390/sports13060192
Miliotis PG, Ntalapera SD, Stergiopoulos DC, Zavvos AC, Klentrou P, Giannopoulou I, Geladas ND. The Effect of Carbohydrate Ingestion on Performance and Indices of Fatigue in Adolescent Soccer Players During a Simulated Game. Sports. 2025; 13(6):192. https://doi.org/10.3390/sports13060192
Chicago/Turabian StyleMiliotis, Panagiotis G., Spyridoula D. Ntalapera, Dimitriοs C. Stergiopoulos, Athanasios C. Zavvos, Panagiota Klentrou, Ifigeneia Giannopoulou, and Nickos D. Geladas. 2025. "The Effect of Carbohydrate Ingestion on Performance and Indices of Fatigue in Adolescent Soccer Players During a Simulated Game" Sports 13, no. 6: 192. https://doi.org/10.3390/sports13060192
APA StyleMiliotis, P. G., Ntalapera, S. D., Stergiopoulos, D. C., Zavvos, A. C., Klentrou, P., Giannopoulou, I., & Geladas, N. D. (2025). The Effect of Carbohydrate Ingestion on Performance and Indices of Fatigue in Adolescent Soccer Players During a Simulated Game. Sports, 13(6), 192. https://doi.org/10.3390/sports13060192







