Accuracy of the SenseWear Armband during Short Bouts of Exercise
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Dependent Variables
2.4. Statistical Analysis
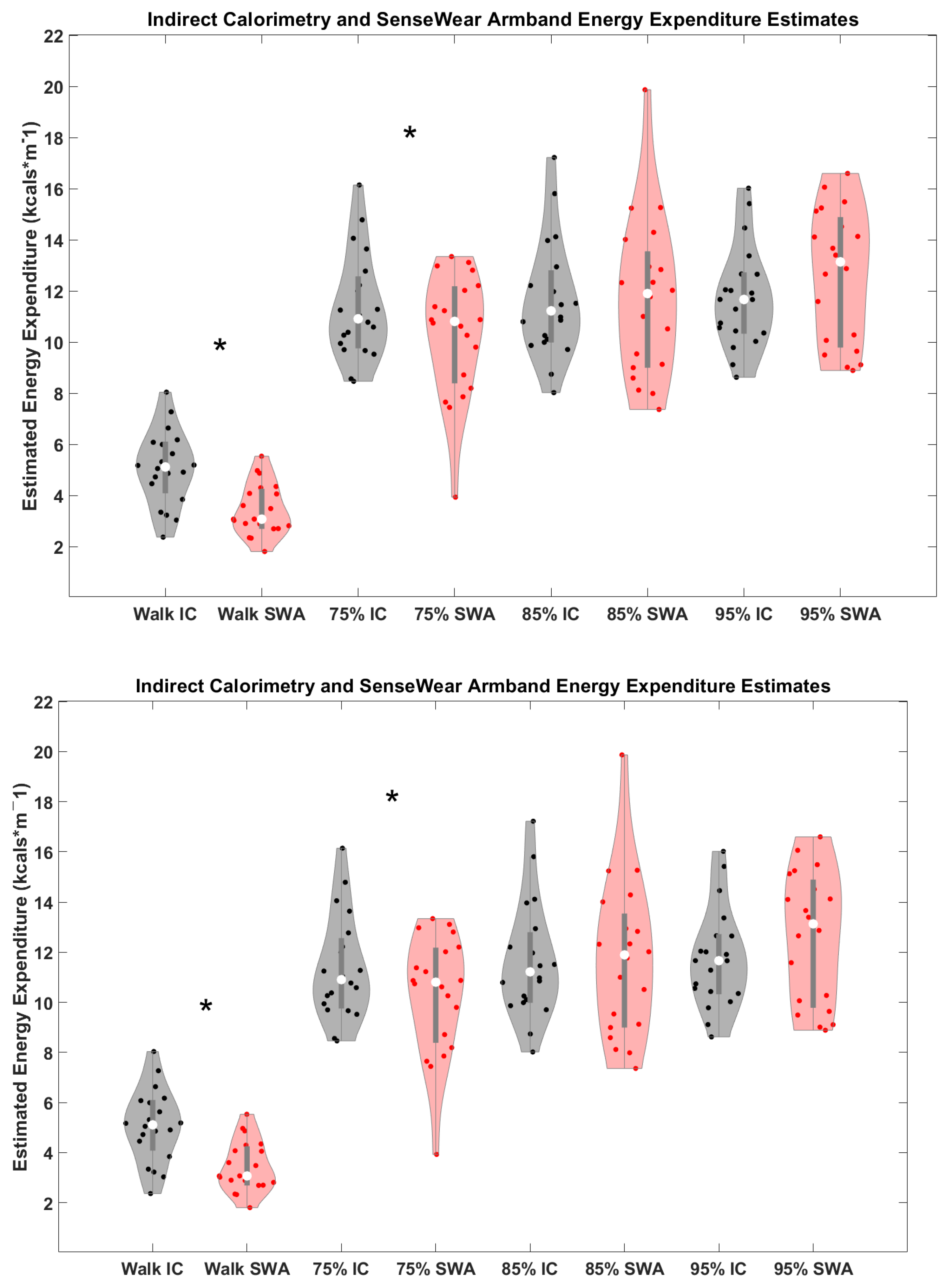
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Melin, A.K.; Areta, J.L.; Heikura, I.A.; Stellingwerff, T.; Torstveit, M.K.; Hackney, A.C. Direct and Indirect Impact of Low Energy Availability on Sports Performance. Scand. J. Med. Sci. Sports 2023, 34, e14327. [Google Scholar] [CrossRef] [PubMed]
- Jurvelin, H.; Tanskanen-Tervo, M.; Kinnunen, H.; Santtila, M.; Kyröläinen, H. Training Load and Energy Expenditure during Military Basic Training Period. Med. Sci. Sports Exerc. 2020, 52, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Freedson, P.S.; Brendley, K.; Ainsworth, B.E.; Kohl, H.W.; Leslie, E.; Owen, N. New Techniques and Issues in Assessing Walking Behavior and Its Contexts. Med. Sci. Sports Exerc. 2008, 40, S574–S583. [Google Scholar] [CrossRef] [PubMed]
- Murakami, H.; Kawakami, R.; Nakae, S.; Yamada, Y.; Nakata, Y.; Ohkawara, K.; Sasai, H.; Ishikawa-Takata, K.; Tanaka, S.; Miyachi, M. Accuracy of 12 Wearable Devices for Estimating Physical Activity Energy Expenditure Using a Metabolic Chamber and the Doubly Labeled Water Method: Validation Study. JMIR MHealth UHealth 2019, 7, e13938. [Google Scholar] [CrossRef] [PubMed]
- Dasa, M.S.; Friborg, O.; Kristoffersen, M.; Pettersen, G.; Sundgot-Borgen, J.; Rosenvinge, J.H. Accuracy of Tracking Devices’ Ability to Assess Exercise Energy Expenditure in Professional Female Soccer Players: Implications for Quantifying Energy Availability. Int. J. Environ. Res. Public. Health 2022, 19, 4770. [Google Scholar] [CrossRef] [PubMed]
- Ingraham, K.A.; Ferris, D.P.; Remy, C.D. Evaluating Physiological Signal Salience for Estimating Metabolic Energy Cost from Wearable Sensors. J. Appl. Physiol. 2019, 126, 717–729. [Google Scholar] [CrossRef] [PubMed]
- Freedson, P.S.; Lyden, K.; Kozey-Keadle, S.; Staudenmayer, J. Evaluation of Artificial Neural Network Algorithms for Predicting METs and Activity Type from Accelerometer Data: Validation on an Independent Sample. J. Appl. Physiol. 2011, 111, 1804–1812. [Google Scholar] [CrossRef] [PubMed]
- Orendurff, M.S. How Humans Walk: Bout Duration, Steps per Bout, and Rest Duration. J. Rehabil. Res. Dev. 2008, 45, 1077–1090. [Google Scholar] [CrossRef]
- Jakicic, J.M.; Marcus, M.; Gallagher, K.I.; Randall, C.; Thomas, E.; Goss, F.L.; Robertson, R.J. Evaluation of the SenseWear Pro Armband™ to assess energy expenditure during exercise. Med. Sci. Sports Exerc. 2004, 36, 897–904. [Google Scholar] [CrossRef]
- Koehler, K.; Drenowatz, C. Monitoring Energy Expenditure Using a Multi-Sensor Device—Applications and Limitations of the SenseWear Armband in Athletic Populations. Front. Physiol. 2017, 8, 983. [Google Scholar] [CrossRef]
- Gastin, P.B.; Cayzer, C.; Dwyer, D.; Robertson, S. Validity of the ActiGraph GT3X+ and BodyMedia SenseWear Armband to Estimate Energy Expenditure during Physical Activity and Sport. J. Sci. Med. Sport 2018, 21, 291–295. [Google Scholar] [CrossRef] [PubMed]
- van Hoye, K.; Mortelmans, P.; Lefevre, J. Validation of the SenseWear Pro3 Armband Using an Incremental Exercise Test. J. Strength Cond. Res. 2014, 28, 2806–2814. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M. Validation of The Bodymedia Mini Armband to Estimate Energy Expenditure of Female Basketball Players during Variable Intensity Game-like Conditions. Doctoral Dissertation, University of Pittsburgh, Pittsburgh, PA, USA, 2014. [Google Scholar]
- Zanetti, S.; Pumpa, K.L.; Wheeler, K.W.; Pyne, D.B. Validity of the SenseWear Armband to Assess Energy Expenditure During Intermittent Exercise and Recovery in Rugby Union Players. J. Strength Cond. Res. 2014, 28, 1090–1095. [Google Scholar] [CrossRef] [PubMed]
- Arvidsson, D.; Slinde, F.; Larsson, S.; Hulthén, L. Energy Cost of Physical Activities in Children: Validation of SenseWear Armband. Med. Sci. Sports Exerc. 2007, 39, 2076–2084. [Google Scholar] [CrossRef] [PubMed]
- Drenowatz, C.; Eisenmann, J.C. Validation of the SenseWear Armband at High Intensity Exercise. Eur. J. Appl. Physiol. 2011, 111, 883–887. [Google Scholar] [CrossRef]
- Koehler, K.; Braun, H.; De Marées, M.; Fusch, G.; Fusch, C.; Schaenzer, W. Assessing Energy Expenditure in Male Endurance Athletes: Validity of the SenseWear Armband. Med. Sci. Sports Exerc. 2011, 43, 1328–1333. [Google Scholar] [CrossRef] [PubMed]
- Hiiloskorpi, H.; Pasanen, M.; Fogelholm, M.; Laukkanen, R.; Manttari, A. Use of Heart Rate to Predict Energy Expenditure from Low to High Activity Levels. Int. J. Sports Med. 2003, 24, 332–336. [Google Scholar] [CrossRef]
- Margaria, R.; Cerretelli, P.; Aghemo, P.; Sassi, G. Energy Cost of Running. J. Appl. Physiol. 1963, 18, 367–370. [Google Scholar] [CrossRef]
- George, J.D.; Stone, W.J.; Burkett, L.N. Non-Exercise V02max Estimation for Physically Active College Students. Med. Sci. Sports Exerc. 1997, 29, 415–423. [Google Scholar] [CrossRef]
- Liguori, G. ACSM’s Guidelines for Exercise Testing and Prescription (American College of Sports Medicine), 11th ed.; Lippincott: New York, NY, USA, 2021; ISBN 978-1-975150-18-1. [Google Scholar]
- Holm, S. A Simple Sequentially Rejective Multiple Test Procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Rosenthal, R. Effect Sizes: Pearson’s Correlation, Its Display via the BESD, and Alternative Indices. Am. Psychol. 1991, 46, 1086–1087. [Google Scholar] [CrossRef]
- Sawilowsky, S.S. New Effect Size Rules of Thumb. J. Mod. Appl. Stat. Methods 2009, 8, 597–599. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.G.; Quintana-Ascencio, P.F. A Solution to Minimum Sample Size for Regressions. PLoS ONE 2020, 15, e0229345. [Google Scholar] [CrossRef] [PubMed]
- Bhammar, D.M.; Sawyer, B.J.; Tucker, W.J.; Lee, J.-M.; Gaesser, G.A. Validity of SenseWear® Armband v5.2 and v2.2 for Estimating Energy Expenditure. J. Sports Sci. 2016, 34, 1830–1838. [Google Scholar] [CrossRef] [PubMed]
- Fruin, M.L.; Rankin, J.W. Validity of a Multi-Sensor Armband in Estimating Rest and Exercise Energy Expenditure. Med. Sci. Sports Exerc. 2004, 36, 1063–1069. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.A.; Laurson, K.R. Validity of the SenseWear Armband Step Count Measure during Controlled and Free-Living Conditions. J. Exerc. Sci. Fit. 2015, 13, 16–23. [Google Scholar] [CrossRef] [PubMed]
- O’Driscoll, R.; Turicchi, J.; Beaulieu, K.; Scott, S.; Matu, J.; Deighton, K.; Finlayson, G.; Stubbs, J. How Well Do Activity Monitors Estimate Energy Expenditure? A Systematic Review and Meta-Analysis of the Validity of Current Technologies. Br. J. Sports Med. 2020, 54, 332–340. [Google Scholar] [CrossRef]
- Cornacchia, M.; Ozcan, K.; Zheng, Y.; Velipasalar, S. A Survey on Activity Detection and Classification Using Wearable Sensors. IEEE Sens. J. 2017, 17, 386–403. [Google Scholar] [CrossRef]
- Hedayatrad, L.; Stewart, T.; Duncan, S. Concurrent Validity of ActiGraph GT3X+ and Axivity AX3 Accelerometers for Estimating Physical Activity and Sedentary Behavior. J. Meas. Phys. Behav. 2020, 4, 1–8. [Google Scholar] [CrossRef]
- Jones, A.M.; Vanhatalo, A.; Burnley, M.; Morton, R.H.; Poole, D.C. Critical Power: Implications for Determination of VO2max and Exercise Tolerance. Med. Sci. Sports Exerc. 2010, 42, 1876–1890. [Google Scholar] [CrossRef] [PubMed]
- Gaesser, G.A.; Poole, D.C. The Slow Component of Oxygen Uptake Kinetics in Humans. Exerc. Sport Sci. Rev. 1996, 24, 35–71. [Google Scholar] [CrossRef] [PubMed]
- Manns, P.J.; Haennel, R.G. SenseWear Armband and Stroke: Validity of Energy Expenditure and Step Count Measurement during Walking. Stroke Res. Treat. 2012, 2012, 247165. [Google Scholar] [CrossRef] [PubMed]
- Cabarkapa, D.V.; Cabarkapa, D.; Philipp, N.M.; Fry, A.C. Impact of the Anatomical Accelerometer Placement on Vertical Jump Performance Characteristics. Sports 2023, 11, 92. [Google Scholar] [CrossRef] [PubMed]
- Andre, D.; Pelletier, R.; Farringdon, J.; Safier, S.; Talbott, W.; Stone, R.; Vyas, N.; Wolf, D.; Vishnubhatla, S.; Boehmke, S.; et al. The Development of the SenseWear® Armband, a Revolutionary Energy Assessment Device to Assess Physical Activity and Lifestyle; Body Media, Inc.: Pittsburgh, PA, USA, 2006; pp. 1–19. [Google Scholar]
- Henriksen, A.; Haugen Mikalsen, M.; Woldaregay, A.Z.; Muzny, M.; Hartvigsen, G.; Hopstock, L.A.; Grimsgaard, S. Using Fitness Trackers and Smartwatches to Measure Physical Activity in Research: Analysis of Consumer Wrist-Worn Wearables. J. Med. Internet Res. 2018, 20, e110. [Google Scholar] [CrossRef] [PubMed]
- Black, K.E.; Baker, D.F.; Sims, S.T. Nutritional Needs of the Female Athlete: Risk and Prevention of Low Energy Availability. Strength Cond. J. 2020, 42, 77–81. [Google Scholar] [CrossRef]
- Colak, M.; Ayan, I.; Dal, U.; Yaroglu, T.; Dag, F.; Yilmaz, C.; Beydagi, H. Anterior Cruciate Ligament Reconstruction Improves the Metabolic Energy Cost of Level Walking at Customary Speeds. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1271–1276. [Google Scholar] [CrossRef]
- Waters, R.L.; Mulroy, S. The Energy Expenditure of Normal and Pathologic Gait. Gait Posture 1999, 9, 207–231. [Google Scholar] [CrossRef]

| IC (kcal) | SWA (kcal) | Mean Difference | Effect Size | p-Value | ICC [95% CI] | |
|---|---|---|---|---|---|---|
| Pref Walk | 3.44 ± 1.00 | 5.06 ± 1.44 | 1.62 ± 1.02 | 1.59 | <0.01 | 0.53 [−0.24, 0.84] |
| 75% Run | 10.30 ± 2.40 | 11.35 ± 2.06 | 1.05 ± 1.68 | 0.63 | 0.01 | 0.79 [0.40, 0.92] |
| 85% Run | 11.71 ± 3.11 | 11.65 ± 2.30 | 0.05 ± 2.42 | 0.02 | 0.92 | 0.76 [0.39, 0.91] |
| 95% Run | 12.60 ± 2.61 | 11.74 ± 1.97 | 0.86 ± 1.97 | 0.43 | 0.07 | 0.76 [0.39, 0.90] |
| Total | 284.95 ± 56.27 | 313.43 ± 54.46 | 28.48 ± 34.43 | 0.83 | <0.01 | 0.84 [0.35, 0.95] |
| Models | Statistical Test | Pref Walk | 75% Run | 85% Run | 95% Run | Total EE |
|---|---|---|---|---|---|---|
| SWA | R2 | 0.50 | 0.53 | 0.40 | 0.44 | 0.65 |
| Adj R2 | 0.47 | 0.50 | 0.37 | 0.41 | 0.63 | |
| SEE | 0.72 | 1.70 | 2.47 | 2.01 | 34.14 | |
| AICc | −10.30 | 28.63 | 39.99 | 36.85 | 144.96 | |
| SWA + HR | R2 | 0.50 | 0.56 | 0.41 | 0.53 | 0.68 |
| Adj R2 | 0.44 | 0.50 | 0.34 | 0.47 | 0.64 | |
| SEE | 0.74 | 1.69 | 2.53 | 1.90 | 33.87 | |
| AICc | −7.61 | 29.92 | 42.79 | 37.30 | 144.03 | |
| SWA + speed | R2 | 0.51 | 0.56 | 0.46 | 0.63 | 0.69 |
| Adj R2 | 0.45 | 0.51 | 0.39 | 0.58 | 0.66 | |
| SEE | 0.74 | 1.68 | 2.42 | 1.69 | 32.93 | |
| AICc | −8.07 | 29.31 | 41.62 | 32.61 | 144.15 | |
| SWA + HR + speed | R2 | 0.51 | 0.57 | 0.47 | 0.63 | 0.70 |
| Adj R2 | 0.42 | 0.49 | 0.37 | 0.57 | 0.64 | |
| SEE | 0.76 | 1.71 | 2.47 | 1.72 | 33.72 | |
| AICc | −4.10 | 32.13 | 42.72 | 27.98 | 145.78 |
| Preferred Walk | Regression Equation | ICC [95%CI] |
|---|---|---|
| SWA † | EE = 0.980 + 0.486 × SWA | 0.81 [0.50, 0.92] |
| SWA + HR | EE = 0.702 + 0.471 × SWA + 0.004 × HR | 0.81 [0.51, 0.93] |
| SWA + SP | EE = 0.406 + 0.473 × SWA + 0.497 × SP | 0.82 [0.53, 0.93] |
| SWA + HR + SP | EE = 0.394 + 0.472 × SWA + 0.001 × HR + 0.490 × SP | 0.82 [0.53, 0.93] |
| 75% Run | ||
| SWA † | EE = 0.844 + 0.189 × SWA | 0.82 [0.55, 0.93] |
| SWA + HR | EE = 6.183 + 0.782 × SWA − 0.031 × HR | 0.84 [0.59, 0.94] |
| SWA + SP | EE = −2.725 + 0.796 × SWA + 1.041 × SP | 0.84 [0.60, 0.94] |
| SWA + HR + SP | EE = 1.475 + 0.772 × SWA − 0.019 × HR + 1.021 × SP | 0.85 [0.61, 0.94] |
| 85% Run | ||
| SWA † | EE = 1.736 + 0.856 × SWA | 0.75 [0.33, 0.89] |
| SWA + HR | EE = 4.126 + 0.846 × SWA − 0.014 × HR | 0.74 [0.33, 0.90] |
| SWA + SP | EE = −4.138 + 0.812 × SWA + 1.953 × SP | 0.78 [0.43, 0.91] |
| SWA + HR + SP | EE = 2.037 + 0.799 × SWA − 0.028 × HR + 1.595 × SP | 0.78 [0.43, 0.91] |
| 95% Run | ||
| SWA | EE = 2.241 + 0.882 × SWA | 0.77 [0.40, 0.91] |
| SWA + HR | EE = 9.810 + 0.828 × SWA − 0.041 × HR | 0.89 [0.71, 0.96] |
| SWA + SP | EE = −6.691 + 0.793 × SWA + 2.706 × SP | 0.88 [0.68, 0.95] |
| SWA + HR + SP † | EE = −2.813 + 0.784 × SWA − 0.015 × HR + 2.369 × SP | 0.88 [0.69, 0.95] |
| Total | ||
| SWA | EE = 23.608 + 0.834 × SWA | 0.90 [0.74, 0.96] |
| SWA + HR † | EE = 135.185 + 0.786 × SWA − 0.680 × HR | 0.90 [0.74, 0.96] |
| SWA + SP | EE = −81.181 + 0.774 × SWA + 44.484 × SP | 0.91 [0.76, 0.96] |
| SWA + HR + SP | EE = −10.143 + 0.763 × SWA − 0.320 × HR + 36.656 × SP | 0.91 [0.76, 0.96] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wedge, R.D.; McCammon, M.; Meardon, S.A. Accuracy of the SenseWear Armband during Short Bouts of Exercise. Sports 2024, 12, 93. https://doi.org/10.3390/sports12040093
Wedge RD, McCammon M, Meardon SA. Accuracy of the SenseWear Armband during Short Bouts of Exercise. Sports. 2024; 12(4):93. https://doi.org/10.3390/sports12040093
Chicago/Turabian StyleWedge, Ryan D., Mike McCammon, and Stacey A. Meardon. 2024. "Accuracy of the SenseWear Armband during Short Bouts of Exercise" Sports 12, no. 4: 93. https://doi.org/10.3390/sports12040093
APA StyleWedge, R. D., McCammon, M., & Meardon, S. A. (2024). Accuracy of the SenseWear Armband during Short Bouts of Exercise. Sports, 12(4), 93. https://doi.org/10.3390/sports12040093






